Abstract
This study was undertaken to assess the role of sex differences in the effects of exercise behavior change on incident metabolic syndrome (MetS) in Changhua County, Taiwan. Using data derived from the Changhua Community-based Integrated Screening (CHCIS), 22,594 eligible residents aged 40 years or older had the screening at least twice from 2005 to 2018. A prospective cohort study was designed to follow up the normal cohort without MetS at baseline to ascertain incident MetS in the light of the criteria of the Epidemiology Task Force Consensus Group. We then evaluated whether there was a sex difference in the outcome of incident MetS attributed to the change in exercise behavior from three (no, irregular, and regular exercise) maintained patterns already defined at baseline to either the enhanced pattern or the reduced pattern by the end of follow-up. We applied Cox proportional hazards regression model stratified by sex for estimating the hazard ratio of any two-group comparison. After adjustment for sociodemographic factors, the number of screenings attended, personal disease history, and other health behaviors, the influence of change in exercise behavior on incident MetS was statistically significant only in men. Specifically, maintaining no exercise showed a lower risk of MetS than maintaining regular exercise 21 % in men. Regarding the change in exercise behavior, men with the enhanced pattern reduced the risk of MetS by 15 % compared with those maintaining regular exercise. The findings suggest that positive changes in exercise behavior reduce the incidence of MetS in men but not in women.
Keywords: Change in exercise behavior, Incidence of metabolic syndrome (MetS), Sex difference
1. Introduction
Physical activity (PA) is recognized as an effective strategy to promote health (Rhodes et al., 2017), prevent non-communicable diseases (NCDs) (World Health Organization, 2013, Waxman, 2004), and decrease premature mortality (Rhodes et al., 2017), and metabolic syndrome (MetS) is one of the NCDs that has been proven to be preventable with PA (Myers et al., 2019, Rhodes et al., 2017). MetS is not only an important precursor to NCDs (Samson and Garber, 2014) but also a cost-effective preventable health condition (Joshi et al., 2020) currently affecting over one billion people worldwide (Saklayen, 2018).
The benefits of PA for MetS include the impact of exercise on insulin resistance, adipose fuel metabolism, inflammation, and epigenetic factors (Myers et al., 2019). Furthermore, longitudinal observational studies, randomized controlled trials, and meta-analysis studies have shown that PA can prevent MetS in the general population and prevent related diseases in MetS patients (Myers et al., 2019). Although only a few studies showed a statistically insignificant correlation between PA and the incidence of MetS (Santos et al., 2010), there is some limited empirical evidence on the relationship between natural changes in PA and MetS occurrence.
In particular, sex is a critical factor to explore in the relationship between changes in PA and MetS occurrence because of (1) sex differences in the incidence of MetS (Hadaegh et al., 2013, Hwang et al., 2013), (2) sex differences in PA behavior (Hallal et al., 2012, Mao et al., 2020), and (3) the possible moderation effects of sex on the relationship between PA and MetS (Chang et al., 2019). It is reasonable to hypothesize that there are sex differences in the association between exercise habits and the development of MetS. Therefore, using data from the Changhua Community-based Integrated Screening (CHCIS), this study investigates the relationship between changes in exercise behavior and the incidence of MetS with a view toward sex stratification.
2. Methods
2.1. Participants
The CHCIS, offered by the Changhua Health Bureau, offers multi-disease screening for people over 30 years of age. The screening modality of CHCIS originated in Keelong City and was referenced from a previous study published elsewhere (Chen et al. 2004). CHCIS commenced in 2005 and is administered annually, providing screening for multiple cancers (liver, breast, colorectal, oral, and cervical) and chronic diseases (hyperlipidemia, hypertension, hyperglycemia, and MetS), biochemical tests (blood and urine samples), and anthropometric measurements (height, weight, and circumference of the waist and hips) (Yeh et al., 2014). In addition, a structured questionnaire is used to understand participants’ health-related lifestyles (exercise, smoking, drinking alcohol, chewing betel nuts, dietary intake) and personal and family disease histories.
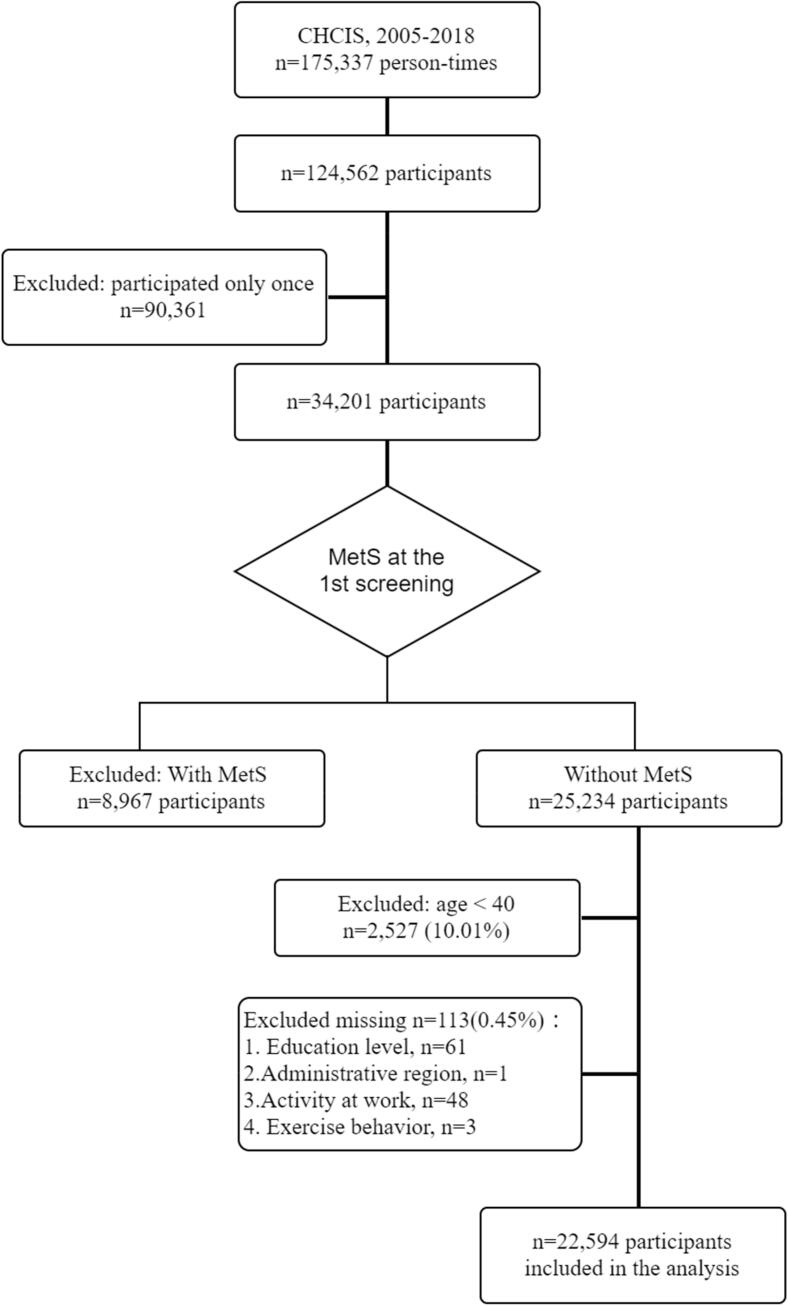
Data were drawn from the CHCIS screening database for the years 2005 to 2018, which contains 175,337 person-times records belonging to 124,562 participants. To delineate the incidence of MetS, we included the participants who were screened at least twice (n = 34,201) and did not have MetS at the first screening (n = 25,234). The exclusion criteria were as follows: (1) aged <40 years (n = 2,527) or records with missing data (n = 113). (Fig. 1).
