Abstract
Globally, food insecurity is becoming a major public health concern, and has seriously been impacted by the COVID-19 pandemic. In the last decade, Rwanda has made significant improvement in terms of overall household food security. However, the magnitude of food insecurity among pregnant women is not well known. This study investigated the magnitude and factors associated with food insecurity among pregnant women during the COVID-19 pandemic.
It was a cross-sectional study conducted in 30 health facilities across the country where a total of 1159 pregnant women in their first trimester of pregnancy were recruited during antenatal care visits (ANC). A pre-tested, standardized, and structured questionnaire was used to collect information on food insecurity based on household food insecurity access scale (HFIAS). Descriptive statistics were used to describe the basic characteristics of the study respondents and the status of household food insecurity. Logistic regression analysis was performed to estimate the predictors of food insecurity at a significance level of 5%. The majority (78.1%) of recruited pregnant women were aged 20 to 35 years and 70.3% were from rural areas. Overall, 53.1% of pregnant women were food insecure during COVID-19 pandemic. Pregnant women with low education level {AOR = 4.58; 95%CI = 1.88–11.15} and from low social economic households {AOR = 2.45; 95%CI = 1.59–3.76} were more likely to become food insecure during COVID-19 pandemic. In addition, women from households with farming as the main source of income had 64% more risk of food insecurity compared to women from household with other sources of monthly income. To achieve the sustainable development goals (SDGs) targets related to food security, there is urgent need to transform the agricultural sector from traditional farming to modern/technology farming. This will reduce the level of food insecurity in developing countries. There is also a need to provide social safety nets to pregnant women from families in lower socio-economic categories during pandemics.
Keywords: COVID-19, Food insecurity, Pregnant women, First trimester, Gestational age, Rwanda
Graphical abstract
1. Introduction
Food insecurity (FI) is defined as lack of nutritionally adequate and safe food or a limited ability to acquire necessary food in socially acceptable ways [1]. Food insecurity has consistently increased at the global level since 2014. A recent report from the Food and Agricultural Organization (FAO) of the United Nations estimated that globally, 750 million people are exposed to severe levels of food insecurity. The same report shows that the global prevalence of both moderate and severe levels of food insecurity (SDG indicator 2.1.2) is estimated to be 25.9% [2].
It has been observed that in most African countries, people who are moderately food insecure do not have regular access to nutritious and sufficient food, even if not necessarily suffering from hunger [3]. In Rwanda, a comprehensive food security and vulnerability analysis (CFSVA) conducted in 2018 found that 18.7% of households had had trouble in accessing sufficient food while the prevalence of severe food insecurity was estimated to be 1.7% [4].
COVID-19 resulted in an increased number of households facing acute food insecurity [5]. In Rwanda, the COVID-19 pandemic might have exacerbated the crisis of food insecurity, disproportionately affecting pregnant women. A report published by the United Nations on the socio-economic impact of COVID-19 in Rwanda showed that food insecurity at the household level had increased during the COVID-19 pandemic due to the loss of wages, employment, and reduced economic activity [6].
Several factors are thought to have played out in the effect of COVID-19 pandemic on food security globally and locally, as per the following theoretical conceptual frameworks.
According to the FAO framework [7] there are four dimensions of food security namely, availability, access, utilization, and stability. Availability is the amount of food present in a country while access refers to effective demand for food, both economic and physical access to food. Utilization is about biological processing of food whereas stability captures the dynamic aspects of the above three. Food being a daily necessity, being food secure requires stability in the other three pillars over time.
Stability of food availability and access were affected by COVID-19-related restrictions on movement, with the fresh produce being most affected [8]. During the COVID-19 period, Rwanda was among the first African countries to close its borders and impose a nationwide lock-down. Although the agriculture sector was typically exempted from lockdown restrictions to ensure continuity of food production, reduced access to labor, given the fact that agricultural production in the country remains heavily human labor intensive, and shortages of intermediate farm inputs due to disruption of global supply chains led to reduction and restrictions on available food. Consumption patterns changed due to reduced availability of the food items requiring quick distribution especially fresh foods [9]. The economic shocks of the pandemic reduced people’s access to preferred foods, leaving the very vulnerable households dependent on a restricted diet provided by relief foods distributed by the Government of Rwanda during the lockdown. With reported reduced consumption of fresh produce and other nutritionally rich foods in the region [10] pregnant women’s micronutrients security was affected, potentially leading to deficiencies in their unborn babies.
The above framework mainly explains the effects of COVID-19 related restrictions to the supply side of food security. The “Food Systems” framework, on the other hand includes “all the elements (environment, people, inputs, processes, infrastructures, institutions) and activities that relate to the production, processing, distribution, preparation and consumption of food, and the output of these activities, including socio-economic and environmental outcomes” [11]. The food system approach recognizes that a change in one component is likely to have ripple effects on the others as all elements are highly interdependent. The food system approach considers the effect of the COVID-19 pandemic restrictions on all aspects of food value chains from production to consumption.
Finally, Amartya Sen’s ‘entitlement approach’, explains the differential impact of COVID-19 pandemic on food security of populations based on the distribution of wealth and resources. ‘Poverty and Famines’ [12] identified four legal sources of food at the individual or household level: production-based, own-labor, trade-based, and transfer entitlement. The production-based group, who constitute the majority of rural communities in Rwanda, faced challenges related to access to inputs and financial systems that support farming activities. The own-labor group, mainly informal casual laborers were hardest hit as most non-essential services sectors like construction were affected by the lockdowns. The same effects were felt by small business owners and traders. The formal employees faced pay cuts and their physical access to food was affected by movement restrictions and “stay-at-home” impositions during peak transmission periods of the pandemic. Those households or individuals relying on cash and food transfers for their food security were affected by the economic impact of the pandemic on the other three types of entitlements described above.
