Abstract
Treatment methods for proximal femoral fractures, when the fractures run from the femoral basal neck to the subtrochanteric area, have not yet been fully reported. Thus, we aimed to clarify osteosynthesis methods based on the fracture frequency and clinical results. We classified the proximal femoral fractures using the Area classification method based on the location (area) of the fracture line. The proximal femur has 4 areas with 3 boundaries; the center of the femoral neck, the boundary between femoral neck and trochanter, and the plane connecting the lower ends of the greater trochanter and the lesser trochanter. Fractures occurring only in Area-1 (proximal from the center of the femoral neck) were classified as Type 1; those in both Areas 1 and 2 (base of the femoral neck) were classified as Type 1-2. Therefore, fractures running from femoral basal neck to the subtrochanteric area were classified as Type 2-3-4. We targeted 60 Type 2-3-4 cases (average age 81 years, 10 men, 50 women) out of 1042 proximal femoral fracture cases who visited 8 hospitals in 2 years. We investigated the presence or absence of lateral trochanteric wall fractures, the selection of internal fixator, and the proportion of poor results. The lateral trochanteric wall fracture was observed in 48% of subjects. Long nails were selected to treat 46% cases, and nails with 2 or 3 proximal lag screws were used in 58% cases. Long nails and those with 2 or 3 lag screws were also used in 59% and 69% of lateral trochanteric wall fractures. Poor results such as cutout or excessive telescoping of lag screw occurred in 11.7% of cases and 17.2% of lateral trochanteric wall fractures. Even in cases where long nails and multiple lag screws were used for femoral trochanteric fractures whose fracture line ran from the femoral basal neck to subtrochanteric area were used, the failure rate was high in the presence of a lateral wall fracture. Therefore, it is necessary to consider careful post-operative treatment for proximal femoral fractures with lateral wall fracture, whose fracture line runs from femoral basal neck to subtrochanteric area.
Keywords: hip fractures, femoral neck fractures, trochanteric fractures, subtrochanteric fractures, internal fixators
1. Introduction
Proximal femoral fractures (PFF) are the most common trauma in the elderly, and the occurrence of PFF is increasing with an aging population.[1] Almost all patients with PFF undergo surgery to recover as soon as possible. Surgeries for PFF include osteosynthesis and total hip replacement (femoral head replacement). Among the PFF, the femoral trochanteric fracture is a fracture of the site where the stem of total hip arthroplasty will be placed, and it is not easy to achieve the stability of the stem. Therefore, osteosynthesis is performed in almost all cases of femoral trochanteric fractures.[2,3] In some cases, issues like re-displacement, pseudarthrosis, and implant cutout occur post-surgery, necessitating another surgery impairing the patient’s quality of life.[4–9]
To reduce the possibility of the above-mentioned post-operative failure, it is necessary to select an appropriate osteosynthesis implant according to the type of fracture. To achieve this, various classifications of PFF have been developed. For example, there is a classification with 3-dimensional computed tomography based on the number of bone-fragments,[10] or AO/OTA classification, which includes femoral neck fractures, femoral basicervical fractures, and femoral trochanteric fractures.[11] However, none of these methods classify fractures based on fracture lines extending into multiple areas of the bone. Fractures that extend over a wide range are dangerous and likely to cause cutout of the implants, re-displacement, or pseudarthrosis. Area classification has been proposed as a comprehensive classification method to detect such dangerous fractures.[12] It also has higher inter-examiner reliability than other classification methods.[12]
In Area classification, the proximal femur is divided into 4 areas by 3 boundaries, and the PFF are classified based on which of these 4 areas have the fracture line. The 3 boundaries are the center of the femoral neck, the boundary between the femoral neck and trochanter, and the plane connecting the lower ends of the greater and the lesser trochanter. When there is a fracture line in Area-1 (proximal area above the center of the femoral neck), it is classified as Type 1, and when there is a fracture line in both Area-1 and Area-2 (distal area under the center of the femoral neck), it is classified as Type 1-2. Therefore, PFF in which the fracture line runs from the femoral basal neck to the subtrochanteric area are classified as Type 2-3-4.
