Abstract
Objective:
Food allergy (FA) affects approximately 8% of children in the United States. Management comprises both preventing and treating allergic reactions, which poses unique challenges in the inner-city school setting. In this article, we review the epidemiology of FA in school-aged children and management challenges and opportunities specific to the inner-city population.
Data sources:
A literature search of the PubMed database was performed to identify published literature on FA epidemiology, FA management, school policies, disparities, inner-city, race, ethnicity, and socioeconomic status.
Study Selections:
Relevant articles on FA management best practices and challenges in schools, with a particular emphasis on inner-city schools and populations and socioeconomic, racial, and ethnic disparities, were reviewed in detail.
Results:
Disparities in FA prevalence, management, and treatment exist. Additional research is needed to better characterize these disparities and elucidate the mechanisms leading to them. There is a lack of evidence-based interventions for the prevention and treatment of food allergic reactions in schools and specifically in inner-city schools, in which a greater proportion of students may rely on school food.
Conclusion:
There are opportunities for partnership among health care providers, schools, and communities to address unmet needs in FA management and disparities in the inner-city school setting.
Introduction
Food allergy (FA) affects nearly 8% of children in the United States and its prevalence is increasing.1 Management relies on avoiding allergens and treating severe reactions with epinephrine. Allergen avoidance in school-aged children poses unique challenges. Children spend most of their time in school and during those hours are highly reliant on the school community for safety. FA is the most common cause of anaphylaxis in schools,2 and 16% to 18% of children with FA experience reactions in school.3 Epinephrine administration rates in school have increased, with a 23% increase per year for reactions to peanuts and tree nuts between 2006 and 2011 in Massachusetts.4 Children with FA also experience increased psychosocial burden and are at increased risk of being bullied in school.5,6
Managing FA in schools is complex, controversial, and variable, and evidence-based guidance is minimal.5 Effective strategies must address both safety and psychosocial considerations. Managing FA in inner-city schools has distinct challenges. Inner-city schools are typically found in older, densely-populated, urban neighborhoods. There is a higher proportion of racial and ethnic minority students, and many students are from families with low income or limited English proficiency. Many inner-city schools struggle with limited funding and resources, increased student-teacher ratios, lack of access to full-time school nurses, and bureaucratic challenges. Whereas there is a critical need to identify and implement evidence-based FA policies that can be easily adopted by all schools, it is important to have a flexible and tailored approach on the basis of understanding the unique needs and challenges of different school settings.
In this article, we review the literature on the epidemiology, risk factors, and comorbidities of FA in inner-city schoolchildren. In many cases, publications on inner-city populations are lacking, so discussion is extrapolated from studies on racial and ethnic minority and socioeconomically disadvantaged children. We also evaluate FA reactions and management in schools and discuss unmet needs and opportunities for partnership among health care providers, schools, and communities to address FA management and disparities in the inner-city population.
Epidemiology of Food Allergy in School-Aged Children
There are disparities in FA prevalence by race, ethnicity, and socioeconomic status (SES).7 In a US Medicaid-enrolled population, FA prevalence was higher among Asian, Black, and Pacific Islander and lower in Hispanic and Native American vs White children.8 In a nationally representative sample of US households, the odds of having FA were highest among Black compared with White children, whereas the odds of having multiple vs a single FA were highest among Black and Asian compared with White children.1 The highest rate of increase in FA prevalence over recent decades was seen in Black children.9 It is unclear whether increased prevalence is because of increased sensitization or improved recognition and diagnosis.10,11
Racial and Ethnic Disparities in Specific Food Allergens
There are racial and ethnic differences in FA prevalence for specific foods (Table 1).12-15 The reasons for these differences are unclear and may be related to timing or type of food introduction, SES, environmental exposures, or barriers to health care. For example, higher cockroach exposure in inner cities may lead to increased sensitization and prevalence of shellfish and fish allergy in inner-city children through cross-reactive tropomyosins.16,17
Table 1.
Specific Food Allergens in US Children by Race and Ethnicity
| Reference | Study population | Race/ethnicity | Statistic | Reported prevalence and odds ratios by food allergen | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Peanuts | Tree nuts | Milk | Egg | Wheat | Soy | Sesame | Fish | Shellfish | Corn | ||||
| Mahdavinia et al,12 2017 | Children 0-17 y old with food allergies seen in allergy/immunology clinics in Chicago, Illinois and Cincinnati, Ohio | White | Prevalence (%) | 65.1 | 45.5 | 24.9 | 38.3 | 7.4 | 7.4 | — | 3.5 | 7.39 | 2.1 |
| Odds ratio | (ref) | (ref) | (ref) | (ref) | (ref) | (ref) | — | (ref) | (ref) | (ref) | |||
| Black | Prevalence (%) | 65.6 | 18.6 | 29.5 | 44.6 | 23.2 | 27.0 | — | 34.39 | 23.5 | 15.1 | ||
| Odds ratio | 1.12 | 0.31a | 0.98 | 1.27 | 2.95a | 3.43a | — | 11.66a | 3.34a | 6.6a | |||
| Hispanic | Prevalence (%) | 52.5 | 25.3 | 25.3 | 45.5 | 11.1 | 12.1 | — | 16.2 | 15.2 | 7.1 | ||
| Odds ratio | 0.65 | 0.49a | 0.82 | 1.19 | 1.31 | 1.40 | — | 4.82a | 2.26a | 3.28a | |||
| Mahdavinia et al,13 2021 | Children 0-12 y old with food allergies seen in allergy/immunology clinics in Chicago, Illinois, Cincinnati, Ohio, and Washington, District of Columbia | White | Prevalence (%) | 62.6 | 51.3 | 25.2 | 42.1 | 5.2 | 5.4 | 20.5 | 8.2 | 8.0 | — |
| Odds ratio | (ref) | (ref) | (ref) | (ref) | (ref) | (ref) | (ref) | (ref) | (ref) | — | |||
| Black | Prevalence (%) | 64.9 | 56.5 | 21.3 | 35.2 | 12.6 | 10.0 | 10.5 | 23.9 | 31.8 | — | ||
| Odds ratio | 0.87 | 1.27 | 0.81 | 0.81 | 2.10 | 0.97 | 0.52 | 2.54a | 3.11a | — | |||
| Coulson et al,14 2020 | Adolescents 11-16 y old whose mothers were recruited in Eastern Massachusetts during pregnancy | White | Odds ratio | (ref) | — | (ref) | (ref) | (ref) | — | — | — | — | — |
| Black | Odds ratio | 2.41a | — | 1.41 | 2.66 | 0.72 | — | — | — | — | — | ||
| Hispanic | Odds ratio | 1.44 | — | NA | NA | NA | — | — | — | — | — | ||
| Mixed race, Asian or Pacific Islander, American Indian or Alaskan Native, or other | Odds ratio | 4.14a | — | 1.52 | 1.35 | 2.29 | — | — | — | — | — | ||
| Wang et al,15 2020 | Children 0-17 y old from a nationally representative panel | White | Odds ratio | — | — | — | — | — | — | — | — | (ref) | — |
| Black | Odds ratio | — | — | — | — | — | — | — | — | 2.3a | — | ||
| Hispanic | Odds ratio | — | — | — | — | — | — | — | — | 1.4 | — | ||
| Asian | Odds ratio | — | — | — | — | — | — | — | — | 1.7 | — | ||
| Mixed race or other | Odds ratio | — | — | — | — | — | — | — | — | 0.9 | — | ||
Abbreviations: NA, not applicable; ref, reference interval.
