Abstract
BACKGROUND
Fexuprazan, a novel potassium-competitive acid blocker, reversibly suppresses the K+/H+-ATPase enzyme in proton pumps within gastric parietal cells. Fexuprazan’s suppression of gastric acid was maintained in healthy individuals for 24 h in a dose-dependent manner.
AIM
To compare fexuprazan to esomeprazole and establish its efficacy and safety in patients with erosive esophagitis (EE).
METHODS
Korean adult patients with endoscopically confirmed EE were randomized 1:1 to receive fexuprazan 40 mg or esomeprazole 40 mg once daily for eight weeks. The primary endpoint was the proportion of patients with healed EE confirmed by endoscopy at week 8. The secondary endpoints included the healing rate of EE at week 4, symptom response, and quality of life assessment. Safety profiles and serum gastrin levels were compared between the groups.
RESULTS
Of the 263 randomized, 218 completed the study per protocol (fexuprazan 40 mg, n = 107; esomeprazole 40 mg, n = 111). Fexuprazan was non-inferior to esomeprazole regarding the healing rate at week 8 [99.1% (106/107) vs 99.1% (110/111)]. There were no between-group differences in the EE healing rate at week 4 [90.3% (93/103) vs 88.5% (92/104)], symptom responses, and quality of life assessments. Additionally, serum gastrin levels at weeks 4 and 8 and drug-related side effects did not significantly differ between the groups.
CONCLUSION
Fexuprazan 40 mg is non-inferior to esomeprazole 40 mg in EE healing at week 8. We suggest that fexuprazan is an alternative promising treatment option to PPIs for patients with EE.
Keywords: Gastroesophageal reflux, Esophagitis, Proton pump inhibitors, Heartburn, Quality of life
Core Tip: A mainstay therapy of erosive esophagitis (EE) is acid suppression using proton pump inhibitors (PPIs), which have shortcomings such as their slow absorption and variability in metabolism. Acid suppression can be competitively and reversibly achieved by a novel potassium-competitive acid blocker, fexuprazan. We compared the efficacy and safety of fexuprazan and esomeprazole (each 40 mg once daily) in patients with EE for 8 wk. We conclude that fexuprazan is a new alternative to PPIs, by showing that fexuprazan is not inferior to esomeprazole in endoscopic healing rate of EE at week 8 and in safety profiles.
INTRODUCTION
Gastro-esophageal reflux disease (GERD) is characterized by heartburn and acid regurgitation symptoms resulting from abnormal gastric reflux into the esophagus[1]. GERD prevalence is increasing in Asian and Western countries[2]. A recent report documented the worldwide prevalence of GERD as 13.3% (10.0% in Asia, 15.4% in North America, and 17.1% in Europe)[3]. The percentage change in age-standardized GERD prevalence in South Korea was 7.6% between 1990 and 2017[2]. GERD is classified as erosive esophagitis (EE) or non-erosive reflux disease (NERD) based on the presence of esophageal mucosal breaks via endoscopic examination[4]. Approximately one-third to half of the patients with EE complain of the typical symptoms of GERD[5]. In addition to typical symptoms, atypical and extraesophageal symptoms in patients with EE may impair health-related quality of life (HRQL)[6,7]. However, a poor HRQL is more likely associated with symptom frequency and severity rather than the presence or absence of EE[8].
A main treatment of GERD has been the use of proton pump inhibitors (PPIs). Current practical guidelines recommend PPIs as the first-line therapy for patients with EE[9]. PPIs irreversibly inhibit (H+/K+)-ATPase within the parietal cells of the gastric mucosa[10]. Studies have demonstrated that PPIs are 40%-50% more effective than placebo in healing of EE and resolving GERD symptoms[11,12]. Furthermore, complete healing of EE has been reported in 80% to 90% of patients after four and eight weeks of PPI treatment, respectively[11]. However, there are shortcomings of PPIs in GERD treatment, including unsatisfactory efficacy in atypical and extraesophageal symptoms and typical symptoms[13]. This might be due to the pitfalls of PPIs: The variability in PPI metabolism based on cytochrome P450 (CYP) 2C19 polymorphisms and the delayed onset of PPIs owing to their slow absorption associated with enteric coating to prevent degradation by acid.
As an alternative to PPI in GERD treatment, a novel potassium-competitive acid blocker (P-CAB), fexuprazan (Daewoong Pharmaceutical Co., Ltd., Seoul, South Korea), was developed[14]. In contrast to PPIs, metabolism of fexuprazan is independent of CYP 2C19; enteric coating is not needed because of acid stability. While PPIs bind irreversibly to only the active forms of the proton pump, fexuprazan can bind to both the active and inactive forms of the proton pump competitively and reversibly. A previous study on healthy individuals demonstrated the effect of fexuprazan’s acid suppression and tolerability, observing that gastric pH > 4 was reached within 2 h and maintained for 24 h in a dose-dependent manner[14].
Nevertheless, the effectiveness and safety of fexuprazan compared to esomeprazole, one of the most widely used PPIs in GERD, have not been confirmed among patients with EE. Therefore, this phase III, double-blind, randomized, active-controlled, multi-center study was conducted to compare the efficacy and safety between fexuprazan and esomeprazole in patients with EE.
MATERIALS AND METHODS
Study design and treatments
This randomized, double-blind, parallel-group, multicenter, and phase III trial was performed in 25 institutions in South Korea between December 2018 and August 2019. Adult patients provided written informed consent prior to enrolment, and then screening test including the endoscopy was performed. Eligible participants were randomized 1:1 to receive either fexuprazan 40 mg or esomeprazole 40 mg following the screening test. At this point, participants were stratified according to Los-Angeles (LA) Classification Grade classified by the result of upper gastrointestinal endoscopy.
To ensure the double-blinded nature of the study, patients were administered once daily with two tablets of the study medication (fexuprazan 40 mg or esomeprazole 40 mg with its matching placebo in the study and control groups, respectively) for eight weeks.
Compliance of the study medication was ascertained at each visit by participants returning the unused portion and empty packaging, and was calculated using the total numbers of tablets to be taken, of tablets actually taken, and of returned and unreturned tablets in each participant.
This study was approved by the institutional review boards of each institution, conducted in compliance with the relevant ethics guidelines, and registered at ClinicalTrials.gov (NCT03736369). All the study medications and procedures performed were in accordance with the 1964 Declaration of Helsinki and its later amendments, or comparable ethical standards.
Participants
Eligible participants were male or female patients (20-75 years old) with EE (LA Classification Grades A to D) confirmed by endoscopy at the same institution within 14 d of study treatment initiation. The major exclusion criteria were Barrett’s esophagus (> 3 cm); esophageal stricture; active peptic ulcers; ulcer-related stenosis; gastrointestinal bleeding; eosinophilic esophagitis; Zollinger-Ellison syndrome; inflammatory bowel diseases; irritable bowel syndrome; pancreatitis; psychiatric disorders; acquired immune deficiency syndrome (AIDS); viral hepatitis; history of gastric acid suppression surgery; significant morbidities in the cardiovascular, respiratory, hepatic, renal, neurologic, endocrine, hematologic, and urologic systems; history of malignancies within five years; drug or alcohol abuse; and hypersensitivity to drugs containing active constituents of esomeprazole or other similar drugs (benzimidazoles and antibiotics). Also excluded were those who had abnormal laboratory values, including alanine aminotransferase (ALT), aspartate transaminase (AST), alkaline phosphatase (ALP), γ-glutamyl transpeptidase (GGT), total bilirubin, creatinine, and blood urine nitrogen > 2´ upper limits of the normal range, and women with child-bearing potential who did not consent to appropriate contraceptive methods use during the study.
