Abstract
Objective:
Emergency obstetric and newborn care services treat 70–80% of maternal deaths. This study aimed to assess satisfaction with comprehensive emergency obstetric and newborn care (CEmONC) services and associated factors among clients in the University of Gondar Specialized Hospital.
Methods:
Institution-based cross-sectional study was conducted on 404 participants using a systematic random sampling method. The study was conducted from March 5 to May 5, 2020, using interviewer-administered structured questionnaires. Binary logistic regression was used to find the association between independent variables and client satisfaction. The level of statistical significance was declared at a p value less than 0.05.
Results:
The overall clients’ satisfaction with CEmONC services was 65.1% (95% confidence interval (CI): 60.9–69.8). Clients’ satisfaction was affected by women who had antenatal care (ANC) of three visits (adjusted odds ratio (AOR): 6.5; 95%, CI: 2.04–20.8), women waited less than 15 min (AOR: 4.15, 95% CI: 1.9–9.06), mothers stayed ⩽1 day (AOR: 0.28, 95% CI: 0.09–0.9) and 2–3 days (AOR: 0.98, 95% CI: 0.1–0.69), obtaining a welcoming environment (AOR: 4.6, 95% CI: 2.15–9.88), and getting providers explanation of examinations (AOR: 3.3, 95% CI: 1.97–5.52).
Conclusion:
The observed clients’ satisfaction with CEmONC services was suboptimal. Having ANC of three visits, waiting less than 15 min, duration of stay, obtaining a welcoming environment, and an explanation of providers’ examination were the identified factors of client’s satisfaction. Therefore, hospital managers and health professionals should work on the identified factors to increase the client’s satisfaction with these services.
Keywords: Client satisfaction, comprehensive emergency obstetric and newborn care services, University of Gondar Specialized Hospital
Introduction
Emergency obstetric and newborn care (EmONC) services can be defined as a set of critical life-saving interventions and care for women as well as newborns during pregnancy, birth, and postpartum period if or when a woman or newborn experiences serious complications.1 Comprehensive emergency obstetric and newborn care (CEmONC) facilities are expected to provide the nine signal functions, including administration of parenteral uterotonics, administration of parenteral antibiotics, administration of parenteral anticonvulsants, removal of retained product of conception (manual vacuum aspiration, dilatation, and curettage), assisted vaginal delivery(vacuum and forceps delivery), manual removal of placenta, resuscitation of newborn, cesarean section, and blood transfusion.1
About 800 women die globally each day from preventable causes of pregnancy and childbirth. Nearly 99% of all maternal deaths occur in developing countries, with Sub-Saharan Africa accounting for more than half of the deaths.2 In Ethiopia, according to the 2016 Ethiopian Demographic and Health Survey (EDHS) report, 412 maternal deaths per every 100,000 live births and 29 neonatal deaths per 1000 live births occurred.3
The main complications that cause 80% of maternal deaths are hemorrhage, sepsis, unsafe abortion, hypertensive disorders of pregnancy, prolonged/obstructed labor, and ectopic pregnancy.2,4,5 An estimated 15% of women are expected to develop these serious complications.1,2 Achieving the sustainable development goal (SDG) target of a worldwide maternal mortality rate (MMR) below 70 requires reducing the MMR by an average of 7.5% each year between 2016 and 2030 globally.5 Accordingly, to achieve this SDG target and to reduce maternal mortality, applying the EmONC services has a pivotal role because it can prevent and treat direct obstetric complications that make up approximately 70–80% of maternal deaths and neonatal deaths by 10–15%.1
Low quality of care is one of the main contributing factors to elevated rates of morbidity and mortality. Even if life-saving interventions are available, women who perceive poor treatment quality may choose to avoid facility-based deliveries,6 which can be a major challenge to achieving SDGs of reducing maternal mortality to 70 per 100,000 live births.7 Therefore, health facilities are highly forced to maintain the quality of different services, including maternal health services to attract the attention of mothers which, in turn, can improve maternal satisfaction and reduce maternal health disease complications.
Client satisfaction is a measure of the quality of medical services, which provides feedback for providers and gives opportunities to improve services.8 Furthermore, WHO focuses on maternal satisfaction as a way of secondary prevention of maternal mortality because satisfied women are more likely to stick to providers’ recommendations.2 If the women are adhering to healthcare providers’ recommendation, they can use maternal services appropriately, and then maternal mortality will be reduced since they will be cured of the illnesses without further complications.
Several studies on the level of satisfaction with maternal care services have been conducted in various countries. Accordingly, a study on satisfaction with maternal and child care in Egypt tertiary hospital revealed that the overall satisfaction was 78.5%,9 and another study in Pakistan revealed that the overall satisfaction level was 61%.10 In a similar study in Iran medical center, the maternal satisfaction level was 59.5%.11 Additionally, a study in Ethiopia about satisfaction with EmONC services was 79.4%12 and another cross-sectional study in Mekelle public hospitals on the gynecology and obstetrics ward admitted patients were 79.7%.13 Moreover, a study on the satisfaction level of institutional delivery service in West Shewa found 60.8%.14
Several factors of client satisfaction with maternal care services have been identified, like sociodemographic characteristics including age,15–19 educational status,15,17,20–22 residence,13,23 and monthly income.15,17,24 Furthermore, maternal satisfaction was influenced by the current obstetric history, which includes parity,16 antenatal care (ANC) follow-up,15,16,18 the desire of the current pregnancy,17,18,25 reason of visit,25 mode of delivery,17,25,26 and presence of companion14,26 influence the maternal satisfaction. Client satisfaction with maternal services was also affected by the accessibility of services such as distance,18,22,26 waiting time,15,17,21,27 duration of hospital stay13,17 and health facility-related factors like availability of equipment12,18,25,26 and drugs,12,15 cleanness,15,18,28 and welcoming of environment.22 It is also affected by the client–provider interaction including an explanation of the procedures,12,14,17,29 consent requesting,14,30 and privacy.13,15,17,22,31 Even though the above several studies were focused maternal satisfaction with delivery services, there was a paucity of evidence in Ethiopia on the satisfaction level of clients with obstetric complications. However, there was still no sufficient evidence about the magnitude and factors of client satisfaction on CEmONC services in Ethiopian referral hospitals.