Type 2-3-4 fractures are classified as trochanteric fractures in general; however, it is extremely unstable because the fracture line extends to the femoral neck and subtrochanteric area, making it difficult to treat with osteosynthesis, even if they can be properly reductioned. Moreover, it has been reported recently that lateral trochanteric wall fractures greatly affect the treatment results for highly unstable trochanteric fractures (Fig. 1).[13,14] However, little research has been done on the frequency of lateral wall fractures present in femoral trochanteric fractures with widespread fracture lines or on how often post-operative failures occur in such fractures. Moreover, little is known regarding the kind of implant selection necessary to prevent such post-operative failures.
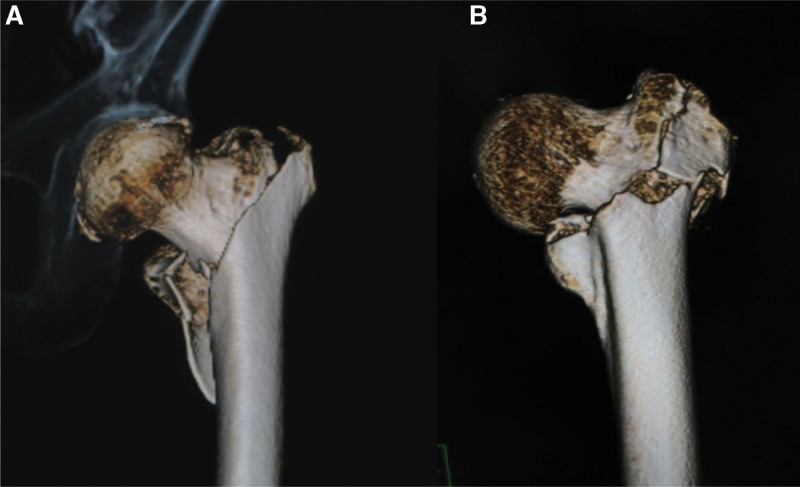
Figure 1.
Area classification, Type 2-3-4 femoral trochanteric fracture. (a) No lateral trochanteric wall fracture. (b) A lateral trochanteric wall fracture is present.
Therefore, in this study, we focused on cases classified as Area classification Type 2-3-4. We investigated the clinical outcomes of this fracture, the frequency of lateral trochanteric wall fractures, the relationship between the lateral wall fractures and clinical results, and the relationship between osteosynthesis implant selection and clinical outcomes.
2. Materials and Methods
This study included data from 1042 patients with PFF who visited 8 general hospitals between January 2014 and December 2015. Based on their preoperative X-ray and computed tomography, including 3-dimensional computed tomography, the orthopedic surgeon at each hospital classified the PFF according to the Area Classification method.[12,15] Because of proven high inter-rater reliability, the Area classification for each case was not done by multiple orthopedic surgeons.[12] Incomplete proximal femur fractures that can only be detected by magnetic resonance imaging were excluded from this study, and only cases diagnosed by X-ray and computed tomography were analyzed. Cases of possible pathological fractures due to tumors were excluded, however, cases of multiple trauma or high-energy trauma cases due to traffic accidents were not excluded.
Overall, 60 cases (average 81 years: 43–96 years, 10 males and 50 females) were classified as Type 2-3-4 and evaluated in this study. We also investigated the presence or absence of lateral trochanteric wall fractures[13,14] and the internal fixator selection for treating these cases.
Patients with cutout or telescoping more than 10 mm of a lag screw and those with nonunion and infection were included in the Failure group. We further investigated the relationship between the proportion of the Failure group (Failure rate) and the presence of lateral trochanteric wall fractures or the differences of internal fixators.
Approval for this study was granted by the institutional review board of our university (IRB No. 2598), and subjects gave their informed consent to participate.
