Abstract
Objectives
Clinicians report that withdrawal of mechanical ventilation in motor neuron disease is challenging. We report on the evaluation of the process and outcomes called for by the Association for Palliative Medicine of Great Britain and Ireland (APM) guidance.
Methods
Excel analysis of a core data set, defined in the APM guidance, and thematic analysis of free-text comments, submitted by a UK clinician soon after withdrawal of mechanical ventilation in any care setting.
Results
Thirty-seven professionals submitted 46 data sets from 4 patients with tracheostomy ventilation (TV) and 42 with non-invasive ventilation (NIV) in 35 months. These took place at home (43%), inpatient hospice (48%), hospital and care homes. Eighty-nine per cent received opioid and/or sedative medication at the initiation of withdrawal, majority of which were subcutaneous. A median of 2 doses (range 1–9) were used to manage symptoms before ventilation withdrawal. Subsequently 73% of patients required either none or one dose of medication. In addition to any background opioid, symptom management required a total parenteral morphine equivalent mean of 20.6 mg (range 0–60 mg) and midazolam mean of 25.8 mg (range 0–120 mg). The median time from first medication to removal of mechanical ventilation was 45 min. Patients with TV died within 30 min of withdrawal. The mode (14 of 42 patients) time to death after NIV withdrawal was 15 min, but ranged between <15 min and 54 hours.
Conclusions
Individualised, proportionate, titrated opioid and sedative medications were used to provide good symptom management, and provided new insight into the substantial variability in what patients require to manage their symptoms and how long the process takes. Most patients required lower doses than in previous literature.
Keywords: chronic conditions, drug administration, ethics, end of life care, neurological conditions
Introduction
When a patient with motor neuron disease (MND) is very dependent on mechanical ventilation, its withdrawal may lead to rapid onset of distressing breathlessness. The degree and acuity of breathlessness and distress are, to some extent, predictable and are related to the level of residual respiratory muscle function. Effective management of the expected symptoms of distress and breathlessness that arise in the withdrawal of mechanical ventilation is a professional responsibility,1 2 and is similar to the anticipatory and ongoing symptom management required for painful procedures and operations. Since some patients will not be able to tolerate even a few minutes without mechanical ventilation while others will be able to tolerate it for several hours, an individualised plan of symptom management is required. However, there is evidence that withdrawal of mechanical ventilation in MND can be challenging for everyone involved.3 4
The Association for Palliative Medicine of Great Britain and Ireland (APM) published a guidance for professionals which was widely endorsed by professional bodies5 and is consistent with the General Medical Council standards of good practice. However, since there is very little clinical evidence about this area of care, the APM requested that professionals submit an anonymised data set after undertaking withdrawal of mechanical ventilation so as to further inform the guidance.
This paper reports the findings from the prospective evaluation of the processes and outcomes of this area of care, aiming to provide a description of the medications that were used to manage symptoms, the temporal characteristics of the withdrawal process, the outcomes for families and professionals, and any challenges identified.
Methods
A proforma for anonymised data was developed alongside the national APM guidance.6 This asked the clinician present at the withdrawal to provide the following:
Demographic and clinically contextual information.
Information about the professionals and their involvement.
Detail about the use of medication before and during the withdrawal of ventilation.
Temporal characteristics of care.
Any challenges in managing symptoms.
Assessment of the experience for the family.
Reflection on their own experience.
The prospective evaluation was widely and repeatedly publicised through the MND Association care centres and regional care advisors; home ventilation services (via the specialists in long-term ventilation at home group); APM advanced neurological illness special interest forum; national palliative care and British Thoracic Society home ventilation meetings. Data were entered into an Excel spreadsheet for analysis and were analysed descriptively. Free-text comments were analysed thematically, employing an inductive, iterative approach.7 Text was manually coded and theme development was driven by the content of the comments and codes.
Results
Data from 46 patients from across England were submitted by 6 ventilation nurse specialists, 2 other nurses, 1 physiotherapist and 28 doctors working in palliative medicine. Most submitted a single case, but three doctors and five ventilation nurse specialists submitted two or three reports. Table 1 summarises the patient characteristics.
Table 1.
