Abstract
Background
Salivary gland tumours (SGT) are a relatively rare group of neoplasms with a wide range of histopathological appearance and clinical features. To date, most of the epidemiological studies on salivary gland tumours are limited for a variety of reason including being out of date, extrapolated from either a single centre or country studies, or investigating either major or minor glands only.
Methods
This study aimed to mitigate these shortcomings by analysing epidemiological data including demographic, anatomical location and histological diagnoses of SGT from multiple centres across the world. The analysed data included age, gender, location and histological diagnosis from fifteen centres covering the majority of the world health organisation (WHO) geographical regions between 2006 and 2019.
Results
A total of 5739 cases were analysed including 65% benign and 35% malignant tumours. A slight female predilection (54%) and peak incidence between the fourth and seventh decade for both benign and malignant tumours was observed. The majority (68%) of the SGT presented in major and 32% in the minor glands. The parotid gland was the most common location (70%) for benign and minor glands (47%) for malignant tumours. Pleomorphic adenoma (70%), and Warthin’s tumour (17%), were the most common benign tumours whereas mucoepidermoid carcinoma (26%) and adenoid cystic carcinoma (17%) were the most frequent malignant tumours.
Conclusions
This multicentre investigation presents the largest cohort study to date analysing salivary gland tumour data from tertiary centres scattered across the globe. These findings should serve as a baseline for future studies evaluating the epidemiological landscape of these tumours.
Keywords: Salivary gland tumours, Salivary gland neoplasms, Head and neck, Multicentre research study, Demographics, Epidemiology, Site distribution, Histological diagnosis
Introduction
Salivary gland tumours (SGT) are a heterogeneous group of neoplasms with a wide range of histological subtypes making diagnosis challenging for pathologists. Fortunately, they are rare, with an annual estimated incidence of approximately 2.5–3.0 per 100 000 people in the Western world [1].
Most SGT are benign with ~ 70% arising in major glands and ~ 25% are from the minor glands. Malignant SGT comprise approximately 2–6% of all head and neck cancers [1, 2] with 15–35% of parotid gland, 41–45% of submandibular and 70–90% of sublingual glands tumour being malignant [3]. In comparison, more than half of the minor glands tumours (including palate, tongue, the floor of the mouth, retromolar region and lips) are likely to be malignant [3–5]. Other rare sites for SGT include the larynx, trachea, lacrimal glands, nasal cavity and heterotopic salivary tissue within the mandible and the lymph nodes [4]. Tumours involving minor glands have worse prognosis, higher recurrence rate and poor outcomes compared to major gland tumours [6].
To date, numerous studies have reported epidemiological data for SGT. However, they are somewhat out of date or reflect relatively small datasets from a single centre or local population only [4, 5, 7–17]. One of the most recent studies from 2012 reported incidence of these tumours in two distant geographical locations without detailed comparative analysis [18]. These shortcomings necessities the need for epidemiological evaluation of SGT from multiple centres preferably different geographical locations across the world with a view to analysing the distribution of different subtypes of SGT as well as identifying trends in the different populations.
Therefore, the aim of this multicentre international study was to analyse SGT data from numerous tertiary hospitals across the world with a view to obtaining up to date frequency and distribution of SGT. Further investigation of demographic and anatomical location of SGT and correlation of findings from different geographical locations was also performed.
Material and Methods
All salivary gland tumours diagnoses between 2006 to 2019 were retrieved from the Pathology databases of the involved Oral and Maxillofacial/Head and Neck Pathology departments. The year 2006 was selected in this study as cut-off year for two main reasons; (1) A number of SGT overviews were published prior to this including analysis of a large cohort from the Lead Institute and (2) Since then there have been significant changes to histological classification of SGT. The UK centres included Sheffield (School of Clinical Dentistry, University of Sheffield and Sheffield Teaching Hospitals NHS Foundation Trust), East Grinstead (Queen Victoria Hospital), Belfast (Belfast Health and Social Care Trust/Queen’s University Belfast), and two centres in London (Royal London Hospital and University College London Hospital). The international collaborators included centres from Italy (Department of Pathology, Camposampiero), Turkey (Department of Tumour Pathology, Istanbul University), Nigeria (including Ibadan, Lagos, Enugu and Port-Harcourt), South Africa (University of Pretoria), Saudi Arabia (Department of Oral Medicine and Diagnostic Sciences, College of Dentistry, King Saud University, Riyadh), Brazil (Piracicaba Dental School, University of Campinas, São Paulo State) and Chile (Universidad de Valparaíso, School of Dentistry) (Fig. 1). These were split into regions for some of the comparative analysis.
Fig. 1.
