Abstract
We identify the sodium leak channel non-selective protein (NALCN) as a key regulator of cancer metastasis and nonmalignant cell dissemination. Among 10,022 human cancers, NALCN loss-of-function mutations were enriched in gastric and colorectal cancers. Deletion of Nalcn from gastric, intestinal or pancreatic adenocarcinomas in mice did not alter tumor incidence, but markedly increased the number of circulating tumor cells (CTCs) and metastases. Treatment of these mice with gadolinium—a NALCN channel blocker—similarly increased CTCs and metastases. Deletion of Nalcn from mice that lacked oncogenic mutations and never developed cancer caused shedding of epithelial cells into the blood at levels equivalent to those seen in tumor-bearing animals. These cells trafficked to distant organs to form normal structures including lung epithelium, and kidney glomeruli and tubules. Thus, NALCN regulates cell shedding from solid tissues independent of cancer, divorcing this process from tumorigenesis and unmasking a potential new target for antimetastatic therapies.
Subject terms: Metastasis, Inflammatory diseases
The ion channel NALCN regulates cell shedding in mice and enhances metastasis in mouse models of cancer. Disseminated cells without oncogenic mutations form normal structures at secondary sites, suggesting that cell shedding is a physiological process that is hijacked during tumorigenesis.
Main
Most patients with cancer die as a result of metastasis1, the process by which cancer cells spread from the primary tumor to other organs in the body2. Blocking metastasis could markedly improve the survival of patients with cancer, but how this process is triggered within the complex cascade of tumorigenesis remains unclear3.
Because metastasis is thought to be a wholly abnormal process, restricted to malignant tissues, attention has focused on identifying genetic mutations as drivers of cancer metastasis. Although this research has unmasked genes that promote metastasis in mouse models and humans, including a variety of ion channels that induce a metastasis-like phenotype by altering the transmembrane voltage to induce changes in gene transcription4–6, so far no recurrent metastasis-specific mutations have been identified2,3,7.
Other cell functions implicated in the metastatic cascade include ‘stem cell-like’ multipotency and plasticity. Stem cell capacity has been ascribed to metastatic cancer cells because of their ability to reconstitute heterogenous malignant cell populations as metastatic tumors8,9. Epithelial mesenchymal transition (EMT)2—a type of cellular plasticity displayed during normal gastrulation and tissue healing—is also an established feature of the metastatic cascade2,10. What remains unclear is how cancers ‘hijack’ these normal cell functions to enable metastasis.
Here, we identify a single ion channel, NALCN, as a key regulator of epithelial cell trafficking to distant tissues. NALCN is responsible for the background sodium leak conductance that maintains the resting membrane potential. It regulates key functions in excitable tissues, for example, respiration and circadian rhythms11–13, and gain-of-function mutations in the gene are associated with neurological disorders14. However, little is known about the role of NALCN in nonexcitable tissues. We show that NALCN regulates the release of malignant and normal epithelial cells into the blood, and their trafficking to distant sites where they form metastatic cancers, or apparently normal tissues, respectively. We thereby demonstrate that the metastatic cascade can be triggered and operate independent of tumorigenesis. These observations have profound implications for understanding epithelial cell trafficking in health and disease and identify a novel target for antimetastatic therapies.
Results
NALCN loss-of-function in cancer
We showed previously that Prominin1 (PROM1) marks basal stem cells in gastric antral glands and that their lineage forms adenocarcinomas in Prom1CreERT2/LacZ;KrasG12D;Trp53Flx/Flx (P1KP) mice15. PROM1+, but not PROM1−, cells isolated from P1KP gastric adenocarcinomas (P1KP-GAC) propagated these tumors as allografts, suggesting that PROM1+ P1KP-GAC cells are the malignant counterparts of antral gland basal stem cells (Extended Data Fig. 1). To understand how antral gland basal stem cells are corrupted during transformation, we compared their transcriptomes with those of PROM1+ P1KP-GAC cells. Ion channels and solute carriers were selectively downregulated in PROM1+ P1KP-GAC cells (Fig. 1a and Supplementary Table 1). Among these, NALCN—a leak sodium channel that contributes to the resting cell membrane potential and cell excitability13,16,17—was restricted in its expression to PROM1+ antral gland basal stem cells and downregulated in PROM1+ P1KP-GAC cells (Fig. 1b). Among 10,022 human cancers within The Cancer Genome Atlas, nonsynonymous mutations in NALCN were enriched in gastric, colorectal, lung, prostate and head and neck cancers (Fig. 1c)18,19. These cancers also contained deletions, and nonsense and frameshift mutations, at a frequency very similar to those observed in TP53 in human cancer20, suggesting NALCN might be a tumor suppressor (Supplementary Table 2).
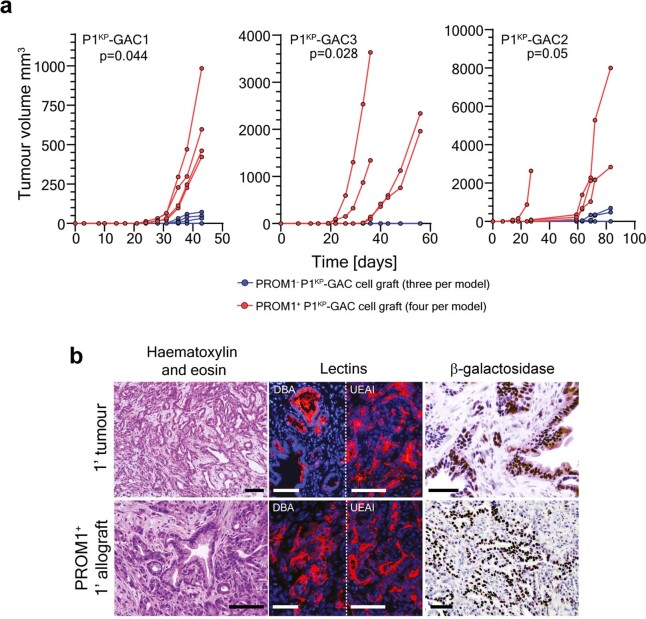
Extended Data Fig. 1. Prom1+P1KP-GAC cells propagate gastric adenocarcinoma as allografts.
(a) Growth of allografts derived from three independent P1KP gastric adenocarcinomas (GAC) in immunocompromised mice (PROM1+ n = 4 and PROM1−n = 3 for each allograft). Statistics are based on Permutation test whereby permuted p-values compare PROM1+ and PROM1− allografts for each tumour type using the average t-statistic between the groups as the test statistic. Two-tailed Permutation test GAC1 p = 0.044, GAC2 p = 0.05, GAC3 p = 0.028. (b) Histology of primary P1KP-GAC and daughter PROM1+ cell allografts. Tumours expressed gastric adenocarcinoma-associated lectins and PROM1 identified by Beta-galactosidase staining from Prom1 CreERT2/LacZ locus (scale=100um). Representative photomicrographs Primary P1KP-GAC n = 3 and PROM1+ cell allografts n = 12 evaluated histologically.
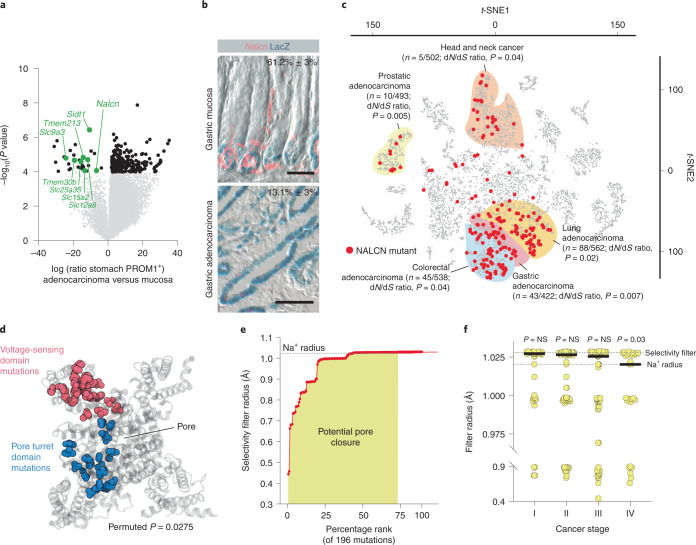
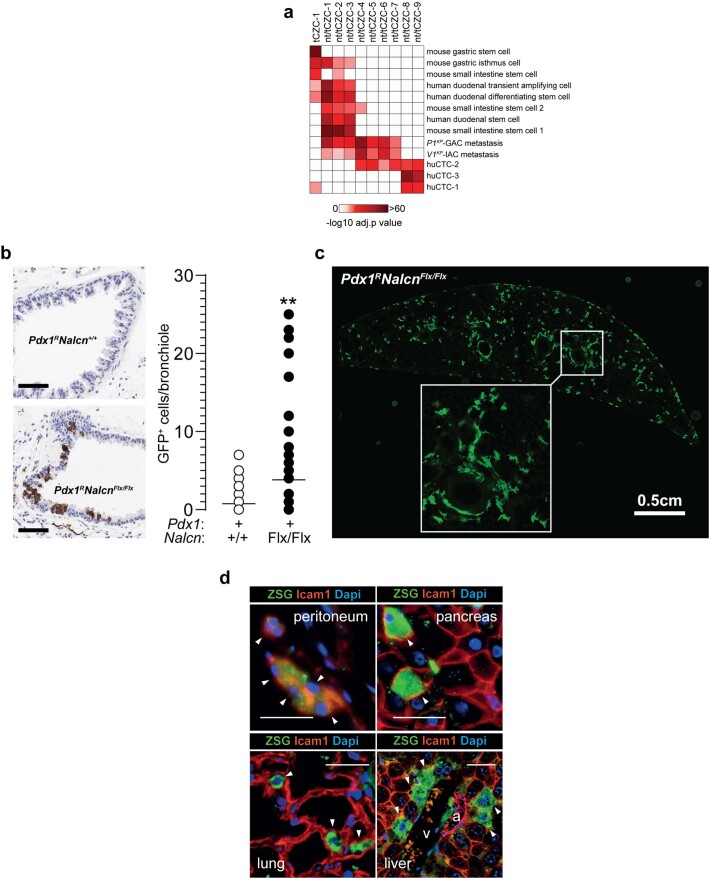
Fig. 1. NALCN loss-of-function in aggressive cancers.
a, Differential gene expression between normal PROM1+ gastric cells and P1KP-GAC cells (downregulated ion channels are highlighted). Benjamini–Hochberg corrected P value, alpha = 0.05. b, Nalcn RNA in situ hybridization and Prom1 expression (β-galactosidase (LacZ)) in Prom1CreERT2/LacZ mouse stomach (n = 3 biological replicates, 10 fields each; upper) and P1KP-GAC (n = 3 biological replicates, 10 fields each; lower). Numbers are shown as mean ± s.e.m. Prom1+/Nalcn+ cells. Scale bar, 50 μm. c, t-SNE plot of 10,022 human cancers (P value, dN/dS shown; Source data). d, Mutant residues enriched in NALCN pore turret (blue) and voltage-sensing (red) domains. P = 0.0275; permuted P value for probability of observing two clusters of 20 and 25 residues. e, Impact of 196 NALCN mutations on selectivity filter radius determined by HOLE analysis. f, NALCN pore closure by NALCN mutations in stage I (n = 47), stage II (n = 73), stage III (n = 74) and stage IV (n = 27) human cancers. Two-tailed Mann–Whitney U-test: stage I versus II, P = 0.3488; stage I versus III, P = 0.1613; stage I versus IV, P = 0.0293. Bar denotes median filter radius.
To determine how nonsynonymous mutations might affect NALCN function in cancer, we used HOLE analysis21 to predict their impact on the ion channel pore radius of NALCN embedded and relaxed within a 575-lipid 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphocholine bilayer in silico12,22,23. This model correctly predicted opening of the NALCN channel by 22 mutations known to confer gain-of-function12, and closure of the channel by two mutations that cause loss-of-function11 (Supplementary Table 3). Nonsynonymous, cancer-associated mutations were clustered within the pore turret and voltage-sensing domains that regulate NALCN channel opening11,12: 75% (n = 147/196) of these mutations were predicted to close the channel (Fig. 1d,e and Supplementary Table 4). Mutations predicted to cause the greatest pore closure were enriched in the most advanced cancers (Fig. 1f). Furthermore, human GACs in which NALCN was mutated, upregulated genes associated with EMT24, metastasis and cell migration (Supplementary Tables 5 and 6).
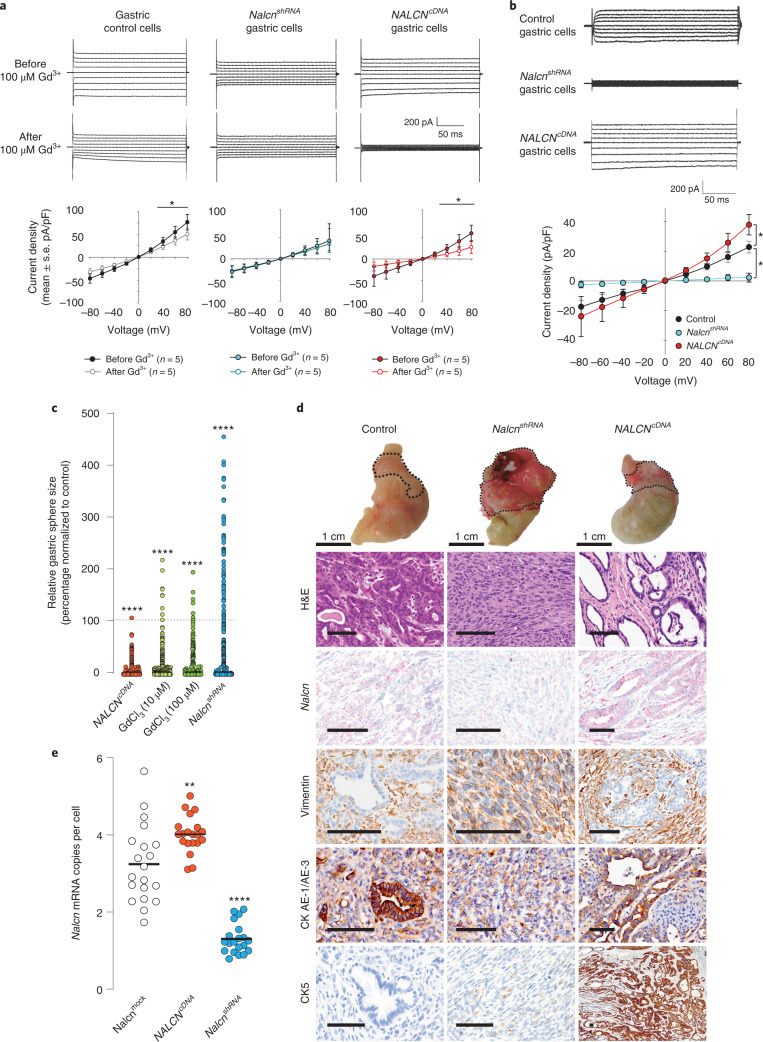
As a first step to test whether Nalcn regulates cancer progression, we altered its function in P1KP-GAC cells using genetic (Nalcn-short hairpin RNA and NALCN-complementary DNA lentiviral transduction) or chemical (gadolinium chloride; GdCl3)13 approaches. Whole-cell voltage-clamp analysis of P1KP-GAC cells showed a linear GdCl3-sensitive current to voltage steps in the ±80 mV range, as previously reported (Fig. 2a,b)13. Decreasing Nalcn expression in P1KP-GAC cells eliminated the NALCN current, increased cell proliferation and conferred an EMT morphology and transcriptome on P1KP-GAC orthotopic allografts (Fig. 2 and Supplementary Tables 7,8). Conversely, increased Nalcn expression increased the GdCl3-sensitive current in P1KP-GAC cells, decreased cell proliferation and conferred a hyperepithelialized morphology on allografts.
