Abstract
There is tremendous interest in understanding how neighborhoods impact health by linking extant social and environmental drivers of health (SDOH) data with electronic health record (EHR) data. Studies quantifying such associations often use static neighborhood measures. Little research examines the impact of gentrification—a measure of neighborhood change—on the health of long-term neighborhood residents using EHR data, which may have a more generalizable population than traditional approaches. We quantified associations between gentrification and health and healthcare utilization by linking longitudinal socioeconomic data from the American Community Survey with EHR data across two health systems accessed by long-term residents of Durham County, NC, from 2007 to 2017. Census block group-level neighborhoods were eligible to be gentrified if they had low socioeconomic status relative to the county average. Gentrification was defined using socioeconomic data from 2006 to 2010 and 2011–2015, with the Steinmetz-Wood definition. Multivariable logistic and Poisson regression models estimated associations between gentrification and development of health indicators (cardiovascular disease, hypertension, diabetes, obesity, asthma, depression) or healthcare encounters (emergency department [ED], inpatient, or outpatient). Sensitivity analyses examined two alternative gentrification measures. Of the 99 block groups within the city of Durham, 28 were eligible (N = 10,807; median age = 42; 83% Black; 55% female) and 5 gentrified. Individuals in gentrifying neighborhoods had lower odds of obesity (odds ratio [OR] = 0.89; 95% confidence interval [CI]: 0.81–0.99), higher odds of an ED encounter (OR = 1.10; 95% CI: 1.01–1.20), and lower risk for outpatient encounters (incidence rate ratio = 0.93; 95% CI: 0.87–1.00) compared with non-gentrifying neighborhoods. The association between gentrification and health and healthcare utilization was sensitive to gentrification definition.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11524-022-00692-w.
Keywords: Gentrification, Social determinants of health, Neighborhoods, Electronic health record (EHR) data
Background
The social and environmental drivers of health (SDOH)—the conditions where people live, work, and play—within a person’s neighborhood profoundly impact health [1–3]. Identifying this information in the electronic health record (EHR) can be challenging as neighborhood-level SDOH data are not recorded as frequently as health data. Linking neighborhood-level SDOH data with EHR data can provide an alternative way to understand the impact of SDOH on health. However, studies that link SDOH and EHR data often use time-invariant, static neighborhood measures.
Gentrification, a neighborhood change process, is a neighborhood level exposure that may act as a SDOH that is often related to the influx of younger, healthier, and wealthier individuals into a neighborhood [4]. This in-migration can lead to the displacement of residents who are less financially resourced yet healthy enough to move, leaving behind fewer healthy long-term residents, who may simultaneously experience an erosion of health-promoting factors such as social cohesion [5]. Alternatively, gentrification and shifts in the population may lead to potentially health-promoting new businesses or amenities [6]. Prior work has shown that gentrification may impact self-reported health, health behaviors, mental health, and healthcare utilization [5, 7–12]. There has been relatively little research, however, on the impact of gentrification on the health of long-term neighborhood residents [10]. Further, prior studies have not leveraged large-scale EHR data with a potentially more generalizable population than traditional cohort studies while also considering multiple definitions of gentrification.
To understand the impact that these dynamic processes may have on the health of communities, population level EHR data—drawn from multiple sources, including health systems and federally qualified health centers—are needed that can capture the presence of important indicators of health and healthcare utilization across a diverse and representative population. With the ubiquity of EHR, new opportunities are emerging to investigate how health and healthcare utilization change as gentrification occurs among individuals living in geographic regions served by healthcare organizations. Neighborhood-level analyses exploring the health of individuals served by healthcare organizations could provide insight into how healthcare utilization and health outcomes might differ by neighborhoods that did and did not experience gentrification.
Using EHR data to describe the health of residents within neighborhoods, we examined the association between gentrification and chronic health conditions. We hypothesized that long-term residents living in gentrifying neighborhoods would have increased risk for health outcomes as compared to long-term residents of neighborhoods that were eligible (i.e., low socioeconomic status), but did not gentrify.
Methods
Overview
We conducted a retrospective cohort study of adult residents of Durham County, NC, living in neighborhoods that did and did not experience gentrification to quantify the association between gentrification and risk for health outcomes and healthcare utilization.
Data Sources
Electronic Health Records
Data on health outcomes and healthcare utilization were obtained from the EHR of the Duke University Health System (DUHS) and Lincoln Community Health Center (LCHC) from 2007 to 2017. DUHS is the predominant healthcare provider for insured Durham County residents as 85% of Durham County residents have a primary or specialty encounter in the DUHS [13]. It includes an academic medical center and two community hospitals linked with a network of outpatient clinics. LCHC is a federally qualified health center in Durham, NC, that serves the uninsured, underinsured, and undocumented residents of the city. As of 2016, 63% of the LCHC population self-identified as Black/African American race, 47% identified as having Hispanic/Latinx ethnicity, and nearly 89% were at or below the 200% level of the federal poverty line. The EHR systems of DUHS and LCHC are linked through a common EHR vendor and are organized in a shared datamart modeled to the PCORnet Common Data Model. Approximately 80% of Durham residents receive their care at DUHS and/or LCHC [14].
Study Population
The source population for this study included adult residents from Durham County, NC, age 19 years or older who had EHR evidence of at least one encounter within the DUHS or LCHC during the baseline (2008–2010) and follow-up time periods (2014–2016). We excluded women who were pregnant at either baseline or follow-up (i.e., 2008–2010 and 2014–2016, respectively) as they are at increased risk for the outcomes of interest as compared to non-pregnant women [15–18]. We restricted our analysis to individuals who were long-term residents of the city of Durham, defined as residents with EHR evidence of having lived at the same address in the same block group during both the baseline and the follow-up study periods.
Gentrification
American Community Survey
The socioeconomic variables used to define the explanatory variable of interest, gentrification, were obtained from the American Community Survey (ACS). The ACS is a national survey that collects information on 3.5 million households related to demographic, social, economic, and housing-related characteristics of a sample of residents within the USA. For this study, 5-year estimates of the ACS from 2006 to 2010 were used to define baseline eligibility to gentrify, and estimates from 2011 to 2015 were used to define gentrification at follow-up.
