Abstract
Macrophages are a heterogeneous class of innate immune cells that offer a primary line of defense to the body by phagocytizing pathogens, digesting them, and presenting the antigens to T and B cells to initiate adaptive immunity. Through specialized pro-inflammatory or anti-inflammatory activities, macrophages also directly contribute to the clearance of infections and the repair of tissue injury. Macrophages are distributed throughout the body and largely carry out tissue-specific functions. In skeletal muscle, macrophages regulate tissue repair and regeneration; however, the characteristics of these macrophages are not yet fully understood, and their involvement in skeletal muscle aging remains to be elucidated. To investigate these functions, it is critical to efficiently isolate macrophages from skeletal muscle with sufficient purity and yield for various downstream analyses. However, methods to prepare enriched skeletal muscle macrophages are scarce. Here, we describe in detail an optimized method to isolate skeletal muscle macrophages from mice. This method has allowed the isolation of CD45 + /CD11b + macrophage-enriched cells from young and old mice, which can be further used for flow cytometric analysis, fluorescence-activated cell sorting (FACS), and single-cell RNA sequencing.
This protocol was validated in: eLife (2022), DOI: 10.7554/eLife.77974
Keywords: Macrophage , CD11b , Skeletal muscle , Aging , Senescence
Background
Macrophages were discovered by Metchnikoff and colleagues more than a century ago as professional phagocytes ( Underhill et al., 2016 ). Later studies revealed that macrophages constitute a heterogenous class of cells that exert diverse functions in tissues throughout the body ( Wynn et al., 2013 ). Macrophages can be divided into two major types: tissue-resident and non-tissue-resident macrophages ( Ginhoux and Guilliams, 2016 ). The former can be further divided into two distinct populations: embryo-derived self-renewing and bone marrow–derived non-self-renewing macrophages. Typical self-renewing macrophages derived from the embryonic yolk sac or fetal liver include microglia, Kupffer cells, alveolar macrophages, and Langerhans cells. Bone marrow–derived non-self-renewing resident macrophages, which must be replenished by circulating monocytes at tissue-specific levels, include tissue-resident macrophages in the intestine, pancreas, and dermis ( Chakarov et al., 2019 ). Non-tissue-resident macrophages are derived from bone marrow progenitor cells and infiltrate tissues following injury or infection ( Kratofil et al., 2017 ). Macrophages are highly versatile cells, capable of ingesting and digesting pathogens as well as necrotic and infected cells, activating T and B lymphocytes, and inducing or suppressing inflammation (Shapouri-Moghaddam et al., 2018). The functional diversity of macrophages is well represented by their dynamic polarization abilities. Depending on signals from the local environment, macrophages can be polarized toward functionally opposite roles: pro-inflammatory M1 or anti-inflammatory M2 subtypes ( Mills et al., 2000 ; Martinez et al., 2008 ). Cytokines produced by Th1 (T helper type 1) lymphocytes, including interferon γ (IFNγ or IFNG) and tumor necrosis factor (TNF), polarize macrophages to the M1 subtype, while cytokines produced by Th2 lymphocytes, such as interleukin (IL) 4 and IL13, promote macrophage M2 polarization ( Mills et al., 2000 ; Martinez et al., 2008 ). Polarized M1 macrophages induce inflammation, destroy pathogens, and clean up cell debris, partly through upregulation of the nitric oxide synthase (NOS) pathway ( Rath et al., 2014 ). By contrast, M2 macrophages suppress inflammation and promote tissue repair, partially through upregulation of the arginase pathway ( Rath et al., 2014 ). While M1 and M2 are well-known macrophage subtypes, more recent single-cell studies have identified additional subtypes in several mouse tissues ( Chakarov et al., 2019 ; Jaitin et al., 2019 ). These subtypes share similarities and differences with M1 and M2, which further reveal the heterogeneity and versatility of macrophages.
Macrophages adapt to individual tissues and largely act in a tissue-dependent manner. Macrophages from different tissues possess distinct gene expression profiles and transcriptional regulatory pathways ( Gautier et al., 2012 ). Recent studies suggest that local environmental factors in each tissue contribute to the tissue specificity of resident macrophages ( Gosselin et al., 2014 ; Lavin et al., 2014 ). For instance, tumor growth factor β (TGFβ or TGFB) promotes the development of microglia by affecting the enhancer/promoter landscape of brain macrophages, while retinoic acid determines peritoneal macrophage specificity ( Hoeksema and Glass, 2019 ). These studies have further uncovered the capacity of macrophages to adapt to local environments and acquire tissue-specific identities.