3. Results
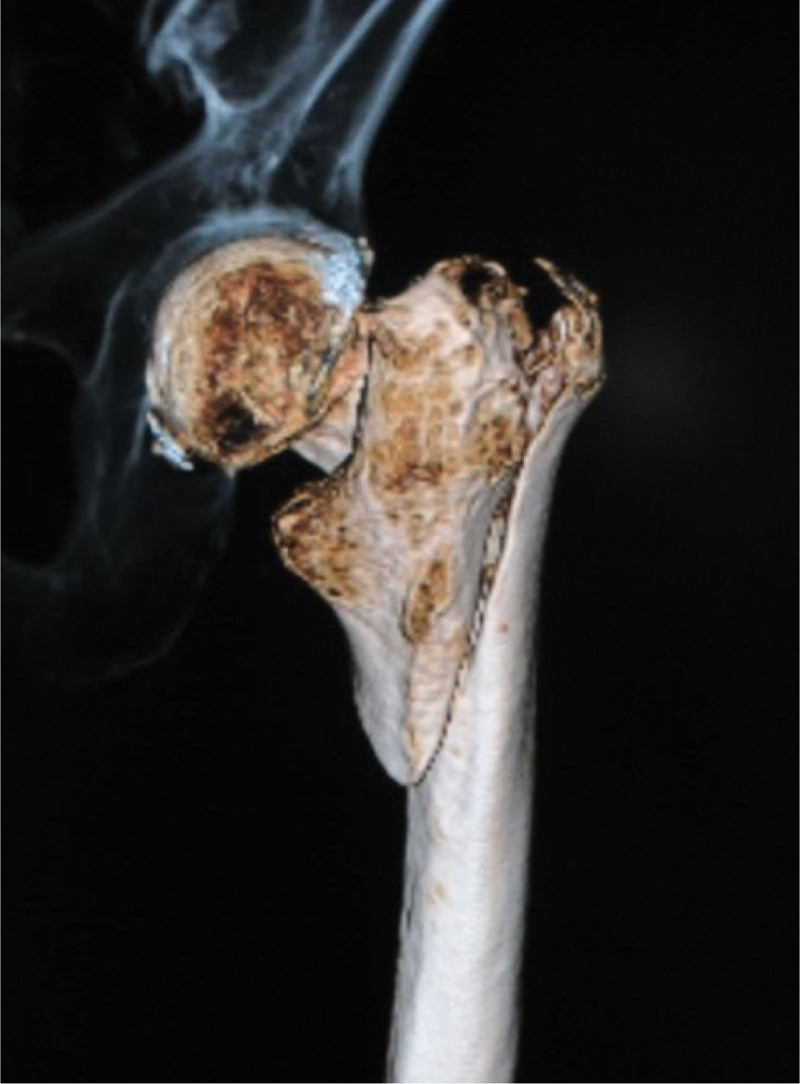
All Type 2-3-4 cases were treated with osteosynthesis. 41 of 60 Type 2-3-4 fracture cases (68%) had large posterolateral fragments (Fig. 2), and 29 of 60 cases (48%) had fracture lines on the proximal lateral trochanteric wall (lateral trochanteric wall fractures) (Fig. 1).[13,14]
Figure 2.
Type 2-3-4 fractures with large posterolateral fragments, appearing like a banana.
There were 25 cases treated with short femoral nails, of which 10 cases underwent osteosynthesis with single lag screws (Gamma3 Locking Nail System, Stryker, MI) and 15 underwent osteosynthesis with double lag screws (IPT Nail System, HOMS, Nagano Japan) (Table 1). There were 28 cases treated with middle or long femoral nails; of these, 8 cases underwent osteosynthesis with a single lag screw (Gamma3 Long Nail System, Stryker, MI) and 20 cases underwent osteosynthesis with double lag screws (IPT middle Nail System, HOMS, Nagano Japan) (Table 2). There were 7 cases treated with compression hip screws; 4 of which underwent treatment with compression hip screws combined with a trochanter plate.
Table 1.
Number of lag screws in cases treated with short femoral nails.
| Single lag screw | 10 cases | 2 cases without lateral wall fracture |
|---|---|---|
| Double lag screw | 15 cases | 6 cases with lateral wall fracture |
Table 2.
Number of lag screws in cases treated with middle or long femoral nails.
| Single lag screw | 8 cases | 3 cases without lateral wall fracture |
|---|---|---|
| Double lag screw | 20 cases | 14 cases with lateral wall fracture |
Overall, 46% of Type 2-3-4 cases were treated with middle or long nails, and 58% were treated with double lag screws.
Middle or long nails and double lag screws were used significantly more often for osteosynthesis in patients with lateral trochanteric wall fractures than in those without (P = .04 for both; chi-square test) (Tables 3 and 4). In other words, middle or long nails and double lag screws tended to be used for Type 2-3-4 and lateral trochanteric wall fractures.
