INTRODUCTION
The coronavirus disease 2019 (COVID-19) pandemic is an unprecedented crisis that has affected healthcare systems worldwide. Starting as a pneumonia of unknown cause in late 2019 in Wuhan, China, it quickly swept through the world and was declared a pandemic by the World Health Organization on 11 March 2020. Although most healthcare institutions have protocols for disease outbreak and epidemic management, many were not prepared to handle a pandemic of such intensity and duration. This was evidenced by the rapid depletion and shortage of resources such as manpower, ventilators, intensive care facilities and personal protective equipment (PPE).[1] To reduce the extent of community transmission, numerous countries experienced lockdowns, allowing only essential services to continue. Orthopaedic departments have reported on measures taken to ensure business continuity and resource optimisation, including postponement of non-essential surgeries,[2] modification of perioperative protocols,[3] continuation of medical education and training via web-based platforms,[4] and a push towards telemedicine in ambulatory care.[5,6,7] For ambulatory clinics specifically, a reduction in non-essential visits is crucial to reduce patient crowding in waiting areas and hospital premises, and prevent patients from being exposed to COVID-19 while commuting to or from the hospital.
NEED FOR RAPID DEPLOYMENT OF A TELEMEDICINE SERVICE
The Department of Orthopaedic Surgery at Singapore General Hospital, Singapore, reviews approximately 126,000 outpatient clinic visits per year, almost exclusively via in-clinic consults. However, after community transmission of COVID-19 within Singapore was identified in early February 2020, steps were quickly taken to mitigate risks for patients and staff within our outpatient clinics.[8] Such measures included: (a) implementation of screening protocols for patients, PPE requirements and isolation protocols; (b) enforcement of social distancing measures for patients and staff; and (c) a reduction of outpatient visits with prioritisation of urgent cases over elective cases.[9] In view of the sudden change in patient management protocols, we proceeded with the rapid deployment of a telemedicine service to implement virtual follow-ups with patients who needed to continue with the management of their non-urgent or non-emergency musculoskeletal conditions.
The rapid deployment of a telemedicine system required certain considerations including patient triage protocols, implementation of technology, administrative protocols, patient safety factors and patient confidentiality factors. The main objective of this rapid deployment process was not to develop an ideal telemedicine system for the management of patients. Rather, it was to mobilise a system in the fastest possible time to achieve continued delivery of high-quality orthopaedic care to our patients while maintaining the appropriate safety nets to ensure patient safety and confidentiality. This article details our considerations before and during the rapid deployment of our orthopaedic telemedicine service that allowed for continued delivery of musculoskeletal care during the COVID-19 pandemic.
PATIENT TRIAGE
Patients were triaged based on department-created guidelines that classified their orthopaedic condition as essential or non-essential [Table 1]. Patients with essential orthopaedic conditions, including acute trauma, oncological, infective or debilitating spinal disease, mainly continued to be followed up closely via in-clinic visits. When deemed appropriate, some patients with longer-term follow-up for essential conditions, such as longer-term follow-up for fracture healing and operatively managed infections, were offered telemedicine consults. Patients deemed to have non-essential conditions either had their appointments postponed or were provided the option of continuing with their regular follow-up via telemedicine. These patients included those with chronic degenerative conditions such as knee osteoarthritis or lumbar spondylosis, limb deformities, and sports injuries such as tendinous, ligamentous and meniscal injuries. Such patients were strongly discouraged from turning up for in-clinic visits unless they had significant pain or disability. Other considerations included whether patients required radiographic or laboratory investigations or if they required wound care services (including removal of stitches or application of dressings).
Table 1.
Guidelines on the triage of essential and non-essential orthopaedic conditions.
