Abstract
Parasitic lung diseases are caused by a number of parasites as a result of transient passage in the lung or as a result of an immunologic reaction. The clinical presentation may be in the form of focal or cystic lesions, pleural effusion or diffuse pulmonary infiltrates. With increasing globalisation, it is important to consider parasitic infections in the differential diagnosis of lung diseases. This is particularly important since early identification and prompt therapy result in full cure of these conditions. In this review, we summarise the most common parasitic lung diseases.
Short abstract
Parasitic lung diseases are not uncommon and should be considered not only in people in endemic areas but also in returning travellers and immigrants. https://bit.ly/3Dc1d1p
Introduction
Parasitic lung diseases are selective diseases caused by a number of parasites. They may be related to the transient passage of the parasites in the lung or as a result of an immunological disease. Since parasites are usually a cause of disease among residents of developing countries, parasitic lung diseases are normally seen in these countries. However, globalisation, increased international travel and immigration may lead to the presentation of patients in well-developed countries as well [1]. In this review, we summarise the most common forms of parasitic lung diseases.
Pattern of parasitic lung disease
The most common causes of parasitic lung disease are listed in table 1. The clinical presentation of such patients may be in the form of focal or cystic lesions, coin-like, consolidation, pleural effusion, diffuse or transient pulmonary infiltrates, or alveolar or interstitial lung changes [2]. The most common routes of transmission of common pulmonary parasites are shown in figure 1. A wide range of parasites cause disease in humans and include nematodes, trematodes, cestodes and protozoa (table 1).
TABLE 1.
Summary of common parasitic lung diseases
| Nematodes | Trematodes | Cestodes | Protozoa |
| Ascariasis: Ascaris lumbricoides Ancylostomiasis: Ancylostoma duodenale and Necator americanus Strongyloidiasis: Strongyloides stercoralis Tropical pulmonary eosinophilia: Wuchereria bancrofti |
Schistosomiasis: Schistosoma haematobium and Schistosoma japonicum Paragonimiasis: Paragonimus westermani |
Hydatid cyst: Echinococcus granulosus and Echinococcus multilocularis | Amoebiasis: Entamoeba histolytica Leishmaniasis (ibaba): Leishmania donovani Malaria: Plasmodium vivax, Plasmodium falciparum, Plasmodium malariae, Plasmodium ovale and Plasmodium knowlesi Toxoplasmosis: Toxoplasma gondii Babesiosis: Babesia microti |
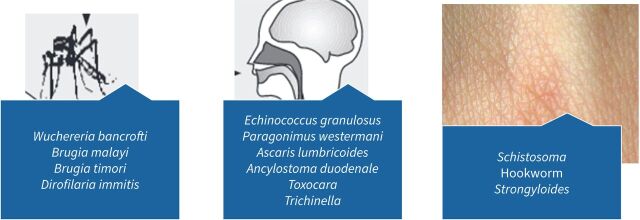
FIGURE 1.
Route of transmission of common lung parasites.
Parasitic eosinophilic lung disease
There are three types of parasitic eosinophilic lung disease, as shown in figure 2. These are Loeffler's syndrome, tropical eosinophilia syndrome (TES) and visceral larva migrans.
FIGURE 2.
Common manifestations of parasitic eosinophilic lung disease.
Loeffler's syndrome
The term Loeffler's syndrome denotes two different syndromes: transient eosinophilic pulmonary infiltrate and eosinophilia with endocarditis or myositis, thus causing some confusion [3]. This confusion is compounded by the subsequent classifications of the causes of Loeffer's syndrome: idiopathic, drugs or infections.
The initial syndrome was associated with pulmonary infiltrates and peripheral eosinophilia as a result of transbronchial migration of Ascaris species [3]. Additionally, the syndrome may result from a hypersensitivity reaction to the transient parasitic immigration into the lungs. It is also known as simple pulmonary eosinophilia as it lacks pulmonary symptoms or is only associated with mild symptoms [4]. It is characterised by a transient pulmonary infiltrate that spontaneously resolves within 2–4 weeks. Patients may have peripheral eosinophilia [2], severe bronchospasm, fatigue and fever [5]. It is more common in children than adults. The syndrome is associated with disruption of the respiratory epithelium, ciliastasis, mucus production and a significant release of platelet activating factor and leukotrienes, which in turn lead to bronchospasm and diffuse lung infiltrate. The major causes of Loeffler's syndrome are Ascaris lumbricoides, Ancylostoma duodenale, Necator americanus and Strongyloides stercoralis [5]. A special form of Loeffler's syndrome is caused by S. stercoralis in immunocompromised patients, such as those on steroid treatment with superinfection [6], and may be associated with Gram-negative bacteraemia.
Diagnosis is based on clinical suspicion as well as demonstration of the parasitic eggs of Ascaris lumbricoides, Ancylostoma duodenale or N. americanus in stool, or of the larva of S. stercoralis in stool, sputum or bronchoalveolar lavage [3]. Treatment is either mebendazole 100 mg orally twice daily for 3 days or albendazole (for children >2 years) 400 mg·day−1 for 3 days [5]. For S. stercoralis with superinfection, the treatment is albendazole 400 mg orally twice daily for 7 days or ivermectin 200 μg·kg−1 orally once daily for 1–2 days [6, 7].
TES
TES is a type of hypersensitivity reaction to a few parasitic agents. The reaction is usually directed towards microfilaria of W. bancrofti and Brugia malayi. Tropical pulmonary eosinophilia (TPE) was first described by Weingarten [8] in 1943 and was initially called “pseudotuberculosis with eosinophilia” [9]. Other names include filarial tropical pulmonary eosinophilia [10]. W. bancrofti, B. malayi and Brugia timori are the aetiologic agents of lymphatic filariasis and are transmitted to humans through different mosquitos, such as Anopheles, Aedes, Culex, Mansonia and Ochlerotatus [11]. Lymphatic filariasis occurs mainly in the tropics and sub-tropics with highest transmission in Central and Latin America, Africa (west, coastal east and southern parts), India, Southeast Asia, Indonesia, Papua New Guinea and the western Pacific [11]. It was indicated that transmission increases with high rainfall and temperature, the growth of certain types of vegetation, and high population density and decreases at high altitudes [11].