NOTE. Findings from selected studies are detailed above. Selected studies were not conducted specifically in inner-city populations. White is the reference group for calculating odds ratios. “—” indicates statistic not evaluated in a given study.
Statistically significant differences in odds ratios.
Risk Factors for Food Allergy Prevalence and Severity
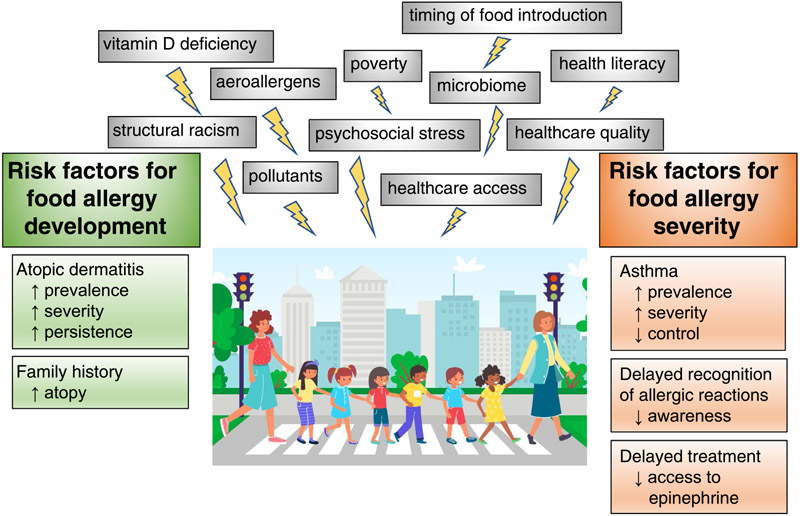
Children living in inner cities may have risk factors for increased FA prevalence and severity (Fig 1). Risk factors for FA are likely multifactorial and may be related to poverty, poor air quality and pollution, aeroallergen exposures, vitamin D deficiency, microbiome, poorquality housing, suboptimal patient or family education, psychosocial stress, and reduced health care access and quality resulting from structural and systemic racism.7,18,19
Figure 1.
Risk factors for food allergy in inner-city children. Risk factors for food allergy development and severity, and the possible interaction with social determinants of health and other social and environmental factors, are summarized.
Atopic Dermatitis
Atopic Dermatitis (AD) has been found in multiple studies to be a major risk factor for developing FA, with patients with severe AD at the highest risk.20 Living in an inner city is associated with increased odds of AD diagnosis.21 Racial and ethnic disparities exist in AD, with increased AD prevalence, severity, and persistence in Black and Hispanic compared with White children in the United States.19 Early-life sensitization to indoor allergens prevalent in inner cities, specifically mouse and cockroach, was associated with increased odds of AD in an inner-city birth cohort.22
Asthma
Asthma prevalence and severity are increased and control is decreased in inner-city and underserved populations.23 Fatal food anaphylaxis is associated with having an asthma diagnosis,24 and severe allergic reactions are more common in patients with uncontrolled asthma.25 Several groups have found high rates of food allergen sensitization, clinical FA, and multiple food triggers in inner-city children with asthma.26-28 A study of inner-city school children with asthma found high FA prevalence (24%), and those with FA had decreased asthma control.26
Vitamin D Deficiency
Vitamin D modulates immune responses and deficiency has been associated with atopic conditions including FA, anaphylaxis, asthma, AD, and allergic rhinitis. The primary source of vitamin D is skin synthesis after sun exposure. Higher concentrations of melanin in skin of color absorb solar ultraviolet B radiation, reducing skin vitamin D synthesis.29 Inner-city children have several risk factors for vitamin D deficiency, including darker skin color, and spending less time outdoors. These risk factors, mediated by vitamin D deficiency, may lead to increased FA prevalence and severity in inner-city children.
Food Allergy Management, Anaphylaxis, and Access to Quality Care
The major risk factor for fatal food anaphylaxis is delayed epinephrine administration. Unfortunately, there are disparities in FA management and access to quality care among minority and low-income children.
A retrospective study from an urban minority hospital-based pediatric clinic found that, whereas most (79.9%) patients with FA were prescribed epinephrine autoinjectors (EAIs), only 67% were referred to allergists and 45% were seen by allergists.27 Only 38.2% of patients had Emergency Action Plan (EAPs) documented in the medical record. Patients evaluated by allergists were more likely to be prescribed EAIs and have EAPs compared with those not seen by allergists. Rates of referral, EAI prescriptions, and EAP documentation did not differ by race.27 A study of children with FA from 2 urban tertiary care centers found that, whereas age at the first visit to an allergist did not differ by race, ethnicity, or insurance status, the duration of allergist follow-up was shorter in Black and Hispanic vs White children, and children insured through Medicaid vs private insurance.12 These factors could lead to underdiagnosis of FA and delayed recognition and treatment of allergic reactions in inner-city children. In the same cohort, there were higher rates of FA-related anaphylaxis and emergency department (ED) visits in Black and Hispanic vs White children. There was no difference in FA-related anaphylaxis and ED visits by insurance type (Medicaid vs private insurance).12 In another study, the rates of pediatric ED visits for food-induced anaphylaxis were highest among Black vs White children and children living in urban vs rural areas.30
It has been observed that fatal anaphylaxis may be more common in Black and South Asian patients, and also in cases in which there is a lack of urticaria during allergic reactions.24 A study of medical students found a disparity in the visual diagnosis of urticaria in skin of color vs light skin (57.5% vs 82.2% diagnosed correctly).31 Many US health care providers report inadequate training in skin conditions in patients of diverse skin colors, particularly among Black patients. This lack of training persists in didactics, textbooks, and peerreviewed literature, which often underrepresent images of patients with skin of color.32 This disparity in accurate recognition of urticaria, a common warning sign of allergic reactions, could lead to delayed diagnosis and treatment of anaphylaxis in patients with skin of color, possibly accounting for an increased risk of fatal reactions.
Strategies to Manage Food Allergies in Schools
School-based FA management requires the involvement of individuals across multiple levels within the school environment.33 The lack of evidence-based interventions to prevent and treat allergic reactions in schools,34 and variation in implementation across schools, may contribute to limited preparedness to treat anaphylaxis in schools and added psychosocial burden on families with FA.35,36 Guidelines for school-based FA management developed by the Centers for Disease Control and Prevention are voluntary in nature.34 Recent practice guidelines for FA management in schools offer recommendations, though some may be difficult to implement in underresourced settings, such as inner-city schools (Table 2).5
Table 2.
