Abstract
Introduction:
While risk factors for cigarette smoking among youth and young adults are well-documented, less is known about the correlates of initiation of other tobacco products. This study aims to provide estimates and correlates of initiation among U.S. youth and young adults.
Methods:
Data on youth aged 12–17 (n=10,072) and young adults aged 18–24 (N=5,727) who provided information on cigarettes, electronic nicotine delivery systems (ENDS), cigars, pipe, hookah and smokeless tobacco use in Wave 1 (W1: 2013–2014)-Wave 4 (W4: 2016–2018) of the nationally-representative PATH Study were used to calculate ever use initiation and correlates of initiation by W4.
Results:
Nearly 6 million youth and 2.5 million young adults used tobacco for the first time between W1–W4. Approximately one quarter of youth and young adult ENDS never users initiated ENDS between W1–W4 of the PATH Study. Among youth, use of other tobacco products, ever substance use, and high externalizing problems were associated with initiation of most products. Among young adults, use of other tobacco products and ever substance use were associated with initiation of most products. In both youth and young adults, Hispanics were more likely to initiate hookah use than their non-Hispanic White counterparts. While male sex was a risk factor for most tobacco product initiation across both age groups, it was not associated with hookah initiation.
Conclusions:
Cigarette and non-cigarette products shared many correlates of initiation, although there are noteworthy demographic differences. Findings can help tailor product specific interventions to reach populations at risk during preliminary stages of use.
1. INTRODUCTION
Cigarette smoking usually begins in youth and young adulthood; few U.S. adult daily cigarette smokers began smoking after age 25.1 While the prevalence of cigarette smoking in the U.S. has declined over time,1 nationally-representative, cross-sectional estimates from the National Youth Tobacco Survey (NYTS), the National Health Interview Survey (NHIS) and Monitoring the Future (MTF) have shown that use of some non-cigarette products such as electronic nicotine delivery systems (ENDS) has risen dramatically in recent years, particularly among youth and young adults.1–3 However, there is currently little research published from longitudinal studies reporting incidence and risks factors for initiation among two groups with high use estimates, youth and young adults.
Although stages of use have not been defined for many non-cigarette products, the underlying stages in the pathway from never use to established use of cigarettes have been defined as progression from non-use preparation stages such as susceptibility, followed by initiation/trial, experimentation, regular use to established use.4 In this paper we focus on new use (initiation) among 1) never users of each individual product (never product-specific users at Wave 1 [W1]) and 2) those who had never used any type of tobacco products (tobacco-naïve at W1). From a public health perspective, information is needed on factors that predict initiation of individual products to determine the impact of public health regulatory actions on non-users and the likelihood of use of each product.5
Correlates of cigarette smoking have been summarized previously,6,7 and although longitudinal data on correlates of non-cigarette use are growing,8–10 more research on other non-cigarette products such as ENDS, cigars, pipe, hookah and smokeless tobacco, and factors associated with initiation can help researchers and policy makers target interventions. Many studies in youth found that demographics, previous tobacco use, previous substance use, familial and peer influences, and mental health problems are associated with cigarette smoking,4,6 but fewer studies have examined these factors across multiple tobacco products in the same sample of individuals longitudinally. The exception is Kasza et al., who recently documented correlates of initiation across products through Wave 3 [W3] of the PATH Study, finding that previous tobacco use consistently predicted tobacco product initiation, and some demographic predictors (sex, race/ethnicity and sexual orientation) varied across products.11 Other studies have found that correlates of non-cigarette products have included alcohol use,12,13 exposure to others using the products,14–16 mental health,9 peer use,7 and receptivity to tobacco advertising.8
The aim of this study is to expand upon previous PATH Study analyses5,8,9,11,14,17–20 by presenting population estimates of tobacco product initiation and correlates of initiation of each product among youth and young adults between W1 (2013–2014) and Wave 4 (W4, 2016-Jan 2018). Specifically, this study adds to the current literature by providing estimates through a more recent follow-up period and including a larger number of potential correlates. Understanding commonalities and differences between tobacco products, not just in demographic characteristics, but also psychosocial risk factors for new tobacco use may help researchers and public health analysts prevent future tobacco use by focusing on the most frequently used new products and unique risk factors for use of each product.
2. METHODS
The PATH Study is a large, nationally representative, longitudinal study of tobacco use and health among youth and adults in the U.S. A detailed description of the PATH Study design and methodology has been published elsewhere.21 Details on interviewing procedures, questionnaires, sampling, weighting, response rates, and accessing the data are described in the PATH Study Restricted Use Files User Guide at https://doi.org/10.3886/Series606. The study was conducted and approved by Westat and the Westat Institutional Review Board. All respondents ages 18 and older provided informed consent, with youth respondents ages 12 to 17 providing assent while each one’s parent/legal guardian provided consent.
The PATH Study W2–W4 data collection protocols followed procedures to interview each respondent close to the 1-year anniversary of their participation in the prior wave. Interviews were sometimes conducted earlier or later, due to varying circumstances, including respondents’ schedules, time needed to contact respondents, and grouping of multiple respondents within a household, thus resulting in some variance in time between interviews (means for youth and adults at each wave ranged from 50 to 54 weeks). Data collection was conducted from September 2013 to December 2014 (W1), October 2014 to October 2015 (W2), October 2015 to October 2016 (W3) and December 2016 to January 2018 (W4). At W1, an additional “shadow sample” of youth ages 9 to 11 was selected to be interviewed at later waves when they aged up to 12 years and is referred to throughout this manuscript as “shadow youth.” See more details at https://doi.org/10.3886/Series606.
Supplemental Table 1 shows weighted response rates (conditional upon W1 participation). Differences in the number of completed interviews between W1 and subsequent waves reflect attrition (e.g., nonresponse, mortality) and the aging of shadow youth to youth and of youth to adults. The unweighted attrition rates among the entire W1 sample (adults and youth combined) are 16% at W2, 21% at W3, and 27% at W4.