Geographical map of the centres participating in the study including five from the UK, one from Europe, five from Africa, two from Asia and two centres from South America
All primary benign and malignant tumours in major and minor salivary glands were included. Other mesenchymal neoplasms and lymphomas were excluded. Clinical information about gender and age of the patient as well as the anatomical site of presentation (major gland or intra-oral location) was also obtained. Tumours involving the sinonasal region, nose and trachea were excluded. The data was anonymised locally before being shared for analysis. Cases with incomplete information were excluded after an initial review and duplicates and recurrences were also removed. Where possible, the histological diagnosis of the cases was reviewed (65% of cases). However due to the large number of cases in the cohort and the resource constraints, this was not possible for every case. Only the updated diagnosis was used for these cases and diagnosis concordance or discordance was not recorded as it was not available for all cases and was deemed beyond the scope of this study. The tumours were classified according to the 2017 WHO classification of salivary gland tumours (18). Twelve types of benign SGT were identified within the cohort, including common entities such as pleomorphic adenoma, Warthin tumour, basal cell adenoma and canalicular adenoma etc. For malignant SGT, 20 different tumour types were identified including mucoepidermoid carcinoma (MEC), adenoid cystic carcinoma (AdCC), acinic cell carcinoma (ACC), polymorphous adenocarcinoma (PAC), carcinoma ex pleomorphic adenoma (Ca ex PA) and adenocarcinoma NOS (AdNOS). Descriptive statistical analysis of the data was performed using frequencies and percentages of the variables in Microsoft Excel (2016). Student’s T test was used to determine statistical significance (where relevant).
Results
Overall
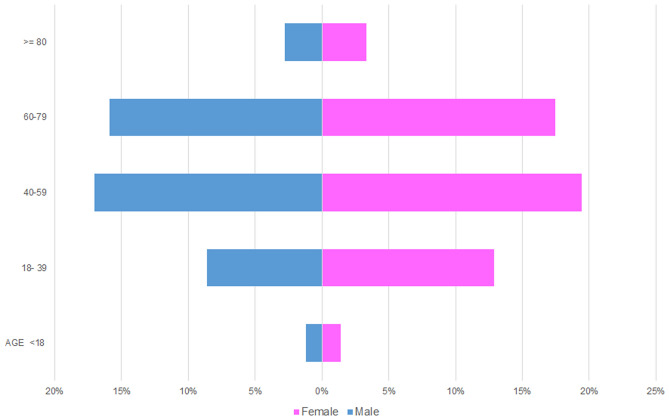
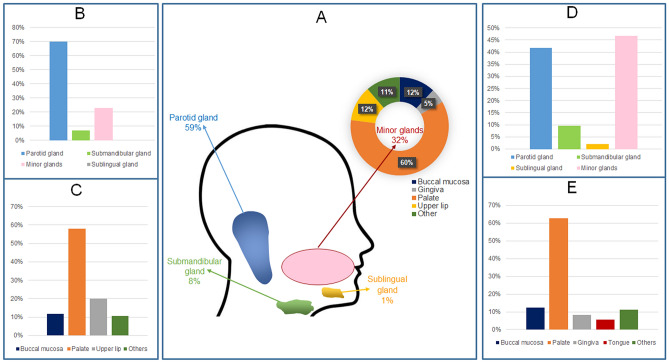
The total number of SGT was 5,739. Of these, 65% were benign tumours (n = 3,751), and 35% (n = 1,988) were malignant (Table 1). There was a slight female predilection (54%, n = 3,093) compared to 46% male patients (n = 2,646). In both benign and malignant tumours, a higher incidence was noted in patients between the fourth to seventh decade of life accounting for 69% of the cases (Fig. 2). Most of the SGT involved the major glands 68% (n = 3,910) with 32% (n = 1,829) involving the minor glands. Parotid gland was the most common site of involvement (59%, n = 3,406). Within the minor glands, the palate was the most common location (60%, n = 1103) (Fig. 3).
Table 1.