Protocol
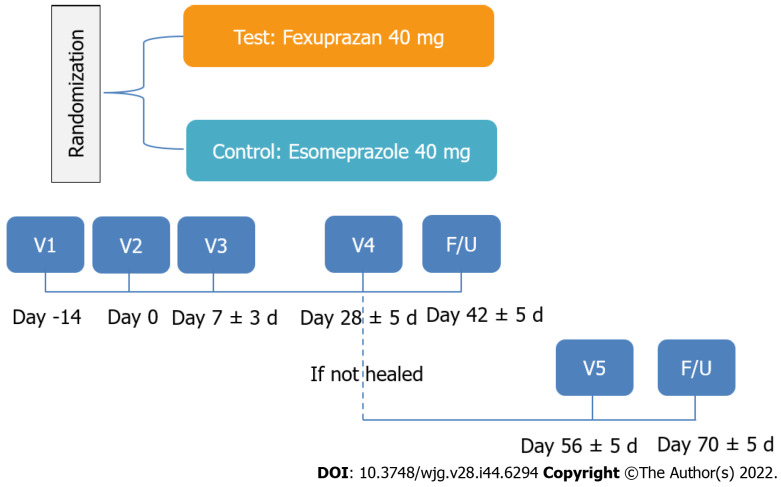
Endoscopy was performed at the start of the screening period and at weeks 4 and 8. EE healing was defined as the complete absence of mucosal breaks. If mucosal breaks did not heal at week 4, the patients continued to receive the study drug until week 8, when endoscopy was performed again. Two weeks after the confirmation of EE healing from the centralized endoscopic evaluation, the patients were evaluated for safety via telephone interviews, and where applicable, they underwent additional tests and procedures (Figure 1).
Figure 1.
Study schema. V: Visit; F/U: Follow-up.
The primary efficacy endpoint was the proportion of patients with endoscopically confirmed EE healing at week 8. The secondary efficacy endpoints were EE healing rate at week 4; the patients’ reported symptom outcomes, symptom assessment by reflux disease questionnaire (RDQ), and GERD-health related quality life (GERD-HRQL). Symptoms were evaluated based on patients’ symptom diaries. Symptom severity in the daytime and at night were measured according to the five-point scale (0: none, 1: mild, 2: moderate, 3: severe, 4: very severe).
The parameters for assessing symptom responses were the first day of the complete resolution of symptoms (heartburn, acid regurgitation, and heartburn/acid regurgitation) after treatment, the proportion of patients without symptoms in the first 7 d and through the 8 wk of treatment, and the proportion of symptom-free days in the first 7 d and through the 8 wk of treatment. Changes in symptoms and GERD-HRQL from baseline at weeks 4 and 8 were evaluated using the RDQ and GERD-HRQL scales, respectively. The RDQ is a self-administered questionnaires comprising of 12 items to assess the frequency and severity of heartburn, acid regurgitation, and dyspepsia. Each item for frequency and severity was scored from 0 to 5; the higher score, the more severe or frequent symptoms[15]. The RDQ demonstrated the validity and reliability for diagnosis of GERD in primary care and community settings[16]. The GERD-HRQL scale comprises 11 items for the symptoms of heartburn and dysphagia, medication effects, and the patients’ health conditions[17]. Each item was scored from 0 to 5; the higher the score, the lower the quality of life. The GERD-HRQL was validated and considered as an appropriate instrument to evaluate typical GERD symptoms[18]. Therefore, previous clinical studies performed in South Korea have used the RDQ and GERD-HRQL to evaluate the therapeutic effect in patients with GERD[19,20].
Additional analyses included heartburn and extraesophageal symptoms of GERD (chronic cough and throat irritation) in terms of the proportion of patients without symptoms and the proportion of symptom-free days in the first 3 d, 7 d and through the 8 wk of treatment. Patients with mod-erate/severe heartburn (RDQ ≥ 3) were also compared between the groups in terms of the proportion of patients without symptoms and the proportion of symptom-free days in the first 3 d, 7 d and through the 8 wk of treatment.
The patients’ baseline characteristics included age, sex, body mass index (BMI), smoking history, drinking history, LA grade, Helicobacter pylori (H. pylori) infections, and CYP2C19 extensive metabolizer (EM)/poor metabolizer (PM) status. Serum gastrin levels were measured at weeks 4 and 8. Safety outcomes were measured by the analysis of adverse events (AEs), vital signs, physical examination, electrocardiogram (ECG) findings and laboratory tests. Adverse events (frequency, severity and seriousness) and concomitant medications were monitored throughout the study. Treatment-emergent adverse event (TEAE) was defined as an AEs newly occurred after the randomization and the first administration of study medication, and adverse drug reaction (ADR) was defined as any untoward and unintended response to the study medication of which causal relationship cannot be excluded.
Sample size
Based on previous studies, we estimated the sample size, assuming that the complete healing rate of mucosal breaks was 94.8% at week 8 after treatment with fexuprazan 40 mg and esomeprazole 40 mg[21,22]. Based on this threshold parameter, the sample size was 104 patients per treatment group, using the following conditions of the PASS program: non-inferiority margin of 10%[23], a one-sided significance level of 2.5%, 90% statistical power, and 1:1 randomization.
Randomization
This study was used stratified block randomization method base on LA grades (A/B/C/D) by the result of upper gastrointestinal endoscopy. An independent statistician generated a randomization list based on stratification factor (LA grades) using the PLAN (Proc Plan) procedure of SAS (ver. 9.4, SAS Institute, Cary, NC, United States). Eligible participants were randomly assigned by the investigators in a ratio of 1:1 via an interactive web-response system (IWRS). Neither participants nor relevant investigators were aware of these assignments.
Statistical analysis
Efficacy was evaluated by both the full analysis set (FAS) and per-protocol set (PPS), and PPS findings were interpreted as the main results. For the safety assessment, statistical analysis was performed on the safety set (SS). The FAS, based on the intention-to treat principle, included patients who received at least one dose of the study drug after randomization and had at least one primary efficacy assessment. The PPS included patients in the FAS who completed the study without any major protocol deviation. The SS group included all patients who received the study drug at least once after randomization.
For symptoms responses daily (day-time and night-time) assessment in the efficacy analysis, missing symptom in day-time or night-time was imputed using the last observation carried forward. Except for this, missing value was set to missing without imputation, and the results of patients who were completed the study early as mucosal breaks were completely healed up to week 4 were used as the results of the week 8.
Summaries of baseline characteristics of patients were presented in FAS. To assess the difference between the treatment group, the two sample t-test or Wilcoxon rank-sum test were used after normality evaluation in continuous baseline characteristics variables, and the chi-square test or Fisher’s exact test were used in categorical baseline characteristics variables.
The primary objective of the study was to demonstrate the non-inferiority of fexuprazan 40 mg compared with esomeprazole 40 mg. The cumulative healing rate of EE and corresponding two-sided 95% confidence interval (CI) were presented for visit (up to week 4 or week 8) by treatment group. The common risk difference of the healing rate of EE up to week 8 between the treatment groups (fexuprazan 40 mg group - esomeprazole 40 mg group) and corresponding two-sided 95% CI using the Cochran-Mantel-Haenszel method adjusted by a stratification factor (baseline LA grade) were presented in the PPS. The non-inferiority of fexuprazan 40 mg to esomeprazole 40 mg was determined the lower limit of its two-sided 95%CI is larger than the non-inferiority margin of -10%. The same analyses were performed for the non-inferiority of healing rate of EE up to week 4. Furthermore, continuous data were analyzed using an analysis of covariance (ANCOVA) model, including treatment group as treatment effect, and baseline score (included if evaluation data were changed from baseline) and baseline LA grade as covariates. The changes from baseline within-treatment group were used the paired t-test or Wilcoxon signed rank test after normality evaluation as a post hoc analysis. Categorical data were analyzed using the Cochran-Mantel-Haenszel method adjusted by baseline LA grade. For the safety analysis, the chi-square test or Fisher’s exact test was used to compare the difference in the incidence of AEs between the treatment groups. All statistical analyses were performed using SAS (ver. 9.4, SAS Institute, Cary, NC, United States) with a two-sided significance level of 5% for all tests.