Fig. 2. NALCN regulates P1KP-GAC proliferation and morphology.
a, Current responses to voltage steps from −80 to 80 mV before (upper) and after (middle) addition of 100 μM gadolinium to P1KP-GAC control, NalcnshRNA- and NALCNcDNA-transfected cells, and current density responses to voltage steps before and after 100 μM gadolinium treatment (n = 5 biological replicate cells; values are mean ± s.e.m.). *P values at +40, + 60 and +80 mV for control gastric cells are 0.039, 0.032 and 0.023, respectively. P values at +40, +60 and +80 mV for NALCNcDNA cells are 0.013, 0.013 and 0.003, respectively (paired t-test). b, NALCN-mediated voltage-clamp ion currents from control, NalcnshRNA- and NALCNcDNA-transfected P1KP-GAC cells, and NALCN leak current density (current/cell membrane capacitance, mean ± s.e.m.) in control, NalcnshRNA- or NALCNcDNA-transfected cells (n = 5 cells each, P values comparing peak current at +80 mV voltage step are 0.05 control versus NALCNcDNA cells and 0.023 control versus NalcnshRNA cells; Holm–Sidak multiple comparison procedure). c, Impact of gadolinium treatment (10 µM, n = 386 organoids; 100 µM, n = 264), NalcnshRNA (n = 611) or NALCNcDNA (n = 1,472) transfection on P1KP-GAC organoid size normalized to average P1KP-GAC control treated organoids (P1KP 0 µM, n = 663 organoids, 4.274 ± 0.6238 (s.e.m.); P1KP shRNA control n = 651 organoids, 15.26 ± 2.406 (s.e.m.); P1KP cDNA control n = 583 organoids, 37.65 ± 5.872 (s.e.m.)). ***Exact P < 0.0001, two-tailed Mann–Whitney U-test. d, Representative macroscopic and photomicroscopic images of control (n = 27), NalcnshRNA (n = 21) or NALCNcDNA (n = 22) transduced P1KP-GAC orthotopic allografts. Nalcn RNA expression (in situ hybridization), and stromal (vimentin) and epithelial (CKAE1/AE3, CK7, CK5) marker immunohistochemistry are shown. Scale bar, 100 μm. e, Nalcn mRNA transcripts per tumor cell recorded in 20 individual tumor sections per treatment type. Bar, median. **P = 0.0024, ****P = 0.00006, two-tailed Mann–Whitney U-test.
Loss of Nalcn promotes cancer metastasis
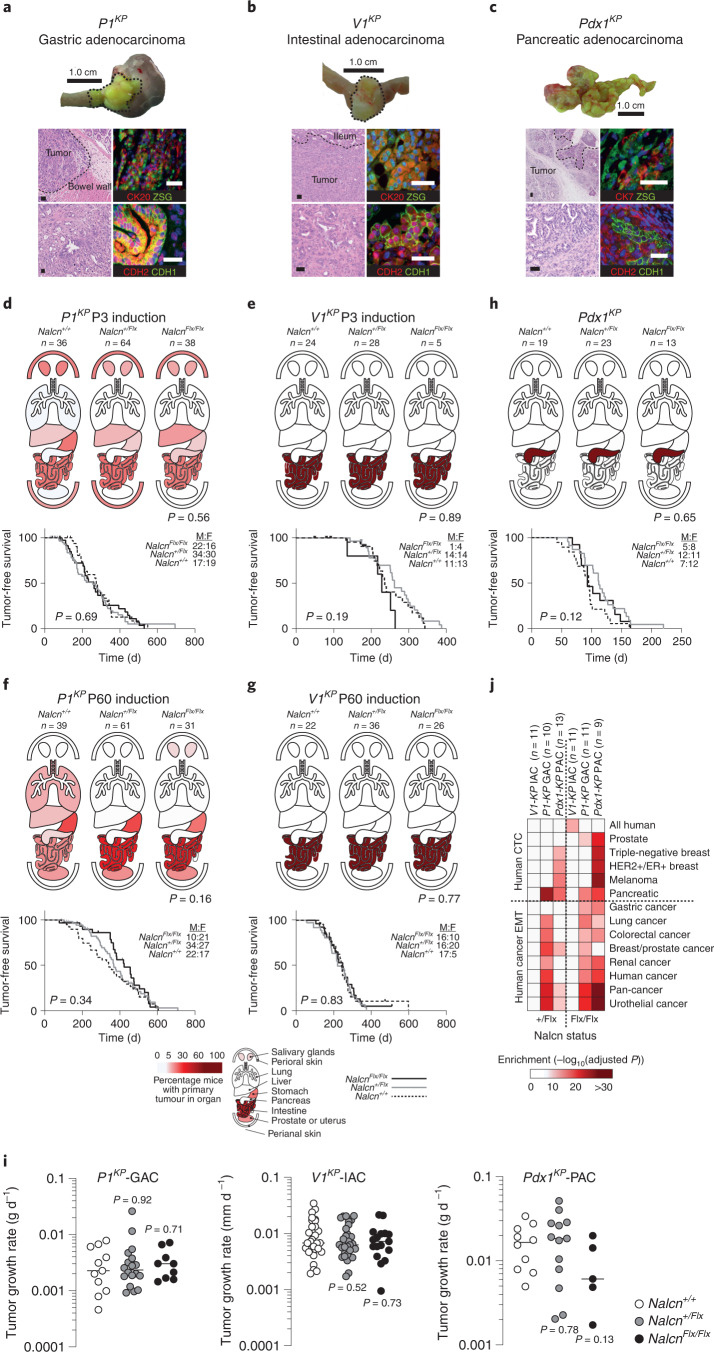
To study how Nalcn loss-of-function impacts cancer initiation and progression in intact tissues, we generated mice harboring a conditional Nalcn allele (NalcnFlx; Extended Data Fig. 2). These mice were bred with P1KP, Villin1-CreERT2;KrasG12D;Trp53Flx/Flx (V1KP) or Pdx1-Cre;KrasG12D;Trp53Flx/+ (Pdx1KP) mice to produce equivalent numbers of male and female mice that were either Nalcn wild-type (Nalcn+/+), Nalcn+/Flx or NalcnFlx/Flx (total n = 551; Supplementary Table 9). All mice carried the Rosa26-ZsGreen (Rosa26ZSG) lineage-tracing allele. Cancers in V1KP and Pdx1KP mice are restricted by Cre expression to the intestine25,26 and pancreas27,28, respectively. Prom1CreERT2/LacZ is expressed by a variety of stem/progenitor cells and induces tumors of the small intestine, liver, lung, salivary glands, prostate, uterus, skin and stomach in P1KP mice15,29. Because tissues can display age-dependent susceptibility to transformation15 we activated Cre-recombination in P1KP and V1KP mice using tamoxifen at postnatal day 3 (P3) or P60. As expected, V1KP (n = 127/141) and Pdx1KP (n = 55/55) mice developed intestinal and pancreatic tumors, respectively, whereas P1KP mice developed tumors in the stomach (n = 49/269), small intestine (n = 59/269) and other sites (n = 108/269)15,26,28; 99% (n = 212/214) of tumors in P1KP mice occurred as single primary tumor (Fig. 3a–g and Supplementary Table 9). Detailed macro- and microscopic analysis of tumors revealed no significant impact of age of induction, sex and/or Nalcn status on tumor incidence, type, tumor-free survival, tumor growth rate, immune cell infiltration, proliferation or other key primary tumor characteristics (Fig. 3, Extended Data Fig. 3a–c and Supplementary Tables 9–11). However, the transcriptomes of P1KP-GAC and Pdx1KP pancreatic adenocarcinomas (Pdx1KP-PACs) were enriched for genes associated with human CTCs and EMT (Fig. 3j).
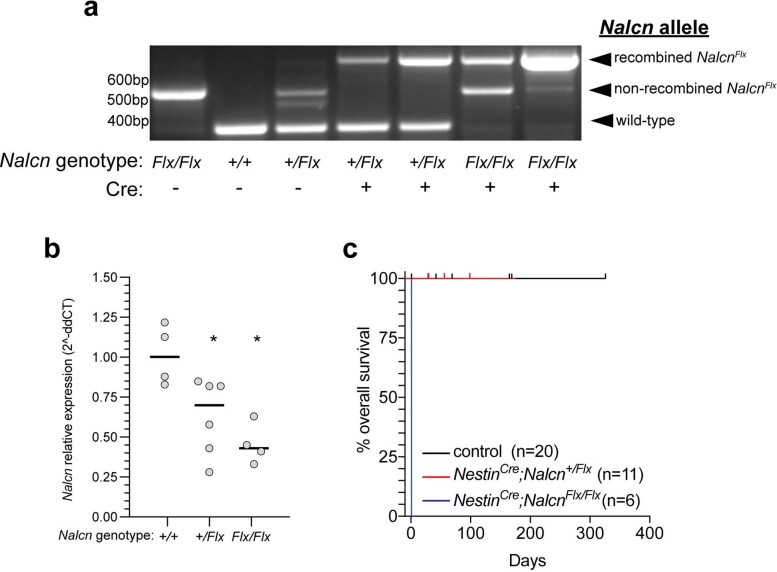
Extended Data Fig. 2. Recombination of the NalcnFlx conditional allele deletes the gene in vivo.
(a) Polymerase chain reaction (PCR) products derived from brains of Nalcn+/+, Nalcn+/Flx, or NalcnFlx/Flx mice with or without the NestinCre allele. (b) Real-time reverse transcriptase PCR analysis of Nalcn RNA expression in brains of Nalcn+/+ (n = 4), Nalcn+/Flx (n = 6), or NalcnFlx/Flx (n = 4) mice carrying the NestinCre allele. bar=median (*p = 0.0190 Nalcn+/Flx, *p = 0.0286 NalcnFlx/Flx; two-tailed Mann-Whitney U Test). (c) Similar to germline deletion of Nalcn, homozygous deletion of Nalcn from the brains of NestinCre;NalcnFlx/Flx (n = 6) mice was lethal at birth due to respiratory arrest, providing functional validation of Nalcn deletion. control (n = 20) and NestinCre;Nalcn+/Flx (n = 11).
Fig. 3. Nalcn deletion does not impact the incidence, tumor-free survival or growth rates of P1KP, V1KP or Pdx1KP primary tumors.
a–c Tumors and representative photomicrographs (H&E from all tumors (left; Supplementary Table 9) and dual immunofluorescence from five independent tumors each (right)) for lineage tracing (ZSG), epithelial (CK7, CK20) and EMT markers (CDH2, CDH1) of P1KP-GAC (a), V1KP-IAC (b) and Pdx1KP-PAC (c). Scale bar, 50 μm. Single-channel images are shown in Supplementary Fig. 1. d–g, Upper: organ heatmaps of tumor incidence in P1KP at P3 and V1KP at mice of each Nalcn genotype recombined at P3 (d,e) or P60 (f,g). Lower: survival curves of mice in each cohort. Male to female ration (M:F) is shown. P1KP P3, P = 0.6912; P1KP P60, P = 0.3897; V1KP P3, P = 0.1900; and V1KP P60, P = 0.8301. Mantel–Cox test. h, Organ primary tumor heatmaps and survival curves of Pdx1KP mice (P = 0.1095). Mantel–Cox test. Source data for d–h are given in Supplementary Table 9. i, Growth rates of P1KP-GAC (n = 38), V1KP-IAC (n = 57) and Pdx1KP-PAC (n = 28) tumors. Two-tailed Mann–Whitney U-tests revealed no significant difference in growth rates among tumors with different Nalcn genotypes P1KP-GAC: Nalcn+/+ (n = 11) versus Nalcn+/Flx (n = 18; P = 0.912), versus NalcnFlx/Flx (n = 9; P = 0.7103). V1KP-IAC: Nalcn+/+ (n = 16) versus Nalcn+/Flx (n = 25; P = 0.5169), versus NalcnFlx/Flx (n = 16; P = 0.7309). Pdx1KP-PAC: Nalcn+/+ (n = 10) versus Nalcn+/Flx (n = 13; P = 0.7844), versus NalcnFlx/Flx (n = 5; P = 0.1292). Bar, median. Source data are given in Supplementary Table 10. j, Gene set enrichment analyses of transcriptomes of Nalcn+/Flx and NalcnFlx/Flx P1KP-GAC, V1KP-IAC and Pdx1KP-PAC versus Nalcn+/+ tumors.