Benign and malignant SGT histological subtype distribution within the cohort
| Diagnosis | Number | % of group | % of all tumours |
|---|---|---|---|
| Benign | |||
| Pleomorphic adenoma | 2621 | 70% | 45% |
| Warthin tumour | 623 | 17% | 11% |
| Basal cell adenoma | 172 | 5% | 3% |
| Canalicular adenoma | 96 | 2% | 2% |
| Cystadenoma | 81 | 2% | 1% |
| Myoepithelioma | 62 | 2% | 1% |
| Oncocytoma | 43 | 1% | 1% |
| Other | 53 | 1% | 1% |
| Benign total | 3751 | ||
| Malignant | |||
| Mucoepidermoid carcinoma | 508 | 26% | 9% |
| Adenoid cystic carcinoma | 336 | 17% | 6% |
| Polymorphous adenocarcinoma | 238 | 12% | 4% |
| Carcinoma ex pleomorphic adenoma | 215 | 11% | 4% |
| Acinic cell carcinoma | 185 | 9% | 3% |
| Adenocarcinoma NOS | 145 | 7% | 3% |
| Salivary duct carcinoma | 79 | 4% | 1% |
| Secretory carcinoma | 51 | 3% | 1% |
| Epithelial myoepithelial carcinoma | 47 | 2% | 1% |
| Myoepithelial carcinoma | 42 | 2% | 1% |
| Basal cell adenocarcinoma | 41 | 2% | 1% |
| Other | 101 | 5% | 2% |
| Malignant total | 1988 | ||
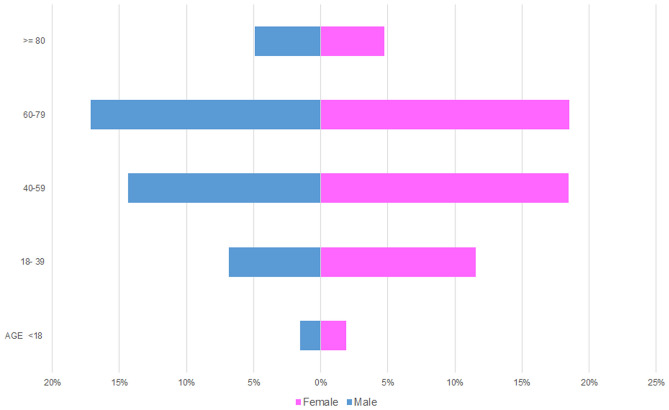
Fig. 2.
Age and gender distribution within the entire SGT cohort
Fig. 3.
Anatomical site distribution of SGT. A major and minor gland distribution across the entire cohort. B Benign tumours in all glands. C Benign tumours in minor glands. D Malignant tumours in all glands. E Malignant tumours in minor glands
Benign Tumours
The most common benign tumour was pleomorphic adenoma accounting for 70% (n = 2621) followed by Warthin tumour (17%, n = 623), basal cell adenoma (3%, n = 172), canalicular adenoma (2%, n = 96), cystadenoma (2%, n = 81), myoepithelioma (2%, n = 62) and oncocytoma (1%, n = 43). All other rare benign tumours including sebaceous adenoma, ductal papilloma, sialoadenoma papilliferum and unclassified salivary tumours comprised 1% (n = 53) of benign tumours (Table 1).
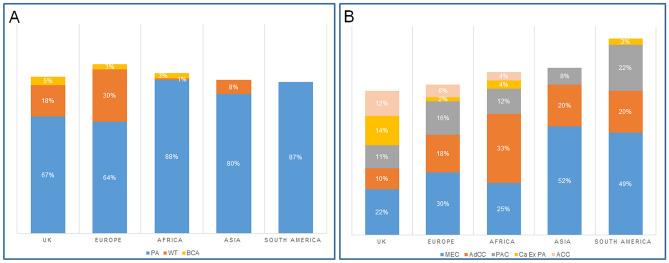
Comparison of the different geographical locations showed that pleomorphic adenoma was the most common benign tumour across all centres with a different range of incidence between centres ranging from 64% in Europe to 87% in South America. Warthin tumour was the second most common tumour for most of the centres with a range of incidence between 1% (African cohort) to 30% in the data from Europe. This was followed by basal cell adenoma accounting for 5% of the UK and 3% of both the European and African cases (Fig. 4).
Fig. 4.
Geographic comparison of the most common benign and malignant SGT. A benign tumours: PA-Pleomorphic adenoma, WT-Warthin tumour, BCA-Basal cell adenoma. B malignant tumours: MEC mucoepidermoid carcinoma, AdCC adenoid cystic carcinoma, PAC polymorphous adenocarcinoma, Ca ex PA carcinoma ex pleomorphic adenoma, ACC Acinic cell carcinoma
Gender Distribution
For benign tumours, there was a slight female predilection (54%, n = 2035) compared to males (46%, n = 1716).
Age Distribution
The average age for benign tumours was 52 years with a female average age of 51.7 and male average of 52.4 years. The age range was very wide (1–98 years). The most commonly affected age group was 40–59 which accounted for 38% of benign tumours (n = 1440) comprising 18% of male (n = 692) and 20% female (n = 748) patients respectively. The least affected age group was patients under 18 years of age who accounted for only 2% (n = 82) of benign tumours (Fig. 5).
Fig. 5.
Age and gender distribution for benign salivary gland tumours
Site Distribution
Benign tumours presented in both major and minor glands with the majority of tumours involving the parotid gland (70%, n = 2582), followed by minor glands (23%, n = 899), submandibular gland (7%, n = 265) and less than 1% (n = 5) involving the sublingual gland. Within the minor glands, the palate was the most common location (58%, n = 519). followed by upper lip (20%, n = 178) and buccal mucosa (12%, n = 104). Other sites included the floor of mouth, gingiva, lower lip, tongue and labial mucosa which altogether comprised 10% (n = 98) of benign tumours (Fig. 3).