Fig. 1.
Flow chart for the study population.
2.2. Definition of variables
2.2.1. Outcome variable: Incidence of MetS
This study used the definition of MetS by the Epidemiology Task Force Consensus Group (Alberti et al., 2005), which is better suited to Asian populations than the definition provided by the National Cholesterol Education Programme Adult Treatment Panel III (Expert Panel on Detection, 2001). The biochemical results of CHCIS screening indicate that those who meet three or more of the following five criteria are considered to have MetS: (1) central obesity (waist circumference ≥ 80 cm for women and ≥ 90 cm for men), (2) hypertriglyceridemia (≥150 mg/dL), (3) low level of high-density lipoprotein cholesterol (<50 mg/dL for females and < 40 mg/dL for males), (4) elevated blood pressure (systolic blood pressure ≥ 130 mmHg or diastolic blood pressure ≥ 85 mmHg) and (5) hyperglycemia (fasting glucose ≥ 100 mg/dL).
2.2.2. Independent variable: Change in exercise behavior
Taiwan’s official recommendations for exercise behavior (Ministry of Education, 1999, Sports Administration, Ministry of Education, 2022) classify it into three categories based on self-reported frequency and duration of exercise in the screening questionnaire: none, irregular, or regular. This classification can also be found in the recent literature (Mao et al., 2020). The main question was “Do you exercise currently?” followed by “On average, how many times a week do you exercise” and “How long do you exercise?” The “regular exercise” group was defined as participants who exercised more than three times a week and for more than 30 min each time. Those who reported that they exercised less than three times per week or <30 min per time were classified into the “irregular exercise” group, and those who did not exercise at all fell into the “no exercise” group.
Then, changes in exercise behavior were identified based on a comparison of exercise behavior at the time MetS occurred and the time of first participation in CHCIS. Changes were classified into five categories: maintain no exercise, maintain irregular exercise, maintain regular exercise, increase, and decrease.
2.2.3. Covariates
-
(1)
Sociodemographic variables. The sociodemographic covariates were described as follows: Age groups were set by dividing participants between <65 and ≥65 years old, as MetS is more likely to occur in people over 65 years of age (Kuk and Ardern, 2010). Education is divided into four categories: junior high school or below, high school, or college or above. According to the administrative division of Changhua County, the area of residence was divided into city, township, or village. Finally, the degree of PA at work was based on participants’ self-reports, including light, moderate, vigorous, and extreme. In this study, extreme and vigorous were combined into one category because too few participants reported their PA at work as extreme.
-
(2)
Personal health at the first screening. Personal health includes body mass index (BMI), the number of MetS components, and personal disease history. The BMI was calculated as weight in kilograms divided by the square of height in meters. Based on the Adult Health Status Standard (Health Promotion Administration, Ministry of Health and Welfare, Taiwan, 2018b), recommended by the Health Promotion Administration in Taiwan, BMI is classified into three groups: <24, 24–27, and ≥27, representing “not overweight,” “overweight,” and “obese,” respectively. The number of MetS components ranged from zero to two (three or higher would be classified as MetS and the participant’s data would be excluded before the analysis). The personal disease history includes diabetes mellitus, hypertension, cardiac disease, and hyperlipidemia, which participants self-reported at the first screening.
-
(3)
Other health-related behaviors. Therefore, we also included other health-related behaviors in the first screening questionnaire as covariates in the analysis, namely smoking, chewing betel nuts, drinking alcohol, and dietary habits. All behaviors are classified according to their health effects, based on the recommendations of the Ministry of Health and Welfare or the results of previous studies. (i) The classification of smoking behavior and betel nut chewing was based on participants’ self-reports in the screening questionnaire on “Do you smoke/chew betel nut?” (with responses of never, formerly, and currently), as seen in other previous studies (Chang et al., 2006, Katzmarzyk et al., 2005). (ii) The drinking alcohol question was “Do you have any drinking habits?” The responses were divided into four categories: never, previously, occasionally, and frequently. (iii) Dietary habits followed the Taiwan dietary guidelines of the Health Promotion Administration (Health Promotion Administration, Ministry of Health and Welfare, Taiwan, 2018a), including vegetable intake (≥3 bowls/day or not), fruit (≥7 times/week or not), beverages (little or other), and snacks (little or other).
2.3. Statistical analyses
Because this study hypothesized that sex affects the association between changes in exercise behavior and MetS, we first investigated whether there was a significant interaction between sex and exercise behavior change. Exercise behavior change was denoted by category variable (five categories), set to four dummy variables (with continuous exercise as the reference group). Using the Cox regression model (not shown in the results table), after controlling for other significant variables, a significant interaction between sex and change in exercise habits was found: (1) the interaction between sex and persistent physical inactivity showed a statistically significant difference (regression coefficient = 0.28157, p = 0.0016), and (2) the interaction between sex and improvement in exercise behavior was at the margin of significance (regression coefficient = 0.15915, p = 0.0644).
Hence, all analyses were stratified by sex. Cox regression analyses were used to evaluate the associations between changes in exercise behavior and the incidence of MetS after adjustment for possible risk factors for MetS confounders. The person-time was calculated as the observational years between the date of the first screening and the date of MetS identification or the last screening. The 22,594 participants in the study population were observed as 119,150 person-years with a range of observational years of 0.41 to 13.13 (mean = 5.27, SD = 2.82).
The results of Cox regression analyses are presented as hazard ratios (HRs) with 95 % confidence intervals. All statistical tests were conducted in SAS (version 9.4), and p < 0.05 was considered statistically significant.
2.4. Ethical review board
This experimental protocol was conducted with the approval of the Ethical Review Board (Chung Shan Medical University Hospital), approval number CS19019.
3. Results
The distribution of the characteristics and health-related behaviors of the 22,495 participants in the first screening is in Table 1. The majority of the participants are female, younger than 65, educated to the level of secondary school level or below, lightly PA at work, and living in a village. The participants were people without metabolic syndrome at the first screening who were relatively healthy, More than half of the participants had a BMI < 24, and less than one-third did not have any of the MetS components. The rate of chronic disease history (e.g., diabetes, hypertension, heart disease, and hyperlipidemia) was very low. The majority of participants had healthy behaviors: no smoking, no betel nut chewing, no alcohol consumption, and little beverage intake. However, the percentage of regular exercise and adequate amounts of vegetables and fruits were relatively low.