2.1. Study Population
The current study analyzes data from the restricted use files (RUF) among all young adults and youth. The sample includes W1 youth ages 12–17 years (n=10,072) and W1 young adults ages 18–24 years (n=5,727) who provided information on tobacco use at W1 through W4. Age groups are defined by a participant’s age at baseline W1. Participants were excluded from the final analysis if their reported age at W2 was younger than their reported age at baseline, if there was a difference of more than two years in self-reported age between W1 and W2 (n=14 youth, n=12 young adults), or they were lost to follow up in the following waves (n=1,906 youth, n=1,582 young adults). Supplemental Table 4 presents information on a subset of W3 youth and young adults (based on W3 age) in order to present initiation estimates for the latest two waves of youth and young adult data available (W3 and W4).
2.2. Tobacco Use Measures
At baseline, all respondents were asked a series of questions regarding ever use of the following tobacco products: cigarettes, ENDS, traditional cigars, cigarillos, filtered cigars, pipe, hookah, snus pouches, other smokeless tobacco (e.g., loose snus, moist snuff, dip, spit, chewing tobacco), and dissolvable tobacco. Product images and brief descriptions, including common brand names, were provided to aid respondents (available at http://doi.org/10.3886/ICPSR36231). Youth were asked about bidis and kreteks use, but adults were not; therefore, these products were excluded from the analysis, unless otherwise specified.
At each follow-up wave all continuing respondents were asked if they had used each product in the past 12 months (initiation). The PATH Study instrument was updated, and questions were changed from asking about e-cigarettes to asking about all ENDS products between W1 and W2. However, for clarity, only the term “ENDS” is used throughout this manuscript.
Construction of variables is described in Appendix A.
2.4. Statistical Analysis
Full-sample and replicate weights were created that adjust for the complex sample design (e.g., oversampling at W1) and nonresponse at W1–W4. PATH Study W1 Cohort weighted estimates represent the U.S. resident population ages 12 years and older at the time the specific data examined were collected (i.e., W1, W2, W3, or W4) who were in the civilian, noninstitutionalized population at W1. This analysis used W4 all-waves weights to obtain statistically valid estimates from longitudinal analyses that examine W1 Cohort data across all waves, 1 through 4. In-depth information about the design of the W1 Cohort is also available at https://doi.org/10.3886/Series606.
All initiation estimates and risk ratios for correlates were calculated using the follow-up longitudinal population and replicate weights that adjusted for the complex study design characteristics (e.g., oversampling at W1) and nonresponse in SAS (version 9.4) survey procedures for proportions and SAS-callable SUDAAN (version 11.0.3) for logistic regressions.
Where presented, variances and 95% Wilson confidence intervals (CIs) of the estimates were calculated using balanced repeated replication (BRR) weights with Fay’s adjustment of 0.3. All estimates with an unweighted denominator <50 or a relative standard error (RSE) ≥30% were flagged. Weighted multiple logistic regressions modeled the associations between correlates and initiation use of each tobacco product. Significance level was set at p<0.05.
We conducted a sensitivity analysis to understand the role of missing covariates on the results. The percentage of missing covariates ranged by product from 12.0% to 14.1% among youth and from 7.8% to 8.4% among young adults. Specifically, this sensitivity analysis used multiple imputation and includes three steps: (1) We imputed five datasets without missing covariates using fully conditional specification method with an arbitrary missing data pattern; (2) We analyzed the five datasets using our original analysis; and (3) We combined the results from the 5 datasets using the traditional approach by Rubin (1987) and Barnard and Rubin (1999).22,23
3. RESULTS
Overall, nearly 6.0 million (32.5%) youth and approximately 2.5 million (25.9%) young adult W1 never tobacco users initiated any tobacco use by W4 (Supplemental Table 2). Among W1 never users of each product, initiation was highest for ENDS in youth (26.7%) and young adults (25.0%) (Figure 1, Supplemental Table 2). In youth, among W1 never users of each specific product, prevalence of initiation in descending order was ENDS, followed by cigarettes (15.8%), cigars (14.4%), hookah (11.8%), smokeless tobacco (6.0%) and pipe (2.6%). Comparatively, in young adults, the order was ENDS, followed by hookah (16.0%), cigars (15.0%), cigarettes (13.5%), pipe (3.4%) and smokeless tobacco (3.3%). Initiation of dissolvable tobacco was less than 1% in both youth and young adults. In general, by W4, the percent of new product use was higher among youth and young adults who had ever used tobacco at W1 than tobacco naïve youth and young adults at W1; however, weighted n’s of some products were higher due to larger denominators among never users (Supplemental Table 3).