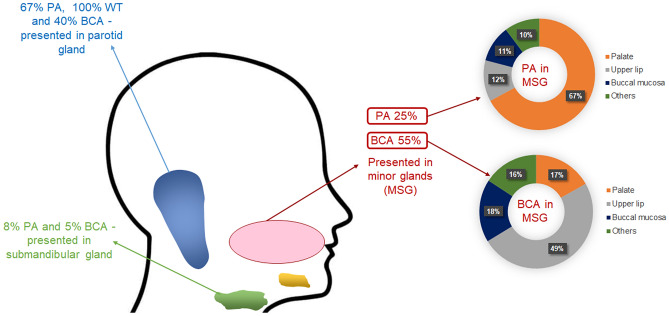
The majority of pleomorphic adenomas involved the parotid gland (67%, n = 1736), followed by minor glands (25%, n = 645) and submandibular gland (8%, n = 217). Only four cases (less than 1%) were identified in the sublingual gland. In the minor glands, (67%, n = 433) of the pleomorphic adenomas involved the palate, followed by upper lip and buccal mucosa (12%, n = 77, 11%, n = 69) respectively. Warthin tumours were exclusive to the parotid gland (n = 623). Most of the basal cell adenomas were reported in minor glands (55%, n = 95), followed by parotid gland (40%, n = 69) and submandibular gland (5%, n = 8). In the minor glands, the upper lip was the most common minor gland site for basal cell adenomas (49%, n = 47) (Fig. 6).
Fig. 6.
Anatomical site distribution of the most common benign SGT. Pleomorphic adenoma (PA), Warthin tumour (WT) and basal cell adenoma (BCA)
Malignant Tumours
The most common malignant tumour was mucoepidermoid carcinoma accounting for 26% of the malignant diagnoses (n = 508) followed by adenoid cystic carcinoma (17%, n = 336), polymorphous adenocarcinoma (12%, n = 238), carcinoma ex pleomorphic adenoma (11%, n = 215), acinic cell carcinoma (9%, n = 185), adenocarcinoma NOS (7%, n = 145), salivary duct carcinoma (4%, n = 79), secretory carcinoma (3%, n = 51), epithelial myoepithelial carcinoma (2%, n = 47), myoepithelial carcinoma (2%, n = 42) and basal cell adenocarcinoma (2%, n = 41). All other rare malignant tumours including, carcinosarcoma, clear cell carcinoma, cystadenocarcinoma, intraductal carcinoma, lymphoepithelial carcinoma, neuroendocrine carcinoma, oncocytic carcinoma, poorly differentiated carcinoma, sebaceous carcinoma, sialoblastoma and squamous cell carcinoma accounted for 5% of malignant tumours collectively (n = 101) (Table 1).
Mucoepidermoid carcinoma was the most common malignant tumour in the majority of centres. The only exception was Africa, where adenoid cystic carcinoma was the most common tumour. Overall, adenoid cystic carcinoma was the second most common malignant SGT for most of the centres with a range of incidence of 10% in UK and 33% in African centres. (Fig. 4).
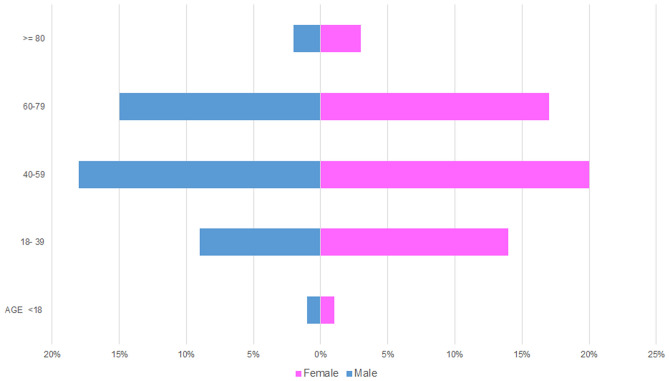
Gender Distribution
There was a slight female predilection for malignant SGT (53% of malignant cases, n = 1,058) compared to males (47%, n = 930).
Age Distribution
The average age for malignant tumours was 56 years with a female average of 54.4 and male average age of 57.4 years. As for benign tumours, the age range was very wide (1 to 106 years). The average age for malignant tumours was significantly higher than benign tumours (p < 0.00001). The most affected age group was 60 to 79-year-old accounting for 36% (n = 708) of malignant tumours, comprising 17% male (n = 340) and 19% female (n = 368) patients respectively. Similar to the benign tumours, the least affected age group was patients under 18 years of age (4%, n = 69) (Fig. 7).
Fig. 7.