TES occurs in only a small fraction (<0.5–1.0%) of patients infected with filaria and has a male predominance of 4:1 [1]. The disease occurs in Southeast Asia, China, India and Africa and may occur outside those geographic areas among immigrants or visitors [12]. The syndrome is slow in onset and occurs over many months. It is characterised by the occurrence of cough, dyspnoea and wheezing associated with systemic symptoms such as fever, malaise and weight loss. The exact pathophysiology of TES is not known, but it is thought that an increased IgE immune response to a filarial antigen known as G-glutamyl transpeptidase (gGT) may lead to a higher risk of TES [13]. The levels of gGT-specific IgE/IgG4 ratio were 45 and 107 in patients with TES and those who live in the tropics without TES [13]. In addition, acidic calcium-independent phospholipase A2 was found to be a master regulator of TPE pathogenesis [14].
The diagnosis of TES/TPE relies on a constellation of findings, which include being a resident of or coming from a filaria endemic area, the presence of blood eosinophilia, the absence of peripheral microfilariae, high antifilarial antibody titres and serum IgE level, as well as a clinical response to diethylcarbamazine (DEC) [13]. TPE may also mimic asthma but is associated with an eosinophilic count of >3×109 cells and a high IgE level of >1000 IU·mL−1 [15]. Diagnosis of TPS is based on the presence of IgG and IgM antifilaria antibodies.
One study found the following sensitivities: filarial antibody test 30%, radiological changes 45.5% and erythrocyte sedimentation rate 80% [16]. The authors proposed the following for the diagnosis of TPS: worsening cough at night, residence in a filarial endemic area, presence of an eosinophil count >3300 cells·mm−3 and a clinical and haematological response to DEC [16]. Another study showed high levels of filarial-specific IgG, IgM and IgE [17]. In a study of 12 patients, the main computed tomography (CT) scan finding was widespread ill-defined bronchocentric nodules [18]. In acute TPE, a mild-to-moderate obstructive pattern is usually observed, and chronic cases may show a restrictive pattern [1].
Therapy usually requires DEC for 3 weeks and is associated with a 20–40% failure rate in those with chronic disease [19], which may be related to inadequate treatment or advanced disease [1]. Residual airway inflammation and reduction of lung function after DEC therapy may be observed and can be treated with a course of corticosteroid or other potent anti-inflammatory agents [19, 20].
Visceral larva migrans
Pulmonary involvement in the case of visceral larva migrans is mainly associated with the migrating larva of Toxocara canis, but might also be caused by Ascaris suum or Toxocara catis [21]. Patients present with cough, wheezing, acute bronchiolitis, asthma and acute pneumonia with or without eosinophilia, and other symptoms related to allergic and inflammatory responses [22]. These symptoms are seen in about 80% of patients with visceral larva migrans [23]. Secondary chronic eosinophilic pneumonia may also develop [24]. Radiography may show nonspecific calcified nodules suggesting old Mycobacterium tuberculosis or other nontuberculous infection (figure 1). The appearance on a CT scan could be multifocal subpleural nodules with halo or ground-glass opacities and ill-defined margins [21] (figure 3). In patients with pulmonary visceral larva migrans due to A. suum, a high-resolution CT scan showed multiple nodules (57%) and nodular ground-glass opacities (29%) [25]. Similar findings were also reported in another study [26]. Diagnosis relies on serum enzyme-linked immunosorbent assay (ELISA) of antibodies directed towards the larva of these worms [27].
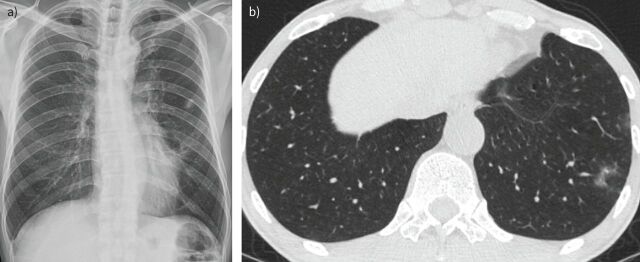
FIGURE 3.
a) Nonspecific calcified nodules suggesting old Mycobacterium tuberculosis or other nontuberculous infection in the left upper lobe in an asymptomatic patient. b) Chest computed tomography (CT) scan of the same patient after 13 months, he was asymptomatic and the follow-up CT showed multifocal ill-defined ground-glass or solid nodular lesions in both lungs.
Pulmonary schistosomiasis
The burden of schistosomiasis is significant, with an estimated 200 million infected people globally, mainly in low- and middle-income countries such as Africa, parts of Asia and South America [28]. Schistosoma may cause an acute or a chronic pulmonary disease or the lung could be involved in Katayama fever [29]. Acute and chronic schistosomiasis results in nodular pulmonary lesions and the disease is likely related to eggs laid by adult worms during their migration in the chronic phase. In addition, the pulmonary nodules formed during Katayama fever (syndrome) are secondary to a systemic immune-allergic reaction [29]. The distinction between acute and chronic schistosomiasis is based on an arbitrary cut-off time frame of 10–12 weeks from the time of exposure [30]. Acute schistosomiasis (Katayama fever) usually occurs among nonimmune travellers and is associated with fever, malaise, fatigue, headache, cough, abdominal pain and urticarial rash [29, 30]. The disease is related to the migration, maturation and egg-production of schistosomal larva [31], and subsequent immunological reactions [31].
Radiographic manifestations may include distinct nodules, ground-glass opacities and mass-like lesions [32]. The diagnosis relies on finding schistosome eggs in stool, urine or tissue biopsy samples [32]. However, in Katayama fever the diagnosis can also be established by serum PCR if urine and stool samples are negative for Schistosoma eggs [33].