FIGURE 1:
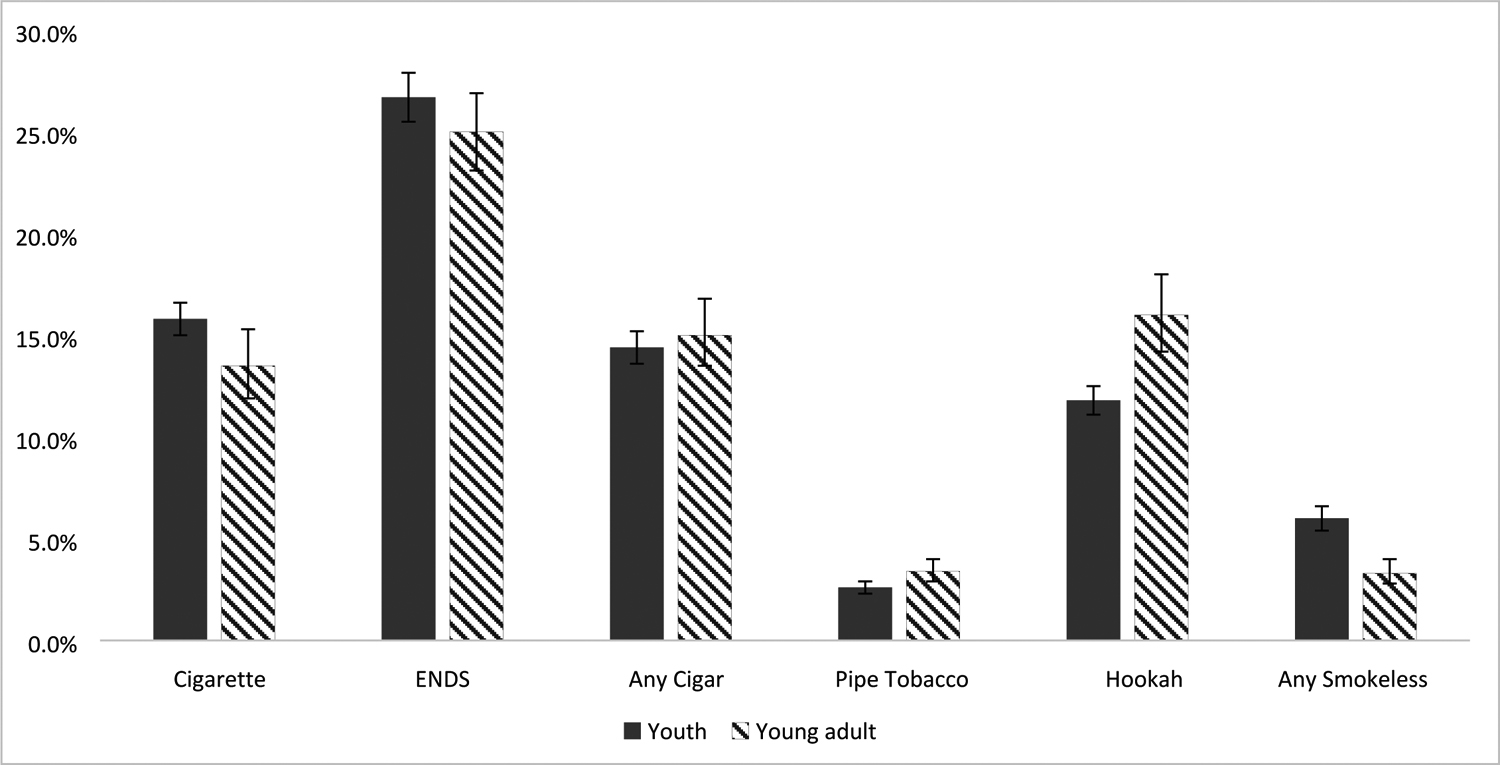
PATH Study New Use by Wave 4 (2016-Jan 2018) Among Wave 1 (2013–2014) Never Users of Each Product
1A number of W1 youth never users of a product were missing item-level data for tobacco use status at W2–W4 (n=14 cigarette, n=48 ENDS, n=67 any cigar, n=44 pipe tobacco, n=26 hookah, n=181 any smokeless tobacco). A number of W1 young adult never users of a product were missing item-level data for tobacco use status at W2–W4 (n<5 cigarette, n=37 ENDS, n=0 any cigar, n<5 pipe tobacco, n<5 hookah, n=12 any smokeless tobacco).
2 This figure includes youth (12–17 years) and young adults (18–24 years) who had never used the specific product in question but may have used other products in the past.
3 Raw n’s, weighted n’s and weighted percentages are available in Supplemental Table 2.
4 Any cigar use = respondents who had ever used any of the three types of cigars (traditional cigars, cigarillos, and filtered cigars)
5 Any smokeless tobacco use = respondents who had ever used either snus pouches or other smokeless tobacco, not including dissolvable tobacco (which was asked as a separate category)
6 Due to the small number of new dissolvable tobacco users at W4, dissolvable tobacco has been removed from the figure.
Supplemental Table 4 shows weighted estimates for initiation of each product from W3 to W4 (among youth and young adults in W3). Like the W1–W4 estimates, initiation in youth was highest for ENDS (6.6%), followed by cigarettes (4.3%), cigars (3.6%), hookah (1.7%), smokeless tobacco (1.4%) and pipe (0.6%). In young adults from W3–W4, similar estimates of young adult nonusers initiated use of cigarettes (5.8%), ENDS (5.5%) and cigars (5.0%), followed by hookah (3.9%), smokeless tobacco (1.6%) and pipe (1.0%).
Table 1 shows adjusted risk ratios of associations between correlates and tobacco use initiation from W1–W4 weighted logistic regression models among youth. Male youth were more likely than females to initiate cigarettes, ENDS, cigars, pipe and smokeless tobacco; however, female youth were more likely than males to initiate hookah. Youth ages 15–17 years (vs. 12–14 years) were more likely to initiate cigarettes, ENDS, cigars or hookah but there was no association between age and pipe or smokeless tobacco initiation. Compared to non-Hispanic White youth, non-Hispanic Black youth were less likely to be initiators of cigarettes, ENDS, pipe and smokeless tobacco but no association was seen with hookah or cigars. Hispanic youth were less likely than non-Hispanic White youth to initiate ENDS, cigars, pipe tobacco and smokeless tobacco but more likely to initiate hookah (no association was seen with cigarettes). Previous use of other tobacco products and ever alcohol use was associated with initiation by W4 for each individual tobacco product. Ever marijuana use was associated with initiation of cigarettes, ENDS, cigars and hookah, but no association was seen with pipe or smokeless tobacco. Past year psychosocial problems, specifically high severity externalizing problems (such as having a hard time paying attention, lying to get what you want and starting a physical fight), were associated with initiation of all products except pipe, while high severity internalizing problems (such as depression, anxiety, and trouble sleeping) were only associated with ENDS initiation. Exposure to tobacco use in the household or exposure to others who smoked cigarettes in the past seven days was associated with initiation of cigarette, ENDS, and cigars. Household use but not exposure to others who smoked cigarettes in the past 7 days was associated with smokeless tobacco initiation.
