Abstract
Caregiver burden is a well-recognised global phenomenon. The primary aim of this review is to summarise the prevalence of caregiver burden and its measurement scales, predictive factors and impact in Singapore. PubMed® and Scopus® databases were searched using the key terms ‘caregiver’, ‘burden’, ‘stress’, ‘strain’ and ‘Singapore’. A total of 206 papers were retrieved and 20 were included. This review showed that a significant proportion of caregivers in Singapore experience caregiver burden. Caregiving experiences and outcomes are affected by cultural, behavioural and socioeconomic factors. Being a Malay caregiver appears to be a protective factor for caregiver burden, whereas having negative coping strategies and care recipients with functional, cognitive and behavioural impairments are positive risk factors. As for outcomes, caregiver burden is associated with poorer self-rated health and reduced quality of life. Multiple instruments have been used to measure caregiver burden, and the Zarit Burden Interview is the most widely used.
Keywords: Caregiver burden, caregiver stress, quality of life, Singapore
INTRODUCTION
Caregivers play an important role as part of the healthcare team that co-manages patients with physicians, and informal caregiving accounts for much of home care.[1] For adults in America, the economic value of informal caregiving has greatly exceeded that of paid services.[2] The domains of caregiving are multidimensional, diverse and far-reaching, as caregivers often provide not only physical (e.g. basic and instrumental activities of daily living) and medical (e.g. nursing, medication administration and titration) care, but also psychological (e.g. emotional support), financial (e.g. paying for medical bills) and social (e.g. arranging or accompanying for appointments) assistance to patients under their care. With these demands, caregivers are often subject to enormous stressors and are potentially at risk for caregiver burden and declining physical and mental health.[3]
Zarit and colleagues defined caregiver burden as “the extent to which caregivers perceive that caregiving has had an adverse effect on their emotional, social, financial, physical and spiritual functioning.”[4] Caregiving burden has negative impact on the well-being of caregivers, including increased mortality,[5] poorer self-care,[6] social isolation,[7] depression,[8] anxiety[9] and financial stress.[10] A recent review suggested that caregiver burden can be the most compelling problem affecting caregivers of chronically ill elderly patients.[11] The burden of caregiving also has negative impact on the well-being of care recipients, such as abandonment and institutionalisation of the care recipient.[12,13,14] Previous research has characterised the various risk factors associated with caregiver burden, including female gender,[15] low education,[16] co-residence with care recipient, depression,[8] social isolation,[7] financial stress,[10] higher caregiving hours, lack of choice in being a caregiver,[17] smaller repertoire of coping strategies[18] and perceived patient distress.[11]
Many instruments for the measurement of caregiver well-being are available, and they cover various domains recommended for inclusion by the Family Caregiver Alliance.[19,20,21] A recent systematic review of tools for measurement of the impact of informal caregiving categorised them according to their degree of integration of dimensions and level of specificity to the caregiving process [Figure 1],[20] and caregiver burden was found to be the most specific and most integrated. Zarit Burden Interview (ZBI), the most widely employed tool to measure caregiver burden, has good test-retest reliability, internal consistency and construct validity.[20,21,22] ZBI is a self-reported caregiver measure that was originally developed by Zarit et al. as a 29-item questionnaire to assess the subjective burden experienced by informal caregivers in various aspects (physical, emotional, social and financial burden, and relationship with care recipient); it was subsequently revised to a shorter 22-item version.[21,23]
Figure 1.
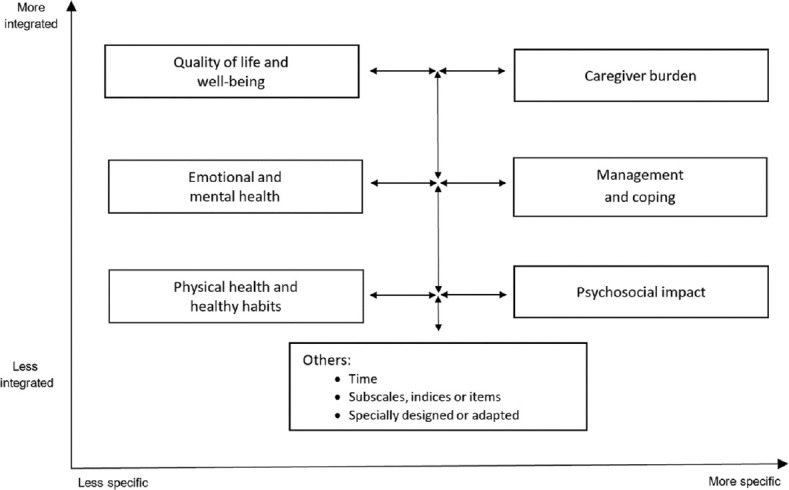
Diagram shows the measurement of impact of informal caregiving according to their degree of integration of dimensions and level of specificity to the caregiving process.
Singapore’s population is rapidly ageing, with an increasing proportion of elderly residents (12.4% in 2016 and expected to double in number by 2030) and a decreasing support ratio (5.4 residents aged 20–64 years per resident aged ≥65 years in 2016 vs. 13.5 in 1970).[24,25] With such changing demographics, informal home-based caregiving is expected to be increasingly demanding, and this may further exacerbate the issue of caregiver burdens. Thus, it is imperative to understand the prevalence, predictive factors and impact of caregiver burdens in Singapore.
Singapore is a unique developed city state in Southeast Asia with a multi-ethnic and multicultural population consisting of 74.3% Chinese, 13.4% Malay, 9.1% Indian and 3.2% other ethnicities as of 2016.[24] Current evidence suggests that caregiving experiences and outcomes are affected by culture, with different levels of burden reported among Asian caregivers and their Western counterparts.[26,27,28] In many Asian societies, including Singapore, traditional Confucian principles such as filial piety may have an impact on the caregiving experience.[29,30] The validity of instruments measuring caregiver burden developed in the West has also been questioned when they are applied to a different population and cultural setting.[31] Therefore, it is of great interest to review studies on caregiver burden conducted in a multi-ethnic, multicultural population in Singapore, and to compare these findings with those from international literature. This will enable recognition of the magnitude of problem within the local context and highlight the presence of critical knowledge gaps that may have health policy implications.
The primary aim of this review paper is to summarise research papers on caregiver burden in Singapore, in terms of its prevalence, measurement scales, predictive factors, and its impact on both caregiver and care recipient outcomes.
METHODS
Search strategies and inclusion criteria
We carried out a systematic literature search using PubMed® and Scopus® up to 30 January 2018. In our search strategy, we included these key terms: caregiver, burden, stress, strain and Singapore. Specifically, the search terms for PubMed were: ((((caregiver[MeSH Terms] OR caregiver*[Title/Abstract]) AND (stress*[Title/Abstract] OR burden*[Title/Abstract] OR strain[MeSH Terms] OR strain*[Title/Abstract]))) AND English[Language]) AND Singapore. The inclusion criteria were full text original studies published in English on the topic of caregiver burden in Singapore. Meta-analyses, case series, case reports, commentaries and reviews were excluded. Studies that were not in English, not conducted on human subjects, or entirely qualitative were also excluded.