Table 3.
Relationship between the presence or absence of lateral trochanteric wall fracture and the length of the nail (P = .04 chi-square test).
| Short nail | Middle or long nail | |
|---|---|---|
| With lateral wall fracture | 8 | 17 |
| Without lateral wall fracture | 17 | 11 |
Table 4.
Relationship between the presence or absence of lateral trochanteric wall fracture and the number of lag screws (P = .04 chi-square test).
| Single lag screw | Double lag screw | |
|---|---|---|
| With lateral wall fracture | 5 | 19 |
| Without lateral wall fracture | 13 | 14 |
There were no cases in which the lag screw was cutout. However, in the 10 cases that underwent osteosynthesis by short femoral nail with a single lag screw, the lag screws in 2 cases were telescoped 10 mm or more. On the other hand, in the 15 cases that underwent osteosynthesis by short femoral nail with a double lag screw, the lag screws of only 1 case telescoped excessively. Of the 28 patients who underwent osteosynthesis with middle or long nails, the lag screw telescoped in only 2 cases.
Additionally, 1 case of prolonged healing occurred among patients who had osteosynthesis by CHS with plate, and 1 case of infection occurred in patients who underwent osteosynthesis with middle nails. As a result, the failure rate was 11.7% (7 of 60 cases).
When limited to those cases with lateral trochanteric wall fractures, there were 4 cases with 10 mm or more lag screw telescoping and 1 case with prolonged healing. Thus, the failure rate of cases with lateral trochanteric wall fractures was 17.2%.
Cases with lateral trochanteric wall fractures tended to have higher failure rates than those without because lateral trochanteric wall fractures were fixed with longer nails and a larger number of lag screws; however, the difference was not statistically significant (P = .19, chi-square test) (Table 5).
Table 5.
Relationship between the presence or absence of lateral trochanteric wall fracture and the failure rate (P = .19 chi-square test).
| Failure case | No failure case | |
|---|---|---|
| With lateral wall fracture | 5 | 24 |
| Without lateral wall fracture | 2 | 29 |
4. Discussion
Of the PFF that account for bedridden elderly, the trochanteric fractures are treated with osteosynthesis. Among such trochanteric fractures, a few fractures extend to the femoral neck or subtrochanteric area. Such fractures are extremely unstable and are difficult to treat with osteosynthesis.
Fractures such as those described above are classified as Type 2-3-4 in Area classification. In this study, we found about half of such fractures involving the lateral trochanteric wall. No reports in the past have addressed the frequency of occurrence of the lateral trochanteric wall fractures.
We found a 10% failure rate of all Type 2-3-4 fractures and a 20% failure when the analysis was limited to lateral trochanteric wall fracture. In other words, excessive telescoping of the lag screw or prolonged healing was observed in more than 15% of those cases.
For nearly all trochanteric fractures, early recovery to gait can be obtained by performing osteosynthesis with a short femoral nail immediately after the injury. However, this study’s results revealed that trochanteric fractures, where the fracture line runs from femoral basal neck to subtrochanteric area, and those fractures involving the lateral trochanteric wall should be treated fairly carefully.
In cases with fractures of the lateral trochanteric wall, sagittal swing motion is likely to occur, leading to failure. However, the sagittal swing motion can be minimized using middle or long nails.[16,17] In this study, middle or long nails were significantly more frequently used in cases with lateral trochanteric wall fractures, and good results were obtained.
The presence of large posterolateral bone fragments has been reported to increase rotational instability.[18] In this study, osteosynthesis implants with multiple lag screws were significantly more frequently used in cases with lateral trochanteric wall fractures. However, there were cases in which short nails were selected, or single lag screws were used because the fracture line’s extent was not carefully confirmed or the importance of lateral trochanteric wall fractures was not recognized. If the experienced surgeon judges it to be an unstable fracture, a strong fixation using the middle or long nails or multiple lag screws is selected. However, if it is not recognized as an unstable fracture, strong fixation will not be made. Then, the complications that could have been avoided will occur.