The above dynamics are thought to have had great bearing on how pregnant women in developing countries including Rwanda experienced the pandemic from a food security perspective.
In developing countries, pregnant women are particularly at increased risk of food insecurity and its health consequences. This has led to highly negative effects on the physical health and mental health of both pregnant women and their children. It was previously reported that women with food insecurity had an increased risk of gestational diabetes [13], iron deficiency [14], anxiety and depression [15,16] because of the difficulty in obtaining food. Food insecurity during pregnancy can have long-term consequences on child growth and development [17].
There is limited information on the magnitude of food insecurity among women during pregnancy and associated risk factors. This study, therefore, sought to investigate the magnitude and determinants of food insecurity among pregnant women during COVID-19 pandemic in Rwanda.
2. Materials and methods
2.1. Study design, setting and participants
A cross-sectional study was conducted among first trimester pregnant women who visited health facilities for antenatal care (ANC) in Rwanda. The study targeted women who had a confirmatory pregnancy test at the selected health facilities. The gestational age in weeks was determined using the last menstrual period reported and confirmed by an ultrasound examination. Pregnant women in their first trimester, residing for at least 6 months in the study area were included in the study. Pregnant women who were unable to give information due to serious illness or with disability were excluded from the study. The eligible respondents were enrolled and recruited from 30 public health facilities across the country.
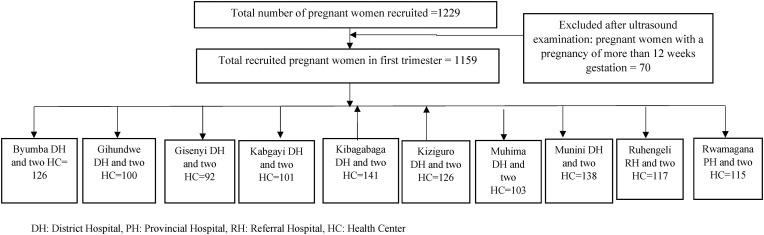
A multi-stage sampling technique was used whereby in the first stage, 30 health facilities (serving as clusters) across the country were selected using simple random sampling technique (Fig. 1 ). Then pregnant women who visited ANC department in selected health facilities and were confirmed to be in their first trimester were included in the study. Study participants were enrolled in the study from July to December 2020. After considering all inclusion criteria (Fig. 1), a total of 1159 pregnant women in the first trimester participated in the study.
Fig. 1.
Study Participants flow chart.
2.2. Data collection procedure and method
Data was collected by 30 trained nurses/midwives with direct supervision of 10 team leaders and the research team. They received a one-day training on the inclusion criteria, sampling and data collection procedure. The questionnaire was pretested among 50 pregnant women who visited ANC services at two Health Centers in Kigali City and the questionnaire was adjusted accordingly after pilot study. During the data collection process, the pregnant women were informed about the objective of the study and gave consent to participate. The questionnaire was divided into socio-demographic, socio-economic, lifestyle and health related characteristics. Mothers were asked about socio-demographic related questions including maternal age, partner’s age, residence, marital status; socio-economic related questions including maternal level of education, partner’s level of education, ownership of a house, main source of income and social-class categories; lifestyle variables include alcohol use, maternal smoking status and partner’s smoking status while health related variables include parity, HIV status, and chronic disease condition.
The food insecurity status was determined using a structured, standardized, and validated tool (Household Food Insecurity Access Scale: HFIAS) developed by Food and Nutrition Technical Assistance (FANTA), to classify households as food secure or not [18,19]. The tool consisted of nine questions showing the frequency of occurrence and severity of food insecurity in the last 4 weeks. The respondents were first asked if a given condition was experienced in which they were to respond yes or no. Then the severity of food insecurity was further assessed in terms of Likert Scale question responses (0 = never, 1 = rarely (1 or 2 times), 2 = sometimes (3–10 times), 3 = often (>10 times)). In this study, the pregnant women were asked to respond the questions on behalf of the household members. When calculating the score, each of the nine questions was scored 0–3, with 0 being "did not occur," 1 being "rarely”, 2 “sometimes," and 3 being "often." The score for each of the nine questions was then added together, and the total score ranges from 0 to 27, indicating the degree of insecure food access. Then the scores were categorized into 4 severity levels as follows: food secure (0 score), mildly food insecure (1–5), moderately food insecure (6–13), and severely food insecure (14–27). To determine the predictors of food insecurity and ease interpretation, the food security status was dichotomized into food secure (with no occurrence for all conditions/items) and food insecure with a ‘Yes’ response to at least one of 1–9 items.
2.3. Data quality management
Every questionnaire was cross-checked before leaving the participant to ensure the completeness of data. All questionnaires were stored in locked cabinets throughout the study period and accessed only by authorized persons to ensure confidentiality and to avoid data loss. Coding and verification of the data was done for easy manipulation, analysis, and presentation.
