Abstract
Background
The shortage of nursing care in US hospitals has become a national concern.
Purpose
The purpose of this manuscript was to determine whether hospital nursing care shortages are primarily due to the pandemic and thus likely to subside or due to hospital nurse understaffing and poor working conditions that predated it.
Methods
This study used a repeated cross-sectional design before and during the pandemic of 151,335 registered nurses in New York and Illinois, and a subset of 40,674 staff nurses employed in 357 hospitals.
Findings
No evidence was found that large numbers of nurses left health care or hospital practice in the first 18 months of the pandemic. Nurses working in hospitals with better nurse staffing and more favorable work environments prior to the pandemic reported significantly better outcomes during the pandemic.
Discussion
Policies that prevent chronic hospital nurse understaffing have the greatest potential to stabilize the hospital nurse workforce at levels supporting good care and clinician wellbeing.
Keywords: Burnout, Nurse understaffing, Patient safety, Pandemic
Introduction
The Surgeon General (2022) recently issued a public advisory declaring health care clinician burnout to be an urgent public health issue in need of immediate action. The American Hospital Association (AHA) in a March 1, 2022, letter to Congress proclaimed workforce challenges a national emergency that demanded immediate attention (AHA, 2022). There is little doubt that many hospitals failed to perform well during the Covid-19 emergency (Fleisher et al., 2022; Joint Commission, 2021). Bloodstream infections, which had declined 31% in the 5 years preceding the pandemic increased 28% in the pandemic's first months (Patel et al., 2021) with similar disappointing trends in other infections, falls, and pressure ulcers (AHRQ, 2021; Rosenthal et al., 2022). The AHA's proposed solutions to the nursing care shortage included increasing the national supply of nurses, recruiting nurses from abroad, addressing clinicians’ “behavioral health needs,” and investigating anticompetitive behavior of travel nurse agencies. Are these the highest priority solutions to the problems of hospitals not being able to recruit and retain enough nurses? Our study of hospital nurses in a large, repeated cross-sectional study before and during the pandemic adds a new perspective on where to look for solutions to the shortage of hospital nursing care.
The solutions may have been in plain sight for two decades. In 2002, two landmark studies (Aiken et al., 2002; Needleman et al., 2002) documented significant associations between hospital patient-to-nurse workloads and patient mortality and nurse burnout. Each one patient increase in nurses’ workloads was associated with a 7% increase in the odds of risk-adjusted patient mortality, a 23% increase in the odds of high nurse burnout, and a 15% increase in the odds of nurse job dissatisfaction (Aiken et al., 2002). A large body of research (Aiken et al., 2018; Lake et al., 2019; Lasater et al., 2021c; Lu et al., 2012; Sloane et al., 2018; Wynendaele et al., 2019) confirms the association of hospital nurse staffing and work environments with patient outcomes and nurse retention.
The only major policy response to chronic hospital nurse understaffing and poor work environments in 20 years has been the implementation in 2004 of a mandated minimum nurse staffing requirement in hospitals throughout California (Aiken et al., 2010; McHugh et al., 2011a, 2012). The unfunded mandate resulted in patients in California hospitals currently receiving, on average, 2 to 3 more hours a day of registered nurse care than patients in other states (Dierkes et al., 2021). Similar safe nurse staffing legislation has been considered in other states but despite research estimating improved patient outcomes and cost savings (Lasater et al., 2021a, 2021b), no other states have implemented minimum hospital nurse staffing requirements.
This study leverages data from the largest repeated survey of registered nurses aggregated by their employing organizations both immediately preceding the pandemic and 18 months into the pandemic. Data document baseline measures and pandemic-related changes in nurse burnout, job dissatisfaction, intent to leave, patient safety and quality of care, nurse staffing, work environments, and confidence in hospital management. Our findings reveal that nurses’ concerns and adverse outcomes which were magnified by the pandemic were evident before the pandemic. We explore how nurse understaffing and poor work environments before the pandemic were associated with nurse wellbeing and intent to stay with their employer during the pandemic, a perspective that is essential in identifying and prioritizing policy actions and managerial changes in hospital workplaces to retain nurses and keep patients safe.
Methods
Data
This study uses repeated cross-sectional data from two surveys of all registered nurses in New York and Illinois collected prepandemic (December 16, 2019–February 24, 2020) and during the pandemic (April 13, 2021–June 22, 2021). All actively licensed registered nurses in New York and Illinois were invited to participate in an online survey. The resulting dataset includes repeated measures in two cross-sections of data from 151,335 nurses (81,263 prepandemic; 70,072 during). Respondents indicated their employment status, including whether they were currently employed in health care in a hospital setting, employed in health care but not in a hospital, employed but not in health care, not currently employed, or retired. These data were used to evaluate changes in employment status to understand the extent to which nursing care shortages during the pandemic were likely due to nurses leaving the profession or hospital practice. This question can only be answered using a sample of all nurses including those that left hospitals as well as those who stayed. Nurses employed in hospitals reported their position (e.g., staff nurse, nurse manager, advanced practice nurse), and type of unit on which they most recently worked (e.g., medical–surgical, intensive care, emergency department). A subset of 40,674 staff nurses that practiced in hospitals at the time of the survey (24,114 prepandemic; 16,560 during) was used to evaluate changes in hospital nurse job outcomes, work environments, and quality and safety of care.