Key characteristics of the 46 patients
| Characteristics | Subcategory | Patients (n) |
| Sex | Male | 37 |
| Female | 9 | |
| Type of ventilation | TV | 4 |
| NIV | 42 | |
| Age group (years) | <30 | 0 |
| 31–50 | 9 | |
| 51–70 | 24 | |
| >70 | 12 | |
| Unknown | 1 | |
| Duration of ventilation (months) | >12 | 30 |
| 6–12 | 7 | |
| 1–6 | 8 | |
| <1 | 1 | |
| Ventilation dependence: how long can the patient manage without assisted ventilation before symptoms occur? | Could not manage at all | 19 |
| A few minutes | 19 | |
| Up to an hour | 5 | |
| A few hours | 3 | |
| Communication by patient, in the last days | By speech | 26 |
| By writing/keyboard | 7 | |
| By blink | 1 | |
| By eye movements | 6 | |
| By arm/facial movement | 2 | |
| No communication | 4 | |
| Place of withdrawal of assisted ventilation | Home | 20 |
| Inpatient hospice | 22 | |
| Care home | 2 | |
| Hospital | 2 |
NIV, non-invasive ventilation; TV, tracheostomy ventilation.
For six patients receiving non-invasive ventilation (NIV), the ventilation was withdrawn in the context of a best interests decision. For one tracheostomy ventilated (TV) patient, the withdrawal was made to enact an advance decision to refuse treatment.
Symptom management prior to initiating withdrawal of mechanical ventilation
Before withdrawal of mechanical ventilation, only 11 patients were not taking any medication for symptom management; 30 were taking an opioid, 29 a benzodiazepine, and 23 of the 30 patients were taking both. Twenty-one patients were using these medications through continuous subcutaneous infusion.
In preparation for initiating the withdrawal of ventilation, 24 of 46 patients had their medications started or changed to a continuous subcutaneous infusion. This was usually the night before. Where a continuous subcutaneous infusion was started de novo (n=15), midazolam was always prescribed with an opioid in all but one case. The median initiated midazolam dose was 10 mg/24 hours (range 5–20 mg). Seven people who were started on a continuous subcutaneous infusion were opioid-naïve and commenced on a median morphine equivalent dose of 10 mg/24 hours (range 10–15 mg).
Of 21 patients who were already on a continuous subcutaneous infusion, 9 had their medications altered. The sedative in the continuous subcutaneous infusion was always increased, and to achieve this three patients required a combination of midazolam and levomepromazine. For one patient who was already on 60 mg midazolam together with 100 mg levomepromazine, phenobarbitone was added as a third drug to manage distress.
Symptom management before mechanical ventilation was removed
The approach to symptom management outlined in the APM guidance is based on the rapidity of distress when NIV was removed for daily tasks. For 7 patients the intention was augmented symptom management, enabling the patient to be sleepy but still aware, and for 39 patients (including all TV patients) the intention was to achieve a total loss of awareness through sedation.
Five patients had no additional medications for symptom management at the initiation of mechanical ventilation withdrawal. For three patients who were unresponsive (to voice, touch and pain), no additional symptom management was thought to be required. One patient had made an abrupt decision to stop ventilation (refused to have the mask back on) and one patient chose not to have anticipatory medication.
Medications were most commonly administered subcutaneously, but five clinicians started with intravenous administration and six clinicians changed to this route at some point in the withdrawal process in order to gain a more rapid response to medications than had been achieved by subcutaneous administration.
The majority (37 of 41) of patients requiring medication received a combination of drugs. Most commonly (27 of 37 patients) this comprised an opioid and midazolam, but 10 patients also received levomepromazine. Two patients received only midazolam, but both were receiving a background infusion of opioid. Two patients received only an opioid, but both were receiving a background infusion of midazolam. One patient received phenobarbitone and an opioid. This patient was already receiving a background infusion of opioid, midazolam, levomepromazine and phenobarbitone.
For those patients where sedation was the intention, clinicians judged whether the ventilation was safe to be withdrawn in the following ways (as indicated in the proforma):
Loss of eyelash/corneal reflex (n=5).
No apparent response to touch or pain (n=23).
No apparent response to voice (n=5).
The patient was asleep/lightly conscious (n=4).
The patient looked calm (n=2).
For the six patients where augmented symptom management was the intention the clinician judged the time for removal in the following ways:
Loss of eyelash/corneal reflex (n=1).
The patient was drowsy but awake (n=2).