Therefore, this study aimed to assess satisfaction with CEmONC services and associated factors among clients in the University of Gondar Specialized Hospital. The result of this study will help to improve the quality of CEmONC services by providing feedback for healthcare providers, hospital managers, and policymakers.
Materials and methods
Study design and setting
An institution-based cross-sectional study design was used. The study was conducted from March 05, 2020 to May 05, 2020, at the University of Gondar Comprehensive Specialized Hospital. The University of Gondar Comprehensive Specialized Hospital is located in Gondar town, which is about 725 km away from the capital city of Addis Ababa and 180 km away from the regional city of Bahir Dar. The University of Gondar Specialized Hospital is a tertiary hospital serving more than 5 million people, and it has about 550 beds. It had four maternity wards and one gynecology ward for obstetric admissions. Since it is a teaching hospital, thousands of students learn by interacting with patients.
Source and study population
All women with abortive pregnancy outcomes and delivery within 7 days of postpartum who received one of the signal functions of CEmONC services at the University of Gondar Specialized Hospital were the source population, whereas randomly selected women with abortive pregnancy outcomes and delivered mother within 7 days of postpartum who received at least one of the signal functions of CEmONC services at the University of Gondar Specialized Hospital were the study population. Mothers who were unable to communicate due to serious illness were excluded.
Sample size determination
The sample size was determined by the single population proportion formula by considering 50% of the proportion since no previous study was done, with the assumption of a 95% confidence interval (CI), a 5% margin of error, and a 10% non-response rate.
n = (Za/2)2*P (1 − P)/d2
n = (1.96)2 *(0.50) (0.50)/(0.0025)
n = 384 after adding the non-response rate of 10%, the sample size was 423.
Sampling procedure and sampling technique
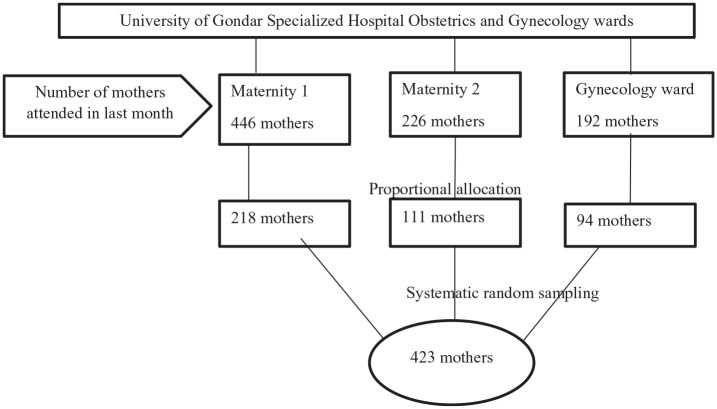
A systematic random sampling technique was used to select study participants in the study. The total sample size calculated for the study (423) was distributed to the obstetric wards in the hospital using proportional allocation based on the previous month’s report of 864 mothers who attended emergency obstetric care. The first client to be included in the study was selected randomly from the first two discharged mothers, and then every other woman was included in the study (Figure 1).
Figure 1.
A sampling procedure of client satisfaction with CEmONC services at the University of Gondar Referral Hospital, Northwest Ethiopia, 2020.
CEmONC: comprehensive emergency obstetric and newborn care.
Variables and measurements
Clients’ satisfaction with CEmONC services was the dependent variable. The independent variables were sociodemographic characteristics (age, religion, marital status, occupation, residence, educational level, income), obstetric factors (gravidity, mode of delivery, the desire of current pregnancy, ANC visit, presence of a companion, birth outcome), health facility-related factors (welcoming environment, cleanliness of the room, cleanness of the toilet), client–provider interaction factors (self-introduction, privacy, explanation of procedures, consent seeking), and accessibility-related factors (waiting time, duration of stay, distance to hospital).
The abortive pregnancy outcomes: Those women who were pregnant and end up with spontaneous abortion and ectopic pregnancy.1
Waiting time: Maternal perception of staying time between arrivals to the time seen by the health professional.
Welcoming environment: the perception of mothers about the care given by the hospital staff from entry to the hospital gate until admission to ward.32
Satisfied: Mothers who scored more than or equal to 75% on the 18 satisfaction measuring items were categorized as satisfied, after transformation of the individual’s satisfaction score from 1% to 100% for each item.32,33
Dissatisfied: Mothers who scored less than 75% on the 18 satisfaction measuring items were categorized as dissatisfied.32,33
Data collection procedure
Data were collected using a pretested and structured interviewer-administered questionnaire at the time of discharge. It contained the sociodemographic characteristics of the mother, the current obstetric history of the mother, accessibility of CEmONC services-related questions, client–provider interaction, and 18 satisfaction measuring questions. Satisfaction measuring questions were adapted from the Averting Maternal Death and Disability program quality improvement tool34 and the literature,12 and presented using a 5-scale Likert scale (1—very dissatisfied, 2—dissatisfied, 3—neutral, 4—satisfied, and 5—very satisfied).
The questionnaire was first prepared in English and translated into the local language (Amharic). Data were collected by three-diploma level female nurses and supervised by the one-degree level midwife.
Data quality assurance
A pretest was conducted using 21 mothers (5% of the study sample size) in Felege Hiwot referral hospital before 2 weeks of actual data collection. The necessary adjustments and modifications were done based on the pretest findings. The 1-day training was given for data collectors and the supervisor about the objective of the study and the data collection technique. The trained supervisor (midwife) checked the completeness and consistency of day-to-day collected data. The overall data collection activity was controlled by the principal investigator of the study. All completed questionnaires were examined every day after data collection for completeness and consistency. The Cronbach’s alpha coefficient for all the satisfaction measurement items was 0.88.