Age and gender distribution for malignant tumours
Site Distribution
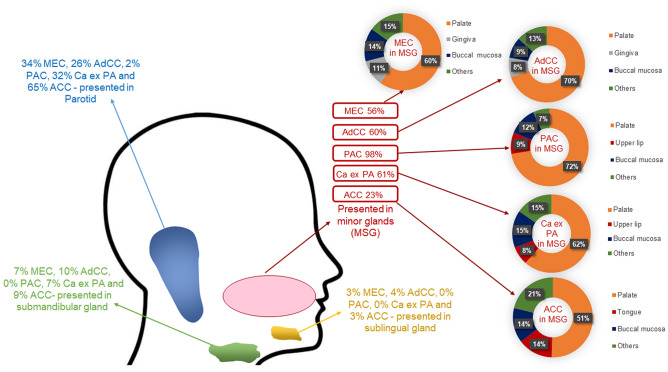
Minor glands were the most common site for malignant tumours (47%, n = 930), followed by parotid gland (42%, n = 828), submandibular gland (10%, n = 189) and sublingual gland (2%, n = 41). Within the minor glands, the palate was the most common location (63%, n = 584) followed by buccal mucosa (12%, n = 114), gingiva (8%, n = 78) and tongue (6%, n = 51). Other rare sites included the floor of the mouth, labial mucosa, upper and lower lip, which accounted altogether for 11% of malignant diagnoses (n = 103) (Fig. 3).
The majority of mucoepidermoid carcinomas involved the minor glands (56%, n = 285), followed by the parotid gland (34%, n = 173), submandibular glands (7%, n = 36) and sublingual glands (3%, n = 12). In the minor glands, 60% (n = 172) of the mucoepidermoid carcinomas occurred in the palate. Most of the adenoid cystic carcinomas (60%, n = 203) involved the minor glands, followed by parotid (26%, n = 87), submandibular (10%, n = 33) and sublingual (4%, n = 13) glands. Within the minor glands, 70% of adenoid cystic carcinomas presented in the palate (n = 141). Most polymorphous adenocarcinomas presented in the minor glands (98%, n = 234), with occasional cases in the parotid gland (2%, n = 4). In the minor glands, the palate was the most common site for the polymorphous denocarcinomas accounting for (72%, n = 170). The majority of carcinoma ex pleomorphic adenomas involved the minor glands (61%, n = 132), followed by the parotid gland (32%, n = 70), submandibular gland (7%, n = 13) and only one case was reported in the sublingual gland. In the minor glands, 62% (n = 82) of carcinoma ex pleomorphic adenomas occurred in the palate. Parotid gland was also the most common site for acinic cell carcinoma (65%, n = 120), followed by the minor glands (23%, n = 42), submandibular gland (9%, n = 17) and sublingual gland (3%, n = 5). The palate was the most common minor gland site for acinic cell carcinomas (50%, n = 21) (Fig. 8).
Fig. 8.
Anatomical site distribution of the most common malignant SGT. Mucoepidermoid carcinoma (MEC), adenoid cystic carcinoma (AdCC), polymorphous adenocarcinoma (PAC), carcinoma ex pleomorphic adenoma (Ca ex PA) and acinic cell carcinoma (ACC)
Discussion
SGT are rare and our study is one of the most extensive recent reports investigating the incidence and demographics of these tumours from multiple centres and the majority of the WHO geographical regions. We collected 5739 cases from pathology centres across the world and found that benign tumours accounted for the majority of SGT (65%) compared to malignant tumours (35%). This finding is consistent with the existing literature [10, 14, 19–21]. There was a slight predilection for females in our study, which has also been reported by some other studies [4, 18, 21–23]. However, some single centres studies have reported a higher incidence of salivary gland tumours in males or an equal gender involvement [9, 10, 12, 13]. Furthermore, we found a peak incidence of SGT between the fourth to seventh decades of life (approximately 69% of cases) which is similar to findings previously reported in the literature [4, 10, 18, 23].
Overall, the parotid gland was the most common location for SGTs accounting for (59%) followed by minor (32%) and submandibular (8%) salivary glands similar to older and similarly large SGT demographical studies [10, 18–24]. Our study shows low prevalence of sublingual tumours (46 out of 5739), similar to findings reported by Satko et al. and Eveson and Cawson [20, 24].
Benign SGT
Our results show that pleomorphic adenoma was the most common benign tumour; this is consistent with prevalence rates reported in the literature [4, 5, 8, 10, 12, 14, 18, 21]. Comparison of incidence between centres showed pleomorphic adenoma to be the most common benign tumour in all geographical locations included in the study ranging from 64% in Europe to 87% in South America. Warthin tumour was the second most common benign tumour which is also similar to earlier demographical studies [8, 11, 18, 23–25]. The present study shows that basal cell adenoma was the third most common benign tumour; however accurate comparisons between previous studies of basal cell and canalicular adenomas is difficult as older studies tended to combine these into a single group of monomorphic adenomas [7, 21, 26]. Curiously no basal cell adenomas were reported in Asia and South America, whereas they comprised 5% of benign SGT in the UK and 3% in both European and African centres. This could be related to the smaller number of cases gathered from these centres or the lower incidence as previous studies have shown that basal cell adenoma is not within the most common five benign tumours in these regions [22, 23, 27]. The possibility of variation in diagnostic criteria can also not be excluded.