Area classification can evaluate the unstable fractures with fracture lines straddling the conventional classification range, which has not been classified by the conventional classification. It is necessary to confirm to what area the fracture line extends by trying to classify PFF by Area classification. As a result, the possibility of overlooking the extent of the fracture line is reduced, and ideal implant selection for suitable osteosynthesis for the fracture becomes possible. In Type 2-3-4 fracture, the lateral trochanteric wall fractures existed in nearly half of the cases; thus, the use of middle or long nails that can use multiple lag screws should be selected for PFF in which fracture line runs from the femoral basal neck to subtrochanteric area.
However, excessive lag screw telescoping or delayed unions occurred despite the use of middle or long nails with multiple lag screws, in some cases of Type 2-3-4 fractures. Therefore, it is necessary to consider careful post-operative treatment such as lengthening the unloading period or combined use of adjuvant therapy such as parathyroid hormone and low-intensity pulsed ultrasound for Type 2-3-4 fractures.[19]
A limitation of this study is that we could not examine the clinical outcome when the treatment methods were decided based on Area classification. In this study, the clinical outcome was investigated when the treatment method was selected at the surgeon’s discretion before the Area classification was created. Nevertheless, because there was a difference in the selection of the internal fixator depending on the presence or absence of lateral trochanteric wall fractures, the selection criteria of the internal fixator were clarified by paying attention to the lateral trochanteric wall fractures.
Another limitation of this study is that it did not include data on the success or failure of the reduction. However, the selection of implant is important regardless of the quality of the surgery, such as the degree of reduction. This is because no matter how perfect the reduction is, if the implant is inadequate, the reducted position cannot be maintained. In addition, each orthopedic surgeon has the skill to always aim for and achieve adequate reduction.
In the future, we will perform multivariate analyses of factors that affect clinical outcomes after using treatment methods based on Area classification, and the results obtained will lead to risk management that is more tailored to the fracture condition. The results of this study are the first step towards leading to the above-mentioned research and towards developing a more appropriate treatment for trochanteric femur fractures.
5. Conclusion
This study the first revealed the frequency of occurrence of the lateral trochanteric wall fractures in PFF whose fracture line runs from femoral basal neck to subtrochanteric area. Long nails and multiple lag screws should be used for such PFF; however, the failure rate was high in the presence of a lateral wall fracture. Therefore, it is necessary to consider careful post-operative treatment for such PFF with lateral wall fracture, whose fracture line runs from femoral basal neck to subtrochanteric area.
Acknowledgements
The authors would like to thank Natsuo Konishi, Hitoshi Kubota, Shin Yamada, Keiji Kamo, Yoshihiko Okudera, Masashi Fujii, Ken Sasaki, Tetsuya Kawano, Yosuke Iwamoto, Itsuki Nagahata, and Takanori Miura for data collection and analysis. The authors would also like to thank Editage (www.editage.com) for English language editing.
Author contributions
Conceptualization: Norio Suzuki, Hiroaki Kijima.
Data curation: Hiroshi Tazawa, Takayuki Tani.
Formal analysis: Hiroaki Kijima.
Investigation: Norio Suzuki.
Methodology: Hiroaki Kijima.
Project administration: Naohisa Miyakoshi.
Resources: Norio Suzuki, Hiroaki Kijima, Hiroshi Tazawa, Takayuki Tani.
Validation: Hiroshi Tazawa.
Visualization: Hiroaki Kijima.
Writing – original draft: Norio Suzuki.
Writing – review & editing: Hiroaki Kijima.
Abbreviation:
- PFF =
- proximal femoral fractures
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors have no funding and conflicts of interest to disclose.
How to cite this article: Suzuki N, Kijima H, Tazawa H, Tani T, Miyakoshi N. Occurrence and clinical outcome of lateral wall fractures in proximal femoral fractures whose fracture line runs from femoral basal neck to subtrochanteric area. Medicine 2022;101:48(e32155).
Contributor Information
Norio Suzuki, Email: norios1975@yahoo.co.jp.
Hiroshi Tazawa, Email: hiroshi_tazawa@akita-med.jrc.or.jp.
Takayuki Tani, Email: tanit2525@gmail.com.
Naohisa Miyakoshi, Email: miyakosh@doc.med.akita-u.ac.jp.