RESULTS
Baseline characteristics of the participants
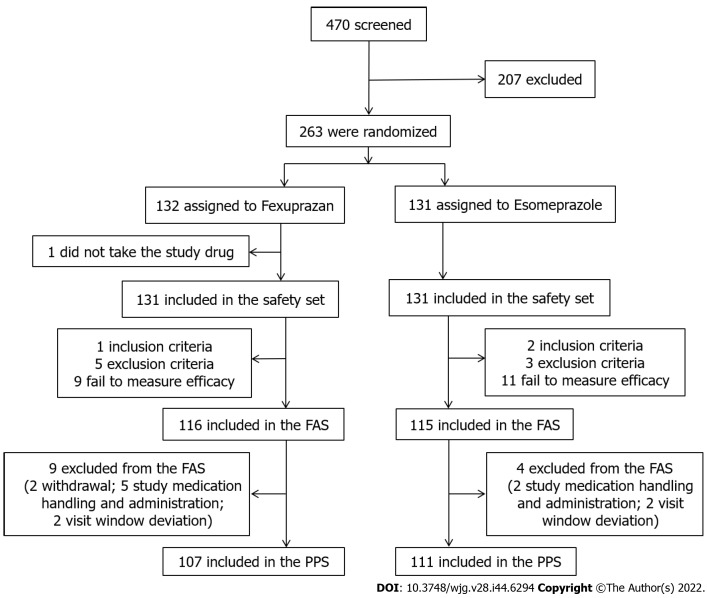
Of the total of 470 patients screened, 263 patients with EE were randomized to receive either fexuprazan 40 mg or esomeprazole 40 mg (Table 1). In total, 231 patients [152 men (65.8%) and 79 women (34.2%); 54.4 ± 12.7 mean age] were included in the FAS and completed the study (n = 116 and 115 in the fexuprazan and esomeprazole groups, respectively). Thirteen patients with study medication-related deviation, visit window deviation and consent withdrawal were excluded from the FAS (9 and 4 in the fexuprazan and esomeprazole groups, respectively), and 218 patients completed the study on the PPS (n = 107 and 111 in the fexuprazan and esomeprazole groups, respectively). The SS included 131 patients each in the fexuprazan and esomeprazole groups (Figure 2).
Table 1.
Baseline characteristics of the patients (full analysis set)
| Variables | Fexuprazan 40 mg (n = 116) | Esomeprazole 40 mg (n = 115) | P value | |
| Age, yr (mean ± SD)5 | 53.70 ± 12.44 | 55.05 ± 12.89 | 0.343w | |
| Sex, n (%)6 | ||||
| Men | 78 (67.2) | 74 (64.3) | 0.643c | |
| Women | 38 (32.8) | 41 (35.7) | ||
| BMI, kg/m2 (SD)5 | 24.42 ± 3.08 | 24.81 ± 3.25 | 0.529w | |
| Smoking history, n (%)6 | ||||
| Non-smokers | 67 (57.8) | 66 (57.4) | 0.978c | |
| Current smokers | 25 (21.6) | 26 (22.6) | ||
| Past smokers | 24 (20.7) | 23 (20.0) | ||
| Drinking history, n (%)6 | ||||
| Non-drinkers | 15 (12.9) | 15 (13.0) | 0.992c | |
| Current drinkers | 77 (66.4) | 77 (67.0) | ||
| Past drinkers | 24 (20.7) | 23 (20.0) | ||
| LA classification1, n (%)6 | ||||
| Grade A | 75 (64.7) | 76 (66.1) | 0.630f | |
| Grade B | 33 (28.4) | 31 (27.0) | ||
| Grade C | 6 (5.2) | 8 (7.0) | ||
| Grade D | 2 ( 1.7) | 0 (0.0) | ||
| Helicobacter pylori 2, n (%)6 | ||||
| Positive | 20 (17.4) | 31 (27.2) | 0.075c | |
| Negative | 95 (82.6) | 83 (72.8) | ||
| CYP2C193, n (%)6 | ||||
| EM | 39 (76.5) | 53 (94.6) | 0.007c | |
| PM | 12 (23.5) | 3 (5.4) | ||
| Severity for heartburn4, n (%)6 | ||||
| Mild | 53 (45.7) | 50 (43.5) | 0.735c | |
| Moderate/severe | 63 (54.3) | 65 (56.5) | ||
Values are mean SD or the number of the patients with percentage, where appropriate.
LA Classification (Grade A: One (or more) mucosal break(s) no longer than 5 mm, that does not extend between the tops of two mucosal folds, Grade B: One (or more) mucosal break(s) more than 5 mm long, that does not extend between the tops of two mucosal folds, Grade C: One (or more) mucosal break(s) that is continuous between the tops of two or more mucosal folds, but which involve(s) less than 75% of the oesophageal circumference, Grade D: One (or more) mucosal break(s) which involve(s) at least 75% of the oesophageal circumference).
Two subjects (Fexuprazan 40 mg: 1 subject, Esomeprazole 40 mg: 1 subject) did not have H. pylori results at baseline.
CYP2C19 genotype results were collected only from the subjects who agreed to the informed consent for genetic testing.
Severity for heartburn was defined based on the baseline Reflux disease questionnaire (RDQ). Mild: RDQ ≤ 2 (Less than or equal to 1 d out of 7 d), Moderate/Severe: RDQ ≥ 3 (Greater than or equal to 2 d out of 7 d).
Testing for difference between treatment groups after normality evaluation [Wilcoxon rank-sum test (w)].
Testing for difference among treatment groups [Chi-square test (c) or Fisher's exact test (f)].
BMI: Body mass index; LA: Los-Angeles; CYP2C19: Cytochrome P 2C19; EM: Extensive metabolizer; PM: Poor metabolizer.
Figure 2.
Flowchart of the study patients. SS: Safety set; FAS: Full analysis set; PPS: Per-protocol set.
There were no significant differences in baseline characteristics between both groups, except CYP2C19 genotypes (EM or PM). A statistically significant difference was seen in the classification of CYP2C19 genotype (P = 0.007), but the result was obtained from only some of the participants who agreed to genotyping (n = 51 and 56 in the fexuprazan and esomeprazole groups, respectively).
The mean compliance rates were 98.6% ± 8.1% and 99.0% ± 2.6% at weeks 4 and 8, and the overall compliance rate with study medication exceeded 95% in all treatment groups without between-group differences.
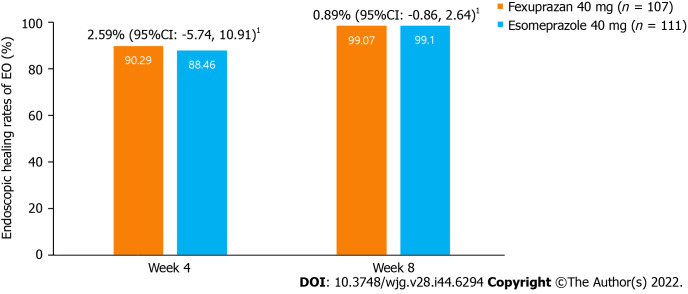
Efficacy
Healing rate of EE: In the PPS, the proportions of patients with complete absence of mucosal breaks at week 8 were 99.1% (106/107) and 99.1% (110/111) in the fexuprazan and esomeprazole groups, respectively. The difference in proportions of patients with complete absence of mucosal breaks adjusted by baseline LA grade [fexuprazan 40 mg group – esomeprazole 40 mg group] was 0.9% (95%CI, -0.9 to 2.6) (Figure 3). The lower limit of two-sided 95%CI at week 8, -0.9%, was greater than the non-inferiority margin of -10%, indicating the non-inferiority of 8-week treatment of fexuprazan 40 mg to esomeprazole 40 mg in EE healing in GERD. At week 4, the healing rates of EE were not different between the two groups [90.3% (93/103) in the fexuprazan group and 88.5% (92/104) in the esomeprazole group, respectively] with a difference of 2.6% (95%CI: -5.7 to 10.9). The lower limit of 95%CI, -5.7%, was also greater than the non-inferiority margin of -10%. These results demonstrate that fexuprazan 40 mg was non-inferior to esomeprazole 40 mg in EE healing in GERD at weeks 4 and 8.
Figure 3.
Erosive esophagitis healing rate at weeks 4 and 8 (per protocol set). Erosive esophagitis (EE) healing was defined as the complete absence of mucosal breaks confirmed by the endoscopy. 1Common risk difference of the healing rate of EE between the treatment groups (two-sided 95%CI) using the Cochran-Mantel-Haenszel method adjusted by baseline Los Angeles grade. EE: Erosive esophagitis; CI: Confidence interval.