One of the manifestations of schistosomiasis is schistosomiasis-induced pulmonary arterial hypertension (SchPAH) [34]. SchPAH is considered a global disease due to the high prevalence of schistosomiasis [35–37], with a prevalence of 5% among those chronically infected with schistosomes [38] and 5–30% in patients with hepatosplenic schistosomiasis secondary to Schistosoma mansoni [39–41]. Another study showed that SchPAH results in 30.8% of all cases of pulmonary hypertension in endemic areas [42]. In a retrospective study from China, only 10 out of 18 829 (0.053%) people with schistosomiasis had pulmonary hypertension diagnosed by echocardiography [43]. Other parasitic causes of pulmonary hypertension include W. bancrofti, Clonorchis sinensis in southeast Asia and Echinococcus (hydatid cysts) [44]. There are three possible explanations for the development of SchPAH: Schistosoma eggs obstructing pulmonary vasculature, schistsomal egg embolisation from portopulmonary hypertension and the development of inflammatory vasculopathy [38]. Pulmonary schistosomiasis is more common from S. mansoni and Schistosoma japonicum. It was found that S. japonicum caused milder SchPAH than that caused by S. mansoni in an animal model, which was thought to be due to the uniform versus clustered distribution of eggs laid by S. mansoni and S. japonicum, respectively [45]. In an experimental study, S. japonicum resulted in 35-fold smaller granulomas than those caused by S. mansoni due to attenuated type 2 inflammation [45].
The pathogenesis of SchPAH is thought to be related to angiogenesis. Thus, inhibition of angiogenesis by the use of bevacizumab was associated with less angiogenesis in a mouse model [46]. Current therapies for SchPAH rely on nitric oxide pathway inhibitors such as phosphodiesterase type 5 inhibitors (sildenafil and tadalafil), soluble guanylyl cyclase stimulators (riociguat), endothelian receptor antagonists (bosentan, ambrisentan and macitentan) and prostacyclin analogues (epoprostenol, treprostinil, iloprost, and the nonprostanoid IP-receptor agonist selexipag), as fully described by Sibomana et al. [47]. Experience has shown that phosphodiesterase type 5 inhibitors improve symptoms and may also increase survival rates [48].
Other Schistosoma-associated pulmonary diseases include spontaneous pneumothorax [49], hydropneumothorax with pleural thickening [32] and nodular pulmonary lesions [50]. The latter can be acute in the case of travellers or chronic in residents of endemic areas [50]. A metabolically active pulmonary nodule with 18F-fluorodeoxyglucose positron emission tomography/CT has been described in relation to schistosomiasis [51].
Paragonimiasis-associated pleural effusion
The most common species associated with paragonimiasis are Paragonimus westermani, Paragonimus miyazakii, Paragonimus mexicanus and Paragonimus skrjabini [52]. After oral ingestion, adult Paragonimus parasites pass through multiple organs or tissues and then later reach pulmonary tissues from the small intestine [52]. Paragonimiasis may be associated with cystic lesions and nodules, and 20% of patients may have asymptomatic lesions [3]. Pleural effusion had been described specifically with paragonimiasis and was reported in 40–70% of patients and associated with eosinophilia [52]. However, paragonimiasis may also cause nodules, infiltrates and cavities [52] (figure 4). The most common radiographic finding is pleural effusion (associated with massive eosinophil infiltration) [53]. Although the classic presentation of Paragonimus infection is cavitary pulmonary lesion, this finding was seen in only 5% of patients [53]. One study of chest CT scans showed nodular opacities (56.4%) and worm migration tracks (18.1%) [54]. A rare presentation of Loeffler's syndrome was also described with P. westermani [55].
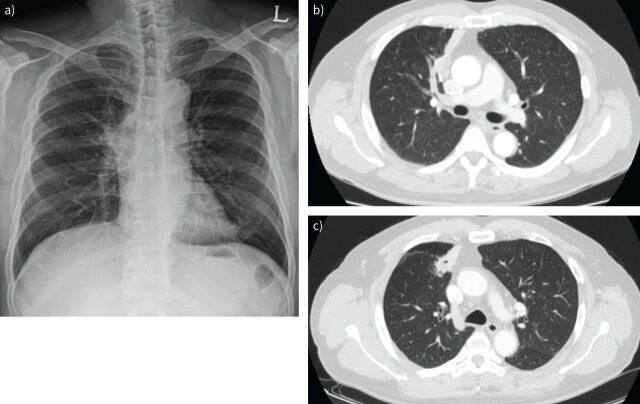
FIGURE 4.
a) Posterior–anterior chest radiograph showing right hilar prominence in a patient with Paragonimus infection. b) Chest computed tomography (CT) scan showing a necrotic consolidation with bronchial cut-off at the right upper lobe anterior segment, suggesting infection/inflammation such as tuberculosis, actinomycosis, pneumonia and less likely a lung cancer in the same patient with Paragonimus infection. c) Follow-up chest CT scan after 8 months of therapy with antibiotics and antifungal therapy showing no improvements and cavitation.
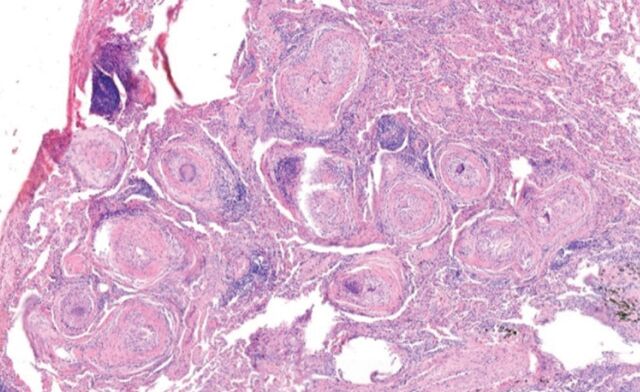
The diagnosis of paragonimiasis relies on detection of Paragonimus eggs in stools, sputum, bronchoalveolar lavage fluid or pleural effusion [53], but this is only seen in a minority (11.7%) of patients. The most widely used serology for the diagnosis of Paragonimus infection is indirect ELISA with a significant cross-reaction with schistosomiasis, fascioliasis and clonorchiasis [56]. Histopathology of tissue may exhibit chronic granulomatous inflammation with numerous parasitic eggs consistent with paragonimiasis (figure 5). The treatment relies on the use of biltricide orally at a dose of 25 mg·kg−1 three times a day for 3 days [57]. A surgical approach is also considered in patients with severe pleural or pleuro-parenchymal pulmonary disease [58].
FIGURE 5.
Histopathology of tissue showing chronic granulomatous inflammation with numerous parasitic eggs consistent with paragonimiasis.