Table 1.
Participant characteristics and health-related behaviors at the first screening by sex (n = 22,594).
| Variable | n | % | Men |
Women |
Variable | n | % | Men |
Women |
||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||||||
| Participants | 22,594 | 100.00 | 7615 | 33.70 | 14,979 | 66.30 | |||||||
| Sociodemographic variables | Health-related behaviors | ||||||||||||
| Age*** | Exercise* | ||||||||||||
| <65 | 20,076 | 88.86 | 6337 | 83.22 | 13,739 | 91.72 | No | 9114 | 40.34 | 2985 | 39.20 | 6129 | 40.92 |
| ≧65 | 2518 | 11.14 | 1278 | 16.78 | 1240 | 8.28 | Irregular | 6435 | 28.48 | 2220 | 29.15 | 4215 | 28.14 |
| Education level*** | Regular | 7045 | 31.18 | 2410 | 31.65 | 4635 | 30.94 | ||||||
| Junior high school or below | 13,336 | 59.02 | 3907 | 51.31 | 9429 | 62.95 | Smoking*** | ||||||
| Senior high school | 6055 | 26.80 | 2265 | 29.74 | 3790 | 25.30 | Never | 18,496 | 81.86 | 3745 | 49.18 | 14,751 | 98.48 |
| College or above | 3203 | 14.18 | 1443 | 18.95 | 1760 | 11.75 | Former | 1608 | 7.12 | 1540 | 20.22 | 68 | 0.45 |
| Degree of PA at work*** | Current | 2490 | 11.02 | 2330 | 30.60 | 160 | 1.07 | ||||||
| Light | 15,077 | 66.73 | 3478 | 45.67 | 11,599 | 77.44 | Chewing betel nuts*** | ||||||
| Moderate | 4493 | 19.89 | 2404 | 31.57 | 2089 | 13.95 | Never | 20,699 | 91.61 | 5738 | 75.35 | 14,961 | 99.88 |
| Vigorous | 3024 | 13.38 | 1733 | 22.76 | 1291 | 8.62 | Former | 1279 | 5.66 | 1270 | 16.68 | 9 | 0.06 |
| Living area*** | Current | 616 | 2.73 | 607 | 7.97 | 9 | 0.06 | ||||||
| City | 4446 | 19.68 | 1252 | 16.44 | 3194 | 21.32 | Drinking alcohol*** | ||||||
| Township | 5395 | 23.88 | 1613 | 21.18 | 3780 | 25.24 | Never | 16,221 | 71.79 | 3393 | 44.56 | 12,828 | 85.64 |
| Village | 12,756 | 56.46 | 4750 | 62.38 | 8005 | 53.44 | Former | 372 | 1.65 | 353 | 4.64 | 19 | 0.13 |
| Personal health | Occasional | 4426 | 19.59 | 2506 | 32.91 | 1920 | 12.82 | ||||||
| BMI*** | Frequent | 1575 | 6.97 | 1363 | 17.90 | 212 | 1.42 | ||||||
| BMI < 24 | 13,051 | 57.76 | 3883 | 50.99 | 9168 | 61.21 | Dietary habits | ||||||
| 24 ≤ BMI < 27 | 6628 | 29.34 | 2764 | 36.30 | 3864 | 25.80 | Vegetables≧3 bowls/day | 2943 | 13.03 | 1005 | 13.20 | 1938 | 12.94 |
| BMI≧27 | 2915 | 12.90 | 968 | 12.71 | 1947 | 13.00 | Fruit≧7 times/week*** | 9194 | 40.69 | 2750 | 36.11 | 6444 | 43.02 |
| Number of MetS components*** | Little beverage*** | 16,184 | 71.63 | 4984 | 65.45 | 11,200 | 74.77 | ||||||
| 0 | 6556 | 29.02 | 1928 | 25.32 | 4628 | 30.90 | Little snack* | 12,226 | 54.11 | 4201 | 55.17 | 8025 | 53.58 |
| 1 | 8585 | 38.00 | 2978 | 39.11 | 5607 | 37.43 | |||||||
| 2 | 7453 | 32.99 | 2709 | 35.57 | 4744 | 31.67 | |||||||
| Personal disease history | |||||||||||||
| Diabetes mellitus*** | 660 | 2.92 | 300 | 3.94 | 360 | 2.40 | |||||||
| Hypertension*** | 2110 | 9.34 | 889 | 11.67 | 1221 | 8.15 | |||||||
| Cardiac disease** | 669 | 2.96 | 263 | 3.45 | 406 | 2.71 | |||||||
| Hyperlipidemia*** | 606 | 2.68 | 251 | 3.29 | 355 | 2.37 | |||||||
| * Indicates the variable showed a statistically significant sex difference by chi-square, * p < 0.05, ** p < 0.01, *** p < 0.001 | |||||||||||||
After stratification by sex and chi-square tests, most variables showed significant sex differences, except for vegetable intake. Women were more likely to be younger, lightly active at work, less educated than men were, and more likely to live in cities or towns. Men were more likely to be overweight, have more MetS components, and have chronic diseases. Furthermore, women seemed to have a healthier lifestyle.
Table 2 shows the frequency distribution of screening according to the occurrence of MetS. The overall mean person-years exceeded 5 years and were significantly higher in the group without MetS than in those with MetS (t = 9.36, p < 0.0001, not shown in table). Nearly-three-fourths of the study participants attended only the second screening. Table 3 shows the distribution of the incidence of MetS and change in exercise behavior by sex. In this study, the cumulative incidence of MetS was 22.98 % during the 14-year observation period for those without MetS at the first screening.
Table 2.
Distribution of screening frequency according to the occurrence of MetS.