Summary of Recommendations for Managing Food Allergic Reactions in Schools
| Recommendation | Strength of recommendation |
Certainty of evidence |
Specific considerations for inner-city schools |
|---|---|---|---|
| Food allergy training, allergy action plans, and site-wide protocols | |||
| 1. Suggest that schools implement training for teachers and other personnel in the prevention, recognition, and treatment of food allergic reactions. | Conditional | Very low |
|
| 2. Suggest that schools require all parents of students with diagnosed food allergy to submit an up-to-date Emergency Action Plan. | Conditional | Very low |
|
| 3. Suggest that schools implement site-wide protocols for management of suspected food allergic reactions in individuals with no Emergency Action Plan on file. | Conditional | Very low |
|
| Epinephrine vs other treatments for allergic reactions | |||
| 4. Suggest that school personnel use epinephrine only when they suspect someone is experiencing anaphylaxis, rather than use epinephrine as the first universal treatment for all suspected allergic reactions. | Conditional | Very low |
|
| 5. Suggest that school personnel do not preemptively administer epinephrine in cases when no signs or symptoms of an allergic reaction have developed, even if a student has eaten a food to which they have a known allergy or history of anaphylaxis. | Conditional | Very low |
|
| Stocking unassigned epinephrine autoinjectors | |||
| 6. Suggest that schools stock unassigned epinephrine autoinjectors on site, instead of requiring students with allergy to submit personal autoinjectors to be stored on site. | Conditional | Very low |
|
| Site-wide food prohibitions and allergen-restricted zones | |||
| 7. Suggest that schools do not prohibit specific foods site-wide (eg, nut-free schools). | Conditional | Very low |
|
| 8. Suggest that schools do not establish allergen-restricted zones (eg, peanut-free classrooms, milk-free tables), except in limited special circumstances. | Conditional | Very low |
|
NOTE. Modified from practice guidelines developed by Waserman et al.5
Restricting Food Allergens in Schools
One of the most common preventive strategies in schools is restricting allergens, though there is limited evidence for effectiveness in preventing allergic reactions. Policies range from banning specific allergens brought in from home or sold in the cafeteria, to restricting where allergens can be eaten (eg, peanut-free tables or classrooms). Specially designated areas are one of the most common policies.4,37
In a study of Massachusetts schools, those with peanut-free tables had lower rates of epinephrine administration vs schools without peanut-free tables; no other food allergen restriction policy was effective at reducing epinephrine administration rates.4 Schools with more restrictive policies had higher proportions of low-income and minority students vs schools without such policies.38 The impetus for implementing more restrictive policies in these schools is unclear, though it could be because of higher FA prevalence among specific students or lack of school resources, such as financial constraints, diminished epinephrine availability, shortage of school nurses, or lack of training. The presence of peanut-free classrooms does not consistently reduce environmental peanut exposure. In a study of inner-city elementary schools, food allergens were detected on tables and floors in all schools, albeit at low levels, and milk and peanut were detected in all table wipe samples.39
In underresourced settings such as inner-city schools, in which there may be limited staff supervision during mealtimes, instituting allergen-restricted zones such as peanut-free tables may promote the safety of students with FA. However, these policies should consider the potential psychosocial impact on children, further discussed below. Providing allergen-restricted zones as an option but not a mandate for children may allow FA management to be personalized to balance the safety and psychosocial needs of individual students.
Stock Epinephrine
The passage of the 2013 School Access to Emergency Epinephrine Act, which incentivizes states to authorize or require that public schools stock undesignated EAIs be used for any student or staff in the event of an allergic reaction, marked an important milestone for treating FA reactions in schools. Before this, Houston elementary schools with high SES were 6 times more likely to have epinephrine injectors compared with lower SES schools.40 Such disparities likely reflect access to care differences by income. All but 1 state now allows stock epinephrine in schools, though only 12 mandate it, and the mandate often depends on the availability of funds.41 This has the potential to further accentuate disparities given the inequitable distribution of resources for stock epinephrine across schools.
A cost-effectiveness analysis of stock epinephrine for the treatment of anaphylactic reactions to peanuts in Chicago public schools found the intervention was cost-effective if the device cost no more than USD 338 annually per school.42 A model in which individual schoolchildren did not provide their own EAI but instead relied on school stock epinephrine led to cost savings. Such a model may also be life-saving for inner-city children with FA, given reduced access to EAIs in this population.43
Emergency Action Plans
A study of school EAPs among students in Chicago public schools found that, in adjusted models, the odds of having an EAP were significantly lower for Black vs White children and for students who received free school lunch vs those who did not.44 The results speak to the racial, ethnic, and socioeconomic segregation of the city given that EAPs require physician verification and minority and low-income families may have lower access to health care.44
Staff Education and Training
Multiple studies have assessed the effectiveness of training school staff to prevent and manage FA reactions.45,46 One study in Houston elementary schools found that, compared with nurses in schools without a FA training program, nurses in schools with a 1-hour training session improved their knowledge of FA reaction treatment.47 There is great variation in who is trained and allowed to administer epinephrine in schools. Among schools participating in a stock epinephrine program, 31% reported that all school staff was trained to administer epinephrine but only 22% of schools reported that all staff was allowed to administer epinephrine.48 The need to have all staff trained and authorized to administer epinephrine is highlighted in a study that found the odds of having unlicensed staff administering epinephrine for a FA reaction was doubled for schools with higher vs lower building-to-nurse ratios.49 This may be particularly salient in inner-city schools in which nurses may oversee multiple schools and in which there is often a shortage of nurses, particularly during the coronavirus disease 2019 (COVID-19) pandemic.50
Psychosocial Impact of Food Allergies and School Policies
Children and families living in inner cities face psychosocial challenges including housing and food insecurity, poverty, reduced access to health care, neighborhood safety concerns, segregation, and structural and systemic racism. These burdens and others can lead to reduced quality of life (QOL) and increased anxiety, worry, and depression.51 For children and families with FA, the chronic and unpredictable nature of FA can further adversely impact psychosocial functioning.52
In school-aged children, caregivers are tasked with developing FA management plans to enable the child’s safe participation in activities outside of the home. Parents and children may have considerable concerns about FA reactions in schools and the ability of school staff to manage anaphylaxis. A survey of primarily White, non-Hispanic, higher-income families of children with FA found that, whereas most reported schools having at least 1 food allergy policy in place, 27.4% of parents had concerns regarding their child’s safety at school and many felt additional policies were necessary to improve the safety of the school environment for their child, particularly regarding epinephrine access, food labeling, and FA education and training.37
Up to half of the children with FA report experiencing bullying, most commonly at school, and children with FA are twice as likely to be bullied compared with children without FA.6,53-56 Bullying is perpetrated most commonly by classmates and other students, but also by teachers and school staff.6,54,56 Common reasons for being bullied included having a FA, being secluded in special groups (eg, sitting at special lunch tables), receiving special treatment, or carrying or wearing allergy medications (eg, EAIs).6,56 Bullying is associated with decreased QOL and increased distress in children and their parents.6 Table 3 summarizes the studies to date evaluating FA-related bullying.6,53-56 Few studies have evaluated the impact of sociodemographic factors on FA-related bullying and none have evaluated rates in inner-city schools.6,53-55 Racial and ethnic differences may exist in FA-related bullying, though most studies were done in primarily White, non-Hispanic, and higher SES cohorts.