Selection of studies and data collection
After duplicate articles were removed using EndNote™ (Clarivate Analytics, Philadelphia, PA, USA), two independent researchers (i.e. first and second authors, YXL and SY) screened the titles and abstracts of the retrieved studies and engaged in discussion whenever discrepancies arose. The full text studies were then independently read and assessed for eligibility by the two researchers. In the case of disagreement during the evaluation process, any discord was resolved by discussion with a third researcher (i.e. lead author, LLL). Once an article was deemed to be eligible, data from the eligible article was extracted independently by YXL and SY using a standardised information extraction format that included the authors, year of study, populations studied (including population size and characteristics), instrument for caregiver measures, prevalence, predictive factors and impact of caregiver burden. Risk of bias assessment (e.g. selection, attrition and detection bias) was performed by LLL by means of one of the SIGN checklists that is appropriate for the study design (https://www.sign.ac.uk/what-we-do/methodology/checklists/).
RESULTS
In total, 206 articles were retrieved from PubMed® and Scopus®. After removing 92 duplicates and 94 articles that did not fulfil the inclusion criteria, the final number of articles included for full text review was 20 [Figure 2]. The percentage agreement between the first and second authors was 90%. Table 1 summarises the key findings of the included articles.[32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51]
Figure 2.
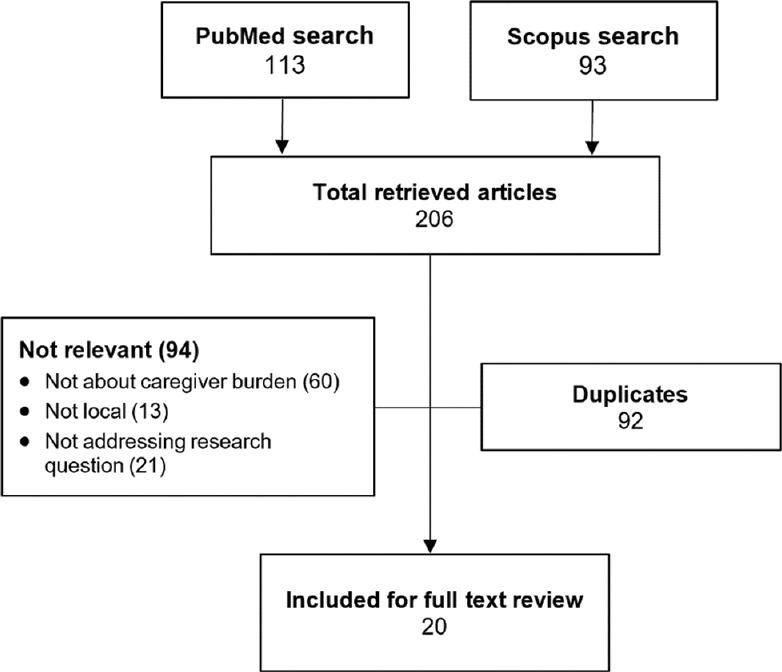
Flow chart shows the retrieval and inclusion of articles.
Table 1.
Summary of key findings of the included studies.
| Study, year | Study aim | Population | Caregiver measure | Study size | Findings | Remarks |
|---|---|---|---|---|---|---|
| Lim et al.,[32] 2018 | Evaluate and compare the level of caregiver burden in young-onset dementia (YOD) and late-onset dementia (LOD) | Caregivers of patients with YOD and those with LOD | ZBI (12-item) | 183 | Prevalence: 52.6% of caregivers of patients with YOD and 32.5% of caregivers of patients with LOD reported a high caregiver burden Predictive factors: 1. Family history of dementia 2. Behavioural symptoms, including disinhibited behavior, delusions and apathy Impact: Nil |
Study sample is relatively small |
| Win et al.,[33] 2017 | Explore the demographic characteristics and burden pattern among caregivers of dementia in the oldest-old | Caregivers of dementia | ZBI | 458 | Prevalence: Nil Predictive factors: Caregivers of dementia in the oldest-old associated with higher ZBI scores Impact: Nil |
Study sample of oldest-old care recipients is relatively small |
| Eom et al.,[34] 2017 | Understand effects of different patient-caregiver relationships and LTC service use on well-being of informal caregivers | Informal caregivers of patients discharged from tertiary hospital with referrals to LTC services | AMA Caregiver Self-assessment Questionnaire (stress); EuroQol-VAS (self-rated general health) | 781 | Prevalence: Nil Predictive factors: 1. Spousal and adult children caregivers showed worse self-rated general health and stress compared to non-immediate family caregivers, but difference did not reach statistical significance 2. Family caregivers who utilised home-based services presented poorer self-rated general health than those who did not use any services Impact: Nil |
No data on caregiver well-being before patient use of LTC services |
| Chua et al.,[35] 2016 | Understand the impact of caregiver burden on QoL, mental health and work capacity | Informal caregivers of advanced cancer patients | ZBI (12-item) | 16 | Prevalence: 50% of caregivers experienced high burden Predictive factors: Balancing multiple responsibilities, significant physical and non-physical caregiving demands, patients with debilitating symptoms, and poor social support Impact: Higher burden is associated with lower QoL, higher depression scores and greater work impairment |
• Small sample size (exploratory study) • Non-random sampling; only English-speaking and available caregivers of inpatients were recruited • Breakdown of frequency of predictors not provided |
| Rajasekaran et al.,[36] 2016 | Predict increased caregiver burden among elderly cancer patients using CGA-based risk factors | Family caregivers of elderly patients with cancer attending an outpatient oncology clinic | ZBI | 244 | Prevalence: 23% of caregivers had mild to severe burden. Predictive factors: Significant variables after multivariate analysis • ECOG 3-4, OR 4.47 (2.27-8.8) • Hb <12 g/dL, OR 2.38 (1.14-4.99) Impact: Nil |
• All outpatients (potential selection bias for patients who are less frail) • Large number of covariates analysed |
| Chang et al.,[37] 2016 | Identify the sociodemographic variables affecting the caregiving experience to relatives with mental illness, and the association between caregiving and psychological distress | Informal caregivers of outpatients attending a tertiary hospital psychiatric clinic | CRA | 344 | Prevalence: Nil Predictive factors: Significant variables after multivariate analysis • Age: those aged 35-49 yr had greater impact on health and schedule vs. those aged <35 yr • Education: those with lower education had greater impact on finances vs. those with university degree • Employment: the unemployed had greater impact on finances • I come: those earning <$2,000/mth perceived greater lack of family support • thnicity: the Chinese had lower self-esteem vs. Malays and Indians Impact: Higher domain scores of CRA were significantly associated with psychological distress even after controlling for sociodemographic factors |
• Certain patient characteristics that could impact caregiving and distress (e.g. age, neuropsychiatric symptoms) were not explored • Analysis by patient diagnosis was not conducted due to inadequate sample size in some groups |
| Vaingankar et al.,[38] 2016 | Describe the factors related to care burden of older adults with care needs, and their association with dementia | Informal caregivers of older adults with care needs | ZBI | 693 | Prevalence: 24.5% of caregivers met criterion for care burden Predictive factors Married caregivers (OR 2.4 vs. never married) • Caregivers with children (OR 0.4 vs. childless) • Younger care recipient (OR 2.5 vs. >84 yr) • Need care most of the time (OR 2.5 vs. no care needed) • BPSD (OR 3.5 vs. no BPSD) • Dementia (OR 2.52 vs. no dementia) • No association with caregiver’s age, gender, ethnicity, education, relationship with recipient, co-residence status and receipt of external help Impact: Nil |
• Population-based sampling using data from a national survey • road definition of informal caregivers, who may not have been the primary caregivers. • Did not evaluate role of paid helpers who took care of a sizeable proportion of participants |
| Griva et al.,[39] 2016 | Compare the psychosocial outcomes in patients undergoing assisted vs. self-care peritoneal dialysis | Caregivers of patients undergoing peritoneal dialysis | ZBI | 111 | Prevalence: Nil Predictive factors: Levels of perceived burden were equal and in the mild to moderate range. Impact: Nil |