In contrast to other studies of nurses during the pandemic that mostly relied on convenience sampling, ours used a sampling frame more likely to yield a representative sample of nurses—state licensure lists of registered nurses. Also, unlike other surveys, we were able to aggregate hospital nurses by their employer. The subset of 40,674 hospital staff nurses in our analytic dataset is employed by 357 unique hospitals, representing 99% of acute care hospitals in New York and Illinois. The overall response rate of all nurses was 18% in the prepandemic survey and 14% for the survey during the pandemic, which is within the usual range of response rates for online surveys. In prior survey research using a similar survey instrument, we utilized a double-sampling approach of nonrespondents for evaluating nonresponse bias and found no significant differences in nurse-reported measures between main-survey respondents and nonrespondents (Lasater et al., 2019).
Measures
Burnout was assessed using the emotional exhaustion subscale of the Maslach Burnout Inventory (Maslach & Jackson, 1981; Maslach et al., 2001). High burnout was defined as scores 27 (Maslach et al., 1997). Job dissatisfaction was a dichotomous variable of “somewhat dissatisfied” and “very dissatisfied” to a single-item question asking nurses how satisfied they were overall with their job (McHugh et al., 2011b). Intent to leave was measured using nurses’ reports of whether they planned to be with their current employer for 1 year. Nurses assessed whether there was enough staff to provide needed care, whether their overall hospital work environment was excellent, good, fair, or poor, and whether there was good teamwork between nurses and physicians (Sloane et al., 2018).
Nurses rated quality of patient care and the effectiveness of management in their hospitals. Patient care measures included: overall quality of care, patient safety, infection prevention, and culture of patient safety. Ratings of the quality of nursing care ranged from “excellent” to “poor” on a four-point Likert scale. Patient safety and infection prevention were rated on a scale (A–F) with grades of C, D, or F considered “unfavorable.” Culture of patient safety items were drawn from the Agency for Healthcare Research and Quality (AHRQ) Hospital Survey on Patient Safety Culture (AHRQ, 2019) asking nurses to rate on a five-point Likert scale ranging from “strongly agree” to “strongly disagree” whether actions of management show patient safety is a top priority, whether nurses feel mistakes are held against them, and whether nurses feel free to question authority. Nurses indicated whether they were confident (i.e., ranging from “very confident” to “not at all confident” on a four-point Likert scale) that management would act to resolve problems in patient care that nurses identify. Nurses indicated whether they agreed with the statement “administration listens and responds to nurses’ concerns” (ranging from “strongly agree” to “strongly disagree” on a four-point Likert scale).
Data Analysis
First, we show changes in nurse employment from the prepandemic period to during the pandemic. We then show percentages of hospital staff nurses reporting concerns about hospital management and patient care quality in the two periods, using chi-square statistics to test the significance of differences across periods. We show percentages of hospital staff nurses overall and in different types of units with high burnout, job dissatisfaction, intent to leave current employer, staffing insufficiency (i.e., not enough staff), work environments that were poor/fair, and not a lot of teamwork between nurses and physicians.
Finally, we aggregate responses from medical–surgical staff nurses prepandemic to create hospital-level measures of mean adult medical–surgical patient-to-nurse staffing ratios and nurse work environments in hospitals prior to the pandemic. This aggregation technique resulted in a subset of 239 hospitals, a smaller number of hospitals than used in the analysis of burnout because some respondents did not provide the name of their employer which was necessary to calculate staffing levels and work environment quality at the hospital level. The resulting hospitals consisted of the following distribution of mean staffing: 39 hospitals had a mean patient-to-nurse staffing ratio of 5 or fewer patients per nurse in the prepandemic cross-section, 112 hospitals had a mean of more than five and less than equal to six patients per nurse, and 88 hospitals had more than six patients per nurse on average. Hospital work environments were categorized by the percentage of medical–surgical staff nurses who rated their work environment as “poor” or “fair” in the prepandemic cross-section: 24 hospitals were categorized as “good” work environments, 128 hospitals had “mixed” work environments, and 87 hospitals had “poor” work environments. Once hospitals were categorized by their prepandemic staffing and work environments, we use percentages and chi-square statistics to show how nurse outcomes, care quality and safety, and concerns with management varied across hospitals during the pandemic based on their prepandemic patient-to-nurse staffing ratios and quality of their work environments.
Findings
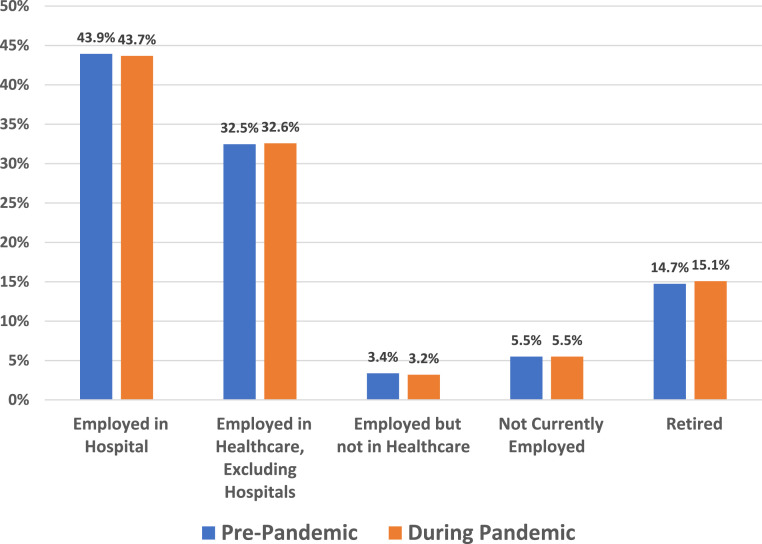
Figure 1 displays the distribution of actively licensed registered nurses by employment status prepandemic and during the pandemic using our entire sample of nurse respondents whether they were employed or not; for the employed nurses we considered employment in all settings. Between the two periods there were no significant changes in employment status (likelihood ratio chi-square statistic = 7.05 with 4 d.f., p = .133 testing the independence of the numbers in the five employment status categories across two time points). The percentage of nurses employed in hospitals did not change by more than a fraction of 1% during the pandemic (p = .322). Had large numbers of nurses left hospitals or health care without being replaced, we would expect to see decreases in percentages of nurses in hospitals and other health care settings and concomitant increases in numbers of nurses that were employed in nonhealth care settings or currently unemployed or retired.