Table 3.
Food Allergy-Related Bullying in US Schoolchildren
| Reference | Study design | Number of participants |
Instrument to measure bullying |
Questionnaire completed by |
Child population | Rate of food allergy-related bullying |
|---|---|---|---|---|---|---|
| Annunziato et al,55 2014 | Longitudinal, single center | 127 | EMPOWER Program Survey | Children | Mainly White (89.5%), non-Hispanic (91.9%), and higher socioeconomic status (65.4% annual household income ≥ $100,000). |
|
| Brown et al,57 2021 | Longitudinal, multicenter | 252 | Self-generated questionnaire | Parents | All non-Hispanic. White (73.4%) and Black (26.6%). Annual household income ≥ $100,000 in 74.1% of White families vs < $50,000 in 60.7% of Black (P < .001). |
|
| Cooke et al,56 2021 | Cross-sectional, multicenter | 121 | EMPOWER Program Survey | Parents and children | Racial/ethnic breakdown was comparable to study clinic populations and household income comparable to the region's US Census Bureau data. Black (37.0%), White (30.0%), Multiracial (12.0%), Other (8.0%); Hispanic (12.0%). Annual household income ≥ $100,000 in 41.0% of families. |
|
| Lieberman et al,54 2010 | Cross-sectional, multicenter | 353 | Self-generated questionnaire | Mainly parents | Mainly White (95.1%), non-Hispanic (97.4%). |
|
| Shemesh et al,6 2013 | Cross-sectional, single center | 251 | EMPOWER Program Survey | Parents and children | Mainly White (85.7%), non-Hispanic (90.4%), and higher socioeconomic status (65.3% annual household income ≥ $100,000). |
|
School FA policies could have a substantial psychosocial impact on children. Bullying related to FA was less frequently reported by students with FA in schools banning peanuts.57 It is possible that schools with policies restricting allergens may have lower rates of allergic reactions; students with FA and their parents may have decreased stress, worry, and anxiety related to FA; and students with FA may experience less FA-related bullying simply owing to the decreased presence of their allergens. However, in schools with allergen-restricted areas such as “peanut-free” lunch tables, it is also possible that students with FA could feel singled out because of their FA and become targets for bullying. In fact, ethnic minority children with low SES recruited from an urban pediatric clinic had high levels of social anxiety because of their FA.58 One potential explanation offered was that, in underresourced schools that may opt to use designated allergen-free tables, children with FA sitting at those tables may feel isolated from peers.58
Food Allergy, Food Insecurity, and School Meals
Food insecurity (FI) is defined as inadequate access to affordable and nutritious food.59 One in 5 children with FA lives in food-insecure households, compared with 1 in 6 children without FA.60 Families at risk of FI perceive the risk that their child with FA will accidentally consume unsafe food to be higher compared with their food-secure counterparts.61 Low-income households of children with FA spend more on FA emergency management (eg, ED visits) compared with their higher-income counterparts, but less on preventive steps (eg, specialty foods).62 FI is associated with higher caregiver stress and worse QOL compared with food-secure households. Among patients with FA, overall QOL is worse in FI compared with food-secure groups.63 Low-income families with FA face a dual burden in ensuring access to safe, allergen-free foods for their children.64 Factors that may contribute to or exacerbate FI for inner-city families are low SES and living in food deserts in which there is limited access to affordable, healthy, and allergen-safe food options.
Families with FI are more likely to obtain food from food banks,61 in which there is added concern over the availability of safe foods.65 Low-income families with FA may struggle with the purchase of safe foods during the monthly Supplemental Nutrition Assistance Program cycle because such foods are often cost-prohibitive and may deplete funds before the renewal of benefits.66 Programs meant to alleviate challenges related to the provision of safe food (Table 4), such as the National School Lunch Program, may play an important role for these families. A recent survey of families with children with FA revealed that 4.7% were at risk of FI and 10.8% were eligible to receive free or reduced-price school meals. Notably, 70% of families eligible to receive free or reduced-price school meals opted out of receiving them; the primary reason being concerns regarding FA (89%).67 The study population was primarily higher income and likely underestimated the burden of FI among families with FA.
Table 4.
Federal Food Assistance Programs in the United States
| Legislation, Policy, or Program |
Description | Website for further information |
|---|---|---|
| Farm Bill | Legislation package that authorizes or reauthorizes the USDA programs across the US food system, including nutrition assistance programs such as the Supplemental Nutrition Assistance Program. | https://www.usda.gov/farmbill |
| SNAP | Nutrition benefits program for low-income families, formerly known as Food Stamps. Benefits are dispersed once per month by means of the Electronic Benefits Transfer program in accordance with the Thrifty Food Plan for specific family sizes. | https://www.fns.usda.gov/snap/supplemental-nutrition-assistance-program |
| EBT | An electronic system that allows SNAP participants to use their benefits to pay for food. | https://www.fns.usda.gov/snap/ebt |
| Thrifty Food Plan | A food plan was developed by the USDA to estimate the lowest cost of a healthy diet for a family of 4. | https://www.fns.usda.gov/snap/thriftyfoodplan |
| Healthy, Hunger-Free Kids Act | Legislation that authorizes funding for the USDA’s child nutrition programs, including the National School Lunch Program. Provides standards for healthy school meals. | https://www.fns.usda.gov/cn/healthy-hunger-free-kids-act |
| NSLP | Federally assisted meal program that provides free or reduced-price lunches to children at school. | https://www.fns.usda.gov/nslp |
| Community Eligibility Provision | Nonpricing meal service option allows schools and school districts in low-income areas to serve free school meals to all students without having to apply. | https://www.fns.usda.gov/cn/community-eligibility-provision |
| Pandemic-EBT | Established by the Families First Coronavirus Response Act to provide benefits to children that would have received free or reduced-price school meals if schools had not been closed because of the COVID-19 pandemic. | https://www.fns.usda.gov/snap/ebt |
Abbreviations: COVID-19, coronavirus disease 2019; EBT, Electronic Benefits Transfer; NSLP, National School Lunch Program; SNAP, Supplemental Nutrition Assistance Program; USDA, US Department of Agriculture.