Statistical analysis
The collected data were entered and coded using Epi Data version 4.6 and exported to Statistical Package for Social Science version 22 for analysis. Different frequency tables, graphs, and descriptive summaries were used to describe the study variables. Bivariable and multivariable logistic regression analyses were used to analyze the association between the outcome variable and various independent variables. Variables with p value <0.2 in the bivariable analysis were entered into multivariable analysis to control for possible confounders. The adjusted odds ratio (AOR) and CI were used to measure the strength of associations. Statistical significance was declared when the p value was less than 0.05.
Results
Sociodemographic characteristics of the respondents
A total of 404 mothers responded to the interviewer-administered questionnaire with a response rate of 95.5%. The median age (with interquartile range (IQR)) of the participants was 28 (IQR: 24–32) years.
Of all the participants, 140 (34.7%) of them were illiterate without any formal education, and almost two-thirds (65.3%) were urban dwellers. Regarding religion, the majority of 351 (86.9%) respondents were orthodox. The vast majority of 364 (90%) respondents were married and 179 (44.3%) of participants were housewives. More than half of the participants (53.5%) had more than 3000 Ethiopian birrs (ETB) of monthly income. The median income of participants was 3500 (IQR: 2000, 6000) ETB (Table 1).
Table 1.
Sociodemographic characteristics of respondents in the University of Gondar Specialized Hospital, Gondar, Ethiopia, March 2020 (n = 404).
| Variable | Frequency | Percent (%) |
|---|---|---|
| Age (years) | ||
| <20 | 16 | 4 |
| 20–34 | 317 | 78.5 |
| >34 | 71 | 17.6 |
| Residence | ||
| Urban | 264 | 65.3 |
| Rural | 140 | 34.7 |
| Religion | ||
| Orthodox | 351 | 86.9 |
| Muslim | 50 | 12.4 |
| Protestant | 3 | 0.7 |
| Maternal educational status | ||
| No formal education | 140 | 34.7 |
| Primary (1–8) | 42 | 10.4 |
| Secondary (9–10) | 107 | 26.5 |
| Above secondary | 115 | 28.5 |
| Maternal occupation | ||
| Housewife | 179 | 44.3 |
| Private employee | 116 | 28.7 |
| Governmental employee | 97 | 24 |
| Others | 12 | 3 |
| Marital status | ||
| Single | 40 | 9.9 |
| Married | 364 | 90.1 |
| Household income (ETB) | ||
| <1000 | 21 | 5.2 |
| 1000–2000 | 102 | 25.2 |
| 2001–3000 | 65 | 16.1 |
| >3000 | 216 | 53.5 |
Other: non-governmental employee, students, unemployed.
ETB: Ethiopian birr.
Obstetric history of the respondents
Among the interviewed participants, 122 (30.2%) had complications caused by prolonged labor, 86 (21.3%) had complications caused by hemorrhage, and 61 (15.1%) were complicated with the abortive pregnancy outcomes. Nearly, two-thirds of participants (63.1%) were having two to five pregnancies and 359 (88.9%) of current pregnancies were planned. More than half (53.2%) of the participants have used an ambulance as a mode of transportation. In all, 355 (87.9%) mothers had a history of ANC follow-up, and out of the total mothers who had ANC attendance, about 226 (63.7%) had four times and above. Moreover, more than one-third of mothers (35.6%) and 117 (34.1%) were delivered by cesarean section and spontaneous vaginal delivery, respectively. Out of the total births, 32 (9.3%) were stillbirths, and 2 (0.6%) neonatal deaths were recorded (Table 2).
Table 2.
Obstetric history of respondents in the University of Gondar Specialized Hospital, Gondar, Ethiopia, March 2020 (n = 404).
| Variable | Frequency | Percent (%) |
|---|---|---|
| Gravidity | ||
| Primi-gravida | 110 | 27.2 |
| Two–five | 255 | 63.1 |
| More than five | 39 | 9.7 |
| Maternal obstetric complication | ||
| Hemorrhage | 86 | 21.3 |
| Prolonged labor | 122 | 30.2 |
| Postpartum sepsis | 30 | 7.4 |
| Abortion | 43 | 10.6 |
| Pregnancy-induced hypertension | 48 | 11.9 |
| Ectopic pregnancy | 18 | 4.5 |
| Newborn distress | 57 | 14.1 |
| ANC follow-up | ||
| Yes | 355 | 87.9 |
| No | 49 | 12.1 |
| Number of ANC visits (n = 355) | ||
| Once | 18 | 5.1 |
| Twice | 12 | 3.4 |
| Three times | 99 | 27.9 |
| Four times and above | 226 | 63.7 |
| Desire for current pregnancy | ||
| Wanted | 359 | 88.9 |
| Unwanted | 45 | 11.1 |
| Type of visit | ||
| Planned | 229 | 56.7 |
| Referred | 175 | 43.3 |
| Mode of transportation | ||
| Ambulance | 215 | 53.2 |
| Public transport | 182 | 45.0 |
| Other | 7 | 1.7 |
| Presence of companion | ||
| Yes | 396 | 98.0 |
| No | 8 | 2.0 |
| Mode of delivery | ||
| Abortive outcome | 61 | 15.1 |
| SVD | 117 | 29 |
| AVD | 104 | 25.7 |
| Cesarean section | 122 | 30.2 |
| Birth outcome (n = 343) | ||
| Alive | 309 | 90.1 |
| Stillbirth | 32 | 9.3 |
| Neonatal death | 2 | 0.6 |
| History of stillbirth (n = 294) | ||
| Yes | 67 | 22.8 |
| No | 227 | 77.2 |
Other: on foot, private transport.
ANC: antenatal care; AVD: assisted vaginal delivery; SVD: spontaneous vaginal delivery.