Defining Gentrification
The primary unit of analysis was the census block group (i.e., neighborhood). A census block group is a geographical unit used by the Census Bureau and is composed of 600–3,000 people. We compared neighborhoods that experienced gentrification between 2006–2010 and 2011–2015 with census block groups that did not experience gentrification. We limited our main analysis to the 99 (of 153 total) block groups within Durham County that were completely within Durham City limits, as there are notable differences in socioeconomic indicators and health in block groups in more urban areas within the city and less urban areas outside of city limits. We considered block groups eligible to be gentrified if they had low socioeconomic status (broadly defined as below the county-level mean in income, rent, and education and above county-level mean in poverty), with differing criteria based on the definition of gentrification used. Ineligible block groups were excluded from analyses [19]. After this exclusion, 28 block groups (N = 10,807) were eligible to be gentrified and included in the analyses.
In our primary analyses, we defined gentrification using mean household income values from 2006–2010 and 2011–2015, mean gross rent price, percent of the population with a bachelor’s degree, and the percent living below the poverty level, as described by Steinmetz-Wood [19]. We considered eligible block groups to have gentrified if they saw an increase in at last three of the four variables (household income, gross rent price, or proportion with a bachelor’s degree; or a reduction in the proportion living below the poverty level) between the baseline (2006–2010) and follow up (2011–2015) time periods.
Health Indicators and Healthcare Utilization Outcomes
The presence or absence of health conditions was ascertained using the EHR during the baseline and follow-up periods and included type 2 diabetes, hypertension, obesity, CVD, depression, and asthma. Diabetes was defined using a published phenotype (i.e., Durham Diabetes Coalition) which included ICD-9 and ICD-10 codes recorded in the inpatient (DUHS), outpatient (DUHS, LCHC), or emergency department (DUHS) (Supplement 1), use of medications to treat diabetes, or hemoglobin A1c ≥ 6.5% [20]. Hypertension was defined according to ICD-9 or ICD-10 diagnosis codes, the average of two consecutive systolic blood pressure measures in 365 days ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg, or use of anti-hypertensive medication. Only blood pressure measurements obtained through outpatient encounters were used as prior work suggests that blood pressure measured in the emergency department (ED) may be systematically biased [21]. Obesity was defined as a body mass index ≥ 30 kg/m2. CVD was defined as a diagnosis of myocardial infarction, stroke, or congestive heart failure (CHF). Depression and asthma were identified through ICD-9 and ICD-10 diagnosis codes. CVD, depression, and asthma diagnoses were ascertained through inpatient, outpatient, or emergency department diagnoses. Three healthcare utilization outcomes examined during baseline and follow-up periods included the number of ED visits, inpatient admissions, and outpatient encounters.
Statistical Analyses
We conducted descriptive analyses to compare baseline characteristics of the study population stratified by the gentrification status of the neighborhood within which they lived. We used longitudinal models to quantify the association between gentrification and indicators of change in health (i.e., incident CVD, hypertension, diabetes, obesity, asthma, and depression) and healthcare utilization (number of ED and inpatient visits) from the baseline to follow-up time periods. We estimated the difference in the change of health indicators and inpatient and emergency department encounters between gentrified and non-gentrified block groups using generalized estimating equations (GEE) with a logit link function. Another outcome was outpatient visits, which was a count variable and thus estimated by a Poisson model using GEE with a log link and an offset for length of follow-up. GEE was used due to the longitudinal nature of the study, where each individual had one observation at baseline and another observation at follow-up. The within-subject correlation was then accounted for by assuming a compound symmetry covariance structure in GEE. With this study design, one can directly estimate the change in risk of having the outcome from baseline to follow-up for individuals within a block group that did or did not gentrify and the difference in the changes comparing gentrified and non-gentrified block groups. The basic parametrization is provided in Supplement 2. Our model controlled for age, race, the Index of Concentration at the Extremes (ICE) for race [22] (a measure of neighborhood level racial segregation), sex, insurance status, and individual-level clustering effect.
Sensitivity Analyses for Different Methods of Defining Gentrification
We conducted sensitivity analyses using two other measures of gentrification (Supplement 3). Ding and colleagues defined gentrification using median home value, median gross rent price, percent with bachelor’s degree, and median household income [23]. Hirsch and colleagues defined gentrification [24] using percent with bachelor’s degree, median contract rent price, and median home value. Hirsch defines gentrification at two levels: gentrification and intense gentrification. Neighborhoods were considered to have experienced gentrification if the increase in proportion of residents with college education was above the median and the increase in gross rent was in the 50–75th percentile or the increase in home value was in the 50–75th percentile. Neighborhoods were considered to have undergone intense gentrification if the increase in proportion of residents with college education was above the median increase and the increase in gross rent was in the 75th percentile or higher or the increase in home value was in the 75th percentile or higher. We conducted additional sensitivity analyses to examine the associations of interest by age/race/sex subgroups. Analyses were conducted in R (R Foundation for Statistical Computing; Vienna, Austria). This study was approved by the Duke University School of Medicine institutional review board.
Results
Baseline Characteristics of Participants
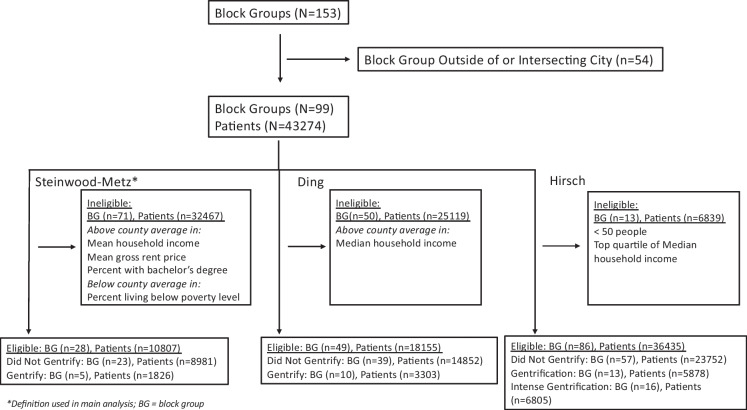
The source population included 43,274 individuals living in 99 block groups within the city of Durham (Fig. 1). After excluding individuals living in neighborhoods not eligible to experience gentrification, 10,807 individuals living in 28 block groups were included in the main analysis. The study population was majority Black residents (83%) and relatively young with a median age of 42 years (interquartile range [IQR]: 28–54); 10% of the population was over the age of 65 years. Overall, 48% received health insurance through a public provider. The block group-level mean household income was $24,887 (SD: $9702), mean monthly rent was $674 (SD: $141), 14% had at least a bachelor’s degree (SD: 10%), and 41% lived below the poverty level (SD: 15%).