| n | % | Observation person-years |
MetS |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| mean | SD | No |
Yes |
|||||||||
| n | row % |
Observation person-years |
n | row % |
Observation person-years |
|||||||
| mean | SD | mean | SD | |||||||||
| Participants | 22,594 | 100.00 | 5.27 | 2.82 | 17,402 | 77.02 | 5.37 | 2.84 | 5192 | 29.84 | 4.96 | 2.73 |
| Number of screenings attended | ||||||||||||
| 2 | 16,618 | 73.55 | 4.40 | 2.38 | 12,465 | 75.01 | 4.41 | 2.36 | 4153 | 24.99 | 4.39 | 2.44 |
| 3 | 4181 | 18.50 | 7.08 | 2.33 | 3419 | 81.77 | 7.16 | 2.28 | 762 | 18.23 | 6.72 | 2.52 |
| 4 | 1205 | 5.33 | 8.89 | 2.25 | 1009 | 83.73 | 8.95 | 2.19 | 196 | 16.27 | 8.57 | 2.54 |
| 5 | 320 | 1.42 | 9.41 | 2.61 | 267 | 83.44 | 9.55 | 2.54 | 53 | 16.56 | 8.70 | 2.88 |
| 6 | 135 | 0.60 | 9.31 | 2.51 | 118 | 87.41 | 9.43 | 2.50 | 17 | 12.59 | 8.43 | 2.52 |
| 7 | 65 | 0.29 | 9.48 | 2.39 | 60 | 92.31 | 9.57 | 2.47 | 5 | 7.69 | 8.46 | 0.51 |
| 8 | 31 | 0.14 | 10.39 | 1.66 | 29 | 93.55 | 10.35 | 1.71 | 2 | 6.45 | 10.97 | 0.07 |
| 9 | 17 | 0.08 | 11.13 | 1.85 | 14 | 82.35 | 11.26 | 1.94 | 3 | 17.65 | 10.54 | 1.48 |
| 10 | 10 | 0.04 | 12.12 | 0.74 | 10 | 100.00 | 12.12 | 0.74 | 0 | . | . | . |
| 11 | 8 | 0.04 | 11.11 | 0.96 | 7 | 87.50 | 11.29 | 0.88 | 1 | 12.50 | 9.87 | |
| 12 | 3 | 0.01 | 12.51 | 0.57 | 3 | 100.00 | 12.51 | 0.57 | 0 | . | . | . |
| 13 | 1 | 0.00 | 12.63 | . | 1 | 100.00 | 12.63 | . | 0 | 0.00 | . | . |
Table 3.
Distribution of the occurrence of MetS at the next screening and changes in exercise behavior by sex (n = 22,594).
| Total |
Men |
Women |
χ2 | p | ||||
|---|---|---|---|---|---|---|---|---|
| Total | % | Total | % | Total | % | |||
| Participants | 22,594 | 100 | 7615 | 33.7 | 14,979 | 66.3 | ||
| 7.88 | 0.005 | |||||||
| Yes | 5192 | 22.98 | 1666 | 21.88 | 3526 | 23.54 | ||
| Change in exercise behavior | 24.05e | <0.0001 | ||||||
| Maintain regular exercise | 4893 | 21.66 | 1703 | 22.36 | 3190 | 21.3 | ||
| Regulara → Xb → Regular | 3395 | 69.38 | 1150 | 67.53 | 2245 | 70.38 | ||
| Regular → Noc → Regular | 60 | 1.23 | 17 | 1.00 | 43 | 1.35 | ||
| Regular → Irregulard → Regular | 178 | 3.64 | 62 | 3.64 | 116 | 3.64 | ||
| Regular → Regular → Regular | 1260 | 25.75 | 474 | 27.83 | 786 | 24.64 | ||
| Maintain irregular exercise | 2691 | 11.91 | 987 | 12.96 | 1704 | 11.38 | ||
| Irregular → X → Irregular | 2005 | 74.51 | 741 | 75.08 | 1264 | 74.18 | ||
| Irregular → No → Irregular | 125 | 4.65 | 33 | 3.34 | 92 | 5.40 | ||
| Irregular → Irregular → Irregular | 407 | 15.12 | 164 | 16.62 | 243 | 14.26 | ||
| Irregular → Regular → Irregular | 154 | 5.72 | 49 | 4.96 | 105 | 6.16 | ||
| Maintain no exercise | 5564 | 24.63 | 1889 | 24.81 | 3675 | 24.53 | ||
| No → X → No | 4358 | 78.32 | 1474 | 78.03 | 2884 | 78.48 | ||
| No → No → No | 938 | 16.86 | 325 | 17.20 | 613 | 16.68 | ||
| No → Irregular → No | 191 | 3.43 | 65 | 3.44 | 126 | 3.43 | ||
| No → Regular → No | 77 | 1.38 | 25 | 1.32 | 52 | 1.41 | ||
| Increase | 5767 | 25.52 | 1842 | 24.19 | 3925 | 26.20 | ||
| No → X → Irregular | 1444 | 25.04 | 461 | 25.03 | 983 | 25.04 | ||
| No → X → Regular | 1128 | 19.56 | 341 | 18.51 | 787 | 20.05 | ||
| No → No → Irregular | 223 | 3.87 | 65 | 3.53 | 158 | 4.03 | ||
| No → No → Regular | 140 | 2.43 | 37 | 2.01 | 103 | 2.62 | ||
| No → Irregular → Irregular | 184 | 3.19 | 64 | 3.47 | 120 | 3.06 | ||
| No → Irregular → Regular | 118 | 2.05 | 27 | 1.47 | 91 | 2.32 | ||
| No → Regular → Irregular | 97 | 1.68 | 30 | 1.63 | 67 | 1.71 | ||
| No → Regular → Regular | 216 | 3.75 | 71 | 3.85 | 145 | 3.69 | ||
| Irregular → X → Regular | 1540 | 26.70 | 531 | 28.83 | 1009 | 25.71 | ||
| Irregular → NO → Regular | 57 | 0.99 | 17 | 0.92 | 40 | 1.02 | ||
| Irregular → Irregular → Regular | 238 | 4.13 | 73 | 3.96 | 165 | 4.20 | ||
| Irregular → Regular → Regular | 382 | 6.62 | 125 | 6.79 | 257 | 6.55 | ||
| Decrease | 3679 | 16.28 | 1194 | 15.68 | 2485 | 16.59 | ||
| Irregular → X → No | 1151 | 31.29 | 371 | 31.07 | 780 | 31.39 | ||
| Irregular → No → No | 162 | 4.40 | 55 | 4.61 | 107 | 4.31 | ||
| Irregular → Irregular → No | 155 | 4.21 | 46 | 3.85 | 109 | 4.39 | ||
| Irregular → Regular → No | 59 | 1.60 | 15 | 1.26 | 44 | 1.77 | ||
| Regular → X → No | 652 | 17.72 | 196 | 16.42 | 456 | 18.35 | ||
| Regular → X → Irregular | 945 | 25.69 | 336 | 28.14 | 609 | 24.51 | ||
| Regular → No → No | 85 | 2.31 | 29 | 2.43 | 56 | 2.25 | ||
| Regular → No → Irregular | 55 | 1.49 | 16 | 1.34 | 39 | 1.57 | ||
| Regular → Irregular → No | 67 | 1.82 | 26 | 2.18 | 41 | 1.65 | ||
| Regular → Irregular → Irregular | 121 | 3.29 | 37 | 3.10 | 84 | 3.38 | ||
| Regular → Regular → No | 72 | 1.96 | 16 | 1.34 | 56 | 2.25 | ||
| Regular → Regular → Irregular | 155 | 4.21 | 51 | 4.27 | 104 | 4.19 | ||
| Shading presents the exercise behavior at three time points. For those who participated more than four times, the middle exercise behavior is the previous exercise behavior at which MetS occurred, and those who did not occur MetS used the exercise behavior at the penultimate screening time. a “regular” was defined as participants who exercised more than three times a week and for more than 30 min each time. b For those who participated only twice, there were only two exercise behaviors, so the middle one is shown by “X”. c “no” was defined as who did not exercise at all. d “Irregular” was defined as participants who exercised less than three times per week or<30 min per time. eThe chi-square test was a bivariate analysis of change in exercise behavior (five categories: maintain regular exercise, maintain irregular exercise, maintain no exercise, increase decrease,) with sex (men/women). | ||||||||
Table 3 presents not only changes in exercise behavior at two points (the first screening and the screening at which MetS was found/the final screening) but also, in more detail, behavior during the period (the penultimate screening or the one before MetS occurred, which is only available for those who attended more than three screenings). We found that: (1) for the maintained regular exercise group, 4.87 % experienced inactivity or irregular exercise; (2) in the maintained irregular exercise group, 4.65 % had experienced inactivity, and 5.72 % had experienced regular exercise; (3) in the maintained no exercise group, 4.81 % had experienced irregular or regular exercise; (4) in the increasing group, only 2.67 % of exercise behaviors had gotten worse and then better; and (5) in the decreasing group, only 3.09 % of exercise behaviors improved and then become worse. Although a few inconsistencies were seen with the direction of the behavioral change subgroup (around 5 % when considering three PA measurements), exercise behavior at the first screening visit and at the one at which MetS was observed occurred was used to define behavioral change.