|
| Tay et al.,[40] 2016 | Examine the associations of burden, coping and self-efficacy with QoL among family caregivers of PWD | Family caregivers of persons with mild-moderate dementia attending a tertiary hospital outpatient clinic | FBIS | 84 | Prevalence: Nil Predictive factors: Older caregivers had reduced burden scores but not better QoL Impact: Burden has significant negative correlation with QoL, particularly in the physical health and environment domains |
• Convenience sampling performed. Majority of caregivers was Chinese and may not be representative of other ethnicities. • Potential variables such as dementia stage, presence of BPSD, use of community services were not considered. |
| Khoo et al.,[41] 2013 | Determine the impact of neuropsychiatric symptoms (NPS) on caregiver distress in PWD | Family caregivers of PWD attending a tertiary hospital memory clinic | NPI-Q | 667 | Prevalence: Nil Predictive factors: NPS of various types significantly predicted caregiver distress, after controlling for type and severity of dementia, and patient’s age, race, gender, education and marital status. The top 3 NPS that predicted the most distress were: agitation, depression and irritability. Apathy caused the least distress. Impact: Nil |
• All were outpatients. • Potential variables, such as caregiver characteristics, were not controlled for. |
| Chan et al.,[42] 2013 | Estimate the health impact of caregiving to older adults requiring assistance | Informal caregivers of older adults requiring assistance in at least 1 ADL | SRH | 1,077 | Prevalence: Nil Predictive factors: 1. Odds for poorer SRH lower among: • Caregivers aged <75 yr • Malay 2. Odds for poorer SRH higher among: • Low educational level • Residence in 1-2 room public housing • Increased number of chronic diseases Impact: Caregivers, compared to non-caregivers, had higher odds of: • Poorer SRH, OR 2.45 (1.84-3.26) • Clinically significant depressive symptoms, OR 2.36 (1.44-3.86) • Outpatient visits, OR 1.27 (1.01-1.59) |
• Large number of covariates included in analysis • Large sample size from a national survey representing the general population and not only those attending healthcare or social services |
| Østbye et al.,[43] 2013 | Assess the impact of support from FDW in moderating caregiving outcomes in informal caregivers of older persons | Informal caregivers of older persons requiring assistance in at least 1 ADL | Modified CRA | 1,190 | Prevalence: Nil Predictive factors: FDW support is associated with better caregiving outcomes, by moderating the association of: • Physical impairment with caregiver’s disturbed schedule and poor health • Memory impairment with caregiver’s disturbed schedule, poor health and lack of finances • Behavioural impairment with caregiver’s lack of family support Impact: Nil |
• Large sample size from a national survey of community-dwelling elderly • Considered many sociodemographic variables of caregiver and recipient as covariates |
| Tan et al.,[44] 2012 | Examine the level of burden experienced by caregivers of persons with schizophrenia in the community | Caregivers of persons with schizophrenia attending outpatient mental health clinic | BAS | 150 | Prevalence: 31.3% of caregivers felt distressed, 24.7% experienced increased social burden and 26.7% had disturbed routines. Predictive factors: Nil Impact: Nil |
• All were outpatients • Convenience sampling |
| Vaingankar et al.,[45] 2012 | Examine the predictors of perceived burden among relatives of people with chronic physical or mental illness | Close relative of person with any chronic physical or mental illness | Family Burden Module | 2,458 | Prevalence: 30.9% perceived high burden resulting from their relative’s health condition. Predictive factors: 1. Multivariate analysis showed the following were more likely to perceive burden: • Women, OR 1.58 (1.17-2.14) • People who could open up to family or friends, OR 1.65 (1.1-2.48) • People with dysthymia, OR 4.91 (1.11-21.77) 2. Malays were less likely to perceive burden, OR 0.68 (0.52-0.89) Impact: Nil |
• Data collected from a national household survey with good response rate (75.9%) • Broad definition of ‘family caregiver’ used in study • Larger number of predictors analysed, but significant predictors only explained 10% of variance; authors attributed this to lack of information on other important factors |
| Lim et al.,[46] 2011 | Examine the factors associated with caregiving outcomes among caregivers of PWD | Family caregivers of PWD attending dementia clinic or recruited through email | ZBI | 107 | Prevalence: Nil Predictive factors: 1. Significant predictors of burden were: • Behavioural problems • Dementia severity • Use of behavioural disengagement and criticism as coping strategies 2. Use of behavioural disengagement and criticism consistently predicted burden above and beyond behavioural problems, even after statistically adjusting for caregiver characteristics 3. Sociodemographic characteristics of caregivers (age, sex, race, relationship with recipient, marital status, employment, education, caregiving duration, co-residency, help from FDW) had no associations with burden 4. High mean score of burden (34.2) associated with caregiving for PWD. Impact: Nil |
• Multiple comparisons were done without adjustment of significance levels (attributed to exploratory nature of study to capitalise on chance findings and avoid overlooking any significant effect) • Predictors of burden accounted for 48% of the variance in this study |
| Siddiqui et al.,[47] 2010 | Evaluate the prevalence of stress in caregivers of elders with osteoporotic hip fractures, and determine the contributory factors | Primary caregivers of patients admitted for osteoporotic hip fracture | CSI | 76 | Prevalence: Proportion of caregivers who were significantly stressed: • 1 wk from admission: 59.2% • 6 mth from admission: 50% Predictive factors: 1. Financial strain was the only significant cause after multivariate analysis, OR 5.04 (1.46-17.38) 2. Mental status and functional status of care recipients were not predictors of caregiver stress. Impact: Nil |
• Majority of patients were Chinese (86.8%) and had high Charlson Comorbidity Index score (63.2%) • 31.5% of the caregivers had maids |
| Mehta et al.,[48] 2005 | Examine the factors affecting stress among family caregivers of older persons | Principal family caregivers of homebound elderly patients | CSS (modified from CSI, locally validated) | 61 | Prevalence: Nil Predictive factors: 1. Increased caregiver stress was associated with ADL and instrumental ADL dependency of care recipient, and performance of physical tasks 2. Female caregivers had higher levels of stress, but difference was not statistically significant 3. Age of caregiver had an extremely low correlation with stress Impact: Nil |
• Purposive, non-random sampling • All patients were Chinese with low income and educational level, as data came from a voluntary welfare agency (Hua Mei Mobile Clinic) |