Skeletal muscle contains numerous diverse resident macrophages, localized in the perimysium and endomysium ( Cui et al., 2019 ), where they resolve infections and repair injury (Arnold et al., 2007; Tidball, 2011 and 2017 ). For example, when skeletal muscle is damaged, monocytes from the bloodstream differentiate and polarize into pro-inflammatory M1 macrophages, which eliminate pathogens and clean up tissue debris. Subsequently, M1 macrophages convert to M2 macrophages to suppress inflammation and repair tissues along with resident M2 macrophages ( Yang and Hu, 2018 ; Cui and Ferrucci, 2020 ). Recently, skeletal muscle macrophages have been associated with physiological adaptations to exercise that differ between young and elderly individuals ( Walton et al., 2019 ; Jensen et al., 2020 ), although the full spectrum of macrophage subtypes in skeletal muscle and their functions are only partially known. We have recently found that macrophages residing in human and mouse skeletal muscle are mostly of the M2 subtype ( Cui et al., 2019 ); however, recent single-cell analyses from skeletal muscle and other tissues suggest that the identities of skeletal muscle macrophages are likely more complex ( Chakarov et al., 2019 ; Jaitin et al., 2019 ; Wang et al., 2020 ). Furthermore, skeletal muscle macrophages have been shown to have mixed origins, including the embryonic yolk sac, fetal liver, and adult bone marrow ( Wang et al., 2020 ). It remains unclear whether macrophages from various origins behave differently, and the function of each macrophage subtype in skeletal muscle physiology and aging is yet to be elucidated.
To answer these questions, it is critical to isolate macrophages from skeletal muscle. There are a few methods for macrophage enrichment from skeletal muscle. One protocol for stem cell isolation from mouse skeletal muscle ( Liu et al., 2015 ) was also effective for macrophage isolation from skeletal muscle ( Kosmac et al., 2018 ). In this study, we sought to formulate a simpler protocol that was effective for the isolation of a macrophage-enriched cell fraction from young and old mouse skeletal muscle. We tested a commercial skeletal muscle dissociation kit combined with a programmable tissue dissociator and added a debris removal step. This kit-based approach allowed us to reduce cell isolation steps and obtain cleaner and more consistent cell preparations. The new protocol was effective for the enrichment of macrophages from skeletal muscle and enabled the characterization of resident macrophages by flow cytometry and single-cell transcriptomic analyses.
Materials and Reagents
100 mm Falcon TM bacteriological Petri dishes with lid (Fisher Scientific, catalog number: 08-757-100D)
GentleMACS C-tubes (Miltenyi Biotec, catalog number: 130-093-237 or 130-096-334)
5 mL Falcon TM polypropylene round-bottomed tubes (Corning, catalog number: 352063)
15 mL Falcon TM tubes
50 mL Falcon TM tubes
1.5 mL Eppendorf TM tubes
Polystyrene containers; “sticky” for cells but could be used after BSA coating
PluriStrainer, 50 µm (pluriSelect, catalog number: 43-50050-01)
10 mL syringe, Luer-Lok tip (BD, catalog number: 309604)
20G × 1.5" blunt tip dispensing fill needles (CML Supply, catalog number: 901-20-150)
Countess TM cell counting chamber slides (Invitrogen, catalog number: C10228)
Skeletal muscles from the hind limbs of 3-month-old and 18-month-old C57BL/6J mice (see below)
70% ethanol
DMEM (ThermoFisher, catalog number: 11965-092). Store at 4 °C. Shelf life is 12 months from date of manufacture
Fetal bovine serum, heat inactivated (ThermoFisher, catalog number: 10438-026). Store at -20 °C. Shelf life is two years from date of manufacture
Penicillin and streptomycin solution (10,000 U/mL) (100×) (Thermo Fisher Scientific, catalog number: 15140122). Store at -20 °C. Shelf life is 12 months from date of manufacture
PBS, pH 7.2 (ThermoFisher, catalog number: 20012-027), free of Ca 2+ and Mg 2+ . Store at 4 °C
RNAseZAP TM zaps (Ambion, catalog number: 9786-9788)