Accessibility of CEmONC services and cleanness of the environment
The median distance traveled to receive the CEmONC service was 15 (IQR: 5–45) km. More than half of 214 (53%) of the participants had traveled less than 25 km. Two-thirds of respondents (66.3%) said they had waited less than 15 min for the services. The median duration of stay in the hospital was 2 (IQR: 2–3) days. In all, 355 (86.6%) of participant mothers believed that the hospital was welcoming, and 219 (55.3%) believed that the toilet was clean (Table 3).
Table 3.
Accessibility of CEmONC service in University of Gondar Specialized Hospital, Gondar, Ethiopia, March 2020 (n = 404).
| Variable | Frequency | Percent |
|---|---|---|
| Distance traveled for service (km) | ||
| <25 | 214 | 53 |
| 25–50 | 103 | 25.5 |
| 51–75 | 31 | 7.7 |
| >75 | 56 | 13.9 |
| Waiting time for services (minutes) | ||
| <15 | 268 | 66.3 |
| 15–30 | 93 | 23 |
| >30 | 43 | 10.6 |
| Duration of stay (days) | ||
| ⩽1 | 54 | 13.4 |
| 2–3 | 301 | 74.5 |
| ⩾4 | 49 | 12.1 |
| Welcoming from the gate | ||
| Yes | 350 | 86.6 |
| No | 54 | 13.4 |
| Toilet utilization | ||
| Yes | 396 | 98.0 |
| No | 8 | 2.0 |
| Cleanness of the toilet (n = 396) | ||
| Clean | 173 | 43.7 |
| Partially clean | 219 | 55.3 |
| Not clean | 4 | 1.0 |
| Cleanness of the ward | ||
| Clean | 226 | 55.9 |
| Partially clean | 176 | 43.6 |
| Not clean | 2 | 0.5 |
Km: kilometer.
Client–provider interaction
The vast majority of participants (94.1%) were not self-introduced by the provider, and 375 (92.8%) of participants believed that their privacy was kept. The majority of 359 (88.9%) participants were asked for consent for procedures and 256 (63.4%) of participants the procedure and examination were explained (Table 4).
Table 4.
Client–provider interaction-related information of respondents in the University of Gondar Specialized Hospital, Gondar, Ethiopia, March 2020 (n = 404).
| Variable | Frequency | Percent (%) |
|---|---|---|
| Self-introduction by the provider | ||
| Yes | 24 | 5.9 |
| No | 380 | 94.1 |
| Explanation of the procedure for the patient | ||
| Yes | 256 | 63.4 |
| No | 148 | 36.6 |
| Consent requesting | ||
| Yes | 359 | 88.9 |
| No | 45 | 11.1 |
| Privacy | ||
| Yes | 375 | 92.8 |
| No | 29 | 7.2 |
Clients’ satisfaction on CEmONC services
The proportion of mothers who were satisfied with CEmONC services in this study was 65.1% (95% CI: 60.9–69.8). Of all the respondents, 76.7% were satisfied with the outcome of the service, while 14.9% of participants were dissatisfied with the acceptance of their opinion. In all, 119 (29.5%) of participants were strongly satisfied with the professional capability to identify their problem providing early responses, whereas 76.7% were neither satisfied nor dissatisfied with the overall care and support given (Table 5).
Table 5.
Level of client satisfaction with CEmONC services at University of Gondar Specialized Hospital, Northwest Ethiopia, March 2020 (n = 404).
| Items | Satisfaction with CEmONC services | ||||
|---|---|---|---|---|---|
| SD (%) | Dissatisfied (%) | Neutral (%) | Satisfied (%) | SS (%) | |
| Health facility environment | |||||
| Health workers availability | 1 (0.2) | 42 (10.4) | 52 (12.9) | 293 (72.5) | 16 (4) |
| Examination equipment availability | 2 (0.5) | 35 (8.7) | 116 (28.7) | 202 (50) | 49 (12) |
| The availability of drugs and medical supplies | 0 | 57 (14.1) | 137 (33.9) | 153 (37.9) | 57 (14.1) |
| Availability of transportation | 1 (0.2) | 50 (12.4) | 63 (15.6) | 223 (55.2) | 67 (16.6) |
| Sufficiency of rooms | 1 (0.2) | 21 (5.2) | 32 (7.9) | 254 (62.9) | 96 (23.8) |
| Cleanliness of wards | 0 | 16 (4) | 45 (11.1) | 286 (70.8) | 57 (14.1) |
| Overall cleanliness of the hospital | 0 | 22 (5.4) | 136 (33.7) | 215 (53.2) | 31 (7.7) |
| Client–provider interaction | |||||
| Care providers’ explanation about condition | 1 (0.2) | 30 (7.4) | 70 (17.3) | 235 (58.2) | 68 (16.8) |
| Involvement in the decision | 0 | 28 (6.9) | 50 (12.4) | 236 (58.4) | 90 (22.3) |
| Acceptance of maternal opinion | 0 | 60 (14.9) | 89 (22) | 169 (41.8) | 86 (21.3) |
| Verbal encouragement and support during labor | 0 | 51 (12.6) | 70 (17.3) | 193 (47.8) | 90 (22.3) |
| Counseling | 1 (0.2) | 28 (6.9) | 50 (12.4) | 239 (59.2) | 86 (21.3) |
| Respect and courtesy | 0 | 18 (4.5) | 45 (11.1) | 241 (59.7) | 100 (24.8) |
| Perceived capability of health staff | 0 | 19 (4.7) | 34 (8.4) | 232 (57.4) | 119 (29.5) |
| Service provision | |||||
| Obtaining price-free drugs | 0 | 50 (12.4) | 124 (30.7) | 153 (37.9) | 77 (19.5) |
| The time spent on the examination | 0 | 13 (3.2) | 49 (12.1) | 285 (70.5) | 57 (14.1) |
| Outcome of the service | 0 | 10 (2.5) | 29 (7.2) | 310 (76.7) | 55 (13.6) |
| Overall care and support given | 0 | 1 (0.2) | 26 (6.4) | 310 (76.7) | 67 (16.6) |
SD: strongly dissatisfied; SS: strongly satisfied.