Pulmonary amebiasis
Entamoeba histolytica is the aetiologic agent of amebiasis and causes intestinal and extraintestinal manifestations including liver and pulmonary amebiasis. It was estimated that 7–20% of patients with liver amebiasis and 2–3% of those with invasive disease also have pleural effusion, lung abscesses or pleural empyema [59]. Amebiasis has also been found to cause empyema and vena cava obstruction [60, 61].
Pulmonary hydatid disease
The larvae of Echinococcus species, especially Echinococcus granulosus, are the aetiologic agent of hydatid disease [2]. The disease was reported in South America, the Mediterranean region, the Middle East, sub-Saharan Africa, Russia and China and its prevalence was estimated to be up to 79 cases per 100 000 people [62]. Pulmonary hydatid disease accounts for 20–30% of hydatid disease [63, 64].
The main presentation is incidental findings on radiography; however, symptoms such as cough, haemoptysis, chest pain or pneumothorax may occur [2]. Radiographic presentations of pulmonary hydatid disease differ between E. granulosus and Echinococcus multilocularis. Hydatid disease due to E. granulosus causes smooth margin, noncalcified nodules or masses when the cysts are not ruptured [65]. On the other hand, E. multilocularis causes alveolar echinococcosis and radiographically presents as lobulated nodules or masses and calcification [66]. The main radiographic characteristics of hydatid cysts are meniscus sign, crescent sign, Cumbo's sign, onion peel sign, water lily sign and mass-within-a-cavity sign [67, 68]. One of the classical radiograph signs of hydatid cysts is the presence of a well-defined round radio-opacity in the lung with or without calcification (figure 6). Hydatid disease of the lung may become secondarily infected and on chest radiography may present with a cyst and an air fluid level (figure 7).
FIGURE 6.

Plain chest radiograph showing a well-defined round radio-opacity in the left lower zone.
FIGURE 7.

Lateral radiograph of the chest showing air fluid level within a pre-existing hydatid cyst suggesting superimposed infections.
Treatment relies on surgical excision of the cyst with or without lung tissue resection [69]. In a systematic review, the use of uni-portal video-assisted thoracoscopic surgery was associated with an overall complication rate of 9.35% and no reported recurrence [69]. Generally, surgical removal of pulmonary hydatid cysts is associated with low morbidity and mortality [70]. One study of 12 patients with pulmonary hydatid disease showed a cure rate of 72% and there was no change in 18% patients using albendazole (800 mg·day−1) for four courses with each course lasting 28 days followed by 14 days drug free [71]. The use of albendazole is not recommended pre-operatively due to thinning of the capsule but it is used post-operatively [64, 72] as surgical therapy and is associated with a high recurrence rate of 25% [73]. In one study, pre-operative albendazole therapy was associated with a reduction in the tensile strength values of the cuticular membrane of the hydatid cysts [72].
One study showed a recurrence rate of 18.7% for those who did not receive albendazole versus 4.16% for those who had pre- and/or post-operative albendazole in liver disease [74]. On the other hand, children especially those with small cysts, young cysts or cysts with daughter cysts may respond well to albendazole therapy without surgery [75]. Needle aspiration of hydatid cysts with antiparasitic therapy before and after the aspiration has also been advocated [76]. One of the therapeutic techniques for hydatid cysts is the use of the percutaneous aspiration of cyst contents, installation of scolicidal agent and re-aspiration (PAIR) technique. This technique had been used with great success with the caveat of the possibility of risks associated with PAIR of pulmonary cysts [77].
Pulmonary dirofilariasis
This parasitic disease is caused by a filarial nematode called Dirofilaria immitis. Mosquitoes transmit the parasites from dogs to humans [78]. Dirofilariasis is diagnosed most commonly in the east coast and southern parts of the United States, with infrequent cases elsewhere in the world [78–82]. A recent study from the Balkan Peninsula reported that two of 46 cases of dirofilariasis were pulmonary infections [80]. The disease is usually asymptomatic and manifests as a solitary pulmonary nodule that requires surgical excision [78, 79]. The disease does not have specific radiographic or symptomatology that differentiates it from other solitary pulmonary lesions [79].
Pulmonary manifestations of malaria
Malaria is caused by Plasmodium falciparum, Plasmodium vivax, Plasmodium ovale and Plasmodium malariae and is transmitted by the Anopheles mosquito [83]. The main symptoms of malaria are fever, chills, sweating, cytopenia and splenomegaly. The most frequent pulmonary manifestation of malaria is acute respiratory distress syndrome and it is one of the criteria for severe and complicated malaria [67]. Other pulmonary manifestations include pleural effusion, interstitial oedema and consolidation [84–86]. Transient cough was described in 36% of patients with P. falciparum infection and in 53% of those with P. vivax or P. ovale infections [87]. In addition, subclinical airflow obstruction was also demonstrated by spirometry as well as the occurrence of impaired gas exchange [87]. Other manifestations included bronchiolitis obliterans organising pneumonia [88]. The diagnosis is usually made by identifying trophozoites or other parasitic forms within the erythrocytes in a thin blood smear or parasites in a thick smear. Serologic and nucleic acid amplification tests are also available.
Points for clinical practice
A number of parasites may cause pulmonary disease as a result of a transient passage in the lung or as a result of an immunological reaction.
The clinical presentation may be in the form of focal or cystic lesions, pleural effusion or diffuse pulmonary infiltrates.
Of particular interest are: Loeffler's syndrome, TES and visceral larva migrans.
Increasing globalisation may lead to the presentation of pulmonary lung disease in travellers and migrants.
Conclusion
The pulmonary involvement of different parasitic agents is well known globally. The most common manifestations involve radiographic abnormalities, with the possible occurrence of solitary pulmonary nodules. Other manifestations may reflect systemic involvements and it is important to recognise these symptoms for proper diagnosis and management, especially among travellers and migrants.
Acknowledgements
Authors thank Hamdan Aljahdali, King Abdulaziz Medical City, King Saud Bin Abdulaziz University of Health Sciences, Riyadh, Saudi Arabia for providing the chest radiographs (figures 6 and 7).
Provenance: Commissioned article, peer reviewed.