In general, the proportion of change in exercise behavior showed that more than a quarter of people increased their PA, while nearly a quarter remained no exercise, and the smallest group maintained irregular exercise.
Among the 22,594 participants and 119,150 person-years of the 14-year study period (2005–2018), the incidence of MetS was 43.58 per 1,000 person-years (Table 4), without statistically significant sex differences (p = 0.29). Among men, there was a statistically significant association between changes in exercise behavior and the incidence of MetS. Men in the maintain no exercise and the increased exercise groups had a statistically significantly lower risk of MetS than men did in the maintained regular exercise group. On the other hand, among women, there was no statistically significant association between changes in exercise behavior and the incidence of MetS, regardless of the reference group.
Table 4.
Relationships between change in exercise behavior and incidence of MetS by Cox regressiona (n = 22,594).
| Sex | Incidence of MetS |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Incidence of MetS |
Model 1 |
Model 2 |
Model 3 |
Model 4 |
|||||||||
| (Per 1,000 |
ref = maintain regular exercise |
ref = maintain irregular exercise |
ref = no exercise |
ref = increase |
|||||||||
| person-years) | HR | 95 % CI | HR | 95 % CI | HR | 95 % CI | HR | 95 % CI | |||||
| Menb | 43.31c | ||||||||||||
| Change in exercise behavior | |||||||||||||
| Maintain regular exercise | 48.44 | – | |||||||||||
| Maintain irregular exercise | 38.95 | 0.93 | 0.78 | 1.11 | – | ||||||||
| Maintain no exercise | 40.07 | 0.79 | 0.68 | 0.92 | 0.85 | 0.71 | 1.02 | – | |||||
| Increase | 42.46 | 0.85 | 0.73 | 0.98 | 0.91 | 0.77 | 1.09 | 1.07 | 0.93 | 1.24 | – | ||
| Decrease | 46.48 | 0.91 | 0.77 | 1.06 | 0.98 | 0.81 | 1.18 | 1.15 | 0.98 | 1.35 | 1.07 | 0.92 | 1.25 |
| Womenb | 43.70c | ||||||||||||
| Change in exercise behavior | |||||||||||||
| Maintain regular exercise | 45.34 | – | |||||||||||
| Maintain irregular exercise | 36.77 | 0.95 | 0.84 | 1.09 | – | ||||||||
| Maintain no exercise | 46.55 | 1 | 0.9 | 1.11 | 1.05 | 0.92 | 1.19 | – | |||||
| Increase | 41.76 | 0.94 | 0.85 | 1.04 | 0.98 | 0.87 | 1.12 | 0.94 | 0.86 | 1.03 | – | ||
| Decrease | 45.59 | 1.01 | 0.91 | 1.13 | 1.06 | 0.93 | 1.22 | 1.02 | 0.91 | 1.13 | 1.08 | 0.98 | 1.2 |
| a Adjusted for all covariates: age, education, degree of PA at work, living area, BMI, number of screenings attended, number of MetS components, personal disease history, health-related behaviors (smoking, chewing betel nuts, drinking alcohol), and dietary habits (vegetables, fruit, beverages, snacks). | |||||||||||||
| b In general, there is no statistically significant sex difference (p = 0.29) in the incidence of MetS by multivariate Cox regression model (n = 22,594). | |||||||||||||
| c Incidence of MetS = number of new cases of MetS/summed person-years of observation. | |||||||||||||
4. Discussion
The results show an association between changes in exercise behavior and the incidence of MetS only for men, where men who persisted in not exercising or increased their exercise behavior had a lower incidence of MetS than those who maintained regular exercise. These results differ from the findings of previous studies, possibly because (1) PA or exercise behavior can change during the study period, but most previous studies used baseline PA as a predictive variable, and (2) the effect of PA on the incidence of MetS may vary by sex.
4.1. PA or exercise behavior can change during the study period
Though habits are not easily changed (Duhigg, 2012), we found that 42.8 % of the participants’ exercise behavior was different from that at the first screening, without intervention. Previous research that used changes in PA or exercise behavior as an independent variable tended to use an interventional design (Mann, 2003) and found that improving PA reduced the incidence of MetS (den Boer et al., 2013, Tran et al., 2017). However, the results of observational studies were inconsistent. Through a longitudinal design, some studies found that physical inactivity at baseline increased the incidence of MetS in Norway (Wilsgaard and Jacobsen, 2007) and Korea (Jo et al., 2020). On the other hand, observational cohort studies showed only insignificant associations between PA and the incidence of MetS in the U.S. (Cheriyath et al., 2010) and Portugal (Santos et al., 2010). All of these studies used baseline PA as a predictive variable and did not consider possible changes in behavior during the study period. One of the strengths of our study was that we delineated the relationships between change in exercise behavior and the incidence of MetS without experimental intervention, and the findings could provide insights into the effect of PA or exercise behavior on MetS that are more detailed.
4.2. The effect of PA on the incidence of MetS may vary by sex
Sex is an important factor in both MetS and PA. There is not only a significant sex difference in the prevalence and incidence of MetS (Hadaegh et al., 2013, Pucci et al., 2017) but also in each of its components (Hwang et al., 2013). In addition, there are sex differences in risk factors for MetS (Scuteri et al., 2009). In terms of exercise behavior, the frequency, intensity, type, or variation has been shown to vary by sex as well (Althoff et al., 2017, Shaw et al., 2010). Therefore, it is reasonable to hypothesize that sex may influence the relationship between changes in exercise behavior and the incidence of MetS. However, because, to our knowledge, no previous studies have examined the possibility, there are no similar studies to compare our findings.
