Abstract
Background
The impact of the coronavirus disease 2019 (COVID-19) pandemic on cancer screening participation is a global concern. A national database of screening performance is available in Japan for population-based cancer screening, estimated to cover approximately half of all cancer screenings.
Methods
Utilizing the fiscal year (FY) 2017–2020 national database, the number of participants in screenings for gastric cancer (upper gastrointestinal [UGI] series or endoscopy), colorectal cancer (fecal occult blood test), lung cancer (chest X-ray), breast cancer (mammography), and cervical cancer (Pap smear) were identified. The percent change in the number of participants was calculated.
Results
Compared with the pre-pandemic period (FY 2017–2019), in percentage terms FY 2020 recorded the largest decline in gastric cancer UGI series (2.82 million to 1.91 million, percent change was −32.2 %), followed by screening for breast cancer (3.10 million to 2.57 million, percent change was −17.2 %), lung cancer (7.92 million to 6.59 million, percent change was −16.7 %), colorectal cancer (8.42 million to 7.30 million, percent change was −13.4 %), cervical cancer (4.26 million to 3.77 million, percent change was −11.6 %), and gastric cancer via endoscopy (1.02 million to 0.93 million, percent change was −9.0 %).
Conclusion
The number of participants in population-based screenings in Japan decreased by approximately 10–30 % during the pandemic. The impact of these declines on cancer detection or mortality should be carefully monitored.
Keywords: Cancer screening, Population-based Cancer Screening, COVID-19, SARS-CoV-2, Coronavirus disease, Cancer prevention
1. Introduction
Cancer screening in Japan is mainly divided into population-based cancer screenings conducted by local governments and worksite-based cancer screenings conducted by business owners for employees. A large-scale questionnaire survey conducted by the central government every three years estimated that about the same number of people who underwent worksite-based cancer screenings participated in population-based cancer screenings [1]. Currently, population-based cancer screening is the only national cancer control program, and it is implemented based on the guidelines of the Ministry of Health, Labor and Welfare (MHLW). Only the results of the population-based cancer screenings are collected annually by the MHLW from the local government and published as a national database on their website [2].
In a population-based cancer screening, the following programs are recommended by the MHLW [3]: gastric cancer screening (upper gastrointestinal [UGI] or endoscopy, every 2 years for individuals aged ≥50 years; annual UGI is also available for individuals aged 40–49 years), colorectal cancer screening (annual fecal occult blood test [FOBT] for individuals aged ≥40 years), lung cancer screening (annual chest x-ray for individuals aged ≥40 years), breast cancer screening (mammography, every 2 years for individuals aged ≥40 years), and cervical cancer screening (Pap smear, every 2 years for individuals aged ≥20 years). Population-based cancer screening is divided into two types of screening system, one is conducted at large-scale facilities for large groups (mass screening), and the other at local medical facilities (individual screening). Local governments set limits on the number of participants for each type according to screening capacity, and residents are free to choose either type.
A national database of population-based screenings is constructed every fiscal year [FY]. This database includes the number of participants, and this is identifiable by the national total, local government, sex, age, and type of screening (mass screening, individual screening).
Globally, the number of cancer screening participants decreased significantly during the pandemic period, raising concerns about delays in cancer diagnosis and treatment [4], [5], [6]. In FY 2020, the Japanese government declared a state of emergency nationwide only once from April 7 to May 25 [7]. The MHLW had requested local governments to temporarily suspend or postpone population-based screenings during the declaration period, and compliance was dependent on each municipality. The aim of this report was to evaluate the changes in the number of population-based cancer screening participants during the COVID-19 pandemic in Japan, using national data.
2. Methods
2.1. Data sources
Based on the national database [2], we identified the total number of participants nationwide from FY 2017 to FY 2020. The pandemic period and control period were considered to be FY 2020 (April 2020–March 2021) and FY 2017–2019 (April 2017–March 2020), respectively. The subjects of analysis were five cancer screenings recommended by the MHLW, and gastric cancer screening was performed separately by UGI and endoscopy (making six screening types in total). Furthermore, the number of participants nationwide for each cancer was identified by sex, age group, and screening type.