Fig. 1.
Study population and gentrification measure for main and sensitivity analyses
Characteristics of Neighborhoods by Gentrification Status
Among the 28 eligible block groups, 5 block groups (n = 1826) experienced gentrification, and 23 (n = 8981) did not experience gentrification. At baseline, neighborhoods that experienced gentrification had a slightly lower proportion of long-term residents who were women (53% vs. 55%; p = 0.04) and White (6% vs. 10%; p < 0.001) than non-gentrified neighborhoods. Gentrified neighborhoods had lower mean rent ($581 vs. $695; p = 0.03) and appeared to have lower median household income ($19,562 vs. $26,045), higher proportion of individuals living below the poverty level (48% vs. 40%), while having a higher proportion of individuals with bachelor’s degree (16% vs. 14%) as compared to neighborhoods that did not gentrify (Table 1). However, these differences were not statistically significant (p > 0.05).
Table 1.
Baseline characteristics of the study population
| Eligible | Not eligible | Eligible + ineligible | |||
|---|---|---|---|---|---|
| Did not gentrify | Gentrified | Total | Total | Total | |
| (N = 8981) | (N = 1826) | (N = 10807) | (N = 32467) | (N = 43274) | |
| Block groups | 23 | 5 | 28 | 71 | 99 |
| Demographics | |||||
| Female (%) | 4964 (55.3%) | 960 (52.6%) * | 5924 (54.8%) | 18,561 (57.2%) | 24485 (56.6%) |
| Age (yrs) (Median, 25th-75th) | 41.4 (27.5–53.8) | 42.8, (29.1–54.1) | 41.7, (27.8–53.9) | 45.4 (32.0–57.8) | 44.5 (30.8–56.9) |
| Percent ≥ 65 years | 940 (10.5%) | 173 (9.5%) | 1113 (10.3%) | 4611 (14.2%) | 5724 (13.2%) |
| Race | |||||
| Black | 7302 (81.3%) | 1620 (88.7%) | 8922 (82.6%) | 13,710 (42.2%) | 22632 (52.3%) |
| White | 897 (10.0%) | 113 (6.2%)* | 1010 (9.3%) | 16,135 (49.7%) | 17145 (39.6%) |
| Others | 782 (8.7%) | 93 (5.1%) | 875 (8.1%) | 2622 (8.1%) | 3497 (8.1%) |
|
Ethnicity Hispanic Non-Hispanic Others Payor | |||||
| Private | 2545 (34.8%) | 499 (33.5%) | 3044 (34.5%) | 17294 (63.6%) | 20338 (47.0%) |
| Public | 3528 (48.3%) | 711 (47.7%) | 4239 (48.2%) | 8009 (29.4%) | 12248 (28.3%) |
| Self-pay | 1230 (16.8%) | 280 (18.8%) | 1510 (17.2%) | 1902 (7.0%) | 3412 (7.9%) |
| Variables defining gentrification | |||||
| Median household income (mean (SD)) | 26045 (9572) | 19562 (9396) | 24887 (9702) | 58114 (28,540) | 48716 (28878) |
| Percent bachelor’s degree (mean (SD)) | 13.9 (10.5) | 16.1 (6.8) | 14.3 (9.8) | 46.9 (21.9) | 37.6 (24.2) |
| Average rent (mean (SD)) | 695 (136) | 581 (135)* | 674 (141) | 937 (272) | 859 (268) |
| Percent below poverty (mean (SD)) | 39.5 (15.2) | 48.4 (13.6) | 41.1 (15) | 14 (16) | 21 (20) |
*p < 0.05 comparing neighborhoods that did and did not gentrify
SD, standard deviation
From baseline to follow-up, mean household income increased by $11,091 in neighborhoods that gentrified but decreased by $498 in those that did not gentrify (p = 0.02). The mean rent price increased by $159 in gentrified neighborhoods, but it decreased by $14 in non-gentrifying neighborhoods (p < 0.01). The proportion of the population living below the poverty level decreased by 21% in gentrified neighborhoods and decreased by 2% in non-gentrified neighborhoods (p value for difference-in-difference = 0.02). There was no appreciable difference in the change in proportion of individuals with bachelor’s degrees between neighborhoods that did and did not gentrify (p = 0.35) (Table 2).
Table 2.
Change from baseline to follow-up of variables used to define gentrification
| Eligible | Not eligible | Eligible + ineligible | |||
|---|---|---|---|---|---|
| Did not gentrify | Gentrified | Total | Total | Total | |
| (N = 8981) | (N = 1826) | (N = 10807) | (N = 32467) | (N = 43274) | |
| Block groups | 23 | 5 | 28 | 71 | 99 |
| Household income (mean (SD)) | − 498 (9629) | 11091 (4549)* | 1731 (9959) | − 3972 (16209) | − 2428 (14947) |
| Percent bachelor’s degree (mean (SD)) | 0.03 (0.11) | 0.08 (0.06)* | 0.04 (0.10) | 0.04 (0.18) | 0.04 (0.16) |
| Difference in rent (mean (SD)) | − 14 (110) | 159 (78)* | 17 (124) | 14 (230) | 15 (203) |
| Percent below poverty (mean (SD)) | − 2 (17) | − 21 (10) | − 5 (17) | 2 (10) | 0 (13) |
*p < 0.05 comparing neighborhoods that did and did not gentrify
SD, standard deviation
Health Outcomes
The overall baseline age-adjusted prevalence of diabetes was 20%; 44% had hypertension; 26% were obese; and 5% had cardiovascular disease (CVD) (Table 3) at baseline and increased significantly between 2006–2010 and 2011–2015 (diabetes to 32%, hypertension to 61%, obesity to 56%, and CVD to 11%). The age-adjusted prevalence of these conditions at baseline was similar among neighborhoods that did and did not experience gentrification. At follow-up, the prevalence of all health conditions, with the exception of hypertension and obesity, was similar between individuals living in neighborhoods that did and did not experience gentrification. Individuals living in neighborhoods that gentrified, as compared to individuals living in neighborhoods that did not gentrify, had a lower odds of obesity (OR = 0.89; 95% CI: 0.81–0.99) (Table 4). Adjusted analyses showed similar changes in CVD, diabetes, hypertension, depression, and asthma between neighborhoods that did and did not gentrify.