Figure 1.
Changes in nurse employment status, prepandemic and during the pandemic.
Notes. Survey data collected by the Center for Health Outcomes and Policy Research at the University of Pennsylvania School of Nursing. Prepandemic data were collected between December 15, 2019 and February 24, 2020. Data during the pandemic were collected between April 13, 2021 and June 22, 2021. A chi-square statistic (L2 = 7.05 with 4 d.f., p = .133) testing the independence of the numbers in the five employment status categories across two time points is insignificant, indicating no overall change.
Table 1 reports survey results from hospital staff nurses only. The findings point to lack of confidence in hospital management prepandemic which worsened during the pandemic. Over 69% of hospital staff nurses in the prepandemic period reported a lack of confidence in hospital management to resolve clinical care problems reported by nurses, and this percentage increased to almost 78% during the pandemic. Similarly, 47% of hospital staff nurses in the prepandemic period reported that administration did not listen or respond to nurses’ concerns which increased to 53% during the pandemic. Some 48% of nurses prepandemic agreed that the “actions of management show patient safety is not a top priority” which rose to 53% during the pandemic. Almost 50% of nurses prepandemic reported feeling that their mistakes were held against them and 56% reported not feeling free to question decisions or actions of authority. Almost 45% of nurses gave their hospitals unfavorable patient safety grades prepandemic and 47% rated patient safety unfavorably during the pandemic. A third of nurses gave their hospitals an unfavorable grade on infection prevention prepandemic which rose to 36% during the pandemic. Nurses’ assessments about quality grew more negative during the pandemic, with higher percentages of nurses rating their hospitals’ overall quality of care as poor/fair during the pandemic (26%) as compared to before (20%).
Table 1.
Hospital Staff Nurses Evaluations of Hospital Management and Patient Care Quality, Prepandemic and During the Pandemic
| Patient Care and Evaluation of Management | Prepandemic | During Pandemic | Change† |
|---|---|---|---|
| Not confident in management resolving clinical care problems | 69.4% | 77.5% | 8.1%*** |
| Administration doesn't listen or respond to nurses’ concerns | 46.8% | 52.9% | 6.1%*** |
| Actions of management show patient safety is not a top priority | 47.7% | 53.3% | 5.8%*** |
| Feel mistakes are held against them | 49.6% | 47.1% | -2.5%*** |
| Do not feel free to question decisions or actions of authority | 56.2% | 52.1% | -4.1%*** |
| Poor/fair quality of care | 19.9% | 25.7% | 5.8%*** |
| Unfavorable infection prevention grade (C, D, or F) | 33.2% | 35.6% | 2.4%*** |
| Unfavorable patient safety grade (C, D, or F) | 44.5% | 47.1% | 2.6%*** |
Notes. Survey data collected by the Center for Health Outcomes and Policy Research at the University of Pennsylvania School of Nursing.
p < .001
Prepandemic data were collected between December 15, 2019 and February 24, 2020. Data during the pandemic were collected between April 13, 2021 and June 22, 2021.
As shown in Table 2 , large percentages of hospital staff nurses before Covid-19 reported high burnout (48%), job dissatisfaction (27%), intent to leave their employer (22%), poor/fair work environments (47%), and not enough staff (57%). These outcomes worsened or remained high during the pandemic—especially among nurses working on medical–surgical units, adult intensive care, and in emergency departments. The largest increases during the pandemic were in the percentage of hospital staff nurses reporting there were not enough staff and the percentage of nurses reporting job dissatisfaction and high burnout. The negative impact of the pandemic was not observed in nurse–physician teamwork which was positive before the pandemic and improved during the pandemic.
Table 2.
Hospital Staff Nurse Reports of High Burnout, Job Dissatisfaction, Intent to Leave, Staffing, and Work Environments, Prepandemic and During the Pandemic
| Nurse Reports⁎ | Prepandemic | During Pandemic | Change† | |
|---|---|---|---|---|
| All staff nurses | High burnout | 48.0% | 51.0% | 3.0%*** |
| (N = 40,674) | Job dissatisfaction | 27.2% | 30.6% | 3.4%*** |
| Intent to leave employer | 21.8% | 24.7% | 2.9%*** | |
| Not enough staff | 56.9% | 67.4% | 10.5%*** | |
| Poor/fair work environment | 46.6% | 42.2% | -4.4%*** | |
| Not a lot of nurse–physician teamwork | 18.9% | 15.1% | -3.8*** | |
| Medical–surgical nurses | High burnout | 54.0% | 58.9% | 4.8%*** |
| Job dissatisfaction | 29.9% | 36.3% | 6.4%*** | |
| (N = 10,743) | Intent to leave employer | 23.5% | 28.0% | 4.5%*** |
| Not enough staff | 64.9% | 75.0% | 10.1%*** | |
| Poor/fair work environment | 46.4% | 46.4% | 0.0% | |
| Not a lot of nurse–physician teamwork | 21.4% | 15.8% | -5.6%*** | |
| Adult intensive care nurses | High burnout | 50.3% | 57.6% | 7.3%*** |
| Job dissatisfaction | 29.7% | 33.9% | 4.2%** | |
| (N = 5,429) | Intent to leave employer | 25.5% | 29.2% | 3.7%** |
| Not enough staff | 57.4% | 73.1% | 15.7%*** | |
| Poor/fair work environment | 49.0% | 46.5% | -2.5% | |
| Not a lot of nurse–physician teamwork | 17.6% | 15.2% | -2.4%* | |
| Emergency department nurses (N = 4,515) | High burnout | 55.9% | 58.1% | 2.2% |
| Job dissatisfaction | 31.4% | 37.4% | 6.0%*** | |
| Intent to leave employer | 24.7% | 28.3% | 3.6%* | |
| Not enough staff | 63.6% | 75.3% | 11.7%*** | |
| Poor/fair work environment | 51.8% | 51.9% | 0.1% | |
| Not a lot of nurse–physician teamwork | 13.9% | 12.3% | -1.6% | |
| Other nurses | High burnout | 41.7% | 43.9% | 2.2%** |
| (N = 19,987) | Job dissatisfaction | 23.8% | 25.6% | 1.8%** |
| Intent to leave employer | 19.0% | 21.1% | 2.1%*** | |
| Not enough staff | 50.3% | 60.4% | 10.1%*** | |
| Poor/fair work environment | 44.7% | 37.0% | -7.7%*** | |
| Not a lot of nurse–physician teamwork | 19.0% | 15.3% | -3.7%*** |
Notes. Survey data collected by the Center for Health Outcomes and Policy Research at the University of Pennsylvania School of Nursing.