| Tan et al.,[49] 2005 | Assess the impact of neuropsychiatric symptoms on distress in family and professional caregivers | Caregivers of patients with dementia | NPI-D and NPI-NH | 85 | Prevalence: Nil Predictive factors: 1. Neuropsychiatric symptoms were positively correlated with caregiver distress 2. Family caregivers were significantly more distressed than professional caregivers over the delusion, agitation, depression and aberrant motor domains Impact: Nil |
This study assessed both family and professional caregivers |
| Siew et al.,[50] 2003 | Examine caregiver stress associated with caring for ADL-dependent elderly in the community | Caregivers of community dwelling ADL-dependent elderly | ZBI | 41 | Prevalence: 53.7% reported little or no burden, 39% reported mild to moderate burden, 7.3% reported moderate to severe burden, none reported severe burden. Predictive factors: Nil Impact: Nil |
Elderly in the study were not severely ADL-dependent |
| Heok et al.,[51] 1997 | Investigate the factors associated with emotional well-being of caregivers of PWD | Family caregivers of elderly Chinese patients with dementia presenting to memory clinic | GHQ-28 | 50 | Prevalence: 56% scored above the threshold Predictive factors: 1. GHQ scores correlated significantly with duration of care, depression and total behavioural score on multiple regression analysis 2. No significant association with gender, age and employment of caregivers; type and severity of dementia Impact: Nil |
Potential selection bias in using hospital patients |
ADL: activities of daily living, AMA: American Medical Association, BAS: Burden Assessment Scale, BPSD: behavioural and psychological symptoms of dementia, CGA: Comprehensive Geriatric Assessment, CQOLC: Caregiver Quality of Life Index-Cancer, CRA: Caregiver Reaction Assessment, CSI: Caregiver Strain Index, CSS: Caregiver Stress Scale, ECOG: Eastern Cooperative Oncology Group, EuroQol-VAS: EuroQol-Visual Analog Scale, FBIS: Family Burden Interview Schedule, FDW: foreign domestic worker, GHQ: General Health Questionnaire, Hb: haemoglobin, LTC: long-term care, NPI-D: Neuropsychiatric Inventory Caregiver Distress Scale, NPI-NH: Neuropsychiatric Inventory Caregiver Nursing Home Version, NPI-Q: Neuropsychiatric Inventory Questionnaire, OR: odds ratio, PWD: person with dementia, QoL: quality of life, SRH: self-rated health, ZBI: Zarit Burden Interview
Studies on caregiver burden in Singapore focused mostly on caregivers of the elderly[36,38,42,43,48,50] and persons with dementia.[40,41,46,51] Other studied populations included caregivers of cancer patients,[35,36] psychiatric patients,[37,44] people with chronic illness,[45] discharged hospital patients with long-term care referrals,[34] hip fracture patients[47] and patients on peritoneal dialysis.[39]
Of the 20 studies, nine presented data on the prevalence of caregiver burden. The prevalence reported ranged from 23.0% to 59.2% in studies conducted in different study populations. For example, among caregivers of community-dwelling elderly, one study found that 24.5% of caregivers fulfilled the criterion for caregiver burden,[38] while another study found 39.0% with mild-moderate burden and 7.3% with moderate-severe burden among caregivers of elderly with dependence in their activities of daily living.[50] In patients with cancer, two studies found significant burden in 23% and 50% of caregivers of patients with cancer attending an outpatient oncology clinic and patients with advanced cancer, respectively.[35,36] A study based on national household survey data found that 30.9% of relatives of persons with chronic physical or mental illness were perceived to have high burden.[45]
In Singapore, the most widely used instrument to measure caregiver burden is ZBI, and it was used in seven out of the 20 studies.[32,33,35,36,39,46,50] Of these seven studies, three were conducted in caregivers of persons with dementia. The ZBI was also used for caregivers of cancer patients, elderly with care needs and patients on peritoneal dialysis. Most studies used the 22-item version of the ZBI.
Multiple studies reported the association between poorer functional status of care recipients[36,48] or higher care demands[35,38,51] and increased caregiver burden. In patients with cognitive impairment, there was increased caregiver burden in those with behavioural and psychological symptoms of dementia (BPSD) or behavioural issues.[38,41,46,51] The presence of dementia and dementia severity were also identified as risk factors for caregiver burden.[38,46]
Sociodemographic variables of caregivers showed mixed results in terms of their effects on caregiver burden. One study showed that being middle-aged was associated with worse outcomes compared to being younger than 35 years.[37] Another study reported that caregivers who were younger than 75 years performed better compared to older caregivers.[42] However, less burden was seen in older caregivers in another study.[40] In some studies, caregiver age was not found to be a significant predictor of caregiver burden.[38,46,48,51] Four studies did not find a significant association between caregiver burden and the gender of the caregiver.[21,38,46,48] Married caregivers and caregivers without children were correlated with increased burden in one study,[38] but this finding was not replicated in another study.[46] Some studies found an effect of ethnicity: Malay caregivers showed less burden and negative impact,[42,45] while Chinese caregivers had greater impairment on self-esteem compared to their Malay and Indian counterparts.[37] Not all studies, however, reported ethnicity as a significant factor.[38,46]
Socioeconomic factors also played a role. Caregivers who were unemployed or had lower income,[37] stayed in one- or two-room public housing,[42] or experienced financial strain[47] had worse outcomes. However, employment was not found to be a significant predictive factor in some studies.[46,51] Having the support of a foreign domestic worker was found to moderate the impact of caregiving for elderly requiring assistance in at least one activity of daily living and was associated with better caregiving outcomes.[43] This mitigating effect of external help was, however, not seen in all studies.[38,46] The coping strategies used by caregivers of persons with dementia also played a role; for instance, the use of behavioural disengagement or criticism as a coping strategy was linked to increased burden.[46]
Four of the included studies measured the associated outcomes of caregiver burden. Increased caregiver burden was associated with reduced quality of life and increased depressive symptoms.[35,40,42] It also disrupted caregivers’ work and schedules.[35,37] Two of these studies found that caregivers were more likely to have poorer self-rated health and more outpatient visits.[37,42]
DISCUSSION
Population studied and prevalence of caregiver burden
Studies on caregiver burden in Singapore have largely concentrated on those caring for the elderly or demented. Caregivers of patients with other medical conditions or demographic characteristics (e.g. paediatric patients with genetic disorders) are under-represented and would, therefore, be prime candidates for further research endeavours. This will likely give a more complete picture of caregiver burden in Singapore.