The patient was asleep/lightly conscious (n=1).
The patient looked calm (n=1).
The patient chose the time when they felt comfortable (n=1).
No clinicians indicated using an alternative or additional methodology for this assessment.
A median and mode of two doses of medication were needed before ventilation was withdrawn, but there was considerable variation in patient requirements, with 10 of 41 (24%) patients requiring only one dose and one person requiring nine doses.
Symptom management after withdrawal of mechanical ventilation
Of the five patients who received no medication before the mechanical ventilation was withdrawn, only one required no medication before they died. Three of these patients received a single combined administration of midazolam and opioid, and one received two combined administrations.
Of the 41 patients who received prewithdrawal medications, 73% required either no further medication (n=19) or only one dose (n=11) after their mechanical ventilation was withdrawn. However, five patients required two doses and six required three doses to ensure their comfort. Table 2 shows the reasons that clinicians provided as to why they judged that the patients required additional medication.
Table 2.
Reasons why the clinician decided to administer medication after mechanical ventilation had been withdrawn
| Slight distress and movement. | More alert, mild distress. | Respiratory rate 40, patient trying to speak, looked in acute distress and frightened. | Although thought to probably be comfortable, he had subtle flickering of eyelids—not clear if it represented reflex/involuntary movements or distress. Brow smooth. |
| Transient twitching of mouth and one eye open briefly. Very brief movement of mouth and eye after 5 min, gave preprepared medication subcutaneously. Response settled spontaneously within a minute. | Eyes open, peripheral cyanosed breathing appeared an effort. Distressed. | He started deteriorating after 30 min. Tachypnoea, secretions, respiratory rate 28, distressed. | |
| Distress. | Patient roused and asked for help. Patient appeared restless. Not fully settled. |
Grimacing. | Appeared distressed, change in facial expression, open eyes, altered breathing. |
| Anxiety and shortness of breath. | Laboured breathing, although not obviously distressed. | Patient showed signs of distress. | Eyes opened, appeared distressed. |
| Respiratory distress, gasping, some agitation. | Not drowsy enough, slightly agitated. | On switching off machine, patient appeared distressed and moved his arms. | Although thought to probably be comfortable, he had subtle flickering of eyelids—not clear if it represented reflex/involuntary. |
| Looked unsettled and family starting to get anxious that he was distressed. | Heavier breathing, doses administered as mask came off. | Became a little agitated. | More alert and moving arms. |
| Sedation. | Patient comfort. | Movements or distress. Brow smooth. | Moved eyebrows. |
Drug doses
There was considerable variation in the doses of drugs required to manage patients’ symptoms. In addition to any ‘background’ opioid in continuous subcutaneous infusion or in patch formulation, the total parenteral morphine equivalent dose required by the 46 patients from the start of mechanical ventilation withdrawal to the time of death ranged from 0 mg to 60 mg. Excluding the ‘0 mg’ patients (n=6), the mean dose was 26.1 mg, with almost 50% of patients requiring a total parenteral morphine equivalent dose of between 10 mg and 25 mg. There was very little difference between those patients who were opioid non-naïve and opioid-naïve, with mean total parenteral morphine equivalent dose of 23.7 mg and 22.9 mg, respectively.
The mean dose of midazolam, in addition to any continuous subcutaneous infusion ‘background’, was 25.8 mg, with a mode (n=10) of 10 mg and ranging from 0 mg (n=2) to 120 mg. Of the 46 patients, 12 required levomepromazine to manage symptoms during withdrawal of mechanical ventilation. In all but one patient, this was in addition to the use of midazolam.
Clinicians reported only three instances of symptoms that were challenging to manage. One reflected that the level of sedation had not been adequate before the mechanical ventilation was removed. The other two patients required high doses and combinations of sedative medication to achieve a sufficient level of reduced awareness.
Duration of the withdrawal process
For the 41 patients who required symptom management before removal of mechanical ventilation, the median time needed was 47.5 min. For the most common (n=31) group of patients (those using NIV who required sedation), the median duration before mechanical ventilation withdrawal was 70 min. The four TV patients showed considerable variation in the time needed before removal of mechanical ventilation (0–275 min) as did those who required augmented symptom management (5–720 min).