Factors associated with client satisfaction on CEmONC services
In bivariable logistic regression analysis, maternal age, residence, educational status, obstetric complication, number of ANC visits, mode of delivery, waiting time, duration of hospital stays, provider explanation about procedures and examinations, welcoming environment, and privacy had an association with clients’ satisfaction with CEmONC services at p value <0.2.
Then, these variables were entered and fitted to multivariable logistic regression to control the confounding effect of one variable to the other predictor variable. In the final model of the multivariable logistic regression analysis, the number of ANC visits, waiting time, duration of hospital stays, welcoming environment, and providers explanation about procedures and examinations were significant factors associated with overall maternal satisfaction toward CEmONC services at p < 0.05.
Accordingly, women who attended ANC visits three times were 6.5 times more likely to be satisfied (AOR: 6.5; 95% CI: 2.04–20.8) than compared to women who attended only once. Besides, women who waited less than 15 min to be seen by the healthcare provider were 4.15 times (AOR: 4.15; 95% CI: 1.9–9.06) more satisfied than women who waited more than 30 min.
Concerning the duration of hospital stay, women stayed less than or equal to 1 day and stayed 2–3 days were 72% (AOR: 0.28; 95% CI: 0.09–0.9) and 2% (AOR: 0.98; 95% CI: 0.1–0.69) less satisfied with CEmONC services compared to women stayed four and more days, respectively. Participants who obtained the welcoming environment were 4.6 times (AOR: 4.6; 95% CI: 2.15–9.88) more satisfied than their counterparts.
Moreover, women who got explanation about the procedures and examinations were 3.3 times (AOR: 3.3; 95% CI: 1.97–5.52) more likely to be satisfied than those who did not obtain explanations (Table 6).
Table 6.
Bivariable and multivariable analyses showing factors affecting clients’ satisfaction on CEmONC services, at the University of Gondar Specialized hospital, 2020 (n = 404).
| Explanatory variable | Satisfaction | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| Satisfied | Unsatisfied | |||
| Maternal age (years) | ||||
| <20 | 8 (50%) | 8 (50%) | 1 | 1 |
| 20–34 | 204 (64.4%) | 113 (35.6%) | 1.8 (0.66–4.94) | 1.93 (0.38–9.57) |
| >34 | 51 (71.8%) | 20 (28.2%) | 2.55 (0.84–7.72) | 1.95 (0.34–11.19) |
| Residence | ||||
| Urban | 156 (59.1%) | 108 (40.9%) | 1 | 1 |
| Rural | 107 (76.4%) | 33 (23.6%) | 2.24 (1.416–3.56)** | 1.54 (0.82–2.9) |
| Educational status | ||||
| No formal education | 104 (74.3%) | 36 (25.7%) | 2.07 (1.22–3.52) | 1.0 (0.45–2.25) |
| Primary (1–8) | 23 (54.8%) | 19 (45.2%) | 0.87 (0.43–1.77) | 0.82 (0.32–2.08) |
| Secondary (9–10) | 69 (64.5%) | 38 (35.5%) | 1.3 (0.76–2.24) | 1.49 (0.77–2.87) |
| Above secondary | 67 (58.3%) | 48 (41.7%) | 1 | 1 |
| Maternal obstetric complication | ||||
| Hemorrhage | 59 (68.6%) | 27 (31.4%) | 1 | 1 |
| Prolonged labor | 84 (68.9%) | 38 (31.1%) | 1.01 (0.56–1.83) | 1.93 (0.81–4.64) |
| Postpartum sepsis | 25 (83.3%) | 5 (16.7%) | 2.3 (0.79–6.62)* | 1.72 (0.37–8.18) |
| Abortion | 14 (32.6%) | 29 (67.4%) | 0.22 (0.10–0.48)** | 0.49 (0.06–3.81) |
| Pregnancy-induced HTN | 33 (68.8%) | 15 (31.2%) | 1.01 (0.48–2.16) | 1.78 (0.66–4.76) |
| Ectopic pregnancy | 10 (55.6%) | 8 (44.4%) | 0.57 (0.2–1.61) | 0.86 (0.62–5.58) |
| Newborn distress | 38 (66.7%) | 19 (33.3%) | 0.92 (0.45–1.87) | 1.50 (0.57–3.98) |
| Number of ANC visits | ||||
| Once | 8 (44.4%) | 10 (55.6%) | 1 | 1 |
| Twice | 7 (58.3%) | 5 (41.7%) | 1.75 (0.4–7.6) | 1.67 (0.32–8.47) |
| Three times | 80 (80.8%) | 19 (19.2%) | 5.26 (1.83–15.1)* | 6.5 (2.04–20.8)** |
| Four times and above | 147 (65%) | 79 (35%) | 2.3 (0.88–6.13) | 2.84 (0.98–8.22) |
| Mode of delivery | ||||
| Abortive outcome | 24 (39.3%) | 37 (60.7%) | 1 | 1 |
| SVD | 91 (77.8%) | 26 (22.2%) | 5.39 (2.75–10.58) | 0.99 (0.06–16.31) |
| AVD | 71 (68.3%) | 33 (31.7%) | 3.32 (1.72–6.4) | 0.60 (0.04–9.97) |
| Cesarean section | 77 (63.1%) | 45 (36.9%) | 2.64 (1.4–4.9) | 0.57 (0.04–8.94) |
| Waiting time for services (minutes) | ||||
| <15 | 193 (72%) | 75 (28%) | 3.25 (1.68–6.3)*** | 4.15 (1.9–9.06)*** |
| 15–30 | 51 (54.8%) | 42 (45.2%) | 1.5 (0.74–3.17) | 1.4 (0.62–3.24) |
| >30 | 19 (44.2%) | 24 (55.8%) | 1 | 1 |
| Duration of hospital stay (days) | ||||
| ⩽1 | 32 (59.3%) | 22 (40.7%) | 0.28 (0.11–0.72)** | 0.28 (0.09–0.90)* |
| 2–3 | 190 (63.1%) | 111 (36.9%) | 0.33 (0.15–0.74)** | 0.98 (0.10–0.69)** |
| ⩾4 | 41 (83.7%) | 8 (16.3%) | 1 | 1 |
| Welcoming environment | ||||
| Yes | 241 (68.9%) | 109 (31.1%) | 3.2 (1.78–5.79)*** | 4.6 (2.15–9.88)*** |
| No | 22 (40.7%) | 32 (59.3%) | 1 | 1 |
| Providers explain about procedures | ||||
| Yes | 193 (75.4%) | 63 (24.6%) | 3.41 (2.22–5.2)*** | 3.3 (1.97–5.52)*** |
| No | 70 (47.3%) | 78 (52.7%) | 1 | 1 |
| Privacy | ||||
| Yes | 252 (67.2%) | 123 (32.8%) | 3.35 (1.53–7.32)** | 1.68 (0.63–4.5) |
| No | 11 (37.9%) | 18 (62.1%) | 1 | 1 |
p < 0.05; **p ⩽ 0.01; ***p ⩽ 0.001.