Table 3.
Age-standardized prevalence of health outcomes and healthcare utilization
| Baseline | Follow-up | p value (baseline vs. follow-up) | |||||
|---|---|---|---|---|---|---|---|
| Did not gentrify | Gentrified | Total | Did not gentrify | Gentrified | Total | ||
| N | 8981 | 1826 | 10807 | 8981 | 1826 | 10807 | |
| Health outcomes | |||||||
| Diabetes | 20 | 20.7 | 20.1 | 31.4 | 32.1 | 31.5 | < 0.01 |
| Hypertension | 43.9 | 45.5 | 44.2 | 60.2 | 63* | 60.7 | < 0.01 |
| Obesity | 26.2 | 26.5 | 26.3 | 56.7 | 53.3* | 56.1 | < 0.01 |
| Cardiovascular disease | 4.6 | 4.3 | 4.5 | 11.1 | 11.1 | 11.1 | < 0.01 |
| Depression | 12.3 | 11.9 | 12.3 | 25.5 | 26.2 | 25.6 | < 0.01 |
| Asthma | 9.4 | 9.9 | 9.5 | 17.1 | 18.3 | 17.4 | < 0.01 |
| Healthcare utilization | |||||||
| Outpatient encounters per year (mean (SD)) | 2.8 (5.5) | 2.7 (5.6) | 2.8 (5.51) | 3.9 (5.9) | 3.7 (5.3)* | 3.87(5.8) | < 0.01 |
| ED Encounters per year (mean (SD)) | 0.7 (1.7) | 0.8 (2.1)* | 0.7 (1.7) | 0.97 (2.0) | 1.04 (1.8)* | 0.98 (2.0) | < 0.01 |
| Inpatient encounters per year (mean (SD)) | 0.1 (0.4) | 0.1 (0.4) | 0.1 (0.4) | 0.2 (0.6) | 0.2 (0.6)* | 0.2 (0.6) | < 0.01 |
*p < 0.05 comparing neighborhoods that did not gentrify vs. those that did gentrify
SD, standard deviation
Table 4.
Association* between gentrification and indicators of change in health and healthcare utilization
| Estimate | 95% CI | p value | ||
|---|---|---|---|---|
| CVD | ||||
| Intercept | 0 | 0 | 0 | < 0.001 |
| Time | 1.98 | 1.83 | 2.14 | < 0.001 |
| Gentrification | 0.93 | 0.78 | 1.12 | 0.44 |
| Diabetes | ||||
| Intercept | 0.02 | 0.01 | 0.02 | < 0.001 |
| Time | 1.55 | 1.49 | 1.61 | < 0.001 |
| Gentrification | 1.00 | 0.89 | 1.13 | > 0.99 |
| Hypertension | ||||
| Intercept | 0.02 | 0.01 | 0.02 | < 0.001 |
| Time | 1.60 | 1.52 | 1.69 | < 0.001 |
| Gentrification | 0.96 | 0.86 | 1.06 | 0.42 |
| Obesity | ||||
| Intercept | 0.07 | 0.06 | 0.08 | < 0.001 |
| Time | 3.24 | 3.09 | 3.39 | < 0.001 |
| Gentrification | 0.89 | 0.81 | 0.99 | 0.026 |
| Depression | ||||
| Intercept | 0.04 | 0.03 | 0.04 | < 0.001 |
| Time | 2.40 | 2.28 | 2.52 | < 0.001 |
| Gentrification | 1.05 | 0.93 | 1.18 | 0.42 |
| Asthma | ||||
| Intercept | 0.05 | 0.04 | 0.06 | < 0.001 |
| Time | 1.97 | 1.87 | 2.08 | < 0.001 |
| Gentrification | 1.03 | 0.9 | 1.19 | 0.65 |
| Emergency department | ||||
| Intercept | 0.84 | 0.76 | 0.93 | < 0.001 |
| Time | 2.19 | 2.08 | 2.30 | < 0.001 |
| Gentrification | 1.10 | 1.01 | 1.20 | 0.024 |
| Inpatient | ||||
| Intercept | 0.02 | 0.02 | 0.02 | < 0.001 |
| Time | 1.23 | 1.13 | 1.33 | < 0.001 |
| Gentrification | 1.09 | 0.97 | 1.23 | 0.16 |
| Outpatient | ||||
| Intercept | 0.26 | 0.24 | 0.30 | < 0.001 |
| Time | 1.15 | 1.11 | 1.20 | < 0.001 |
| Gentrification | 0.93 | 0.87 | 1.00 | 0.05 |
Models adjusted for age, race, ICE, sex, insurance status, and the individual-level clustering effect
Healthcare Utilization
At baseline, individuals had on average 2.8 outpatient encounters, 0.7 ED visits, and 0.1 inpatient admissions per year (Table 3) and increased significantly between 2006–2010 and 2011–2015 (outpatient encounters per year: 3.9; ED visits per year: 0.98; inpatient encounters per year: 0.2). Individuals living in neighborhoods that gentrified, as compared to individuals living in neighborhoods that did not gentrify, had a higher odds of an emergency room encounter (OR = 1.10; 95% CI: 1.01–1.20) and lower risk of outpatient encounters (IRR: 0.93; 95% CI: 0.87–1.00) (Table 4). Adjusted analyses no difference in inpatient encounters between people living neighborhoods that did and did not gentrify (OR = 1.09; 95% CI: 0.97–1.23).
