Abstract
Objective:
The COVID-19 pandemic has generated debate as to whether community-level behavioral restrictions are worth the emotional costs of such restrictions. Using a longitudinal design, we juxtaposed the relative impacts of state-level restrictions and case counts with person-level direct and media-based exposures on distress, loneliness, and traumatic stress symptoms (TSS) during the COVID-19 pandemic in the United States.
Method:
From March 18, 2020 to April 18, 2020 and September 9, 2020 to October 16, 2020, a representative probability sample of U.S. adults (N = 5,594) completed surveys of their psychological responses and personal direct and media-based exposures to the COVID-19 pandemic. Survey data were merged with publicly available data on the stringency of state-level mitigation policies (e.g., school/business closures) during this period and longitudinal case/death counts for each state.
Results:
Three multilevel models (outcomes: distress, loneliness, TSS) were constructed. Measurements of dependent variables (Level 1) were nested within respondents (Level 2) who were nested within states (Level 3). State-level mitigation, cases, or deaths were not associated with any dependent variables (all p’s > .05). However, person-level exposures, including having contracted COVID-19 oneself (distress b = .22, p < .001; loneliness b = .13, p = .03; TSS b = .18, p = .001), knowing others who were sick (distress b = .04, p < .001; loneliness b = .02, p < .001; TSS b = .05, p < .001) or died (distress b = .10, p = .001; loneliness b = .10, p = .003; TSS b = .16, p < .001), and exposure to pandemic-related media (distress b = .12, p < .001; loneliness b = .09, p < .001; TSS b = .16, p < .001), were positively associated with outcomes.
Conclusions:
Personal exposures to COVID-19 are more strongly associated with psychological outcomes than statewide mitigations levied to stop disease spread. Results may inform public health response planning for future disease outbreaks.
Keywords: COVID-19, pandemic, statewide restrictions, media, psychological symptoms
The psychological impacts of the COVID-19 pandemic and associated mitigation efforts have been a topic of concern among social scientists and clinicians since the earliest outbreaks were recorded in the United States in 2020. The potential for a “parallel mental health crisis” was raised as the death toll from the pandemic was beginning to mount (Pfefferbaum & North, 2020). These concerns were supported by early research on the psychological responses to COVID-19, which suggested as the pandemic evolved, psychological distress increased (Holingue et al., 2020; Holman, Thompson, et al., 2020). Furthermore, the need to engage in prolonged social distancing for safety during the pandemic left many people feeling isolated and lonely (Killgore et al., 2020; Philpot et al., 2021; Zaninotto et al., 2022). Indeed, a recent meta-analysis of longitudinal research comparing pre- and postpandemic mental health found a significant increase in mental health symptoms after the onset of the pandemic (Robinson et al., 2022). Notably, however, these increases in psychological distress were not dramatic as some had anticipated (Shevlin et al., 2020), and seemed to taper off as the months wore on and people readjusted to their new normal (Robinson et al., 2022). Taken together, data thus far suggest that although COVID-19 has resulted in some elevation in psychological distress, many have exhibited striking psychological resiliency, in alignment with previous studies of adaptation to collective trauma (Garfin & Silver, 2016).
However, there has been widespread public debate in the United States over the psychological implications of COVID-19 mitigation efforts. An early rapid review of previous infectious disease outbreaks suggested that prior mandatory quarantines have been associated with negative psychological outcomes, with stressors (e.g., fears, boredom, financial loss, length of restrictions) associated with worse outcomes (e.g., posttraumatic stress disorder, anger; Brooks et al., 2020; Garfin et al., 2022). State-level mitigation efforts (e.g., lockdowns) to address the COVID-19 pandemic in the United States have been unprecedented in their scope and duration, prompting concerns that social distancing policies may cause more harm than good. The evidence from longitudinal studies lends some credence to these concerns. There appears to be a small effect of lockdowns on increasing psychological maladies (Prati & Mancini, 2021). However, there is substantial heterogeneity among the findings in this area (Aknin, De Neve, et al., 2022; Prati & Mancini, 2021), and more work must be done to better understand these relationships. In particular, some studies report that loneliness did not increase in the early months of the pandemic, whereas others found that loneliness rose in late 2020 as new surges in cases/deaths led to prolonged social distancing (Su et al., 2022). With the rise of new COVID-19 variants and the possibility of future viral threats increasing in the coming years (Rogalski et al., 2017), it is likely that mitigation measures may be necessary in the future as well—thus, highlighting the importance of understanding the psychological impact of these measures (Lee et al., 2021).
Unfortunately, psychological responses to the COVID-19 pandemic remain poorly understood. Much of the research on psychological responses to COVID-19 has relied on nonprobability convenience/opt-in samples that often produce biased results (Pierce et al., 2020) and self-report metrics of exposure to community restrictions (e.g., Ebrahimi et al., 2021). Mental health data from representative, probability-based samples have not yet been combined with objective measures of government-imposed restrictions in United States samples, though there are some clues from European studies. Data were combined from the Survey on Health, Aging, and Retirement in Europe (SHARE) and the Oxford University Coronavirus Government Response Tracker (OxCGRT; Hale et al., 2021) to assess the relationship between the stringency of government pandemic response policies and psychological symptoms. These assessments were inconclusive, with some outcomes showing positive relationships with mitigation stringency and others showing null or negative relationships among representative samples of adults (Aknin, Andretti, et al., 2022; Perelman et al., 2022; Voss et al., 2021). Thus, the extent to which strict mitigation measures are associated with psychological outcomes is still an open question, particularly in the United States, where mitigation policies varied dramatically by state over the course of the pandemic. Indeed, there may be many other predictors as well; knowing someone who was sick or died, media exposure (Garfin et al., 2020), and severe mitigation efforts (e.g., state mandated school and business closures) are all potential explanatory variables. Additionally, the question of whether governmental restrictions and/or personal direct exposures were related to loneliness has received little attention in large-scale, population-based studies.