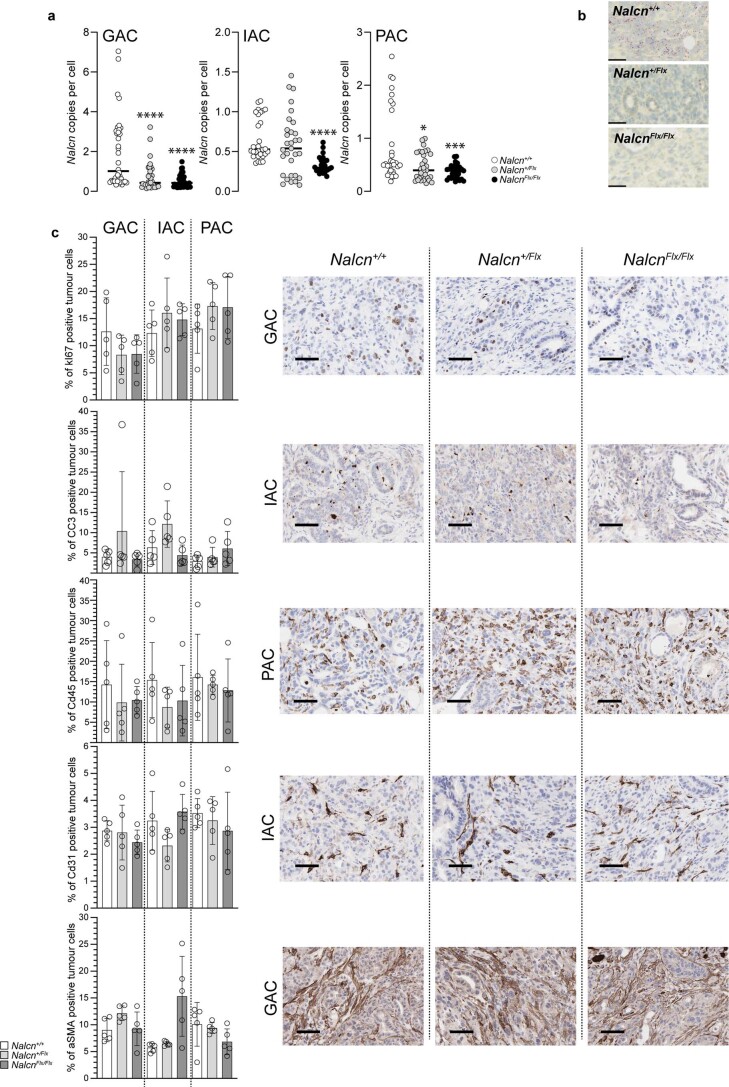
Extended Data Fig. 3. Nalcn deletion does not affect cell proliferation, apoptosis, immune-infiltration, vasculature or ASMA expression in primary tumours in P1KP, V1KP or Pdx1KP mice.
(a) HALO-quantification of Nalcn mRNA transcripts per cell detected by RNA-scope analysis in mouse gastric (GAC), intestinal (IAC) and pancreatic (PAC) adenocarcinomas of the indicated Nalcn genotype (bar=median; *p = 0.0294; ***p = 0.0004; ****=p < 0.0001, two-tailed Mann-Whitney test). Data are tumour fields (5–8 images per tumour) from n = 5 tumours for each Nalcn genotype of P1KP-GAC, V1KP-IAC and Pdx1KP-PAC mice (total n = 45 unique tumours, 289 unique tumour fields). (b) Representative photomicrographs of Nalcn RNA in situ hybridization in GACs (n = 15 biologically distinct tumours, 100 tumour fields) of the indicated Nalcn genotype (scale=50 μm). (c) Left in each is HALO-quantification (Data are mean ± SD) of immunohistochemically-detected tumour cell expression of MKI67 (proliferation), cleaved Caspase-3 (CC3; apoptosis), CD45 (immune cell infiltration), CD31 (endothelial cells) and alpha-smooth muscle actin ASMA; stroma) in five complete biologically independent tumour fields for each Nalcn genotype of P1KP-GAC, V1KP-IAC and Pdx1KP-PAC mice (total n = 45 unique tumours). Two-tailed Mann-Whitney U tests revealed no significant difference in these markers among tumours with different Nalcn genotypes. P-values GAC, IAC, PAC of Nalcn+/+ vs Nalcn+/Flx, Nalcn+/+ vs NalcnFlx/Flx, respectively: KI67 (0.4206, 0.4206, 0.4206, 0.5476, 0.2222, 0.5476), CC3 (0.9999, 0.5476, 0.0952, 0.5476, 0.9999, 0.2222), CD45(0.6905, 0.8413, 0.1508, 0.3095, 0.6905, 0.8413), ASMA(0.0556, 0.8413, 0.3095, 0.0556, 0.2222, 0.1508), CD31(0.9999, 0.0952, 0.0952, 0.4206, 0.8413, 0.1508). Right in each are exemplar photomicrographs of the indicated marker in the indicated tumour type (scale=50um).
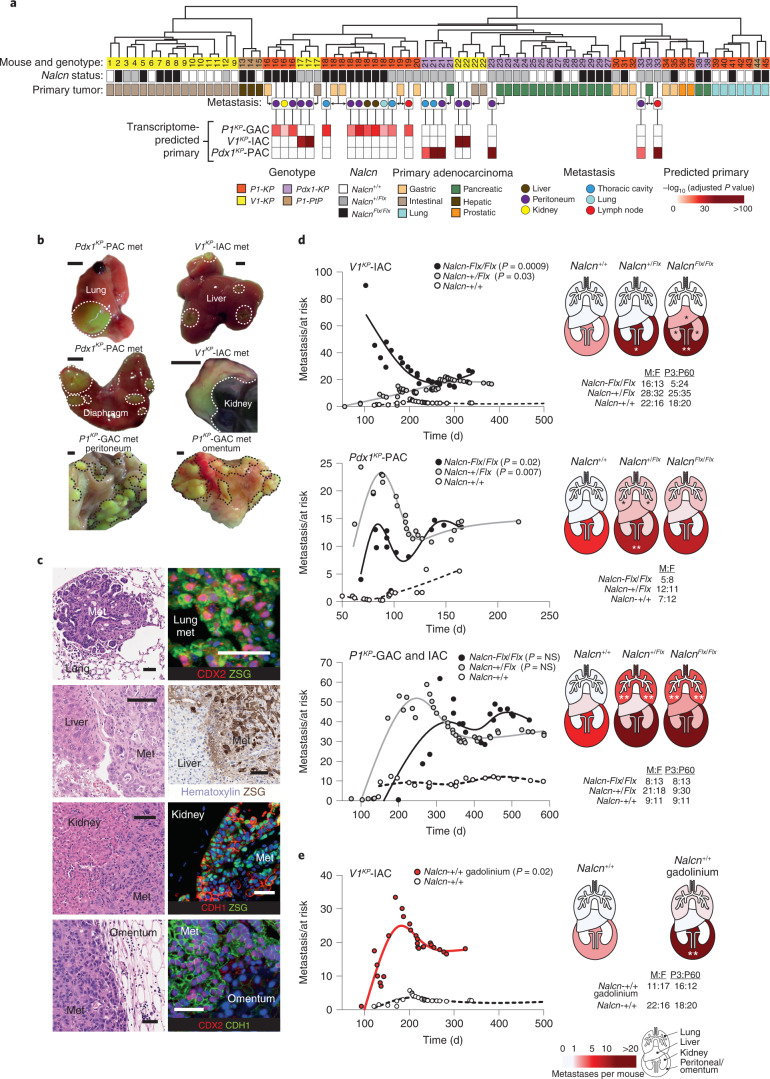
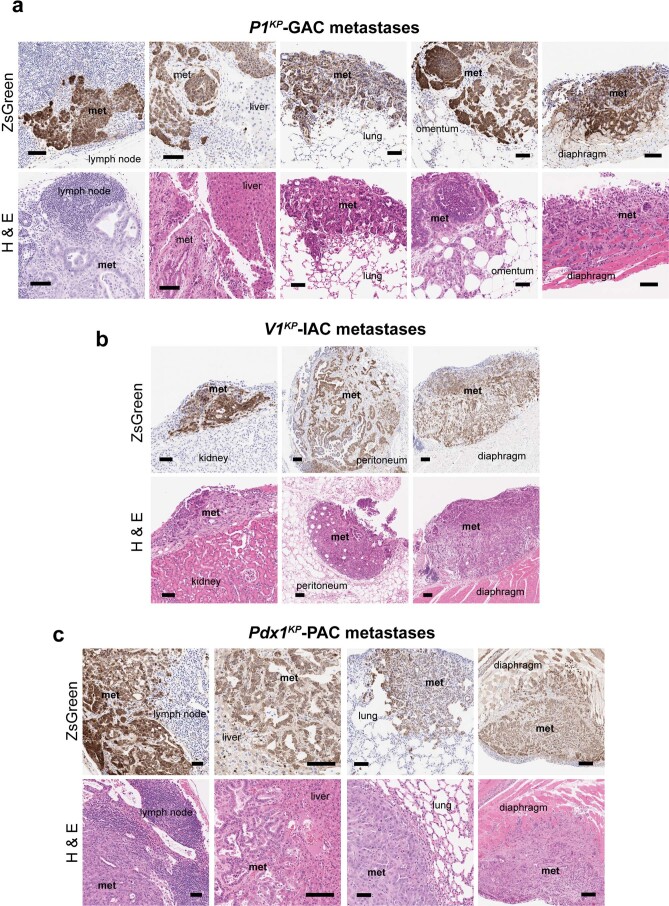
In keeping with these transcriptomic changes, deletion of Nalcn dramatically increased cancer metastasis in P1KP, V1KP and Pdx1KP mice (Fig. 4a–d, Extended Data Fig. 4 and Supplementary Table 12). Metastatic and primary tumors were distinguished from one another by combined histology review, cosegregation of ‘matched’ primary and secondary tumor transcriptomes by unsupervised hierarchical clustering, and enrichment of histology-predicted primary tumor gene sets within metastatic tumor transcriptomes (Fig. 4a,c and Extended Data Fig. 4). V1KP intestinal adenocarcinomas (V1KP-IACs, n = 27 mice) and Pdx1KP-PACs (n = 19 mice) in Nalcn+/+ mice, produced 2.82 ± 4.88 (mean ± s.e.m.) and 5.53 ± 4.02 metastases per mouse, respectively (Fig. 4d and Supplementary Tables 9 and 12). In stark contrast, these same tumors in V1KP;Nalcn+/Flx (n = 51), V1KP;NalcnFlx/Flx (n = 26), Pdx1KP;Nalcn+/Flx (n = 23) and Pdx1KP;NalcnFlx/Flx (n = 13) mice, produced 16.82 ± 5.69 (two-tailed Mann–Whitney U-test, P = 0.03 relative to Nalcn+/+), 26.04 ± 10.18 (P = 0.0009), 15.04 ± 3.62 (P = 0.007) and 13.46 ± 5.01 (P = 0.02) metastases per mouse, respectively. Nalcn deletion from V1KP-IACs increased metastasis in particular to the peritoneum, kidneys and liver: Nalcn deletion from Pdx1KP-PACs increased metastasis to the peritoneum and lungs (Fig. 4d). Nalcn deletion also increased metastasis of IAC and GAC in P1KP mice (n = 80) from 11.60 ± 3.45 metastases per P1KP;Nalcn+/+ mouse to 42.21 ± 11.23 metastases per P1KP;Nalcn+/Flx mouse and 40.24.0 ± 15.51 metastases per P1KP;NalcnFlx/Flx mouse (Fig. 4d and Supplementary Tables 9 and 12).
Fig. 4. NALCN loss-of-function increases tumor metastasis.
a, Unsupervised hierarchical clustering of P1KP (GAC, n = 10; lung adenocarcinoma, n = 6; prostatic adenocarcinoma, n = 2), V1KP (IAC, n = 19), Pdx1KP (PAC, n = 13) and P1;PtenFlx/Flx;Trp53Flx/Flx (P1PtP) (hepatobiliary, n = 3; lung adenocarcinoma, n = 1) primary tumors and metastatic (liver, n = 2; peritoneum, n = 11; kidney, n = 1; thoracic cavity, n = 4; lung, n = 1; lymph node, n = 2) tumors. Heatmap reports enrichment of primary tumor transcriptomes in metastatic tumors. b, Exemplar ZSG+ metastatic tumors (met, outlined). Scale bar, 0.5 cm. c, Photomicrographs (H&E (left) and immunohistochemistry/fluorescence(right)) of the metastases in b. Scale bar, 50 μm. All enumerated metastases were evaluated using H&E (full list is given in Supplementary Table 9; n = 7,076 metastases); n = 59 metastases were evaluated by ZSG for IHC and n = 20 metastases were evaluated by immunofluorescence. Single-channel images are shown in Supplementary Fig. 1. d, Left: cumulative total number of adenocarcinoma metastases per mouse post Cre-recombination (two-tailed Mann–Whitney U-test, total tumor burden in Nalcn-deleted versus wild-type mice; Supplementary Table 9). Right: total metastases per mouse in anatomical regions. Male/female (M:F) and P3/P60 mice are shown. V1KP IAC for individual organs: liver, *P = 0.0371 (NalcnFlx/Flx); kidney, *P = 0.0229 (NalcnFlx/Flx); and peritoneum, *P = 0.0492 (Nalcn+/Flx) and **P = 0.0015 (NalcnFlx/Flx). Pdx1KP PAC individual organs: lung, *P = 0.0328 (Nalcn+/Flx); and peritoneum, **P = 0.0050 (Nalcn+/Flx). P1KP GAC and IAC individual organs: lung, **P = 0.0085 (Nalcn+/Flx) and **P = 0.0048 (NalcnFlx/Flx). e, Metastatic burden and organ metastases in V1KP-IAC gadolinium or control treated mice. **P = 0.0090, two-tailed Mann–Whitney U-test.
Extended Data Fig. 4. Metastases of P1KP-GAC, V1KP-IAC and Pdx1KP-PAC.
Photomicrographs of (a) P1KP-GAC, (b) V1KP-IAC and (c) Pdx1KP-PAC metastases to the indicated tissues. Top in each, immunohistochemistry of ZsGreen staining. Bottom in each, haematoxlin and eosin (H & E) stain (scale=100um). All enumerated metastases were evaluated by H&E (full list Supplementary Table 7; n = 7,076 metastases) n = 59 metastases evaluated by ZSG for IHC.
To further validate Nalcn loss-of-function as a driver of cancer metastasis, we treated additional cohorts of V1KP;Nalcn+/+ (n = 37), V1KP;Nalcn+/Flx (n = 17) and V1KP;NalcnFlx/Flx (n = 8) mice with GdCl3 (2 μg per kg (body weight) per week). IACs in GdCl3-treated V1KP;Nalcn+/+ mice (n = 28) produced 18.32 ± 5.95 metastases per mouse compared with only 2.82 ± 4.88 in controls (P = 0.02; Fig. 4e and Supplementary Table 12). However, GdCl3 did not increase metastasis in either V1KP;Nalcn+/Flx or V1KP;NalcnFlx/Flx mice, confirming that the agent phenocopied the Nalcn-deletion metastatic phenotype, specifically.