Skeletal Muscle Dissociation kit (Miltenyi Biotec, catalog number: 130-098-305). Make aliquots for enzymes P, D, and A, and store them at -20 °C immediately after arrival. Shelf life is six months after aliquot
Debris removal solution (Miltenyi Biotec, catalog number: 130-109-398). Protect from light and store at 4 °C. Expiration date is labeled on the vial
Red blood cell lysis solution (Miltenyi Biotec, catalog number: 130-094-183). Protect from light and store at 4 °C. Expiration date is labeled on the vial
Auto MACS TM rinsing solution (Miltenyi Biotec, catalog number: 130-091-222). Protect from light and store at room temperature. Expiration date is labeled on the bottle
MACS TM BSA stock solution (Miltenyi Biotec, catalog number: 130-091-376). Protect from light and store at 4 °C. Expiration date is labeled on the bottle. After opening, the solution should be used within three days
0.5 M EDTA (ThermoFisher, catalog number: 15575020). Store at room temperature
Trypan Blue solution (Invitrogen, catalog number: T10282). Store at room temperature
-
Antibodies: All antibodies and isotype controls from Biolegend should be stored undiluted at 4 °C and protected from light. Do not freeze. Shelf life is approximately two years
PE anti-mouse/human CD11b antibody (Biolegend, catalog number: 101208, Clone M1/70)
PE Rat IgG2b, κ Isotype Ctrl antibody (Biolegend, catalog number: 400607, Clone RTK4530)
APC anti-mouse CD45 antibody (Biolegend, catalog number: 103111, Clone 30-F11)
APC Rat IgG2b, κ Isotype Ctrl antibody (Biolegend, catalog number: 400611, RTK4530)
FITC anti-mouse CD206 (MMR) antibody (Biolegend, catalog number: 141703, Clone C068C2)
FITC Rat IgG2a, κ Isotype Ctrl antibody (Biolegend, catalog number: 400505, Clone RTK2758)
TruStain FcX TM (anti-mouse CD16/32) antibody (Fc blocker) (Biolegend, catalog number: 101319). Store undiluted at 4 °C and protected from light
Fixable Viability Dye eFluor TM 780 (Invitrogen, catalog number: 65-0865-14). Store at -80 °C and protect from light and moisture. Expiration date is labeled on the vial
DMEM-I and DMEM-II medium (see Recipes)
Digestive enzymes (see Recipes)
PEB buffer for cell isolation and flow cytometry (see Recipes)
Reagent combination to label macrophages for flow cytometry (see Recipes)
Equipment
Dissection tools: forceps, scalpels, and scissors
Pipettes
-80 °C freezer, -20 °C freezer, 4 °C refrigerator
GentleMACS TM Octo Dissociator with heaters (Miltenyi Biotec, catalog number: 130-096-427)
Countess TM II FL automated cell counter (Invitrogen, catalog number: AMQAF1000)
BD FACSCanto TM II Cell Analyzer (BD, catalog number: REF338960)
Centrifuge 5702R (Eppendorf, catalog number: 022626205)
Centrifuge 5415R (Eppendorf, catalog number: 22-62-140-8)
Procedure
Note: The following protocol was designed for isolating mononuclear cells from skeletal muscle from two adult C57BL/6J mice.
-
Muscle preparation
Decontaminate the tools for muscle dissection, including forceps, scalpels, and scissors, with RNaseZAP TM wipes and rinse thoroughly with double-distilled water (ddH 2 O). Decontaminate the procedure area by spraying with 70% ethanol.
Prepare three 100 mm Petri dishes, each containing 10 mL DMEM-I (see Recipes). Place on ice for washing and trimming of isolated muscles. To collect dissected muscles from two mice, prepare two 50 mL Falcon tubes, each containing 5 mL of DMEM-I, and place on ice.
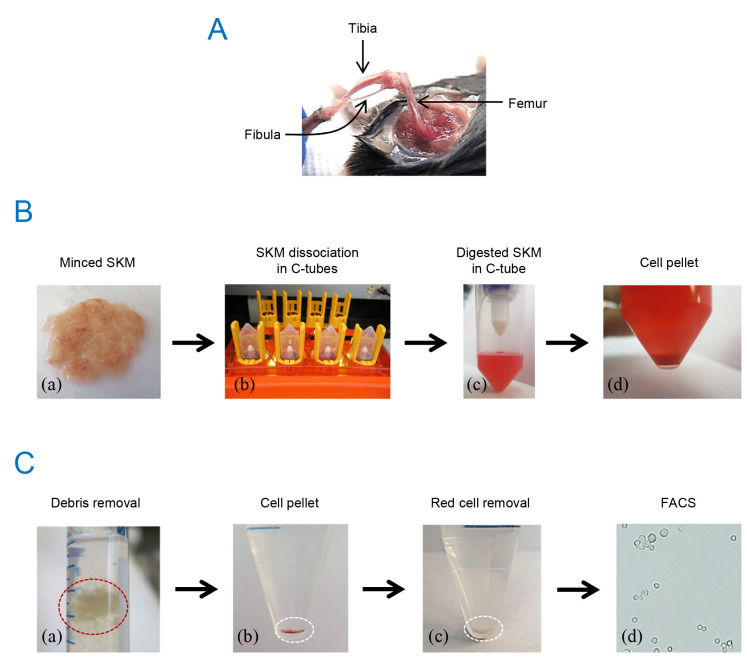
Sacrifice a mouse by cervical dislocation or CO 2 asphyxiation and spray 70% ethanol over the entire mouse. Incise the skin at the ankle and peel off the skin from the hind limb. Dissect out all muscles surrounding the femur, tibia, and fibula ( Figure 1A ), and place into the 100 mm dishes containing DMEM-I. Cut out the fat, blood vessels, and tendons under a dissection microscope. Collect the trimmed muscles in the 50 mL Falcon tube containing DMEM-I; weigh the tube before and after sampling and record the muscle weight. Two hind limbs from an adult mouse provide approximately 1 g of muscle. Collect the muscles from the second mouse following the same procedure.