p < .05; **p < .01; *** p < .001
Prepandemic data were collected between December 15, 2019 and February 24, 2020. Data during the pandemic were collected between April 13, 2021 and June 22, 2021.
In Table 3 we show how the outcomes and concerns expressed by hospital staff nurses during the pandemic are associated with mean medical–surgical patient-to-nurse staffing ratios prepandemic. Percentages of nurses reporting each outcome during the pandemic are grouped according to reports of their hospital's mean medical–surgical staffing in the prepandemic cross-section. Nurses in hospitals in which the mean number of patients assigned to each nurse was high prepandemic were more likely to issue unfavorable reports about their own outcomes (e.g., burnout, job dissatisfaction, intent to leave employer), patient outcomes (e.g., poor quality of care, unfavorable patient safety), and lack confidence in hospital management during the pandemic.
Table 3.
Hospital Staff Nurse Reports of Job Outcomes, Patient Care Quality, and Hospital Management Support During the Pandemic are Associated with Patient-to-Nurse Staffing Ratios Prepandemic
| Percent of Nurses Reporting Various Outcomes During Pandemic | Hospital Mean Medical–Surgical Patients Per Nurse Prepandemic⁎ |
||
|---|---|---|---|
|
5 N = 39 |
>5 and 6 N = 112 |
>6 N = 88 |
|
| High burnout | 48.7% | 52.0% | 53.4% |
| Dissatisfied with job | 25.1% | 32.1% | 35.0% |
| Intent to leave employer | 21.5% | 24.3% | 26.7% |
| Not confident in management resolving clinical care problems | 72.0% | 77.5% | 82.1% |
| Actions of management show patient safety is not a top priority | 45.1% | 55.0% | 58.5% |
| Administration doesn't listen or respond to nurses’ concerns | 44.0% | 53.9% | 58.2% |
| Unfavorable patient safety grade (C, D, or F) | 33.9% | 46.7% | 54.6% |
| Unfavorable infection prevention grade (C, D, or F) | 27.0% | 33.8% | 41.8% |
| Poor/fair quality of care | 15.7% | 24.7% | 33.0% |
| Not a lot of teamwork between nurses and physicians | 12.6% | 13.7% | 18.0% |
Notes. Survey data collected by Center for Health Outcomes and Policy Research at the University of Pennsylvania School of Nursing.
Chi-square tests reveal that the differences in each of the reported outcomes between the three categories (defined by the hospital mean medical–surgical patients per nurse prepandemic) are significant at the p < .01 level of confidence.
Similar differences are shown in Table 4 , in which nurses in hospitals with “poor” work environments in the prepandemic period reported the greatest concerns with their own wellbeing, patient outcomes, and lack of confidence in hospital management during the pandemic.
Table 4.
Hospital Staff Nurse Reports of Job Outcomes, Patient Care Quality, and Hospital Management Support During the Pandemic Are Associated With Nurse Work Environments Prepandemic
| Percent of Nurses Reporting Various Outcomes During Pandemic | Hospital Nurse Work Environment Prepandemic⁎ |
||
|---|---|---|---|
| Good N = 24 |
Mixed N = 128 |
Poor N = 87 |
|
| High burnout | 42.1% | 51.3% | 55.7% |
| Dissatisfied with job | 19.9% | 29.9% | 37.8% |
| Intent to leave employer | 19.7% | 23.8% | 26.9% |
| Not confident in management resolving clinical care problems | 63.1% | 76.4% | 84.7% |
| Actions of management show patient safety is not a top priority | 35.5% | 51.6% | 64.3% |
| Administration doesn't listen or respond to nurses’ concerns | 36.3% | 49.8% | 63.9% |
| Unfavorable patient safety grade (C, D, or F) | 24.6% | 42.1% | 60.6% |
| Unfavorable infection prevention grade (C, D, or F) | 17.3% | 29.9% | 48.4% |
| Poor/fair quality of care | 9.4% | 21.9% | 36.0% |
| Not a lot of teamwork between nurses and physicians | 9.8% | 12.9% | 19.3% |
Notes. Survey data collected by Center for Health Outcomes and Policy Research at the University of Pennsylvania School of Nursing.
Chi-square tests reveal that the differences in each of the reported outcomes between the three categories (defined by the percentage of nurses who rated their hospital work environment as “poor” or “fair” prepandemic) are significant at the p < .001 level of confidence.