Among inner-city schoolchildren, free or reduced-price school meals are often the default thanks to the Community Eligibility Provision, which was authorized as part of the 2010 Healthy, Hunger-Free Kids Act, allowing schools and local educational agencies located in low-income areas to provide free breakfast and lunch to all students.68 A study of caregivers of children with FA in Chicago, Illinois, Cincinnati, Ohio, and Washington, District of Columbia, found the odds of eating food prepared at school were 2.5 times higher in Black vs White children, though it is unclear what is driving this difference.69
Special Case: The Coronavirus Disease 2019 Pandemic
The ongoing COVID-19 pandemic led to widespread school closures. For families with FA at risk of FI and relying on school meals, the pandemic may be an additional source of strain.51,59 Compared with households without dietary restrictions, households with FA were more likely to experience FI in the year before the pandemic and more likely to experience incident or worsening FI during the pandemic.70 Multiple school districts developed innovative ways to ensure that children kept receiving school meals while school was conducted remotely, including by creating pick-up sites at school and dropping off meals along bus routes.71 This may further exacerbate disparities if schools with more resources are better able to adapt and innovate.
Opportunities to Address Food Allergy Management and Disparities
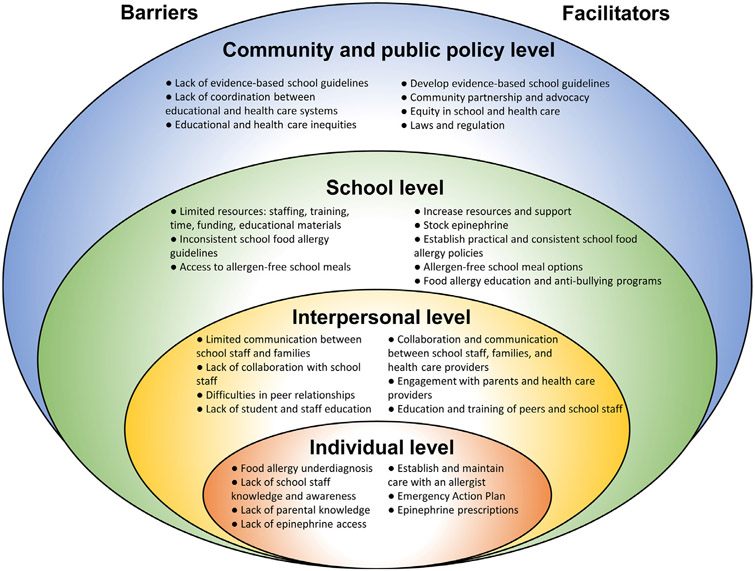
Opportunities exist at many levels for patients, health care providers including allergists and primary care providers, schools, and communities to partner to identify and address disparities in FA management in inner-city schools (Fig 2).
Figure 2.
Socioecological model of barriers to and facilitators for inner-city school food allergy management. Individual-level comprises children with food allergies and their parents. Interpersonal level comprises relationships among patients, families, peers, school staff, and health care providers. School-level comprises school nurses, teachers, and other school staff. Community and public policy level comprises relationships among institutions, laws, and policies.
Individual Level
For children with FA and their parents, increased awareness of FA risk factors, signs, and symptoms can lead to earlier diagnosis of FA and treatment of anaphylaxis, leading to improved health outcomes. Allergists and other health care providers can identify patients that may be at risk of underdiagnosis or undertreatment of FA and increase outreach across levels of the socioecological model to raise awareness and provide access to high-quality care. Health care providers can ensure their patients have written EAPs that are updated annually and EAI prescriptions to bring to schools and reduce the financial burden on families by prescribing low-cost alternatives to EAIs and connecting families with financial assistance programs.72
Interpersonal Level
The interpersonal level comprises interconnections among patients, families, peers, school staff, and health care providers. Providing school nurses, teachers, and staff with high-quality FA education may lead to better recognition of allergic reactions, higher quality FA management, and raise awareness of bullying. In managing children with long-term health conditions such as FA, school nurses perceive a lack of parental support and knowledge of health conditions.73 Parents perceive limited communication and lack of collaboration with school staff, and concern about their children’s relationships with their peers because of their medical conditions.74
Parents, school staff, and classmates can overcome these barriers by collaborating and communicating to develop FA management and education plans. Educating and training school staff and peers can demystify and correct misconceptions regarding FA. This may lead to improved awareness and management, increased understanding of challenges children with FA face, and decreased FA-related teasing and bullying. Allergists can play a critical role in facilitating these interpersonal discussions and bridging communication gaps.
School Level
Many school-level barriers to providing optimal FA management are exacerbated by conditions inherent to inner-city schools. School nurses cite insufficient staffing, lack of school programs for stock epinephrine and providing education and training, lack of evidence-based school guidelines, lack of time, and poor institutional support.73 Parents of children with FA have concerns regarding lack of school nurses, inconsistencies in school staff carrying or trained to use EAIs, limited availability of EAIs, limited allergen-free environments, and concerns that allergen information on school lunch menus is often unavailable.37,74 Nurses and parents both cite concerns for limited FA education materials.73,74
Providing sufficient nurse staffing and education is critical to addressing these needs. Although many schools may not have a full-time school nurse, providing FA education and training to all school staff and students is important, and allergists can provide this education through outreach and partnership with schools. FA training among the school staff is associated with improvements in their ability to recognize symptoms and identify the appropriate treatment of allergic reactions and may improve school-level FA management preparedness.45 Key stakeholders including parents, school staff, and allergists can partner to develop school FA management guidelines that are sensitive to the safety and needs of students with FA and the larger school community.45,72,75 Students should be provided access to safe snacks and meals at school, with clear allergen labeling. For families with young children, menus must be provided in advance so parents can review ingredients and make plans for alternative choices if needed. For low-income families who rely on free or reduced-price school meals, providing subsidized allergen-free meal options is important to minimize financial strain. Finally, schools should have robust antibullying policies to promote the safety and well-being of students with FA.
Community and Policy Level
At the community and policy level, there is a lack of evidence-based FA management guidelines and a lack of coordination between school and health care systems. Further research is needed into the impact of school FA policies on allergic reactions, particularly from schools representing diverse students and regions. Allergists can work with communities and local and national governments to standardize and implement evidence-based policies to promote the safety and well-being of children with FA. Efforts to promote equitable access to high-quality schools and health care are critically needed to provide inner-city children with the necessary resources.
Conclusion
The goal of the schools' FA management includes minimizing the risk of allergic reactions while maximizing the emotional well-being of students. All children with FA, regardless of zip code, SES, race, or ethnicity, deserve to attend school in a physically and emotionally secure environment fostering education, safety, and social inclusion. The impact of the multiple facets of social determinants of health on FA is not well understood and many unanswered questions remain, as summarized in Table 5. Challenges in addressing FA in inner-city children include the paucity of research in underrepresented and underserved populations, and the historical focus on race and ethnicity in the scientific literature, which can fail to acknowledge the underlying structural racism and health inequities that may better account for observed disparities in FA outcomes. Allergists play an important role in the FA community by providing care to patients, outreach to communities, and advancing research. By understanding the unique challenges in caring for patients with FA from diverse backgrounds, we can develop strategies to ensure that all children with FA receive the care they deserve.