2.4. Data analysis
The data was entered and analyzed using IBM SPSS statistics 25. The basic characteristics and status of food insecurity were described using counts and percentages. Bivariate and multivariable logistic regression analysis was computed to determine the independent predictors of food insecurity. First bivariate analysis was done to identify variables significantly associated with the food insecurity (p value <0.05). Then to control for possible confounding variables and identify independent predictors of food insecurity, a multivariate logistic regression was performed. Variables significant during bivariate analysis were fitted together in the multivariable logistic regression and eight factors remained in the final model. A backward selection procedure was used. The goodness of fit was assessed using the Hosmer-Leme show test with Chi-square value 2.17 and p value of 0.975 which indicates that the fitted model was appropriate. Statistical significance was declared at a p value of < 0.05, and the degree of association between independent variables and the food insecurity was measured by adjusted odds ratio (AOR) with 95% confidence interval (CI).
2.5. Ethical considerations
Ethical clearance was obtained from Rwanda National Ethics Committee with reference number No.131/RNEC/2020 and permission letter was obtained from each selected Hospital. Written informed consent was obtained from the study participants after a full explanation of the purpose of the study. Participants who could not read made a thump-print after obtaining a verbal explanation from the interviewer. Study participants were free to refuse or withdraw from the study at any time without any penalty. Furthermore, the participants were assured about the confidentiality of the information and no personal identifiers were put on the questionnaires.
3. Results
3.1. Characteristics of study participants
Majority of (78.1%) of the pregnant women were in the age group of 20 to 35 years. Likewise, their spouses’ or partners’ age in the same age group were 68.8%. Majority (70.3%) of the women were from rural areas and about half of them were married (52.1%). Regarding education, most (59.4%) attained primary level of education while only 5.6% attended tertiary education. Similarly, most of their spouses’ (60.7%) had a primary level of education (Table 1 ). The study revealed that 60.6% of the study participants own a house. Concerning the employment status, more than half (54.1%) and their spouses (55.7%) were farmers followed by being housewives (21.2%). According to the social class classification in Rwanda, over half of the respondents (68.2%) fall in category one and two corresponding to low socio-economic category.
Table 1.
Characteristics of study participants.
| Characteristics | Frequency (n = 1159) | Percent (%) |
|---|---|---|
| Age in years | ||
| 15-19 | 69 | 6.0 |
| 20-35 | 905 | 78.1 |
| >35 | 185 | 16.0 |
| Spouse’s/partner's age in years | ||
| 15-19 | 14 | 1.2 |
| 20-35 | 797 | 68.8 |
| >35 | 348 | 30.0 |
| Residence | ||
| Rural | 815 | 70.3 |
| Urban | 344 | 29.7 |
| Marital status | ||
| Married | 604 | 52.1 |
| Cohabiting | 471 | 40.6 |
| Single | 84 | 7.2 |
| Level of education | ||
| No formal education | 108 | 9.3 |
| Primary | 689 | 59.4 |
| Secondary | 297 | 25.6 |
| Tertiary | 65 | 5.6 |
| Spouse/partner's level of education | ||
| No formal education | 107 | 9.2 |
| Primary | 703 | 60.7 |
| Secondary | 256 | 22.1 |
| Tertiary | 93 | 8.0 |
| Ownership of the house | ||
| Own house | 702 | 60.6 |
| Rented house | 419 | 36.2 |
| Others | 38 | 3.3 |
| Main Source of household income | ||
| Employed/Monthly income | 285 | 24.6 |
| Business | 175 | 15.1 |
| Farmer | 645 | 55.7 |
| Others | 54 | 4.7 |
| Socio-class category | ||
| Category 1 | 199 | 17.2 |
| Category 2 | 591 | 51.0 |
| Category 3 | 369 | 31.8 |
| Alcohol Use | ||
| Yes | 249 | 21.5 |
| No | 910 | 78.5 |
| Smoking status | ||
| Yes | 13 | 1.1 |
| No | 1146 | 98.9 |
| Spouse/partner's smoking status | ||
| Yes | 81 | 7.0 |
| No | 1078 | 93.0 |
| Parity | ||
| Primi-gravida | 469 | 40.5 |
| One | 270 | 23.3 |
| Two | 169 | 14.6 |
| Three | 110 | 9.5 |
| Four | 63 | 5.4 |
| Five and above | 78 | 6.7 |
| HIV status | ||
| Positive | 27 | 2.3 |
| Negative | 1132 | 97.7 |
| Other chronic diseases | ||
| Yes | 50 | 4.3 |
| No | 1109 | 95.7 |
As indicated in Table 1, around one fifth (21.5%) of the women were taking alcohol. However, there were only 1.1% smokers. The result in Table 1 also indicates that 7.0% of their partners were smokers. The highest percentage (40.5%) of the women who participated in the study were in their first pregnancy. We found that 2.3% of women who participated in the study were HIV positive and 4.3% had other chronic diseases.
3.2. Magnitude of household food insecurity
According to responses to the HFIAS in the preceding 4 weeks, worrying about having enough food was reported by 34.8% of the pregnant women. Respondents who affirmed that their households were not able to eat preferred foods, had limited variety of foods, ate some foods that they did not want to eat and at any point had no food to eat in the preceding 4 weeks due to lack of resources were 44.6%, 40.1% 46.2% and 24.8% respectively. Similarly, those who experienced eating smaller meals and fewer meals were (38.1%) and (36.0%), respectively. The proportion of affirmative responses for going to bed hungry and staying a whole day and night without eating anything in the preceding 4 weeks prior to the study were (18.6%) and (13.4%) respectively (Table 2 ).
Table 2.