Sensitivity Analysis
In sensitivity analyses, we compared baseline and health outcome characteristics of people who did and did not move. A relatively small portion (n = 453) of the source population (N = 11,260) moved. Individuals who moved, as compared to those that did not move, were slightly more likely to be female, older, white, and have public health insurance (Supplemental Table 1a). Among movers, 59% lived in neighborhoods that ended up gentrifying. Movers who lived in neighborhoods that gentrified, as compared to movers that lived in neighborhoods that did not gentrify, were more likely to be female, older, white, and have private insurance (Supplemental Table 1b). At baseline, movers overall and those that lived in neighborhoods that gentrified had a slightly higher prevalence of diabetes and CVD, lower prevalence of obesity and hypertension, and lower rates of outpatient and ED encounters (Supplemental Tables 2a and 2b). Residents living in block groups that will gentrify had lower odds of moving as compared to residents living in block groups that will not gentrify (OR: 0.60, 95% CI: 0.44, 0.81; results not shown).
We explored the sensitivity of our findings to two additional measures of gentrification (Supplement 3). In analyses employing both the Ding and Hirsch measures, a greater number of neighborhoods were eligible to be gentrified (40, 87, respectively) and more neighborhoods did gentrify (7, 29, respectively) than in the main analysis (28 eligible, 5 gentrified) (Supplement 4). When using the Ding and Hirsch measures, as compared to the Steinmetz-Wood definition, neighborhoods experienced gentrification included a greater proportion of White residents, greater proportion of residents on private insurance, and improved values on metrics that defined gentrification.
Similar to our primary analysis, in models that used the Ding definition of gentrification, gentrification was associated with greater odds of asthma and ED encounters (Supplement 5a). All other associations remained null. In models that defined gentrification at two levels (i.e., Hirsch measure), similar to the main analysis, individuals living in less intensely gentrified neighborhoods, as compared to individuals living in neighborhoods that did not gentrify, had lower odds of obesity and higher odds of an ED encounter (Supplement 5b). All other associations between less intense gentrification and health outcomes and healthcare utilization were null. In comparison, individuals living in intensely gentrified, as compared to individuals living in neighborhoods that did not experience gentrification, had a lower odds of diabetes, hypertension, and obesity and higher odds of ED encounters (Supplement 5b). The results also suggest that long-term residents of neighborhoods that intensely gentrified may have higher odds of depression than long term residents of neighborhoods that did not gentrify (OR = 1.06; 95% CI: 1.00–1.14). In additional exploratory analyses, gentrification status was not associated with health outcomes or healthcare utilization when stratified by age, race, or sex (Supplement 6a–c).
Discussion
We present a novel use of EHR data to explore the impact of gentrification on patient health outcomes. Our findings suggest minimal association between gentrification and indicators of health among long-term residents of Durham County, NC, over a 10-year time period. Long-term residents living in neighborhoods that gentrified had a slightly higher odds of an ED encounter. These results were sensitive to the definition of gentrification used (i.e., more specific [Steinmetz-Wood] vs. more sensitive definition [Ding, Hirsch]). The association between gentrification and ED encounter persisted with the Ding definition and other health outcomes were associated with gentrification when more sensitive definitions were used.
Increasingly, data on the social and environmental drivers of health are being linked to EHR data for inferential and prediction purposes [25–28]. However, neighborhoods are not static, and increasingly, it is recognized that neighborhood change may distinctly impact health. It is critical to link time-varying information on neighborhoods with EHR data. Gentrification is a dynamic process of neighborhood change signified by the influx of younger, healthier, and wealthier individuals. Gentrification has been examined extensively in other fields, such as economics and sociology, and its relation to crime, labor markets, and educational opportunities [29–31]. A growing body of literature supports the idea that gentrification is associated with health [32]. Few studies have examined the indicators of health and healthcare utilization included in our analyses. They have focused on self-reported health, health-related behaviors, and sub-clinical health indicators such as high blood pressure [7–10, 33, 34]. These studies have reported conflicting results. Some studies report gentrification is not associated with higher self-reported health or higher levels of stress, while others found a positive association between gentrification and higher self-reported health and an inverse association with hypertension [7–9, 34]. These studies examined health outcomes at a single time point; our study examined a change in health outcomes and healthcare utilization between baseline and follow-up periods.
Exploratory analyses within this study suggest there may be differences in hypertension by age, and in CVD, diabetes, hypertension, obesity, depression, ED, and inpatient encounters by race. Our findings are supported by other studies which suggest that gentrification is associated with certain negative health outcomes among African Americans and older adults [8, 9, 35]. Black residents within neighborhoods that are gentrifying, as compared to their White neighbors, may have poorer self-rated health, increased rates of preterm birth, and higher mortality [9, 36, 37]. There is considerably less research on the how gentrification impacts older adults. Limited data suggests that older residents living in gentrifying neighborhoods, as compared to older residents living in affluent neighborhoods, may have more depression and anxiety symptoms and lower overall mental health [35]. Similar to our study, this study did note that economically vulnerable older residents living in gentrifying neighborhoods had higher self-rated health than economically vulnerable residents living in low-income neighborhoods. This suggests that older vulnerable residents may benefit from resources being introduced through reinvestment in gentrifying neighborhoods. Prior research suggests that neighborhood resources may promote health and quality of life in older adults through increased mobility and social participation [38]. Studies have not extensively examined other health outcomes.
There is less data on the impact of gentrification on healthcare utilization. One study did show that the rate of mental health-related encounters was not different between long-term residents living in gentrified as compared to non-gentrified neighborhoods [10]. This was part of a larger study that reported higher rates of encounters in displaced residents as compared to long-term residents living in gentrified neighborhoods. Long-term residents of neighborhoods have been shown to be older and subsequently sicker than displaced residents who tend to be younger and healthier [10]. Within long-term residents, gentrification may negatively alter the collective efficacy of a neighborhood, resulting in decreased social cohesion and social control. This in turn can result in social polarization and segregation, which has been shown to lead to greater stress and high risk for illness and death [39–45]. Others have posited gentrification may improve health through greater access to resources (e.g., grocery stores, health clinics) not previously available. We may not have seen an association between gentrification and health outcomes because gentrification introduced resources that allowed long-term residents to better manage their health than long-term residents living in neighborhoods that did not gentrify.