As the results in the exploratory analysis, healing rates of EE were not statistically significantly different according to CYP2C19 genotype (EM or PM) and H. pylori infection (positive or negative). Healing rates of EE at weeks 4 and 8 in EM participants (n = 88) were not different between fexuprazn and esomeprazole groups [91.7% (33/36) vs 89.4% (42/47) at week 4; 100.0% (36/36) vs 98.1% (51/52) at week 8]. EE healing rates at weeks 4 and 8 in PM participants (n = 14) were not different between the treatment groups [70.0% (7/10) vs 100.0% (3/3) at week 4; 90.9% (10/11) vs 100.0% (3/3) at week 8]. Healing rates of EE in H. pylori-positive participants (n = 47) were 100.0% (17/17) and 88.46% (23/26) in the fexuprazan and esomeprazole groups at week 4, and all of H. pylori-positive participants were completely healed at week 8. Healing rates of EE in H. pylori-negative participants (n = 169) were 88.2% (75/85) vs 88.3% (68/77) at week 4, and 98.9% (87/88) vs 98.8 (80/81) at week 8 in the fexuprazan and esomeprazole groups.
Symptom response: Fexuprazan exhibited an overall symptom relief comparable to esomeprazole. The differences between the groups were not significant with respect to the first day of the complete resolution of symptoms (resolution of typical symptoms for 7 d) after treatment: the median values of days to complete resolution for heartburn, acid regurgitation, and heartburn/acid regurgitation were 13, 8, and 18 d vs 10, 6, and 16 d in the fexuprazan and esomeprazole groups, respectively. There were no statistically significant differences in the proportions of patients without symptoms in the first 7 d (26.2%, 25.2%, and 15.0%, vs 21.6%, 27.9%, and 11.7%, for heartburn, acid regurgitation, and heartburn/acid regurgitation, in the fexuprazan and esomeprazole groups, respectively) and through the 8 wk (20.6%, 21.5%, and 10.3%, vs 17.1%, 27.0%, and 9.9%). Similarly, there were no statistically significant differences in the proportion of symptom-free day/night-time in the first 7 d and through the 8 wk between both groups. (Supplementary Tables 1-4).
In the RDQ and GERD-HRQL, the frequency and severity of heartburn and acid regurgitation improved in both groups, with no significant difference in changes from baseline at weeks 4 and 8 (Tables 2 and 3).
Table 2.
Change in reflux disease questionnaires symptom scores from baseline at weeks 4 and 8 (per protocol set)
|
Fexuprazan 40 mg
|
Esomeprazole 40 mg
|
||||||
|
Baseline (n = 107)
|
Week 4 (n = 103)
|
Week 8 (n = 107)
|
Baseline (n = 111)
|
Week 4 (n = 104)
|
Week 8 (n = 111)
|
||
| Frequency | |||||||
| Heartburn | |||||||
| mean ± SD | 1.92 ± 1.23 | 0.91 ± 1.37 | 0.86 ± 1.33 | 2.12 ± 1.42 | 0.80 ± 1.29 | 0.70 ± 1.28 | |
| Change from baseline (mean ± SD) | - | -0.96 ± 1.50 | -1.06 ± 1.49 | - | -1.33 ± 1.69 | -1.42 ± 1.64 | |
| P value1 | - | < 0.001w | < 0.001w | - | < 0.001w | < 0.001w | |
| LS mean difference from esomeprazole | - | 0.19 | 0.22 | - | - | - | |
| P value2 | - | 0.280 | 0.184 | - | - | - | |
| Reflux | |||||||
| mean ± SD | 2.14 ± 1.29 | 0.93 ± 1.48 | 0.92 ± 1.49 | 1.95 ± 1.29 | 0.61 ± 1.07 | 0.59 ± 1.12 | |
| Change from baseline (mean ± SD) | - | -1.19 ± 1.58 | -1.22 ± 1.53 | - | -1.32 ± 1.44 | -1.36 ± 1.40 | |
| P value1 | - | < 0.001w | < 0.001w | - | < 0.001w | < 0.001w | |
| LS mean difference from esomeprazole | - | 0.28 | 0.28 | - | - | - | |
| P value2 | - | 0.112 | 0.101 | - | - | - | |
| Severity | |||||||
| Heartburn | |||||||
| mean ± SD | 1.81 ± 1.18 | 0.57 ± 0.78 | 0.53 ± 0.77 | 2.10 ± 1.24 | 0.45 ± 0.75 | 0.42 ± 0.79 | |
| Change from baseline (mean ± SD) | - | -1.23 ± 1.26 | -1.28 ± 1.26 | - | -1.63 ± 1.29 | -1.68 ± 1.27 | |
| P value1 | - | < 0.001w | < 0.001w | - | < 0.001w | < 0.001w | |
| LS mean difference from esomeprazole | - | 0.16 | 0.16 | - | - | - | |
| P value2 | - | 0.116 | 0.121 | - | - | - | |
| Reflux | |||||||
| mean ± SD | 2.06 ± 1.22 | 0.61 ± 0.92 | 0.58 ± 0.90 | 1.97 ± 1.21 | 0.40 ± 0.69 | 0.39 ± 0.73 | |
| Change from baseline (mean ± SD) | - | -1.43 ± 1.23 | -1.48 ± 1.20 | - | -1.55 ± 1.23 | -1.58 ± 1.19 | |
| P value1 | - | < 0.001w | < 0.001w | - | < 0.001w | < 0.001w | |
| LS mean difference from esomeprazole | - | 0.20 | 0.18 | - | - | - | |
| P value2 | - | 0.066 | 0.089 | - | - | - | |
Testing for change within-treatment groups [paired t-test (t) or Wilcoxon signed rank test (w)].
Testing for difference between treatment groups (ANCOVA model with treatment group as a factor, baseline score and stratification factor (baseline LA classification) as covariates).
Note: If subjects did not have any RDQ assessment data by week 4, were treated as missing at week 4. RDQ: Reflux disease questionnaires; LS mean: Least square mean.
Table 3.
Change in gastroesophageal reflux disease-health related quality of life score from baseline at weeks 4 and 8 (per protocol set)
| GERD-HRQL |
Fexuprazan 40 mg
|
Esomeprazole 40 mg
|
||||
|
Baseline (n = 107)
|
Week 4 (n = 102)
|
Week 8 (n = 106)
|
Baseline (n = 111)
|
Week 4 (n = 104)
|
Week 8 (n = 111)
|
|
| mean ± SD | 11.88 ± 8.11 | 4.21 ± 6.17 | 4.01 ± 6.20 | 12.98 ± 9.62 | 3.42 ± 5.04 | 3.32 ± 5.54 |
| Change from baseline (mean ± SD) | - | -7.71 ± 8.37 | -7.90 ± 8.56 | - | -9.84 ± 8.70 | -9.67 ± 8.56 |
| P value1 | - | < 0.001w | < 0.001t | - | < 0.001w | < 0.001w |
| LS mean difference from esomeprazole | - | 1.06 | 1.05 | - | - | - |
| P value2 | - | 0.137 | 0.151 | - | - | - |
Testing for change within-treatment groups [paired t-test (t) or Wilcoxon signed rank test (w)].
Testing for difference between treatment groups (ANCOVA model with treatment group as a factor, baseline score and stratification factor (baseline LA classification) as covariates).
Note: If subjects did not have any Gastroesophageal reflux disease-health related quality of life (GERD-HRQL) assessment data by week 4, were treated as missing at week 4. One subject in fexuprazan 40 mg did not have GERD-HRQL assessment data post baseline. GERD-HRQL: Gastroesophageal reflux disease-health related quality of life; LS mean: Least square mean.
In the results of subgroup analyses, fexuprazan demonstrated better heartburn relief in patients with moderate-to-severe symptoms who had experienced heartburn for 2 or more days in the week before treatment: the proportions of those without heartburn on the first day 3 were significantly greater in the fexuprazan group than in the esomeprazole group (22.4% vs 7.9%, P = 0.026 at the day/night-time; 29.3% vs 12.7%, P = 0.037 at the day-time; 34.5% vs 17.5%, P = 0.035 at the night-time) (Supp-lementary Table 5). The extraesophageal symptom of chronic cough improved better with fexuprazan: the least squares (LS) means of days without chronic cough were significantly greater in the fexuprazan group than in the esomeprazole group on the days 3, 7, and week 8 (P = 0.006, P = 0.003, and P = 0.002, respectively). The extraesophageal symptom of throat irritation improved in both groups on days 3, 7, and week 8 without significant differences between the treatment groups (Supplementary Table 6).