The prevalence of caregiver burden in the included studies was reported to be 23.0%–59.2%. This is similar to the prevalence reported by other studies outside Singapore that used similar measurement scales.[52,53,54,55] With Singapore’s ageing population and more elderly developing multiple and complex health conditions, the prevalence would be expected to increase even further.[25] Health policymakers may be better informed to allocate appropriate resources to develop integrated and targeted health intervention programmes in the community to address this pressing issue.
Measures of caregiver burden
ZBI is the most widely used among the included studies and has been validated in Singapore.[56] The use of the ZBI as a measure has certain advantages. Firstly, it has been extensively studied and validated in a wide variety of settings, with well-documented psychometric properties. Secondly, its wide use allows healthcare providers to standardise reporting of caregiver burden and easily compare results obtained across different studies. However, its use as a unidimensional measure to produce a summary score may overlook the uniqueness and rich data from the individual dimensions.[31]
One observation is that studies in Singapore have uniformly adopted the use of quantitative measures to evaluate caregiver burden. The advantages of quantitative measures are their value for statistical analysis, as well as the ease of adaptation for use in clinical settings due to their directness and practicality. However, it has been argued that caregivers may conceptualise burden in ways that differ from descriptions used in measures, leading to a potential failure of the instruments to capture the entire breadth of burden.[31] Future mixed method approaches may enhance the comprehensiveness of research on this topic.
Predictive factors
The predictive ability of sociodemographic factors has been mixed in this review, which is consistent with other international studies which found that caregiver outcomes may not directly correlate with caregiver sociodemographic factors.[23,57,58,59] For example, female caregivers were shown to be at higher risk in some studies,[60,61] but not in others.[62,63] Some studies showed Malay caregivers experienced less burden and negative impact,[42,45] whereas other studies reported ethnicity as not a significant factor.[38,46] The real-life difficulty in predicting caregiver burden based on sociodemographic factors was also reflected in one study done on a broad population, which used national household survey data with a large sample size and good response rate but only found a limited number of predictors.[45] Furthermore, these predictors only explained 10% of the variance observed, which the authors attributed to a lack of information on other significant factors related to burden. This suggests that there are likely to be hidden predictors and confounders that are beyond the usual variables captured, which warrants more explorative qualitative studies. Further studies may also explore the complex interplay of the role of culture, social values and sociodemographic factors. Coping strategies appeared to influence the perceived burden in Singapore caregivers.[46] This is consistent with other studies which reported that strategies focused on problem-solving may be more effective in reducing caregiver burden than strategies that are focused on emotions.[64,65] This is of potential value, as caregiver coping strategy is a modifiable variable that can be pre-empted and targeted in tailored health intervention programmes for them. A future research direction may be an interventional trial to assess the effectiveness of coping strategy programmes to reduce caregiver burden.
Pertaining to care recipient factors, caregiver burden increased with caregiving demands, physical dependency and duration of time spent on care.[35,36,38,48] Similar findings about the impact of physical dependency have also been shown in other studies.[66] In addition, behavioural and neuropsychiatric symptoms, as well as the presence and severity of dementia were found to increase caregiver burden.[38,41,46,51] This is also consistent with findings in the existing literature that behavioural disturbances are often the most prominent predictive factor of burden.[67,68]
Impact of caregiver burden
The included studies evaluated the negative impact of caregiver burden on caregivers. This is important, as caregivers can be forgotten in the doctor-patient relationship.[69,70,71] Engaging the caregivers and addressing their needs are crucial, as caregivers play an essential role in keeping patients well in the community.[64,68,72] Further research efforts may also focus on how other caregiving constructs, such as caregiver grief, can have a negative impact on adverse caregiver outcomes.[73,74] On the other hand, it is also imperative to evaluate the effect of caregiver burden on care recipients (patients); however, none of the included studies had done so. Given the measured prevalence of caregiver burden in Singapore, it would be of great concern if caregiver burden translates into worse clinical outcomes for patients and increased healthcare costs. Future research efforts may focus on whether caregiver burden is associated with worse patient outcomes such as mortality, quality of life and healthcare expenditure.
Strengths and limitations
This article is an attempt to review the existing medical literature on caregiver burden in Singapore – a developed, multiracial and multicultural city-state. Our findings highlight important challenges in studying this highly subjective issue with cultural sensitivity. This article further builds on the current literature on caregiver burden by providing unique experiences in a multicultural setting in Singapore, which can inform future studies that intend to examine caregiver burden in other settings with non-homogeneous cultural backgrounds. One limitation of this review is that the focus of studies done in Singapore may limit its generalisability. Secondly, the risk of bias was assessed by one author. The search strategy may be further optimised by including more comprehensive search terms (such as ‘carer’) and other databases such as PsychInfo and CINAHL. Furthermore, this review did not have a registered protocol prior to the commencement of the study, which is another of its limitation. Finally, the broad topic of this review may limit its applicability to specific patient populations.