Status of household food insecurity access scale (HFIAS) questions.
| Household hunger scale indicators in the past 4 weeks | Yes, n(%) | No, n(%) | Percentage of occurrence (yes) |
||
|---|---|---|---|---|---|
| Rarely, n(%) | Sometimes, n(%) | Often, n(%) | |||
| Did you worry that your household would not have enough food? | 403(34.8) | 756(65.2) | 104(9.0) | 225(19.4) | 74(6.4) |
| Were you or any household member not able to eat the kinds of foods you preferred because of a lack of resources? | 517(44.6) | 642(55.4) | 108(9.3) | 301(26.0) | 108(9.3) |
| Did you or any household member have to eat a limited variety of foods due to a lack of resources? | 465(40.1) | 694(59.9) | 113(9.7) | 268(23.1) | 84(7.2) |
| Did you or any household member have to eat some foods that you really did not want to eat because of a lack of resources to obtain other types of food? | 536(46.2) | 623(53.8) | 136(11.7) | 296(25.5) | 104(9.0) |
| Did you or any household member have to eat a smaller meal than you felt you needed because there was not enough food? | 441(38.1) | 718(61.9) | 114(9.8) | 245(21.1) | 82(7.1) |
| Did you or any other household member have to eat fewer meals in a day because there was not enough food? | 417(36.0) | 742(64.0) | 121(10.4) | 226(19.5) | 70(6.0) |
| Was there ever no food to eat of any kind in your household because of lack of resources to get food? | 287(24.8) | 872(75.2) | 80(6.9) | 166(14.3) | 41(3.5) |
| Did you or any household member go to sleep at night hungry because there was not enough food? | 215(18.6) | 944(81.4) | 79(6.8) | 117(10.1) | 19(1.6) |
| Did you or any household member go a whole day and night without eating anything because there was not enough food? | 155(13.4) | 1004(86.6) | 44(3.8) | 94(8.1) | 17(1.5) |
After computing the scores using the nine HFIAS questions, the proportion of those who were food secure was 46.9%, mildly food insecure (12.4%), moderately food insecure (23.0%), while those severely food insecure were 17.8% as indicated in Table 3 . After considering those with at least one experience of the HFIAS questions, 53.1% pregnant women were classified as food insecure during COVID-19 pandemic.
Table 3.
Magnitude of food insecurity among pregnant women in the first trimester.
| Household Food Insecurity status | Count | Percent (95%CI) |
|---|---|---|
| Food secure | 543 | 46.9(43.9–49.8) |
| Mild food insecurity | 144 | 12.4(10.6–14.5) |
| Moderate food insecurity | 266 | 23.0(20.6–25.5) |
| Severe food insecurity | 206 | 17.8(15.6–20.1) |
3.3. Factors associated with household food insecurity among pregnant women in Rwanda during the COVID-19 pandemic
The factors significantly associated with food insecurity at bivariate analysis (p value <0.05) were age of the woman, spouse’s age, residence, marital status, woman’s and spouse’s level of education, ownership of the house, main source of household income, social class category, alcohol use, spouse’s smoking status, and parity. These variables were considered during multivariable logistic regression analysis. After running multivariable analysis seven independent predictors of food insecurity were identified including marital status, level of education, main source of household income, social class category, alcohol use, spouse/partner's smoking status and parity.
According to the results, married women were 0.38 times less likely to be food insecure compared to single women {AOR = 0.38; 95%CI = 0.38–0.68}. Women with no formal education were 4.58 times more likely food insecure than women with tertiary level of education {AOR = 4.58; 95%CI = 1.88–11.15}. Women from households with business as main source of income were 0.6 times less likely food insecure {AOR = 0.60; 95%CI = 0.38–0.97}, than those whose main source of income was monthly salary. Women whose main source of income was from farming were 1.6 times more likely food insecure {AOR = 1.64; 95%CI = 1.09–2.465. Women in the social class one (Poor socio-economic category) were 2.45 times {AOR = 2.45; 95%CI = 1.59–3.76} more likely to have food insecurity compared those in social class three (middle class). Women taking alcohol were 2.47-fold more likely food insecure than those who indicated otherwise {AOR = 2.47; 95%CI = 1.72–3.54}. Similarly, women whose spouses smoked cigarettes were 2.2 times more likely to have food insecurity {AOR = 2.20; 95%CI = 1.18–4.20}. Women with parity one were 1.8 times {AOR = 1.82; 95%CI = 1.27–2.63}, those with parity two 3.2 times {AOR = 3.22; 95%CI = 2.06–50.50}, those with parity three 4 times {AOR = 4.02; 95%CI = 1.18–4.20},those with parity four 3 times {AOR = 3.03; 95%CI = 1.56–5.91} and those with parity five and above 3.8 times {AOR = 3.80; 95%CI = 1.91–7.56} more likely to have household food insecurity than those women who were pregnant for the first time (Table 4 ).
Table 4.