Safety
Safety analyses were performed for 262 patients who received at least one dose of the study meditation. The overall incidences of TEAEs and ADRs were not significantly different between the treatment groups; TEAEs were reported by 22 patients (16.8%) and 25 (19.1%), and ADRs were reported by 9 patients (6.9%) and 7 patients (5.3%) in the fexuprazan and esomeprazole groups, respectively (Table 4). The severity of TEARs was mostly mild (61 events), with six moderate events (diarrhea, nausea, dysgeusia, pruritus, pain, and cystitis) and only one severe event (influenza). All ADRs were either mild (21 events) or moderate (3 events). There were 2 patients (1.5%) with ADRs (diarrhea and pruritus) leading to discontinuation of the study medication in the fexuprazan group, not esomeprazole group. However, there was no statistically significant difference in the incidence of ADRs leading to discontinuation between both groups. No serious TEARs or ADRs were reported in either group of patients (Supplementary Table 7). The most frequently occurring (≥ 2%) TEAEs were shown in Table 4.
Table 4.
Overall Summary of treatment-emergent adverse events (safety set)
|
Fexuprazan 40 mg (n = 131)
|
Esomeprazole 40 mg (n = 131)
|
Total (n = 262)
|
|
|
n
(%) [number of event]
| |||
| Subjects with TEAEs | 22 (16.8) [34] | 25 (19.1) [34] | 47 (17.9) [68] |
| 95%CI | [10.4, 23.2] | [12.4, 25.8] | [13.3, 22.6] |
| P value1 | 0.629c | ||
| Subjects with ADRs | 9 (6.9) [13] | 7 (5.3) [11] | 16 (6.1) [24] |
| 95%CI | [2.5, 11.2] | [1.5, 9.2] | [3.2, 9.0] |
| P value1 | 0.606c | ||
| Subjects with serious TEAEs | 0 | 0 | 0 |
| Subjects with serious ADRs | 0 | 0 | 0 |
| Most frequently occurring (≥ 2%) TEAEs by system organ class and preferred term | |||
| System organ class preferred term | |||
| Gastrointestinal disorders | |||
| Diarrhoea | 4 (3.1) [4] | 2 (1.5) [2] | 6 (2.3) [6] |
| Nervous system disorders | |||
| Dizziness | 1 (0.8) [1] | 3 (2.3) [3] | 4 (1.5) [4] |
Testing for difference among treatment groups [Chi-square test (c)].
Note: Denominator of percentage is the number of subjects in each treatment group. TEAEs: Treatment-emergent adverse events; ADRs: Adverse drug reactions.
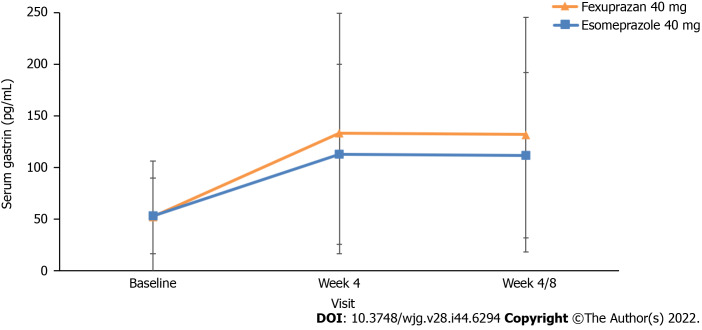
The serum gastrin levels intended to increase, and their differences between the treatment groups were not significant at weeks 4 and 8 (Figure 4). There were no clinically significant changes in the laboratory test, vital signs, physical examination and ECG findings, and no liver enzyme elevations were reported.
Figure 4.
Changes from baseline in serum gastrin levels at weeks 4 and 8 (per-protocol set).
DISCUSSION
This study demonstrated the non-inferior efficacy and safety of fexuprazan 40 mg once daily to esomeprazole 40 mg once daily in the healing of EE at week 8 in patients with EE. The rates of healing EE were not different between the two groups at week 4. No differences between the groups were found in the secondary endpoints regarding symptom responses, including the first day of the complete resolution of symptoms (heartburn and acid regurgitation) and the proportions of patients without symptoms along with the proportions of symptom-free days in the first 7 d and throughout 8 wk of the treatment period. Furthermore, the two groups did not differ in the changes in RDQ and in GERD-HRQL from baseline at weeks 4 and 8. Serum gastrin levels and safety-related TEAEs and ADRs did not differ.
Our results were consistent with those of other P-CABs (tegoprazan and vonoprazan) in comparison with PPIs. Studies in patients with GERD and healthy volunteers have revealed the efficacy and safety of tegoprazan and vonoprazan, to be similar to those of PPIs. In a phase I study of tegoprazan, which has been used since 2018 after approval in South Korea, it safely inhibited acid secretion compared to esomeprazole[24]. In a multicenter, randomized, double-blind, and parallel-group non-inferiority study on 302 patients with endoscopically confirmed EE[19], tegoprazan 50 mg and 100 mg indicated cumulative healing rates of 98.9% and 98.9% at week 8, respectively, compared to the 98.9% healing rate of esomeprazole 40 mg. Regarding vonoprazan, its efficacy has been identified in clinical and pharmacological factors, including healing EE, symptom responses, maintenance treatment effect after healing EE, efficacy in refractory GERD, the effect of intermittent therapy, and the pH 4 holding time ratio[25-28]. A study of short-term symptom response at week 4 was similar: 88.0% and 81.8% in the esomeprazole 20 mg and vonoprazan 20 mg groups, respectively[29]. In a dose-ranging study, vonoprazan 5, 10, 20, and 40 mg exhibited non-inferior efficacy to lansoprazole 30 mg in the healing rates of EE at week 8[30]. In those with severe grades of EE and extensive metabolizers, treatments with vonoprazan 20 mg and lansoprazole 30 mg for 8 wk did not differ in the rates of EE healing[23]. Additionally, the recurrence rates of EE were significantly lower after a 24-wk treatment using 10 mg and 20 mg vonoprazan than with lansoprazole 15 mg[31]. Regarding the effect of vonoprazan on gastric acidity, the pH 4 holding time ratio significantly increased from 73.21% to 96.46% and from 69.97% to 100.00% in the 20 mg and 40 mg groups, respectively[26].
In this study, fexuprazan led to rapid treatment response in patients with moderate-to-severe heartburn. The proportion of patients without heartburn on day 3 who had moderate-to-severe symptoms was significantly higher with fexuprazan than with esomeprazole, in both day-time and night-time, and also at night-time only. Nocturnal heartburn was reportedly presented in approximately 80% of patients with frequent heartburn and impaired sleep quality and daytime HRQL[6,32]. Moreover, the continuous use of PPIs was not effective for nocturnal heartburn in 30% of patients with reflux esophagitis[33], and in over 50% of patients with symptomatic EE[34]. Thus, this study suggests that fexuprazan may provide rapid symptom resolution in patients with nocturnal heartburn and refractory response to PPI treatment. The rapid response of symptoms to P-CABs was identified in another study revealing that vonoprazan 20 mg relieved heartburn symptoms on day 1 in more patients than lansoprazole 30 mg[35]. Although the present study did not demonstrate faster healing of EE, there have been studies showing rapid healing of EE after 2-week treatment of vonoprazan than PPIs[23,36]. Accordingly, in conjunction of this faster healing in EE with our finding of rapid symptom response by fexuprazan, it is cautiously suggested that patients with EE may need a relatively short-term treatment period by fexuprazan than PPIs. Further studies on shorter treatment in EE by fexuprazan are needed.
The pharmacodynamic and pharmacokinetic profiles of fexuprazan explain the rapid onset and sustained inhibition of acid secretion in GERD. Studies of fexuprazan in healthy individuals revealed that the mean percentage of time of gastric pH > 4 was achieved in 80% of 24 h and even at night. However, esomeprazole achieved a lower mean percentage time of gastric pH > 4, which was also lower at night[14]. With regard to the pharmacokinetic parameters, Cmax was reached within 1-4 h after dosing, and the mean elimination half-life was approximately 9 h. Fexuprazan also exhibited dose-response relationships. Plasma concentrations increased proportionately with the doses ranging from 10-320 mg, whereas multiple doses did not cause significant accumulation. The elimination pathway of fexuprazan was not a renal route but probably via the liver or gut. Furthermore, in contrast to PPIs, food intake was not necessary for optimal action, as the parameters of gastric pH and plasma concentrations of fexuprazan did not change with a high-fat diet. Adverse drug effects on the liver were not higher with fexuprazan than with placebo, in contrast to the 0.2% potential liver toxicity in the pre-clinical experiment of vonoprazan[37]. Moreover, the gastrin-increasing effect of fexuprazan was similar to that of other PPIs, and was less frequent than that of vonoprazan[38]. Furthermore, the effects on gastric acid suppression, serum gastrin elevation, and dose response relationship were also consistent in different populations including Korean, Caucasian, and Japanese ethnicities[39].