CONCLUSION
There is a significant prevalence of caregiver burden in Singapore. The ZBI is the most commonly used tool to measure caregiver burden in Singapore. In particular, caregivers of people with functional, cognitive and behavioural impairments appear to be at increased risk of burden. In our local context, caregiver burden is associated with various adverse caregiver outcomes, such as reduced quality of life and increased depressive symptoms. Given the limited number of studies in Singapore, future research efforts may include: studies that focus on under-represented populations beyond the elderly with dementia; mixed method studies to uncover more predictive factors for caregiver burden, especially cultural and sociodemographic factors in the Malay population; and studies that examine the impact of caregiver burden on care recipients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Towle RM, Tan CG, Saptu K, Ong LJ, Yap MM, Kheng JH, et al. What do caregivers value and is there agreement in perception of met needs between nurses and caregivers?Singapore Med J. 2019;60:575–82. doi: 10.11622/smedj.2019040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Section for Enhancing Geriatric Understanding and Expertise Among Surgical and Medical Specialists (SEGUE), American Geriatrics Society. Retooling for an aging America: Building the healthcare workforce. A white paper regarding implementation of recommendation 4.2 of this Institute of Medicine Report of April 14, 2008, that “All licensure, certification and maintenance of certification for healthcare professionals should include demonstration of competence in care of older adults as a criterion.”. J Am Geriatr Soc. 2011;59:1537–9. doi: 10.1111/j.1532-5415.2011.03503.x. [DOI] [PubMed] [Google Scholar]
- 3.Chang HY, Chiou CJ, Chen NS. Impact of mental health and caregiver burden on family caregivers'physical health. Arch Gerontol Geriatr. 2010;50:267–71. doi: 10.1016/j.archger.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: A longitudinal study. Gerontologist. 1986;26:260–6. doi: 10.1093/geront/26.3.260. [DOI] [PubMed] [Google Scholar]
- 5.Schulz R, Beach SR. Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. JAMA. 1999;282:2215–9. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 6.Hoffman GJ, Lee J, Mendez-Luck CA. Health behaviors among Baby Boomer informal caregivers. Gerontologist. 2012;52:219–30. doi: 10.1093/geront/gns003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodakowski J, Skidmore ER, Rogers JC, Schulz R. Role of social support in predicting caregiver burden. Arch Phys Med Rehabil. 2012;93:2229–36. doi: 10.1016/j.apmr.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gallagher D, Rose J, Rivera P, Lovett S, Thompson LW. Prevalence of depression in family caregivers. Gerontologist. 1989;29:449–56. doi: 10.1093/geront/29.4.449. [DOI] [PubMed] [Google Scholar]
- 9.Cameron JI, Franche RL, Cheung AM, Stewart DE. Lifestyle interference and emotional distress in family caregivers of advanced cancer patients. Cancer. 2002;94:521–7. doi: 10.1002/cncr.10212. [DOI] [PubMed] [Google Scholar]
- 10.Salmon JR, Kwak J, Acquaviva KD, Brandt K, Egan KA. Transformative aspects of caregiving at life's end. J Pain Symptom Manage. 2005;29:121–9. doi: 10.1016/j.jpainsymman.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 11.Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: A clinical review. JAMA. 2014;311:1052–60. doi: 10.1001/jama.2014.304. [DOI] [PubMed] [Google Scholar]
- 12.Logsdon RG, Gibbons LE, McCurry SM, Teri L. Quality of life in Alzheimer's disease: Patient and caregiver reports. J Ment Health Aging. 1999;5:21–32. [Google Scholar]
- 13.Siegel K, Raveis VH, Houts P, Mor V. Caregiver burden and unmet patient needs. Cancer. 1991;68:1131–40. doi: 10.1002/1097-0142(19910901)68:5<1131::aid-cncr2820680541>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 14.Yaffe K, Fox P, Newcomer R, Sands L, Lindquist K, Dane K, et al. Patient and caregiver characteristics and nursing home placement in patients with dementia. JAMA. 2002;287:2090–7. doi: 10.1001/jama.287.16.2090. [DOI] [PubMed] [Google Scholar]
- 15.Gallicchio L, Siddiqi N, Langenberg P, Baumgarten M. Gender differences in burden and depression among informal caregivers of demented elders in the community. Int J Geriatr Psychiatry. 2002;17:154–63. doi: 10.1002/gps.538. [DOI] [PubMed] [Google Scholar]
- 16.Vincent C, Desrosiers J, Landreville P, Demers L BRAD group. Burden of caregivers of people with stroke: Evolution and predictors. Cerebrovasc Dis. 2009;27:456–64. doi: 10.1159/000210092. [DOI] [PubMed] [Google Scholar]
- 17.Schulz R, Beach SR, Cook TB, Martire LM, Tomlinson JM, Monin JK. Predictors and consequences of perceived lack of choice in becoming an informal caregiver. Aging Ment Health. 2012;16:712–21. doi: 10.1080/13607863.2011.651439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim H, Chang M, Rose K, Kim S. Predictors of caregiver burden in caregivers of individuals with dementia. J Adv Nurs. 2012;68:846–55. doi: 10.1111/j.1365-2648.2011.05787.x. [DOI] [PubMed] [Google Scholar]
- 19.Family Caregiver Alliance. Selected Caregiver Assessment Measures: A Resource Inventory for Practitioners. 2nd ed. 2012. Dec, [Last accessed on 23 Jan 2018]. Available from: https://www.carealliance.ie/userfiles/file/SelCGAssmtMeas_ResInv_FINAL_12_10_12.pdf .
- 20.Mosquera I, Vergara I, Larrañaga I, Machón M, del Río M, Calderón C. Measuring the impact of informal elderly caregiving: A systematic review of tools. Qual Life Res. 2016;25:1059–92. doi: 10.1007/s11136-015-1159-4. [DOI] [PubMed] [Google Scholar]
- 21.Van Durme T, Macq J, Jeanmart C, Gobert M. Tools for measuring the impact of informal caregiving of the elderly: A literature review. Int J Nurs Stud. 2012;49:490–504. doi: 10.1016/j.ijnurstu.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 22.Whalen KJ, Buchholz SW. The reliability, validity and feasibility of tools used to screen for caregiver burden: A systematic review. JBI Libr Syst Rev. 2009;7:1373–430. doi: 10.11124/01938924-200907320-00001. [DOI] [PubMed] [Google Scholar]
- 23.Zarit SH, Reever KE, Bach-Peterson J. Relatives of the impaired elderly: Correlates of feelings of burden. Gerontologist. 1980;20:649–55. doi: 10.1093/geront/20.6.649. [DOI] [PubMed] [Google Scholar]
- 24.Department of Statistics, Singapore. Population trends. [Last accessed on 23 Jan 2018]. Available from: https://www.singstat.gov.sg/find-data/search-by-theme/population/population-and-population-structure/visualising-data/population-trends .
- 25.Speech by Mr Gan Kim Yong, Minister for Health, at the SG50 Scientific Conference on Ageing, on 19 March 2015. In: Ministry of Health, Singapore. [Last accessed on 23 Jan 2018]. Available from: https://www.moh.gov.sg/news-highlights/details/speech-by-mr-gan-kim-yong-minister-for-health-at-the-sg50-scientific-conference-on-ageing-on-19-march-2015 .