TABLE 1:
Factors Associated with Initiation by PATH Study W4 among W1 Youth Never Users, by Tobacco Product
| Adjusted Relative Risk (95% Confidence Interval) of W2–W4 Initiation | ||||||
|---|---|---|---|---|---|---|
| Wave 1 | Cigarettes 1,326 Initiators1 | ENDS 2,278 Initiators2 | Any Cigar 1,223 Initiators3 | Pipe Tobacco 244 Initiators4 | Hookah Use 1,035 Initiators5 | Any Smokeless 510 Initiators6 |
| Demographics | ||||||
| Male vs. Female | 1.2 (1.1–1.4) | 1.2 (1.1–1.3) | 1.8 (1.6–2.0) | 2.3 (1.7–3.1) | 0.9 (0.8–1.0) | 3.4 (2.7–4.3) |
| Age 15–17 years vs. 12–14 years | 1.5 (1.3–1.7) | 1.2 (1.1–1.3) | 2.3 (2.0–2.7) | 1.3 (1.0–1.7) | 2.6 (2.2–3.0) | 1.1 (0.9–1.3) |
| Race/ethnicity7: NH Black vs. NH White | 0.6 (0.5–0.7) | 0.6 (0.5–0.7) | 1.1 (0.9–1.4) | 0.2 (0.1–0.5) | 1.1 (0.9–1.4) | 0.3 (0.2–0.5) |
| Hispanic or Latino vs. NH White | 0.9 (0.8–1.1) | 0.9 (0.8–1.0) | 0.8 (0.7–0.9) | 0.6 (0.4–0.8) | 1.3 (1.1–1.5) | 0.4 (0.3–0.6) |
| NH AI or AN or more than one race vs. NH White | 0.7 (0.6–0.9) | 0.8 (0.7–0.9) | 0.7 (0.6–0.9) | 1.0 (0.6–1.6) | 1.2 (1.0–1.5) | 0.3 (0.2–0.5) |
| Previous Substance Use at W1 | ||||||
| Previous vs. No Tobacco Use | 1.8 (1.6–2.1) | 1.6 (1.4–1.8) | 1.6 (1.4–1.9) | 3.6 (2.3–5.7) | 1.6 (1.3–1.9) | 2.5 (2.0–3.2) |
| Ever vs. Never Alcohol Use | 1.5 (1.3–1.8) | 1.7 (1.5–1.8) | 1.7 (1.5–2.0) | 1.6 (1.1–2.3) | 1.8 (1.6–2.1) | 1.4 (1.1–1.8) |
| Ever vs. Never Marijuana Use | 1.5 (1.3–1.8) | 1.4 (1.2–1.6) | 1.6 (1.3–1.8) | 1.1 (0.8–1.6) | 1.6 (1.3–2.0) | 1.1 (0.8–1.4) |
| Psychosocial (High GAIN Subscale Score) | ||||||
| Substance Use | 1.0 (0.6–1.6) | 1.5 (1.1–2.1) | 1.1 (0.8–1.6) | 1.4 (0.9–2.3) | 1.3 (0.9–1.8) | 1.4 (0.9–2.2) |
| Internalizing | 1.1 (0.9–1.3) | 1.2 (1.1–1.3) | 1.1 (1.0–1.2) | 0.7 (0.5–1.1) | 0.9 (0.8–1.1) | 0.9 (0.7–1.1) |
| Externalizing | 1.4 (1.2–1.6) | 1.3 (1.2–1.4) | 1.3 (1.1–1.5) | 1.3 (0.9–1.8) | 1.2 (1.1–1.4) | 1.3 (1.1–1.7) |
| Exposure to Other’s Use of Tobacco | ||||||
| Household use | 1.3 (1.1–1.4) | 1.2 (1.1–1.3) | 1.2 (1.1–1.4) | 1.0 (0.7–1.3) | 1.0 (0.9–1.2) | 1.6 (1.2–2.0) |
| Others smoking in the past 7 days | 1.3 (1.2–1.5) | 1.2 (1.1–1.3) | 1.2 (1.1–1.3) | 1.4 (1.0–2.0) | 1.1 (1.0–1.3) | 1.2 (0.9–1.5) |
Each Relative Risk (RR) is adjusted for all other factors in the table; RR in bold represents statistically significantly more (if the RR>1) or fewer (if the RR<1) new users for the tobacco product for the group vs. the reference group; Due to rounding up or rounding down, some RRs are statistically significant even if their 95% CIs appear to include 1.
n=145 new W2–W4 past 12-month cigarette users were missing covariates and were not included in the model.
n=262 new W2–W4 past 12-month ENDS users were missing covariates and were not included in the model.
n=98 new W2–W4 past 12-month any cigar users were missing covariates and were not included in the model.
n=30 new W2–W4 past 12-month pipe users were missing covariates and were not included in the model.
n=112 new W2–W4 past 12-month hookah users were missing covariates and were not included in the model.
n=63 new W2–W4 past 12-month any smokeless tobacco users were missing covariates and were not included in the model.
NH = Non-Hispanic; AI = American Indian; AN = Alaskan Native, Asian, Native Hawaiian, other Pacific Islander
Any cigar use = respondents who had ever used any of the three types of cigars (traditional cigars, cigarillos, and filtered cigars).
Any smokeless tobacco use = respondents who had ever used either snus pouches or other smokeless tobacco, not including dissolvable tobacco (which was asked as a separate category).
Due to the small number of new dissolvable tobacco users at W4 dissolvable tobacco has been removed from the table, although dissolvable tobacco remains one of the products included in the any tobacco use and other tobacco use variables.
Table 2 shows adjusted results from W1–W4 weighted logistic regression models among young adults. Young adult males were more likely to initiate each product except hookah than females and young adults ages 18–20 years (vs. 21–24 years) were more likely to initiate each tobacco product. Non-Hispanic Blacks were more likely than non-Hispanic Whites to initiate cigars or hookah, but non-Hispanic Whites were more likely to initiate smokeless tobacco. Hispanics were more likely to initiate cigarettes, ENDS, hookah and less likely to use smokeless tobacco than non-Hispanic Whites. Previous tobacco use was associated with new initiation of each product. Ever alcohol and ever marijuana use were associated with initiation of cigarettes, ENDS, cigars and hookah, but no association was seen with pipe or smokeless tobacco. Household exposure to tobacco and exposure to other smokers in the past seven days was associated with initiation of ENDS. Exposure to household tobacco use was associated with smokeless tobacco and pipe initiation.