| Essential conditions | Non-essential conditions (suitable for postponement/telemedicine consult) |
|---|---|
| Acute trauma (<3 months) requiring radiographic evaluation | Long-term follow up for previous fractures (>3 months) |
|
| |
| Acute infections | Healed wounds or resolved skin and soft tissue infections |
|
| |
| Malignant bone or soft tissue tumours Pathological/impending pathological fractures | Benign tumours on yearly surveillance Follow-up of benign histopathology results |
|
| |
| Osteoporosis requiring laboratory investigations or changes in treatment regimen | Stable osteoporosis on regular follow-up |
|
| |
| Progressive neurological deficits with disability (including weakness, numbness, myelopathy, claudication) | Stable or improving neurological symptoms Follow-up of benign cross-sectional imaging results |
|
| |
| Postoperative wound management, including removal of stitches or wound surveillance | Postoperative patients for long-term follow-up (e.g. yearly follow-up after total knee arthroplasty) |
| Any condition resulting in severe pain or disability | Conservatively managed conditions on routine follow-up |
TECHNOLOGICAL RESOURCES
Various videoconferencing software platforms have been described in the implementation of telemedicine.[10] In the United States, platforms compliant with the Health Insurance Portability and Accountability Act (HIPAA) such as American Well (Amwell, Boston, MA, USA), MDLink (Kingston, Jamaica), Polycom RealPresence (Plantronics, Santa Cruz, CA, USA) are commonly used. These systems can be integrated with electronic medical record (EMR) systems and are hosted on hospital servers. Patients usually connect to these secure hospital servers via a remote patient portal. However, our institution uses the Sunrise Clinical Manager (Allscripts Healthcare Solutions Inc, Chicago, IL, USA) as an EMR system, which does not natively support telemedicine integration. In the context of an urgent need for the development of a telemedicine service, implementation of such systems would have required several modifications at significant cost and lead time, and they were thus determined to be unsuitable for our requirements. Hence, alternative consumer-oriented platforms were considered, such as the widely used WhatsApp (Facebook, Menlo Park, CA, USA), Skype (Microsoft, Redmond, WA, USA) and Zoom (Zoom Video Communications, San Jose, CA, USA). We chose Zoom due to its increasing ubiquity in the backdrop of widespread adoption of ‘work from home’ arrangements resulting from the COVID-19 pandemic. The department purchased a monthly Zoom ‘Pro’ subscription and utilised it for all teleconsultations. Considerations for using Zoom were its low cost, strong reliability, use of enterprise-grade end-to-end Advanced Encryption Standard (AES) 256-bit encryption, recent improvements to security and high local penetration rate. Although the platform was non-HIPAA compliant, we took steps to ensure that patient data remains confidential, as discussed later in this article. While not available at the time of implementation, as of April 2020, Zoom offers a HIPAA-compliant version named ‘Zoom for Healthcare’.[11]
There were several considerations in our choice of equipment. Our institution adopted a policy of Internet separation on computers with access to the EMR system. While these measures reduce the risk of any possible data breach and ensure patient confidentiality, the use of Internet-based videoconferencing software was not possible on such computers. Hence, separate Internet-enabled laptops were obtained from our information technology (IT) department for this purpose. We also worked with the IT department to ensure that these laptops had sufficient computing power and audiovisual capabilities. The laptops were tested in the consultation room at times of varied clinic loads to ensure the reliability of the Internet connection and quality of the video consult. Up to two laptops were used per clinic session to ensure there was sufficient Internet bandwidth for videoconferencing use.
DEVELOPMENT OF TELEMEDICINE PROTOCOLS
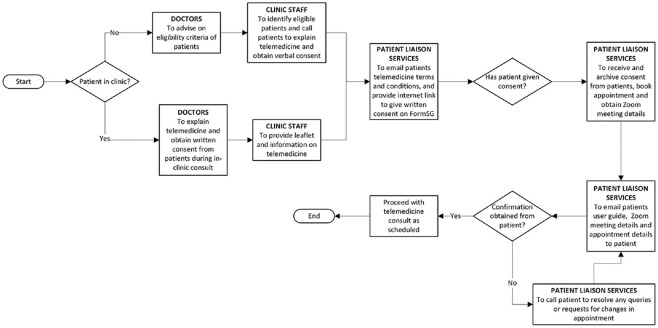
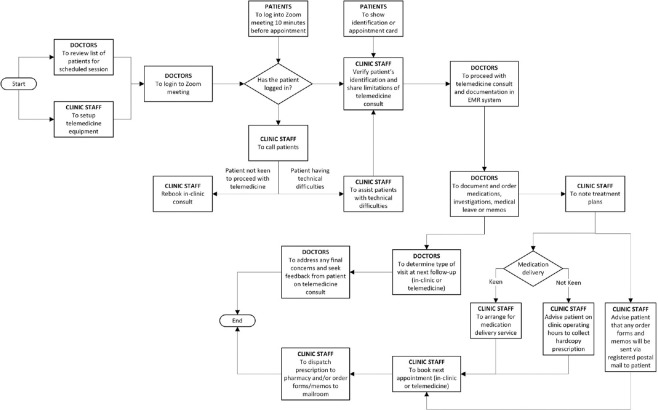
Administratively, our department collaborated with multiple stakeholders within our institution to develop a standardised workflow for the implementation of telemedicine services. These offices included the Office for Service Transformation (OST), Patient Liaison Service office, and Specialist Outpatient Clinic office. The protocols were separated into three main categories: pre-consult, consult and post-consult. A timeline on communication and messaging of patients was also developed to ensure that patients were aware that their appointments were virtual in nature (not physical) and understand how to access the virtual telemedicine consult. These protocols were developed to ensure proper coordination of the various offices, which would be involved at different timepoints during the entire process. Details on these protocols are found in Figures 1–3.