The rates of health outcomes and healthcare utilization may be impacted by neighborhood selection. Some studies suggest that poor health predict living in a poorer neighborhood after displacement [46, 47]. Others suggest that the magnitude of association between pre-move health factors and neighborhood factors are small, indicating that residential self-selection is not a major source of bias [48]. In our study, it is noteworthy that because we are using EHR data, higher rates of conditions might be due to increased access to resources through gentrification. That is, if more health clinics are introduced in a neighborhood through gentrification, we might identify a greater number of people with health conditions. However, we included long term residents of these neighborhoods who were likely living in the neighborhoods before many of the amenities were available.
Gentrification has been theorized to impact health through changes to the physical environment and changes to the social environment [30]. This impacts physical and mental health through changes in healthcare utilization, health-related behaviors, and/or biological response. Prior studies have suggested that the association between gentrification and higher ED admissions might be related to disruptions to access to primary healthcare [10] among residents who were displaced by gentrification. Among residents who remain in neighborhoods that gentrify, increased ED use might be related to increases in gentrification associated crime [47] or exacerbation of health conditions which necessitate emergency department encounters [34]. For example, gentrification can lead to decrease in social cohesion which can impact a person’s ability to manage their diabetes and/or hypertension. This can result in individuals needing emergent care. Gentrification may have less of an impact on distal health outcomes such as CVD due to the impact of traditional risk factors such as age and smoking. This may explain why inpatient encounters are not impacted. The Ding and Hirsch definitions are more sensitive measures of gentrification; that is, they identified more tracts as gentrified. The point estimate of the association seen with these definitions is largely similar to the main definition, while the confidence intervals are narrower, potentially due to a greater number of block groups eligible.
Further research is needed to study the mechanism by which gentrification impacts health, the impact of gentrification on both long-term residents and displaced residents, and proportional contribution of decreased social cohesion and added resources to health risk.
An important challenge in studying gentrification is the method used to define gentrification. Currently, there is no gold standard definition of gentrification [32]. Studies that use quantitative definitions of gentrification apply two important criteria. The first is that neighborhoods must be eligible to be gentrified based on comparing neighborhood-level socioeconomic indicators with similar indicators at the city or county level [7, 8, 49]. The second is that there has to be a change in z-score value, percent, or numerical change from a baseline period to a follow-up period for variables of interest (e.g., median household income, median home value, and proportion with a bachelor’s degree). The definition we used in the main analysis is a conservative definition and has been used previously and includes variables that are used across multiple definitions [19, 23, 33, 50–52]. To test the sensitivity our definition, we calculated the associations of interest using other less conversative, though commonly used, definitions [23, 24]. We found that the association between gentrification and health outcomes and utilization is sensitive to the definition used. There is a need to either standardize methods to define gentrification or develop an objective definition of gentrification that does not rely on comparison to a broader geographic area. This can promote evidence generation of the impact of gentrification on health which, in turn, can inform policies to mitigate potential negative effects. These policies can include income ceilings to buy homes, eviction moratoriums, housing subsidies, small business loans, or protections on longstanding culturally significant entities.
There are notable strengths to this study. Studies that use data from the EHR implicitly include individuals with access to healthcare. Because of this, individuals from lower socioeconomic classes are often excluded from studies in which EHR data draw from highly insured populations. We were able to use linked and deduplicated EHR data from two distinct health systems, including one of which specifically serves the uninsured, underinsured, and undocumented residents of Durham County; greater than 80% of Durham residents have had a clinical encounter with at least one of these health systems. This may help to limit the selection bias introduced by using data from the EHR for research. We also considered multiple definitions of gentrification, allowing us to test the sensitivity of our results to the definition used. In addition, the outcomes enumerated in this study included multiple indicators of health and healthcare utilization, assessed over almost 10 years of follow-up.
There are limitations to note. This study included long-term residents of Durham, who may have a different demographic and clinical characteristic as compared to residents who moved in or out of Durham during the study period. By enumerating outcomes using two health systems located in Durham, NC, we may exclude outcomes and healthcare utilization that occur outside of the DUHS or LCHC and those outside of the time frames we considered. For some conditions, such as obesity, diabetes, and hypertension, this may not greatly impact our results as these conditions can be ascertained in future encounters. Our results may indicate that the health impacts of gentrification arise later than measured in our study. Gentrification may impact other indicators of health or healthcare utilization that were not measured in this study, such as control of diabetes or hypertension. In addition, we present results without a correction for multiple comparisons; some results may be due to chance.