All four TV patients died within 30 min of mechanical ventilation removal, but there was very considerable variation in this time for the 42 patients using NIV. While the mode (n=14) was 5–15 min and the median around 30 min, four lived for more than 5 hours, three of them despite being unable to manage more than a few minutes without NIV. Patients who were reported as being able to manage a few hours off their NIV before symptoms arose (n=3) lived for 30 min to 54 hours after withdrawal of their mechanical ventilation. Patients where the intention was augmented symptom management lived for 20 min to 54 hours after their mechanical ventilation was withdrawn.
For the majority of patients (60%), the whole process, from the decision to actively start the withdrawal process to patient death, took 2 hours or less, and the mean duration was around 5 hours. For just over 10% of patients, however, the process was much longer, notably beyond a working day.
Outcomes for the family
Clinicians reported that there were difficult reactions from family members in six cases. These related to the following:
The family not being in full agreement with the patient’s decision.
The family being upset by potential signs of patient distress.
The family being upset by profound cyanosis.
The outcome for the family was indicated by the clinician according to predefined categories as ‘positive’ in 38 cases, distressed but normal grieving in 2 cases, and difficult and beyond their experience of normal grieving in 5 cases (missing data for 1 case).
For the five families that had apparent difficulties, additional comments by the clinician and record of family feedback provide insight into this.
“Could have been better warned that death may not be immediate.”
“Difficult as it was unplanned and wife had mental health issues. Daughter and son very composed.”
“No advance decision to refuse treatment. Next of kin had lasting power of attorney. Starting the NIV was a best interests decision and perhaps improved discussions with family about NIV withdrawal when NIV first considered would have helped.”
“Family very supportive of patient’s decision.”
“They felt very well supported by NIV team – I believe he waited until we were there.”
“Next of kin thought patient would ‘fall asleep’. In fact, he was awake for majority of the time. Next of kin would have liked it to occur at home in the evening but due to staffing and that the patient too poorly to transfer, not possible.”
“They were distressed but grateful I think for how it was handled and thanked us for kindness and time. The biggest thing was having time available and both staff members did not have anything booked for the whole day. This time was useful and essential.”
Feedback from families for whom the clinician perceived that the experience was positive focused on a number of themes:
That the death was peaceful and dignified: “Surprised how peaceful/dignified. Very pleased.”
That the patient had achieved what they wanted: “Very grateful for the way it was managed - they said they didn’t feel it could have been managed any better and that they were pleased that he had still been involved in decision making and in control right up until the last.”
That the support from the team was strong: “They were pleased they were supported by a team they knew well and grateful to be able to support the patient in what were his long term wishes.”
Personalised care for them and the patient:
”They chose to leave the room while the machine was switched off. As he was so settled after the mask was removed, they were given the option to come back in, which they did and very much appreciated being with him while he died in a relaxed manner with no mask. They were relieved that he was relaxed and stated he wasn’t suffering anymore. Appreciated all the support they had received.”
”They found the explanation of legal right to choose to stop medical treatment as distinct from assisted suicide very helpful to enable them to discuss with others. They were very relieved and grateful that their loved one had had a very peaceful death and said it had been just as he would have wanted, and therefore, how they wanted too.”
Outcomes for the lead clinician
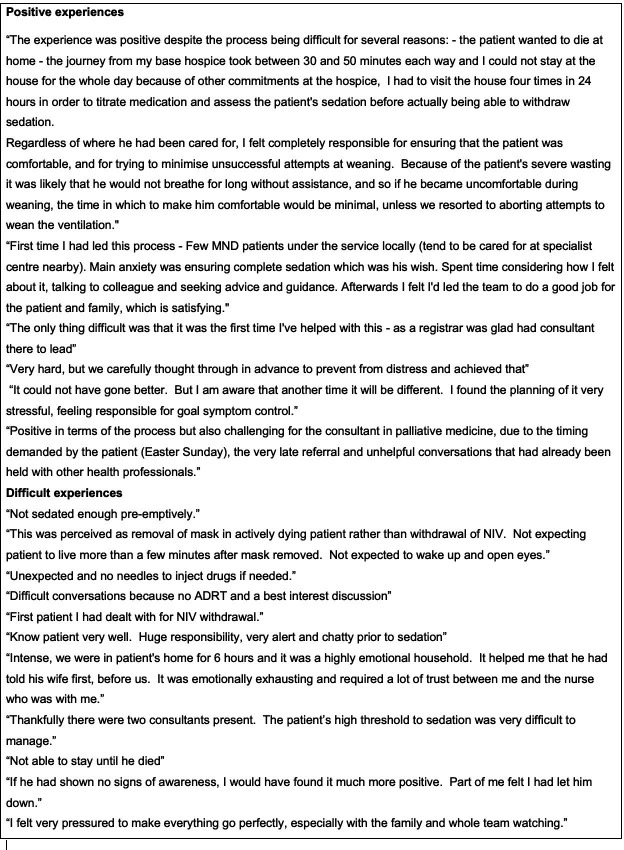
The outcome for the clinician completing the proforma was indicated according to predefined categories as ‘positive’ in 30 cases. Four clinicians were ‘neutral’, expressing that the experience was more stressful and impactful than most deaths. Eleven clinicians found the experience ‘difficult’. Some provided detailed reflection on their experience, as shown in figure 1.