In the literature, benign tumours have been reported to occur more in younger and female patients [23]. Our study shows a similar finding where benign tumours appeared to be more common in female patients; however, the average ages were quite similar (51.7 years in female compared to 52.4 in male patients).
The majority of the benign tumours were located in the parotid gland (70%), followed by minor [23%] and submandibular (7%) glands. We found only five benign cases (less than 1%) involving the sublingual gland. Similar findings were seen in other older SGT studies with some variations in distribution across different anatomical sites [4, 10, 14, 18, 21, 23].
The most common location for the pleomorphic adenoma was the parotid gland (67%), followed by minor glands and the submandibular gland (25% and 8% respectively. This observation was consistent with previous reports [4, 11, 13, 18, 23]. Warthin tumour was seen exclusively in the parotid gland (100%). This observation is similar to other studies suggesting that this tumour exclusively involves parotid gland [11, 13, 23]. Basal cell adenomas were reported in minor glands in 55% of the cases and about 40% were seen in the parotid gland. Accurate comparison with the literature was not possible due to the small number of reported studies and cases.
Malignant SGT
Mucoepidermoid carcinoma was the most common malignant salivary gland tumour accounting for 26% of diagnoses; this is in agreement with previously reported prevalence rates worldwide [4, 8, 21, 23]. We found that mucoepidermoid carcinoma was the most common tumour in all centres except Africa where adenoid cystic carcinoma (33%) was the most common malignant diagnoses. Bello et al., 2012, reported somewhat similar findings with adenoid cystic carcinoma as the most common malignant tumour in their 2012 study [18]. However, this was limited to data from two centres and did not examine the geographical differences in depth. The second most common malignant diagnosis for most of the centres in our study was adenoid cystic carcinoma accounting for 17% of all malignancies similar to other reports [5, 8, 11, 12, 21, 23] although some variations in its incidence have been reported. For mucoepidermoid carcinoma and adenoid cystic carcinoma molecular techniques such as FISH, PCR and NGS can help with the final diagnosis however, these tests are not widely available and/or affordable around the world [28]. Even in the UK, routine testing for MAML2 rearrangement in mucoepidermoid carcinoma has been the norm only since 2015–2016 with FISH the most widely available test, whereas MYB testing in adenoid cystic carcinoma is still only available in a handful of specialist centres. This is shown by the fact that within our cohort, a limited number of cases (2015 onwards) were tested (50 mucoepidermoid carcinomas and 15 adenoid cystic carcinomas). The next most common diagnoses were polymorphous adenocarcinoma and carcinoma ex pleomorphic adenoma accounting for 12 and 11% of diagnoses respectively. In fact, there is significant variability in the literature about the incidence of these two entities which is perhaps related to small and unicentric cohorts. Similarly, acinic cell carcinoma was the fifth most common diagnosis (9%) although, some studies have reported it as the third most common malignant SGT [4, 5] however these findings were also based on a small cohort size from only one centre. Adenocarcinoma NOS was the next most common diagnosis accounting for 7% of cases which may not reflect the exact incidence of this entity as development of ancillary molecular and sequencing techniques has led to more specific diagnoses and reduction in the use of this diagnosis [29].
Malignant SGT are more likely to occur in older patients [22, 23]. Our study shows similar results where the average age for malignant tumours was significantly higher than benign tumours (p < 0.00001). Malignant SGT involved the parotid gland in about 42% of cases, which aligns with known literature [11, 14]. The incidence of malignant tumours in minor salivary glands was slightly higher than the parotid gland (i.e. 47%), highlighting the importance of considering malignant SGT in differential diagnoses [14, 30]. In the present study, 42 out of 46 cases involving the sublingual gland were malignant tumours, which is similar to Tian et al.’s findings from 2010 where they reported 95% of sublingual tumours to be malignant [10].
The most common location for mucoepidermoid carcinoma was minor glands (56%), followed by parotid, submandibular and sublingual (34%, 7% and 3% respectively) glands which is in agreement with the findings of Jones et al.,2008 but in disagreement with other reports which have found parotid to be the most common site [11, 13, 23]. This could be due to the fact that a number of these cases were reported in specialist oral and maxillofacial pathology units (some of which usually only report intra-oral specimens) although many of the included centres also have expertise in head and neck (H&N) pathology.
Understanding the epidemiological landscape and distribution of histological subtypes of salivary gland tumours is crucial for a better diagnosis of this diverse and complex group of tumours. It would be useful for future studies to include more geographical locations as well as other H&N and ENT centres. It would also be useful to establish international datasets of these tumours for use by other researchers (whole slide image or research repositories) including histological reassessment and classification according to the most recent WHO criteria.