Predictors of household food insecurity among pregnant women in Rwanda.
| Factor | Food insecure, n (%) | Food secure, n (%) | COR (95% CI) | AOR (95% CI) |
|---|---|---|---|---|
| Age in years | ||||
| 15-19 | 41(59.4) | 28(40.6) | 1.42(0.80–2.51) | 0.77(0.37–1.59) |
| 20-35 | 450(49.7) | 455(50.3) | 2.10(1.50–2.94) *** | 0.72(0.46–1.12) |
| >35 | 125(67.6) | 60(32.4) | 1.00 | 1.00 |
| Spouse’s/partner's age in years | ||||
| 15-19 | 10(71.4) | 4(28.6) | 0.52(0.16–1.71) | 0.38(0.10–1.38) |
| 20-35 | 408(51.2) | 389(48.8) | 1.25(0.97–1.62) | 0.73(0.51–1.03) |
| >35 | 198(56.9) | 150(43.1) | 1.00 | 1.00 |
| Residence | ||||
| Rural | 477(58.5) | 338(41.5) | 2.08(1.61–2.69) *** | 1.04(0.75–1.45) |
| Urban | 139(40.4) | 205(59.6) | 1.00 | 1.00 |
| Marital status | ||||
| Married | 306(50.7) | 298(49.3) | 0.51(0.32–0.83) ** | 0.38(0.21–0.68) ** |
| Cohabiting | 254(53.9) | 217(46.1) | 0.58(0.36–0.95) | 0.40(0.23–0.72) |
| Single | 56(66.7) | 28(33.3) | 1.00 | 1.00 |
| Level of education | ||||
| No formal education | 86(79.6) | 22(20.4) | 19.19(8.62–42.70) *** | 4.58(1.88–11.15) ** |
| Primary | 403(58.5) | 286(41.5) | 6.92(3.55–13.46) *** | 1.65(0.78–3.47) |
| Secondary | 116(39.1) | 181(60.9) | 3.15(1.58–6.27) ** | 1.69(0.80–3.57) |
| Tertiary | 11(16.9) | 54(83.1) | 1.00 | 1.00 |
| Spouse/partner's level of education | ||||
| No formal education | 86(80.4) | 21(19.6) | 14.95(7.52–29.72) *** | 2.23(0.93–5.37) |
| Primary | 415(59.0) | 288(41.0) | 5.26(3.14–8.82) *** | 1.45(0.73–2.89) |
| Secondary | 95(37.1) | 161(62.9) | 2.15(1.24–3.76) ** | 1.03(0.53–2.01) |
| Tertiary | 20(21.5) | 73(78.5) | 1.00 | 1.00 |
| Ownership of the house currently reside in | ||||
| Own house | 412(58.7) | 290(41.3) | 1.00 | 1.00 |
| Rented house | 174(41.5) | 245(58.5) | 0.50(0.39–0.64) *** | 0.89(0.65–1.65) |
| Others | 30(78.9) | 8(21.1) | 2.64(1.19–5.84) | 2.08(0.80–5.37) |
| Main source of household income | ||||
| Employed with monthly salary | 106(37.2) | 179(62.8) | 1.00 | 1.00 |
| Owner a small business | 45(25.7) | 130(74.3) | 0.58(0.39–0.88) * | 0.60(0.38–0.97) * |
| Subsistence Farming | 436(67.6) | 209(32.4) | 3.52(2.63–4.71) *** | 1.64(1.09–2.46) * |
| Others | 29(53.7) | 25(46.3) | 1.96(1.09–3.52) * | 1.58(0.79–3.16) |
| Socio-class category | ||||
| aCategory 1 | 135(67.8) | 64(32.2) | 3.33(2.32–4.79) *** | 2.45(1.59–3.76) *** |
| bCategory 2 | 338(57.2) | 253(42.8) | 2.11(1.62–2.75) *** | 2.02(1.47–2.78) *** |
| cCategory 3 | 143(38.8) | 226(61.2) | 1.00 | 1.00 |
| Alcohol use | ||||
| Yes | 183(73.5) | 66(26.5) | 3.05(2.24–4.16) *** | 2.47(1.72–3.54) *** |
| No | 433(47.6) | 477(52.4) | 1.00 | 1.00 |
| Smoking status | ||||
| Yes | 9(69.2) | 4(30.8) | 1.99(0.61–6.52) | |
| No | 607(53.0) | 539(47.0) | 1.00 | |
| Spouse/partner's smoking status | ||||
| Yes | 62(76.5) | 19(23.5) | 3.08(1.82–5.23) *** | 2.20(1.18–4.20) * |
| No | 554(51.4) | 524(48.6) | 1.00 | 1.00 |
| Parity | ||||
| Primigravida | 203(43.3) | 266(56.7) | 1.00 | 1.00 |
| One | 135(50.0) | 135(50.0) | 1.31(0.97–1.77) | 1.82(1.27–2.63) ** |
| Two | 106(62.7) | 63(37.3) | 2.21(1.53–3.16) *** | 3.22(2.06–50.5) *** |
| Three | 77(70.0) | 33(30.0) | 3.06(1.96–4.78) *** | 4.02(2.29–7.08) *** |
| Four | 41(65.1) | 22(34.9) | 2.44(1.41–4.23) ** | 3.03(1.56–5.91) *** |
| Five and above | 54(69.2) | 24(30.8) | 2.95(1.76–4.93) *** | 3.80(1.91–7.56) *** |
| HIV status | ||||
| Positive | 16(59.3) | 11(40.7) | 1.29(0.59–2.80) | |
| Negative | 600(53.0) | 532(47.0) | 1.00 | |
| History of chronic diseases | ||||
| Yes | 30(60.0) | 20(40.0) | 1.34(0.75–2.38) | |
| No | 586(52.8) | 523(47.2) | 1.00 | |
AOR: Adjusted Odds Ratio COR: Crude Odds Ratio; CI: Confidence Interval; *P value <0.05; **P value <0.01; ***P value <0.001.