TABLE 2:
Factors Associated with Initiation by PATH Study W4 among W1 Young Adult Never Users, by Product
| Adjusted Relative Risk (95% Confidence Interval) of W2–W4 Initiation | ||||||
|---|---|---|---|---|---|---|
| Wave 1 | Cigarettes 329 Initiators1 | ENDS 979 Initiators2 | Any Cigar 475 Initiators3 | Pipe Tobacco 208 Initiators4 | Hookah Use 488 Initiators5 | Any Smokeless 175 Initiators6 |
| Demographics | ||||||
| Male vs. Female | 1.6 (1.3–2.1) | 1.2 (1.0–1.3) | 1.7 (1.4–2.1) | 2.4 (1.6–3.5) | 1.1 (0.9–1.4) | 3.8 (2.5–5.8) |
| Age 18–20 years vs. 21–24 years | 2.1 (1.6–2.7) | 1.6 (1.4–1.8) | 1.4 (1.1–1.7) | 1.6 (1.1–2.3) | 1.6 (1.3–2.0) | 1.9 (1.3–2.8) |
| Race/ethnicity7: NH Black vs. NH White | 1.2 (0.8–1.7) | 0.9 (0.7–1.1) | 1.7 (1.3–2.2) | 0.9 (0.6–1.3) | 2.1 (1.7–2.7) | 0.4 (0.3–0.7) |
| Hispanic or Latino vs. NH White | 1.5 (1.2–2.0) | 1.2 (1.1–1.4) | 0.9 (0.7–1.1) | 1.2 (0.8–1.7) | 1.6 (1.2–2.2) | 0.6 (0.4–0.9) |
| NH AI or AN or more than one race vs. NH White | 0.9 (0.6–1.5) | 1.1 (0.8–1.5) | 0.7 (0.5–1.1) | 0.9 (0.5–1.8) | 1.5 (1.0–2.3) | 0.5 (0.3–1.0) |
| Previous Substance Use at W1 | ||||||
| Previous vs. No Tobacco Use | 1.5 (1.2–2.0) | 2.5 (2.0–3.2) | 2.2 (1.6–2.8) | 5.0 (1.9–13.0) | 1.4 (1.0–1.9) | 2.2 (1.0–4.8) |
| Ever vs. Never Alcohol Use | 1.5 (1.1–2.0) | 1.2 (1.0–1.5) | 1.3 (1.0–1.7) | 0.9 (0.5–1.5) | 1.8 (1.3–2.5) | 1.0 (0.6–1.7) |
| Ever vs. Never Marijuana Use | 1.4 (1.0–1.9) | 1.2 (1.1–1.5) | 1.4 (1.1–1.7) | 0.8 (0.6–1.2) | 1.7 (1.2–2.3) | 1.1 (0.7–1.6) |
| Psychosocial (High GAIN Subscale Score) | ||||||
| Substance Use | 3.1 (2.1–4.7) | 1.3 (1.0–1.7) | 1.3 (0.8–2.1) | 2.6 (1.6–4.3) | 1.4 (0.8–2.3) | 1.8 (1.0–3.2) |
| Internalizing | 1.3 (0.9–1.7) | 1.0 (0.8–1.2) | 1.0 (0.7–1.3) | 0.7 (0.4–1.1) | 1.1 (0.8–1.4) | 0.7 (0.4–1.2) |
| Externalizing | 0.7 (0.5–1.0) | 1.1 (0.9–1.4) | 1.1 (0.8–1.4) | 1.1 (0.7–1.8) | 1.0 (0.7–1.3) | 1.1 (0.7–1.8) |
| Exposure to Other’s Use of Tobacco | ||||||
| Household use | 1.2 (0.9–1.6) | 1.2 (1.1–1.4) | 1.0 (0.8–1.3) | 1.4 (1.0–2.0) | 0.9 (0.7–1.1) | 1.7 (1.2–2.6) |
| Others smoking in the past 7 days | 1.3 (1.0–1.7) | 1.3 (1.1–1.5) | 1.1 (0.9–1.3) | 1.5 (1.0–2.4) | 1.2 (0.9–1.5) | 1.4 (0.9–2.4) |
Each Relative Risk (RR) is adjusted for all other factors in the table; RR in bold represents statistically significantly more (if the RR>1) or fewer (if the RR<1) new users for the tobacco product for the group vs. the reference group; Due to rounding up or rounding down, some RRs are statistically significant even if their 95% CIs appear to include 1.
n=21 new W2–w4 past 12-month cigarette users were missing covariates and were not included in the model.
n=71 new W2–W4 past 12-month ENDS users were missing covariates and were not included in the model.
n=34 new W2–W4 past 12-month any cigar users) were missing covariates and were not included in the model.
n=20 new W2–W4 past 12-month pipe users were missing covariates and were not included in the model.
n=39 new W2–W4 past 12-month hookah users were missing covariates and were not included in the model.
n=9 new W2–W4 past 12-month any smokeless users were missing covariates and were not included in the model.
NH = Non-Hispanic; AI = American Indian; AN = Alaskan Native, Asian, Native Hawaiian, other Pacific Islander
Any cigar use = respondents who had ever used any of the three types of cigars (traditional cigars, cigarillos, and filtered cigars)
Any smokeless tobacco use = respondents who had ever used either snus pouches or other smokeless tobacco, not including dissolvable tobacco (which was asked as a separate category)
Due to the small number of new dissolvable tobacco users at W4 dissolvable tobacco has been removed from the table, although dissolvable tobacco remains one of the products included in the any tobacco use and other tobacco use variables.
Results from the sensitivity analysis using multiple imputation for the missing covariates yielded similar results as the complete case analysis. Therefore, the original complete case analysis was presented in the tables.