Previous articles in this series: No. 1: Kumar K, Daley CL, Griffith DE, et al. Management of Mycobacterium avium complex and Mycobacterium abscessus pulmonary disease: therapeutic advances and emerging treatments. Eur Respir Rev 2022; 31: 210212. No. 2: Cilloniz C, Luna CM, Hurtado JC, et al. Respiratory viruses: their importance and lessons learned from COVID-19. Eur Respir Rev 2022; 31: 220051. No. 3: Cavallazzi R, Ramirez JA. How and when to manage respiratory infections out of hospital. Eur Respir Rev 2022; 31: 220092. No. 4: Reynolds D, Burnham JP, Vazquez Guillamet C, et al. The threat of multidrug-resistant/extensively drug-resistant Gram-negative respiratory infections: another pandemic. Eur Respir Rev 2022; 31: 220068. No. 5: Puerta-Alcalde P, Garcia-Vidal C. Non-Aspergillus mould lung infections. Eur Respir Rev 2022; 31: 220104.
Number 6 in the Series “Respiratory infections” Edited by Antoni Torres and Michael S. Niederman
Conflict of interest: All authors have no conflicts of interest to disclose
References
- 1.Santeliz JV. Tropical pulmonary eosinophilia: an epidemiological and clinical review. Int J Respir Pulm Med 2019; 6: 102. doi: 10.23937/2378-3516/1410102 [DOI] [Google Scholar]
- 2.Kunst H, Mack D, Kon OM, et al. Parasitic infections of the lung: a guide for the respiratory physician. Thorax 2011; 66: 528–536. doi: 10.1136/thx.2009.132217 [DOI] [PubMed] [Google Scholar]
- 3.Pérez-Arellano JL, Andrade MA, López-Abán J, et al. Helminths and the respiratory system. Arch Bronconeumol 2006; 42: 81–91. doi: 10.1016/S1579-2129(06)60122-5 [DOI] [PubMed] [Google Scholar]
- 4.Fujimura J, Murakami Y, Tsuda A, et al. A neonate with Löffler syndrome. J Perinatol 2001; 21: 207–208. doi: 10.1038/sj.jp.7200507 [DOI] [PubMed] [Google Scholar]
- 5.Ribeiro JD, Fischer GB. Eosinophilic lung diseases. Paediatr Respir Rev 2002; 3: 278–284. doi: 10.1016/S1526-0542(02)00273-7 [DOI] [PubMed] [Google Scholar]
- 6.Shorman M, Al-Tawfiq JA. Strongyloides stercoralis hyperinfection presenting as acute respiratory failure and Gram-negative sepsis in a patient with astrocytoma. Int J Infect Dis 2009; 13: e288–e291. doi: 10.1016/j.ijid.2008.11.019 [DOI] [PubMed] [Google Scholar]
- 7.Rajapurkar M, Hegde U, Rokhade M, et al. Respiratory hyperinfection with Strongyloides stercoralis in a patient with renal failure. Nat Clin Pract Nephrol 2007; 3: 573–577. doi: 10.1038/ncpneph0598 [DOI] [PubMed] [Google Scholar]
- 8.Weingarten R J. Tropical eosinophilia. Lancet 1943; 1: 103–105. [Google Scholar]
- 9.Chitkara RK, Krishna G. Parasitic pulmonary eosinophilia. Semin Respir Crit Care Med 2006; 27: 171–184. doi: 10.1055/s-2006-939520 [DOI] [PubMed] [Google Scholar]
- 10.Joob B, Wiwanitkit V. Filarial tropical pulmonary eosinophilia. J Asthma 2020; 57: 230. doi: 10.1080/02770903.2018.1561892 [DOI] [PubMed] [Google Scholar]
- 11.Cano J, Rebollo MP, Golding N, et al. The global distribution and transmission limits of lymphatic filariasis: past and present. Parasit Vectors 2014; 7: 466. doi: 10.1186/s13071-014-0466-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boggild AK, Keystone JS, Kain KC. Tropical pulmonary eosinophilia: a case series in a setting of nonendemicity. Clin Infect Dis 2004; 39: 1123–1128. doi: 10.1086/423964 [DOI] [PubMed] [Google Scholar]
- 13.Lobos E, Nutman TB, Hothersall JS, et al. Elevated immunoglobulin E against recombinant Brugia malayi γ-glutamyl transpeptidase in patients with bancroftian filariasis: Association with tropical pulmonary eosinophilia or putative immunity. Infect Immun 2003; 71: 747–753. doi: 10.1128/IAI.71.2.747-753.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sharma P, Sharma A, Ganga L, et al. Acidic calcium-independent phospholipase A2 regulates eosinophil-mediated pathology during filarial manifestation of tropical pulmonary eosinophilia. J Immunol 2021; 206: 722–736. doi: 10.4049/jimmunol.2000604 [DOI] [PubMed] [Google Scholar]
- 15.Tsanglao WR, Nandan D, Chandelia S, et al. Filarial tropical pulmonary eosinophilia: a condition masquerading asthma, a series of 12 cases. J Asthma 2019; 56: 791–798. doi: 10.1080/02770903.2018.1490748 [DOI] [PubMed] [Google Scholar]
- 16.Cooray JHL, Ismail MM. Re-examination of the diagnostic criteria of tropical pulmonary eosinophilia. Respir Med 1999; 93: 655–659. doi: 10.1016/S0954-6111(99)90106-3 [DOI] [PubMed] [Google Scholar]
- 17.Nutman TB, Vijayan VK, Pinkston P, et al. Tropical pulmonary eosinophilia: analysis of antifilarial antibody localized to the lung. J Infect Dis 1989; 160: 1042–1050. doi: 10.1093/infdis/160.6.1042 [DOI] [PubMed] [Google Scholar]
- 18.Angirish B, Jankharia B, Sanghavi P. The role of HRCT in tropical pulmonary eosinophilia. Eur J Radiol 2020; 131: 109207. doi: 10.1016/j.ejrad.2020.109207 [DOI] [PubMed] [Google Scholar]
- 19.Madan M, Gupta P, Mittal R, et al. Tropical pulmonary eosinophilia: effect of addition of corticosteroids after failure of diethylcarbamazine therapy. Adv Respir Med 2017; 84: 51–54. doi: 10.5603/ARM.2017.0010 [DOI] [PubMed] [Google Scholar]