Conclusions
Salivary gland tumours are rare, but show a gradual increasing incidence over the last decade and a half. We report the largest multicentre investigation of SGT to date showing that the majority are benign (65%), with a slight predilection for females (54%). Approximately 69% of SGT occur in patients between the fourth to seventh decade of life with a significant difference between the average age for benign and malignant tumours. Pleomorphic adenoma was the most common benign and mucoepidermoid carcinoma the most common malignant tumour. The majority of SGT presented in the major glands (68%), with the parotid gland being the most common location (70%) for benign and minor glands (47%) for malignant tumours. More extensive studies of SGT need to be conducted to understand and update the epidemiological landscape of these tumours and correlate it with prognosis.
Author Contributions
Study design (IA, SAK), Data collection and analysis (all authors), Manuscript preparation (IA, SAK), Manuscript review (all authors).
Funding
This work forms a part of the first author’s PhD, which is funded by King Saud University, Riyadh, Saudi-Arabia.
Data Availability
Anonymised data and materials available upon request and through the publication.
Code Availability
Not applicable.
Declarations
Conflict of interest
No conflict of interests to disclose.
Ethical Approval
In place. Reference- 20/WS/0017.
Research Involving in Humans and/or Animals Rights
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Speight PM, Barrett AW. Salivary gland tumours. Oral Dis. 2002;8(5):229–240. doi: 10.1034/j.1601-0825.2002.02870.x. [DOI] [PubMed] [Google Scholar]
- 2.Mahomed Y, Meer S. Primary epithelial minor salivary gland tumors in South Africa: a 20-year review. Head Neck Pathol. 2020;14(3):715–723. doi: 10.1007/s12105-019-01111-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guzzo M, Locati LD, Prott FJ, Gatta G, McGurk M, Licitra L. Major and minor salivary gland tumors. Crit Rev Oncol Hematol. 2010;74(2):134–148. doi: 10.1016/j.critrevonc.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 4.Jones AV, Craig GT, Speight PM, Franklin CD. The range and demographics of salivary gland tumours diagnosed in a UK population. Oral Oncol. 2008;44(4):407–417. doi: 10.1016/j.oraloncology.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 5.Sardar MA, Ganvir SM, Hazarey VK. A demographic study of salivary gland tumors. SRM J Res Dent Sci. 2018;9(2):67. doi: 10.4103/srmjrds.srmjrds_57_17. [DOI] [Google Scholar]
- 6.Dos Santos ES, Rodrigues-Fernandes CI, Speight PM, Khurram SA, Alsanie I, Normando AGC, Prado-Ribeiro AC, Brandão TB, Kowalski LP, Guerra ENS, Lopes MA. Impact of tumor site on the prognosis of salivary gland neoplasms: a systematic review and meta-analysis. Crit Rev Oncol Hematol. 2021;162:103352. doi: 10.1016/j.critrevonc.2021.103352. [DOI] [PubMed] [Google Scholar]
- 7.Waldron CA, El-Mofty SK, Gnepp DR. Tumors of the intraoral minor salivary glands: a demographic and histologic study of 426 cases. Oral Surg Oral Med Oral Pathol. 1988;66(3):323–333. doi: 10.1016/0030-4220(88)90240-X. [DOI] [PubMed] [Google Scholar]
- 8.Fiorella R, Di Nicola V, Fiorella ML, Spinelli DA, Coppola F, Luperto P, Madami L. Major salivary gland diseases. Multicentre study. Acta Otorhinolaryngol Italica. 2005;25(3):182. [PMC free article] [PubMed] [Google Scholar]
- 9.Boukheris H, Curtis RE, Land CE, Dores GM. Incidence of carcinoma of the major salivary glands according to the WHO classification, 1992 to 2006: a population-based study in the United States. Cancer Epidemiol Prev Biomark. 2009;18(11):2899–2906. doi: 10.1158/1055-9965.EPI-09-0638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tian Z, Li L, Wang L, Hu Y, Li J. Salivary gland neoplasms in oral and maxillofacial regions: a 23-year retrospective study of 6982 cases in an eastern Chinese population. Int J Oral Maxillofac Surg. 2010;39(3):235–242. doi: 10.1016/j.ijom.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 11.Bradley PJ, McGurk M. Incidence of salivary gland neoplasms in a defined UK population. Br J Oral Maxillofac Surg. 2013;51(5):399–403. doi: 10.1016/j.bjoms.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 12.Girdler R, Odell E, Putnam G. Epidemiology and management of major salivary gland cancers. London: Public Health England; 2016. [Google Scholar]