4.3. Possible reasons for sex differences in the effects of change in exercise behavior on the incidence of MetS
Our study found that men who maintained no exercise and increased exercise were significantly less likely to have MetS. The possible reasons are as follows: (1) A higher proportion of men who maintain no exercise are engaged in more strenuous work than those who maintain regular exercise (73 % for the former and 32 % for the latter, not shown in the table). Therefore, because of the higher total PA (which includes work), the risk of MetS may be lower in men who are physically inactive than in physically active men. A previous study (Mengesha et al., 2019) that used the GPAQ survey found that workplace activities contributed the highest percentage to total PA compared to recreational activities and travel to and from places, and men are more involved in PA at work than women (Hamrik et al., 2014). (2) In addition, we were encouraged to find that those who increased their exercise were significantly less likely to develop MetS than those who maintain regular exercise, but this result was only seen in male participants. Such results not only echo previous intervention studies that increased exercise can prevent the occurrence of chronic diseases (Pedersen and Saltin, 2006) (including MetS (van Namen et al., 2019)) but also provide new evidence that voluntary changes in exercise behavior (without external intervention) can be beneficial in preventing the occurrence of MetS.
However, why did the change in exercise behavior not have a significant effect on the incidence of MetS in women? Possible reasons are that (i) the type and intensity of exercise differ between sexes (Molanorouzi et al., 2015) and (ii) there are sex differences in the mechanisms of exercise effects on MetS. According to Park et al. (2021), regular exercise has no direct effect on the risk of metabolic disease but is mediated by other physiological factors; for instance, body composition (e.g., cell mass, mineral mass, and protein mass) plays an important role for men but obesity-related biomarkers (e.g., body fat) are key factors for women.
4.4. Findings other than the main research purpose
While it was not the main purpose of this study, we estimated the cumulative incidence of MetS by person-years in Changhua County as 43.58 per 1,000 person-years, which was similar to previous studies in other countries (Hadaegh et al., 2013, Santos et al., 2010). This implies there was no significant bias in the integrated screening group in our study.
5. Limitations
The limitations of this study are as follows. The first is related to the measurement and classification of exercise behavior. Exercise behaviors are self-reported in this study, which could lead to measurement errors due to recall bias and social desirability. Self-reported exercise is more likely to focus on high-intensity exercise while ignoring low- to moderate-intensity exercise (Ara et al., 2015). However, self-reported PA questionnaires have been used to estimate PA levels in large cohort studies (Ara et al., 2015); it is a practical assessment in a community-based screening program with implications for public health and the health of the general population. The existing literature also indicates no significant tendency to overestimate or underestimate PA in self-reporting compared to measurement methods (Prince et al., 2008). The PA questions in this study are similar to items in the Behavioral Risk Factor Surveillance System (BRFSS), and past studies have indicated the reliability and validity of PA measurements in BRFSS (Pierannunzi et al., 2013).
Second, due to the limited information on PA, only the amount of exercise was asked and not the overall daily activities (such as sedentary), which may have an impact on the occurrence of MetS.
Third, the CHCIS is conducted annually, and members of the public participate voluntarily. The definition of change in exercise behavior in this study was based on the exercise behavior at the first screening compared to exercise behavior at the screening where MetS occurred. We ignored any changes in exercise behavior during the observation period as well as the exact time of its onset. This means that changes in PA could have happened after MetS was observed. However, the description of the change in exercise behavior in Table 3 showed that the consistency between the occurrence of MetS and the exercise behavior of the previous screening was quite high (89–97 %), and it can be inferred that even though changes in PA may have happened after MetS appeared, this does not have a serious impact on the study results or its implications.
6. Conclusion
Using a large and long-term community cohort, we found sex differences in the effect of change in exercise behavior on the incidence of MetS, with positive changes in exercise behavior only reducing the occurrence of MetS for men.
Funding
This work was supported by the Ministry of Science and Technology, Taiwan (MOST 108-2410-H-040-009).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A.
Table A1.
Hazard ratios (95 % CI) for the incidence of MetS.
| Variables | Men |
Women |
||||
|---|---|---|---|---|---|---|
| HR | 95 % CI | HR | 95 % CI | |||
| Change in exercise behavior | ||||||
| Maintain regular exercise | Ref. | Ref. | ||||
| Maintain irregular exercise | 0.93 | 0.78 | 1.11 | 0.95 | 0.84 | 1.09 |
| Maintain no exercise | 0.79 | 0.68 | 0.92 | 1.00 | 0.90 | 1.11 |
| Increase | 0.85 | 0.73 | 0.98 | 0.94 | 0.85 | 1.04 |
| Decrease | 0.91 | 0.77 | 1.06 | 1.01 | 0.91 | 1.13 |
| Number of screenings attended | 0.52 | 0.48 | 0.564 | 0.49 | 0.46 | 0.52 |
| Sociodemographic variable | ||||||
| Age | ||||||
| <65 | Ref. | Ref. | ||||
| ≧65 | 2.12 | 1.85 | 2.43 | 2.01 | 1.80 | 2.25 |
| Education level | ||||||
| Junior high school or below | 1.13 | 0.97 | 1.32 | 1.34 | 1.17 | 1.54 |
| Senior high school | 1.16 | 0.99 | 1.35 | 1.13 | 0.97 | 1.31 |
| College or above | Ref. | Ref. | ||||
| Degree of PA at work | ||||||
| Light | Ref. | Ref. | ||||
| Moderate | 0.91 | 0.80 | 1.02 | 0.96 | 0.87 | 1.07 |
| Vigorous | 1.00 | 0.87 | 1.14 | 0.83 | 0.74 | 0.93 |
| Living area*** | ||||||
| City | 1.09 | 0.94 | 1.26 | 0.99 | 0.90 | 1.09 |
| Township | 0.92 | 0.81 | 1.04 | 0.94 | 0.87 | 1.02 |
| Village | Ref. | Ref. | ||||
| Personal health | ||||||
| BMI*** | ||||||
| BMI < 24 | Ref. | Ref. | ||||
| 24 ≤ BMI < 27 | 1.84 | 1.63 | 2.07 | 1.68 | 1.55 | 1.82 |
| BMI ≧ 27 | 2.17 | 1.88 | 2.50 | 1.80 | 1.64 | 1.97 |
| Number of MetS components | ||||||
| 0 | Ref. | Ref. | ||||
| 1 | 2.25 | 1.84 | 2.74 | 2.46 | 2.18 | 2.78 |
| 2 | 4.41 | 3.64 | 5.35 | 4.48 | 3.97 | 5.06 |
| Personal disease history | ||||||
| Diabetes mellitus | 1.45 | 1.20 | 1.76 | 1.47 | 1.26 | 1.72 |
| Hypertension | 1.40 | 1.22 | 1.59 | 1.47 | 1.33 | 1.62 |
| Cardiac disease | 0.95 | 0.74 | 1.22 | 1.13 | 0.96 | 1.34 |
| Hyperlipidemia | 1.19 | 0.95 | 1.49 | 1.17 | 0.98 | 1.39 |
| Health-related behaviors | ||||||
| Smoking | ||||||
| Never | Ref. | Ref. | ||||
| Former | 1.00 | 0.87 | 1.15 | 0.63 | 0.33 | 1.22 |
| Current | 1.19 | 1.05 | 1.35 | 1.16 | 0.78 | 1.72 |
| Chewing betel nuts | ||||||
| Never | Ref. | Ref. | ||||
| Former | 1.04 | 0.90 | 1.21 | 2.87 | 0.98 | 8.40 |
| Current | 1.15 | 0.96 | 1.36 | 0.55 | 0.14 | 2.22 |
| Drinking alcohol | ||||||
| Never | Ref. | Ref. | ||||
| Former | 1.2 | 0.9 | 1.5 | 0.25 | 0.06 | 1.06 |
| Occasional | 0.9 | 0.8 | 1.1 | 0.87 | 0.66 | 1.16 |
| Frequent | 1.0 | 0.9 | 1.2 | 0.97 | 0.87 | 1.08 |
| Dietary habits | ||||||
| Vegetable ≧ 3 bowls/day | 1.03 | 0.89 | 1.18 | 1.10 | 1.00 | 1.22 |
| Fruit ≧ 7 times/week | 1.12 | 1.01 | 1.25 | 1.02 | 0.95 | 1.09 |
| Little beverage | 0.99 | 0.89 | 1.10 | 0.97 | 0.89 | 1.05 |
| Little snack | 0.97 | 0.87 | 1.07 | 1.10 | 1.03 | 1.18 |
| Adjusted for all covariates: age, education, degree of PA at work, living area, BMI, number of screenings attended, number of MetS components, personal disease history, health-related behaviors (smoking, chewing betel nuts, drinking alcohol), and dietary habits (vegetables, fruit, beverages, snacks). | ||||||
Data availability
The data that has been used is confidential.