ANC: antenatal care; AOR: adjusted odd ratio; AVD: assisted vaginal delivery; CEmONC: comprehensive emergency obstetric and newborn care; CI: confidence interval; COR: crude odd ratio; HTN: hypertension; SVD: spontaneous vaginal delivery.
Discussion
This study showed that the overall satisfaction of women with CEmONC services was 65.1% (95% CI: 60.9–69.8).
This study finding was consistent with studies done on maternal care satisfaction in countries such as Pakistan 61%,10 as well as studies in Ethiopia on satisfaction with institutional delivery service at Jimma Omo Nada district 62.8%.18
Whereas the finding of this study was higher than a study conducted in Addis Ababa, Ethiopia 21%.17 This variation might be due to the study population and study setting differences since residents of Addis Ababa might be more educated and more knowledgeable than the Gondar population they might expect more and which made them less satisfied.32 In addition, this study finding was also higher than a study done at the University of Gondar Specialized Hospital on satisfaction with the existing labor and delivery service 31.3%.32 The variation might be due to the real quality improvement of the maternal services in the hospital or it might be due to the study population of mothers with obstetric complications might be more satisfied when they are relieved from their complications.
However, this study finding was lower than a study conducted in countries in Nepal 89.88%,35 Egypt 78.5%,9 Nigeria teaching hospital 80%,24 and Bangladesh 85%.27 This variation might be due to the health institution or facility difference, the cultural and socioeconomic differences of mothers. This study finding was also lower than a study done in Ethiopia Jimma zone public health facilities 79.4%,12 Mekelle public health hospitals 79.7%,13 and Felege Hiwot referral hospital 74.9%.16 This variation might be due to the study population or it might be due to the operational definition they used for satisfaction or the real quality of maternal service.
Client satisfaction with service outcome was 76.7%, which was higher than the 52.6% found in a study of Jimma zone public facilities.12 This variation might be due to the real service quality differences or differences in methods and study population, as well as it might be due to the difference in the quality of service provided.
The number of ANC visits, waiting time to be seen by the healthcare providers, duration of stay, welcoming hospital environment, and providers’ explanation of procedures and examination were significant predictors of satisfaction with CEmONC services.
In this study, mothers who had ANC follow-up of three visits were 6.5 times more likely to satisfy than those with the first visit (AOR: 6.5; 95% CI: 2.04–20.8). In agreement with this result, a study on satisfaction with institutional delivery service in Assela hospital reported that women with more ANC visits were associated with good satisfaction,15 and another study conducted in Omo Nada district also indicated that ANC follow-up had increased maternal satisfaction two times.18 In addition, a study conducted on the perceived quality of basic EmONC services indicated that women who had ANC follow-up had high odds of perceived good quality.23 This might be due to mothers with more ANC visits might have the opportunity to know their delivery attendant, which might create a smooth environment that providers and mothers become friendly during delivery care.18 In addition, it could be due to mothers with ANC follow-up might have the opportunity for early identification of obstetric complications to get care early. Moreover, the third ANC visit might be linked with the identification of most obstetric complications and congenital anomalies. This implies that maternal ANC follow-up will increase maternal satisfaction with CEmONC services. However, this finding is contrary to a study conducted in Bahir Dar Felege Hiwot Hospital which found that ANC follow-up decreases maternal satisfaction.16 This difference might be related to maternal expectation or might be due to the study population difference of mothers without obstetric complications might expect more quality of care with more ANC follow-up.
This study revealed that mothers who had waited less than 15 min to be seen by the provider were 4.15 times more satisfied than mothers who waited more than 30 min (AOR: 4.15; 95% CI: 1.9–9.06). This finding was in agreement with the finding in Arba Minch town public health facilities, which reported that mothers who waited for less than 15 min were 3.4 times more satisfied than those who waited for more than 15 min.21 The possible reason for this might be the fact that the severity of the maternal complaint increases as waiting time increases. This implies that shortening waiting time will increase maternal satisfaction with CEmONC services.
Besides, women who stayed less than or equal to 1 day had decreased their satisfaction by 72% (AOR: 0.28; 95% CI: 0.09–0.9) and stayed 2–3 days decreased by 2% compared to women who stayed four or more days (AOR: 0.98; 95% CI: 0.1–0.69). This finding was in accordance with the study done in Addis Ababa, which reported that women stayed more than 2 days were 4.3 times more satisfied.17 The possible explanation might be due to the maternal perception of getting better care through longer stays and caring for the fear of other complications.17 As a result, if the mothers perceived getting better service to manage the near future complications and stayed for more days, this might have led them to have higher satisfaction. However, it was contrary to a study in Mekelle public hospitals which found that patients who stayed less than 4 days were 2.27 times more satisfied.13 This difference might be due to the study population and study setting. That is, this study was done on complicated obstetric mothers rather than all women admitted to obstetrics and gynecology wards, which were done in Mekelle public health hospitals. In this regard, clients who develop pregnancy-related complications might directly be linked with pain and dissatisfaction.