Table 5.
Assessment of Unmet Needs in Food Allergy Among Inner-City Schoolchildren
| Food allergy epidemiology |
| Determine food allergy prevalence across diverse populations |
| Understand the role of social determinants of health in food allergy prevalence |
| Access to health care |
| Identify barriers to food allergy diagnosis |
| Identify barriers to medical care |
| Improve access to written Emergency Action Plans |
| Improve access to epinephrine autoinjectors |
| Improve screening for food insecurity in primary care and allergy clinics |
| Food allergy management in schools |
| Develop evidence-based school food allergy policies |
| Implement food allergy management policies in schools |
| Identify barriers to a successful implementation of food allergy management strategies in schools |
| Implement food allergy education for students and staff |
| Identify barriers to communication between school staffand families |
| Increase access to stock epinephrine |
| Psychosocial impact |
| Identify risk factors for impaired psychosocial functioning in inner-city children and families |
| Increase psychosocial support for children and families |
| Increase awareness of food allergy–related bullying |
| Implement anti-bullying programs in schools |
| Economic impact |
| Increase access to low-cost allergen-free foods for families at risk of food insecurity |
| Increase availability of allergen-free school meals |
Key Messages.
Food allergy management consists of both preventing and treating allergic reactions, which poses unique challenges in the inner-city school setting.
Managing food allergy in schools is complex, controversial, and highly variable, and evidence-based guidance is minimal.
Disparities in food allergy prevalence, management, and treatment exist.
Further research is needed to better characterize and address these disparities and understand the mechanisms leading to them.
There are opportunities for partnership among health care providers, schools, and communities to address unmet needs in food allergy management and disparities in the inner-city school setting.
Funding:
This research is supported by the National Institutes of Health K23 AI143962 (Dr Bartnikas), K24 AI106822 (Dr Phipatanakul), and The Allergy and Asthma Awareness Initiative, Inc (Dr Phipatanakul).
Footnotes
Disclosures: The authors have no conflicts of interest to report.
References
- 1.Gupta RS, Warren CM, Smith BM, Blumenstock JA, Jiang J, Davis MM, et al. The public health impact of parent-reported childhood food allergies in the United States. Pediatrics. 2018;142:(6) e20181235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McIntyre CL, Sheetz AH, Carroll CR, Young MC. Administration of epinephrine for life-threatening allergic reactions in school settings. Pediatrics. 2005;116(5):1134–1140. [DOI] [PubMed] [Google Scholar]
- 3.Nowak-Wegrzyn A, Conover-Walker MK, Wood RA. Food-allergic reactions in schools and preschools. Arch Pediatr Adolesc Med. 2001;155(7):790–795. [DOI] [PubMed] [Google Scholar]
- 4.Bartnikas LM, Huffaker MF, Sheehan WJ, Kanchongkittiphon W, Petty CR, Leibowitz R, et al. Impact of school peanut-free policies on epinephrine administration. J Allergy Clin Immunol. 2017;140(2):465–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Waserman S, Cruickshank H, Hildebrand KJ, Mack D, Bantock L, Bingemann T, et al. Prevention and management of allergic reactions to food in child care centers and schools: practice guidelines. J Allergy Clin Immunol. 2021;147(5):1561–1578. [DOI] [PubMed] [Google Scholar]
- 6.Shemesh E, Annunziato RA, Ambrose MA, Ravid NL, Mullarkey C, Rubes M, et al. Child and parental reports of bullying in a consecutive sample of children with food allergy. Pediatrics. 2013;131(1):e10–e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davis CM, Apter AJ, Casillas A, Foggs MB, Louisias M, Morris EC, et al. Health disparities in allergic and immunologic conditions in racial and ethnic underserved populations: a work group report of the AAAAI Committee on the Underserved. J Allergy Clin Immunol. 2021;147(5):1579–1593. [DOI] [PubMed] [Google Scholar]
- 8.Bilaver LA, Kanaley MK, Fierstein JL, Gupta RS. Prevalence and correlates of food allergy among Medicaid-enrolled United States children. Acad Pediatr. 2021;21(1):84–92. [DOI] [PubMed] [Google Scholar]
- 9.Keet CA, Savage JH, Seopaul S, Peng RD, Wood RA, Matsui EC. Temporal trends and racial/ethnic disparity in self-reported pediatric food allergy in the United States. Ann Allergy Asthma Immunol. 2014;112(3):222–229. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McGowan EC, Peng RD, Salo PM, Zeldin DC, Keet CA. Changes in food-specific IgE over time in the National Health and Nutrition Examination Survey (NHANES). J Allergy Clin Immunol Pract. 2016;4(4):713–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McGowan EC, Matsui EC, Peng R, Salo PM, Zeldin DC, Keet CA. Racial/ethnic and socioeconomic differences in self-reported food allergy among food-sensitized children in National Health and Nutrition Examination Survey III. Ann Allergy Asthma. Immunol. 2016;117(5):570–572. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahdavinia M, Fox SR, Smith BM, James C, Palmisano EL, Mohammed A, et al. Racial differences in food allergy phenotype and health care utilization among US children. J Allergy Clin Immunol Pract. 2017;5(2):352–357. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mahdavinia M, Tobin MC, Fierstein JL, Andy-Nweye AB, Bilaver LA, Fox S, et al. African American children are more likely to be allergic to shellfish and finfish: findings from FORWARD, a multisite cohort study. J Allergy Clin Immunol Pract. 2021;9(7):2867–2873.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Coulson E, Rifas-Shiman SL, Sordillo J, Bunyavanich S, Camargo CA Jr, Platts-Mills TAE, et al. Racial, ethnic, and socioeconomic differences in adolescent food allergy. J Allergy Clin Immunol Pract. 2020;8(1):336–338. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang HT, Warren CM, Gupta RS, Davis CM. Prevalence and characteristics of shellfish allergy in the pediatric population of the United States. J Allergy Clin Immunol Pract. 2020;8(4):1359–1370. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shroba J, Rath N, Barnes C. Possible role of environmental factors in the development of food allergies. Clin Rev Allergy Immunol. 2019;57(3):303–311. [DOI] [PubMed] [Google Scholar]
- 17.Wang J, Calatroni A, Visness CM, Sampson HA. Correlation of specific IgE to shrimp with cockroach and dust mite exposure and sensitization in an inner-city population. J Allergy Clin Immunol. 2011;128(4):834–837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poowuttikul P, Saini S, Seth D. Inner-city asthma in children. Clin Rev Allergy Immunol. 2019;56(2):248–268. [DOI] [PubMed] [Google Scholar]