References
- Alberti K.G.M., Zimmet P., Shaw J. The metabolic syndrome—a new worldwide definition. Lancet. 2005;366(9491):1059–1062. doi: 10.1016/S0140-6736(05)67402-8. [DOI] [PubMed] [Google Scholar]
- Althoff T., Hicks J.L., King A.C., Delp S.L., Leskovec J. Large-scale physical activity data reveal worldwide activity inequality. Nature. 2017;547(7663):336–339. doi: 10.1038/nature23018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ara I., Aparicio-Ugarriza R., Morales-Barco D., de Souza W.N., Mata E., González-Gross M. Physical activity assessment in the general population; validated self-report methods. Nutricion Hospitalaria. 2015;31(3):211–218. doi: 10.3305/nh.2015.31.sup3.8768. [DOI] [PubMed] [Google Scholar]
- Chang S.H., Chang Y.Y., Wu L.Y. Gender differences in lifestyle and risk factors of metabolic syndrome: do women have better health habits than men? J. Clin. Nurs. 2019;28(11–12):2225–2234. doi: 10.1111/jocn.14824. https://onlinelibrary.wiley.com/doi/10.1111/jocn.14824 [DOI] [PubMed] [Google Scholar]
- Chang W.C., Hsiao C.F., Chang H.Y., Lan T.Y., Hsiung C.A., Shih Y.T., Tai T.Y. Betel nut chewing and other risk factors associated with obesity among Taiwanese male adults. Int. J. Obes. (Lond) 2006;30(2):359–363. doi: 10.1038/sj.ijo.0803053. [DOI] [PubMed] [Google Scholar]
- Chen T.H.H., Chiu Y.H., Luh D.L., Yen M.F., Wu H.M., Chen L.S.…Chen C.H. Community-based multiple screening model: Design, implementation, and analysis of 42,387 participants Taiwan community-based integrated screening group. Cancer: Interdiscip. Int. J. Am. Cancer Soc. 2004;100(8):1734–1743. doi: 10.1002/cncr.20171. [DOI] [PubMed] [Google Scholar]
- Cheriyath P., Duan Y., Nambiar L., Liao D. Obesity, physical activity and the development of metabolic syndrome: the Atherosclerosis Risk in Communities study. Eur. J. Prev. Cardiol. 2010;17(3):309–313. doi: 10.1097/HJR.0b013e32833189b8. [DOI] [PubMed] [Google Scholar]
- den Boer A.T., Herraets I., Stegen J., Roumen C., Corpeleijn E., Schaper N., Feskens E., Blaak E. Prevention of the metabolic syndrome in IGT subjects in a lifestyle intervention: results from the SLIM study. Nutr. Metab. Cardiovasc. Dis. 2013;23(11):1147–1153. doi: 10.1016/j.numecd.2012.12.005. [DOI] [PubMed] [Google Scholar]
- Duhigg C. Vol. 34. Random House; 2012. (The Power of Habit: Why We Do What We Do in Life and Business). [Google Scholar]
- Expert Panel on Detection E. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- Hadaegh F., Hasheminia M., Lotfaliany M., Mohebi R., Azizi F., Tohidi M., Sen U. Incidence of metabolic syndrome over 9 years follow-up; the importance of sex differences in the role of insulin resistance and other risk factors. PLoS One. 2013;8(9):e76304. doi: 10.1371/journal.pone.0076304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallal P.C., Andersen L.B., Bull F.C., Guthold R., Haskell W., Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- Hamrik Z., Sigmundová D., Kalman M., Pavelka J., Sigmund E. Physical activity and sedentary behaviour in Czech adults: results from the GPAQ study. Eur. J. Sport Sci. 2014;14(2):193–198. doi: 10.1080/17461391.2013.822565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Promotion Administration, Ministry of Health and Welfare, Taiwan (2018). Handbook of Daily Food Guide. https://www.hpa.gov.tw/Pages/EBook.aspx?nodeid=1208.
- Health Promotion Administration, Ministry of Health and Welfare, Taiwan (2018). Criteria for identifying Body Mass Index in adults.https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=542&pid=9737.