Discussion
Overall, our findings suggest that the pandemic was not the root cause but a contributing factor in hospital nurse recruitment and retention challenges during the pandemic. Our survey responses from all nurses, whether working or not before and during the pandemic, do not support the widely held belief that nurses left health care or hospital practice in large numbers during the pandemic. The evidence of declining confidence in hospital management along with high burnout, job dissatisfaction, and intent to leave before and during the pandemic suggests that nurses may have been changing employers in higher numbers, including working for supplemental staffing agencies, which contributed to a perception of more nurses leaving clinical care than can be documented.
Our findings confirmed among hospital nurses that high nurse burnout, job dissatisfaction, intent to leave hospital employer, and lack of confidence in hospital management predated the pandemic. Immediately prior to Covid-19, 48% of hospital nurses in our study experienced high burnout; more than a year into the pandemic, the percentage of high burnout went up only 3% to 51%. The high rates of nurse burnout during the pandemic appear to be largely a consequence of high burnout prior to the pandemic. Addressing the root causes of high nurse burnout and hospital job dissatisfaction before the pandemic is critical to achieving a stable, qualified hospital nurse workforce going forward.
Importantly, our results show that hospital nurse understaffing and poor work environments prior to the Covid-19 emergency were associated with unfavorable outcomes during the pandemic. Before Covid-19, 57% of hospital staff nurses said there were too few nurses to care for patients which increased to 67% during the pandemic. Almost half of nurses (47%) rated their hospital work environments as “poor” or “fair” prepandemic; during the pandemic 42% rated their work environments unfavorably. High nurse burnout, job dissatisfaction, and intent to leave were worse during the pandemic in hospitals that were poorly staffed before the pandemic and/or had unfavorable work environments before the pandemic. The proportion of hospital staff nurses during the pandemic intending to leave their employer was significantly higher in hospitals with the worst nurse staffing and poorest work environments in the prepandemic period suggesting that both chronic understaffing and subpar work environments dually threaten nurse retention.
Also, nurses’ negative appraisals of quality of care and patient safety during the pandemic were substantially worse in hospitals in which nurses cared for more patients each before the pandemic. For example, 33% of nurses in hospitals where mean prepandemic medical–surgical staffing was more than six patients per nurse reported poor/fair quality of care during the pandemic, compared with half that many, only 16% of nurses, in hospitals where the mean prepandemic staffing was 5 or fewer patients per nurse.
Before the pandemic, an astounding 70% of hospital staff nurses lacked confidence in management in their employing organization to resolve clinical care problems identified by nurses, and close to half of nurses reported their employer did not listen or respond to their concerns. Nurses’ negative appraisals of hospital management increased further during the pandemic when nurse layoffs and furloughs were common. Almost half of nurses reported prepandemic that the actions of hospital management show patient safety is not a top priority which increased to 53% during the pandemic. Also, both before and during the pandemic nearly half of nurses reported they feel like mistakes are held against them and they do not feel free to question decisions and actions of authority-disturbing evidence of the failure of hospital management to embrace the basic tenets of keeping patients safe. The recent case (Kalman & Norman, 2022) of a hospital nurse being fired by her hospital and convicted of criminally negligent homicide for a medication error reportedly associated with a system failure adds further distress to a burned out and discouraged nurse workforce and is a real-world example of why nurses lack confidence in management and lack loyalty to their employing hospitals.
One finding to be celebrated is that nurses reported that nurse–physician relations were good prior to the pandemic and even improved some during the pandemic. Interprofessional relationships and interdisciplinary teamwork among clinicians seem strong, in contrast to the substantial lack of confidence nurses have in hospital management.
Study Strengths and Limitations
While the timing of our surveys is unique in having a baseline immediately before the Covid-19 pandemic and a second survey during the pandemic, we have measures at only two points in time, so caution is warranted in making causal inferences. Our survey is unique among others available in that nurses were invited to participate from a sampling frame consisting of all licensed registered nurses in two large states as compared to convenience samples. Also, nurses are linked to their place of employment providing a unique perspective on nursing practice within individual hospitals. Survey response rates are not optimal although not out of line with recent experience with large online surveys. Our previous research shows that nonresponders do not rate nursing care differently from those that do respond, and that nonresponse is not a factor that influences the kind of outcomes we are studying (Lasater et al., 2019). Nurses who did not report their hospital name were somewhat more likely to report more negatively about their hospitals’ quality; however, in most cases the differences were not statistically significant. Some may consider nurse reports of patient care quality as subjective but our previously published research shows that nurse reports of quality and safety of care are highly predictive of objectively measured patient outcomes including mortality, failure to rescue, and patient satisfaction (McHugh & Stimpfel, 2012). Finally, the pandemic has continued for a year after our “during the pandemic” survey so it is possible that conditions have changed further over time.
Implications for Policy
The most common suggestion for addressing the present shortage of nursing care in hospitals is to increase the national supply of nurses, although evidence does not suggest this strategy will be effective. The numbers of US educated nurses graduating annually has been steadily increasing for decades even during the pandemic and currently over 185,000 new nurses enter the workforce each year (National Council of State Boards of Nursing, 2021). In 2017, the National Center for Health Workforce Analysis (U.S. Department of Health and Human Services, 2017) projected a national registered nurse excess of about 8% by 2030. There is little association between increases in the national supply of nurses and hospital patient-to-nurse ratios. Immediately before the pandemic, after a decade that added a million registered nurses to the national supply, mean patient-to-nurse staffing ratios varied widely across hospitals in New York and Illinois from a low of 4.3 patients per nurse in adult medical and surgical inpatient units to a high of 10.5 patients per nurse (Lasater et al., 2021c). This lack of an association between supply and hospital nursing care shortage is also shown at the state-level where RNs per 1,000 population vary substantially. California, the only state with mandated nurse staffing ratios, has among the fewest nurses with 9.25 RNs per 1,000 population while Massachusetts, a state with 16.04 RNs per 1,000, turned down legislation setting minimum hospital nurse staffing standards because of fears of nurse shortages.