Importantly, governmental mitigation efforts have not yet been contrasted with individual-level COVID-19 exposures that likely predict psychological distress: direct exposure to the actual virus (e.g., physical illness or knowing someone who died) and media-based exposure. The former has ample support as a likely predictor of psychological distress, with bereavement noted as a profound life stressor (Zisook et al., 1998) associated with mental health ailments (Stroebe et al., 2007) including depression (Grace, 2021; Norris & Murrell, 1990) and traumatic stress responses (Zisook et al., 1998) in general and during COVID-19 (Grace, 2021). Direct exposure through contracting COVID-19 may also portend elevated psychiatric symptoms. For example, a systematic review of SARS survivors documented elevated traumatic stress responses and depression over time (Rogers et al., 2020). These findings were echoed in several high-quality studies of survivors of COVID-19, including a large cohort study that evaluated the mental health outcomes among discharged patients (Huang et al., 2021). Similarly, a systematic review of COVID-19 “long haulers” demonstrated notable PTSD, depression, and other psychiatric morbidity presenting among survivors in several studies, with rates ranging from 23 to 56% (Nalbandian et al., 2021). Yet most studies of survivors of COVID-19 and other viral infections focused on patient populations, with few studies that address the mental health effects of viral infections in the general population.
A robust body of research also implicates COVID-19 related media exposure as a potent predictor of COVID-19-related psychological distress (Garfin et al., 2020; Holman, Thompson, et al., 2020; Xiong et al., 2020). Research conducted early in the pandemic using representative samples by our team (Holman, Thompson, et al., 2020) and others (Holingue et al., 2020; Riehm et al., 2020; Twenge & Joiner, 2020) found a positive relationship between media-exposure and mental distress. Although high-quality longitudinal research on COVID-19 related media exposure and psychological outcomes is rare, research conducted after previous crises indicates that effects may persist over time (Garfin et al., 2015; Holman Garfin, et al., 2020) and contribute to the development of a negative cycle of distress over time (Thompson et al., 2019). This may be particularly important during COVID-19, a chronic stressor where levels of media consumption may have waxed and waned over time (Pearman et al., 2021) as new variants emerged leading to spikes in COVID-19 cases and deaths. In sum, the relationship between COVID-19 related media exposure and psychological distress using longitudinal assessments of both media exposure and distress requires further investigation.
In the present study, we sought to illustrate the relationships between objective measures of pandemic severity—that is, state-level case and death counts, and state-level mitigation stringency over time—and psychological symptoms over the first 6 months of the COVID-19 pandemic. We also sought to juxtapose the state-level objective exposures with person-level direct and media-based exposures to the pandemic (e.g., reports of knowing others who got sick or died, hours of media exposure to pandemic-related coverage) to identify which had greater relative impact on psychological symptoms, controlling for demographics. On two occasions during 2020, soon after the initial outbreaks and again 6 months later, we assessed psychological symptoms and COVID-19 exposures in a large, nationally representative, probability-based sample of Americans. We also compiled state-level mitigation severity and disease spread data for each respondent over time. These data were linked with our survey data to assess the relationships between self-reports of pandemic experiences and objective measures of pandemic severity with global distress, loneliness, and traumatic stress symptoms.
Method
Transparency and Openness
All data and code are available on the Open Science Framework (OSF). Analyses were preregistered (https://osf.io/xbkt4).
Sample and Procedures
Respondents for this study were drawn from the NORC AmeriSpeak Panel, a probability-based panel of 35,000 U.S. households. NORC uses random door-to-door recruitment of individuals to the AmeriSpeak panel (via U.S. mail, telephone, and field interviews), who are then selected to participate in surveys by web. No one can volunteer for the AmeriSpeak panel. The Wave 1 survey was fielded to a sample of 11,139 panelists in three consecutive 10-day cohorts from March 18, 2020 to April 18, 2020 (Holman, Thompson, et al., 2020). Participants received an email stating that the survey was available whereupon they completed the survey online anonymously. Surveys are confidential, self-administered, and accessible any time for a designated period. Participants can complete them only once. NORC compensates AmeriSpeak panelists with points, exchangeable for merchandise, worth a cash equivalent (in this case $4). The Wave 1 survey yielded 6,598 completed surveys (59.2% completion rate); 84 cases (1.3%) were removed from the final sample due to unreliable survey completion times (under 6.5 min) or extensive missing data (>50% of questions), leaving N = 6,514 panelists (58.5% participation rate; Holman, Thompson, et al., 2020). The Wave 2 survey was fielded approximately 6 months later (September 26, 2020 to October 16, 2020) to all available Wave 1 panelists (6,501 panelists). Panelists were offered the cash equivalent of $6 for completing this survey. A total of 5,722 panelists completed the Wave 2 survey; 61 responses (1.1%) were removed for unreliable survey completion time or extensive missing data, leaving a final sample of N = 5,661 (87.1% completion rate, retention rate 86.9%). This study was approved by the Institutional Review Board of the University of California, Irvine. Participants provided informed consent when they joined the NORC panel and were informed that their identities would remain confidential.
Measures
Dependent Measures
Global Distress.
At both waves, 12 items assessed global distress. Nine items assessing depression, anxiety, and somatization from the abbreviated Brief Symptom Inventory-18 (Derogatis, 2001), along with three items assessing hostility from the original 53-item Brief Symptom Inventory (Derogatis, 1982) were used in the present study. Using a 5-point Likert-type scale ranging from 0 (not at all) to 4 (extremely, respondents reported feelings of distress experienced in the past week. Across waves, scale reliability was good (Wave a α = .85; Wave 2 α = .86). Responses were averaged across items at each wave.
Loneliness.
At both waves, loneliness was measured using the Three-Item Loneliness Scale (Hughes et al., 2004), adapted from the R-UCLA Loneliness Scale (Russell et al., 1980). Using a 5-point Likert-type scale ranging from 1 (never) to 5 (all the time), respondents reported feelings of loneliness experienced in the past week. Across waves, scale reliability was good (Wave 1 α = .84; Wave 2 α = .89). Responses were averaged across items at each wave.
Traumatic Stress Symptoms.
Two measures assessed traumatic stress symptoms at Waves 1 and 2 due to the timing of our assessments and the diagnostic criteria for acute stress disorder (measured within 30 days of a traumatic event) versus posttraumatic stress disorder (measured more than 30 days postevent). At Wave 1 (assessed acutely within days of the Presidential declaration of a pandemic in March 2020), respondents completed a modified version of the Acute Stress Disorder-5 Scale (Bryant, 2016) to capture the acute stress symptoms experienced in the past week. Example items included “Have you had distressing dreams about the Coronavirus outbreak?” and “Did you try to avoid situations or conversations that reminded you of the Coronavirus outbreak?” Responses across each item ranged from 1 (not at all) to 5 (a great deal). Scale reliability was good (α = .87). At Wave 2 (approximately 6 months into the pandemic), pandemic-specific posttraumatic stress symptoms were measured via the Primary Care PTSD Screen (Prins et al., 2016), which was modified to allow responses from 1 (not at all) to 5 (a great deal). Example items included “Been constantly on guard, watchful, or easily startled?” and “Felt numb or detached from others?” Scale reliability was good (α = .83). At each wave, items were averaged to create composite variables.