Cut and slice the harvested muscles with scissors on ice, leaving 1–2 mL of DMEM-I on the Petri dish and removing the rest. Holding one end of a piece of muscle with forceps, use the scissors to cut the muscle into small pieces (approximately 1 mm 3 fragments). After cutting, gather all the muscle pieces in the center of the dish and mince with scissors for an additional 2–3 min [ Figure 1B (a)].
-
Mononuclear cell isolation
Transfer the minced muscle tissues from one mouse into two C-tubes containing the enzyme mix (5 mL each) and close the tubes tightly.
Mount the C-tubes onto the GentleMAC Octo Dissociator with heaters [ Figure 1B (b)]. Choose the 37C-mr-SMDK-2 program. Start the digestion, which takes approximately 1.5 h.
After digestion, briefly centrifuge the C-tubes [ Figure 1B (c)]. At this step, combine the two C-tubes containing muscle suspensions that were dissected from the same mouse (5 + 5 = 10 mL) into one tube. Use a 10 or 15 mL syringe and a 20G blunt needle (pre-washed with 70% ethanol and distilled water or with DMEM-I) to slowly aspirate and eject the muscle suspension 10 times. Eject the suspension toward the wall of the tube to avoid foaming. This step further breaks down the tissue debris and increases cell yield.
Add 10 mL of DMEM-II to each suspension to dilute and deactivate the enzymes. Pipette the suspension onto a cell strainer (50 µm mesh size) and collect the flowthrough into a 50 mL Falcon tube. Wash each strainer with 10 mL of DMEM-II twice. Use a 200 µL pipette to collect any remaining liquid from the underside of the strainer. Each tube will contain 40 mL cell suspension.
Discard the strainer and centrifuge the cell suspension at 600 × g for 15 min at room temperature. A clear pellet will be visible at the bottom of the tube [ Figure 1B (d)]. Discard the supernatant completely. Dissolve the pellet in 1 mL DMEM-II and transfer to a 1.5 mL Eppendorf tube.
Centrifuge at 500 × g and 4 °C for 10 min in a bench-top centrifuge. Discard the supernatant and resuspend the pellet in 0.5 mL cold PBS. Place on ice.
-
Debris removal
Note: This step efficiently removes fiber debris from the digested skeletal muscles and significantly improves the purity of mononuclear cells ( Figure 1C ).
Carefully transfer the cell suspension to a 15 mL Falcon tube containing 5.7 mL of cold (4 °C) PBS (0.5 mL of cell suspension + 5.7 mL of PBS = 6.2 mL).
Add 1.8 mL of cold debris removal solution; mix well by slowly pipetting up and down 10 times using a 10 mL pipette.
Slightly tilt the tube and very slowly and gently overlay the cell suspension with 4 mL of cold PBS. Ensure that the PBS and the cell suspension phases do not mix.
Centrifuge at 3,000 × g and 4 °C for 10 min. Discard the supernatant completely; this contains tissue debris [ Figure 1C (a)]. The cell pellet at the bottom contains the mononuclear cells [ Figure 1C (b)].
Add cold PBS to a final volume of 15 mL. Gently invert the tube three times. Do not vortex.
Centrifuge at 1,000 × g and 4 °C for 10 min. Discard the supernatant completely.
Resuspend cells in 0.5 mL of PEB (see Recipes) by pipetting gently and slowly. Place on ice.
-
Red blood cell lysis
Make 10 mL of 1× red blood cell lysis solution by diluting 10× lysis solution with double-distilled water (ddH 2 O). Do not use deionized water (including deionized DEPC water). Store at room temperature.
Mix one volume of cell suspension with 10 volumes of 1× red blood cell lysis solution (e.g., 0.5 mL of cell suspension + 5 mL of 1× lysis solution) in a 15 mL tube. Vortex for 5 s and incubate for 2 min at room temperature. Longer incubation may damage the cells.
Centrifuge at 500 × g for 10 min at room temperature [ Figure 1C (c)]. Discard the supernatant completely and resuspend the pellet in 0.5 mL of PEB. Place cells on ice.
Mix 5 µL cells with 5 µL of Trypan Blue and count the number of cells using the Countess TM machine. Approximately two million live mononuclear cells can be obtained from a mouse using the above procedure.
-
Flow cytometry analysis of isolated mononuclear cells
For analytical studies, evenly divide approximately two million cells into nine 1.5 mL Eppendorf tubes (50 μL in each), including a tube with unstained live cells, a tube with heat-induced dead cells, and tubes with isotype controls, single antibody controls, or combined antibodies. Add viability dye eFluor 780, Fc blocker, isotype control, or antibodies to each tube as explained below.
Figure 1. Outline of macrophage isolation from mouse skeletal muscle.