NALCN regulates CTCs
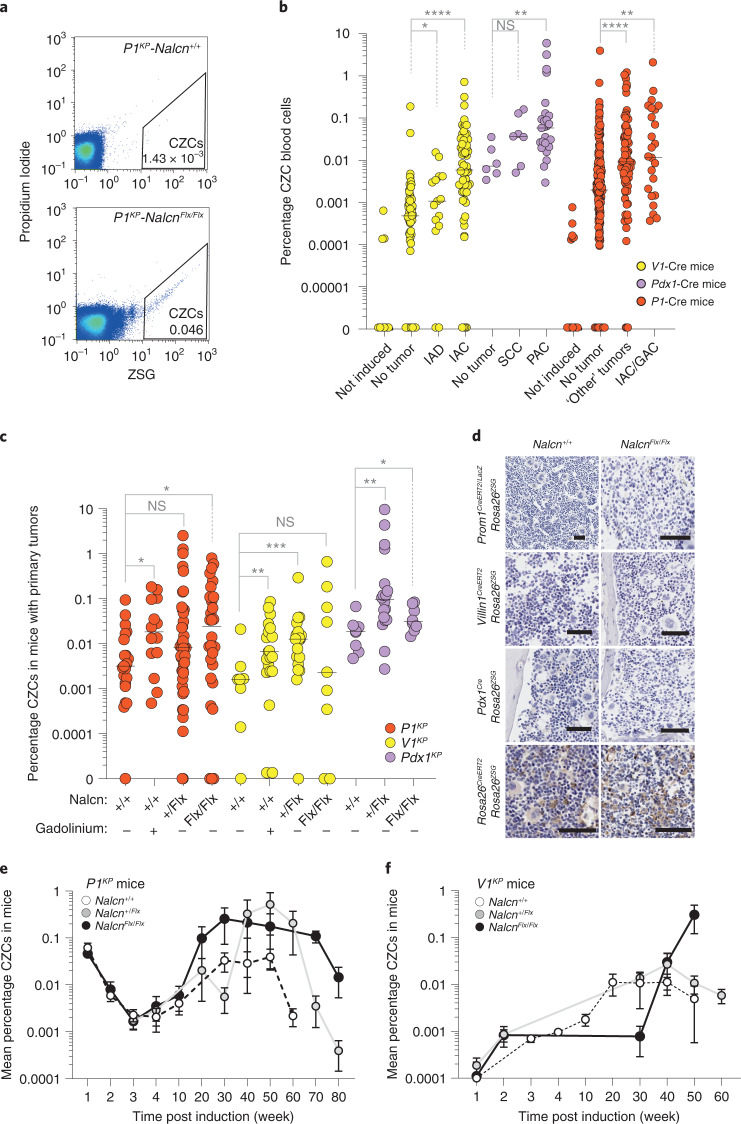
Because Nalcn deletion increased tumor metastasis and the expression by GACs, IACs and PACs of genes enriched in human CTC transcriptomes (Fig. 3j), we reasoned that Nalcn might regulate the release of CTCs from primary tumors: CTCs are shed from tumors into the blood as precursors of metastasis30. To test this, nucleated, GAC, IAC and PAC cells that had been genetically tagged by recombination of the Rosa26ZSG lineage-tracing allele in the corresponding epithelium were isolated from whole blood and quantified using ZsGreen (ZSG)-fluorescence-activated cell sorting (FACS). Serial, peripheral blood samples taken from Prom1CreERT2/LacZ (n = 397), Villin-1CreERT2 (n = 162) or Pdx1Cre (n = 40) mice that carried the Rosa26ZSG allele and various combinations of oncogenic and NalcnFlx alleles were analyzed (Supplementary Table 13). An average (± s.e.m.) of 3.8 × 103 ± 0.9 × 103 circulating ZSG+ cells (CZCs) per ml of blood (0.066% ± 0.02% total cells) were isolated from all mice after an average of 254 ± 9.1 d following Cre-recombination (Fig. 5a–c and Supplementary Table 13). Across all three Cre-lines, the number of CZCs was highly correlated with both the presence of a primary tumor (Fig. 5b) and the total number of metastases (multiple linear regression, T = 10.43, P = 0.000043; Supplementary Table 13), independent of mouse sex or age of induction. Nalcn deletion, or GdCl3 treatment, significantly increased the level of CZCs in tumor-bearing P1KP, V1KP and Pdx1KP mice (Fig. 5c). Because neither Prom1CreERT2/LacZ, Villin-1CreERT2 nor Pdx1Cre recombine hematopoeitic cells in the bone marrow (Fig. 5d), these data strongly suggest that CZCs are CTCs shed from primary tumors through a process regulated by NALCN. In the immediate 5-week period following tamoxifen recombination, similar levels of circulating CZCs were observed among P1KP and V1KP mice that were Nalcn+/+, Nalcn+/Flx or NalcnFlx/Flx, suggesting that Nalcn regulates cell shedding as a late event (Fig. 5e,f and Supplementary Table 13); however, the time taken for lineage tracing to reach steady state in our mice may underestimate CZC numbers at early time points.
Fig. 5. NALCN loss-of-function increases nucleated CZCs in P1KP, V1KP and Pdx1KP mice.
a, FACS profiles gating CZCs in blood samples of P1KP Nalcn+/+ and NalcnFlx/Flx mice (per cent nucleated cells). Gating strategy is shown in Supplementary Fig. 2. b, Scatter plot of CZCs (per cent of total nucleated blood cells) of Prom1CreERT2/LacZ (n = 397), Villin-1CreERT2 (n = 162) or Pdx1Cre (n = 40) mice that did, or did not, contain a primary tumor. Data are biologically independent peripheral blood samples. Bar, median. V1-Cre: *P = 0.0499, ****P < 0.0001; Pdx1-Cre: not significant (NS) P = 0.0513, **P = 0.0033; P1-Cre: **P = 0.0033, ****P < 0.0001; two-tailed Mann–Whitney U-test. Source data are available in Supplementary Table 13. c, Scatter plot of CZCs according to genotype and gadolinium treatment in tumor-bearing animals. Data are biologically independent peripheral blood samples. Bar, median. P1KP (n = 112): *P = 0.02, NS P = 0.1204 ; V1KP (n = 64): **P = 0.0088, ***P = 0.0004, NS P = 0.4213; Pdx1KP (n = 34): *P = 0.0499, **P = 0.0027; two-tailed Mann–Whitney U-test. Source data are available in Supplementary Table 13. d, Representative photomicrographs of ZSG immunohistochemistry of bone marrow of mice of the indicated genotype at a minimum of 100 d post Cre-recombination. Scale, 100 μm. Three mice were evaluated for each Cre strain. e,f, FACS quantification of CZCs in P1KP (Nalcn+/+, n = 11; Nalcn+/Flx, n = 4; NalcnFlx/Flx, n = 6) (e) and V1KP (Nalcn+/+, n = 9; Nalcn+/Flx, n = 4; NalcnFlx/Flx, n = 4) (f) mice (mean ± s.e.m.) from 1-week post tamoxifen induction. Source data are given in Supplementary Table 13.
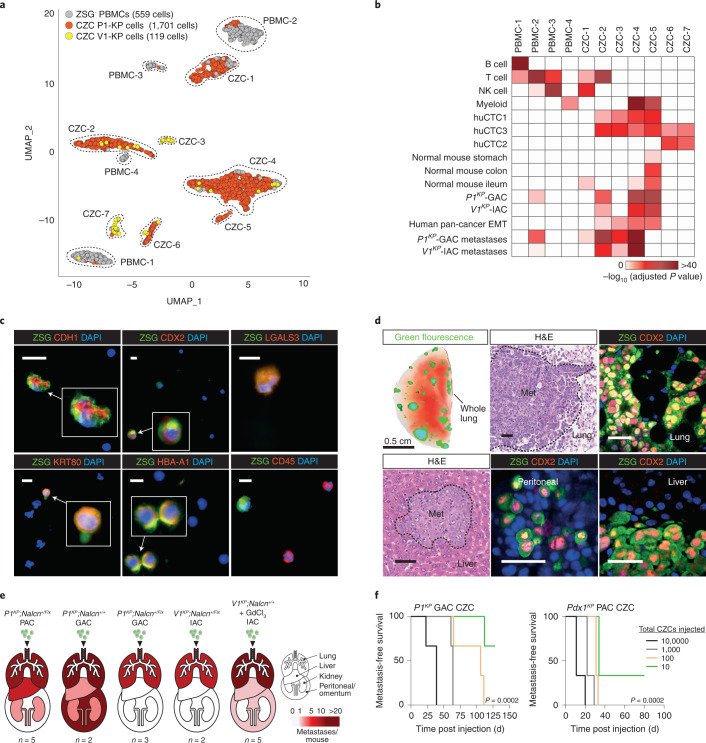
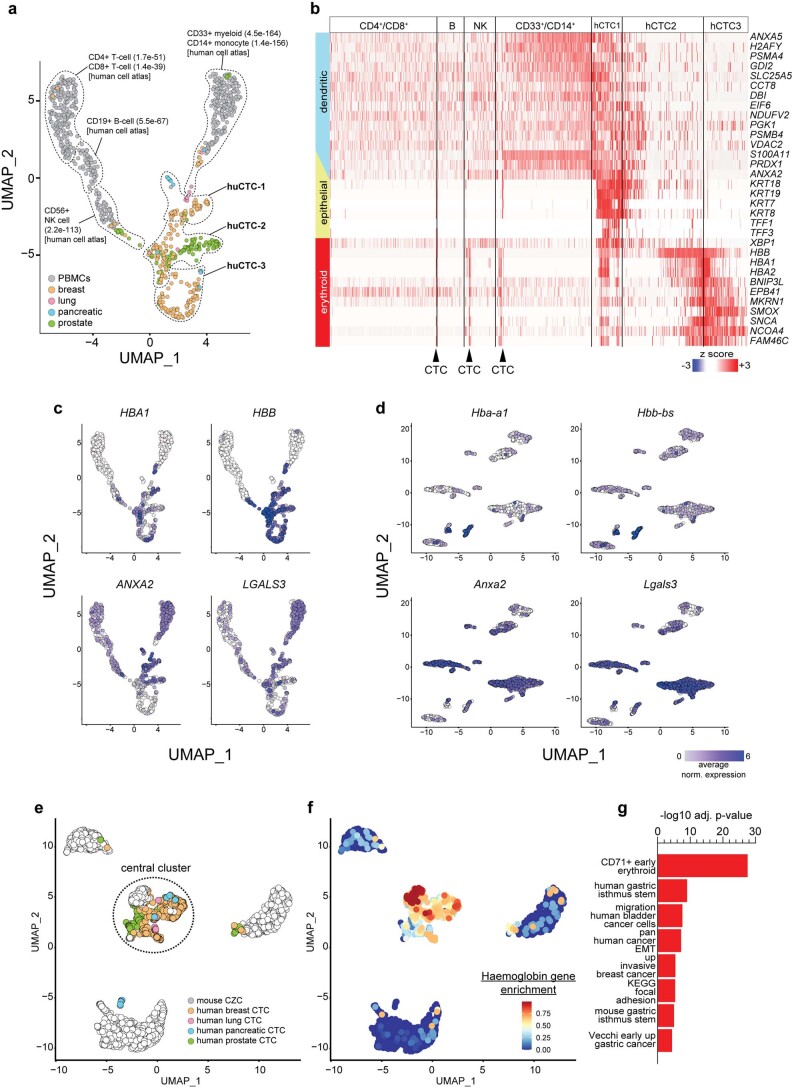
To better understand the origin of CZCs, we generated single-cell RNA sequence profiles of CZCs isolated from mice with P1KP-GAC (n = 1,701 cells) or V1KP-IAC (n = 119), as well as peripheral blood mononuclear cells (PBMCs, n = 559; Fig. 6a), and compared these with published single-cell RNA sequence profiles of human breast, lung, pancreatic and prostate CTCs (n = 360) and PBMCs (n = 500)31–36. Human CTCs comprised three overlapping clusters (Extended Data Fig. 5a–c and Supplementary Tables 14 and 15): ‘huCTC1’ (enriched with cancer metastasis, EMT and epithelial gene sets); huCTC3 (enriched with early-erythroid and EMT gene sets); and huCTC2 (sharing profiles of huCTC1 and huCTC3). huCTC1–3 expressed β-globin (HBB)—a survival factor for human CTCs33—as well as HBA1, HBA2 and HBD. Mouse CZCs formed seven clusters whose transcriptomes significantly matched huCTC1 (mCZC2–7), huCTC2 (mCZC2, 3, 5–7) and huCTC3 (mCZC2–7), and included orthologs of HBA1, HBA2 (Hba-a1, Hba-a2), HBB (Hbb-bs, Hbb-bt), ANXA2 and LGALS3, as well as genes expressed in normal and malignant stomach and small intestine (Fig. 6a,b, Extended Data Fig. 5c–g and Supplementary Tables 16 and 17). Normalization and Uniform Manifold Approximation and Projections (UMAP) of all single-cell RNA sequence profiles also revealed significant overlap in mouse CZC and human CTC transcriptomes, especially those enriched for CD71+ erythroid genes (Extended Data Fig. 5e–g and Supplementary Table 18). Coimmunofluorescence of peripheral blood smears taken from mice with V1KP-IAC and P1KP-GAC confirmed CZC expression of HBA-A1, LGALS3, and epithelial cell markers (KRT80, CDH1) and CDX2 that marks intestinal epithelium (Fig. 6c). PBMCs did not express these markers but did express markers of PBMCs (for example, CD45).
Fig. 6. Nucleated CZCs in P1KP, V1KP and Pdx1KP mice are CTCs.
a, UMAP of SCS profiles of CZCs (n = 1,820) and PBMCs (n = 559). b, Gene set enrichment from 2,086 gene sets in UMAP clusters in a. c, Coimmunofluorescence of CZCs and PBMCs in P1KP (upper) and V1KP (lower) mice (ZSG; scale bar, 10 μm). Representative photomicrographs of 22 cells identified across n = 20 blood films assessed from n = 5 tumor-bearing animals. d, Autofluorescence of Pdx1KP-PAC CZC metastases in whole lung of recipient immunocompromised mouse (upper left; scale bar, 0.5 cm). Other images show H&E (representative image of 3,061 metastases evaluated) or coimmunofluorescence of metastases (representative images of 28 metastases evaluated) of P1KP-GAC or V1KP-IAC CZC metastases in recipient mice (scale bar, 50 μm). Single-channel images are shown in Supplementary Fig. 1. e, Total metastases per organ in recipient mice injected with 25,000 CZCs. P1KP Nalcn+/Flx PAC, n = 5 mice; P1KP Nalcn+/+ GAC, n = 2 mice; P1KP Nalcn+/Flx GAC, n = 3 mice; V1KP Nalcn+/Flx IAC, n = 2 mice; V1KP Nalcn+/+ + GdCl3 IAC, n = 5 mice. Source data are given in Supplementary Table 19. f, Metastasis-free survival of immunodeficient NOD scid gamma recipient mice injected with different numbers (10,000, 1,000, 100 or 10) of P1KP GAC or Pdx1KP PAC CZCs (n = 3 mice for each condition). ***P = 0.0002 Mantel–Cox statistic. Source data are available in Supplementary Table 19.