State-Level Independent Measures
State-Level Policy Stringency.
State-level policy stringency was assessed using data from the OxCGRT. State-level mitigation policies were assessed because most policies in the initial months of the pandemic were implemented at the state level (Documenting America’s Path to Recovery, n.d.). Also, because state mandates are a floor below which city/county/regional restrictions could not go, they likely represent the minimum level of restrictions in a state at a given point in time. OxCGRT data were downloaded from a public GitHub repository (Hale et al., 2021; https://www.bsg.ox.ac.uk/research/research-projects/covid-19-government-response-tracker). The project tracks and collects information on governmental policy actions to curb the spread of COVID-19 and condenses that information into a set of indices that reflect the extent of those actions. Of these policy indices, we relied on the Stringency Index, which is comprised of “C” category measures (i.e., containment and closure policies) such as closing schools and initiating stay-at-home orders, as well as one “H” category measure (i.e., public information campaigns). Stringency indices were plotted over time for each U.S. state from the onset of the pandemic (beginning January 1, 2020) until September 26, 2020 (the onset of our Wave 2 data collection effort). The area of each state’s distribution was computed to form a metric of the state’s overall commitment to COVID-mitigation measures. Computing the area of the distribution over time, versus using the mean stringency index value across time for each state, provides more nuance in understanding a state’s commitment to restrictive measures. Relying on mean values smooths over the fluctuations in a distribution over time, potentially obscuring meaningful differences between states and in some cases either over- or underestimating a state’s commitment over time. The area of the distribution avoids this altogether by computing a raw metric that accounts for these fluctuations (additional information about this area metric is provided in the online supplementary materials). States with less stringent policies over time exhibited smaller area values compared with states with more stringent policies (which in turn exhibited larger area values). Area values across states were normally distributed and standardized.
COVID-19 Case and Mortality Rates.
Incidence and mortality rates per 100,000 people by state were downloaded from the COVID-19 Data Repository administered by the Center for Systems Science and Engineering at Johns Hopkins University (https://github.com/CSSEGISandData/COVID-19). Incidence and mortality rates were plotted over time for each U.S. state beginning April 12, 2020 (the first date for which data were available) until September 26, 2020 (the onset of our Wave 2 data collection effort) and the area of each state’s distribution across these variables was computed to form metrics of the overall impact of COVID-19 (via incidence and mortality). States with fewer cases and deaths, respectively, over time exhibited smaller area values compared with states with more cases or deaths (which in turn exhibited larger area values). Area values across states were normally distributed and standardized (see online supplementary materials).
Person-Level Independent Variables
Media Exposure to the COVID-19 Pandemic.
At each wave, respondents indicated their average daily hours of media exposure to COVID-related news in the past week (indirect media exposure; see Holman, Thompson, et al., 2020) on traditional media (TV, radio, and print news), online news sources, and social media platforms. Response options ranged from 0 to 11 or more. Responses across these three media types were summed to create a composite variable reflecting a sum of total daily hours of media exposure. Because individuals could simultaneously engage across more than one media source, scores ranged from 0 to 33.
Personal Exposure to COVID-19.
At both waves, respondents reported how many people they knew who got sick with COVID-19 (currently or recovered), whether they knew someone who died from COVID-19, and whether they had personally become sick with COVID-19. These variables were respectively combined over time to form cumulative indicators of COVID-related personal exposure to illness and death. The number of people participants knew who had been sick with COVID-19 ranged from 0 to 43; personal knowledge of someone who had died from COVID-19 and having been sick with COVID-19 oneself were both dichotomous (0 = no, 1 = yes).
Key Covariates
Several covariates known to be associated with psychological symptoms in the context of large-scale traumatic events in prior research (Holman et al., 2014) were included in adjusted models. These covariates included demographic variables including age, gender, race/ethnicity, education, household size, and urban/rural residential area. Respondents also provided prepandemic health status (collected by NORC) upon enrollment into the AmeriSpeak panel 12–18 months before the pandemic began. These data were collected using a modified version of the National Health Interview Survey assessment of doctor-diagnosed mental and physical health ailments (U.S. Department of Health and Human Services, 2001). Specifically, participants reported whether a doctor had ever diagnosed them with several physical and mental health ailments. Prior mental health diagnoses were coded as 0 (no prior mental health diagnosis) or 1 (prior anxiety, depression, or any other emotional, nervous, or psychiatric diagnosis). Prior physical health diagnoses were coded as a count of eight possible prior diagnoses (i.e., high cholesterol, hypertension, diabetes/high blood sugar, heart disease, stroke, cancer, lung disease, and other diagnoses; range 0 to 8).
Analytic Strategy
Survey data were merged with the state-level data on policy stringency and cases/deaths for analysis. Unless otherwise indicated, all descriptive and inferential statistics were weighted using poststratification weights to adjust for probability of selection into the AmeriSpeak panel and to account for differences between our sample and U.S. Census benchmarks and attrition over time. Sampling weights were calculated with respect to age, sex, education, race/Hispanic ethnicity, and Census Division, as well as interactions of age × gender, age × race/ethnicity, and race/ethnicity × gender, based on estimates from the Current Population Survey (for more information about how the sample compares to Census benchmarks; see Table S1).
Given the nested structure of the data, multilevel models were performed using Stata 16.1 (StataCorp). In these multilevel models, measurements of dependent variables (Level 1) were nested within respondents (Level 2) who were nested within states (Level 3). Fixed effects included the main state-level independent variables including the Stringency Index, COVID-related cases, and COVID-related deaths. Key independent respondent-level variables such as personally knowing people who got very sick or died from COVID-19 and personally having become sick with COVID-19 oneself; demographics (age, gender, race/ethnicity, education, household size, urban/rural area); doctor-diagnosed mental and physical health ailments measured before the pandemic; COVID-19 related media exposure; and survey wave, respectively. In each model, random intercepts for respondents and states were specified. Random slopes for survey wave were also specified for all models to account for participant-specific trajectories in the dependent variables over time, thereby accounting for the shared variation in the dependent variables attributable to the repeated nature of the analysis. Data were analyzed using a complete case analysis due to low missingness across study variables (less than 1% missing for key study variables).