Category 1: Very poor and vulnerable citizens who were homeless and unable to feed themselves without assistance.
Category 2: Citizens who were able to afford some form of rented or low-class owned accommodation, but who were not gainfully employed and could only afford to eat once or twice a day.
Category 3: Citizens who were gainfully employed or were even employers of labour. This category included small farmers who had moved beyond subsistence farming, or owners of small and medium-scale enterprises.
4. Discussion
The COVID-19 pandemic has affected both the health of billions of people globally and introduced food insecurity to their households. The World Food Programme estimates that in LMICs 272 million people are already or are at risk of becoming acutely food-insecure [20]. The World Bank's latest report indicates the impacts of the pandemic has led to a significant increase in global food insecurity among vulnerable groups in almost every country with the impacts expected to continue [21]. The situation is not different in Rwanda with the current study reporting a 53.1% prevalence of food insecurity among pregnant women during the COVID-19 pandemic. Women further explained that the levels of food insecurity in their households varied, however, the situation had worsened over the period of lockdown. This could have been because of disruption of all activities that relate to food production, processing, distribution, and preparation. It was observed that during lockdown and travel restrictions, households with pregnant women, children, and larger families consistently found it even harder to put food on the table. Increasing food insecurity during the pandemic has been reported in many other settings.
It has been documented that restricting people's movements often result in constraining their economic opportunities [22]. These restrictions have severe health and wellbeing impacts on already poor and vulnerable populations. Many fragile populations, including pregnant women, children, slum dwellers, the sick, cannot make economic sacrifices as they would leave them starving [23,24]. For the poor, tending to livelihood activities, ensuring an income, and food security, represent more of a concern than the possibility of contracting COVID-19.
Food insecurity is critical during pregnancy [16,25]. This is because nutritional requirements increase due to physiological changes that occur in pregnant women such as an increase in basal metabolism caused by accelerated synthesis of fetal, placenta, uterine, mammary tissues, and an increase in metabolically active tissue and cardio-respiratory work. Additionally, the processes to prepare or to get food may become more difficult, and pregnant women may be restricted in doing some activities such as farming, and this, in turn, leads to household food insecurity.
In the multivariate analysis, married women were less likely to be food insecure compared to single women. This is not surprising because in African settings men are by default the household heads and are expected to provide for their family. This is consistent with previous studies which showed that men being the head of the household is associated with a higher likelihood of food security [26,27]. Findings also revealed that women with no formal education were 5 times more likely to be food insecure than their counterparts who were educated. In line with the present findings, low education levels were consistently reported as the main predictor of food insecurity among the women [[28], [29], [30]]. This is due to the fact that most women with low education are unemployed, have lower earning capacity and mostly depend on their husbands for provision.
Findings on social class indicated that women who were in lower social class were more likely to be food insecure, compared to those in higher social class. The finding is consistent with a study conducted in South Africa, which found that food insecurity was prevalent (42%) among women from low socio-economic conditions [31]. This is because people in lower socioeconomic classes depend on daily wages and casual labor which were severely disrupted during the pandemic, rendering them food insecure. The protective effects of marriage, education, and higher socioeconomic status on food insecurity were also reported in a similar study in Nepal [32].
Increasing parity was also found to be associated with food insecurity. Women with higher parity were two to four times more likely to be food insecure compared to those who were pregnant for the first time. This is because higher parity increases women’s social vulnerability and hence increases their risk of household food insecurity. A recent study conducted in the US reported that households with children were at high risk of food insecurity during COVID-19 pandemic [33]. However, this study did not directly assess the effect of the number of children on the severity of food insecurity during COVID-19 pandemic.
As previously demonstrated [34], substance use was also found to be positively associated with food insecurity with those who took alcohol or whose partners smoked being more likely to be food insecure than their counterparts. The relationship between substance use and food insecurity has been shown to be bidirectional. A high prevalence (21.5%) of alcohol consumption during pregnancy was observed among pregnant women in Rwanda. Similarly, this high prevalence of alcohol consumption during pregnancy has been observed in other African countries for example alcohol consumption during pregnancy was reported as 20.5% in Uganda and 18.5% in Zambia [35]. Alcohol consumption during pregnancy in most African countries may be influenced by lack of access to public health information about the negative effect of alcohol consumption during pregnancy [36]. It may also be influenced by the low-cost of locally made alcoholic beverages that are commonly sold without a license.
The strengths of the study include the use of the standardized tool to assess food security status among pregnant women as well as using a large country-wide representative sample. Nevertheless, the findings should be considered in the following context: The timing of the harvest season and COVID-19 restrictions could have played a big role in food insecurity levels; food security status was assessed using self-report, and hence recall bias also could have played a role as respondents were interviewed regarding their food intake in the preceding 4 weeks and therefore, the prevalence of food insecurity during pregnancy may have been overestimated in the current study. It should also be noted that the nature of cross-sectional study design may not effectively establish a cause-effect relationship. Despite those limitations, the study contributes significantly to the knowledge on the status of food security among pregnant women during the COVID-19 pandemic.
5. Conclusions
From the above findings, it can be concluded that food insecurity at the household level increased during the COVID-19 pandemic and pregnant women were most affected. Nutrition-sensitive interventions to boost agricultural productivity in general and more specifically targeting women of reproductive age are potential areas of intervention in reducing food insecurity faced by pregnant women and can aid in achieving the SDG indicator targets related to food security. Other interventions that could reduce food insecurity include the introduction of organic farming, community awareness campaigns of food security, food storage, and utilization. There is a need to include screening for food insecurity in antenatal care package, this will provide a unique opportunity to identify pregnant women at-risk of food insecurity. Furthermore, during the period of pandemic community health workers should be engaged in identifying pregnant women from food insecure households, this will provide an early opportunity to connect them with the supplemental nutrition assistance program at community level or at health facilities.