Figure 1.
Flowchart shows the pre-consultation protocol.
Figure 3.
Flowchart shows the video consultation protocol.
IMPLEMENTATION OF TELEMEDICINE SERVICES
Pre-consultation
Patients were recruited for the telemedicine service either during in-clinic visits or remotely via EMR review. Once these patients were identified, either the physician or an OST staff member would call the patient to explain the rationale of the telemedicine consult and obtain verbal consent. In line with privacy regulations, patients would then need to provide written consent via a secured online form, named ‘FormSG’, that was designed with sufficient security features to handle confidential governmental information in Singapore. Data transmitted was encrypted and stored within secured servers located in Singapore. Once patients provided written consent, emails were sent to them containing a user guide for the Zoom application, system requirements, Zoom session information including the meeting identification number and password, and appointment details. Reminders were also sent to the patient via text messaging [Figure 2].
Figure 2.
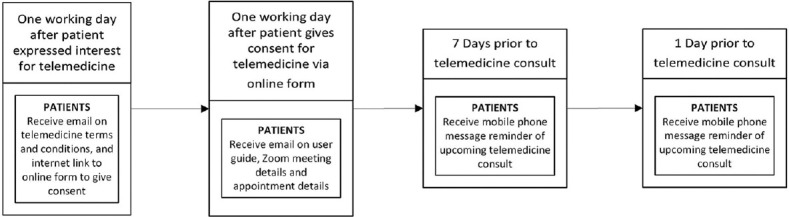
Flowchart shows the communication and messaging timeline for patients.
Consultation
Patients were instructed to log in to Zoom ten minutes before their scheduled appointment time. If they experienced difficulties, a clinic staff member on standby would assist them via telephone call. Once the identity of the patients had been confirmed with an identity card or appointment card, verbal consent would be obtained again prior to the commencement of the telemedicine consult. A typical consult would last for 5–10 minutes and comprise an assessment of their general well-being, progress related to their current orthopaedic condition and a simple physical examination. Due to the inherent limitations of telemedicine, clinical examination relied mainly on a visual inspection of clinical signs, such as gait or range of motion. On completion of the consult, a treatment plan would be formulated for each patient. In conjunction with patients, a clinical decision would be made on the type of consult (in-clinic or telemedicine) for the next visit.
A trained clinic staff member would be present before, during and after the telemedicine consult to render assistance to patients and doctors when technical issues arise. If technical issues resulted in an interruption of the telemedicine consult, the clinic staff member would assist the patient over the phone to re-establish the teleconsultation. If there was a prolonged delay, doctors might attend to other patients before returning to the patient to complete the consult. If a re-connection could not be established despite technical assistance, an in-clinic visit would be rescheduled for the affected patient. Charges were waived for all patients whose telemedicine consult was deemed inadequate or had to be rescheduled for any reason, be it technical or medical.
Post-consultation
After the consultation, arrangements were made to send order forms, medical certificates (MCs), medication, or memos to the patient. Anecdotally, demand for our medication delivery service had expanded rapidly since the outbreak of COVID-19, and this service has since been extended to patients who utilise telemedicine services. To further reduce contact, patients could make payment remotely via electronic means or telephone. MCs, order forms and memos would then be sent to them via registered mail to facilitate tracking for audit purposes. Attending surgeons would then document the telemedicine consult on the EMR platform, specifically noting the time, duration and meeting identification number for audit purposes.