Results
The final weighted sample was demographically representative of the U.S. population (see Table S1; all reported statistics in this section are weighted). The mean age of participants was 47.51 years (range: 18–97 years); the sample was 52.0% female. The sample was 63.6% non-Hispanic White; 11.8% non-Hispanic Black; 8.7% non-Hispanic other/2+ races, and 16.0% Hispanic. In addition, 9.7% had less than a high school education, 28.5% had a high school diploma, 28.1% had some college, and 33.7% had a bachelor’s degree or greater. The mean household size for the sample was 2.86 persons (SD = 1.54) and 67.8% of participants indicated living in an NCES locale classified as urban. Participants reported an average of 1.05 physician-diagnosed physical health ailments (SD = 1.23; range: 0–8) and 18.1% reported a prior diagnosis of a mental health disorder. The mean number of people that participants knew who had become sick with COVID-19 was 1.15 (SD = 2.42; range: 0–43). Furthermore, 17.2% knew at least one person who had died from COVID-19; 4.9% of the sample had themselves contracted COVID-19. Mean levels of psychological symptomatology were low (global distress: Mgrand = .66, SD = .67; loneliness: Mgrand = 2.15, SD = 1.06; traumatic stress: Mgrand = 1.82, SD = .79). Psychological outcomes were significantly correlated with one another. General distress and traumatic stress symptoms were strongly corelated (r = .71; p < .001). Loneliness was also correlated with both general distress (r = .62; p < .001) and traumatic stress symptoms (r = .55; p < .001).
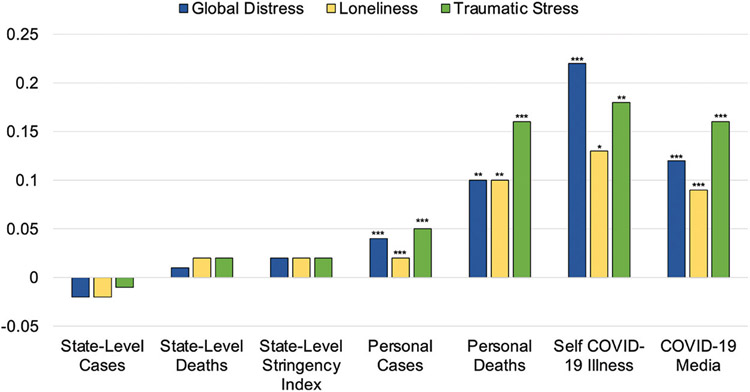
In multilevel regression models, global distress and loneliness increased significantly from the early onset of the pandemic 6 months later; however, traumatic stress symptoms decreased significantly (all p’s <.001). State-level restriction indicators were not associated with psychological outcomes (all p’s > .05). However, person-level experiences of COVID-19 exposure were significantly positively associated with all three outcomes. Having been sick with COVID-19 oneself was most strongly associated with psychological symptoms, followed by personally knowing someone who had died from COVID-19 and knowing more people who had been sick with COVID-19. Hours of media exposure to COVID-19-related news coverage were also positively associated with all three outcomes. Regression coefficients for each of these key predictors across all outcomes are presented in Figure 1, and results of the multilevel regression models appear in Table 1.
Figure 1. Standardized Coefficients for Multilevel Models Predicting Global Distress, Loneliness, and Traumatic Stress (N = 5,594).
Note. See the online article for the color version of this figure.
* p < .05. ** p < .01. *** p < .001.
Table 1.
Multilevel Models Predicting Global Distress, Loneliness, and Traumatic Stress (N = 5,594)
| Global distress |
Loneliness |
Traumatic stress |
||||
|---|---|---|---|---|---|---|
| Fixed effects parameters | b | 95% CI | b | 95% CI | b | 95% CI |
| State-level cases | −0.02 | [−0.05, 0.001] | −0.02 | [−0.05, 0.005] | −0.01 | [−0.03, 0.02] |
| State-level deaths | 0.01 | [−0.01, 0.03] | 0.02 | [−0.01, 0.05] | 0.02 | [−0.01, 0.04] |
| State-level stringency index | 0.02 | [−0.003, 0.04] | 0.02 | [−0.01, 0.05] | 0.02 | [−0.004, 0.03] |
| Personal COVID-19 illness | 0.04*** | [0.03, 0.05] | 0.02*** | [0.01, 0.03] | 0.05*** | [0.04, 0.07] |
| Personal COVID-19 death | 0.10** | [0.04, 0.16] | 0.10** | [0.03, 0.17] | 0.16*** | [0.11, 0.22] |
| Self COVID-19 illness | 0.22*** | [0.11, 0.33] | 0.13* | [0.02, 0.24] | 0.18** | [0.08, 0.28] |
| COVID-19 media | 0.12*** | [0.11, 0.14] | 0.09*** | [0.07, 0.11] | 0.16*** | [0.15, 0.18] |
| Agea | ||||||
| 30–44 | −0.11* | [−0.20, −0.02] | −0.13** | [−0.23, −0.04] | −0.01 | [−0.10, 0.08] |
| 45–59 | −0.31*** | [−0.39, −0.23] | −0.30*** | [−0.37, −0.23] | −0.18*** | [−0.26, −0.10] |
| 60+ | 0.49*** | [−0.56, −0.42] | —0.40*** | [−0.48, −0.32] | −0.36*** | [−0.45, −0.27] |
| Race/Ethnicityb | ||||||
| Black, non-Hispanic | −0.19*** | [−0.27, −0.11] | −0.05 | [−0.14, 0.04] | −0.10* | [−0.18, −0.01] |
| Other, non-Hispanic | 0.02 | [−0.07, 0.11] | 0.04 | [−0.04, 0.13] | 0.02 | [−0.07, 0.11] |
| Hispanic | 0.14* | [0.03, 0.26] | 0.08 | [−0.03, 0.18] | 0.11* | [0.02, 0.21] |
| Educationc | ||||||
| High school graduate | −0.05 | [−0.21, 0.12] | −0.03 | [−0.18, 0.11] | −0.16 | [−0.33, 0.01] |
| Some college | −0.07 | [−0.26, 0.11] | −0.02 | [−0.18, 0.15] | −0.15 | [−0.33, 0.03] |
| Bachelor’s+ | −0.07 | [−0.26, 0.12] | −0.04 | [−0.21, 0.13] | −0.09 | [−0.27, 0.10] |
| Female gender | 0.13*** | [0.09, 0.18] | 0.19*** | [0.15, 0.22] | 0.23*** | [0.19, 0.27] |
| Household size | 0.0 | [−0.02, 0.04] | 0.09*** | [−0.12, −0.06] | 0.001 | [−0.02, 0.02] |
| Urban residence | 0.04* | [0.01, 0.08] | 0.03 | [−0.01, 0.08] | 0.05* | [0.01, 0.09] |
| Prior mental health diagnosis | 0.65*** | [0.58, 0.71] | 0.50*** | [0.43, 0.57] | 0.46*** | [0.40, 0.51] |
| Prior physical health diagnosis | 0.07*** | [0.06, 0.09] | 0.06*** | [0.04, 0.08] | 0.04*** | [0.03, 0.06] |
| Survey wave | 0.30*** | [0.27, 0.33] | 0.17*** | [0.14, 0.19] | −0.07*** | [−0.10, −0.05] |
| Constant | −0.19* | [−0.36, −0.02] | −0.15 | [−0.30, 0.01] | −0.08 | [−0.24, 0.07] |
| Random effects | Variance | 95% CI | Variance | 95% CI | Variance | 95% CI |
| State intercept | 0.001 | [0.0001, 0.01] | 0.001 | [0.0004, 0.01] | 0.001 | [0.0001, 0.01] |
| Participant intercept | 0.62 | [0.39, 0.97] | 0.75 | [0.45, 1.25] | 0.63 | [0.37, 1.09] |
| Survey wave slope | 0.60 | [0.26, 1.40] | 0.65 | [0.21, 1.96] | 0.71 | [0.28, 1.78] |