Figure 1.
Reflections by clinicians on their experience. ADRT, advance decision to refuse treatment; MND, motor neuron disease; NIV, non-invasive ventilation.
Discussion
This is the largest data set reported to date in the UK or internationally across multiple care services concerning the withdrawal of mechanical ventilation from patients with MND. The findings provide key and hitherto unknown information that will allow informed discussions with patients and families about what may happen, how long it may take for symptoms to be well managed before the mask or ventilation equipment is removed, and how long it may be before the person dies after the ventilation has been stopped. This study also provides important new evidence to inform debates pertaining to suffering, dignity and control at the end of life with MND.8
The individual patient and family scenarios varied considerably, and the care patients required presented an array of challenges. The evidence base prior to this paper concerning the drugs and the doses to be used that constitutes effective, proportionate, defensible practice in anticipation of symptoms is very limited. This paper reports an evaluation of practice and shows that the use of medications was individualised, aligned with the suggested starting point of the APM guidance and titrated according to patient need. Most practitioners delivered medication via the subcutaneous route. This reportedly enabled the end of life care processes for these patients to feel similar to those of other patients and to reduce the feeling of it being more complex or extraordinary. There is no one-size-fits-all, and the findings describe proportionate, titrated, individualised symptom management and effective personalised care. The reflections of clinicians in figure 1 provide some insights into this. The six patient case series of Messer et al 9 (some of whom were subsequent to the publication of the APM guidance and are included in the 46 data sets of this paper) provides some detail into how this personalised care is enacted in practice.
Table 2 identifies that the decisions to administer medication(s) to manage symptoms after withdrawal of mechanical ventilation were based on a number of clinical judgements. It would be useful if there were more robust and validated decision-making aids to guide this. The Respiratory Distress Observation Scale is designed to provide such guidance when patients are unable to self-report breathlessness.10 However, this scale relies on intact respiratory and facial muscle functions, which were sometimes not present in the patients of this evaluation. No clinicians reported using the patient’s pulse rate as a barometer of distress. Such measures may be a useful addition to guidance and for future evaluation of the processes and outcomes of care.
The opioid and sedative doses in this evaluation contrast remarkably with the two previous published case series. Dreyer et al 11 reviewed withdrawal of TV from patients with MND in Denmark over 10 years. Sedation was intentionally achieved before the withdrawal of ventilation using morphine (median 100 mg, range 60–400 mg) and diazepam (median 100 mg, range 20–120 mg). Meyer et al 12 published a case series from Berlin of nine patients where the cumulative dose of morphine was 185–380 mg for patients who had residual respiratory function and 120 mg for patients with minimal spontaneous breathing.
In Dreyer et al’s review,11 the mean time to death after discontinuation of ventilation for patients receiving augmented symptom managment was 32.6 hours (range 0.33–164 hours) and for those receiving sedation a mean of 0.31 hours (range 0.15–0.63 hours). These compare with our figures of time from withdrawal to death of 0.27–54 hours and 0.1–10 hours, respectively.
There are some potential limitations to this evaluation. While we have been able to review 46 geographically widespread cases of this rare area of care provided by 37 clinicians, it is likely that this is an incomplete data set for England in the 35 months. A key question is whether it is accurate that only palliative medicine and nurse/allied health professional ventilation specialists undertake withdrawal of mechanical ventilation. Reports from neurologists or other physicians, for example, are absent in this evaluation. It is strongly recommended, however, that palliative care is involved with patients with MND early in their illness, and commencement of mechanical ventilation is a trigger point for such referral if not already established. This case series might indicate palliative care support is in place for all patients withdrawing from ventilation and could be a marker of excellent patient pathways.