In our study, fexuprazan improved one of the extraesophageal symptoms of GERD better than esomeprazole. Despite its unknown pathophysiology, patients with GERD-related chronic cough have been treated with PPIs with unsatisfactory symptom control. The superior efficacy of PPIs over placebo has not been confirmed in patients with GERD-related chronic cough in recent randomized controlled trials (RCTs)[40,41]. In addition, a meta-analysis of 5 RCTs did not suggest any evidence in favor of PPI therapy[42]. Taken the effect of fexuprazan in this study with the overall inadequate efficacy of PPIs in chronic cough, we suggest that fexuprazan could provide a better solution than PPIs for GERD-related chronic cough.
This study revealed elevated serum gastrin levels, but these were not significantly different between both groups. Previous reports have revealed higher serum gastrin levels in the P-CAB group than in the PPI group[37,43]. In the study of 212 outpatients, the serum gastrin in the P-CAB group had 2-3 fold and 1-2 fold increases than the normal and PPI groups, respectively[43]. However, increased serum gastrin levels were limited, particularly in patients with normal mucosa or mild atrophic gastritis. Additional limitations were the treatment periods of less than one year and the sampling time at pre-meal rather than at the peak level of 30 min after meals.
This study had some limitations. First, the number of patients classified as LA grade C/D was small. Actually, those with LA grades C/D accounted for only 6.2% of the fexuprazan and 7.0% of the esomeprazole groups. Therefore, it was difficult to confirm the advantage of fexuprazan, better clinical performances due to unique pharmacokinetics and pharmacodynamics of fexuprazan in severe EE than PPIs, as in other P-CAB studies[30]. Future fexuprazan studies need to be focused on significantly larger number of patients with severe EE (LA grades C/D). Second, the treatment period was only eight weeks, and studies on the long-term safety or recurrence rates after EE healing are required in the future, considering the insufficient data regarding the long-term safety of P-CABs. Third, when evaluating symptom severity, the possible effects of comorbidities such as chronic obstructive pulmonary disease were not considered[44].
CONCLUSION
We concluded that fexuprazan 40 mg once daily has non-inferior efficacy and safety to esomeprazole 40 mg once daily in healing EE at weeks 4 and 8. From the symptom evaluation through the symptom diary, RDQ and GERD-HRQL, it was confirmed that fexuprazan improved symptoms of heartburn and acid regurgitation and quality of life similarly to esomeprazole. The increase in serum gastrin levels by fexuprazan was not different from that of esomeprazole. Future research on fexuprazan is needed to evaluate the long-term efficacy and safety of fexuprazan in GERD including EE, PPI-refractory GERD, and other acid-related diseases along with the long-term maintenance therapy including on demand or intermittent treatment.
ARTICLE HIGHLIGHTS
Research background
Currently, a mainstay therapy of erosive esophagitis (EE) is proton pump inhibitors (PPIs), which have disadvantages like their delayed absorption and variable efficacy due to differences in drug metabolism A novel potassium-competitive acid blocker, fexuprazan, suppresses the K+/H+-ATPase enzyme reversibly and competetively in proton pumps within gastric parietal cells.
Research motivation
A previous study of fexuprazan on healthy individuals demonstrated the effect of its acid suppression and tolerability, by showing that gastric pH > 4 was reached within 2 h and maintained for 24 h in a dose-dependent manner. However, the efficacy and safety of fexuprazan in EE have not been compared to esomeprazole, one of the most widely used PPIs in gastro-esophageal reflux disease (GERD) including EE.
Research objectives
The aim of this phase III, double-blind, randomized, active-controlled, multi-center study was to compare the efficacy and safety between fexuprazan and esomeprazole in patients with EE.
Research methods
Adult patients who have EE confirmed by endoscopy were randomized 1:1 to receive fexuprazan 40 mg or esomeprazole 40 mg once daily for eight weeks in South Korea between December 2018 and August 2019. The primary endpoint was healing rates confirmed by endoscopy at week 8. The secondary endpoints included the proportion of patients with healed EE at week 4, symptom response, and GERD-related quality of life assessed from the evaluation through the symptom diary, reflux disease questionnaire (RDQ) and GERD-health related quality life (GERD-HRQL) questionnares. We also compared safety profiles and serum gastrin levels between the groups.
Research results
This study shows that fexuprazan 40 mg once daily is non-inferior to esomeprazole 40 mg once daily in healing rates of at weeks 4 and 8 and in symptom improvement of heartburn and acid regurgitation and RDQ and GERD-HRQL. In 218 participants who completed the study per protocol (fexuprazan 40 mg, n = 107; esomeprazole 40 mg, n = 111), fexuprazan was non-inferior to esomeprazole regarding the healing rate at week 8 [99.1% (106/107) vs 99.1% (110/111)], and at week 4 [90.3% (93/103) vs 88.5% (92/104)], symptom responses, and quality of life assessments. Also, serum gastrin levels at weeks 4 and 8 and drug-related side effects were not significantly different between the groups.
Research conclusions
This study results indicate that fexuprazan 40 mg once daily can be an alternative of esomeprazole 40 mg once daily for patients with erosive esophagitis in terms of efficacy and safety.
Research perspectives
Further research on fexuprazan should be directed to evaluate the long-term efficacy and safety of fexuprazan in various acid-related gastrointestinal diseases including NERD, PPI-refractory GERD, H. pylori infection, peptic ulcer diseases, and so on.
Footnotes
Institutional review board statement: This study was approved by the institutional review boards (IRBs) of each institution, conducted in compliance with the relevant ethics guidelines. All the study medications and procedures performed were in accordance with the 1964 Declaration of Helsinki and its later amendments, or comparable ethical standards.
Clinical trial registration statement: This study is registered at ClinicalTrials.gov. The registration identification number is NCT03736369.
Informed consent statement: All study participants provided informed written consent prior to study enrollment.
Conflict-of-interest statement: The corresponding author, Lee OY, had been a member of outside directors at the Daewoong Pharmaceutical Co., Ltd, form the period March 24 2018 to Nov 2 2021. All other authors declare no conflict of interests regarding this study.
CONSORT 2010 statement: The authors have read the CONSORT 2010 Checklist, and the manuscript was prepared and revised according to the CONSORT 2010 Checklist.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Korean Society of Gastointestinal Endoscopy; Korean Society of Neurogastroenterology and Motility; The Korean Society of Gastroenterology; and Korean Association of Internal Medicine.
Peer-review started: September 4, 2022
First decision: October 4, 2022
Article in press: November 9, 2022
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Feizi A, Iran; Vakhshoori M, Iran S-Editor: Gong ZM L-Editor: A P-Editor: Gong ZM
Contributor Information
Kang Nyeong Lee, Department of Internal Medicine, Hanyang University College of Medicine, Seoul 04763, South Korea.
Oh Young Lee, Department of Internal Medicine, Hanyang University College of Medicine, Seoul 04763, South Korea. leeoy@hanyang.ac.kr.
Hoon Jai Chun, Department of Internal Medicine, Korea University Anam Hospital, Seoul 02841, South Korea.
Jin Il Kim, Department of Internal Medicine, The Catholic University of Korea, Yeouido ST. Mary’s Hospital, Seoul 07260, South Korea.
Sung Kook Kim, Department of Internal Medicine, Kyungpook National University Hospital, Daegu 41944, South Korea.
Sang Woo Lee, Department of Internal Medicine, Korea University Ansan Hospital, Ansan-si 15355, South Korea.
Kyung Sik Park, Department of Internal Medicine, Keimyung University Dongsan Hospital, Daegu 42601, South Korea.
Kook Lae Lee, Department of Internal Medicine, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul 07061, South Korea.