| Survey Wave × Participant Covariance | −0.18 | [−0.42, 0.05] | −0.28 | [−0.62, 0.06] | −0.24 | [−0.55, 0.06] |
| Residual | 0.04 | [0.0001, 17.15] | 0.06 | [0.0005, 8.06] | 0.05 | [0.0003, 10.56] |
Note. Continuous measures were standardized about the grand mean for analysis to report standardized estimates. Estimates were weighted to adjust for probability of selection into the AmeriSpeak panel and to account for differences between the sample and U.S. Census benchmarks and attrition over time.
Reference group for age is 18–30.
Reference group for race/ethnicity is White, non-Hispanic.
Reference group for education is less than high school.
p < .05.
p < .01.
p < .001.
There were also significant differences in outcomes over time for individuals from different demographic groups. Age was negatively associated with all three outcomes, such that older age groups reported lower symptoms than did those in the 18–29 age bracket. Women also reported more symptoms across all outcomes than did men. Non-Hispanic Black participants also reported lower global distress and traumatic stress symptoms, while Hispanic participants reported greater global distress and traumatic stress symptoms compared with non-Hispanic White participants. Urban residents also reported greater global distress and traumatic stress symptoms. Household size was negatively associated with loneliness, but not significantly associated with other outcomes. Prior mental and physical health diagnoses were also positively associated with all outcomes.
Discussion
The present study uniquely juxtaposes personal versus statewide factors toward a more complete understanding of how people respond to a collective trauma—in this case, the COVID-19 pandemic. According to Bronfenbrenner’s (1979) ecological systems theory, the broader environment plays a vital role in psychological development; however, the understanding of macrolevel variables (e.g., community, state, or national characteristics) is underdeveloped in the literature (for exceptions, see Gruebner et al., 2015; Jose et al., 2017). Most studies do not integrate these macrolevel variables with individual-level data, particularly in the context of community-wide stressors. While our study did not find associations among state-level cases, deaths, or mitigation stringency and psychological outcomes, other research has found associations with neighborhood characteristics and mental health during prior viral outbreaks (Jose et al., 2017), highlighting the importance of considering the broader environmental context in the study of responses to collective traumas.
Although previous findings have demonstrated a significant relationship between lockdowns and other pandemic mitigation measures and psychological symptoms (Prati & Mancini, 2021), the present study did not find support for this relationship when using an objective measure of state-level mitigation severity, nor did it find a significant relationship between statewide cases or deaths and symptomatology. In contrast, there were robust significant relationships between personal direct experiences with the pandemic—that is, knowing someone who got very sick or died or getting sick oneself—and increased global distress, loneliness, and traumatic stress symptoms. The present study also found a significant association between exposure to pandemic-related media coverage and increased symptoms over time, extending prior findings in this area (Holman, Thompson, et al., 2020). These results suggest that personal experiences may be more strongly and uniquely associated with psychological symptomatology than are state-level restrictions. While public debate in the United States has proposed that statewide restrictions are harmful for mental health, the present findings do not indicate a direct relationship between such restrictions and psychological symptoms. Instead, it appears that direct exposure to the effects of the virus itself—or media coverage of it—was more strongly associated with psychological symptoms. In other words, personally knowing someone who has died appears substantially more stressful than the impersonal fact of higher death counts in one’s state. These findings were also robust when controlling for demographic factors that are known to be associated with increased psychological symptoms, such as gender, and that have been linked to poorer outcomes from COVID-19, such as race/ethnicity.
These findings bolster and extend prior work in the field in several ways. First, the relationships between becoming personally sick or knowing someone with COVID-19 and psychological distress was found throughout the general populace, expanding prior work that primarily focused on those with severe illness such as those who had been hospitalized (Rogers et al., 2020), who presented with postacute COVID-19 syndrome or “long COVID” (Nalbandian et al., 2021), or who cared for loved ones with severe and/or persistent COVID-19 (Azoulay et al., 2021). Similar to cross-sectional survey data (Grace, 2021), using longitudinal data we found that knowing someone who died was a potent predictor of distress. This supports prior research on the association between bereavement and the stress response including psychological distress (Stroebe et al., 2007) and addresses the general dearth of empirical data on the psychological impact of COVID-19-related bereavement (Stroebe & Schut, 2021) or knowing someone sick with COVID-19 (Azoulay et al., 2021). Importantly, we note bereavement may also be associated with subsequent consequences for physical health (Stroebe et al., 2007), which may have implications for public health and clinical practice as society continues to deal with the COVID-19 pandemic and its aftermath.