- 26.Dilworth-Anderson P, Williams IC, Gibson BE. Issues of race, ethnicity, and culture in caregiving research: A 20-year review (1980-2000) Gerontologist. 2002;42:237–72. doi: 10.1093/geront/42.2.237. [DOI] [PubMed] [Google Scholar]
- 27.Patterson TL, Semple SJ, Shaw WS, Yu E, He Y, Zhang MY, et al. The cultural context of caregiving: A comparison of Alzheimer's caregivers in Shanghai, China and San Diego, California. Psychol Med. 1998;28:1071–84. doi: 10.1017/s0033291798007053. [DOI] [PubMed] [Google Scholar]
- 28.Lai DW. Cultural predictors of caregiving burden of Chinese-Canadian family caregivers. Can J Aging. 2007;26(Suppl 1):133–47. doi: 10.3138/cja.26.suppl_1.133. [DOI] [PubMed] [Google Scholar]
- 29.Ng HY, Griva K, Lim HA, Tan JY, Mahendran R. The burden of filial piety: A qualitative study on caregiving motivations amongst family caregivers of patients with cancer in Singapore. Psychol Health. 2016;31:1293–310. doi: 10.1080/08870446.2016.1204450. [DOI] [PubMed] [Google Scholar]
- 30.Tuomola J, Soon J, Fisher P, Yap P. Lived experience of caregivers of persons with dementia and the impact on their sense of self: A qualitative study in Singapore. J Cross Cult Gerontol. 2016;31:157–72. doi: 10.1007/s10823-016-9287-z. [DOI] [PubMed] [Google Scholar]
- 31.Bastawrous M. Caregiver burden--A critical discussion. Int J Nurs Stud. 2013;50:431–41. doi: 10.1016/j.ijnurstu.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 32.Lim L, Zhang A, Lim L, Choong TM, Silva E, Ng A, et al. High caregiver burden in young onset dementia: What factors need attention? J Alzheimers Dis. 2018;61:537–43. doi: 10.3233/JAD-170409. [DOI] [PubMed] [Google Scholar]
- 33.Win KK, Chong MS, Ali N, Chan M, Lim WS. Burden among family caregivers of dementia in the oldest-old: An exploratory study. Front Med (Lausanne) 2017;4:205. doi: 10.3389/fmed.2017.00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eom K, Penkunas MJ, Chan AWM. Effect of caregiving relationship and formal long-term care service use on caregiver well-being. Geriatr Gerontol Int. 2017;17:1714–21. doi: 10.1111/ggi.12958. [DOI] [PubMed] [Google Scholar]
- 35.Chua CK, Wu JT, Wong YY, Qu L, Tan YY, Neo PS, et al. Caregiving and its resulting effects--the care study to evaluate the effects of caregiving on caregivers of patients with advanced cancer in Singapore. Cancers (Basel) 2016;8:105. doi: 10.3390/cancers8110105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rajasekaran T, Tan T, Ong WS, Koo KN, Chan L, Poon D, et al. Comprehensive Geriatric Assessment (CGA) based risk factors for increased caregiver burden among elderly Asian patients with cancer. J Geriatr Oncol. 2016;7:211–8. doi: 10.1016/j.jgo.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 37.Chang S, Zhang Y, Jeyagurunathan A, Lau YW, Sagayadevan V, Chong SA, et al. Providing care to relatives with mental illness: Reactions and distress among primary informal caregivers. BMC Psychiatry. 2016;16:80. doi: 10.1186/s12888-016-0786-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vaingankar JA, Chong SA, Abdin E, Picco L, Jeyagurunathan A, Zhang Y, et al. Care participation and burden among informal caregivers of older adults with care needs and associations with dementia. Int Psychogeriatr. 2016;28:221–31. doi: 10.1017/S104161021500160X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Griva K, Goh CS, Kang WCA, Yu ZL, Chan MC, Wu SY, et al. Quality of life and emotional distress in patients and burden in caregivers: A comparison between assisted peritoneal dialysis and self-care peritoneal dialysis. Qual Life Res. 2016;25:373–84. doi: 10.1007/s11136-015-1074-8. [DOI] [PubMed] [Google Scholar]
- 40.Tay KC, Seow CC, Xiao C, Lee HM, Chiu HF, Chan SW. Structured interviews examining the burden, coping, self-efficacy, and quality of life among family caregivers of persons with dementia in Singapore. Dementia (London) 2016;15:204–20. doi: 10.1177/1471301214522047. [DOI] [PubMed] [Google Scholar]
- 41.Khoo SA, Chen TY, Ang YH, Yap P. The impact of neuropsychiatric symptoms on caregiver distress and quality of life in persons with dementia in an Asian tertiary hospital memory clinic. Int Psychogeriatr. 2013;25:1991–9. doi: 10.1017/S1041610213001518. [DOI] [PubMed] [Google Scholar]
- 42.Chan A, Malhotra C, Malhotra R, Rush AJ, Østbye T. Health impacts of caregiving for older adults with functional limitations: Results from the Singapore survey on informal caregiving. J Aging Health. 2013;25:998–1012. doi: 10.1177/0898264313494801. [DOI] [PubMed] [Google Scholar]
- 43.Østbye T, Malhotra R, Malhotra C, Arambepola C, Chan A. Does support from foreign domestic workers decrease the negative impact of informal caregiving?Results from Singapore survey on informal caregiving. J Gerontol B Psychol Sci Soc Sci. 2013;68:609–21. doi: 10.1093/geronb/gbt042. [DOI] [PubMed] [Google Scholar]
- 44.Tan SC, Yeoh AL, Choo IB, Huang AP, Ong SH, Ismail H, et al. Burden and coping strategies experienced by caregivers of persons with schizophrenia in the community. J Clin Nurs. 2012;21:2410–8. doi: 10.1111/j.1365-2702.2012.04174.x. [DOI] [PubMed] [Google Scholar]
- 45.Vaingankar JA, Subramaniam M, Abdin E, He VY, Chong SA. “How much can I take?” : Predictors of perceived burden for relatives of people with chronic illness. Ann Acad Med Singap. 2012;41:212–20. [PubMed] [Google Scholar]
- 46.Lim J, Griva K, Goh J, Chionh HL, Yap P. Coping strategies influence caregiver outcomes among Asian family caregivers of persons with dementia in Singapore. Alzheimer Dis Assoc Disord. 2011;25:34–41. doi: 10.1097/WAD.0b013e3181ec18ae. [DOI] [PubMed] [Google Scholar]
- 47.Siddiqui MQ, Sim L, Koh J, Fook-Chong S, Tan C, Howe TS. Stress levels amongst caregivers of patients with osteoporotic hip fractures-A prospective cohort study. Ann Acad Med Singap. 2010;39:38–42. [PubMed] [Google Scholar]
- 48.Mehta KK. Stress among family caregivers of older persons in Singapore. J Cross Cult Gerontol. 2005;20:319–34. doi: 10.1007/s10823-006-9009-z. [DOI] [PubMed] [Google Scholar]