Extended Data Fig. 5. Human circulating tumour cells (CTCs) and peripheral blood mononuclear cells (PBMCs).
(a) UMAP of single cell RNA sequencing (SCS) profiles of human CTCs and PBMCs (see main text for SCS sources). Genesets enriched in the indicated SCS clusters are shown with adjusted p-value for enrichment in parenthesis. (b) Heatmap of indicated gene expression from relevant genesets enriched in each cell from each cluster in (a). (c) Feature plots of exemplar genes enriched in human CTCs in (a). (d) Mouse orthologues of human genes in (c) mapped onto the UMAP of mouse CZCs and PBMCs in main Fig. 3b. (e) UMAPs of SCS profiles of common orthologues expressed in human CTCs and mouse tCZCs. (f) Enrichment of haemoglobin gene expression in UMAP shown in (e). (g) Geneset enrichments in the dotted-line enclosed, central cluster relative to the other SCS profiles is reported in (e).
To test directly whether CZCs possess metastatic potential, we injected separate aliquots of 25,000 CZCs isolated from mice with P1KP-PAC, P1KP-GAC or V1KP-IAC into the tail veins of immunocompromised mice. Within 75 d, all mice developed numerous ZSG+ metastases in the lungs, liver, kidneys and/or peritoneum (Fig. 6d,e and Supplementary Table 19). Similar studies with increasing cell dilutions showed that as few as ten CZCs were required to generate metastasis (Fig. 6f and Supplementary Table 19). Thus, CZCs are highly enriched for CTCs that recapitulate the transcriptome of human CTCs and are shed into the peripheral blood through a process regulated by Nalcn.
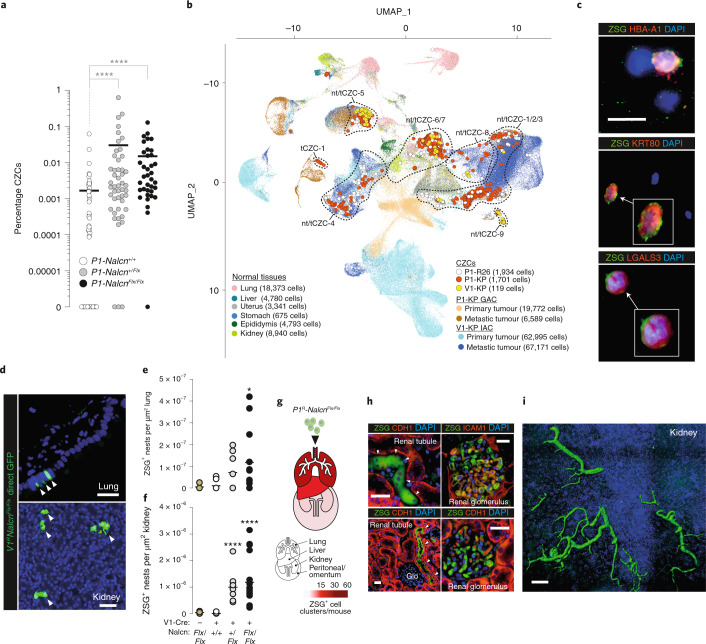
NALCN and circulating noncancer cells
Preventing CTC shedding into the peripheral blood could stop metastasis, but disentangling this process from the complex cascade of tumorigenesis has proved challenging. Deletion of Nalcn from freshly isolated P1;NalcnFlx/Flx gastric stem cells that lacked oncogenic alleles, rapidly upregulated genes associated with invasion (for example, Mmp7, Mmp9, Mmp10 and Mmp19) and gastric EMT (for example, Zeb1, Fstl1, Sparc, Sfrp4, Cdh6 and Timp3; Supplementary Tables 20 and 21), suggesting NALCN might regulate cell shedding from solid tissues independent of transformation. To test this, we looked for CZCs in the peripheral blood of Prom1CreERT2/LacZ;Rosa26ZSG;Nalcn+/+ (P1RNalcn+/+, n = 87), P1RNalcn+/Flx (n = 50) and P1RNalcnFlx/Flx (n = 37) mice that lacked oncogenic alleles and never developed tumors (Supplementary Table 13). Remarkably, deletion of Nalcn increased the numbers of CZCs in these mice to levels similar to those observed in tumor-bearing animals (Figs. 5b,c and 7a). Single-cell RNA sequencing (SCS) profiles of CZCs isolated from nontumor-bearing (ntCZC) mice co-clustered with CZCs from tumor-bearing animals (tCZC; Fig. 7b). The great majority of tCZC and ntCZC SCSs did not cluster with SCS profiles of primary IACs, GACs or normal tissues, but with SCS profiles of metastases (Fig. 7b and Supplementary Table 22). SCS profiles of both tCZCs and ntCZCs matched those of human CTCs and, similar to human CTCs2, expressed genes associated with stem and progenitor cells; although tCZCs were relatively more enriched for metastasis and invasion-associated gene sets (Extended Data Fig. 6a and Supplementary Tables 23 and 24). Coimmunofluorescence of blood smears confirmed that both ntCZCs and tCZCs share markers of huCTCs, including HBA-A1 (Figs. 6c and 7c).
Fig. 7. NALCN loss-of-function increases shedding of ntCZCs.
a, ntCZCs identified in individual nontumor-bearing P1RNalcn+/+ (n = 87), P1RNalcn+/Flx (n = 50) and P1RNalcnFlx/Flx (n = 37) mice. Bar, median. ****P < 0.0001, two-tailed Mann–Whitney U-test. Source data are available in Supplementary Table 13. b, UMAP of 201,183 SCS profiles of PBMCs, tCZCs and ntCZCs as well as cells derived from the indicated normal and malignant mouse tissues. c, Coimmunofluorescence of ntCZCs and PBMCs in peripheral blood smears of P1RNalcnFlx/Flx mice (ZSG; scale bar, 10 μm). Representative photomicrographs of 11 cells identified in n = 20 blood films from n = 4 mice. Single-channel images are shown in Supplementary Fig. 1. d–f, Direct ZSG-immunofluorescence photomicrographs of ZSG+ cells in lung and kidney (scale bar, 50 μm) (d), and enumerated in lung (no Cre, n = 2 mice, 5 lung lobes; Nalcn+/+, n = 3 mice, 9 lung lobes; Nalcn+/Flx, n = 3 mice, 8 lung lobes; NalcnFlx/Flx, n = 5 mice, 12 lung lobes; NS P = 0.1312, *P = 0.0168, two-tailed Mann–Whitney U-test) (e) and kidney (no Cre, n = 2 mice, 4 kidney sections; Nalcn+/+, n = 3 mice, 11 kidney sections; Nalcn+/Flx, n = 3 mice, 10 kidney sections; NalcnFlx/Flx, n = 5 mice, 18 kidney sections; ****P < 0.0001, two-tailed Mann–Whitney U-test) (f). g, Organ heatmap of total numbers of ZSG+ cell clusters per mouse identified in organs of recipient mice injected with P1RNalcnFlx/Flx ntCZCs. h, Coimmunofluorescence of P1RNalcnFlx/Flx ntCZCs (arrows) incorporated into the kidneys of recipient mice (arrows indicated ZSG+ cells; scale bar, 50 μm). Representative photomicrograph of n = 5 ZSG rests identified in one tissue field from n = 5 mice. Single-channel images are shown in Supplementary Fig. 1. GLO, glomerulus. i, Confocal laser scanning microscope image of P1RNalcnFlx/Flx CZCs incorporated into the renal cortex of recipient mice. Scale bar, 100 μm. Representative image of n = 2 mouse kidneys assessed.
Extended Data Fig. 6. NALCN loss-of-function circulating non-tumour cells (ntCZCs) resemble human and mouse CTCs and embed in distant organs.
(a) Heatmap reporting geneset enrichment analysis in the UMAP clusters identified in main Fig. 7b. Test Genesets were derived from 2,086 different tissue and cell types including bulk RNAseq of mouse normal tissues and tumours, huCTC signatures, and mouse and human intestinal stem and mature cell signatures (see Methods). (b) ZSG immunohistochemistry of aged Pdx1RNalcn+/+ (top left) and Pdx1RNalcnFlx/Flx (bottom left) mouse lung bronchioles (scale=100um). Right, the number of ZSG+ cells/bronchiole in the lungs of Pdx1RNalcn+/+ (n = 2 mice, 6 lung lobes, 121 bronchiole) and Pdx1RNalcnFlx/Flx (n = 1 mouse, 4 lung lobes, 57 bronchioles). (bar=median; **p = 0.0051 two-tailed Mann-Whitney U Test). (c) Two-photon direct ZSG+ cell clusters detected in entire lung section of a Pdx1RNalcnFlx/Flx mouse. (d) Exemplar co-immunofluorescence of tail vein injected P1RNalcnFlx/Flx ntCZCs (arrows) incorporated into the organs of recipient mice (arrows indicated ZSG+ cells, scale bar=50um).
To understand the fate of ntCZCs, we looked for ZSG+ cells in the lungs and kidneys of aged V1R and Pdx1R Nalcn+/+, Nalcn+/Flx and/or NalcnFlx/Flx mice. Remarkably, ZSG+ cell clusters were readily detected in these organs in Nalcn-deleted animals, but were absent or detected at significantly lower levels in Nalcn+/+ mice, suggesting that ntCZCs traffic to, and embed within, distant organs (Fig. 7d–f and Extended Data Fig. 6b,c). To test this more directly, we injected separate aliquots of 25,000 ntCZCs isolated from P1RNalcnFlx/Flx mice into the tail veins of six immunocompromised mice. All recipient mice remained clinically well after an average of 100 d, but contained numerous ZSG+/Cdh1+/Icam1+ donor-cell clusters within their lungs, liver, kidneys and peritoneum at a frequency similar to metastatic tumors formed by tail-vein injections of tCZCs (Figs. 6e, 7g–i and Extended Data Fig. 6d). Trafficked ntCZCs formed apparently normal structures in target organs, the most extreme example being kidney glomeruli and tubules (Fig. 7h,i). Thus, NALCN regulates cell shedding from solid tissues independent of cancer, divorcing this process from tumorigenesis and unmasking an oncogene-independent metastatic pathway.
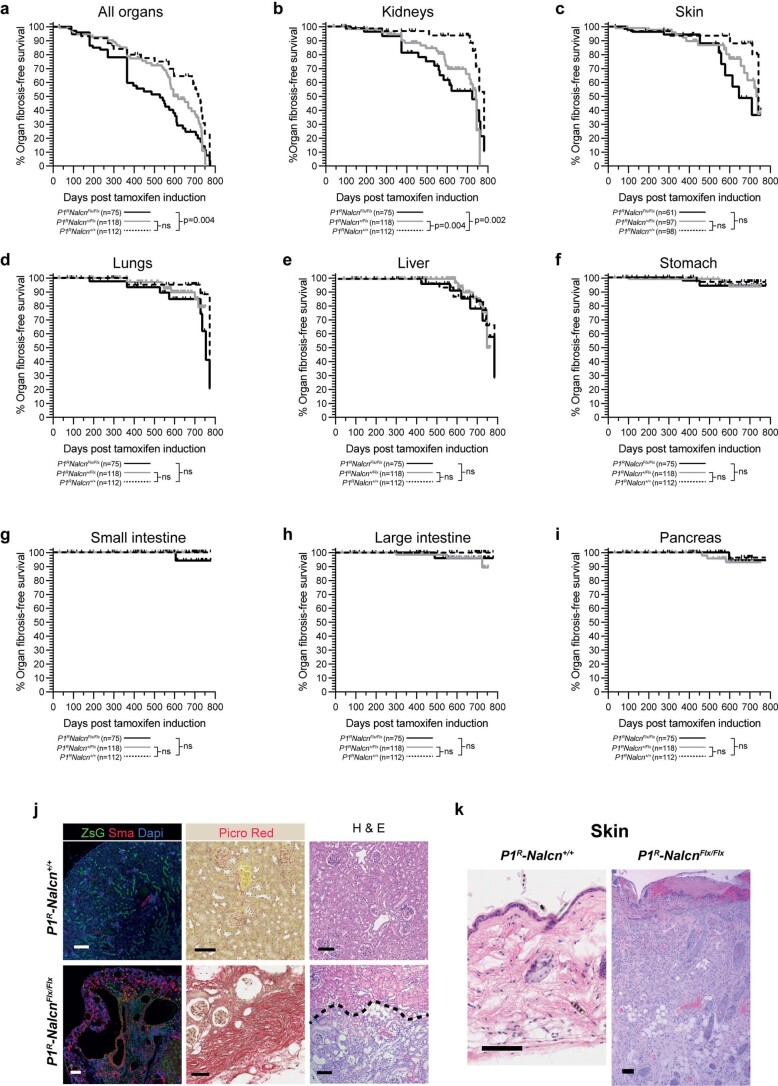
NALCN-blockade causes systemic fibrosis
Although P1RNalcn+/Flx (n = 118) and P1RNalcnFlx/Flx (n = 112) mice did not develop cancer, whole-body autopsy of these mice revealed severe kidney and skin fibrosis relative to P1RNalcn+/+ (n = 65) mice (Supplementary Table 25 and Extended Data Fig. 7). This pathology arose after ≥400 d and replicated that of gadolinium-induced systemic fibrosis (GISF), a debilitating condition manifested by severe organ fibrosis following administration of gadolinium-based contrast agents37. How gadolinium-based contrast agents cause GISF is unknown, but suggested mechanisms include tissue retention of gadolinium-based contrast agents and the mobilization and recruitment of bone marrow-derived fibrocytes38. Our data suggest strongly that blockade of the NALCN channel by gadolinium mobilizes epithelial cells in a variety of epithelial tissues that traffic to the kidney and other organs, eventually eliciting a fibrotic response, causing GISF.
Extended Data Fig. 7. Organ fibrosis following conditional deletion of Nalcn at P3 in P1R mice.