(A) Hind limb after muscle harvest. (B) Minced muscle from mouse hind limbs (a), cell dissociator (b), digested muscle in a C-tube (c), and cell pellet after centrifugation (d). (C) Debris removed by the debris removal solution (a), cell pellet after debris removal (b), cell pellet after red cell removal (c), and cells after sorting (d, 20× brightfield image).
Procedures for staining
Immunofluorescence staining for surface marker proteins enables us to identify specific immune cell populations. To confirm the enrichment of macrophages, we stained using three antibodies that recognized leukocytes (CD45), myeloid lineage cells including macrophages (CD11b), and M2 macrophages (CD206). See Table 1 for reagent combination.
Table 1. Reagent combination for staining .
| Tubes | Viability Dye (eFluor 780) | Fc blocker | Isotype control | Antibody |
|---|---|---|---|---|
| 1 | ||||
| 2 | 1 µL | |||
| 3 | 1 µL | 1 µL | 1 µL (IgG-PE) | |
| 4 | 1 µL | 1 µL (CD11b-PE) | ||
| 5 | 1 µL | 1 µL | 1 µL (IgG-APC) | |
| 6 | 1 µL | 1 µL (CD45-APC) | ||
| 7 | 1 µL | 1 µL | 1 µL (IgG-FITC) | |
| 8 | 1 µL | 1 µL (CD206-FITC) | ||
| 9 | 1 µL | 1 µL |
1 µL (CD11b-PE) 1 µL (CD45-APC) 1 µL (CD206-FITC) |
Add 50 µL of PEB to tube 1 (unstained) and place on ice.
Incubate tube 2 at 65 °C for 10 min to generate the dead cell control. Subsequently, add 950 µL of PEB to bring the volume to 1 mL. Place on ice.
Add 950 µL of PEB to the remaining tubes to bring the volume to 1 mL. Add 1 µL of viability dye (eFluor 780) to tubes 2, 3, 5, 7, and 9 (tubes 3, 5, and 7 are IgG isotype controls). Mix immediately by inverting the tubes 5–10 times. Incubate for 10 min at 4 °C.
Centrifuge tubes 3, 5, 7, and 9 at 500 × g for 5 min, discard the supernatants, and resuspend in 1 mL of PEB. Centrifuge tube 2 at 12,000 × g and 4 °C for 5 min, discard the supernatant, and resuspend the pellet in 100 µL of PEB. Place tube 2 on ice.
Add 1 µL of Fc blocker to tubes 3–9 and gently vortex for 1 s; repeat three times. Incubate for 5 min at room temperature (~25 °C).
Centrifuge tubes 3–9 at 500 × g and 4 °C for 5 min. Discard supernatants and resuspend the pellet in 100 µL of PEB.
Add 1 µL of IgG-PE, 1 µL of IgG-APC, or 1 µL of IgG-FITC to tubes 3, 5, and 7, respectively.
Add 1 µL of CD11b-PE antibody, 1 µL of CD45-APC antibody, or 1 µL of CD206-FITC antibody to tubes 4, 6, and 8, respectively (tubes 4, 6, and 8 are for compensation). Add 1 µL of CD11b-PE, 1 µL of CD45-APC, and 1 µL of CD206-FITC to tube 9. Gently vortex for 1 s and repeat three times. Incubate for 40 min at 4 °C.
Centrifuge tubes 3–9 at 500 × g and 4 °C for 5 min, discard the supernatant and resuspend the pellet in 500 µL of PEB. Gently vortex for 1 s and repeat three times.
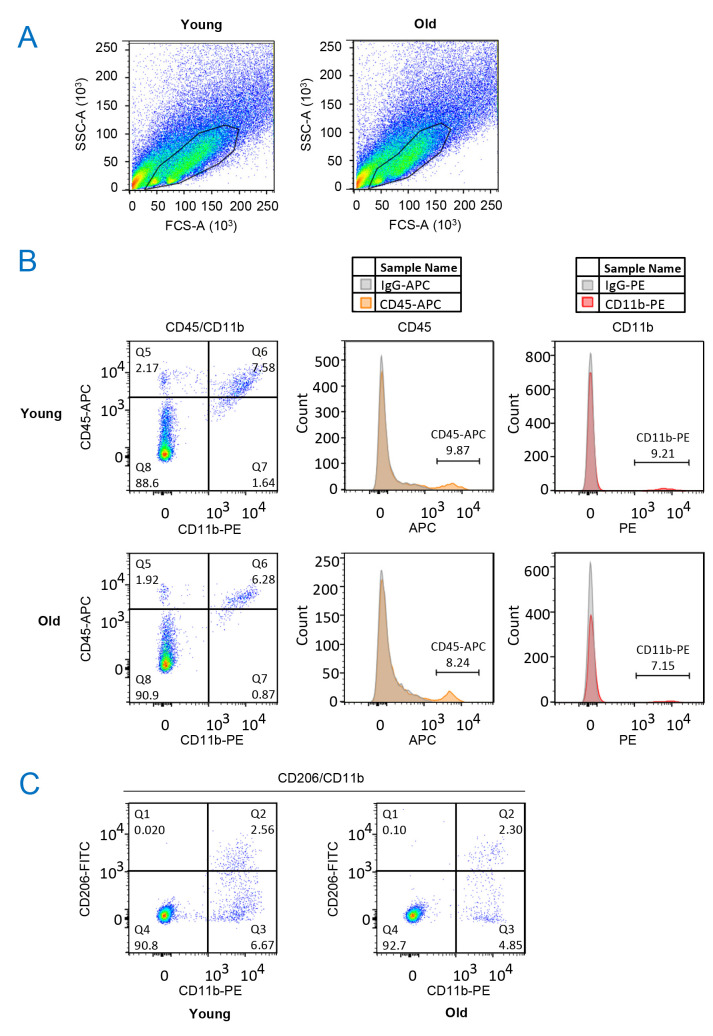
Spin down tubes 3–9 at 500 × g and 4 °C for 5 min, aspirate the supernatant and resuspend the cells in 100 µL of PEB. Cells are ready for flow cytometry analysis. Figure 2 shows the results of flow cytometry analysis of isolated mononuclear cells.