- 20.Vijayan VK, Sankaran K, Venkatesan P, et al. Effect of diethylcarbamazine on the alveolitis of tropical eosinophilia. Respiration 1991; 58: 255–259. doi: 10.1159/000195941 [DOI] [PubMed] [Google Scholar]
- 21.Sakai S, Shida Y, Takahashi N, et al. Pulmonary lesions associated with visceral larva migrans due to Ascaris suum or Toxocara canis: imaging of six cases. Am J Roentgenol 2006; 186: 1697–1702. doi: 10.2214/AJR.04.1507 [DOI] [PubMed] [Google Scholar]
- 22.Chitkara RK, Sarinas PSA. Dirofilaria, visceral larva migrans, and tropical pulmonary eosinophilia. Semin Respir Infect 1997; 12: 138–148. [PubMed] [Google Scholar]
- 23.Demirci M, Unlü M, Fidan F, et al. Eosinophilic pneumonia due to toxocariasis: an adult case report. Turkiye parazitolojii Derg 2012; 36: 258–259. doi: 10.5152/tpd.2012.61 [DOI] [PubMed] [Google Scholar]
- 24.Inoue K, Inoue Y, Arai T, et al. Chronic eosinophilic pneumonia due to visceral larva migrans. Intern Med 2002; 41: 478–482. doi: 10.2169/internalmedicine.41.478 [DOI] [PubMed] [Google Scholar]
- 25.Matsumoto N, Tsubouchi H, Setoguchi K, et al. Clinico-radiologic characteristics of pulmonary visceral larva migrans caused by Ascaris suum. Intern Med 2021; 60: 2899–2903. doi: 10.2169/internalmedicine.6109-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Okada F, Ono A, Ando Y, et al. Pulmonary computed tomography findings of visceral larva migrans caused by Ascaris suum. J Comput Assist Tomogr 2007; 31: 402–408. doi: 10.1097/01.rct.0000243444.18363.69 [DOI] [PubMed] [Google Scholar]
- 27.Khalil HM, Azab ME, Safar EH, et al. Immunodiagnostics of visceral toxocariasis. J Egypt Soc Parasitol 1989; 19: 381–393. [PubMed] [Google Scholar]
- 28.Dzudie A, Dzekem BS, Ojji DB, et al. Pulmonary hypertension in low- and middle-income countries with focus on sub-Saharan Africa. Cardiovasc Diagn Ther 2020; 10: 316–324. doi: 10.21037/cdt.2019.07.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gobbi F, Tamarozzi F, Buonfrate D, et al. New insights on acute and chronic schistosomiasis: do we need a redefinition? Trends Parasitol 2020; 36: 660–667. doi: 10.1016/j.pt.2020.05.009 [DOI] [PubMed] [Google Scholar]
- 30.Colley DG, Bustinduy AL, Secor WE, et al. Human schistosomiasis. Lancet 2014; 383: 2253–2264. doi: 10.1016/S0140-6736(13)61949-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Houlder EL, Costain AH, Cook PC, et al. Schistosomes in the lung: immunobiology and opportunity. Front Immunol 2021; 12: 635513. doi: 10.3389/fimmu.2021.635513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vadala R, Shamsi I, Dabral C, et al. Pleural schistosomiasis masquerading as tubercular pyopneumothorax: world's first case report. Lung India 2021; 38: 183–185. doi: 10.4103/lungindia.lungindia_232_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cnops L, Huyse T, Maniewski U, et al. Acute schistosomiasis with a Schistosoma mattheei×Schistosoma haematobium hybrid species in a cluster of 34 travelers infected in South Africa. Clin Infect Dis 2021; 72: 1693–1698. doi: 10.1093/cid/ciaa312 [DOI] [PubMed] [Google Scholar]
- 34.Posada-Martínez EL, Gonzalez-Barrera LG, Liblik K, et al. Schistosomiasis & Heart - On behalf of the neglected tropical diseases and other infectious diseases affecting the heart (the NET-Heart Project) [Esquistossomose e o coração – em nome das doenças tropicais negligenciadas e outras doenças infecciosas que afetam o coração (Projeto NET-Heart)]. Arq Bras Cardiol 2022; 118: 885–893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hoeper MM, Humbert M, Souza R, et al. A global view of pulmonary hypertension. Lancet Respir Med 2016; 4: 306–322. doi: 10.1016/S2213-2600(15)00543-3 [DOI] [PubMed] [Google Scholar]
- 36.Maarman GJ, Shaw J, Allwood B. Pulmonary hypertension in majority countries: opportunities amidst challenges. Curr Opin Pulm Med 2020; 26: 373–383. doi: 10.1097/MCP.0000000000000702 [DOI] [PubMed] [Google Scholar]
- 37.Rahaghi FN, Hilton JF, Corrêa RA, et al. Arterial vascular volume changes with haemodynamics in schistosomiasis-associated pulmonary arterial hypertension. Eur Respir J 2021; 57: 2003914. doi: 10.1183/13993003.03914-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mickael CS, Graham BB. The role of type 2 inflammation in Schistosoma-induced pulmonary hypertension. Front Immunol 2019; 10: 27doi: 10.3389/fimmu.2019.00027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.De Cleva R, Herman P, Pugliese V, et al. Prevalence of pulmonary hypertension in patients with hepatosplenic mansonic schistosomiasis – prospective study. Hepatogastroenterology 2003; 50: 2028–2030. [PubMed] [Google Scholar]
- 40.Barbosa MM, Lamounier JA, Oliveira EC, et al. Pulmonary hypertension in schistosomiasis mansoni. Trans R Soc Trop Med Hyg 1996; 90: 663–665. doi: 10.1016/S0035-9203(96)90424-1 [DOI] [PubMed] [Google Scholar]
- 41.Lapa M, Dias B, Jardim C, et al. Cardiopulmonary manifestations of hepatosplenic schistosomiasis. Circulation 2009; 119: 1518–1523. doi: 10.1161/CIRCULATIONAHA.108.803221 [DOI] [PubMed] [Google Scholar]