In this study, an explanation of the procedures and examinations was also one of the most important predictors of client satisfaction with CEmONC services. Accordingly, mothers who obtained explanations about the procedures were 3.3 times more likely to be satisfied than their counterparts (AOR: 3.3; 95% CI: 1.97–5.52). This finding was supported by the study carried out in West Shewa zone public health facilities, which revealed that mothers whose care providers explained what was being done were 2.2 times more satisfied than their counterparts.14 This study finding also agrees with the study conducted in Asrade Zewdie memorial hospital, which revealed that mothers whose care providers answered their questions during delivery were more satisfied than those who did not.22 The possible explanation for this might be that mothers whom the provider did not explain the procedure might likely to perceive as the provider undermined them and feel that did not consider their right for involvement in decision of their care.14 This implies that providers’ explanation is very important to increases maternal satisfaction for EmONC services.
Moreover, clients who considered the hospital as a welcoming environment were 4.6 times more satisfied than their counterparts (AOR: 4.6; 95% CI: 2.15–9.88). This finding agrees with the study done in Asrade Zewdie hospital, mothers with a welcoming environment were three times more likely to be satisfied than their counterparts.22 The possible explanation for this might be that mothers who did not obtain welcome at the hospital might perceive as the hospital workers ignore them, which implies that warm welcoming by the hospital staff will increase maternal satisfaction with CEmONC services.
Limitations of the study
The mothers were interviewed within the hospital, and they might give responses favoring the care providers, which resulted in increasing the magnitude of satisfaction due to social desirability bias. Involving only one facility might not represent the satisfaction level of CEmONC services, and only quantitative data may not explore the other maternal satisfaction factors. Pilot test was not conducted for the questionnaire used in this study.
Conclusion
The observed satisfaction of clients toward CEmONC services in the University of Gondar Specialized Hospital was suboptimal.
Moreover, the study identified that number of ANC visits, waiting time, duration of stay, obtaining a welcoming environment, and an explanation of providers’ examination were significant predictors of clients’ satisfaction with CEmONC services.
We recommend that the federal ministry of health, regional health bureau, zonal health office, and health institutions should have to work on maternal awareness for adherence to the recommended ANC follow-up. Healthcare providers should avoid longer waiting times for mothers with obstetric complications and explain procedures and examinations to mothers. Further studies with qualitative methods and diverse study settings were also recommended for researchers.
Acknowledgments
The authors would like to thank all respondents for their willingness to participate in the study. We are also grateful to the University of Gondar Comprehensive and Specialized Hospital, and the University of Gondar, Institute of Public Health. Finally, our appreciation goes to data collectors for their unreserved contribution to the data collection process.
Footnotes
Authors’ contributions: M.G conceived the study, adapted the tool, coordinated the data collection activity, and carried out the statistical analysis. A.K and D.M participated in the design of the study, development of the tool, performed the statistical analysis and M.G and S.F drafted the manuscript. All authors read and approved the final manuscript.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval was obtained from the Institutional Research Review Committee of the Institute of Public Health, the University of Gondar with a reference number of (IPH/837/06/12). A support letter (Ref. No-HSP/8768/12) from the Department of Health Systems and Policy and a final approval support letter to conduct the study were obtained from the medical director of the University of Gondar Comprehensive Specialized Hospital.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from the study participants and they were assured that the documented personal information would be confidentially kept.
Informed consent: Written informed consent was obtained from all participants before the study.
ORCID iDs: Misganaw Guadie Tiruneh  https://orcid.org/0000-0002-9543-9416
https://orcid.org/0000-0002-9543-9416
Sefineh Fenta  https://orcid.org/0000-0002-3051-1296
https://orcid.org/0000-0002-3051-1296
Data availability: Data will be available with a reasonable request.
Trial registration: Not applicable.
References
- 1. Bailey P, Lobis S, Maine D, et al. Monitoring emergency obstetric care: a handbook. Geneva: World Health Organization, 2009. [Google Scholar]
- 2. WHO. Maternal mortality. Geneva: World Health Organization, 2014. [Google Scholar]
- 3. Central Statistical Agency. Ethiopian demographic and health survey 2016. Addis Ababa: The DHS Program, 2017. [Google Scholar]
- 4. Miltenburg AS, Kiritta RF, Bishanga TB, et al. Assessing emergency obstetric and newborn care: can performance indicators capture health system weaknesses? BMC Pregnancy Childbirth 2017; 17(1): 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. WHO. Trends in maternal mortality. Geneva: World Health Organization, 2015. [Google Scholar]
- 6. Austin A, Langer A, Salam RA, et al. Approaches to improve the quality of maternal and newborn health care: an overview of the evidence. Reprod Health 2014; 11: S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. UN. Transforming our world: the 2030 agenda for sustainable development. New York, NY: UN, 2016. [Google Scholar]
- 8. Donabedian AJAA. The definition of quality and approaches to its measurement. Chicago, IL: Health Administration Press, 1980. [Google Scholar]
- 9. Sayed W, Abd ElAal DEM, Mohammed HS, et al. Maternal satisfaction with delivery services at tertiary university hospital in upper Egypt, is it actually satisfying? Int J Reprod Contracept Obstet Gynecol 2018; 7: 7. [Google Scholar]
- 10. Ashraf M, Ashraf F, Rahman A, et al. Assessing women’s satisfaction level with maternity services: Evidence from Pakistan. Int J Collab Res Intern Med Public Health 2012; 4(11): 1841–1851. [Google Scholar]