4. DISCUSSION
This study provides national estimates of tobacco product initiation and correlates of initiation from W1–W4 of the PATH Study among youth and young adults. Most youth and young adults who were tobacco-naïve in W1 remained tobacco naïve over four-year follow-up. However, the absolute number of new tobacco users among youth and young adults is considerable: among never users of any product in W1 of the PATH Study, nearly 6 million youth (32.5%) and an estimated 2.5 million young adults (25.9%) in the U.S. used a tobacco product for the first time by W4. This represents approximately 5,400 youth and 2,300 young adult never tobacco users who initiated tobacco product use each day during three waves of follow-up W2–W4 (approximately 3 years).
In youth, the products with the highest overall initiation from W1–W4 were ENDS, followed by cigarettes, any cigar (including traditional cigars, cigarillos and filtered cigars), hookah, any smokeless and traditional pipe. In young adults, after ENDS, the highest overall initiation was seen for hookah, cigars, and cigarettes followed by pipe and smokeless tobacco. Consistent with results from MTF, new ENDS use among youth and young adults was higher than new cigarette use in W1–W4,24 however cigarette, cigar, and hookah initiation in W1–W4 was over 10% in both youth and young adults, suggesting combustible tobacco product use is still an important public health problem.
We also examined whether previously identified correlates of cigarette smoking were consistent for initiation of non-cigarette products. In youth, the majority of our findings are in line with factors previously associated with tobacco use and initiation.6,11 Our findings suggest although males are at higher risk for initiation of most products, except for hookah where females were at higher risk. This suggests that sex should be considered in hookah education and prevention programs. In addition, our analyses show in both youth and young adults, previous tobacco use, alcohol or marijuana use is associated with new product initiation for most products. This finding is consistent with previous literature and highlights users of alcohol, marijuana and other tobacco products as an at-risk population for new tobacco product initiation.
We found psychosocial problems were associated with initiation of most products in youth, but not young adults. Previous PATH Study analyses of tobacco-naïve youth in W1–W2 found past year internalizing (such as depression, anxiety, and trouble sleeping) and externalizing (such as having a hard time paying attention, lying to get what you want and starting a physical fight) problems were associated with ENDS only initiation, and externalizing problems were associated with cigarette initiation or dual (cigarette/ENDS) initiation.25 Our work confirms that, in youth, both internalizing and externalizing problems are associated with ENDS initiation, and externalizing problems are associated with cigarette initiation, although our sample was not limited to tobacco-naïve youth. Our study extends previous work by finding externalizing problems were also associated with cigar, hookah and smokeless tobacco initiation in youth. We did not see any association between tobacco product initiation and internalizing or externalizing problems among young adults in our study. The results of our study are different than a separate W1–W2 PATH paper which found lifetime internalizing and externalizing problems were associated with initiation in youth and young adults,9 but we used past-year internalizing and externalizing problems.
While other studies have found an association between the exposure to friends or household members using tobacco products and ENDS and cigarettes,26 our study expands upon the finding that exposure to tobacco use by others (household and exposure to others smoking) is an important risk factor for cigarettes and ENDS but also cigars in youth, and household use is an important risk factor for initiation of any smokeless tobacco in youth. Our study did not find an association between these factors for cigarettes in young adults, but did for ENDS, and found household use was a risk factor for smokeless tobacco and pipe initiation in young adults.
For individual products, our findings were consistent with previous studies that have shown similarities between risk factors and correlates of use for cigarettes and ENDS, including exposure to others using the products, psychosocial variables and use of alcohol or marijuana.14–16 Similar to previous studies, we found alcohol use was associated with new hookah use in youth and young adults,12 as was marijuana and previous tobacco use.27 For smokeless tobacco, consistent with other studies of youth, alcohol use was associated with new smokeless tobacco use,13 although the same was not true of young adults. Few studies have examined initiation of cigars in youth, although our study found correlates of initiation for cigars was similar to those of cigarettes.
This study found racial and ethnic demographic differences in tobacco product initiation correlates in U.S. youth and young adults during this time period. First, Hispanics in both age groups were more likely to initiate hookah use than their non-Hispanic White counterparts, a finding that has been documented previously among youth.11 Hispanic young adults were also more likely than their non-Hispanic counterparts to initiate ENDS and cigarettes. Non-Hispanic Black young adults were more likely to initiate cigar use than their non-Hispanic White counterparts. Taken together, these differences by race/ethnicity can inform health messaging that is targeted to young populations at high risk for tobacco initiation. Conversely, Non-Hispanic Black youth are at a lower risk for initiation for almost all tobacco products compared to their Non-Hispanic White counterparts. Future studies examining why Black adolescents delay use could help us understand how to better foster delay in other groups.
Consistent with Kasza et al., previous tobacco use was associated with initiation of all products in youth and young adults.11 This may be due to initiation of one tobacco product decreasing perceived harm and increasing susceptibility and willingness to try other products,28 or due to a higher risk profile for initiation among those initiating multiple products. In general, many correlates of initiation of non-cigarette products were similar to previously identified correlates that were mainly based on cigarette smoking, but this study allows for examination and comparison of these correlates across the other five products. This implies that prevention messages targeted to those aspects should have wide impact across all products.
We found many young adults already tried tobacco products at W1, leading to a reduced size of young adults at risk for new tobacco product use. Young adults who reach young adulthood without ever having tried a certain tobacco product may be fundamentally different from those youth who experiment for the first time before age 18; those most susceptible to tobacco may initiate at a younger age, which may modify the underlying risk profile of the young adults eligible for the analysis. Furthermore, a smaller number of observations in the young adult sample may have affected our ability to detect differences in the young adult sample, especially in adjusted models. However, it is important to note that young adults ages 18–20 years were more likely to initiate tobacco use than young adults ages 21–24 years. The 18–20-year-old age group is important to continue to monitor given the national law passed in 2019 that raised the minimum age for sale of tobacco products from 18 to 21 years. The timeframe of our study was before the passage of this law, but future studies can continue to monitor initiation rates in these youngest adults (18–20 years) who now are underage consumers.