This study used publicly available open data sources [2], and thus did not require informed consent. As mentioned below in the limitations of this study, because it is currently not possible to calculate the actual cancer screening rate in Japan, we used the number of participants in this study.
2.2. Descriptive statistics
The number of participants in each year was summarized by the national total, sex, age group, and type of screening. The percentage change in the number of participants in each screening during the pandemic period (FY 2020), compared with the control period (FY2017–2019), was calculated as follows:
| (Number of participants in FY 2020 – Average number of participants in the past 3 years) / Average number of participants in the past 3 years· |
Participant numbers may have changed significantly in FY2017–2019, for sensitivity analysis, the percent change in participant numbers from 2019 to 2020 was calculated as follows:
| (Number of participants in FY 2020 – Number of participants in FY 2019) / Number of participants in FY 2019· |
3. Results
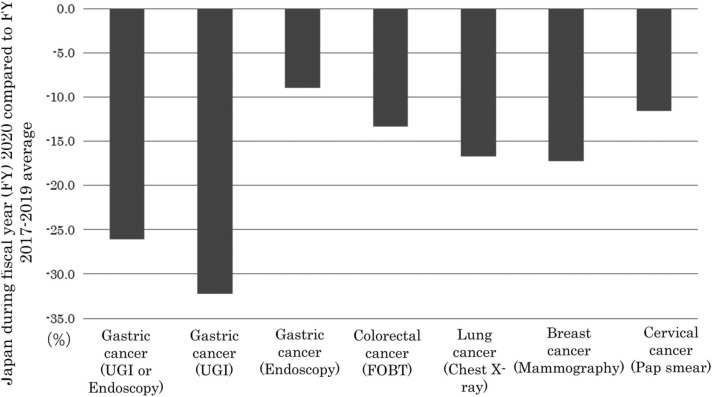
Table 1 shows the number of participants in FY 2020 and the average number of participants in the previous 3 years by sex, age group, and screening type. The number of participants in FY 2017–2019 was almost the same for each cancer type (Supplementary file). Compared with that before the pandemic, the total number of participants in FY 2020 decreased from 2.82 million to 1.91 million (gastric cancer, UGI), 1.02 million to 0.93 million (gastric cancer, endoscopy), 8.42 million to 7.30 million (colorectal cancer), 7.92 million to 6.59 million (lung cancer), 3.10 million to 2.57 million (breast cancer), and 4.26 million to 3.77 million (cervical cancer). The percentage change was the largest for gastric cancer (UGI, −32.2 %), followed by breast cancer (−17.2 %), lung cancer (−16.7 %), colorectal cancer (−13.4 %), cervical cancer (−11.6 %), and gastric cancer (endoscopy, −9.0 %) ( Fig. 1).
Table 1.
Participation in cancer screening programs in Japan during fiscal year (FY) 2017–2020 (percentages in parentheses).