Conclusion
We provide an approach to link extant SDOH data to EHR data to quantify the association between time-varying changes to neighborhoods and its impact on health and healthcare utilization. Our results did not find a consistent association across definitions of gentrification and health outcomes. Future research should incorporate additional health indicators, including other mental health conditions, stress markers, and more proximal measures, including management of health conditions such as diabetes and hypertension. Dynamic changes to neighborhoods through forces such as gentrification may be important social drivers of health and allude to modifiable mechanisms through which neighborhood changes impact health, as well as inform effective, targeted interventions. Policies should be considered to limit the potential negative impacts of gentrification on health and healthcare utilization.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
NAB was supported by a grant from the National Heart, Lung, and Blood Institute (K01HL140146), and MLM was supported by funding from VA Health Services Research and Development (RCS 10-391, CIN 14-310). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author Contribution
NAB developed the study concept. NAB, LEB, MP, MSB, and BAG developed the study design. Methodology and analytical approaches were developed by NAB, MP, MSB, BAG, ZY, SP, JH, and MLM. MP and ZY conducted the analyses. Review of the statistical analyses and results was done by NAB, LEB, MP, ZY, SP, MSB, AGH, BAG, MLM, PP, NSM, DM, CJD, and MLM. NAB wrote the manuscript. Critical review and revisions of the manuscript were undertaken by all authors.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Acevedo-Garcia D, Lochner KA, Osypuk TL, Subramanian SV. Future directions in residential segregation and health research: a multilevel approach. Am J Public Health. 2003;93(2):215–221. doi: 10.2105/ajph.93.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brody GH, Lei MK, Chen E, Miller GE. Neighborhood poverty and allostatic load in African American youth. Pediatrics. 2014;134(5):e1362–e1368. doi: 10.1542/peds.2014-1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345(2):99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 4.R A. Measuring gentrication and displacement in greater London. Urban Studies. 2000;37(1):149–165. doi: 10.1080/0042098002339. [DOI] [Google Scholar]
- 5.Versey HS. A tale of two Harlems: gentrification, social capital, and implications for aging in place. Soc Sci Med. 2018;214:1–11. doi: 10.1016/j.socscimed.2018.07.024. [DOI] [PubMed] [Google Scholar]
- 6.Cole HVS, Mehdipanah R, Gullon P, Triguero-Mas M. Breaking down and building up: gentrification, its drivers, and urban health inequality. Curr Environ Health Rep. 2021;8(2):157–166. doi: 10.1007/s40572-021-00309-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gibbons J, Barton M, Brault E. Evaluating gentrification’s relation to neighborhood and city health. PLoS ONE. 2018;13(11):e0207432. doi: 10.1371/journal.pone.0207432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gibbons J, Barton MS. The association of minority self-rated health with black versus white gentrification. J Urban Health. 2016;93(6):909–922. doi: 10.1007/s11524-016-0087-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Izenberg JM, Mujahid MS, Yen IH. Health in changing neighborhoods: a study of the relationship between gentrification and self-rated health in the state of California. Health Place. 2018;52:188–195. doi: 10.1016/j.healthplace.2018.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lim S, Chan PY, Walters S, Culp G, Huynh M, Gould LH. Impact of residential displacement on healthcare access and mental health among original residents of gentrifying neighborhoods in New York City. PLoS ONE. 2017;12(12):e0190139. doi: 10.1371/journal.pone.0190139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pennay A, Manton E, Savic M. Geographies of exclusion: street drinking, gentrification and contests over public space. Int J Drug Policy. 2014;25(6):1084–1093. doi: 10.1016/j.drugpo.2014.06.001. [DOI] [PubMed] [Google Scholar]
- 12.Whittle HJ, Palar K, Hufstedler LL, Seligman HK, Frongillo EA, Weiser SD. Food insecurity, chronic illness, and gentrification in the San Francisco Bay Area: an example of structural violence in United States public policy. Soc Sci Med. 2015;143:154–161. doi: 10.1016/j.socscimed.2015.08.027. [DOI] [PubMed] [Google Scholar]
- 13.Lang JE, Tang M, Zhao C, Hurst J, Wu A, Goldstein BA. 2020 Well-child care attendance and risk of asthma exacerbations. Pediatrics 146(6) 10.1542/peds.2020-1023 [DOI] [PMC free article] [PubMed]
- 14.Spratt SE, Batch BC, Davis LP, et al. Methods and initial findings from the Durham Diabetes Coalition: integrating geospatial health technology and community interventions to reduce death and disability. J Clin Transl Endocrinol. 2015;2(1):26–36. doi: 10.1016/j.jcte.2014.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Archambault C, Arel R, Filion KB. Gestational diabetes and risk of cardiovascular disease: a scoping review. Open Med. 2014;8(1):e1–9. [PMC free article] [PubMed] [Google Scholar]
- 16.Bellamy L, Casas JP, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373(9677):1773–1779. doi: 10.1016/S0140-6736(09)60731-5. [DOI] [PubMed] [Google Scholar]
- 17.Fraser A, Nelson SM, Macdonald-Wallis C, et al. Associations of pregnancy complications with calculated cardiovascular disease risk and cardiovascular risk factors in middle age: the Avon Longitudinal Study of Parents and Children. Circulation. 2012;125(11):1367–1380. doi: 10.1161/CIRCULATIONAHA.111.044784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pirkola J, Pouta A, Bloigu A, et al. Prepregnancy overweight and gestational diabetes as determinants of subsequent diabetes and hypertension after 20-year follow-up. J Clin Endocrinol Metab. 2010;95(2):772–778. doi: 10.1210/jc.2009-1075. [DOI] [PubMed] [Google Scholar]
- 19.Steinmetz-Wood M, Wasfi R, Parker G, Bornstein L, Caron J, Kestens Y. Is gentrification all bad? Positive association between gentrification and individual's perceived neighborhood collective efficacy in Montreal. Canada. Int J Health Geogr. 2017;16(1):24. doi: 10.1186/s12942-017-0096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spratt SE, Pereira K, Granger BB, et al. Assessing electronic health record phenotypes against gold-standard diagnostic criteria for diabetes mellitus. J Am Med Inform Assoc. 2017;24(e1):e121–e128. doi: 10.1093/jamia/ocw123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Phelan M, Bhavsar NA, Goldstein BA. Illustrating informed presence bias in electronic health records data: how patient interactions with a health system can impact inference. EGEMS (Wash DC) 2017;5(1):22. doi: 10.5334/egems.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Krieger N, Feldman JM, Waterman PD, Chen JT, Coull BA, Hemenway D. Local residential segregation matters: stronger association of census tract compared to conventional city-level measures with fatal and non-fatal assaults (total and firearm related), using the index of concentration at the extremes (ICE) for racial, economic, and racialized economic segregation, Massachusetts (US), 1995–2010. J Urban Health. 2017;94(2):244–258. doi: 10.1007/s11524-016-0116-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ding L, Hwang J, Divringi E. Gentrification and residential mobility in Philadelphia. Reg Sci Urban Econ. 2016;61:38–51. doi: 10.1016/j.regsciurbeco.2016.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hirsch JA SL. A measure of gentrification for use in longitudinal public health studies based in the United States. Philadelphia, PA: Drexel University; 2019. https://drexel.edu/~/media/Files/uhc/briefs/Gentrification_Brief.ashx?la=en