Fibrosis-free survival for all organs (a) or the indicated organs (b-i). P value reports the log-rank statistic (Mantel-Cox). The numbers of animals of each genotype are shown. p-values for each graph comparing P1RNalcn+/+ and P1RNalcn+/Flx and P1RNalcn+/+ and P1RNalcnFlx/Flx, respectively: All organs (0.0664, 0.0035), Kidneys (0.0037, 0.0022), Skin (0.1195, 0.0569), Lungs(0.3791, 0.1000), Liver(0.8846, 0.7250), Stomach(0.4938, 0.4225), Small intestine(>0.9999, 0.2348), Large intestine(0.1312, 0.2655), Pancreas(0.4764, 0.7571). (j) Photomicrographs of haematoxlin and eosin (H & E) and Picro-Sirus Red stain and co-immunofluorescence of ZsGreen, alpha-smooth muscle actin (ASMA) and Dapi in kidney from P1RNalcn+/+ and P1RNalcnFlx/Flx mice aged >400 days. Note in P1RNalcnFlx/Flx kidney: extensive fibrosis below the hashed line (H & E); marked Picro-Sirius Red staining indicating extensive fibrosis; ZsGreen recombination, gross distortion of normal kidney architecture and extensive alpha-SMA expression. (k) Photomicrographs of H & E stained skin from P1RNalcn+/+ and P1RNalcnFlx/Flx mice aged >400 days. Note in P1RNalcnFlx/Flx skin: ulceration and thickening of cornified layer, marked thickening of squamous cell layer and fibrosis of dermal layer. (scale 100um).
Discussion
Developing antimetastatic therapies has proven difficult because targets in primary tumors that drive metastasis have proved hard to find2. By divorcing the process of CTC shedding from ‘upstream’ tumorigenesis, our data unmask manipulation of NALCN function as a promising new approach to block metastasis. In particular, drugs capable of reopening the NALCN channel might be effective antimetastatic therapies. Precedent for this approach is provided by drugs that open the chloride channel mutated in cystic fibrosis39. If successful, such agents may also be useful for treating GISF.
It is important to note that our observations are based on deleting Nalcn from mouse tissues, whereas NALCN in human cancers is affected predominantly by nonsynonymous mutations. Although our in silico modeling suggests strongly that these cancer-associated mutations close the NALCN channel, it will be important to demonstrate this functionally by modeling nonsynonymous Nalcn mutations in vivo. These studies should also include testing in patient-derived xenografts of gastric, colon and other cancers to confirm that NALCN regulates trafficking of human as well as mouse cells.
Loss-of-function mutations in NALCN may also help explain various enigmatic features of human cancer. Metastases can emerge many years after removal of a localized cancer40, or in the absence of a primary tumor41. Loss of NALCN function in our mice caused an abundant and persistent shedding of cells that embed in distant organs, even in the absence of a primary tumor. Because human epithelial tissues contain fields of phenotypically normal cells that harbor oncogenic mutations42,43, then loss of NALCN function in these cells could provide a source of CTCs that form metastases in the absence of a primary tumor, or long after a primary tumor has been removed. It is likely that such cells would need to acquire additional mutations to form tumors at the metastatic site, compatible with the relative rarity of these phenomena. Our data may also explain why CTCs have been found in the bone marrow of patients who lack metastases. Although these cells could represent ‘dormant’ CTCs, as previously suggested3, equivalent to ntCZCs in our mice, they may be shed from nontransformed epithelia that have lost NALCN function, but not gained the ability to form metastatic tumors. Our serial analysis of CZCs in mice suggest that cell shedding following NALCN loss-of-function is a late, rather than early, event; although NALCN mutations could promote both linear and parallel progression models of cancer44.
Our data also provide clues as to how NALCN might regulate epithelial cell shedding. We observed upregulation of genes associated with EMT and invasion within 72 h of deleting Nalcn from normal gastric stem cells; suggesting that this channel might regulate gene transcription in a similar manner to that reported for calcium ion channels6,45. Our electrophysiology studies demonstrate that GAC cells possess a NALCN-mediated current. However, more detailed electrophysiology studies are required to determine the precise mechanism by which NALCN regulates gene expression and cell shedding and whether this involves maintenance of the resting membrane potential.
The development of renal and skin fibrosis reminiscent of GISF in aged Nalcn-deleted mice, pinpoint NALCN channel blockade as the likely cause of this debilitating condition. P1KP mice succumbed to cancer well before the onset of organ fibrosis in P1R mice, and Nalcn deletion in P1R mice did not induce stomach, intestine, lung, pancreas or liver fibrosis—principal sites of primary and metastatic tumors in P1KP mice. Thus, fibrosis is unlikely to have contributed to metastasis in Nalcn-deleted mice. However, because limited exposure to gadolinium can induce GISF in humans, it is a note of concern that gadolinium-contrast imaging of cancer patients could accelerate metastasis.
Methods
Culture of stomach stem cells
Gastric glands were isolated46 by perfusing mice with 30 mM EDTA/PBS, stomach removal and scraping pyloric mucosa into 10 mM EDTA/PBS at 4 °C. Dissociated, filtered and resuspended cells were placed in Matrigel (catalog number 354230, BD Biosciences) and culture medium: advanced DMEM/F12 (catalog number 31330038, Thermo Fisher Scientific), B27 (catalog number 12587010, Thermo Fisher Scientific), N2 (catalog number A1370701, Thermo Fisher Scientific), N-acetylcysteine (catalog number A9165, Sigma-Aldrich) and 10 nM gastrin (catalog number G9145, Sigma-Aldrich) containing growth factors (50 ng ml−1 EGF (PeproTech), 1 mg ml−1 R-spondin1 (catalog number 120-38, PeproTech), 100 ng ml−1 Noggin (catalog number 250-38, PeproTech), 100 ng ml−1 FGF10 (catalog number 100-26, PeproTech) and Wnt3A conditioned media (L Wnt-3A, catalog number ATCC-CRL-2647, American Type Culture Collection). Gastric spheres were passaged by dispase (catalog number D4818, Sigma-Aldrich) digestion and dissociation into single cells (StemPro Accutase, Life Technologies). Gadolinium (catalog number 439770, Sigma-Aldrich) was diluted in the culture medium and overlaid on Matrigel embedded cells (Supplementary Tables 26 and 27).
Lentiviral production and transduction
Nalcn-shRNA lentivirus was produced as described previously47. Three shRNAs per target (two open reading frames one 3′-untranslated region) were cloned into pFUGWH1-RFPTurbo and cotransfected with plasmids pVSV-G and pCMVd8.9 into 293FT (Thermo Fisher Scientific, catalog number R70007) cells. NALCN cDNA (NM_052867) was from OriGene (catalog number RC217074). In total 2 × 104 gastric cells were mixed with lentiviruses (20 particles per cell) plated in Matrigel. Transduced red fluorescence+ (shRNA) or green fluorescence+ (cDNA) cells were sorted using a Becton Dickinson Aria II Cell Sorter (Supplementary Tables 26 and 28).
Whole-cell electrophysiology
The NALCN channel current was measured as reported48. Whole-cell recordings were obtained from stomach tumor cells on 12-mm cover slips coated with Matrigel at a density of 25,000 cells per ml and superfused (2–3 ml min−1) with warm (30–32 °C) recording solution containing 120 mM NaCl, 5 mM CsCl, 2.5 mM KCl, 2 mM CaCl2, 2 mM MgCl2, 1.25 mM NaH2PO4, 26 mM NaHCO3, 20 mM glucose and 1 M tetrodotoxin (300–310 mOsm), with 95% O2/5% CO2. Patch pipettes (open pipette resistance, 3–4 MΩ) were filled with an internal solution containing 125 mM CsMeSO3, 2 mM CsCl, 10 mM HEPES, 0.1 mM EGTA, 4 mM MgATP, 0.3 mM NaGTP, 10 mM Na2 creatine phosphate, 5 mM QX-314 and 5 mM tetraethylammonium Cl (pH 7.4, adjusted with CsOH, 290–295 mOsm). Tetrodotoxin and QX-314 were included to block voltage-sensitive sodium channels in recorded cells, whereas cesium and tetraethylammonium Cl blocked voltage-sensitive potassium channels. Voltage-clamp recordings were made using a Multiclamp 700B (Molecular Devices), digitized (10 kHz; DigiData 1322A, Molecular Devices) and recorded using pCLAMP v.10.0 software (Molecular Devices). In all experiments, membrane potentials were corrected for a liquid junction potential of –10 mV. After forming a gigaseal onto a cell and rupturing the cell membrane, tumor cell membrane potential was held at −70 mV. Cell membrane capacitance, membrane resistance and pipette access resistance were then measured with the pCLAMP cell membrane test function. Recordings were excluded if pipette access resistance was higher than 20 MΩ or if access resistance changed by more than 20% during the experiment. After cell membrane resistance had stabilized, membrane potential was then stepped to 0 mV for 100 ms followed by a series of 250 ms voltage steps from −80 mV to +80 mV in 20-mV increments and the current response to these voltage steps was recorded. GdCl3 (100 μM) was then applied to the bath solution to eliminate the voltage-independent ‘leak’ current associated with Nalcn. Calculation of the Nalcn current was performed offline by subtracting the current response in GdCl3 from the previous GdCl3-free current recording. Tumor cell Nalcn current density was determined by dividing the Nalcn current by cell membrane capacitance. To verify successful expression of the RFP+ (NalcnshRNA) or GFP+ (NALCNcDNA) construct, cells were imaged with two-photon laser scanning microscopy (Prairie Technologies) using a Ti:sapphire Chameleon Ultra femtosecond-pulsed laser (Coherent), and ×60 (0.9 NA) water-immersion infrared objective (Olympus). Red fluorescent protein was visualized using an excitation wavelength of 1030 nM, whereas green fluorescent protein (GFP) was visualized using an excitation wavelength of 820 nM (Supplementary Tables 26 and 28).
Gastric adenocarcinoma allografts
P1KP-GAC orthotopic and flank allografts were generated under protocols approved by the Institutional Animal Care and Use Committee of St. Jude Children’s Research Hospital (IACUC-SJ). For orthotopic grafts, a longitudinal abdominal incision was made to expose the pyloric valve of CD-Foxn1NU mice and 2 × 105 freshly dissociated P1KP-GAC cells suspended in Matrigel and fast green (Santa Cruz) were injected into the pyloric stomach epithelium. The wound was closed and mice were monitored daily for tumor development. Under veterinary guidance and IACUC-SJ approved measures, animals reaching humane end points were immediately euthanized and a full autopsy completed (Supplementary Tables 26 and 29).
Generation of NalcnFlx allele
Mice were derived from targeted embryonic stem cells (ESCs) (UCDAVIS KOMP Repository Knockout Mouse Project clone EPD0383_5_C01). ESCs were screened using KOMP PCR strategies for Nalcntm1a(KOMP)Wstsi. ESCs were implanted into recipient C57/Bl6 mice in accordance with protocols approved by IACUC-SJ. Wild-type Nalcn and NalcnFlx alleles were detected using standard PCR and primers (UCDAVIS KOMP Repository Knockout Mouse Project clone EPD0383_5_C01). Nalcn RNA expression was quantified by quantitative PCR (qPCR) with reverse transcription and a Bio-Rad CFX96 Touch Real-Time PCR Detection System with primers (see Supplementary Tables 26 and 29–31 for details on animals and oligonucleotide sequences).
Tumorigenesis and surveillance
All animal studies within the United Kingdom (UK) were performed under the Animals (Scientific Procedures) Act 1986 in accordance with UK Home Office licenses (Project License 70-8823, P47AE7E47, PP7834816) and approved by the Cancer Research UK (CRUK) Cambridge Institute Animal Welfare and Ethical Review Board. Mice were housed in individually ventilated cages with wood chip bedding and nestlets with environmental enrichment (cardboard fun tunnels and chew blocks) under a 12 h light/dark cycle at 21 ± 2 °C and 55% ± 10% humidity. Diet was irradiated LabDiet 5R58 with ad libitum water. Animals carrying the modified Nalcn allele were bred to RosaFLPe-expressing mice to remove LacZ and Neo cassette. Animals with complete recombination were bred with: Prom1C-L29; Nestin-cre49; Rosa-CreERT50; villin-CreER25; Pdx1-cre28; RosaZSG51; and KrasG12D/+52, Trp53flx53. Cre-recombination was activated by dosing with 1 mg of tamoxifen per 40 g (body weight) at P3 or 8 mg tamoxifen per 40 g (body weight) at P60. Mice were maintained for up to 2 years and full-body autopsy was performed as described4 at humane end points or the indicated time point, whichever was first. All tissues were inspected for macroscopic tumors with direct green fluorescence detection. Tissues were formalin fixed, paraffin embedded with portions also snap frozen or used for tissue dissociation for sequencing (Supplementary Tables 26 and 29).
Histology
Hematoxylin and eosin (H&E) staining was performed using standard procedures (catalog number 7221, 7111, Thermo Fisher Scientific). Fibrosis was assessed using modified Masson’s trichrome and Picrosirius Red stains. Immunohistochemistry was performed using standard procedures and primary antibodies: Ki67 (catalog number IHC-00375, Bethyl Laboratories, 1:1,000), ZSG (catalog number 632474, Clontech, 1:2,000), pan cytokeratin (AE1/AE3) (catalog number 901-011-091620, BioCare Medical, 1:100), CK5 (catalog number ab52635, Abcam, 1:100), vimentin (catalog number 5741S, Cell Signaling Technology, 1:200), cleaved caspase 3 (catalog number 9664, Cell Signaling Technology, 1:200), CD31 (catalog number 77699, Cell Signaling Technology, 1:100), α-smooth muscle actin (catalog number ab5694, Abcam 1:500), CD45 (catalog number ab25386, Abcam, 5 μg ml−1). Secondary antibodies were antirabbit poly-horseradish peroxidase-IgG (included in kit) or rabbit antirat (catalog number A110-322A, Bethyl Laboratories, 1:250). Digital images of entire tissue sections were captured using the Leica Aperio AT2 digital scanner (×40, resolution 0.25 μM per pixel), viewed using the Leica Aperio Image Scope v.12.3.2.8013 and quantified by HALO (Indica Labs) image analysis (Supplementary Tables 28 and 33).