| FY 2017–2019, avg. | FY 2020 | Percentage change | |||||
|---|---|---|---|---|---|---|---|
| Gastric cancer (UGI or Endoscopy) | |||||||
| Total | 3,837,143 | 2,837,083 | -26.1 | ||||
| Sex | Male | 1,678,154 | (43.7) | 1,263,891 | (44.5) | -24.7 | |
| Female | 2,158,989 | (56.3) | 1,573,192 | (55.5) | -27.1 | ||
| Age, y | 40–49 | 411,252 | (10.7) | 280,183 | (9.9) | -31.9 | |
| 50–59 | 539,951 | (14.1) | 423,897 | (14.9) | -21.5 | ||
| 60–69 | 1,217,547 | (31.7) | 814,228 | (28.7) | -33.1 | ||
| 70–79 | 1,327,201 | (34.6) | 1,046,644 | (36.9) | -21.1 | ||
| 80- | 341,191 | (8.9) | 272,131 | (9.6) | -20.2 | ||
| Type of screening | Mass screening | 2,143,680 | (55.9) | 1,412,663 | (49.8) | -34.1 | |
| Individual screening | 1,693,463 | (44.1) | 1,424,420 | (50.2) | -15.9 | ||
| Gastric cancer (UGI) | |||||||
| Total | 2,819,623 | 1,910,660 | -32.2 | ||||
| Sex | Male | 1,248,063 | (44.3) | 863,923 | (45.2) | -30.8 | |
| Female | 1,571,561 | (55.7) | 1,046,737 | (54.8) | -33.4 | ||
| Age, y | 40–49 | 411,252 | (14.6) | 280,183 | (14.7) | -31.9 | |
| 50–59 | 392,302 | (13.9) | 273,295 | (14.3) | -30.3 | ||
| 60–69 | 895,957 | (31.8) | 549,058 | (28.7) | -38.7 | ||
| 70–79 | 910,524 | (32.3) | 659,832 | (34.5) | -27.5 | ||
| 80- | 209,588 | (7.4) | 148,292 | (7.8) | -29.2 | ||
| Type of screening | Mass screening | 2,125,243 | (75.4) | 1,396,841 | (73.1) | -34.3 | |
| Individual screening | 694,380 | (24.6) | 513,819 | (26.9) | -26.0 | ||
| Gastric cancer (Endoscopy) | |||||||
| Total | 1,017,519 | 926,423 | -9.0 | ||||
| Sex | Male | 430,091 | (42.3) | 399,968 | (43.2) | -7.0 | |
| Female | 587,428 | (57.7) | 526,455 | (56.8) | -10.4 | ||
| Age, y | 50–59 | 147,649 | (14.5) | 150,602 | (16.3) | 2.0 | |
| 60–69 | 321,590 | (31.6) | 265,170 | (28.6) | -17.5 | ||
| 70–79 | 416,677 | (41.0) | 386,812 | (41.8) | -7.2 | ||
| 80- | 131,603 | (12.9) | 123,839 | (13.4) | -5.9 | ||
| Type of screening | Mass screening | 18,437 | (1.8) | 15,822 | (1.7) | -14.2 | |
| Individual screening | 999,082 | (98.2) | 910,601 | (98.3) | -8.9 | ||
| Colorectal cancer (FOBT) | |||||||
| Total | 8,424,776 | 7,298,673 | -13.4 | ||||
| Sex | Male | 3,321,617 | (39.4) | 2,893,898 | (39.6) | -12.9 | |
| Female | 5,103,159 | (60.6) | 4,404,775 | (60.4) | -13.7 | ||
| Age, y | 40–49 | 856,762 | (10.2) | 693,443 | (9.5) | -19.1 | |
| 50–59 | 953,545 | (11.3) | 816,647 | (11.2) | -14.4 | ||
| 60–69 | 2,368,211 | (28.1) | 1,802,854 | (24.7) | -23.9 | ||
| 70–79 | 3,086,488 | (36.6) | 2,874,921 | (39.4) | -6.9 | ||
| 80- | 1,159,770 | (13.8) | 1,110,808 | (15.2) | -4.2 | ||
| Type of screening | Mass screening | 3,569,051 | (42.4) | 2,787,198 | (38.2) | -21.9 | |
| Individual screening | 4,855,726 | (57.6) | 4,511,475 | (61.8) | -7.1 | ||
| Lung cancer (Chest X-ray) | |||||||
| Total | 7,918,697 | 6,593,528 | -16.7 | ||||
| Sex | Male | 3,198,703 | (40.4) | 2,679,184 | (40.6) | -16.2 | |
| Female | 4,719,994 | (59.6) | 3,914,344 | (59.4) | -17.1 | ||
| Age, y | 40–49 | 710,592 | (9.0) | 556,306 | (8.4) | -21.7 | |
| 50–59 | 778,708 | (9.8) | 639,820 | (9.7) | -17.8 | ||
| 60–69 | 2,189,666 | (27.7) | 1,571,519 | (23.8) | -28.2 | ||
| 70–79 | 3,010,602 | (38.0) | 2,684,477 | (40.7) | -10.8 | ||
| 80- | 1,229,129 | (15.5) | 1,141,406 | (17.3) | -7.1 | ||
| Type of screening | Mass screening | 4,409,525 | (55.7) | 3,163,019 | (48.0) | -28.3 | |
| Individual screening | 3,509,172 | (44.3) | 3,430,509 | (52.0) | -2.2 | ||
| Breast cancer (Mammography) | |||||||