Recent meta-analytic findings suggest media exposure during COVID-19 has demonstrated small yet consistent adverse effects on mental health (Chu et al., 2022). We extend this work by measuring media exposure over time and contrasting these effects with both direct exposure to COVID-19 and state-level indicators of exposure. We find the effect size for media exposure was similar to those associated with direct experiences (knowing someone who died or who was sick or personal illness). We note these relatively small effects of multiple exposures may compound over time, with incremental impacts on the mental health of the populace (Kar et al., 2013; May & Wisco, 2016). In contrast, statewide restrictions did not predict distress, highlighting the importance of regulating individual behavior (e.g., avoiding disease exposure and high levels of media exposure) to promote adaptive psychological responses during times of crisis.
The United States in 2020 presented a unique context in which to study these issues. The implementation and downstream effects of COVID-19 mitigation policies were hotly contested topics of discussion in the United States. In an election year marked by intense political polarization, the experience of the pandemic contributed to a cascade of trauma over the course of 2020 (Silver et al., 2021). Should state-wide mitigation measures become necessary again as cases rise with future variants (Christie et al., 2021), the present findings may inform the conversation around how best to implement these policies. Our results suggest that statewide mitigation may not be as detrimental to mental health as direct exposure to the actual virus or sensationalized media coverage of the crisis.
Although our measures of state-level variables do not capture granular differences at the county or zip code levels, results represent an important step in understanding the mechanisms for the impact of the pandemic on mental well-being. Because our measures of state-level policy stringency and pandemic severity were coarse, it is possible that they did not adequately reflect the specific restrictions/mandates affecting respondents’ behavior. That is, a finer assessment of county- or community-level restrictions/mandates may be needed to identify associations between restrictions/mandates and psychological symptoms. However, as outlined above, we believe, while the measure is imperfect, it still has utility for assessing mitigation stringency, especially during the early months of the pandemic when most policies were implemented at the state level. Nevertheless, future research should utilize more fine-grained data on pandemic severity and mitigation stringency at the community level to better understand how we might calibrate interventions to prevent disease without undermining public mental health (e.g., Jose et al., 2017). Such an investigation should also investigate whether/how the relationship between policy stringency and psychological symptoms may differ among specific demographic groups who were affected most directly by the pandemic (e.g., lower socioeconomic status, racial minority groups). The effects of statewide lockdowns likely also had direct impacts on people’s lives (e.g., lost social connection, finding childcare). Indeed, it is possible the person-level measures of exposure were themselves influenced by the stringency of statewide mitigation policies and case and death counts, which also likely operated in tandem with one another (i.e., more stringent measures implemented as cases rose, resulting in reduced disease spread over time). Future research might tease apart the interrelations among these secondary stressors and explore their independent/unique effects on psychological outcomes over time.
One consideration when interpreting these findings is their positionality in time. The outcomes and the measure of media exposure in the present study represent two snapshots in time—one in the early days of the pandemic and one 6 months later. In contrast, the state-level measures capture the variability in pandemic conditions over the course of the entire 6-month period. Similarly, the measures of personal COVID-19 illness and knowledge of others who had become sick or died represent the accumulation of participant experiences since the beginning of the pandemic. Future studies tracking this information in a more fine-grained way (e.g., via ecological momentary assessment) could help tease apart the nuances in their impact at the person level over time.
Despite these limitations, this study has several strengths, including a high-quality sample and creative use of objective state-level metrics. As such, the findings from the present study may be considered generalizable to the population of the United States. Longer term follow-up will determine whether these findings are robust over the coming years as communities experience differential vaccination rates, the lifting of restrictions, and waxing and waning COVID-19 spread as new variants arise. Future research may also explore how the cascade of trauma in the United States contributed to trajectories of psychological symptoms over time (Silver et al., 2021).
Conclusion
Experts indicate that future pandemics will undoubtedly occur, as will widespread mitigation efforts to stop the spread of novel viruses. Although we find no evidence for negative psychological outcomes related to such mitigation measures, this work suggests that understanding the person-level psychological implications of such events is essential to planning large-scale public health response. Insofar as personal experiences are associated with psychological symptoms, it is incumbent upon state and local officials to implement targeted measures to prevent loss of life in their communities. Finally, we would encourage the public to take heed of such measures to limit the potential detrimental psychological outcomes that accompany sickness and loss.
Supplementary Material
Acknowledgments
Project support was provided by U.S. National Science Foundation Grants SES 2026337 and SES 2049932 to Roxane Cohen Silver, E. Alison Holman, and Dana Rose Garfin. Dana Rose Garfin was supported by National Institute on Minority Health and Health Disparities Award K01 MD013910. Authors report no conflicts of interest. All data and code are available on the Open Science Framework (OSF). Analyses were preregistered (https://osf.io/xbkt4).
We thank the NORC AmeriSpeak team of J. Michael Dennis and David Reisner for survey research and sampling guidance, for preparation of the online surveys, and for preparation of the data files. We also thank Emma Grisham, Daniel Relihan, and Kayley Estes for contributions to the larger project from which these data were drawn.