- Hwang J.H., Kam S., Shin J.-Y., Kim J.-Y., Lee K.-E., Kwon G.-H., Chun B.-Y., Chae S.C., Yang D.H., Park H.S. Incidence of metabolic syndrome and relative importance of five components as a predictor of metabolic syndrome: 5-year follow-up study in Korea. J. Korean Med. Sci. 2013;28(12):1768. doi: 10.3346/jkms.2013.28.12.1768. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3857373/pdf/jkms-28-1768.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jo H., Kim J.-Y., Jung M.-Y., Ahn Y.-S., Chang S.-J., Koh S.-B. Leisure time physical activity to reduce metabolic syndrome risk: a 10-year community-based prospective study in Korea. Yonsei Med. J. 2020;61(3):218–228. doi: 10.3349/ymj.2020.61.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi P., Ghosh K., Natarajan V.S., Mandal P. Impact of healthcare access and socio-economic conditions on prevalence of metabolic syndrome: evidence from 2015 brfss. Int. J. Bus. Excell. 2020;21(3):429–443. [Google Scholar]
- Katzmarzyk P.T., Church T.S., Janssen I., Ross R., Blair S.N. Metabolic syndrome, obesity, and mortality: impact of cardiorespiratory fitness. Diabetes Care. 2005;28(2):391–397. doi: 10.2337/diacare.28.2.391. [DOI] [PubMed] [Google Scholar]
- Kuk J.L., Ardern C.I. Age and sex differences in the clustering of metabolic syndrome factors: association with mortality risk. Diabetes Care. 2010;33(11):2457–2461. doi: 10.2337/dc10-0942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann C. Observational research methods. Research design II: cohort, cross-sectional, and case-control studies. Emerg. Med. J. 2003;20(1):54–60. doi: 10.1136/emj.20.1.54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao H.-Y., Hsu H.-C., Lee S.-D. Gender differences in related influential factors of regular exercise behavior among people in Taiwan in 2007: a cross-sectional study. PLoS One. 2020;15(1):e0228191. doi: 10.1371/journal.pone.0228191. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6993962/pdf/pone.0228191.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mengesha M.M., Roba H.S., Ayele B.H., Beyene A.S. Level of physical activity among urban adults and the socio-demographic correlates: a population-based cross-sectional study using the global physical activity questionnaire. BMC Public Health. 2019;19(1):1–11. doi: 10.1186/s12889-019-7465-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Education . Ministry of Education; Taiwan: 1999. Enhance Students’ Physical Fitness Middle Run Plan. [Google Scholar]
- Molanorouzi K., Khoo S., Morris T. Motives for adult participation in physical activity: type of activity, age, and gender. BMC Public Health. 2015;15(1):1–12. doi: 10.1186/s12889-015-1429-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers J., Kokkinos P., Nyelin E. Physical activity, cardiorespiratory fitness, and the metabolic syndrome. Nutrients. 2019;11(7):1652. doi: 10.3390/nu11071652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J., Choi J., Kim J.-E., Lee M., Shin A., Lee J.-K., Kang D., Choi J.-Y. Network of biomarkers and their mediation effects on the associations between regular exercise and the incidence of cardiovascular & metabolic diseases. Sci. Rep. 2021;11(1):1–11. doi: 10.1038/s41598-021-92312-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen B.K., Saltin B. Evidence for prescribing exercise as therapy in chronic disease. Scandinavian journal of medicine & science in sports. 2006;16(S1):3–63. doi: 10.1111/j.1600-0838.2006.00520.x. [DOI] [PubMed] [Google Scholar]
- Pierannunzi C., Hu S.S., Balluz L. A systematic review of publications assessing reliability and validity of the Behavioral Risk Factor Surveillance System (BRFSS), 2004–2011. BMC Med. Res. Method. 2013;13(1):1–14. doi: 10.1186/1471-2288-13-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prince S.A., Adamo K.B., Hamel M.E., Hardt J., Gorber S.C., Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int. J. Behav. Nutr. Phys. Act. 2008;5(1):1–24. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pucci G., Alcidi R., Tap L., Battista F., Mattace-Raso F., Schillaci G. Sex-and gender-related prevalence, cardiovascular risk and therapeutic approach in metabolic syndrome: a review of the literature. Pharmacol. Res. 2017;120:34–42. doi: 10.1016/j.phrs.2017.03.008. [DOI] [PubMed] [Google Scholar]
- Rhodes R.E., Janssen I., Bredin S.S., Warburton D.E., Bauman A. Physical activity: health impact, prevalence, correlates and interventions. Psychol. Health. 2017;32(8):942–975. doi: 10.1080/08870446.2017.1325486. [DOI] [PubMed] [Google Scholar]
- Saklayen M.G. The global epidemic of metabolic syndrome. Curr. Hypertens. Rep. 2018;20(2):1–8. doi: 10.1007/s11906-018-0812-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samson S.L., Garber A.J. Metabolic syndrome. Endocrinol. Metab. Clin. 2014;43(1):1–23. doi: 10.1016/j.ecl.2013.09.009. [DOI] [PubMed] [Google Scholar]
- Santos A.C., Severo M., Barros H. Incidence and risk factors for the metabolic syndrome in an urban South European population. Prev. Med. 2010;50(3):99–105. doi: 10.1016/j.ypmed.2009.11.011. [DOI] [PubMed] [Google Scholar]
- Scuteri A., Morrell C.H., Najjar S.S., Muller D., Andres R., Ferrucci L., Lakatta E.G. Longitudinal paths to the metabolic syndrome: can the incidence of the metabolic syndrome be predicted? The Baltimore Longitudinal Study of Aging. J. Gerontol. Ser. A: Biomed. Sci. Med. Sci. 2009;64(5):590–598. doi: 10.1093/gerona/glp004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw B.A., Liang J., Krause N., Gallant M., McGeever K. Age differences and social stratification in the long-term trajectories of leisure-time physical activity. J. Gerontol. B Psychol. Sci. Soc. Sci. 2010;65(6):756–766. doi: 10.1093/geronb/gbq073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sports Administration, Ministry of Education Sports Statistics. 2022. https://isports.sa.gov.tw/apps/Download.aspx?SYS=TIS&MENU_CD=M07&ITEM_CD=T01&MENU_PRG_CD=4&ITEM_PRG_CD=2 Retrieved from.
- Tran V.D., James A.P., Lee A.H., Jancey J., Howat P.A., Mai T.P., L. Effectiveness of a community-based physical activity and nutrition behavior intervention on features of the metabolic syndrome: a cluster-randomized controlled trial. Metab. Syndr. Relat. Disord. 2017;15(2):63–71. doi: 10.1089/met.2016.0113. [DOI] [PubMed] [Google Scholar]
- van Namen M., Prendergast L., Peiris C. Supervised lifestyle intervention for people with metabolic syndrome improves outcomes and reduces individual risk factors of metabolic syndrome: a systematic review and meta-analysis. Metabolism. 2019;101:153988. doi: 10.1016/j.metabol.2019.153988. [DOI] [PubMed] [Google Scholar]
- Waxman A. WHO global strategy on diet, physical activity and health. Food Nutr. Bull. 2004;25(3):292–302. doi: 10.1177/156482650402500310. https://journals.sagepub.com/doi/pdf/10.1177/156482650402500310 [DOI] [PubMed] [Google Scholar]
- Wilsgaard T., Jacobsen B.K. Lifestyle factors and incident metabolic syndrome: the Tromsø Study 1979–2001. Diabetes Res. Clin. Pract. 2007;78(2):217–224. doi: 10.1016/j.diabres.2007.03.006. https://www.diabetesresearchclinicalpractice.com/article/S0168-8227(07)00209-4/fulltext [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2013). Global action plan for the prevention and control of noncommunicable diseases 2013-2020. World Health Organization.
- Yeh Y.-P., Hu T.-H., Cho P.-Y., Chen H.-H., Yen A.-F., Chen S.-S., Chiu S.-H., Fann J.-Y., Su W.-W., Fang Y.-J., Chen S.-T., San H.-C., Chen H.-P., Liao C.-S. Evaluation of abdominal ultrasonography mass screening for hepatocellular carcinoma in Taiwan. Hepatology. 2014;59(5):1840–1849. doi: 10.1002/hep.26703. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that has been used is confidential.