ENSURING PATIENT SAFETY
Patient safety necessarily involves the accurate assessment of a patient’s condition and appropriate management. This is to ensure that no unnecessary harm is caused to patients and that optimal care is delivered. As specified in the Singapore Medical Council Ethical Code and Ethical Guidelines 2016, all physicians utilising telemedicine must endeavour to provide the same quality and standard of care as for in-person medical care.[12] By extension, telemedicine consults are subject to the same medicolegal standards as in-clinic visits. To this end, the guidelines state that “remote follow-up of patients is acceptable but there must be no evidence to suggest any clinically serious deterioration or new problems or complications, in which case such patients must be assessed in person”. In the context of our telemedicine service, all new cases to our department were first evaluated through an in-clinic consultation. Only follow-up patients with a known diagnosis and treatment plan were suitable to triage for telemedicine.
For follow-up via telemedicine, patients were selected based on strict criteria. Such patients included those who either had a stable musculoskeletal diagnosis, had no red flag symptoms (e.g. night pain, loss of weight or loss of appetite, recent trauma, fever), or had been deemed to have good progress postoperatively. In addition, they had to be able to competently utilise virtual conference platforms. Since the current processes and messaging were in the English language, only patients who were confident with using online platforms such as Zoom, had a stable Internet connection at home, and were either able to understand the English language or had a family member who could understand the English language (and was able to provide the necessary translation) were offered our telemedicine service. These factors were classified by our department as inclusion and exclusion criteria for the utilisation of telemedicine services. A summary of these criteria is found in Box 1. Attending orthopaedic surgeons in our department would make the final decision on whether patients were suitable for telemedicine. Examples of cases seen using the telemedicine service in our department are detailed in Table 2.
Box 1.
Inclusion and exclusion criteria for the use of telemedicine.
| Inclusion criteria |
|---|
| Presence of non-essential condition |
|
|
| Able to understand and use Zoom software |
|
|
| Presence of stable Internet connection at home |
|
|
| Exclusion criteria |
|
|
| Unable to understand English AND no family members who can understand English |
|
|
| Presence of red flag symptoms |
|
|
| Unable to determine if postoperative progress will be positive |
Table 2.
List of conditions reviewed via telemedicine.
| Conservatively managed conditions | Surgically managed conditions |
|---|---|
| Cervical spondylosis | Clavicle fracture s/p open reduction and internal fixation |
|
| |
| Rotator cuff tendinopathy | Rotator cuff tendinitis s/p hydrocortisone and lignocaine injection |
|
| |
| Frozen shoulder | Open reduction and internal fixation of proximal humerus fracture complicated by loosening of implants s/p revision open reduction and internal fixation |
|
| |
| Non-specific low back pain | Neck of femur fracture with background hip osteoarthritis s/p total hip replacement |
|
| |
| Prolapsed intervertebral disc | Infected total hip replacement s/p revision total hip replacement |
|
| |
| Degenerative disc disease | Foot infection complicated by septic shock s/p below-knee amputation |
|
| |
| Spinal stenosis | Knee meniscus tear s/p arthroscopic repair |
|
| |
| Hip osteoarthritis | Anterior cruciate ligament tear s/p arthroscopic repair |
|
| |
| Knee osteoarthritis | Knee osteoarthritis s/p total knee replacement |
|
| |
| Ankle osteoarthritis | Patella fracture s/p open reduction and internal fixation |
|
| |
| Ankle instability | Anterior talofibular ligament tear s/p ArthroBrostrom repair |
|
| |
| Achilles tendinitis | Achilles tendinitis with Haglund’s deformity s/p Haglund’s resection |
|
| |
| Plantar fasciitis | Infected foot wound s/p debridement |
|
| |
| Posterior tibial tendon dysfunction | Abscess s/p incision and drainage |
|
| |
| Hallux valgus | Hallux valgus s/p hallux valgus correction |
s/p: status post
Only fully accredited specialist orthopaedic surgeons were involved in telemedicine consults. This was to ensure that patients received appropriate specialist medical care from doctors who were sufficiently trained to do so and as it would be difficult for junior doctors to consult senior doctors if any challenges were encountered.