Figure 2. Flow cytometry analysis of isolated mononuclear cells.
(A) Isolated mononuclear cells from young and old skeletal muscle were gated in a Forward/Side scatter plot. (B) Gated cells (from A) were further analyzed for CD45 and CD11b expression. CD45 + /CD11b + cells were separated from the main cell population (left, gate Q6). The double-positive cells accounted for 7.58% of the total cells in the young preparations and 6.28% in the old preparations (left). CD45 + cells accounted for 9.87% of the total cells in the young preparations and 8.24% in the old preparations (center). CD11b + cells accounted for 9.21% of the total cells in the young preparations and 7.15% in the old preparations (right). CD11b + cells were clearly separated from the main population and almost all CD11b + cells were CD45 + . (C) Putative M2 macrophage marker CD206 was highly expressed (gate Q2) in 27.7% of CD11b + cells (gates Q2+Q3) in the young preparations (left) and in 32.1% of CD11b + cells in the old preparations (right). BD FACSCanto TM II cell analyzer and FlowJo 10 software were used for analysis.
Notes
Here, we tested a commercial skeletal muscle dissociation kit combined with a programmable tissue dissociator and added a debris removal step. This protocol allowed the isolation of high-purity skeletal muscle macrophages. We generally obtain approximately two million live mononuclear cells from two hind limbs of a mouse, among which ~5–9% of cells are CD11b + /CD45 + . This number is sufficient for FACS and single-cell transcriptomics analyses.
Several steps in our protocol were included to improve the purity and yield of macrophages. Firstly, the combination of tissue weight and enzyme mix affects cell yield. In our experience, 0.5 g muscle per 5 mL enzyme mix provided superior muscle digestion and cell yield as compared with 1 g muscle per 5 mL enzyme mix. Hence, we use two C-tubes, each containing approximately 0.5 g muscle and 5 mL enzyme mix, for one mouse. Secondly, we compared two digestion programs—37C-mr-SMDK-1 (1 h) and 37C-mr-SMDK-2 (1.5 h)—in a GentleMAC octo dissociator with heaters. The 1.5-h program provided a more thorough digestion and better cell yield. Thirdly, the debris removal solution effectively removed most of fiber debris, which allowed for much cleaner cell preparations. We highly recommend the debris removal steps.
Perfusing mice with saline solution through the inferior vena cava before sacrifice can be performed to reduce the presence of circulating immune cells in the skeletal muscle preparation.
Splenocytes, which can be easily harvested from the same mouse, are another option for generating dead cells.
Staining for additional markers, e.g., F4/80 and MHCII, will help to confirm macrophage specificity.
Recipes
-
Medium
-
DMEM-I
DMEM containing 1× penicillin and streptomycin solution. Store at 4 °C. Use within one month of preparation.
-
DMEM-II
DMEM-I supplemented with 5% heat-inactivated fetal bovine serum. Store at 4 °C. Use within one month of preparation.
-
-
Digestive enzymes
A skeletal muscle dissociation kit (see Reagents) was used for mononuclear cell isolation. Upon arrival of the kit, reconstitute and aliquot enzymes D, P, and A, and store at -20 °C.
Prepare an enzyme mix for cell dissociation. Remove the enzymes from the -20 °C freezer and place at room temperature (~25 °C) for 5–10 min. An enzyme master mix will be prepared first. This master mix must be freshly prepared each time.
-
Each GentleMACS C-tube will include 4.7 mL of DMEM supplemented with:
1× antibiotics
200 μL of enzyme D
50 μL of enzyme P
36 μL of enzyme A
Total 5 mL
-
Make 20 mL of enzyme master mix for four C-tubes to digest muscles from two mice, as follows:
20.21 mL of DMEM
860 μL of enzyme D
215 μL of enzyme P
154.8 μL of enzyme A (one tube × 4.3)
Total 21.65 mL
Resuspend the enzyme master mix.