Suck Chei Choi, Department of Internal Medicine, Wonkwang University Hospital, Iksan 54538, South Korea.
Jae-Young Jang, Department of Internal Medicine, KyungHee University Medical Center, Seoul 02447, South Korea.
Gwang Ha Kim, Department of Internal Medicine, Pusan National University School of Medicine and Biomedical Research Institute, Pusan National University Hospital, Busan 47241, South Korea.
In-kyung Sung, Department of Internal Medicine, KKonkuk University Medical Center, Seoul 05030, South Korea.
Moo In Park, Department of Internal Medicine, Kosin University Gaspel Hospital, Busan 49267, South Korea.
Joong Goo Kwon, Department of Internal Medicine, Daegu Catholic University Medical Center, Daegu 42471, South Korea.
Nayoung Kim, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam-si 13620, Gyeonggi-do, South Korea.
Jae Jun Kim, Department of Internal Medicine, Samsung Medical Center, Seoul 06351, South Korea.
Soo Teik Lee, Department of Internal Medicine, Chonbuk National University Hospital, Jeonju-si 54907, South Korea.
Hyun Soo Kim, Department of Internal Medicine, Chonnam National University Hospital, Gwangju 61469, South Korea.
Ki Bae Kim, Department of Internal medicine, Chungbuk National University School of Medicine, Cheong Ju 28644, South Korea.
Yong Chan Lee, Department of Internal Medicine, Severance Hospital, Seoul 03722, South Korea.
Myung-Gyu Choi, Department of Internal Medicine, The Catholic University of Korea, Seoul ST. Mary’s Hospital, Seoul 06591, South Korea.
Joon Seong Lee, Digestive Disease Center, Soonchunhyang University College of Medicine, Seoul 04401, South Korea.
Hwoon-Yong Jung, Department of Internal Medicine, Asan Medical Center, Seoul 05505, South Korea.
Kwang Jae Lee, Department of Gastroenterology, Ajou University School of Medicine, Suwon 16499, South Korea.
Jie-Hyun Kim, Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul 06273, South Korea.
Hyunsoo Chung, Department of Internal Medicine, Seoul National University Hospital, Seoul 03080, South Korea.
Data sharing statement
Data are available upon reasonable request.
References
- 1.Katz PO, Gerson LB, Vela MF. Guidelines for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2013;108:308–328; quiz 329. doi: 10.1038/ajg.2012.444. [DOI] [PubMed] [Google Scholar]
- 2.GBD 2017 Gastro-oesophageal Reflux Disease Collaborators. The global, regional, and national burden of gastro-oesophageal reflux disease in 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol Hepatol. 2020;5:561–581. doi: 10.1016/S2468-1253(19)30408-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eusebi LH, Ratnakumaran R, Yuan Y, Solaymani-Dodaran M, Bazzoli F, Ford AC. Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018;67:430–440. doi: 10.1136/gutjnl-2016-313589. [DOI] [PubMed] [Google Scholar]
- 4.Fass R. Erosive esophagitis and nonerosive reflux disease (NERD): comparison of epidemiologic, physiologic, and therapeutic characteristics. J Clin Gastroenterol. 2007;41:131–137. doi: 10.1097/01.mcg.0000225631.07039.6d. [DOI] [PubMed] [Google Scholar]
- 5.Ha NR, Lee HL, Lee OY, Yoon BC, Choi HS, Hahm JS, Ahn YH, Koh DH. Differences in clinical characteristics between patients with non-erosive reflux disease and erosive esophagitis in Korea. J Korean Med Sci. 2010;25:1318–1322. doi: 10.3346/jkms.2010.25.9.1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shaker R, Castell DO, Schoenfeld PS, Spechler SJ. Nighttime heartburn is an under-appreciated clinical problem that impacts sleep and daytime function: the results of a Gallup survey conducted on behalf of the American Gastroenterological Association. Am J Gastroenterol. 2003;98:1487–1493. doi: 10.1111/j.1572-0241.2003.07531.x. [DOI] [PubMed] [Google Scholar]
- 7.Wahlqvist P, Karlsson M, Johnson D, Carlsson J, Bolge SC, Wallander MA. Relationship between symptom load of gastro-oesophageal reflux disease and health-related quality of life, work productivity, resource utilization and concomitant diseases: survey of a US cohort. Aliment Pharmacol Ther. 2008;27:960–970. doi: 10.1111/j.1365-2036.2008.03671.x. [DOI] [PubMed] [Google Scholar]
- 8.Irvine EJ. Quality of life assessment in gastro-oesophageal reflux disease. Gut. 2004;53 Suppl 4:iv35–iv39. doi: 10.1136/gut.2003.034314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sandhu DS, Fass R. Current Trends in the Management of Gastroesophageal Reflux Disease. Gut Liver. 2018;12:7–16. doi: 10.5009/gnl16615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sachs G, Shin JM, Howden CW. Review article: the clinical pharmacology of proton pump inhibitors. Aliment Pharmacol Ther. 2006;23 Suppl 2:2–8. doi: 10.1111/j.1365-2036.2006.02943.x. [DOI] [PubMed] [Google Scholar]
- 11.Castell DO, Richter JE, Robinson M, Sontag SJ, Haber MM. Efficacy and safety of lansoprazole in the treatment of erosive reflux esophagitis. The Lansoprazole Group. Am J Gastroenterol. 1996;91:1749–1757. [PubMed] [Google Scholar]
- 12.Richter JE, Bochenek W. Oral pantoprazole for erosive esophagitis: a placebo-controlled, randomized clinical trial. Pantoprazole US GERD Study Group. Am J Gastroenterol. 2000;95:3071–3080. doi: 10.1111/j.1572-0241.2000.03254.x. [DOI] [PubMed] [Google Scholar]
- 13.Dickman R, Maradey-Romero C, Gingold-Belfer R, Fass R. Unmet Needs in the Treatment of Gastroesophageal Reflux Disease. J Neurogastroenterol Motil. 2015;21:309–319. doi: 10.5056/jnm15105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sunwoo J, Oh J, Moon SJ, Ji SC, Lee SH, Yu KS, Kim HS, Lee A, Jang IJ. Safety, tolerability, pharmacodynamics and pharmacokinetics of DWP14012, a novel potassium-competitive acid blocker, in healthy male subjects. Aliment Pharmacol Ther. 2018;48:206–218. doi: 10.1111/apt.14818. [DOI] [PubMed] [Google Scholar]
- 15.Shaw M, Dent J, Beebe T, Junghard O, Wiklund I, Lind T, Johnsson F. The Reflux Disease Questionnaire: a measure for assessment of treatment response in clinical trials. Health Qual Life Outcomes. 2008;6:31. doi: 10.1186/1477-7525-6-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shaw MJ, Talley NJ, Beebe TJ, Rockwood T, Carlsson R, Adlis S, Fendrick AM, Jones R, Dent J, Bytzer P. Initial validation of a diagnostic questionnaire for gastroesophageal reflux disease. Am J Gastroenterol. 2001;96:52–57. doi: 10.1111/j.1572-0241.2001.03451.x. [DOI] [PubMed] [Google Scholar]
- 17.Velanovich V, Vallance SR, Gusz JR, Tapia FV, Harkabus MA. Quality of life scale for gastroesophageal reflux disease. J Am Coll Surg. 1996;183:217–224. [PubMed] [Google Scholar]
- 18.Velanovich V. The development of the GERD-HRQL symptom severity instrument. Dis Esophagus. 2007;20:130–134. doi: 10.1111/j.1442-2050.2007.00658.x. [DOI] [PubMed] [Google Scholar]