- 11. Taghavi S, Ghojazadeh M, Azami-Aghdash S, et al. Assessment of mothers’ satisfaction with the care of maternal care in Specialized Educational-Medical Centers in obstetrics and gynecological disease in Northwest, Iran. J Res Clin Med 2014; 3(2): 77–86. [Google Scholar]
- 12. Kumsa A, Tura G, Nigusse A, et al. Satisfaction with emergency obstetric and new born care services among clients using public health facilities in Jimma Zone, Oromia Regional State, Ethiopia; a cross sectional study. BMC Pregnancy Childbirth 2016; 16: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Marama T, Bayu H, Merga M, et al. Patient satisfaction and associated factors among clients admitted to obstetrics and gynecology wards of public hospitals in Mekelle town, Ethiopia: an Institution-Based Cross-Sectional Study. Obstet Gynecol Int 2018; 2018: 2475059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bulto GA, Demissie DB, Tasu TL, et al. Mother’s satisfaction with the existing labor and delivery care services at public health facilities in West Shewa zone, Oromia region, Ethiopia. BMC Pregnancy Childbirth 2020; 20: 303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Amdemichael R, Tafa M, Fekadu H. Maternal satisfaction with the delivery services in Assela Hospital, Arsi zone, Oromia region. Obstet Gynecol 2014; 4(12): 2161. [Google Scholar]
- 16. Mekonnen ME, Yalew WA, Anteneh ZA. Women’s satisfaction with childbirth care in Felege Hiwot Referral Hospital, Bahir Dar city, Northwest Ethiopia, 2014: cross sectional study. 2015; BMC Res Notes 8: 528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Melese T, Gebrehiwot Y, Bisetegne D, et al. Assessment of client satisfaction in labor and delivery services at a maternity referral hospital in Ethiopia. Pan Afr Med J 2014; 17: 76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tadesse BH, Bayou NB, Nebeb GT. Mothers’ satisfaction with institutional delivery service in public health facilities of Omo Nada District, Jimma Zone. J Clin Med Res 2017; 6(1): 23–30. [Google Scholar]
- 19. Yohannes B, Tarekegn M, Paulos W. Mothers” utilization of antenatal care and their satisfaction with delivery services in selected public health facilities of Wolaita Zone, Southern Ethiopia. Int J Sci Technol Res 2013; 2(2): 74–85. [Google Scholar]
- 20. Enabudoso E, Isara A. Determinants of patient satisfaction after cesarean delivery at a university teaching hospital in Nigeria. Int J Gynecol Obstet 114(3): 251–254. [DOI] [PubMed] [Google Scholar]
- 21. Dewana Z, Fikadu T, Abdulahi M, et al. Client perspective assessment of women’s satisfaction towards labour and delivery care service in public health facilities at Arba Minch town and the surrounding district, Gamo Gofa zone, south Ethiopia. J Reprod Health 2016; 13(1): 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Asres GD. Satisfaction of maternal care among women delivered at Asrade Zewude Memorial Primary Hospital, Bure, West Gojjam, Amhara, Ethiopia: a cross sectional study. J Public Health Epidemiol 2018; 10(5): 147–154. [Google Scholar]
- 23. Berhane B, Gebrehiwot H, Weldemariam S, et al. Quality of basic emergency obstetric and newborn care (BEmONC) services from patients’ perspective in Adigrat town, Eastern zone of Tigray, Ethiopia. 2017: a cross sectional study. BMC Pregnancy Childbirth 2019; 19(1): 190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nnebue C, Ebenebe U, Adinma E, et al. Clients’ knowledge, perception and satisfaction with quality of maternal health care services at the primary health care level in Nnewi, Nigeria. Niger J Clin Pract 2014; 17(5): 594–601. [DOI] [PubMed] [Google Scholar]
- 25. Bitew K, Ayichiluhm M, Yimam K. Maternal satisfaction on delivery service and its associated factors among mothers who gave birth in public health facilities of Debre Markos Town, Northwest Ethiopia. BioMed Res Int 2015; 2015: 460767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tesfaye R, Worku A, Godana W, et al. Client satisfaction with delivery care service and associated factors in the public health facilities of Gamo Gofa zone, Southwest Ethiopia: in a resource limited setting. Obstet Gynecol Int 2016; 2016: 5798068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Islam F, Rahman A, Halim A, et al. Perceptions of health care providers and patients on quality of care in maternal and neonatal health in fourteen Bangladesh government healthcare facilities: a mixed-method study. BMC Health Serv Res 2015; 15: 237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Austin A, Gulema H, Belizan M, et al. Barriers to providing quality emergency obstetric care in Addis Ababa, Ethiopia: healthcare providers’ perspectives on training, referrals and supervision, a mixed methods study. BMC Pregnancy Childbirth 2015; 15: 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Avortri GS, Beke A, Abekah-Nkrumah G. Predictors of satisfaction with child birth services in public hospitals in Ghana. Int J Health Care Qual Assur 2014; 24(3): 223–237. [DOI] [PubMed] [Google Scholar]
- 30. Dhital SR, Dhital MK, Aro AR. Clients’ perspectives on the quality of maternal and neonatal care in Banke, Nepal. Health Sci J 2015; 9(2): 1–6. [Google Scholar]
- 31. Gonie A, Tebeje B, Sinaga M. Satisfaction towards skilled delivery services and associated factors among mothers who gave birth at government health facilities, Jimma Town, Ethiopia. Clin Mother Child Health 2018; 15(3): 2. [Google Scholar]
- 32. Gashaye KT, Tsegaye AT, Shiferaw G, et al. Client satisfaction with existing labor and delivery care and associated factors among mothers who gave birth in university of Gondar teaching hospital; Northwest Ethiopia: institution based cross-sectional study. PLoS One 2019; 14(2): e0210693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Gebru DM, Biks GA, Tsegaye G, et al. Factors of patient satisfaction in adult outpatient departments of private wing and regular services in public hospitals of Addis Ababa, Ethiopia: a comparative cross-sectional study. BMC Health Serv Res 2019; 19: 869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. EngenderHealth and AMDD. Quality improvement for emergency obstetric care: Leadership manual and toolbook. New York: EngenderHealth, 2003. [Google Scholar]
- 35. Panth A, Kafle P. Maternal satisfaction on delivery service among postnatal mothers in a Government Hospital, Mid-Western Nepal. Obstet Gynecol Int 2018; 2018: 4530161. [DOI] [PMC free article] [PubMed] [Google Scholar]