- 13.Kızıl Y, Aydil U, Ekinci Ö, Dilci A, Köybaşıoğlu A, Düzlü M, İnal E. Salivary gland tumors in Turkey: demographic features and histopathological distribution of 510 patients. Indian J Otolaryngol Head Neck Surg. 2013;65(1):112–120. doi: 10.1007/s12070-012-0594-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sentani K, Ogawa I, Ozasa K, Sadakane A, Utada M, Tsuya T, Kajihara H, Yonehara S, Takeshima Y, Yasui W. Characteristics of 5015 salivary gland neoplasms registered in the Hiroshima tumor tissue registry over a period of 39 years. J Clin Med. 2019;8(5):566. doi: 10.3390/jcm8050566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hay AJ, Migliacci J, Karassawa Zanoni D, McGill M, Patel S, Ganly I. Minor salivary gland tumors of the head and neck—memorial Sloan Kettering experience: incidence and outcomes by site and histological type. Cancer. 2019;125(19):3354–3366. doi: 10.1002/cncr.32208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alramadhan SA, Fitzpatrick SG, Cohen DM, Bhattacharyya I, Islam MN. Retrospective study of buccal mucosal salivary neoplasms. Head Neck Pathol. 2020;14:1013–1020. doi: 10.1007/s12105-020-01190-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.El-Naggar AK, Chan JKC, Rubin Grandis J, Takata T, Slootweg PJ. International Agency for Research on Cancer WHO classification of head and neck tumours. Lyon: International Agency for Research on Cancer; 2017. [Google Scholar]
- 18.Bello IO, Salo T, Dayan D, Tervahauta E, Almangoush A, Schnaiderman-Shapiro A, Barshack I, Leivo I, Vered M. Epithelial salivary gland tumors in two distant geographical locations, Finland (Helsinki and Oulu) and Israel (Tel Aviv): a 10-year retrospective comparative study of 2,218 cases. Head Neck Pathol. 2012;6(2):224–231. doi: 10.1007/s12105-011-0316-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ellis GL. Tumors of the salivary glands. Washington, DC: Armed Forces Institute of Pathology. Atlas of Tumor Pathology; 1996. [Google Scholar]
- 20.Eveson JW, Cawson RA. Salivary gland tumours. A review of 2410 cases with particular reference to histological types, site, age and sex distribution. J Pathol. 1985;146(1):51–58. doi: 10.1002/path.1711460106. [DOI] [PubMed] [Google Scholar]
- 21.Spiro RH. Salivary neoplasms: overview of a 35-year experience with 2,807 patients. Head Neck Surg. 1986;8(3):177–184. doi: 10.1002/hed.2890080309. [DOI] [PubMed] [Google Scholar]
- 22.Fonseca FP, Carvalho MV, de Almeida OP, Rangel AL, Takizawa MC, Bueno AG, Vargas PA. Clinicopathologic analysis of 493 cases of salivary gland tumors in a Southern Brazilian population. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114(2):230–239. doi: 10.1016/j.oooo.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 23.Ito FA, Ito K, Vargas PA, De Almeida OP, Lopes MA. Salivary gland tumors in a Brazilian population: a retrospective study of 496 cases. Int J Oral Maxillofac Surg. 2005;34(5):533–536. doi: 10.1016/j.ijom.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 24.Satko I, Stanko P, Longauerová I. Salivary gland tumours treated in the stomatological clinics in Bratislava. J Cranio-Maxillofac Surg. 2000;28(1):56–61. doi: 10.1054/jcms.1999.0092. [DOI] [PubMed] [Google Scholar]
- 25.Neville BW, Damm DD, Allen CM, Chi AC. Oral and maxillofacial pathology. Amsterdam: Elsevier Health Sciences; 2015. [Google Scholar]
- 26.Fantasia JE, Neville BW. Basal cell adenomas of the minor salivary glands: a clinicopathologic study of seventeen new cases and a review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 1980;50(5):433–440. doi: 10.1016/S0030-4220(80)80012-0. [DOI] [PubMed] [Google Scholar]
- 27.Al Sheddi MA. Salivary glands tumors: a single institution experience in Saudi Arabia. Biosci, Biotechnol Res Asia. 2016;9(1):193–198. doi: 10.13005/bbra/981. [DOI] [Google Scholar]
- 28.Khurram SA, Barrett AW, Speight PM. Diagnostic difficulties in lesions of the minor salivary glands. Diagn Histopathol. 2017;23(6):250–259. doi: 10.1016/j.mpdhp.2017.04.008. [DOI] [Google Scholar]
- 29.Rooper LM, Mansour M, Yonescu R, Oliai BR, Bishop JA, Westra WH. The decline of salivary adenocarcinoma not otherwise specified as a tumor entity: reclassification using contemporary immunohistochemical profiling and diagnostic criteria. Am J Surg Pathol. 2021;45(6):753–764. doi: 10.1097/PAS.0000000000001636. [DOI] [PubMed] [Google Scholar]
- 30.Mariz BALA, do Socorro Queiroz Feio P, Roza ALOC, de Andrade BAB, Agostini M, Romañach MJ, Fonseca FP, Pontes HAR, Ribeiro ACP, Brandão TB, Rocha AC. Clinical predictors of malignancy in palatal salivary gland tumors. Oral Dis. 2019;25(8):1919–1924. doi: 10.1111/odi.13181. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymised data and materials available upon request and through the publication.
Not applicable.