| Total | 3,100,533 | 2,565,900 | -17.2 | ||||
| Age, y | 40–49 | 879,936 | (28.4) | 727,345 | (28.3) | -17.3 | |
| 50–59 | 681,034 | (22.0) | 586,869 | (22.9) | -13.8 | ||
| 60–69 | 835,959 | (27.0) | 633,753 | (24.7) | -24.2 | ||
| 70–79 | 607,644 | (19.6) | 530,876 | (20.7) | -12.6 | ||
| 80- | 95,960 | (3.1) | 87,057 | (3.4) | -9.3 | ||
| Type of screening | Mass screening | 1,495,147 | (48.2) | 1,105,214 | (43.1) | -26.1 | |
| Individual screening | 1,605,385 | (51.8) | 1,460,686 | (56.9) | -9.0 | ||
| Cervical cancer (Pap smear) | |||||||
| Total | 4,260,272 | 3,767,370 | -11.6 | ||||
| Age, y | 20–29 | 380,885 | (8.9) | 397,995 | (10.6) | 4.5 | |
| 30–39 | 781,530 | (18.3) | 702,443 | (18.6) | -10.1 | ||
| 40–49 | 939,360 | (22.0) | 831,412 | (22.1) | -11.5 | ||
| 50–59 | 722,492 | (17.0) | 655,134 | (17.4) | -9.3 | ||
| 60–69 | 800,719 | (18.8) | 618,666 | (16.4) | -22.7 | ||
| 70–79 | 551,198 | (12.9) | 484,993 | (12.9) | -12.0 | ||
| 80- | 84,088 | (2.0) | 76,727 | (2.0) | -8.8 | ||
| Type of screening | Mass screening | 1,195,295 | (28.1) | 856,012 | (22.7) | -28.4 | |
| Individual screening | 3,064,977 | (71.9) | 2,911,358 | (77.3) | -5.0 | ||
Fig. 1.
The percentage decrease in the number of screening participants during the pandemic (FY 2020) compared to the FY 2017–2019 average.
Before and during the pandemic, the number of female participants was approximately 1.2–1.5 times higher than that of male participants. The decrease in the number of participants during the pandemic period was larger in females for gastric, colorectal, and lung cancers (percentage change ranged from −30.8 % to −7.0 % for males and −33.4 % to −10.4 % for females). By age group, the largest number of participants were in their 70 s (gastric, colorectal, and lung) and 40 s (breast and cervical) both before and during the pandemic. The decrease in the number of participants during the pandemic period was the largest for individuals in their 60 s for all cancers (percentage change ranged from −38.7 % to −17.5 % for those in their 60 s and −31.9 % to 4.5 % for other age groups). By screening type, before and during the pandemic, the participation rate in mass screening was the highest for gastric cancer via UGI (73.1–75.4 %). The decrease in the number of participants during the pandemic period was larger for mass screening of all cancers (percentage change ranged from −34.3 % to −14.2 % in mass screening and −26.0 to −2.2 % in individual screening). Among all population-based cancer screenings, the largest reduction in the number of participants was noted in mass screening for gastric cancer via UGI (percentage change was −34.3 %).
Supplementary Table shows the result of sensitivity analysis. During FY 2017–2019, the total number of participants decreased from 3.04 million to 2.59 million (gastric cancer, UGI), 8.47 million to 8.35 million (colorectal cancer), 7.94 million to 7.87 million (lung cancer), and 4.29 million to 4.23 million (cervical cancer), while the total number of participants increased from 0.90 million to 1.11 million (gastric cancer, endoscopy) and 3.08 million to 3.11 million (breast cancer). The percentage of decrease in the number of screening participants during the pandemic (FY 2020) compared to FY 2019 was the largest for gastric cancer (UGI, −26.1 %), followed by breast cancer (−17.5 %), gastric cancer (endoscopy, −16.6 %), lung cancer (−16.2 %), colorectal cancer (−12.6 %), and cervical cancer (−10.8 %).