References
- [1].Orimo H, Yaegashi Y, Hosoi T, et al. Hip fracture incidence in Japan: estimates of new patients in 2012 and 25-year trends. Osteoporos Int. 2016;27:1777–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Kraus M, Krischak G, Wiedmann K, et al. Clinical evaluation of PFNA® and relationship between the tip-apex distance and mechanical failure. Unfallchirurg. 2011;114:470–8. [DOI] [PubMed] [Google Scholar]
- [3].Mereddy P, Kamath S, Ramakrishnan M, et al. The AO/ASIF proximal femoral nail antirotation (PFNA): a new design for the treatment of unstable proximal femoral fractures. Injury. 2009;40:428–32. [DOI] [PubMed] [Google Scholar]
- [4].Muhm M, Hillenbrand H, Danko T, et al. Early complication rate of fractures close to the hip joint. Dependence on treatment in on-call services and comorbidities. Unfallchirurg. 2015;118:336–46. [DOI] [PubMed] [Google Scholar]
- [5].Bonnaire F, Weber A, Bösl O, et al. Cutting out in pertrochanteric fractures--problem of osteoporosis?. Unfallchirurg. 2007;110:425–32. [DOI] [PubMed] [Google Scholar]
- [6].Bojan AJ, Beimel C, Taglang G, et al. Critical factors in cut-out complication after gamma nail treatment of proximal femoral fractures. BMC Musculoskelet Disord. 2013;14:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Hsueh KK, Fang CK, Chen CM, et al. Risk factors in cutout of sliding hip screw in intertrochanteric fractures: an evaluation of 937 patients. Int Orthop. 2010;34:1273–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Al-Majed AA, Hammer J, Mayr E, et al. Biomechanical characterisation of osteosyntheses for proximal femur fractures: helical blade versus screw. Stud Health Technol Inform. 2008;133:1–10. [PubMed] [Google Scholar]
- [9].Babhulkar S. Unstable trochanteric fractures: issues and avoiding pitfalls. Injury. 2017;48:803–18. [DOI] [PubMed] [Google Scholar]
- [10].Wada K, Mikami H, Amari R, et al. A novel three-dimensional classification system for intertrochanteric fractures based on computed tomography findings. J Med Invest. 2019;66:362–6. [DOI] [PubMed] [Google Scholar]
- [11].Muller ME. The comprehensive classification of fractures of long bones. In: Allgower M, (ed). Manual of internal fixation: techniques recommended by the AO-ASIF Group. 3rd ed. Berlin: Spriger-Verlag; 1991:118–50. [Google Scholar]
- [12].Kijima H, Yamada S, Konishi N, et al. The reliability of classifications of proximal femoral fractures with 3-dimensional computed tomography: the new concept of comprehensive classification. Adv Orthop. 2014;2014:359689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Haidukewych GJ. Intertrochanteric fractures: ten tips to improve results. Instr Course Lect. 2010;59:503–9. [PubMed] [Google Scholar]
- [14].Gotfried Y. The lateral trochanteric wall: a key element in the reconstruction of unstable pertrochanteric hip fractures. Clin Orthop Relat Res. 2004;425:82–6. [PubMed] [Google Scholar]
- [15].Kijima H, Yamada S, Konishi N, et al. The choice of internal fixator for fractures around the femoral trochanter depends on area classification. Springerplus. 2016;5:1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Terada C. Tips and pitfalls of the treatment for femoral trochanteric fractures using intramedullary nail (in Japanese). Orthop Surg Traumatol. 2016;59:1603–13. [Google Scholar]
- [17].Kane P, Vopat B, Paller D, et al. A biomechanical comparison of locked and unlocked long cephalomedullary nails in a stable intertrochanteric fracture model. J Orthop Trauma. 2014;28:715–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Yamane K, Narasaki S, Nakanishi K, et al. Rotational instability of trochanteric fracture of the femur (in Japanese). J Jpn Soc Fract Rep. 2012;34:85–8. [Google Scholar]
- [19].Watanabe M. The effectiveness of the low-intensity pulsed ultrasound (LIPUS) on acceleration of bone healing following the open reduction and internal fixation of trochanteric fractures of the femur (in Japanese). J Jpn Soc Fract Rep. 2014;36:155–9. [Google Scholar]