To ensure that patients received appropriate management, the protocols developed ensured that patients who were scheduled for follow-up with our telemedicine service received appropriate sick leave and medications. To facilitate the entire virtual consultation process, Singapore General Hospital assisted with expediting the development and approval of services, including next-day home delivery of medications and the provision of digital sick leave. Digital sick leave refers to patients receiving links to their MCs through our institution’s mobile application. They could print this MC out themselves or provide a screenshot of their digital MC to their employer. Billing was handled remotely, with invoices sent to patients’ households and modes of payment made available online or via telephone.
MAINTAINING PATIENT CONFIDENTIALITY
Telemedicine services inherently expose patients to cybersecurity risks and potential breach of confidentiality. To preserve the integrity of patient and service provider communications, the Ministry of Health, Singapore, and the Integrated Health Information Systems (IHIS) office developed the National Telemedicine Guidelines 2015 (NTG)[13] to ensure patient and personal data protection for telemedicine services throughout Singapore. These regulations are compliant with the Personal Data Protection Act 2012, which addressed the need for consent and protocols ensuring that the use and transmission of personal data over the telemedicine platform was for clinical uses only. The NTG, mirroring HIPAA requirements in the United States, specifies requirements pertaining to the reliability, quality, safety and security of telemedicine platforms. In conjunction with OST and IHIS, the department ensured that our processes adhered to these regulations. This included using a secure videoconferencing platform (i.e., Zoom) with AES 256-bit end-to-end encryption, procedures for the authentication of users and the enabling of audit trails for record-keeping purposes. These processes were in addition to existing institutional IT security policies, including ensuring that laptops used had appropriate malware software and were password-protected, that the EMR was password-protected, and that the entire system would not allow the sharing of patient data to anyone not involved in care of the patients.
LIMITATIONS
We identified some limitations during our deployment process. Firstly, surgeons reported that telemedicine consults were more time-consuming than in-person clinic visits. For example, 15–25 patients are usually seen during an in-person clinic session, in contrast to 5–10 telemedicine patients over a similar period. Based on feedback from the surgeons involved, this stemmed from unfamiliarity with the telemedicine platform and difficulties of coordinating with patients. We believe that as we continue to refine our telemedicine system, these initial problems can be ironed out, to fully reap the reported efficiencies of such a system. Secondly, adoption among surgeons and patients was low (less than 10% of all total visits). On this front, our clinics have actively reached out to surgeons and patients to improve awareness of this system, while we continue to improve our system processes. Thirdly, significant costs were incurred in the implementation of our system even though the number of patients seen was relatively small. Significant costs were incurred in procurement of technological resources (e.g., laptops, Zoom account), utilisation of clinic resources and time costs for doctors. While cost savings of between 12% and 72% have been reported by other studies,[14,15] these have yet to be appraised in our system. However, we are optimistic that our system will demonstrate its cost-effectiveness. Anecdotally, patients who utilised our telemedicine system were highly satisfied, citing time savings and convenience. From a health service perspective, direct costs are reduced in telemedicine, as clinic resources are freed up. Furthermore, by utilising technology, we can extend specialist orthopaedic care to patients who may not have the means or mobility to go to hospital for in-clinic visits. Nonetheless, a prospective study is currently under way to evaluate the direct and indirect cost savings as well as the safety and effectiveness of our telemedicine system.
CONCLUSION
While most telemedicine systems traditionally cite the benefits of improved access to healthcare for rural communities,[16] to our knowledge, our study is the first to report on the rapid deployment of an orthopaedic telemedicine service in an urbanised environment. The abovementioned factors were the pertinent factors prioritised by the department as it aimed to rapidly deploy its telemedicine service, made necessary by COVID-19-related stay home regulations. These factors were focused upon to ensure the business continuity of the department in the management of patients with non-essential musculoskeletal conditions. Other orthopaedic departments have reported the enhanced diagnostic utility of telemedicine services via the use of adjuncts such as a digital goniometer, applications that can measure the size and progress of wounds, and others that can analyse gait.[6] However, given the time and resource constraints at the start of the COVID-19 pandemic, this was not the focus of the telemedicine service we deployed. Nevertheless, as our department continues to develop its processes, these factors will be considered in augmenting our telemedicine service. Future work on this system will focus on evaluating the validity and effectiveness of a telemedicine service in the management of patients with a diverse range of musculoskeletal conditions. We are confident that such a system will demonstrate its proof of value and will continue to remain relevant in a post-COVID-19 world as we seek to provide high-quality, value-driven care for our patients.