4. Discussion
This study revealed that the COVID-19 pandemic was associated with an approximately 10–30 % decrease in the number of participants in Japanese population-based screenings. In percentage terms, gastric cancer screening had the greatest decrease in the number of participants. According to a previous study using a hospital-based cancer registry covering 70 % of newly diagnosed cancers in Japan, of cancers diagnosed by screening in 2020 (by population-based screening and other screening types), gastric cancer decreased the most since the pre-pandemic period [8]. In our report, the number of participants declined the most in mass screenings for gastric cancer UGI. This is probably because this number was large even before the pandemic, and many local governments were unable to implement the necessary COVID-19 protective precautions in a short period of time to safely carry out mass screenings. The recommendation to temporarily postpone mass gastric cancer screenings by related academic societies may also have influenced the decisions of local governments [9].
Participants in some cancer screenings have been declining before 2020, so part of the decrease in FY2020 would probably also have taken place without COVID-19. Sensitivity analysis comparing FY 2020 and FY 2019 were generally similar to the main results (FY 2020 vs FY2017–2019): reductions in the number of participants for five cancers ranged from approximately 10–26 %, with gastric cancer showing the largest percentage reduction.
The gap of the percentage reduction in the two comparisons (FY2020 vs FY2017–2019, FY2020 vs FY2019), was largest for gastric cancer screening. Compared to FY 2019 and FY 2017–2019, the percentage of decrease in 2020 were − 26.1 % and − 32.2 % for UGI and − 16.6 % and − 9.0 % for endoscopy, respectively. These gaps are due to a decrease in participation in UGI screening and an increase in participation in endoscopic screening over the three years to 2020. Since endoscopic screening started in 2016 in addition to UGI screening, which started in the 1980 s, participants may have shifted from UGI screening to endoscopic screening.
There is no clear explanation regarding why the number of female participants and participants in their 60 s declined during the pandemic. Reasons for reduced participation in these strata should be further assessed through questionnaires. In Japan, many workers retire between the ages of 60 and 65 years and lose their eligibility for worksite-based cancer screening. Local governments do not individually identify residents who are disqualified from worksite-based cancer screening each year, so retirees are not called for population-based screening. If retirees wish to participate in population-based cancer screening, they must be referred to the local government and make an appointment. Those who retired during the COVID-19 pandemic may have been more reluctant to access population-based cancer screening than before.
In all cancers, mass screening resulted in greater attrition in participants than individual screening. Compared to individual screening, it is more difficult to maintain distance during the test in mass screening, which may increase the risk of infection among participants. Therefore, it is possible that local governments actively suspended mass screenings, or that residents avoided participating in mass screenings.
The strength of this paper is that it is the first to report changes in the number of cancer screening participants during the COVID-19 pandemic using Japanese national data. There are three limitations to our report. First, it is not clear whether the decline in participation in cancer screening is due to the cancellation of cancer screening by local governments or the refusal of residents to participate in cancer screening. If the number of participants in cancer screening decreased significantly at the time when the MHLW requested local governments to temporarily suspend screening (April-May 2020), cancellation of screening by the local government may have contributed to the decrease in the number of participants. However, this hypothesis could not be confirmed because the database of population-based screening programs does not provide monthly patient numbers (only annual totals are provided). During the first period of the state of emergency (April-May 2020), the Japanese government asked its citizens to strictly limit going outdoors. However, since June, behavioral restrictions had been limited to particularly high-risk behaviors and did not include participation in screening. The impact of these policies on changes in participation was not evaluated.
The second limitation is that the study relied on comparing the total number of screenings between different years and did not account for age standardization—changes in the size or age structure of the population between 2017 and 2020 could influence the results somewhat. Currently it is not possible to calculate the actual cancer screening rate in Japan, therefore we used the number of participants in this study. It is a serious drawback of the current Japanese cancer screening system that the actual measurement of the screening rate is not clear. There are two main reasons for this. One is that the local governments do not precisely identify those eligible for population-based cancer screening (e.g., unemployed persons, employees of companies that do not offer worksite-based cancer screening, retirees, etc.). Another reason is that there is no legal basis for worksite-based cancer screenings, and most of them are currently conducted as opportunistic screenings, and these results (such as the number of those eligible and participants) are not collected. All cancer screening rates (estimated value, including population-based screening and work-site screening) are identified only through questionnaire survey every 3 years.