Ethics approval and consent to participate
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving research study participants were approved by the Rwanda National Ethics Committee with reference number No.131/RNEC/2020 and permission letter was obtained from each selected Hospitals. Written informed consent was obtained from all subjects."
Consent for publication
Not applicable.
Funding
This research was funded by the Rwanda National Council of Science and Technology (NCST). The funding body was not involved in any part of the study design, implementation, or analysis.
Authors' contributions
The authors’ responsibilities were as follows- ER, MH, NG, MM: Designed the research protocol, followed up data collection, and had primary responsibility for the final content; VM, CN, PM: contributed to the design of the study, data analysis, and report writing, and all authors: read and approved the final manuscript.
Declaration of competing interest
The authors declare that they have no conflict of interests.
Acknowledgements
This work was carried out with financial support from the Government of Rwanda through National Council for Science and Technology under Excellence Research Grant with grant Number: NCST-NRIF/ERG-BATCH1/P05/2019. We gratefully acknowledge the contribution of participating mothers, nurses, midwives, hospitals, and health centers.
List of abbreviations
- ANC
Antenatal care
- CFSVA
Comprehensive food security and vulnerability analysis
- HFIAS
Household food insecurity access scale
- LMP
Last menstrual period
- FANTA
Food and Nutrition Technical Assistance
- FAO
Food and Agricultural Organization
- FI
Food insecurity
- SDGs
Sustainable development goals
Data availability
Data will be made available on request.
References
- 1.Bickel Gary, Mark Nord, Cristofer Price, William Hamilton, Cook J: Guide to Measuring Household Food Security, Revised 2000. U.S. Department of Agriculture, Food and Nutrition Service, Alexandria VA. March, 2000. Or in short form as USDA, Guide 2000. 2000.
- 2.FAO. IFAD. UNICEF. WFP . FAO; Rome: 2020. WHO: the State of Food Security and Nutrition in the World 2020. Transforming Food Systems for Affordable Healthy Diets. [DOI] [Google Scholar]
- 3.FAO. ECA. AUC . Transforming Food Systems for Affordable Healthy Diets. FAO; Accra: 2020. Africa regional overview of food security and nutrition. [Google Scholar]
- 4.NISR: Rwanda . 2018. Comprehensive Food Security and Vulnerability Analysis 2018. [Google Scholar]
- 5.Shahzad M.A., Qing P., Rizwan M., Razzaq A., Faisal M. COVID-19 pandemic, determinants of food insecurity, and household mitigation measures: a case study of Punjab, Pakistan. Healthcare. 2021;9:621. doi: 10.3390/healthcare9060621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.UN-Rwanda . 2020. The Socio-Economic Impact of COVID-19 in Rwanda. [Google Scholar]
- 7.FAO Global strategic framework for food security & nutrition (GSF); committee on world foodsecurity. 2014. https://www.fao.org/fileadmin/templates/cfs/Docs1314/GSF/GSF_Version_3_EN.pdf
- 8.Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C.…Agha R. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int. J. Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Water for Food COVID-19 impact on agricultural entrepreneurship in Rwanda. https://waterforfood.nebraska.edu/-/media/projects/dwfi/blogs/2020/research-handouts/covidagentrepreneurship.pdf
- 10.Kansiime M.K., Tambo J.A., Mugambi I., Bundi M., Kara A., Owuor C. COVID-19 implications on household income and food security in Kenya and Uganda: findings from a rapid assessment. World Dev. 2021;137 doi: 10.1016/j.worlddev.2020.105199. pmid:32982018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.HLPE Impacts of COVID-19 of food security and nutrition: developing effective policy responses to address the hunger and malnutrition pandemic. 2020. Rome. [DOI]
- 12.Sen A. Oxford University Press; Oxford: 1981. Poverty and Famines. ([Google Scholar]) [Google Scholar]
- 13.Kazemi F., Masoumi S.Z., Shayan A., Shahidi Yasaghi S.Z. Prevalence of food insecurity in pregnant women and its association with gestational weight gain pattern, neonatal birth weight, and pregnancy complications in Hamadan County, Iran. Agric. Food Secur. 2018;9(1):12. 2020. [Google Scholar]
- 14.Park Cy, Fau - Eicher-Miller H.A., Ha E.-M. - Iron deficiency is associated with food insecurity in pregnant females in the United States: National Health and Nutrition Examination Survey 1999-2010. J. Acad. Nutr. Diet. 2014;114(12):1967–1973. doi: 10.1016/j.jand.2014.04.025. [DOI] [PubMed] [Google Scholar]
- 15.W R.C., Phillips Sm Fau, Orzol S.M., O S.M. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics. 2006;118(3) doi: 10.1542/peds.2006-0239. 2006-0239. [DOI] [PubMed] [Google Scholar]
- 16.Alanderson Alves Ramalho, Andrade Martins Fernanda, Jorge K.R. Food insecurity during the gestational period and factors associated with maternal and child health. J Nutr Health Food Eng. 2017;7(4):337–343. 10.15406/jnhfe.2017.07.00245. 2017. [Google Scholar]