- 25.Bhavsar NA, Gao A, Phelan M, Pagidipati NJ, Goldstein BA. Value of neighborhood socioeconomic status in predicting risk of outcomes in studies that use electronic health record data. JAMA Netw Open. 2018;1(5):e182716. doi: 10.1001/jamanetworkopen.2018.2716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghazi L, Oakes JM, MacLehose RF, Luepker RV, Osypuk TL, Drawz PE. Neighborhood Socioeconomic Status and Identification of patients With CKD using electronic health records. Am J Kidney Dis. 2021;78(1):57–65. doi: 10.1053/j.ajkd.2020.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nouri S, Lyles CR, Rubinsky AD, et al. Evaluation of neighborhood socioeconomic characteristics and advance care planning among older adults. JAMA Netw Open. 2020;3(12):e2029063. doi: 10.1001/jamanetworkopen.2020.29063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meeker JR, Burris HH, Bai R, Levine LD, Boland MR. Neighborhood deprivation increases the risk of Post-induction cesarean delivery. J Am Med Inform Assoc. 2022;29(2):329–334. doi: 10.1093/jamia/ocab258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Newman K, Wyly EK. The right to stay put, revisited: gentrification and resistance to displacement in New York City. Urban Studies. 2006;43(1):23–57. doi: 10.1080/00420980500388710. [DOI] [Google Scholar]
- 30.Shaw K, Hagemans I. @ Gentrification without displacement’ and the consequent loss of place: the effects of class transition on low-income residents of secure housing in gentrifying areas. Int J Urban Reg Res. 2015;39:323–341. doi: 10.1111/1468-2427.12164. [DOI] [Google Scholar]
- 31.Wyly EK, Hammel DJ. Gentrification, segregation, and discrimination in the American urban system. Environment and Planning A: economy and Space. 2004;36(7):1215–1241. doi: 10.1068/a3610. [DOI] [Google Scholar]
- 32.Bhavsar NA, Kumar M, Richman L. Defining gentrification for epidemiologic research: a systematic review. PLoS ONE. 2020;15(5):e0233361. doi: 10.1371/journal.pone.0233361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Izenberg JM, Mujahid MS, Yen IH. Gentrification and binge drinking in California neighborhoods: it matters how long you've lived there. Drug Alcohol Depend. 2018;188:1–9. doi: 10.1016/j.drugalcdep.2018.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Morenoff JD, House JS, Hansen BB, Williams DR, Kaplan GA, Hunte HE. Understanding social disparities in hypertension prevalence, awareness, treatment, and control: the role of neighborhood context. Soc Sci Med. 2007;65(9):1853–1866. doi: 10.1016/j.socscimed.2007.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smith RJ, Lehning AJ, Kim K. Aging in place in gentrifying neighborhoods: implications for physical and mental health. Gerontologist. 2018;58(1):26–35. doi: 10.1093/geront/gnx105. [DOI] [PubMed] [Google Scholar]
- 36.Smith GS, Breakstone H, Dean LT, Thorpe RJ., Jr Impacts of gentrification on health in the US: a systematic review of the literature. J Urban Health. 2020;97(6):845–856. doi: 10.1007/s11524-020-00448-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Huynh M, Maroko AR. Gentrification and preterm birth in New York City, 2008–2010. J Urban Health. 2014;91(1):211–220. doi: 10.1007/s11524-013-9823-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Levasseur M, Genereux M, Bruneau JF, et al. Importance of proximity to resources, social support, transportation and neighborhood security for mobility and social participation in older adults: results from a scoping study. BMC Public Health. 2015;15:503. doi: 10.1186/s12889-015-1824-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Butler TRG. Social capital, gentrification and neighbourhood change in London: a comparison of three south London neighbourhoods. Urban Studies. 2001;38:2145–2162. doi: 10.1080/00420980120087090. [DOI] [Google Scholar]
- 40.Uitermark JDJ, Kleinhans R. Gentrification as a governmental strategy: social control and social cohesion in Hoogvliet, Rotterdam. Environ Plan A. 2007;39:125. doi: 10.1068/a39142. [DOI] [Google Scholar]
- 41.LL. Gentrification and social mixing: towards an inclusive urban renaissance? Urban Studies. 2008;45:2449–2470. doi: 10.1177/0042098008097099. [DOI] [Google Scholar]
- 42.M D. Love thy neighbour? Social mixing in London’s gentrification frontiers. Environ Plan A. 2010;42:524. doi: 10.1068/a41379. [DOI] [Google Scholar]
- 43.Yy L. Gentrification and crime: identification using the 1994 Northridge earthquake in Los Angeles. J Urban Aff. 2010;32:549–577. doi: 10.1111/j.1467-9906.2010.00506.x. [DOI] [Google Scholar]
- 44.BacquéMh FY, Launay L, Vermeersch S. Social mix policies in Paris: discourses, policies and social effects. Int J Urban Reg Res. 2011;35:256–273. [PubMed] [Google Scholar]
- 45.Cm S. The influence of gentrification on gang homicides in Chicago neighborhoods, 1994 to 2005. Crime Delinq. 2014;60:569–591. doi: 10.1177/0011128712446052. [DOI] [Google Scholar]
- 46.Arcaya MC, Subramanian SV, Rhodes JE, Waters MC. Role of health in predicting moves to poor neighborhoods among Hurricane Katrina survivors. Proc Natl Acad Sci U S A. 2014;111(46):16246–16253. doi: 10.1073/pnas.1416950111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Diez Roux AV, Mair C. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 48.James P, Hart JE, Arcaya MC, Feskanich D, Laden F, Subramanian SV. Neighborhood self-selection: the role of pre-move health factors on the built and socioeconomic environment. Int J Environ Res Public Health. 2015;12(10):12489–12504. doi: 10.3390/ijerph121012489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gibbons J. Are gentrifying neighborhoods more stressful? A multilevel analysis of self-rated stress. SSM Popul Health. 2019;7:100358. doi: 10.1016/j.ssmph.2019.100358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cole HVS, Triguero-Mas M, Connolly JJT, Anguelovski I. Determining the health benefits of green space: does gentrification matter? Health Place. 2019;57:1–11. doi: 10.1016/j.healthplace.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 51.Linton SL, Cooper HL, Kelley ME, et al. Cross-sectional association between ZIP code-level gentrification and homelessness among a large community-based sample of people who inject drugs in 19 US cities. BMJ Open. 2017;7(6):e013823. doi: 10.1136/bmjopen-2016-013823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Anguelovski I, Cole HVS, O'Neill E, et al. Gentrification pathways and their health impacts on historically marginalized residents in Europe and North America: global qualitative evidence from 14 cities. Health Place. 2021;72:102698. doi: 10.1016/j.healthplace.2021.102698. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.