- 49.Tan LL, Wong HB, Allen H. The impact of neuropsychiatric symptoms of dementia on distress in family and professional caregivers in Singapore. Int Psychogeriatr. 2005;17:253–63. doi: 10.1017/s1041610205001523. [DOI] [PubMed] [Google Scholar]
- 50.Siew CW, Ho HK, Cheong SK, Tan BY, Lim FS, Emmanuel SC. Caregiver stress in activities of daily living-dependent elderly aged more than 65 years. Ann Acad Med Singap. 2003;32(5 Suppl):S69–71. [PubMed] [Google Scholar]
- 51.Heok KE, Li TS. Stress of caregivers of dementia patients in the Singapore Chinese family. Int J Geriatr Psychiatry. 1997;12:466–9. [PubMed] [Google Scholar]
- 52.Brodaty H, Woodward M, Boundy K, Ames D, Balshaw R PRIME Study Group. Prevalence and predictors of burden in caregivers of people with dementia. Am J Geriatr Psychiatry. 2014;22:756–65. doi: 10.1016/j.jagp.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 53.Ilse IB, Feys H, de Wit L, Putman K, de Weerdt W. Stroke caregivers'strain: Prevalence and determinants in the first six months after stroke. Disabil Rehabil. 2008;30:523–30. doi: 10.1080/09638280701355645. [DOI] [PubMed] [Google Scholar]
- 54.Tooth L, McKenna K, Barnett A, Prescott C, Murphy S. Caregiver burden, time spent caring and health status in the first 12 months following stroke. Brain Inj. 2005;19:963–74. doi: 10.1080/02699050500110785. [DOI] [PubMed] [Google Scholar]
- 55.Limpawattana P, Theeranut A, Chindaprasirt J, Sawanyawisuth K, Pimporm J. Caregivers burden of older adults with chronic illnesses in the community: A cross-sectional study. J Community Health. 2013;38:40–5. doi: 10.1007/s10900-012-9576-6. [DOI] [PubMed] [Google Scholar]
- 56.Seng BK, Luo N, Ng WY, Lim J, Chionh HL, Goh J, et al. Validity and reliability of the Zarit Burden Interview in assessing caregiving burden. Ann Acad Med Singap. 2010;39:758–63. [PubMed] [Google Scholar]
- 57.Deeken JF, Taylor KL, Mangan P, Yabroff KR, Ingham JM. Care for the caregivers: A review of self-report instruments developed to measure the burden, needs, and quality of life of informal caregivers. J Pain Symptom Manage. 2003;26:922–53. doi: 10.1016/s0885-3924(03)00327-0. [DOI] [PubMed] [Google Scholar]
- 58.Elmståhl S, Malmberg B, Annerstedt L. Caregiver's burden of patients 3 years after stroke assessed by a novel caregiver burden scale. Arch Phys Med Rehabil. 1996;77:177–82. doi: 10.1016/s0003-9993(96)90164-1. [DOI] [PubMed] [Google Scholar]
- 59.Robinson BC. Validation of a caregiver strain index. J Gerontol. 1983;38:344–8. doi: 10.1093/geronj/38.3.344. [DOI] [PubMed] [Google Scholar]
- 60.Zahid MA, Ohaeri JU. Relationship of family caregiver burden with quality of care and psychopathology in a sample of Arab subjects with schizophrenia. BMC Psychiatry. 2010;10:71. doi: 10.1186/1471-244X-10-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chien LY, Chu H, Guo JL, Liao YM, Chang LI, Chen CH, et al. Caregiver support groups in patients with dementia: A meta-analysis. Int J Geriatr Psychiatry. 2011;26:1089–98. doi: 10.1002/gps.2660. [DOI] [PubMed] [Google Scholar]
- 62.Annerstedt L, Elmståhl S, Ingvad B, Samuelsson SM. Family caregiving in dementia--an analysis of the caregiver's burden and the “breaking-point” when home care becomes inadequate. Scand J Public Health. 2000;28:23–31. doi: 10.1177/140349480002800106. [DOI] [PubMed] [Google Scholar]
- 63.Chumbler NR, Grimm JW, Cody M, Beck C. Gender, kinship and caregiver burden: The case of community-dwelling memory impaired seniors. Int J Geriatr Psychiatry. 2003;18:722–32. doi: 10.1002/gps.912. [DOI] [PubMed] [Google Scholar]
- 64.Carretero S, Garcés J, Ródenas F, Sanjosé V. The informal caregiver's burden of dependent people: Theory and empirical review. Arch Gerontol Geriatr. 2009;49:74–9. doi: 10.1016/j.archger.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 65.Pearlin LI, Skaff MM. Gatz M, editor. Stressors and adaptation in late life. Emerging Issues in Mental Health and Aging. American Psychiatric Association. 1995:97–123. [Google Scholar]
- 66.Logsdon RG, Teri L, McCurry SM, Gibbons LE, Kukull WA, Larson EB. Wandering: A significant problem among community-residing individuals with Alzheimer's disease. J Gerontol B Psychol Sci Soc Sci. 1998;53:P294–9. doi: 10.1093/geronb/53b.5.p294. [DOI] [PubMed] [Google Scholar]
- 67.Etters L, Goodall D, Harrison BE. Caregiver burden among dementia patient caregivers: A review of the literature. J Am Acad Nurse Pract. 2008;20:423–8. doi: 10.1111/j.1745-7599.2008.00342.x. [DOI] [PubMed] [Google Scholar]
- 68.Dunkin JJ, Anderson-Hanley C. Dementia caregiver burden: A review of the literature and guidelines for assessment and intervention. Neurology. 1998;51(Suppl 1):S53–60. doi: 10.1212/wnl.51.1_suppl_1.s53. discussion S65-7. [DOI] [PubMed] [Google Scholar]
- 69.Silliman RA. Caring for the frail older patient: The doctor-patient-family caregiver relationship. J Gen Intern Med. 1989;4:237–41. doi: 10.1007/BF02599531. [DOI] [PubMed] [Google Scholar]
- 70.Schoenmakers B, Buntinx F, Delepeleire J. What is the role of the general practitioner towards the family caregiver of a community-dwelling demented relative?A systematic literature review. Scand J Prim Health Care. 2009;27:31–40. doi: 10.1080/02813430802588907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Emlet CA. Assessing the informal caregiver: Team member or hidden patient?Home Care Provid. 1996;1:255–62. doi: 10.1016/s1084-628x(96)90046-5. 275. [DOI] [PubMed] [Google Scholar]
- 72.Levine C, Halper D, Peist A, Gould DA. Bridging troubled waters: Family caregivers, transitions, and long-term care. Health Aff (Millwood) 2010;29:116–24. doi: 10.1377/hlthaff.2009.0520. [DOI] [PubMed] [Google Scholar]
- 73.Liew TM, Tai BC, Yap P, Koh GC. Contrasting the risk factors of grief and burden in caregivers of persons with dementia: Multivariate analysis. Int J Geriatr Psychiatry. 2019;34:258–64. doi: 10.1002/gps.5014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Liew TM, Tai BC, Yap P, Koh GC. Comparing the effects of grief and burden on caregiver depression in dementia caregiving: A longitudinal path analysis over 2.5 years. J Am Med Dir Assoc. 2019;20:977–83. doi: 10.1016/j.jamda.2018.11.016. e4. [DOI] [PubMed] [Google Scholar]