- 17.Gresham E., Bisquera A., Byles J.E., Hure A.J. Effects of dietary interventions on pregnancy outcomes: a systematic review and meta-analysis. Matern. Child Nutr. 2016;12(1):5–23. doi: 10.1111/mcn.12142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.SIPRING/FANTA: Household Food Insecurity Access Scale (HFIAS) for Measurement of Food Access Indicators Guide. 2007. [Google Scholar]
- 19.Deitchler M., Ballard T., Swindale A., Coates J. 2010. Validation of a Measure of Household Hunger for Cross-Cultural Use. [Google Scholar]
- 20.WFP: World Food Programme . 2020. COVID-19 Will Double Number of People Facing Food Crises unless Swift Action Is Taken.https://wwwwfporg/news/covid-19-will-double-number-people-facing-food-crises-unless-swift-action-taken [Google Scholar]
- 21.WB: The World Bank . 2022. Food Security and COVID-19.https://wwwworldbankorg/en/topic/agriculture/brief/food-security-and-covid-19 [Google Scholar]
- 22.Jackson James K., Weiss Martin A., Schwarzenberg Andres B., Nelson Rebecca M., Sutter Karen M., Sutherland M.D. Global economic effects of COVID-19. 2021. https://sgp.fas.org/crs/row/R46270.pdf
- 23.Dahab M., van Zandvoort K., Flasche S., Warsame A., Ratnayake R., Favas C., Spiegel P.B., Waldman R.J., Checchi F. COVID-19 control in low-income settings and displaced populations: what can realistically be done? Conflict Health. 2020;14(1):54. doi: 10.1186/s13031-020-00296-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choithani C. What happens to the wives of male migrant workers, who run entire households in villages? Available at. 2020. https://thewire.in/women/lockdown-migrant-workers-wives
- 25.Laraia B.A., Siega-Riz A.M., Gundersen C., Dole N. Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. J. Nutr. 2006;136(1):177–182. doi: 10.1093/jn/136.1.177. 110.1093/jn/1136.1091.1177. [DOI] [PubMed] [Google Scholar]
- 26.Mbunge E. Effects of COVID-19 in South African health system and society: an explanatory study. Diabetes Metabol. Syndr. 2020;14(6):1809–1814. doi: 10.1016/j.dsx.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bapolisi W.A., Ferrari G., Bisimwa G., Merten S. Gendered determinants of food insecurity in ongoing regional conflicts, North and South Kivu, the Democratic Republic of Congo. Agric. Food Secur. 2021;10(1):13. [Google Scholar]
- 28.Zm S., Sulaiman N Fau, Jalil R.A., Jalil Ra Fau, Yen W.C., Yen Wc Fau, Yaw Y.H., Yaw Yh Fau, Taib M.N.M., Taib Mn Fau, Kandiah M., Fau - Lin K.G., Kg L. Food insecurity and the metabolic syndrome among women from low income communities in Malaysia. Asia Pac. J. Clin. Nutr. 2014;23(1):138–147. doi: 10.6133/apjcn.2014.23.1.05. Kandiah M. [DOI] [PubMed] [Google Scholar]
- 29.Bawadi H.A., Tayyem R.F., Dwairy A.N., Al-Akour N. Prevalence of food insecurity among women in northern Jordan. J. Health Popul. Nutr. 2012;30(1):49–55. doi: 10.3329/jhpn.v30i1.11276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Demétrio F., Teles C.A.S., Santos D.B.D., Pereira M. Food insecurity in pregnant women is associated with social determinants and nutritional outcomes: a systematic review and meta-analysis. Ciência Saúde Coletiva. 2020;25(7):2663–2676. doi: 10.1590/1413-81232020257.24202018. 2610.1590/1413-81232020257.81224202018. [DOI] [PubMed] [Google Scholar]
- 31.Abrahams Z., Lund C., Field S., Honikman S. Factors associated with household food insecurity and depression in pregnant South African women from a low socio-economic setting: a cross-sectional study. Soc. Psychiatr. Psychiatr. Epidemiol. 2018;53(4):363–372. doi: 10.1007/s00127-018-1497-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pandey S., Fusaro V. Food insecurity among women of reproductive age in Nepal: prevalence and correlates. BMC Publ. Health. 2020;20(1):175. doi: 10.1186/s12889-020-8298-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Parekh N., Ali S.H., O'Connor J., Tozan Y., Jones A.M., Capasso A., Foreman J., DiClemente R.J. Food insecurity among households with children during the COVID-19 pandemic: results from a study among social media users across the United States. Nutr. J. 2021;20(1):73. doi: 10.1186/s12937-021-00732-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim-Mozeleski JE, Pandey R: The Intersection of Food Insecurity and Tobacco Use: A Scoping Review. In. [DOI] [PMC free article] [PubMed]
- 35.Popova S., Lange S., Probst C., Shield K., Kraicer-Melamed H., Ferreira-Borges C., Rehm J. Actual and predicted prevalence of alcohol consumption during pregnancy in the WHO African Region. Trop. Med. Int. Health. 2016;21(10):1209–1239. doi: 10.1111/tmi.12755. [DOI] [PubMed] [Google Scholar]
- 36.Adusi-Poku Y., Edusei A.K., Bonney A.A., Tagbor H., Nakua E., Otupiri E. Pregnant women and alcohol use in the Bosomtwe district of the Ashanti region-Ghana. Afr. J. Reprod. Health. 2012;16(1):55–60. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.