A strength of our study is that we were able to stratify the sample by tobacco-naïve never users at baseline, allowing us to isolate youth and young adults who reported no use of each product, and those who were completely tobacco-naïve at W1. We found higher initiation in those who previously used another tobacco product than the tobacco-naïve. However, some limitations should be considered when interpreting these findings. Given the rise in the popularity of JUUL-like devices,29 estimates of new use could be higher in the PATH Study after January 2018. In order to facilitate comparison across models for each of the tobacco products, parsimonious models were not developed with covariates known to be correlated with each product, and some of the models may be over specified.30 In addition, since correlates were measured at W1, our analysis does not take into account for the any time-varying component of these risk factors over the course of the study period. Finally, we did not adjust the significance threshold for multiple comparisons primarily because the adjustment may be conservative for the number of comparisons made, and we did not want to overlook possibly interesting findings because of the multiplicity adjustment that reduces the Type I error and thus increases the probability of Type II error.31,32
As few studies have examined initiation and correlates of use across multiple products using the same measures, these findings may help researchers and public health analysts focus on the most frequently used new products and common risk factors. Information on youth correlates of non-cigarette products expands upon previously known factors associated with new cigarette smoking. Future research can examine other long-term trajectories of use over multiple waves, including switching between tobacco products or adding products, longitudinal changes in frequency of product use, and product-specific correlates. Expanded data on behavioral use transitions can be used to update inputs to population health models. Furthermore, estimates of initiation by product and correlates of initiation could be used to monitor and tailor product-specific prevention messages and intervention campaigns for the identified demographic groups at higher risk.
Supplementary Material
HIGHLIGHTS.
By follow-up, nearly 6 million youth used tobacco for the first time
By follow-up, nearly 2.5 million young adults used tobacco for the first time
Electronic nicotine devices had the highest proportion of new users
Cigarette and non-cigarette products share many correlates of initiation
Some noteworthy demographic differences exist in tobacco product initiation
Appendix A: Creation of Variables
Construction of Initiation Variables
Use of any tobacco product and use of each of seven product classes (cigarette, ENDS, any cigar [traditional cigar, cigarillos, filtered cigars], any smokeless tobacco [snus pouches or non-snus pouch smokeless tobacco], pipe tobacco, hookah, dissolvable tobacco) were assessed at baseline. At follow-up, initiation (new use in the past 12 months) of each tobacco product was assessed among those who had never used the tobacco product at baseline as well as among tobacco-naïve individuals. Any individual who had not used a product before baseline but reported new use after or during follow-up was considered to have initiated that product.
Those who had never heard of or never used each tobacco product at W1 were considered never users of that product. At each wave of W2–W4, any tobacco use, use of the seven product classes, and polytobacco product use were calculated for the past 12 months. At each wave, any tobacco use was defined as use of any of the seven tobacco product classes. Any cigar use was constructed such that if a respondent had ever used any of the three types of cigars (traditional cigars, cigarillos, and filtered cigars), they were counted as an any cigar user. Any smokeless tobacco use was constructed in a similar manner: if respondents had ever used either snus pouches or other smokeless tobacco, not including dissolvable tobacco (which was asked as a separate category), they were categorized as an any smokeless tobacco user. For any tobacco, any cigar or any type of smokeless tobacco, complete product response information was required to categorize participants as non-users of each product but was not required to categorize participants as any tobacco users. Individual product use (cigarette, ENDS, pipe tobacco, hookah, dissolvable tobacco) was calculated based on responses to questions about that specific product at each wave. Missing data for individual product use was based on missing responses to that particular question.
New past 12-month use of any tobacco was calculated as the proportion of never users of any tobacco product at W1 who used any tobacco product in the past 12 months at each wave of W2–W4.
New past 12-month use of each tobacco product for seven classes of tobacco products was calculated as the proportion of never users of a specific tobacco product at W1 who reported initiation of that tobacco product in the past 12 months at each wave of W2–W4.
Initiation of each tobacco product for seven classes of tobacco products was calculated as the proportion of never users of a specific tobacco product at W1 who reported initiation of that tobacco product by W4.
Correlates
Demographic correlates included age, sex, and race/ethnicity. Missing data on demographics and education were imputed as described in the PATH Study Restricted Use Files User Guide (United States Department of Health and Human Services 2019). Household exposure to tobacco use was explored by assessing cigarette smoking and tobacco use among household members, as well as any exposure to others smoking within the past seven days. Ever use of marijuana and alcohol were assessed. Internalizing factors (depression, anxiety, distress, and trouble sleeping) and externalizing factors (having a hard time paying attention, having a hard time listening to directions, lying to get what you want, bullied or threatened others, started a physical fight, felt restless, and answered before the other person finished asking the question) were also assessed. Severity of substance abuse symptoms, internalizing, and externalizing were assessed using subscales of the Global Appraisal of Individual Needs Short Screener (GAIN-SS).1 Problems experienced within the past 12 months were tallied and dichotomized by severity, with four or more problems reported in the past 12 months categorized as a high substance use, internalizing, and externalizing disorder score.
Sensation-seeking variables and academic performance were not available in the young adult cohort and were therefore not included in these analyses in order to ensure consistency across age groups.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Dennis ML, Chan YF, Funk RR. Development and validation of the GAIN Short Screener (GSS) for internalizing, externalizing and substance use disorders and crime/violence problems among adolescents and adults. Am J Addict. 2006;15 Suppl 1:80–91.
DISCLAIMER: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the U.S. Department of Health and Human Services or any of its affiliated institutions or agencies.