For immunofluorescence, tissue sections were incubated with primary antibodies: rhodamine-labeled DBA (catalog number RL-1032, Vector Laboratories, 1:100), rhodamine-labeled UEA I (catalog number RL-1062, Vector Laboratories, 1:100), ZSG (catalog number TA180002, Origene, 1:1,000), CK7 (catalog number ab181598, Abcam, 1:200), CK20 (catalog number ab97511, Abcam, 1:200), E-cadherin (catalog number AF748, R&D Systems, 1:100), N-cadherin (catalog number 13116, Cell Signaling Technology, 1:100), Icam1 (catalog number ab179707, Abcam, 1:100), Cdx2 (catalog number ab76541, Abcam, 1:100), Krt80 (catalog number 16835-1-AP, ProteinTech, 1:100), Hba-a1 (catalog number ab92492, Abcam, 1:100), Lgals3 (catalog number ab209344, Abcam, 1:200), CD45 (catalog number ab10558, Abcam, 1:200). Secondary antibodies included Alexa 488, 594 and 647 (catalog numbers A-11055, A-21207 and A-31571, Thermo Fisher Scientific, 1:500). Sections were counterstained (4,6-diamidino-2-phenylindole (DAPI); catalog number 4083, Cell Signaling, 1:10,000) and images captured using a Zeiss ImagerM2 and Apotome microscope or Zeiss Axioscan.Z1 (Zeiss) at ×40 magnification and processed using ZEN2.3 (Zeiss) software (Supplementary Tables 28 and 33). Single-channel images are shown in Supplementary Fig. 1
Nalcn RNA expression was detected in formalin-fixed, paraffin-embedded sections using the Advanced Cell Diagnostics (ACD) RNAscope 2.5 LS Reagent Kit-RED (ACD, catalog number 322150) and RNAscope 2.5 LS Mm Nalcn (ACD, catalog number 415168). Probe hybridization and signal amplification were performed according to the manufacturer’s instructions. Fast Red detection of mouse Nalcn was performed was performed on the Bond Rx using the Bond Polymer Refine Red Detection Kit (Leica Biosystems, catalog number DS9390) according to the manufacturer’s protocol. Whole-tissue sections were imaged on the Aperio AT2 (Leica Biosystems) and analyzed as for immunohistochemistry using HALO (Indica Labs) imaging analysis software. β-Galactosidase staining was performed exactly as described4 (Supplementary Tables 26, 28 and 30).
Histological review, primary and metastatic tumor classification were performed by performed by expert pathologists (P. Vogel and B. Mahler-Araujo) blinded to mouse genotype and clinical history. The numbers of ZSG+ cell clusters or metastases were counted in each organ in each mouse. Tissue fibrosis was assessed by expert pathologist R. Nazarian using sections stained with H&E, Masson’s trichrome and Picrosirius Red.
Whole-tissue imaging
Kidneys were exsanguinated, perfused with PBS and 4% PFA by PBS washes and immersion reagent 1a (150 g of ultrapure water, 20 g of Triton X-100 (catalog number 10254583, Thermo Fisher Scientific), 10 g of 100% solution of N,N,N′,N′-tetrakis (2-hydroxypropyl)ethylenediamine (catalog number 122262, Sigma), 20 g of urea (catalog number 140750010, ACROS Organics), 1 ml of 5 M NaCl) containing 10 μM DAPI (catalog number 4083; Cell Signaling Technology) at 37 °C and 80 r.p.m. The solution was exchanged every 2 d until the tissue was cleared. Cleared tissues were washed and immersed in 50% PBS/50% reagent 2 (15 g of ultrapure water, 50 g of sucrose (catalog number 220900010, ACROS Organics), 25 g of urea (catalog number 140750010, ACROS Organics), 10 g of 2,2,2-nitrilotriethanol (catalog number 90279, Sigma)) for 6 h (room temperature, with gentle shaking) followed by immersion in 100% reagent 2 (10 ml) for 1 d (room temperature). Tissues were mounted and scanned on a TCS SP5 confocal laser scanning microscope (Leica) at ×10 objective for DAPI and endogenous expression of ZSG. Images were processed using Imaris x64 v.9.3.0 software (Oxford Instruments) (Supplementary Tables 26, 28 and 30).
Serial two-photon tomography imaging was performed on a TissueCyte 1000 instrument (TissueVision) in which a series of mosaic two-dimensional images are taken of the tissue, followed by physical sectioning with a vibratome and a subsequent round of imaging. This continues in an automated fashion, generating 15 μm serial two-photon tomography sections that can be mounted on standard microscopy slides, imaged by Axioscan fluorescence scanning (Zeiss) for section identification and realignment. Fiducial agarose marker beads labeled with GFP are distributed throughout the embedding medium to help in the realignment of the samples for consequent use (Supplementary Tables 26, 28 and 30).
Harvesting and injection of circulating ZSG cells
Peripheral blood (500 µl to 1 ml) was harvested from mice at autopsy into 10 µl of 0.5 M EDTA, diluted in PBS and assessed by MACSQuant Analyzer (Miltenyi Biotech Inc.) for ZSG expression (525/50 nm (FITC) versus 614/50 nm (propidium iodide)). Cells for SCS and tail-vein injection were sorted using a BD FACSAria II Cell Sorter (BD Biosciences) excitation at 525/50 nm (FITC) versus 614/50 nm (propidium iodide). Nontamoxifen-induced mouse peripheral blood served as a negative control to set gate parameters (Supplementary Figs. 2 and 3). Some 25,000 ZSG+ cells were sorted and injected into recipient NOD SCID gamma mice (Charles River) and aged. For serial dilution assessment of tCZC metastasis initiation, tCZCs were isolated from donor tumor-bearing animals via FACS based on ZSG expression and placed into culture medium. Culture medium was as follows: Advanced DMEM/F12 (catalog number 31330038, Thermo Fisher Scientific), 2mM l-glutamine (catalog number 25030024, Thermo Fisher Scientific), B27 (catalog number 12587010, Thermo Fisher Scientific) and N2 (catalog number A1370701, Thermo Fisher Scientific), containing growth factors (50 ng ml−1 epidermal growth factor (PeproTech), 100 ng ml−1 basic fibroblast growth factor (catalog number 100-18c, PeproTech) and 1% FBS (catalog number 10500064, Thermo Fisher Scientific). Cells were grown at 37 °C in 5% CO2. Recipient NOD SCID gamma mice (Charles River) were injected with either 10, 100, 1,000 or 10,000 tCZCs via tail-vein injection and aged. Full autopsy and tissue harvesting were performed as described above. Full autopsy and tissue harvesting were performed as described above (Supplementary Tables 26, 28 and 29).
Bulk RNA sequencing
Total RNA was extracted from tissues using Maxwell RSC miRNA Tissue Kit (catalog number AS1460, Promega). RNA quality was assessed using TapeStation System (catalog number 5067-5579, Agilent). RNA libraries and downstream sequencing were carried out as previously described54. The Illumina TruSeq stranded messenger RNA kit (catalog number 20020595, Illumina) was used to prepare RNA libraries and RNA quality confirmed using TapeStation (Agilent) and quantified using a KAPA qPCR library quantification kit for Illumina platforms (catalog number KK4873, KAPA Biosystems). Samples were normalized using the Agilent Bravo, pooled and sequenced on Illumina NovaSeq SP flowcell to generate single-end 50 bp reads at 20 million reads per sample.
Single-end 50 bp RNA reads were aligned to GRCm38 with HISAT2 (with default parameters). Each sample was sequenced across several lanes; per-lane BAM files were merged into per-sample BAM files. Quality control metrics were collected for each file, including duplication statistics and number of reads assigned to genes. Reads were counted on annotated features with subreads featureCounts, providing ‘total’, ‘aligned to the genome’ and ‘assigned to a gene’ (that is, included in the analysis) counts. Percentages of aligned bases were computed for several categories: coding, untranslated region, intronic and intergenic. Other quality control metrics were the percentage of reads on the correct strand, median coefficient of variation of coverage, median 5′ bias, median 3′ bias and the ratio of 5′ to 3′ coverage. Quality control also included an expression heatmap drawn using log2-transformed counts. The log2-transformed counts were generated from normalized counts using the log2 function in R and counts function from DEseq2. Genes were regarded as displaying differential expression between sample cohorts if they displayed of ≥1 or ≤−1 log(fold difference) in expression levels with an adjusted P ≤ 0.05 (Supplementary Tables 26, 28 and 30).
Single-cell RNA sequencing
Animals were perfused with PBS followed by 100 U ml−1 of collagenase type IV in HBSS with Ca2+ and Mg2+ (Life Technologies) media containing 3 mM CaCl2. Whole organs were dissected, dissociated and placed into 2 ml of the appropriate dissociation buffer: lung and stomach were dissociated with 200 U ml−1 of collagenase type IV (Sigma) and 100 μg μl−1 of DNAse I (Roche) in HBSS with Ca2+ and Mg2+ (Life Technologies) media containing 3 mM CaCl2; liver was dissociated with collagenase type I (100 U ml−1), dispase (2.4 U ml−1) DNAse I (100 μg ml−1) in HBSS with Ca2+ and Mg2+ (Life Technologies) media containing 3 mM CaCl2; kidney was dissociated with papain (20 U ml−1) and DNAse I (100 mg ml−1) in DMEM high glucose, 2 mM l-glutamine (Life Technologies) with 1× Pen-Strep and 10% FBS; uterus and epididymis were dissociated with collagenase type I (100 U ml−1) and DNAse I (100 mg ml−1) in in HBSS with Ca2+ and Mg2+ (Life Technologies) media containing 3 mM CaCl2. Cells suspensions were filtered washed with HBSS without calcium and magnesium and centrifuged for 5 min at 300g at 4 °C for 5 min.
Single-cell suspensions of solid tissues were multiplexed and labeled with Cell Hashing conjugates: antimouse hashtags from 0301 to 0315 (BioLegend) before sequencing. All nucleated cells and ZSG+ cells isolated from peripheral blood were not multiplexed but placed into a 10x Genomics pipeline. SCS libraries were prepared using Chromium Single Cell 3′ Library & Gel Bead Kit v.3, Chromium Chip B Kit and Chromium Single Cell 3′ Reagent Kits v.3 User Guide (manual CG000183 Rev A; 10x Genomics). Cell suspensions were loaded on the Chromium instrument with the expectation of collecting gel-bead emulsions containing single cells. RNA from the barcoded cells for each sample was subsequently reverse-transcribed in a C1000 Touch thermal cycler (Bio-Rad) and all subsequent steps to generate single-cell libraries were performed according to the manufacturer’s protocol with no modifications (for most of the samples 12 cycles was used for cDNA amplification, 16 for samples with very low cell concentration). cDNA quality and quantity were measured with Agilent TapeStation 4200 (High Sensitivity D5000 ScreenTape) after which 25% of material was used for preparation of the gene expression library. Library quality was confirmed with Agilent TapeStation 4200 (High Sensitivity D1000 ScreenTape to evaluate library sizes) and Qubit 4.0 Fluorometer (Qubit dsDNA HS Assay Kit (Thermo Fisher Scientific) to evaluate double-stranded DNA quantity). Each sample was normalized and pooled in equal molar concentrations. To confirm concentration pools underwent qPCR using KAPA Library Quantification Kit on QuantStudio 6 Flex before sequencing. Pools were sequenced on an Illumina NovaSeq6000 sequencer with the following parameters: 28 bp, read 1; 8 bp, i7 index; and 91 bp, read 2.
Raw RNA reads were processed with cellranger using mm10 from 10x as the reference genome to create filtered gene expression matrixes. Cell barcodes detected by cellranger were used as input to CITESeq for hashtagged sequence data (solid organs) generating a counts matrix with cell barcodes and hashtag oligo sequences per cell. The HTODemux function from Seurat was then used to identify clusters and classify cells according to their barcodes, including negative and doublet cells. Quality control metrics were generated using Scater followed by single-cell object conversion to Seurat objects, merging of objects and then analyses run using the standard Seurat pipeline (Supplementary Tables 26, 28 and 30).
SCS profiles of human CTCs (GSE75367; GSE74639; GSE60407; GSE67980; GSE114704; GSE144494) and 500 cells from Illumina 10x for human PBMC raw counts were merged in python v.3.7.3 using the pandas library. Only common genes between datasets were analyzed. Seurat objects were created from PBMCs and CTCs. Following this step, data were analyzed using the standard Seurat pipeline (Supplementary Table 33).
For direct comparison of human CTCs and mouse tCZCs, 15,328 orthologs were identified and profiles processed through the standard Seurat workflow that includes a per-cell normalization of each gene expression count. Enrichment of a hemoglobin gene expression was carried out in UCell and enrichment scores generated with a two-tailed Mann–Whitney U statistic.
Statistics and reproducibility
Clinical and mutation/CNA data were from the Cancer Genome Atlas via cBioportal, selecting for studies included as part of the Pan-Cancer Atlas55. Gene expression data was from Xenabrowser56. dN/dS was calculated using the dNdScv R package18. t-distributed stochastic neighbor embedding (t-SNE) was performed with the sklearn library in python using the ‘BarnesHut’ method, with a perplexity of 15, learning rate of 1,000 and 1,000 iterations. Contours were drawn as kernel density estimates of the density of nonsynonymous NALCN mutations for each cancer subtype with a significant (P ≤ 0.05) dN/dS score individually.
NALCN cryo-electron microscopy12 structure 6XIW was downloaded from pdb, simulated in MemprotMD22,23, energy minimized using the steepest descents for 5,000 steps and converted to a MARTINI coarse-grained57 representation embedded in a 1-palmitoyl-2-oleoyl-sn-glycero-3-phosphocholine bilayer with 575 lipids. The membrane was self-assembled by position restraining the protein and simulating for 200 ns to allow the membrane to form. The CG system was simulated for 1,000 ns before converting back to atomistic detail using CG2AT. The resultant atomistic membrane system was simulated in fully atomistic detail using the gromos53a6 forcefield for 400 ns. Mutational impact on pore size was calculated using HOLE21. Mutations were introduced into the simulated NALCN structure using the modeler mutation optimization protocol, and the resultant HOLE pore profiles aligned on their selectivity filters (Supplementary Table 28).
Spatial clustering of mutations was performed by calculating the distance between the center of mass of each pair of mutated residues (in the wild-type structure), and grouping residues into clusters with distances between any one pair of residues <12 Å. We calculated an expected distribution through randomly sampling the structure for the same number of mutations observed overall 100,000 times. Comparison of the observed clusters with the distribution of random samples was used to calculate a P value. All code generated for spatial clustering and analysis, with a workable example is available at: https://github.com/shorthouse-mrc/NALCN.
Unsupervised hierarchical clustering was performed using Morpheus (https://software.broadinstitute.org/morpheus) and genset enrichment using g:Profiler (version e104_eg51_p15_3922dba). Tissue type deconvolution was performed using xCell (http://xCell.ucsf.edu/) (Supplementary Table 28).
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Online content
Any methods, additional references, Nature Research reporting summaries, source data, extended data, supplementary information, acknowledgements, peer review information; details of author contributions and competing interests; and statements of data and code availability are available at 10.1038/s41588-022-01182-0.