The third limitation of this study is that changes in the number of participants in worksite-based screenings were not assessed due to the lack of a publicly available database as mentioned above. Differences in pandemic impacts should be assessed based on the data from large screening sites covering both population-based and workplace screenings. In the future, national screening programs should be integrated, and a comprehensive database should be constructed to improve cancer screening.
5. Conclusion
Based on a national database, the number of participants in population-based screenings in Japan decreased by approximately 10–30 % during the pandemic. The impact of these declines on cancer detection or cancer mortality should be carefully monitored. As an intermediate step, it is important to monitor cancer screening attendance in the post-COVID-19 pandemic period to see if attendance returns to pre-COVID-19 pandemic levels.
Author contribution.
Ryoko Machii (RM) and Hirokazu Takahashi (HT) conceived the idea of the study. RM drafted the original manuscript. HT supervised the conduct of this study. All authors reviewed the manuscript draftand revised it critically on intellectual content. All authors approved the final version of the manuscript to be published.
Funding
This work was supported by Health, Labour and Welfare Policy Research Grants and Research for Promotion of Cancer Control Programmes in Japan.
CRediT authorship contribution statement
Ryoko Machii and Hirokazu Takahashi contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.canep.2022.102313.
Appendix A. Supplementary material
Supplementary material.
.
References
- 1.Ministry of Health, Labour and Welfare, Comprehensive survey of living conditions. 〈https://www.mhlw.go.jp/english/database/db-hss/cslc-index.html〉 (Accessed 28 September 2022).
- 2.Ministry of Health, Labour and Welfare. Report on Regional Public Health Services and Health Promotion, Services Portal Site of Official Statistics of Japan Website. 〈https://www.e-stat.go.jp/stat-search/files?page=1&toukei=00450025&kikan=00450&tstat=000001030884〉 (in Japanese) (cited 7 July 2022).
- 3.Ministry of Health, Labour and Welfare, Guideline for population based cancer screening program. 〈https://www.mhlw.go.jp/bunya/kenkou/gan_kenshin.html〉 (in Japanese) (cited 7 July 2022).
- 4.Bakouny Z., Paciotti M., Schmidt A.L., Lipsitz S.R., Choueiri T.K., Trinh Q.D. Cancer screening tests and cancer diagnoses during the COVID-19 pandemic. JAMA Oncol. 2021;7:458–460. doi: 10.1001/jamaoncol.2020.7600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen R.C., Haynes K., Du S., Barron J., Katz A.J. Association of cancer screening deficit in the United States with the COVID-19 pandemic. JAMA Oncol. 2021;7:878–884. doi: 10.1001/jamaoncol.2021.0884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gathani T., Clayton G., MacInnes E., Horgan K. The COVID-19 pandemic and impact on breast cancer diagnoses: what happened in England in the first half of 2020. Br. J. Cancer. 2021;124:710–712. doi: 10.1038/s41416-020-01182-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cabinet Secretariat, COVID-19 information and resources. 〈https://corona.go.jp/news/news_20200421_70.html〉 (in Japanese) (cited 7 July 2022).
- 8.Okuyama A., Watabe M., Makoshi R., Takahashi H., Tsukada Y., Higashi T. Impact of the COVID-19 pandemic on the diagnosis of cancer in Japan: analysis of hospital-based cancer registries. Jpn. J. Clin. Oncol. 2022:hyac129. doi: 10.1093/jjco/hyac129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Japanese Society of Gastrointestinal Cancer Screening, Response to the new coronavirus infection (COVID-19) for gastrointestinal cancer screening. 〈https://www.jsgcs.or.jp/importants/archives/36〉 (in Japanese) (cited 7 July 2022).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material.