- 42.Nunes MCP, Guimarães MH, Diamantino AC, et al. Cardiac manifestations of parasitic diseases. Heart 2017; 103: 651–658. doi: 10.1136/heartjnl-2016-309870 [DOI] [PubMed] [Google Scholar]
- 43.Deng Q, Hu B, Zhang Y, et al. Suspected myocardial injury in patients with COVID-19: evidence from front-line clinical observation in Wuhan, China. Int J Cardiol 2020; 311: 116–121. doi: 10.1016/j.ijcard.2020.03.087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Butrous G. Pulmonary vascular diseases associated with infectious disease—schistosomiasis and human immunodeficiency viruses. Clin Chest Med 2021; 42: 71–80. doi: 10.1016/j.ccm.2020.11.007 [DOI] [PubMed] [Google Scholar]
- 45.Kassa B, Lee MH, Kumar R, et al. Experimental Schistosoma japonicum-induced pulmonary hypertension. PLoS Negl Trop Dis 2022; 16: e0010343. doi: 10.1371/journal.pntd.0010343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Saad MA H, El-Anwar N. Bevacizumab as a potential anti-angiogenic therapy in schistosomiasis: a double-edged, but adjustable weapon. Parasite Immunol 2020; 42: e12724. doi:http://doi.org/ [DOI] [PubMed] [Google Scholar]
- 47.Sibomana JP, Campeche A, Carvalho-Filho RJ, et al. Schistosomiasis pulmonary arterial hypertension. Front Immunol 2020; 11: 608883. doi: 10.3389/fimmu.2020.608883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ferrari TCA, Albricker ACL, Gonçalves IM, et al. Schistosome-associated pulmonary arterial hypertension: a review emphasizing pathogenesis. Front Cardiovasc Med 2021; 8: 724254 doi: 10.3389/fcvm.2021.724254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bamefleh H, Al-Hussain GO. Secondary spontaneous pneumothorax caused by pulmonary schistosomiasis. Cureus 2021; 13: e18709. doi: 10.7759/cureus.18709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mortier C, Aubry C, L'Ollivier C, et al. Schistosoma haematobium infection with pulmonary involvement in a traveller returning from Congo: a case report and systematic review of literature on nodular pulmonary schistosomiasis. Travel Med Infect Dis 2021; 44: 102182. doi: 10.1016/j.tmaid.2021.102182 [DOI] [PubMed] [Google Scholar]
- 51.Cimini A, Ricci M, Chiaravalloti A, et al. A rare case of pulmonary schistosomiasis: 18F-fluorodeoxyglucose positron emission tomography/computed tomography findings. Indian J Nucl Med 2020; 35: 336–338. doi: 10.4103/ijnm.IJNM_79_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nakamura-Uchiyama F, Mukae H, Nawa Y. Paragonimiasis: a Japanese perspective. Clin Chest Med 2002; 23: 409–420. doi: 10.1016/S0272-5231(01)00006-5 [DOI] [PubMed] [Google Scholar]
- 53.Nagayasu E, Yoshida A, Hombu A, et al. Paragonimiasis in Japan: a twelve-year retrospective case review (2001–2012). Intern Med 2015; 54: 176–186. doi: 10.2169/internalmedicine.54.1733 [DOI] [PubMed] [Google Scholar]
- 54.Li KK, Jin GY, Kwon KS. What findings on chest CTs can delay diagnosis of pleuropulmonary paragonimiasis? Tomography 2022; 8: 1493–1502. doi: 10.3390/tomography8030122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Furuya S, Fukui S, Maekawa Y, et al. Paragonimus westermani as a cause of Löeffler's syndrome. IDCases 2022; 27: e01427. doi: 10.1016/j.idcr.2022.e01427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Nakamura-Uchiyama F, Hiromatsu K, Ishiwata K, et al. The current status of parasitic diseases in Japan. Intern Med 2003; 42: 222–236. doi: 10.2169/internalmedicine.42.222 [DOI] [PubMed] [Google Scholar]
- 57.Yoshida A, Doanh PN, Maruyama H. Paragonimus and paragonimiasis in Asia: an update. Acta Trop 2019; 199: 105074. doi: 10.1016/j.actatropica.2019.105074 [DOI] [PubMed] [Google Scholar]
- 58.Pezzella AT, Yu HS, Kim JE. Surgical aspects of pulmonary paragonimiasis. Cardiovasc Dis 1981; 8: 187–194. [PMC free article] [PubMed] [Google Scholar]
- 59.Shamsuzzaman SM, Hashiguchi Y. Thoracic amebiasis. Clin Chest Med 2002; 23: 479–492. doi: 10.1016/S0272-5231(01)00008-9 [DOI] [PubMed] [Google Scholar]
- 60.Lichtenstein A, Kondo AT, Visvesvara GS, et al. Pulmonary amoebiasis presenting as superior vena cava syndrome. Thorax 2005; 60: 350–352. doi: 10.1136/thx.2004.021014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zakaria A, Al-Share B, Al Asad K. Primary pulmonary amebiasis complicated with multicystic empyema. Case Rep Pulmonol 2016; 2016: 8709347. doi: 10.1155/2016/8709347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Şimşek S, Akgül Özmen C. Unusual imaging characteristics of thoracic hydatid disease. Radiol Bras 2022; 55: 128–133. doi: 10.1590/0100-3984.2021.0041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Parlak E, Kerget F, Demirdal T, et al. The epidemiology, clinical manifestations, radiology, microbiology, treatment, and prognosis of echinococcosis: results of NENEHATUN study. Vector Borne Zoonotic Dis 2021; 21: 948–954. doi: 10.1089/vbz.2021.0029 [DOI] [PubMed] [Google Scholar]