Supplementary information
Supplementary Figs. 1–3.
Supplementary Tables 1–33.
Source data
Statistical source data.
Statistical source data.
Statistical source data.
Statistical source data.
Statistical source data.
Statistical source data.
Statistical source data.
Unprocessed gel.
Statistical source data.
Statistical source data.
Acknowledgements
This work was supported by grants to: R.J.G. (CRUK Major Centre and Cambridge Institute Core Awards and St. Jude Children’s Research Hospital/American Lebanese Syrian Associated Charities (ALSAC)); S.S.Z. (ALSAC, National Institutes of Health CA021765, MH097742, DC012833); B.A.H. (Royal Society Research Fellowship UF130039, Medical Research Council research grant MR/S000216/1); E.P.R. (Marie Skłodowska-Curie Individual Fellowship from European Commission and Cancer Center Neurobiology and Brain Tumor Program Garwood Named Fellowship from St. Jude Children’s Research Hospital). We thank the CRUK Cambridge Institute genomics, flow cytometry, light microscopy, biological resource unit, bioinformatics, research instrumentation and cell services, histopathology core facilities and the cell and tissue imaging resources and the Animal Resources Center at St. Jude Children’s Research Hospital for technical assistance.
Extended data
Author contributions
E.P.R. conducted the great majority of the experiments, contributed to the conception of the research, experimental design and writing of the manuscript. D.S., A.J., L.P.H., M.O., M.P.-R., A.F., G.J.H., R.T., F.C.L., J.A.B., B.A.H., S.S.Z., D.J.W., L.Z. and J.K. conducted important experiments, provided critical advice on experimental design and/or interpretation and contributed to writing of the manuscript. B.M.-A., P.V. and R.M.N. provided pathology expert review and contributed to writing of the manuscript. R.J.G. conceived the research and experimental design, supervised the research and was primary author of the manuscript.
Data availability
All the raw sequencing data have been deposited in the Gene Expression Omnibus with the following accession numbers: mouse RNA-seq of tumors and metastases (GSE210134) and mouse single cell RNA-seq of CZCs, PBMCs, tumors, metastases and solid tissues (GSE210134). Murine Prom1+ gastric mucosa and adenocarcinoma data GEO accession number: GSE78076. NALCN mutation and TSNE plot were generated with Pan-Cancer Atlas data from TCGA via cbioPortal and Xenabrowser. Cancer staging data were generated with Pan-Caner Atlas from TCGA and COSMIC data. NALCN structure 6XIW was from pdb. Human CTC and gene signature datasets are from the following GEO accession numbers: GSE75367, GSE74639, GSE60407, GSE67980, GSE114704, GSE144494. Human PBMC data are from Illumina 10x (10k Human PBMCs, 3’ v3.1, Chromium X). Source data are provided with this paper.
Code availability
All bulk and single-cell analyses and visualizations were performed using R software (v.3.6.1), R studio (v.1.3.1093) and Python (v.3.9). Details on specific packages are included in the Methods section and also at https://github.com/shorthouse-mrc/NALCN. No custom code was used for any part of the data processing or analysis.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
is available for this paper at 10.1038/s41588-022-01182-0.
Supplementary information
The online version contains supplementary material available at 10.1038/s41588-022-01182-0.
References
- 1.Dillekås, H., Rogers, M. S. & Straume, O. Are 90% of deaths from cancer caused by metastases? Cancer Med.8, 5574–5576 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ganesh, K. & Massagué, J. Targeting metastatic cancer. Nat. Med.27, 34–44 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Massagué, J. & Obenauf, A. C. Metastatic colonization by circulating tumour cells. Nature529, 298–306 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.House, C. D. et al. Voltage-gated Na+ channel SCN5A is a key regulator of a gene transcriptional network that controls colon cancer invasion. Cancer Res.70, 6957–6967 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheth, M. & Esfandiari, L. Bioelectric dysregulation in cancer initiation, promotion, and progression. Front. Oncol.12, 846917 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang, T. et al. The calcium pump PMCA4 prevents epithelial–mesenchymal transition by inhibiting NFATc1-ZEB1 pathway in gastric cancer. Biochim. Biophys. Acta Mol. Cell. Res.1867, 118833 (2020). [DOI] [PubMed] [Google Scholar]
- 7.Nguyen, B. et al. Genomic characterization of metastatic patterns from prospective clinical sequencing of 25,000 patients. Cell185, 563–575.e11 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ganesh, K. et al. L1CAM defines the regenerative origin of metastasis-initiating cells in colorectal cancer. Nat. Cancer1, 28–45 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laughney, A. M. et al. Regenerative lineages and immune-mediated pruning in lung cancer metastasis. Nat. Med.26, 259–269 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pastushenko, I. et al. Identification of the tumour transition states occurring during EMT. Nature556, 463–468 (2018). [DOI] [PubMed] [Google Scholar]
- 11.Chua, H. C., Wulf, M., Weidling, C., Rasmussen, L. P. & Pless, S. A. The NALCN channel complex is voltage sensitive and directly modulated by extracellular calcium. Sci. Adv.6, eaaz3154 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kschonsak, M. et al. Structure of the human sodium leak channel NALCN. Nature587, 313–318 (2020). [DOI] [PubMed] [Google Scholar]
- 13.Lu, B. et al. The neuronal channel NALCN contributes resting sodium permeability and is required for normal respiratory rhythm. Cell129, 371–383 (2007). [DOI] [PubMed] [Google Scholar]
- 14.Bend, E. G. et al. NALCN channelopathies: distinguishing gain-of-function and loss-of-function mutations. Neurology87, 1131–1139 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhu, L. et al. Multi-organ mapping of cancer risk. Cell166, 1132–1146 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ren, D. Sodium leak channels in neuronal excitability and rhythmic behaviors. Neuron72, 899–911 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cochet-Bissuel, M., Lory, P. & Monteil, A. The sodium leak channel, NALCN, in health and disease. Front. Cell. Neurosci.8, 132 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martincorena, I. et al. Universal patterns of selection in cancer and somatic tissues. Cell171, 1029–1041 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weinstein, J. N. et al. The Cancer Genome Atlas Pan-Cancer analysis project. Nat. Genet.45, 1113–1120 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joerger, A. C. & Fersht, A. R. The p53 pathway: origins, inactivation in cancer, and emerging therapeutic approaches. Annu. Rev. Biochem.85, 375–404 (2016). [DOI] [PubMed] [Google Scholar]
- 21.Smart, O. S., Neduvelil, J. G., Wang, X., Wallace, B. A. & Sansom, M. S. P. OLE: a program for the analysis of the pore dimensions of ion channel structural models. J. Mol. Graph.14, 354–360 (1996). [DOI] [PubMed] [Google Scholar]
- 22.Newport, T. D., Sansom, M. S. P. & Stansfeld, P. J. The MemProtMD database: a resource for membrane-embedded protein structures and their lipid interactions. Nucleic Acids Res.47, D390–D397 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stansfeld, P. J. et al. MemProtMD: automated insertion of membrane protein structures into explicit lipid membranes. Structure23, 1350–1361 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koplev, S., Lin, K., Dohlman, A. B. & Ma’ayan, A. Integration of pan-cancer transcriptomics with RPPA proteomics reveals mechanisms of epithelial–mesenchymal transition. PLoS Comput. Biol.14, e1005911 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.El Marjou, F. et al. Tissue-specific and inducible Cre-mediated recombination in the gut epithelium. Genesis39, 186–193 (2004). [DOI] [PubMed] [Google Scholar]
- 26.Jackstadt, R. et al. Epithelial NOTCH signaling rewires the tumor microenvironment of colorectal cancer to drive poor-prognosis subtypes and metastasis. Cancer Cell36, 319–336 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Magnuson, M. A. & Osipovich, A. B. Pancreas-specific Cre driver lines and considerations for their prudent use. Cell Metab.18, 9–20 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hingorani, S. R. et al. Preinvasive and invasive ductal pancreatic cancer and its early detection in the mouse. Cancer Cell4, 437–450 (2003). [DOI] [PubMed] [Google Scholar]
- 29.Zhu, L. et al. Prominin 1 marks intestinal stem cells that are susceptible to neoplastic transformation. Nature457, 603–607 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pantel, K. & Alix-Panabières, C. Liquid biopsy and minimal residual disease — latest advances and implications for cure. Nat. Rev. Clin. Oncol.16, 409–424 (2019). [DOI] [PubMed] [Google Scholar]
- 31.Miyamoto, D. T. et al. RNA-Seq of single prostate CTCs implicates noncanonical Wnt signaling in antiandrogen resistance. Science349, 1351–1356 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ting, D. T. et al. Single-cell RNA sequencing identifies extracellular matrix gene expression by pancreatic circulating tumor cells. Cell Rep.8, 1905–1918 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zheng, Y. et al. Expression of β-globin by cancer cells promotes cell survival during blood-borne dissemination. Nat. Commun.8, 14344 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ebright, R. Y. et al. Deregulation of ribosomal protein expression and translation promotes breast cancer metastasis. Science367, 1468–1473 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jordan, N. V. et al. HER2 expression identifies dynamic functional states within circulating breast cancer cells. Nature537, 102–106 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dimitrov-Markov, S. et al. Discovery of new targets to control metastasis in pancreatic cancer by single-cell transcriptomics analysis of circulating tumor cells. Mol. Cancer Ther.19, 1751–1760 (2020). [DOI] [PubMed] [Google Scholar]
- 37.Todd, D. J. & Kay, J. Gadolinium-induced fibrosis. Annu. Rev. Med.67, 273–291 (2016). [DOI] [PubMed] [Google Scholar]
- 38.Wagner, B. et al. Nephrogenic systemic fibrosis: evidence for oxidative stress and bone marrow-derived fibrocytes in skin, liver, and heart lesions using a 5/6 nephrectomy rodent model. Am. J. Pathol.181, 1941–1952 (2012). [DOI] [PubMed] [Google Scholar]
- 39.Habib, A. R. et al. A systematic review of the clinical efficacy and safety of CFTR ModulatORS IN CYstic fibrosis. Sci. Rep.9, 7234 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pantel, K., Brakenhoff, R. H. & Brandt, B. Detection, clinical relevance and specific biological properties of disseminating tumour cells. Nat. Rev. Cancer8, 329–340 (2008). [DOI] [PubMed] [Google Scholar]
- 41.Kolling, S. et al. ‘Metastatic cancer of unknown primary’ or ‘primary metastatic cancer’? Front. Oncol.9, 1546 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Martincorena, I. et al. Tumor evolution. High burden and pervasive positive selection of somatic mutations in normal human skin. Science348, 880–886 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Martincorena, I. et al. Somatic mutant clones colonize the human esophagus with age. Science362, 911–917 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Klein, C. A. Parallel progression of primary tumours and metastases. Nat. Rev. Cancer9, 302–312 (2009). [DOI] [PubMed] [Google Scholar]
- 45.Barbado, M., Fablet, K., Ronjat, M. & De Waard, M. Gene regulation by voltage-dependent calcium channels. Biochim. Biophys. Acta1793, 1096–1104 (2009). [DOI] [PubMed] [Google Scholar]
- 46.Barker, N. et al. Lgr5(+ve) stem cells drive self-renewal in the stomach and build long-lived gastric units in vitro. Cell Stem Cell6, 25–36 (2010). [DOI] [PubMed] [Google Scholar]
- 47.Robinson, G. et al. Novel mutations target distinct subgroups of medulloblastoma. Nature488, 43–48 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lu, B. et al. Peptide neurotransmitters activate a cation channel complex of NALCN and UNC-80. Nature457, 741–744 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tronche, F. et al. Disruption of the glucocorticoid receptor gene in the nervous system results in reduced anxiety. Nat. Genet.23, 99–103 (1999). [DOI] [PubMed] [Google Scholar]
- 50.Ventura, A. et al. Restoration of p53 function leads to tumour regression in vivo. Nature445, 661–665 (2007). [DOI] [PubMed] [Google Scholar]
- 51.Madisen, L. et al. A robust and high-throughput Cre reporting and characterization system for the whole mouse brain. Nat. Neurosci.13, 133–140 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jackson, E. L. et al. Analysis of lung tumor initiation and progression using conditional expression of oncogenic K-ras. Genes Dev.15, 3243–3248 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Marino, S., Vooijs, M., van Der Gulden, H., Jonkers, J. & Berns, A. Induction of medulloblastomas in p53-null mutant mice by somatic inactivation of Rb in the external granular layer cells of the cerebellum. Genes Dev.14, 994–1004 (2000). [PMC free article] [PubMed] [Google Scholar]
- 54.Patmore, D. M. et al. DDX3X suppresses the susceptibility of hindbrain lineages to medulloblastoma. Dev. Cell54, 455–470.e5 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gao, J. et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal.6, pl1 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Goldman, M. et al. Visualizing and interpreting cancer genomics data via the Xena platform. Nat. Biotechnol.38, 675–678 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Monticelli, L. et al. The MARTINI coarse-grained force field: extension to proteins. J. Chem. Theory Comput.4, 819–834 (2008). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figs. 1–3.
Supplementary Tables 1–33.
Statistical source data.
Statistical source data.
Statistical source data.
Statistical source data.
Statistical source data.
Statistical source data.
Statistical source data.
Unprocessed gel.
Statistical source data.
Statistical source data.
Data Availability Statement
All the raw sequencing data have been deposited in the Gene Expression Omnibus with the following accession numbers: mouse RNA-seq of tumors and metastases (GSE210134) and mouse single cell RNA-seq of CZCs, PBMCs, tumors, metastases and solid tissues (GSE210134). Murine Prom1+ gastric mucosa and adenocarcinoma data GEO accession number: GSE78076. NALCN mutation and TSNE plot were generated with Pan-Cancer Atlas data from TCGA via cbioPortal and Xenabrowser. Cancer staging data were generated with Pan-Caner Atlas from TCGA and COSMIC data. NALCN structure 6XIW was from pdb. Human CTC and gene signature datasets are from the following GEO accession numbers: GSE75367, GSE74639, GSE60407, GSE67980, GSE114704, GSE144494. Human PBMC data are from Illumina 10x (10k Human PBMCs, 3’ v3.1, Chromium X). Source data are provided with this paper.
All bulk and single-cell analyses and visualizations were performed using R software (v.3.6.1), R studio (v.1.3.1093) and Python (v.3.9). Details on specific packages are included in the Methods section and also at https://github.com/shorthouse-mrc/NALCN. No custom code was used for any part of the data processing or analysis.