Add 5 mL of enzyme mix to each of the four GentleMACS C-tubes and place on ice. Use two C-tubes to digest skeletal muscles from one mouse. Given that approximately 1 g of skeletal muscle can be obtained from two hind legs of a mouse, approximately 0.5 g muscle tissues will be digested in 5 mL of enzyme mix in each C-tube.
-
Buffers for flow cytometry analysis
PEB buffer:
1,450 mL of Auto MACS rinsing solution
150 mL of MACS BSA stock solution
24 mL of 0.5 M EDTA
The PEB buffer contains 1% BSA and 10 mM of EDTA
Store at 4 °C. Use within three months of preparation.
-
Reagent combination to label macrophages for flow cytometry
Evenly divide approximately two million cells into nine 1.5 mL Eppendorf tubes (50 μL in each). Tube 1 contains unstained live cells and tube 2 contains heat-induced dead cells. Tubes 3, 5, and 7 contain isotype controls, and tubes 4, 6, and 8 contain single antibody controls. Tube 9 contains the combined antibodies. Add eFluor 780, Fc blocker, isotype control, or antibodies to each tube as described in Table 1 . See Procedures for staining (Section F) for more details.
Acknowledgments
This work was supported by the Intramural Research Program of the National Institute on Aging. The authors thank Dr. Ramaiah Nagaraja for helpful technical assistance. This protocol derives from the main paper (Krasniewski et al, 2022).
Competing interests
The authors declare no competing interests.
Ethics
Animal use was approved by the Animal Care and Use Committee of the National Institute on Aging, NIH. Approved ID is 476-LGG-2024, which is effective until 2024.
Citation
Readers should cite both the Bio-protocol article and the original research article where this protocol was used.
Q&A
Post your question about this protocol in Q&A and get help from the authors of the protocol and some of its users.
References
- 1. Arnold L. , Henry A. , Poron F. , Baba-Amer Y. , van Rooijen N. , Plonquet A. , Gherardi R. K. and Chazaud B. ( 2007 . ). Inflammatory monocytes recruited after skeletal muscle injury switch into antiinflammatory macrophages to support myogenesis . J Exp Med 204 ( 5 ): 1057 - 1069 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Chakarov S. , Lim H. Y. , Tan L. , Lim S. Y. , See P. , Lum J. , Zhang X. M. , Foo S. , Nakamizo S. , Duan K. , et al. .( 2019 . ). Two distinct interstitial macrophage populations coexist across tissues in specific subtissular niches . Science 363 ( 6432 ): eaau0964 . [DOI] [PubMed] [Google Scholar]
- 3. Cui C. Y. , Driscoll R. K. , Piao Y. , Chia C. W. , Gorospe M. and Ferrucci L. ( 2019 . ). Skewed macrophage polarization in aging skeletal muscle . Aging Cell 18 ( 6 ): e13032 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cui C. Y. and Ferrucci L. ( 2020 . ). Macrophages in skeletal muscle aging . Aging(Albany NY) . 12 ( 1 ): 3 - 4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gautier E. L. , Shay T. , Miller J. , Greter M. , Jakubzick C. , Ivanov S. , Helft J. , Chow A. , Elpek K. G. , Gordonov S. , et al. .( 2012 . ). Gene-expression profiles and transcriptional regulatory pathways that underlie the identity and diversity of mouse tissue macrophages . Nat Immunol 13 ( 11 ): 1118 - 1128 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gosselin D. , Link V. M. , Romanoski C. E. , Fonseca G. J. , Eichenfield D. Z. , Spann N. J. , Stender J. D. , Chun H. B. , Garner H. , Geissmann F. , et al. .( 2014 . ). Environment drives selection and function of enhancers controlling tissue-specific macrophage identities . Cell 159 ( 6 ): 1327 - 1340 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ginhoux F. and Guilliams M. ( 2016 . ). Tissue-Resident Macrophage Ontogeny and Homeostasis . Immunity 44 ( 3 ): 439 - 449 . [DOI] [PubMed] [Google Scholar]