Footnotes
Supplemental materials: https://doi.org/10.1037/hea0001233.supp
References
- Aknin LB, Andretti B, Goldszmidt R, Helliwell JF, Petherick A, De Neve JE, Dunn EW, Fancourt D, Goldberg E, Jones SP, Karadag O, Karam E, Layard R, Saxena S, Thornton E, Whillans A, & Zaki J (2022). Policy stringency and mental health during the COVID-19 pandemic: A longitudinal analysis of data from 15 countries. The Lancet. Public Health, 7(5), e417–e426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aknin LB, De Neve JE, Dunn EW, Fancourt DE, Goldberg E, Helliwell JF, Jones SP, Karam E, Layard R, Lyubomirsky S, Rzepa A, Saxena S, Thornton EM, VanderWeele TJ, Whillans AV, Zaki J, Karadag O, & Ben Amor Y (2022). Mental health during the first year of the COVID-19 pandemic: A review and recommendations for moving forward. Perspectives on Psychological Science, 17(4), 915–936. 10.1177/17456916211029964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azoulay É, Curtis JR, & Kentish-Barnes N (2021). Ten reasons for focusing on the care we provide for family members of critically ill patients with COVID-19. Intensive Care Medicine, 47(2), 230–233. 10.1007/s00134-020-06319-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U (1979). The ecology of human development. Harvard University Press. [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, & Rubin GJ (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant RA (2016). Acute stress disorder: What it is and how to treat it. Guilford Press. [Google Scholar]
- Christie A, Brooks JT, Hicks LA, Sauber-Schatz EK, Yoder JS, & Honein MA (2021). Guidance for implementing COVID-19 prevention strategies in the context of varying community transmission levels and vaccination coverage. Morbidity and Mortality Weekly Report, 70(30), 1044–1047. 10.15585/mmwr.mm7030e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu TH, Yeo TED, & Su Y (2022). Effects of exposure to COVID-19 news and information: A meta-analysis of media use and uncertainty-related responses during the pandemic. Journalism & Mass Communication Quarterly, 99(1), 89–112. 10.1177/10776990211068857 [DOI] [Google Scholar]
- Derogatis LR (1982). Brief Symptom Inventory: Administration and procedures manual - I. Clinical Psychometric Research, Inc. [Google Scholar]
- Derogatis LR (2001). BSI18, Brief Symptom Inventory 18: Administration, scoring and procedures. NCS Assessments. [Google Scholar]
- Documenting America’s Path to Recovery. (n.d.). Ballotpedia: The Encyclopedia of American Politics. Retrieved April 29, 2022, from https://ballotpedia.org/Documenting_America%27s_Path_to_Recovery#Coronavirus_responses_by_state
- Ebrahimi OV, Hoffart A, & Johnson SU (2021). Physical distancing and mental health during the COVID-19 pandemic: Factors associated with psychological symptoms and adherence to pandemic mitigation strategies. Clinical Psychological Science, 9(3), 489–506. 10.1177/2167702621994545 [DOI] [Google Scholar]
- Garfin DR, Djokovic L, Silver RC, & Holman EA (2022). Acute stress, worry, and impairment in healthcare and non-healthcare essential workers during the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy. Advance online publication. 10.1037/tra0001224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfin DR, Holman EA, & Silver RC (2015). Cumulative exposure to prior collective trauma and acute stress responses to the Boston marathon bombings. Psychological Science, 26(6), 675–683. 10.1177/0956797614561043 [DOI] [PubMed] [Google Scholar]
- Garfin DR, & Silver RC (2016). Responses to natural disasters. In Friedman HS (Ed.), Encyclopedia of mental health (2nd ed., Vol. 4, pp. 35–46). Academic Press. 10.1016/B978-0-12-397045-9.00161-0 [DOI] [Google Scholar]
- Garfin DR, Silver RC, & Holman EA (2020). The novel coronavirus (COVID-2019) outbreak: Amplification of public health consequences by media exposure. Health Psychology, 39(5), 355–357. 10.1037/hea0000875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace MK (2021). COVID-19 bereavement, depressive symptoms, and binge drinking. SSM - Mental Health, 1, Article 100041. 10.1016/j.ssmmh.2021.100041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruebner O, Lowe SR, Sampson L, & Galea S (2015). The geography of post-disaster mental health: Spatial patterning of psychological vulnerability and resilience factors in New York City after Hurricane Sandy. International Journal of Health Geographics, 14(1), 16. 10.1186/s12942-015-0008-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale T, Angrist N, Goldszmidt R, Kira B, Petherick A, Phillips T, Webster S, Cameron-Blake E, Hallas L, Majumdar S, & Tatlow H (2021). A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nature Human Behaviour, 5(4), 529–538. 10.1038/s41562-021-01079-8 [DOI] [PubMed] [Google Scholar]
- Holingue C, Kalb LG, Riehm KE, Bennett D, Kapteyn A, Veldhuis CB, Johnson RM, Fallin MD, Kreuter F, Stuart EA, & Thrul J (2020). Mental distress in the United States at the beginning of the COVID-19 pandemic. American Journal of Public Health, 110(11), 1628–1634. 10.2105/AJPH.2020.305857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman EA, Garfin DR, & Silver RC (2014). Media’s role in broadcasting acute stress following the Boston Marathon bombings. Proceedings of the National Academy of Sciences of the United States of America, 111(1), 93–98. 10.1073/pnas.1316265110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holman EA, Garfin DR, Lubens P, & Silver RC (2020). Media exposure to collective trauma, mental health, and functioning: Does it matter what you see? Clinical Psychological Science, 8(1), 111–124. 10.1177/2167702619858300 [DOI] [Google Scholar]
- Holman EA, Thompson RR, Garfin DR, & Silver RC (2020). The unfolding COVID-19 pandemic: A probability-based, nationally representative study of mental health in the United States. Science Advances, 6(42), eabd5390. 10.1126/sciadv.abd5390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, Kang L, Guo L, Liu M, Zhou X, Luo J, Huang Z, Tu S, Zhao Y, Chen L, Xu D, Li Y, Li C, Peng L, … Cao B (2021). 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. The Lancet, 397(10270), 220–232. 10.1016/S0140-6736(20)32656-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes ME, Waite LJ, Hawkley LC, & Cacioppo JT (2004). A short scale for measuring loneliness in large surveys: Results from two population-based studies. Research on Aging, 26(6), 655–672. 10.1177/0164027504268574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jose R, Holman EA, & Silver RC (2017). The importance of the neighborhood in the 2014 Ebola outbreak in the United States: Distress, worry, and functioning. Health Psychology, 36(12), 1181–1185. 10.1037/hea0000518 [DOI] [PubMed] [Google Scholar]
- Kar N, Krishnaraaj R, & Rameshraj K (2013). Long-term mental health outcomes following the 2004 Asian tsunami disaster: A comparative study on direct and indirect exposure. Disaster Health, 2(1), 35–45. 10.4161/dish.24705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killgore WDS, Cloonan SA, Taylor EC, Miller MA, & Dailey NS (2020). Three months of loneliness during the COVID-19 lockdown. Psychiatry Research, 293, 113392. 10.1016/j.psychres.2020.113392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JH, Lee H, Kim JE, Moon SJ, & Nam EW (2021). Analysis of personal and national factors that influence depression in individuals during the COVID-19 pandemic: A web-based cross-sectional survey. Globalization and Health, 17(1), 3. 10.1186/s12992-020-00650-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- May CL, & Wisco BE (2016). Defining trauma: How level of exposure and proximity affect risk for posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 8(2), 233–240. 10.1037/tra0000077 [DOI] [PubMed] [Google Scholar]
- Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, Cook JR, Nordvig AS, Shalev D, Sehrawat TS, Ahluwalia N, Bikdeli B, Dietz D, Der-Nigoghossian C, Liyanage-Don N, Rosner GF, Bernstein EJ, Mohan S, Beckley AA, … Wan EY (2021). Post-acute COVID-19 syndrome. Nature Medicine, 27(4), 601–615. 10.1038/s41591-021-01283-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris FH, & Murrell SA (1990). Social support, life events, and stress as modifiers of adjustment to bereavement by older adults. Psychology and Aging, 5(3), 429–436. 10.1037/0882-7974.5.3.429 [DOI] [PubMed] [Google Scholar]
- Pearman O, Boykoff M, Osborne-Gowey J, Aoyagi M, Ballantyne AG, Chandler P, Daly M, Doi K, Fernández-Reyes R, Jiménez-Gómez I, Nacu-Schmidt A, McAllister L, McNatt M, Mocatta G, Petersen LK, Simonsen AH, & Ytterstad A (2021). COVID-19 media coverage decreasing despite deepening crisis. The Lancet. Planetary Health, 5(1), e6–e7. 10.1016/S2542-5196(20)30303-X [DOI] [PubMed] [Google Scholar]
- Perelman J, Xavier M, & Barros PP (2022). How do European mature adults and elderly perceive SARS-COV-2 and associated control measures? A cross-country analysis of mental health symptoms in June and July 2020. International Journal of Public Health, 67, 1604218. 10.3389/ijph.2022.1604218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum B, & North CS (2020). Mental health and the COVID-19 pandemic. The New England Journal of Medicine, 383(6), 510–512. 10.1056/NEJMp2008017 [DOI] [PubMed] [Google Scholar]
- Philpot LM, Ramar P, Roellinger DL, Barry BA, Sharma P, & Ebbert JO (2021). Changes in social relationships during an initial “stay-at-home” phase of the COVID-19 pandemic: A longitudinal survey study in the U.S. Social Science & Medicine, 274, 113779. 10.1016/j.socscimed.2021.113779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M, McManus S, Jessop C, John A, Hotopf M, Ford T, Hatch S, Wessely S, & Abel KM (2020). Says who? The significance of sampling in mental health surveys during COVID-19. The Lancet. Psychiatry, 7(7), 567–568. 10.1016/S2215-0366(20)30237-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati G, & Mancini AD (2021). The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychological Medicine, 51(2), 201–211. 10.1017/S0033291721000015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, Kaloupek DG, Schnurr PP, Kaiser AP, Leyva YE, & Tiet QQ (2016). The Primary Care PTSD Screen for DSM-5 (PC-PTSD-5): Development and evaluation within a veteran primary care sample. Journal of General Internal Medicine, 31(10), 1206–1211. 10.1007/s11606-016-3703-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riehm KE, Holingue C, Kalb LG, Bennett D, Kapteyn A, Jiang Q, Veldhuis CB, Johnson RM, Fallin MD, Kreuter F, Stuart EA, & Thrul J (2020). Associations between media exposure and mental distress among U.S. adults at the beginning of the COVID-19 pandemic. American Journal of Preventive Medicine, 59(5), 630–638. 10.1016/j.amepre.2020.06.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson E, Sutin AR, Daly M, & Jones A (2022). A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. Journal of Affective Disorders, 296, 567–576. 10.1016/j.jad.2021.09.098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogalski MA, Gowler CD, Shaw CL, Hufbauer RA, & Duffy MA (2017). Human drivers of ecological and evolutionary dynamics in emerging and disappearing infectious disease systems. Philosophical Transactions of the Royal Society of London: Series B, Biological Sciences, 372(1712), 20160043. 10.1098/rstb.2016.0043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers JP, Chesney E, Oliver D, Pollak TA, McGuire P, Fusar-Poli P, Zandi MS, Lewis G, & David AS (2020). Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: A systematic review and meta-analysis with comparison to the COVID-19 pandemic. The Lancet. Psychiatry, 7(7), 611–627. 10.1016/S2215-0366(20)30203-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell D, Peplau LA, & Cutrona CE (1980). The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology, 39(3), 472–480. 10.1037/0022-3514.39.3.472 [DOI] [PubMed] [Google Scholar]
- Shevlin M, McBride O, Murphy J, Miller JG, Hartman TK, Levita L, Mason L, Martinez AP, McKay R, Stocks TVA, Bennett KM, Hyland P, Karatzias T, & Bentall RP (2020). Anxiety, depression, traumatic stress and COVID-19-related anxiety in the U.K. general population during the COVID-19 pandemic. BJPsych Open, 6(6), e125. 10.1192/bjo.2020.109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver RC, Holman EA, & Garfin DR (2021). Coping with cascading collective traumas in the United States. Nature Human Behaviour, 5(1), 4–6. 10.1038/s41562-020-00981-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroebe M, & Schut H (2021). Bereavement in times of COVID-19: A review and theoretical framework. Omega: Journal of Death and Dying, 82(3), 500–522. 10.1177/0030222820966928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroebe M, Schut H, & Stroebe W (2007). Health outcomes of bereavement. The Lancet, 370(9603), 1960–1973. 10.1016/S0140-6736(07)61816-9 [DOI] [PubMed] [Google Scholar]
- Su Y, Rao W, Li M, Caron G, D’Arcy C, & Meng X (2022). Prevalence of loneliness and social isolation among older adults during the COVID-19 pandemic: A systematic review and meta-analysis. International Psychogeriatrics. Advance online publication. 10.1017/S1041610222000199 [DOI] [PubMed] [Google Scholar]
- Thompson RR, Jones NM, Holman EA, & Silver RC (2019). Media exposure to mass violence events can fuel a cycle of distress. Science Advances, 5(4), eaav3502. 10.1126/sciadv.aav3502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge JM, & Joiner TE (2020). U.S. Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depression and Anxiety, 37(10), 954–956. 10.1002/da.23077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2001). National Center for Health Statistics: National Health Interview Survey Questionnaire 2000. [Google Scholar]
- Voss G, Paiva AF, & Delerue Matos A (2021). A study of the association between the stringency of COVID-19 government measures and depression in older adults across Europe and Israel. International Journal of Environmental Research and Public Health, 18(15), 8017. 10.3390/ijerph18158017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, & McIntyre RS (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64. 10.1016/j.jad.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaninotto P, Iob E, Demakakos P, & Steptoe A (2022). Immediate and longer-term changes in the mental health and well-being of older adults in England during the COVID-19 pandemic. JAMA Psychiatry, 79(2), 151–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zisook S, Chentsova-Dutton Y, & Shuchter SR (1998). PTSD following bereavement. Annals of Clinical Psychiatry, 10(4), 157–163. 10.1023/a:1022342028750 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.