- 19.Croce EA, Levy ML, Adamson AS, Matsui EC. Reframing racial and ethnic disparities in atopic dermatitis in Black and Latinx populations. J Allergy Clin Immunol. 2021;148(5):1104–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fleischer DM, Chan ES, Venter C, Spergel JM, Abrams EM, Stukus D, et al. A consensus approach to the primary prevention of food allergy through nutrition: guidance from the American Academy of Allergy, Asthma, and Immunology; American College of Allergy, Asthma, and Immunology; and the Canadian Society for Allergy and Clinical Immunology. J Allergy Clin Immunol Pract. 2021;9:22–43. e4. [DOI] [PubMed] [Google Scholar]
- 21.Shaw TE, Currie GP, Koudelka CW, Simpson EL. Eczema prevalence in the United States: data from the 2003 National Survey of Children’s Health. J Invest Dermatol. 2011;131(1):67–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Donohue KM, Al-alem U, Perzanowski MS, Chew GL, Johnson A, Divjan A, et al. Anti-cockroach and anti-mouse IgE are associated with early wheeze and atopy in an inner-city birth cohort. J Allergy Clin Immunol. 2008;122(5):914–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Permaul P, Phipatanakul W. School environmental intervention programs. J Allergy Clin Immunol Pract. 2018;6(1):22–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mikhail I, Stukus DR, Prince BT. Fatal anaphylaxis: epidemiology and risk factors. Curr Allergy Asthma Rep. 2021;21(4):28. [DOI] [PubMed] [Google Scholar]
- 25.Eigenmann PA, Ebisawa M, Greenhawt M, Hourihane JO, Perry TT, Remington BC, et al. Addressing risk management difficulties in children with food allergies. Pediatr Allergy Immunol. 2021;32(4):658–666. [DOI] [PubMed] [Google Scholar]
- 26.Friedlander JL, Sheehan WJ, Baxi SN, Kopel LS, Gaffin JM, Ozonoff A, et al. Food allergy and increased asthma morbidity in a School-based Inner-City Asthma Study. J Allergy Clin Immunol Pract. 2013;1(5):479–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taylor-Black S, Wang J. The prevalence and characteristics of food allergy in urban minority children. Ann Allergy Asthma Immunol. 2012;109(6):431–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang J, Visness CM, Sampson HA. Food allergen sensitization in inner-city children with asthma. J Allergy Clin Immunol. 2005;115(5):1076–1080. [DOI] [PubMed] [Google Scholar]
- 29.Antonucci R, Locci C, Clemente MG, Chicconi E, Antonucci L. Vitamin D deficiency in childhood: old lessons and current challenges. J Pediatr Endocrinol Metab. 2018;31(3):247–260. [DOI] [PubMed] [Google Scholar]
- 30.Sakai-Bizmark R, Friedlander SMI, Oshima K, Webber EJ, Mena LA, Marr EH, et al. Urban/rural residence effect on emergency department visits arising from food-induced anaphylaxis. Allergol Int. 2019;68(3):316–320. [DOI] [PubMed] [Google Scholar]
- 31.Fenton A, Elliott E, Shahbandi A, Ezenwa E, Morris C, McLawhorn J, et al. Medical students’ ability to diagnose common dermatologic conditions in skin of color. J Am Acad Dermatol. 2020;83(3):957–958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buster KJ, Stevens EI, Elmets CA. Dermatologic health disparities. Dermatol Clin. 2012;30(1):53–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dupuis R, Kinsey EW, Spergel JM, Brown-Whitehorn T, Graves A, Samuelson K, et al. Food allergy management at school. J Sch Health. 2020;90(5):395–406. [DOI] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. Voluntary Guidelines for Managing Food Allergies in Schools and Early Care and Education Programs. Washington, DC: US Department of Health and Human Services; 2013. [Google Scholar]
- 35.Golding MA, Gunnarsson NV, Middelveld R, Ahlstedt S, Protudjer JLP. A scoping review of the caregiver burden of pediatric food allergy. Ann Allergy Asthma. Immunol. 2021;127(5):536–547. e3. [DOI] [PubMed] [Google Scholar]
- 36.Tsuang A, Wang J. Childcare and school management issues in food allergy. Curr Allergy Asthma Rep. 2016;16(12):83. [DOI] [PubMed] [Google Scholar]
- 37.Mustafa SS, Russell AF, Kagan O, Kao LM, Houdek DV, Smith BM, et al. Parent perspectives on school food allergy policy. BMC Pediatr. 2018;18(1):164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bartnikas LM, Huffaker MF, Sheehan WJ, Kanchongkittiphon W, Petty CR, Leibowitz R, et al. Racial and socioeconomic differences in school peanut-free policies. J Allergy Clin Immunol Pract. 2020;8(1):340–342. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Maciag MC, Sheehan WJ, Bartnikas LM, Lai PS, Petty CR, Filep S, et al. Detection of food allergens in school and home environments of elementary students. J Allergy Clin Immunol Pract. 2021;9(10):3735–3743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shah SS, Parker CL, Smith EO, Davis CM. Disparity in the availability of injectable epinephrine in a large, diverse US school district. J Allergy Clin Immunol Pract. 2014;2(3):288–293.e1. [DOI] [PubMed] [Google Scholar]
- 41.Volerman A, Brindley C, Amerson N, Pressley T, Woolverton N. A national review of state laws for stock epinephrine in schools. J Sch Health. 2022;92(2):209–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shaker MS, Greenhawt MJ. Analysis of value-based costs of undesignated school stock epinephrine policies for peanut anaphylaxis. JAMA Pediatr. 2019;173(2):169–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tarr Cooke A, Meize-Grochowski R. Epinephrine auto-injectors for anaphylaxis treatment in the school setting: a discussion paper. SAGE Open Nurs. 2019;5:2377960819845246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gupta RS, Rivkina V, DeSantiago-Cardenas L, Smith B, Harvey-Gintoft B, Whyte SA. Asthma and food allergy management in Chicago public schools. Pediatrics. 2014;134(4):729–736. [DOI] [PubMed] [Google Scholar]
- 45.Waserman S, Shah A, Cruikshank H, Avilla E. Recognition and management of food allergy and anaphylaxis in the school and community setting. Immunol Allergy Clin North Am. 2022;42(1):91–103. [DOI] [PubMed] [Google Scholar]
- 46.White L, Aubin J, Bradford C, Alix C, Hughes L, Phipatanakul W. Effectiveness of a computer module to augment the training of school staff in the management of students with food allergies. Ann Allergy Asthma. Immunol. 2015;114(3):254–255. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shah SS, Parker CL, Davis CM. Improvement of teacher food allergy knowledge in socioeconomically diverse schools after educational intervention. Clin Pediatr (Phila). 2013;52(9):812–820. [DOI] [PubMed] [Google Scholar]