- 64.Aydin Y, Ulas AB, Ince I, et al. Evaluation of albendazole efficiency and complications in patients with pulmonary hydatid cyst. Interact Cardiovasc Thorac Surg 2022; 34: 245–249. doi: 10.1093/icvts/ivab259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Garg MK, Sharma M, Gulati A, et al. Imaging in pulmonary hydatid cysts. World J Radiol 2016; 8: 581–587. doi: 10.4329/wjr.v8.i6.581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kantarci M, Bayraktutan U, Karabulut N, et al. Alveolar echinococcosis: spectrum of findings at cross-sectional imaging. Radiographics 2012; 32: 2053–2070. doi: 10.1148/rg.327125708 [DOI] [PubMed] [Google Scholar]
- 67.Martínez S, Restrepo CS, Carrillo JA, et al. Thoracic manifestations of tropical parasitic infections: a pictorial review. Radiographics 2005; 25: 135–155. doi: 10.1148/rg.251045043 [DOI] [PubMed] [Google Scholar]
- 68.Kuzucu A. Parasitic diseases of the respiratory tract. Curr Opin Pulm Med 2006; 12: 212–221. doi: 10.1097/01.mcp.0000219271.80804.9e [DOI] [PubMed] [Google Scholar]
- 69.Ahmed SK, Essa RA, Bapir DH. Uniportal video-assisted thoracoscopic surgery (u-VATS) for management of pulmonary hydatid cyst: a systematic review. Ann Med Surg 2022; 75: 103474. doi: 10.1016/j.amsu.2022.103474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ülkü R, Yilmaz HG, Onat S, et al. Surgical treatment of pulmonary hydatid cysts: report of 139 cases. Int Surg 2006; 91: 77–81. [PubMed] [Google Scholar]
- 71.Nahmias J, Goldsmith R, Soibelman M, et al. Three- to 7-year follow-up after albendazole treatment of 68 patients with cystic echinococcosis (hydatid disease). Ann Trop Med Parasitol 1994; 88: 295–304. doi: 10.1080/00034983.1994.11812870 [DOI] [PubMed] [Google Scholar]
- 72.Usluer O, Kaya SO, Samancilar O, et al. The effect of preoperative albendazole treatment on the cuticular membranes of pulmonary hydatid cysts: should it be administered preoperatively? Kardiochirurgia i Torakochirurgia Pol 2014; 11: 26–29. doi: 10.5114/kitp.2014.41926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Dehkordi AB, Sanei B, Yousefi M, et al. Albendazole and treatment of hydatid cyst, review of literature. Infect Disord Drug Targets 2019; 19: 101–104. doi: 10.2174/1871526518666180629134511 [DOI] [PubMed] [Google Scholar]
- 74.Arif SH, Shams-Ul-Bari, Wani NA, et al. Albendazole as an adjuvant to the standard surgical management of hydatid cyst liver. Int J Surg 2008; 6: 448–451. doi: 10.1016/j.ijsu.2008.08.003 [DOI] [PubMed] [Google Scholar]
- 75.Keramidas D, Mavridis G, Soutis M, et al. Medical treatment of pulmonary hydatidosis: complications and surgical management. Pediatr Surg Int 2004; 19: 774–776. doi: 10.1007/s00383-003-1031-4 [DOI] [PubMed] [Google Scholar]
- 76.Akhan O, Özmen MN, Dinçer A, et al. Percutaneous treatment of pulmonary hydatid cysts. Cardiovasc Intervent Radiol 1994; 17: 271–275. doi: 10.1007/BF00192450 [DOI] [PubMed] [Google Scholar]
- 77.Gabal AM, Khawaja FI, Mohammad GA. Modified PAIR technique for percutaneous treatment of high-risk hydatid cysts. Cardiovasc Intervent Radiol 2005; 28: 200–208. doi: 10.1007/PL00021047 [DOI] [PubMed] [Google Scholar]
- 78.Asimacopoulos PJ, Katras A, Christie B. Pulmonary dirofilariasis: the largest single-hospital experience. Chest 1992; 102: 851–855. doi: 10.1378/chest.102.3.851 [DOI] [PubMed] [Google Scholar]
- 79.Saha BK, Bonnier A, Chong WH, et al. Human pulmonary dirofilariasis: a review for the clinicians. Am J Med Sci 2022; 363: 11–17. doi: 10.1016/j.amjms.2021.07.017 [DOI] [PubMed] [Google Scholar]
- 80.Momčilović S, Gabrielli S, Đenić N, et al. New cases of human dirofilariosis on the Balkan Peninsula – “Masked intruders” uncovered by a surgeon. Parasitol Int 2022; 86: 102482. doi: 10.1016/j.parint.2021.102482 [DOI] [PubMed] [Google Scholar]
- 81.Miterpáková M, Antolová D, Rampalová J, et al. Dirofilaria immitis pulmonary dirofilariasis, Slovakia. Emerg Infect Dis 2022; 28: 482–485. doi: 10.3201/eid2802.211963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Takei D, Yamaki M, Noriyuki T, et al. Pulmonary dirofilariasis. Kyobu Geka 2015; 68: 76–79. [PubMed] [Google Scholar]
- 83.Al-Tawfiq JA. Epidemiology of travel-related malaria in a non-malarious areas in Saudi Arabia. Saudi Med J 2006; 27: 1781–1782. [PubMed] [Google Scholar]
- 84.Taylor WRJ, White NJ. Malaria and the lung. Clin Chest Med 2002; 23: 457–468. doi: 10.1016/S0272-5231(02)00004-7 [DOI] [PubMed] [Google Scholar]
- 85.Taylor WRJ, Cañon V, White NJ. Pulmonary manifestations of malaria: recognition and management. Treat Respir Med 2006; 5: 419–428. doi: 10.2165/00151829-200605060-00007 [DOI] [PubMed] [Google Scholar]
- 86.Taylor WRJ, Hanson J, Turner GDH, et al. Respiratory manifestations of malaria. Chest 2012; 142: 492–505. doi: 10.1378/chest.11-2655 [DOI] [PubMed] [Google Scholar]
- 87.Anstey NM, Jacups SP, Cain T, et al. Pulmonary manifestations of uncomplicated falciparum and vivax malaria: cough, small airways obstruction, impaired gas transfer, and increased pulmonary phagocytic activity. J Infect Dis 2002; 185: 1326–1334. doi: 10.1086/339885 [DOI] [PubMed] [Google Scholar]
- 88.Yale SH, Adlakha A, Sebo TJ, et al. Bronchiolitis obliterans organizing pneumonia caused by Plasmodium vivax malaria. Chest 1993; 104: 1294–1296. doi: 10.1378/chest.104.4.1294 [DOI] [PubMed] [Google Scholar]