The shortage of nursing care in hospitals is largely the result of chronic nurse understaffing by design. Focusing policy attention primarily on substantial and rapid increases in the supply of nurses diverts attention from more promising solutions to the chronic shortage of nursing care in hospitals as well as in other settings such as nursing homes and schools where the number of budgeted positions for nurses is the problem that needs a solution. Also, policies to rapidly increase RN supply could undermine national nurse workforce goals by attracting new poor-quality nursing schools with unfavorable graduation rates and a proliferation of programs that do not produce nurses with bachelor's degrees as recommended by the National Academy of Medicine (Institute of Medicine, 2011).
Fifteen states currently address hospital nurse staffing in law (de Cordova et al., 2019a, 2019b). However, only in California where minimum nurse staffing is mandated is there an association between state legislation and improved nurse staffing (Han et al., 2021). California implemented minimum required hospital nurse staffing almost 20 years ago with positive results (Aiken et al., 2010; Dierkes et al., 2021). Significant improvements in nurse staffing were achieved in California safety-net hospitals, one of the few observed improvements in nurse staffing in minority serving hospitals since the passage of Medicare and Medicaid (McHugh et al., 2012). Hospitals that staffed better than the minimum required before the law did not decrease their staffing to the minimum, thus demonstrating that safe nurse staffing standards do not require “one size to fit all,” a slogan used liberally by opponents of safe nurse staffing standards. And other negative unintended consequences such as hospital or emergency department closures due to staffing legislation were not observed (McHugh et al., 2011a). Recent research in other states has shown that pending staffing legislation is in the public's interest because of the substantial variation in patient-to-nurse ratios across hospitals within states which is associated with higher deaths as well as higher costs due to longer stays and more readmissions (Lasater et al., 2021a, 2021b).
There is no evidence that mandated nurse staffing committees, the most prevalent form of state nurse staffing legislation, have any impact on improved staffing (Han et al., 2021). While state legislation to require public reporting of hospital nurse staffing has not shown much impact (de Cordova et al., 2019b; Han et al., 2021) the Medicare Hospital Compare website is more visible and accessible to the public than state reports of staffing but currently does not report on hospital nurse staffing. Remedying this important omission could make hospital nurse staffing more transparent to the public and motivate improvements.
A concern by opponents of legislating minimum hospital staffing requirements is the risk of creating a short-term nurse shortage at state or local levels that could disrupt health services. The Nurse Licensure Compact, which has been passed in 39 US states and territories, addresses that risk by allowing nurses to practice in any Compact state. The Compact offers the advantage of comprehensive vetting of nurses’ qualifications and avoiding delays in issuing state-based licenses (Alexander et al., 2021). Nurse employers should advocate for its passage given the substantial delays in processing RN licenses that have worsened during Covid, and slow onboarding of newly hired nurses (Fast, 2022).
A recent Harris poll showed 90% of the public surveyed favored requiring safe nurse staffing standards in hospitals and nursing homes (NursesEverywhere, 2020). Given the strong headwinds from deep pocket special interests opposed to states establishing hospital minimum nurse staffing requirements, federal options should be pursued. The most promising federal option is to establish minimum safe nurse staffing standards for hospitals as a condition of participation in Medicare (Aiken & Fagin, 2022). There is precedent in Medicare nurse staffing requirements for nursing homes, even though the current staffing standard there is too low to produce safe care. Medicare conditions of participation have previously been used to solve vexing problems including the desegregation of hospitals and the implementation of the employee Covid-19 vaccine mandate in hospitals that was upheld by the Supreme Court. Similar policy intervention is warranted to require hospitals participating in Medicare to meet evidence-based nurse staffing standards to ensure safe care for the public and to reduce outcomes disparities in understaffed minority serving hospitals.
Further explication of Medicare's value-based purchasing policies to create a visible funding stream for professional nurses, as is common for other health professionals, is promising as a potentially cost neutral strategy to explicitly reward hospitals and other providers for employing enough nurses to provide safe care of high quality. Evidence-based nurse staffing has been shown to reduce length of stay, readmissions, and never events such as health care-acquired infections that save lives and avoid pain and suffering as well as saving Medicare money (Lasater et al., 2021a; Yakusheva et al., 2020).
Implications for Practice
Interventions for improving subpar work environments are not codified in policy, but rather in administrative decision-making about how to structure and operate complex organizations. One example of an evidence-based organizational intervention that has been shown to improve nurse work environments is the American Nurses Credentialing Center Magnet Recognition Program (Kutney-Lee et al., 2015). The Magnet program offers an actionable blueprint for how organizations can transform culture to enhance clinician wellbeing and patient care outcomes. Organizations committed to improving their work environments and attracting and retaining registered nurses may find success in following the organizational principles, such as structural empowerment and engagement of clinicians in decision-making, characteristic of Magnet hospitals.