While an incomplete or unrepresentative data set has implications for the generalisability of some conclusions concerning what has happened to patients, the overall finding, that a peaceful death with symptoms well managed can be achieved, provides an important evidence base for clinicians to inform their practice and their discussions with patients and their families.
Conclusion
This study provides new information to inform discussions with patients and preparation within the clinical team. The APM guidance provides a sound basis for care that will achieve good symptom management. The dose of medications required by patients is variable, and medications need to be individualised using a proportionate and titrated approach. The duration of the withdrawal process was also variable, but for 60% this was less than 2 hours.
Acknowledgments
The authors thank the 37 clinicians who submitted their data. The members of the APM guidance development are acknowledged for their work in developing the data collection proforma and commenting on the findings of the evaluation in report form. The MNDA supported data collection through promotion of the project through clinical networks.
Footnotes
Contributors: CF with others designed the study. CF and DW collated and analysed the data and drafted the paper.
Funding: Some funding for CF’s time was provided by the Motor Neurone Disease Association (MNDA), and other funding was provided by the employing organisation LOROS Hospice, Leicester.
Disclaimer: The funders had no role in the study design, analysis or interpretation of the data.
Competing interests: CF has received other competitive grant funding from the Motor Neurone Disease Association.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This was an anonymised evaluation of care and did not require research ethics approval.
References
- 1. R v Bodkin Adams [1957] CLR 365.
- 2. House of Lords debate re Annie Lindsell. Hansard HL 1997:721–4. [Google Scholar]
- 3. Faull C, Rowe Haynes C, Oliver D. Issues for palliative medicine doctors surrounding the withdrawal of non-invasive ventilation at the Request of a patient with motor neurone disease: a scoping study. BMJ Support Palliat Care 2014;4:43–9. 10.1136/bmjspcare-2013-000470 [DOI] [PubMed] [Google Scholar]
- 4. Phelps K, Regen E, Oliver D, et al. Withdrawal of ventilation at the patient's Request in MND: a retrospective exploration of the ethical and legal issues that have arisen for doctors in the UK. BMJ Support Palliat Care 2017;7:189–96. 10.1136/bmjspcare-2014-000826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Faull C. Withdrawal of assisted ventilation at the Request of a patient with motor neurone disease. Association for palliative medicine, 2015. Available: https://apmonline.org/committee-pages/apm-professional-guidelines/ [Accessed 20 Jul 2019].
- 6. Withdrawal of assisted ventilation at the Request of a patient: audit of process and outcomes, 2015. Available: https://apmonline.org/committee-pages/apm-professional-guidelines/ [Accessed 20 Jul 2019].
- 7. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 8. Noel Conway v Secretary of State for Justice [2017] EWHC 2447. Available: https://www.supremecourt.uk/docs/r-on-the-application-of-conway-v-secretary-of-state-for-justice-court-order.pdf [Accessed 20 Jul 2019].
- 9. Messer B, Armstrong A, Doris T, et al. Requested withdrawal of mechanical ventilation in six patients with motor neuron disease. BMJ Support Palliat Care 2020;10:10–13. 10.1136/bmjspcare-2017-001464 [DOI] [PubMed] [Google Scholar]
- 10. Campbell ML, Templin T, Walch J. A respiratory distress observation scale for patients unable to self-report dyspnea. J Palliat Med 2010;13:285–90. 10.1089/jpm.2009.0229 [DOI] [PubMed] [Google Scholar]
- 11. Dreyer PS, Felding M, Klitnæs CS, et al. Withdrawal of invasive home mechanical ventilation in patients with advanced amyotrophic lateral sclerosis: ten years of Danish experience. J Palliat Med 2012;15:205–9. 10.1089/jpm.2011.0133 [DOI] [PubMed] [Google Scholar]
- 12. Meyer T, Dullinger JS, Münch C, et al. Elektive termination Der Beatmungstherapie bei Der amyotrophen Lateralsklerose. Nervenarzt 2008;79:684–90. 10.1007/s00115-008-2439-9 [DOI] [PubMed] [Google Scholar]