REFERENCES
- 1.U.S. Department of Health and Human Services. Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2012. [Google Scholar]
- 2.Wang TW, Gentzke AS, Creamer MR, et al. Tobacco product use and associated factors among middle and high school students - United States, 2019. MMWR Surveill Summ. 2019;68(12):1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Creamer MR, Wang TW, Babb S, et al. Tobacco product use and cessation indicators among adults - United States, 2018. MMWR Morb Mortal Wkly Rep. 2019;68(45):1013–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mayhew KP, Flay BR, Mott JA. Stages in the development of adolescent smoking. Drug and Alcohol Dependence. 2000;59 Suppl 1:S61–81. [DOI] [PubMed] [Google Scholar]
- 5.Stanton CA SE, Seaman EL, et al. Initiation of any tobacco and five tobacco products across 3 years among youth, young adults, and adults in the United States: Findings from the PATH Study Waves 1–3 (2013–2016). Tobacco Control 2020; 29(Suppl 3), s178–s190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Center for Behavioral Health Statistics and Quality. Results from the 2018 National Survey on Drug Use and Health: Detailed Tables. In: Substance Abuse and Mental Health Services Administration, ed. Rockville, MD: 2019. [Google Scholar]
- 7.Wellman RJ, Dugas EN, Dutczak H, et al. Predictors of the onset of cigarette smoking: A systematic review of longitudinal population-based studies in youth. Am J Prev Med. 2016;51(5):767–778. [DOI] [PubMed] [Google Scholar]
- 8.Pierce JP, Sargent JD, Portnoy DB, et al. Association between receptivity to tobacco advertising and progression to tobacco use in youth and young adults in the PATH Study. JAMA Pediatrics. 2018;172(5):444–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Green VR, Conway KP, Silveira ML, et al. Mental health problems and onset of tobacco sse among 12- to 24-Year-Olds in the PATH Study. Journal of the American Academy of Child and Adolescent Psychiatry. 2018;57(12):944–954.e944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Academies of Sciences, Engineering, and Medicine. Public Health Consequences of E-Cigarettes. Washington (DC): National Academies Press (US); 2018. [PubMed] [Google Scholar]
- 11.Kasza KA, Edwards KC, Tang Z, et al. Correlates of tobacco product initiation among youth and adults in the USA: findings from the PATH Study Waves 1–3 (2013–2016). Tobacco Control. 2020;29(Suppl 3):s191–s202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fielder RL, Carey KB, Carey MP. Predictors of initiation of hookah tobacco smoking: a one-year prospective study of first-year college women. Psychol Addict Behav. 2012;26(4):963–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chaffee BW, Couch ET, Urata J, Gansky SA, Essex G, Cheng J. Predictors of smokeless tobacco susceptibility, initiation, and progression over time among adolescents in a rural cohort. Subst Use Misuse. 2019;54(7):1154–1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sawdey MD, Day HR, Coleman B, et al. Associations of risk factors of e-cigarette and cigarette use and susceptibility to use among baseline PATH study youth participants (2013–2014). Addictive Behaviors. 2019;91:51–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wills TA, Knight R, Williams RJ, Pagano I, Sargent JD. Risk factors for exclusive e-cigarette use and dual e-cigarette use and tobacco use in adolescents. Pediatrics. 2015;135(1):e43–e51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barrington-Trimis JL, Berhane K, Unger JB, et al. Psychosocial factors associated with adolescent electronic cigarette and cigarette use. Pediatrics. 2015;136(2):308–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silveira ML, Conway KP, Green VR, et al. Longitudinal associations between youth tobacco and substance use in waves 1 and 2 of the Population Assessment of Tobacco and Health (PATH) Study. Drug and Alcohol Dependence. 2018;191:25–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rose SW, Glasser AM, Zhou Y, et al. Adolescent tobacco coupon receipt, vulnerability characteristics and subsequent tobacco use: analysis of PATH Study, Waves 1 and 2. Tobacco Control. 2018;27(e1):e50–e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kasza KA, Borek N, Conway KP, et al. Transitions in tobacco product use by U.S. Adults between 2013(−)2014 and 2014(−)2015: Findings from the PATH Study Wave 1 and Wave 2. International Journal of Environmental Research and Public Health. 2018;15(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheng YC, Rostron BL, Day HR, et al. Patterns of use of smokeless tobacco in US adults, 2013–2014. American Journal of Public Health. 2017;107(9):1508–1514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tobacco Control. 2016; 26(4), 371–378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rubin DB. Multiple imputation for nonresponse in surveys. Vol 81: John Wiley & Sons; 2004. [Google Scholar]
- 23.Barnard J, Rubin DB. Miscellanea. Small-sample degrees of freedom with multiple imputation. Biometrika. 1999;86(4):948–955. [Google Scholar]
- 24.Johnston LD, Miech, R. A., O’Malley, P. M.,, Bachman JG, Schulenberg, J. E., & Patrick, M. E. Monitoring the Future national survey results on drug use 1975–2019: Overview, key findings on adolescent drug use. In. Ann Arbor: Institute for Social Research, University of Michigan; (2020). [Google Scholar]
- 25.Riehm KE, Young AS, Feder KA, et al. Mental health problems and initiation of e-cigarette and combustible cigarette use. Pediatrics. 2019;144(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kintz N, Liu M, Chou CP, et al. Risk factors associated with subsequent initiation of cigarettes and e-cigarettes in adolescence: A structural equation modeling approach. Drug and Alcohol Dependence. 2020;207:107676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Villanti AC, Cobb CO, Cohn AM, Williams VF, Rath JM. Correlates of hookah use and predictors of hookah trial in U.S. young adults. Am J Prev Med. 2015;48(6):742–746. [DOI] [PubMed] [Google Scholar]
- 28.Chaffee BW, Cheng J. Tobacco product initiation is correlated with cross-product changes in tobacco harm perception and susceptibility: Longitudinal analysis of the Population Assessment of Tobacco and Health youth cohort. Prev Med. 2018;114:72–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Huang J, Duan Z, Kwok J, et al. Vaping versus JUULing: how the extraordinary growth and marketing of JUUL transformed the US retail e-cigarette market. Tobacco Control. 2019;28(2):146–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–1379. [DOI] [PubMed] [Google Scholar]
- 31.Perneger TV. What’s wrong with Bonferroni adjustments. Bmj. 1998;316(7139):1236–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990:43–46. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