Conclusion
Chronic nurse understaffing and poor work environments in hospitals that existed prior to the Covid-19 pandemic and worsened during it are the major explanations for why many hospitals cannot hire and keep enough nurses even though Covid-19 hospitalizations have dropped. Without fundamental improvements in hospital nurse staffing and work environments, the shortage of nursing care in hospitals will not likely abate even after the Covid-19 pandemic has run its course. Increasing the supply of nurses through short-term emergency measures is unlikely to solve the problem. Hospitals need to hire more permanent registered nurses, provide more favorable work environments, and earn back the confidence of nurses that quality and safety of patient care are institutional priorities. Because most hospitals have not implemented substantial improvements in either staffing or work environments over the past decade (Aiken et al., 2018; Sloane et al., 2018), policymakers should mandate hospitals to meet minimum safe nurse staffing standards. A continuation of chronic nurse understaffing and unacceptable working conditions in hospitals will not restore the public's or nurses’ confidence in hospitals.
Authors’ Contributions
L.H.A.: Conceptualization, funding, data collection, writing, interpretation of results, policy implications; D.M.S.: Study design, analysis, interpretation of findings, writing; M.D.M.: Conceptualization, funding, data collection, interpretation of results, policy implications; C.A.P.: Conceptualization, interpretation of findings, writing, manuscript review; K.B.L.: Conceptualization, funding, data collection, analysis, writing, policy implications.
Acknowledgments
This research was supported by the National Council on State Boards of Nursing, the National Institute of Nursing Research, National Institutes of Health (R01NR014855 and T32NR00714), and Agency for Healthcare Research and Quality (R01HS028978 Lasater). The authors thank Timothy Cheney for analytic assistance and the tens of thousands of nurses who responded to our survey during challenging times.
References
- Agency for Healthcare Research and Quality (AHRQ) 2022. Hospital survey on patient safety culture.https://www.ahrq.gov/sops/surveys/hospital/index.html Retrieved August 2, 2022, from. [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality (AHRQ) AHRQ; 2021. NPSD data spotlight, patient safety and COVID-19: A qualitative analysis of concerns during the public health emergency. [Google Scholar]
- Aiken L.H., Clarke S.P., Sloane D.M., Sochalski J., Silber J. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. Journal of the American Medical Association. 2002;288(16):1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Aiken, L. H., & Fagin, C. M. (2022). Medicare can help fix the nurse shortage in hospitals. STAT. https://www.statnews.com/2022/02/08/medicare-can-help-fix-the-nurse-shortage-in-hospitals/.
- Aiken L.H., Sloane D.M., Barnes H., Cimiotti J.P., Jarrin O., McHugh M.D. Nurses’ and patients’ appraisals show patient safety in hospitals remains a concern. Health Affairs. 2018;37(11):1744–1751. doi: 10.1377/hlthaff.2018.0711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken L.H., Sloane D.M., Cimiotti J., Clarke S., Flynn L., Spetz J., Seago J.A., Smith H.L. Implications of the California nurse staffing mandate for other states. Health Services Research. 2010;45(4):904–921. doi: 10.1111/j.1475-6773.2010.01114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander M., Martin B., Kaminski-Ozturk N., Zhong E., Smiley R. Envisioning the future of nursing regulation through research: A global agenda. Journal of Nursing Regulation. 2021;12(3):5–10. [Google Scholar]
- American Hospital Association (AHA) (2022). Challenges facing America's health care workforce as the U.S. enters third year of COVID-19 pandemic. https://www.aha.org/news/news/2022-03-02-aha-urges-congress-address-health-care-workforce-challenges.
- de Cordova P.B., Pogorzelska-Mazianz M., Eckenhoff M.E., McHugh M.D. Public reporting of nurse staffing in the United States. Journal of Nursing Regulation. 2019;10(3):14–20. doi: 10.1016/S2155-8256(19)30143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Cordova P.B., Rogowski J., Riman K.A. Effects of public reporting legislation of nurse staffing: A trend analysis. Policy, Politics, & Nursing Practice. 2019;20(2):92–104. doi: 10.1177/1527154419832112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dierkes A., Do D., Morin H., Rochman M., Sloane D.M., McHugh M.D. The impact of California's staffing mandate and the economic recession on registered nurse staffing levels: A longitudinal analysis. Nursing Outlook. 2021;70(2):219–227. doi: 10.1016/j.outlook.2021.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fast, A. (2022). Nurses are waiting months for licenses as hospital staffing shortages spread. National Public Radio, Morning Edition. https://www.npr.org/2022/03/10/1084897499/nurses-are-waiting-months-for-licenses-as-hospital-staffing-shortages-spread.
- Fleisher L.A., Schreiber M., Cardo D., Srinivasan A. Health care safety during the pandemic and beyond: Building a system that ensures resilience. New England Journal of Medicine. 2022;386(7):609–611. doi: 10.1056/NEJMp2118285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han X., Pittman P., Barnow B. Alternative approaches to ensuring adequate nurse staffing: The effect of state legislation on hospital nurse staffing. Medical Care. 2021;59(10 Suppl 5):S463. doi: 10.1097/MLR.0000000000001614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine . National Academies Press; Washington, DC: 2011. The future of nursing: Leading change, advancing health. [PubMed] [Google Scholar]
- Joint Commission . 2021. New and revised emergency management standards.https://www.jointcommission.org/-/media/tjc/documents/standards/prepublications/hap_july2022_prepublication_report_em_chapter_revisions.pdf [Google Scholar]
- Kalman, B., & Norman, H. (2022). Why nurses are raging and quitting after the RaDonda Vaught verdict. Shots: Health News from NPR. npr.org/sections/heath-shots/2022/04/05/1090915329/why-nurses-are-raging-and-quitting-after-the-radonda-vaught-verdict.