- 8. Hoeksema M. A. and Glass C. K. ( 2019 . ). Nature and nurture of tissue-specific macrophage phenotypes . Atherosclerosis 281 : 159 - 167 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jaitin D. A. , Adlung L. , Thaiss C. A. , Weiner A. , Li B. , Descamps H. , Lundgren P. , Bleriot C. , Liu Z. , Deczkowska A. , et al. .( 2019 . ). Lipid-Associated Macrophages Control Metabolic Homeostasis in a Trem2-Dependent Manner . Cell 178 ( 3 ): 686 - 698 e614 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jensen S. M. , Bechshoft C. J. L. , Heisterberg M. F. , Schjerling P. , Andersen J. L. , Kjaer M. and Mackey A. L. ( 2020 . ). Macrophage Subpopulations and the Acute Inflammatory Response of Elderly Human Skeletal Muscle to Physiological Resistance Exercise . Front Physiol 11 : 811 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kosmac K. , Peck B. D. , Walton R. G. , Mula J. , Kern P. A. , Bamman M. M. , Dennis R. A. , Jacobs C. A. , Lattermann C. , Johnson D. L. , et al. .( 2018 . ). Immunohistochemical Identification of Human Skeletal Muscle Macrophages . Bio-protocol 8 ( 12 ): e2883 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kratofil R. M. , Kubes P. and Deniset J. F. ( 2017 . ). Monocyte Conversion During Inflammation and Injury . Arterioscler Thromb Vasc Biol 37 ( 1 ): 35 - 42 . [DOI] [PubMed] [Google Scholar]
- 13. Krasniewski L. K. , Chakraborty P. , Cui C. Y. , Mazan-Mamczarz K. , Dunn C. , Piao Y. , Fan J. , Shi C. , Wallace T. , Nguyen C. , et al. .( 2022 . ). Single-cell analysis of skeletal muscle macrophages reveals age-associated functional subpopulations . eLife 11 : e77974 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lavin Y. , Winter D. , Blecher-Gonen R. , David E. , Keren-Shaul H. , Merad M. , Jung S. and Amit I. ( 2014 . ). Tissue-resident macrophage enhancer landscapes are shaped by the local microenvironment . Cell 159 ( 6 ): 1312 - 1326 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Liu L. , Cheung T. H. , Charville G. W. and Rando T. A. ( 2015 . ). Isolation of skeletal muscle stem cells by fluorescence-activated cell sorting . Nat Protoc 10 ( 10 ): 1612 - 1624 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mills C. D. , Kincaid K. , Alt J. M. , Heilman M. J. and Hill A. M. ( 2000 . ). M-1/M-2 macrophages and the Th1/Th2 paradigm . J Immunol 164 ( 12 ): 6166 - 6173 . [DOI] [PubMed] [Google Scholar]
- 17. Martinez F. O. , Sica A. , Mantovani A. and Locati M. ( 2008 . ). Macrophage activation and polarization . Front Biosci 13 : 453 - 461 . [DOI] [PubMed] [Google Scholar]
- 18. Rath M. , Muller I. , Kropf P. , Closs E. I. and Munder M. ( 2014 . ). Metabolism via Arginase or Nitric Oxide Synthase: Two Competing Arginine Pathways in Macrophages . Front Immunol 5 : 532 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Shapouri-Moghaddam A. , Mohammadian S. , Vazini H. , Taghadosi M. , Esmaeili S. A. , Mardani F. , Seifi B. , Mohammadi A. , Afshari J. T. and Sahebkar A. ( 2018 . ). Macrophage plasticity, polarization, and function in health and disease . J Cell Physiol 233 ( 9 ): 6425 - 6440 . [DOI] [PubMed] [Google Scholar]
- 20. Tidball J. G. ( 2011 . ). Mechanisms of muscle injury, repair, and regeneration . Compr Physiol 1 ( 4 ): 2029 - 2062 . [DOI] [PubMed] [Google Scholar]
- 21. Tidball J. G. ( 2017 . ). Regulation of muscle growth and regeneration by the immune system . Nat Rev Immunol 17 ( 3 ): 165 - 178 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Underhill D. M. , Gordon S. , Imhof B. A. , Nunez G. and Bousso P. ( 2016 . ). Elie Metchnikoff(1845-1916): celebrating 100 years of cellular immunology and beyond . Nat Rev Immunol 16 ( 10 ): 651 - 656 . [DOI] [PubMed] [Google Scholar]
- 23. Walton R. G. , Kosmac K. , Mula J. , Fry C. S. , Peck B. D. , Groshong J. S. , Finlin B. S. , Zhu B. , Kern P. A. and Peterson C. A. ( 2019 . ). Human skeletal muscle macrophages increase following cycle training and are associated with adaptations that may facilitate growth . Sci Rep 9 ( 1 ): 969 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Wang X. , Sathe A. A. , Smith G. R. , Ruf-Zamojski F. , Nair V. , Lavine K. J. , Xing C. , Sealfon S. C. and Zhou L. ( 2020 . ). Heterogeneous origins and functions of mouse skeletal muscle-resident macrophages . Proc Natl Acad Sci U S A 117 ( 34 ): 20729 - 20740 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wynn T. A. , Chawla A. and Pollard J. W. ( 2013 . ). Macrophage biology in development, homeostasis and disease . Nature 496 ( 7446 ): 445 - 455 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yang W. and Hu P. ( 2018 . ). Skeletal muscle regeneration is modulated by inflammation . J Orthop Translat 13 : 25 - 32 . [DOI] [PMC free article] [PubMed] [Google Scholar]