REFERENCES
- 1.Ranney ML, Griffeth V, Jha AK. Critical supply shortages-The need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med. 2020;382:e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 2.DePhillipo NN, Larson CM, O’Neill OR, LaPrade RF. Guidelines for ambulatory surgery centers for the care of surgically necessary/time-sensitive orthopaedic cases during the COVID-19 pandemic. J Bone Joint Surg Am. 2020;102:933–6. doi: 10.2106/JBJS.20.00489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Service BC, Collins AP, Crespo A, Couto P, Gupta S, Avilucea F, et al. Medically necessary orthopaedic surgery during the COVID-19 pandemic: Safe surgical practices and a classification to guide treatment. J Bone Joint Surg Am. 2020;102:e76. doi: 10.2106/JBJS.20.00599. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz AM, Wilson JM, Boden SD, Moore TJ, Jr, Bradbury TL, Jr, Fletcher ND. Managing resident workforce and education during the COVID-19 pandemic. JB JS Open Access. 2020;5:e0045. doi: 10.2106/JBJS.OA.20.00045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382:1679–81. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 6.Tanaka MJ, Oh LS, Martin SD, Berkson EM. Telemedicine in the era of COVID-19: The virtual orthopaedic examination. J Bone Joint Surg Am. 2020;102:e57. doi: 10.2106/JBJS.20.00609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith AC, Thomas E, Snoswell CL, Haydon H, Mehrotra A, Clemensen J, et al. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19) J Telemed Telecare. 2020;26:309–13. doi: 10.1177/1357633X20916567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liow MHL, Tay KXK, Yeo NEM, Tay DKJ, Goh SK, Koh JSB, et al. Ensuring business continuity of musculoskeletal care during the COVID-19 pandemic. JB JS Open Access. 2020;5:e0050. doi: 10.2106/JBJS.OA.20.00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liow MHL, Tay KXK, Yeo NEM, Tay DKJ, Goh SK, Koh JSB, et al. From “business continuity” to “back to business” for orthopaedic surgeons during the COVID-19 pandemic. Bone Jt Open. 2020;1:222–8. doi: 10.1302/2633-1462.16.BJO-2020-0036.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Loeb AE, Rao SS, Ficke JR, Morris CD, Riley LH, 3rd, Levin AS. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28:e469–76. doi: 10.5435/JAAOS-D-20-00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zoom Video Communications I. Healthcare Plan. [Last accessed on 26 Aug 2022]. Available from: https://zoom.us/healthcare .
- 12.Singapore Medical Council. Ethical Code and Ethical Guidelines 2016 Edition. [Last accessed on 26 Aug 2020]. Available from: https://www.healthprofessionals.gov.sg/docs/librariesprovider2/guidelines/2016-smc-ethical-code-and- ethical-guidelines---(13sep16).pdf .
- 13.Ministry of Health, Singapore. National telemedicine guidelines for Singapore. MH 25: 22/1. MOHD Circular 06/2015. [Last accessed on 26 Aug 2020]. Available from: https://www.moh.gov.sg/docs/librariesprovider5/licensing-terms-and-conditions/national-telemedicine-guidelines-for-singapore-(dated-30-jan-2015).pdf .
- 14.Harno K, Arajärvi E, Paavola T, Carlson C, Viikinkoski P. Clinical effectiveness and cost analysis of patient referral by videoconferencing in orthopaedics. J Telemed Telecare. 2001;7:219–25. doi: 10.1258/1357633011936435. [DOI] [PubMed] [Google Scholar]
- 15.Aponte-Tinao LA, Farfalli GL, Albergo JI, Plazzotta F, Sommer J, Luna D, et al. Face to face appointment vs. telemedicine in first time appointment orthopedic oncology patients: A cost analysis. Stud Health Technol Inform. 2019;264:512–5. doi: 10.3233/SHTI190275. [DOI] [PubMed] [Google Scholar]
- 16.Lanham NS, Bockelman KJ, McCriskin BJ. Telemedicine and orthopaedic surgery: The COVID-19 pandemic and our new normal. JBJS Rev. 2020;8:e2000083. doi: 10.2106/JBJS.RVW.20.00083. [DOI] [PubMed] [Google Scholar]