- Kutney-Lee A., Stimpfel A.W., Sloane D.M., Cimiotti J.P., Quinn L.W., Aiken L.H. Changes in patient and nurse outcomes associated with Magnet hospital recognition. Medical Care. 2015;53(6):550. doi: 10.1097/MLR.0000000000000355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake E.T., Sanders J., Duan R., Riman K.A., Schoenauer K.M., Chen Y. A meta-analysis of the associations between the nurse work environment in hospitals and 4 sets of outcomes. Medical Care. 2019;57(5):353–361. doi: 10.1097/MLR.0000000000001109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasater K.B., Aiken L.H., Sloane D.M., French R., Martin B., Reneau K., Alexander M., McHugh M.D. Patient outcomes and cost savings associated with hospital safe nurse staffing legislation: An observational study. BMJ Open. 2021;11(12) doi: 10.1136/bmjopen-2021-052899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasater K.B., Aiken L.H., Sloane D.M., French R., Martin B., Reneau K., Alexander M., McHugh M.D. Chronic hospital nurse understaffing meets COVID-19: An observational study. BMJ Quality & Safety. 2021;30(8):639–647. doi: 10.1136/bmjqs-2020-011512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasater K.B., Aiken L.H., Sloane D.M., McHugh M.D., Smith H.L. Is hospital nurse staffing legislation in the public's interest?: An observational study in New York State. Medical Care. 2021;59(5):444. doi: 10.1097/MLR.0000000000001519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lasater K.B., Jarrin O., Aiken L.H., Sloane D.M., McHugh M.D., Smith H.L. A methodology for studying organizational performance: A multistate survey of front-line providers. Medical Care. 2019;57(9):742–749. doi: 10.1097/MLR.0000000000001167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu H., Barriball L., Zhang X., While A.E. Job satisfaction among hospital nurses revisited: A systematic review. International Journal of Nursing Studies. 2012;49(8):1017–1038. doi: 10.1016/j.ijnurstu.2011.11.009. [DOI] [PubMed] [Google Scholar]
- Maslach C., Jackson S.E. The measurement of experienced burnout. Journal of Organizational Behavior. 1981;2(2):99–113. [Google Scholar]
- Maslach C., Jackson S.E., Leiter M.P. Scarecrow Education; 1997. Maslach burnout inventory. [Google Scholar]
- Maslach C., Schaufeli W.B., Leiter M.P. Job burnout. Annual Review of Psychology. 2001;52(1):397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- McHugh M.D., Brooks Carthon M., Wu E., Kelly L., Sloane D.M., Aiken L.H. Impact of nurse staffing mandates on safety-net hospitals: Lessons from California. The Milbank Quarterly. 2012;90(1):160–186. doi: 10.1111/j.1468-0009.2011.00658.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh M.D., Kelly L., Sloane D.M., Aiken L.H. Contradicting fears, California's nurse-to-patient mandate did not reduce the skill level of the nursing workforce in hospitals. Health Affairs. 2011;30(7):1299–1306. doi: 10.1377/hlthaff.2010.1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh M.D., Kutney-Lee A., Cimiotti J., Sloane D.M., Aiken L.H. Nurses’ widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Affairs. 2011;30(2):202–210. doi: 10.1377/hlthaff.2010.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh M.D., Stimpfel A.W. Nurse reported quality of care: A measure of hospital quality. Research in Nursing & Health. 2012;35(6):566–575. doi: 10.1002/nur.21503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Council of State Boards of Nursing. (2021). 2021 NCLEX pass rates. https://www.ncsbn.org/15858.htm.
- Needleman J., Buerhaus P., Mattke S., Stewart M., Zelevinsky K. Nurse-staffing levels and the quality of care in hospitals. New England Journal of Medicine. 2002;346(22):1715–1722. doi: 10.1056/NEJMsa012247. [DOI] [PubMed] [Google Scholar]
- NursesEverywhere. (2021, August 3). Expand nursing care survey: A research brief. https://3aaa9248-e569-4da8-ada5-c4c9b14e503e.filesusr.com/ugd/d52815_ea23c1bba67c46eebe9692cf2b69a54b.pdf.
- Patel P.R., Weiner-Lastinger L.M., Dudeck M.A., Fike L.V. Impact of COVID-19 pandemic on central-line–associated bloodstream infections during the early months of 2020. National Healthcare Safety Network. Infection Control & Hospital Epidemiology. 2021;43(6):790–793. doi: 10.1017/ice.2021.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal V.D., Matra S.N., Divatia J.V., Biswas S., et al. The impact of COVID-19 on healthcare-associated infections in intensive care units in low- and middle-income countries: International Nosocomial Infection Control Consortium (INICC) findings. International Journal of Infectious Diseases. 2022;118:83–88. doi: 10.1016/j.ijid.2022.02.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloane D.M., Smith H.L., McHugh M.D., Aiken L.H. Effect of changes in hospital nursing resources on improvements in patient safety and quality of care: A panel study. Medical Care. 2018;56:1001–1008. doi: 10.1097/MLR.0000000000001002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surgeon General . Office of the Surgeon General; 2022. New surgeon general advisory sounds alarm on health worker burnout and resignation.https://www.hhs.gov/about/news/2022/05/23/new-surgeon-general-advisory-sounds-alarm-on-health-worker-burnout-and-resignation.html [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis . 2017. National and regional supply and demand projections of the nursing workforce: 2014-2030. Rockville, Maryland. [Google Scholar]
- Wynendaele H., Willems R., Trybou J. Systematic review: Association between the patient-nurse ratio and nurse outcomes in acute care. Journal of Nursing Management. 2019;27(5):896–917. doi: 10.1111/jonm.12764. [DOI] [PubMed] [Google Scholar]
- Yakusheva O., Rambur B., Buerhaus P. Value-informed practice can help reset the hospital-nurse relationship. JAMA Health Forum. 2020;1(8) doi: 10.1001/jamahealthforum.2020.0931. [DOI] [PubMed] [Google Scholar]