- 48.Hogue SL, Goss D, Hollis K, Silvia S, White MV. Training and administration of epinephrine auto-injectors for anaphylaxis treatment in US schools: results from the EpiPen4Schools(®) pilot survey. J Asthma Allergy. 2016;9:109–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tsuang A, Demain H, Patrick K, Pistiner M, Wang J. Epinephrine use and training in schools for food-induced anaphylaxis among non-nursing staff. J Allergy Clin Immunol Pract. 2017;5(5):1418–1420. e3. [DOI] [PubMed] [Google Scholar]
- 50.Graham KA. Philly’s school nurses are exhausted as staff shortages and COVID-19 double their workload. The Philadelphia Inquirer. 2021. https://www.inquirer.com/education/school-nurse-covid-philadelphia-20210920.html. Accessed January 28, 2022. [Google Scholar]
- 51.Abrams EM, Greenhawt M, Shaker M, Pinto AD, Sinha I, Singer A. The COVID-19 pandemic: adverse effects on the social determinants of health in children and families. Ann Allergy Asthma Immunol. 2022;128(1):19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Westwell-Roper C, To S, Andjelic G, Lu C, Lin B, Soller L, et al. Food-allergy-specific anxiety and distress in parents of children with food allergy: a systematic review. Pediatr Allergy Immunol. 2022;33(1):e13695. [DOI] [PubMed] [Google Scholar]
- 53.Herbert L, Shemesh E, Bender B. Clinical management of psychosocial concerns related to food allergy. J Allergy Clin Immunol Pract. 2016;4(2):205–213. [DOI] [PubMed] [Google Scholar]
- 54.Lieberman JA, Weiss C, Furlong TJ, Sicherer M, Sicherer SH. Bullying among pediatric patients with food allergy. Ann Allergy Asthma Immunol. 2010;105(4):282–286. [DOI] [PubMed] [Google Scholar]
- 55.Annunziato RA, Rubes M, Ambrose MA, Mullarkey C, Shemesh E, Sicherer SH. Longitudinal evaluation of food allergy-related bullying. J Allergy Clin Immunol Pract. 2014;2(5):639–641. [DOI] [PubMed] [Google Scholar]
- 56.Cooke F, Ramos A, Herbert L. Food allergy-related bullying among children and adolescents. J Pediatr Psychol. 2022;47(3):318–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Brown D, Negris O, Gupta R, Herbert L, Lombard L, Bozen A, et al. Food allergy-related bullying and associated peer dynamics among Black and White children in the FORWARD study. Ann Allergy Asthma Immunol. 2021;126(3):255–263. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Goodwin RD, Rodgin S, Goldman R, Rodriguez J, deVos G, Serebrisky D, et al. Food allergy and anxiety and depression among ethnic minority children and their caregivers. J Pediatr. 2017;187:258–264. e1. [DOI] [PubMed] [Google Scholar]
- 59.Brown E, Das R, Brewer AG, Martinez E, Bilaver LA, Gupta RS. Food insecure and allergic in a pandemic: a vulnerable population. J Allergy Clin Immunol Pract. 2020;8(7):2149–2151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Johns CB, Savage JH. Access to health care and food in children with food allergy. J Allergy Clin Immunol. 2014;133(2):582–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tackett AP, Farrow ML, McQuaid EL. Food security, utilization of food assistance programs, and caregiver perceptions of food-induced anaphylaxis risk in children with food allergies. Pediatr Allergy Immunol Pulmonol. 2018;31(2):91–96. [Google Scholar]
- 62.Bilaver LA, Kester KM, Smith BM, Gupta RS. Socioeconomic disparities in the economic impact of childhood food allergy. Pediatrics. 2016;137:(5)e20153678. [DOI] [PubMed] [Google Scholar]
- 63.Dilley MA, Rettiganti M, Christie L, O'Brien E, Patterson M, Weeks C, et al. Impact of food allergy on food insecurity and health literacy in a tertiary care pediatric allergy population. Pediatr Allergy Immunol. 2019;30(3):363–369. [DOI] [PubMed] [Google Scholar]
- 64.Bozen A, Zaslavsky JM, Cohn D, Samady W, Lombard L, Nadeau K, et al. Barriers to food allergy management among Americans with low income. Ann Allergy Asthma. Immunol. 2020;125(3):341–343. [DOI] [PubMed] [Google Scholar]
- 65.Minaker LM, Elliott SJ, Clarke A. Exploring low-income families’ financial barriers to food allergy management and treatment. J Allergy (Cairo). 2014;2014:160363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kinsey EW, Dupuis R, Oberle M, Cannuscio CC, Hillier A. Chronic disease self-management within the monthly benefit cycle of the Supplemental Nutrition Assistance Program. Public Health Nutr. 2019;22(12):2248–2259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dupuis R, Herbert L, Young M, Sicherer S, Phipatanakul W, Bartnikas L. Disrupted foodways: food allergies and food insecurity. J Allergy Clin Immunol. 2022;149:(2)AB106. https://www.jacionline.org/article/S0091-6749(21)02190-4/. [Google Scholar]
- 68.United States Department of Agriculture. The Community Eligibility Provision (CEP); 2015. Available at: https://frac.org/research/resource-library/community-eligibility-cep-database. Accessed January 17, 2022.
- 69.Vincent E, Bilaver LA, Fierstein JL, Thivalapill N, Pappalardo AA, Coleman A, et al. Associations of food allergy-related dietary knowledge, attitudes, and behaviors among caregivers of black and white children with food allergy. J Acad Nutr Diet. 2022;122(4):797–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Guillaume JD, Jagai JS, Makelarski JA, Abramsohn EM, Lindau ST, Verma R, et al. COVID-19-Related food insecurity among households with dietary restrictions: a national survey. J Allergy Clin Immunol Pract. 2021;9(9):3323–3330. e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kinsey EW, Hecht AA, Dunn CG, Levi R, Read MA, Smith C, et al. School closures during COVID-19: opportunities for innovation in meal service. Am J Public Health. 2020;110(11):1635–1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wang J, Bingemann T, Russell AF, Young MC, Sicherer SH. The allergist’s role in anaphylaxis and food allergy management in the school and childcare setting. J Allergy Clin Immunol Pract. 2018;6(2):427–435. [DOI] [PubMed] [Google Scholar]
- 73.Uhm JY, Choi MY, Lee H. School nurses’ perceptions regarding barriers and facilitators in caring for children with chronic diseases in school settings: a mixed studies review. Nurs Health Sci. 2020;22(4):868–880. [DOI] [PubMed] [Google Scholar]
- 74.Uhm JY, Choi MY. Barriers to and facilitators of school health care for students with chronic disease as perceived by their parents: a mixed systematic. Healthcare (Basel). 2020;8(4):506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Greenhawt M, Shaker M, Stukus DR, Fleischer DM, Hourihane J, Tang MLK, et al. Managing food allergy in schools during the COVID-19 pandemic. J Allergy Clin Immunol Pract. 2020;8(9):2845–2850. [DOI] [PMC free article] [PubMed] [Google Scholar]