- 19.Lee KJ, Son BK, Kim GH, Jung HK, Jung HY, Chung IK, Sung IK, Kim JI, Kim JH, Lee JS, Kwon JG, Park JH, Huh KC, Park KS, Park MI, Kim N, Lee OY, Jee SR, Lee SK, Youn SJ, Kim SK, Lee ST, Hong SJ, Choi SC, Kim TN, Youn YH, Park HJ, Kang MJ, Park CH, Kim BT, Youn S, Song GS, Rhee PL. Randomised phase 3 trial: tegoprazan, a novel potassium-competitive acid blocker, vs. esomeprazole in patients with erosive oesophagitis. Aliment Pharmacol Ther. 2019;49:864–872. doi: 10.1111/apt.15185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jeon HK, Kim GH, Lee MW, Joo DC, Lee BE. Randomized Controlled Trial Comparing the Efficacy of Sustained-Release Formula of Mosapride-Plus-Esomeprazole Combination Therapy to Esomeprazole Monotherapy in Patients with Gastroesophageal Reflux Disease. J Clin Med. 2022;11 doi: 10.3390/jcm11071965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Richter JE, Kahrilas PJ, Johanson J, Maton P, Breiter JR, Hwang C, Marino V, Hamelin B, Levine JG Esomeprazole Study Investigators. Efficacy and safety of esomeprazole compared with omeprazole in GERD patients with erosive esophagitis: a randomized controlled trial. Am J Gastroenterol. 2001;96:656–665. doi: 10.1111/j.1572-0241.2001.3600_b.x. [DOI] [PubMed] [Google Scholar]
- 22.Labenz J, Armstrong D, Lauritsen K, Katelaris P, Schmidt S, Schütze K, Wallner G, Juergens H, Preiksaitis H, Keeling N, Nauclér E, Eklund S Expo Study Investigators. A randomized comparative study of esomeprazole 40 mg vs pantoprazole 40 mg for healing erosive oesophagitis: the EXPO study. Aliment Pharmacol Ther. 2005;21:739–746. doi: 10.1111/j.1365-2036.2005.02368.x. [DOI] [PubMed] [Google Scholar]
- 23.Ashida K, Sakurai Y, Hori T, Kudou K, Nishimura A, Hiramatsu N, Umegaki E, Iwakiri K. Randomised clinical trial: vonoprazan, a novel potassium-competitive acid blocker, vs. lansoprazole for the healing of erosive oesophagitis. Aliment Pharmacol Ther. 2016;43:240–251. doi: 10.1111/apt.13461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Han S, Choi HY, Kim YH, Nam JY, Kim B, Song GS, Lim HS, Bae KS. Randomised clinical trial: safety, tolerability, pharmacokinetics, and pharmacodynamics of single and multiple oral doses of tegoprazan (CJ-12420), a novel potassium-competitive acid blocker, in healthy male subjects. Aliment Pharmacol Ther. 2019;50:751–759. doi: 10.1111/apt.15438. [DOI] [PubMed] [Google Scholar]
- 25.Hoshino S, Kawami N, Takenouchi N, Umezawa M, Hanada Y, Hoshikawa Y, Kawagoe T, Sano H, Hoshihara Y, Nomura T, Iwakiri K. Efficacy of Vonoprazan for Proton Pump Inhibitor-Resistant Reflux Esophagitis. Digestion. 2017;95:156–161. doi: 10.1159/000456072. [DOI] [PubMed] [Google Scholar]
- 26.Iwakiri K, Sakurai Y, Shiino M, Okamoto H, Kudou K, Nishimura A, Hiramatsu N, Umegaki E, Ashida K. A randomized, double-blind study to evaluate the acid-inhibitory effect of vonoprazan (20 mg and 40 mg) in patients with proton-pump inhibitor-resistant erosive esophagitis. Therap Adv Gastroenterol. 2017;10:439–451. doi: 10.1177/1756283X17705329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kato M, Ito N, Demura M, Kubo K, Mabe K, Harada N. Study for every other day administration of vonoprazan in maintenance treatment of erosive GERD: study protocol for a multicentre randomised cross-over study. BMJ Open Gastroenterol. 2018;5:e000197. doi: 10.1136/bmjgast-2017-000197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Umezawa M, Kawami N, Hoshino S, Hoshikawa Y, Koizumi E, Takenouchi N, Hanada Y, Kaise M, Iwakiri K. Efficacy of On-Demand Therapy Using 20-mg Vonoprazan for Mild Reflux Esophagitis. Digestion. 2018;97:309–315. doi: 10.1159/000485795. [DOI] [PubMed] [Google Scholar]
- 29.Sakurai K, Suda H, Fujie S, Takeichi T, Okuda A, Murao T, Hasuda K, Hirano M, Ito K, Tsuruta K, Hattori M. Short-Term Symptomatic Relief in Gastroesophageal Reflux Disease: A Comparative Study of Esomeprazole and Vonoprazan. Dig Dis Sci. 2019;64:815–822. doi: 10.1007/s10620-018-5365-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ashida K, Sakurai Y, Nishimura A, Kudou K, Hiramatsu N, Umegaki E, Iwakiri K, Chiba T. Randomised clinical trial: a dose-ranging study of vonoprazan, a novel potassium-competitive acid blocker, vs. lansoprazole for the treatment of erosive oesophagitis. Aliment Pharmacol Ther. 2015;42:685–695. doi: 10.1111/apt.13331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ashida K, Iwakiri K, Hiramatsu N, Sakurai Y, Hori T, Kudou K, Nishimura A, Umegaki E. Maintenance for healed erosive esophagitis: Phase III comparison of vonoprazan with lansoprazole. World J Gastroenterol. 2018;24:1550–1561. doi: 10.3748/wjg.v24.i14.1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Farup C, Kleinman L, Sloan S, Ganoczy D, Chee E, Lee C, Revicki D. The impact of nocturnal symptoms associated with gastroesophageal reflux disease on health-related quality of life. Arch Intern Med. 2001;161:45–52. doi: 10.1001/archinte.161.1.45. [DOI] [PubMed] [Google Scholar]
- 33.Kinoshita Y, Hongo M Japan TWICE Study Group. Efficacy of twice-daily rabeprazole for reflux esophagitis patients refractory to standard once-daily administration of PPI: the Japan-based TWICE study. Am J Gastroenterol. 2012;107:522–530. doi: 10.1038/ajg.2012.19. [DOI] [PubMed] [Google Scholar]
- 34.Chey WD, Mody RR, Izat E. Patient and physician satisfaction with proton pump inhibitors (PPIs): are there opportunities for improvement? Dig Dis Sci. 2010;55:3415–3422. doi: 10.1007/s10620-010-1209-2. [DOI] [PubMed] [Google Scholar]
- 35.Oshima T, Arai E, Taki M, Kondo T, Tomita T, Fukui H, Watari J, Miwa H. Randomised clinical trial: vonoprazan versus lansoprazole for the initial relief of heartburn in patients with erosive oesophagitis. Aliment Pharmacol Ther. 2019;49:140–146. doi: 10.1111/apt.15062. [DOI] [PubMed] [Google Scholar]
- 36.Xiao Y, Zhang S, Dai N, Fei G, Goh KL, Chun HJ, Sheu BS, Chong CF, Funao N, Zhou W, Chen M. Phase III, randomised, double-blind, multicentre study to evaluate the efficacy and safety of vonoprazan compared with lansoprazole in Asian patients with erosive oesophagitis. Gut. 2020;69:224–230. doi: 10.1136/gutjnl-2019-318365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Echizen H. The First-in-Class Potassium-Competitive Acid Blocker, Vonoprazan Fumarate: Pharmacokinetic and Pharmacodynamic Considerations. Clin Pharmacokinet. 2016;55:409–418. doi: 10.1007/s40262-015-0326-7. [DOI] [PubMed] [Google Scholar]
- 38.Jenkins H, Sakurai Y, Nishimura A, Okamoto H, Hibberd M, Jenkins R, Yoneyama T, Ashida K, Ogama Y, Warrington S. Randomised clinical trial: safety, tolerability, pharmacokinetics and pharmacodynamics of repeated doses of TAK-438 (vonoprazan), a novel potassium-competitive acid blocker, in healthy male subjects. Aliment Pharmacol Ther. 2015;41:636–648. doi: 10.1111/apt.13121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hwang JG, Jeon I, Park SA, Lee A, Yu KS, Jang IJ, Lee S. Pharmacodynamics and pharmacokinetics of DWP14012 (fexuprazan) in healthy subjects with different ethnicities. Aliment Pharmacol Ther. 2020;52:1648–1657. doi: 10.1111/apt.16131. [DOI] [PubMed] [Google Scholar]
- 40.Faruqi S, Molyneux ID, Fathi H, Wright C, Thompson R, Morice AH. Chronic cough and esomeprazole: a double-blind placebo-controlled parallel study. Respirology. 2011;16:1150–1156. doi: 10.1111/j.1440-1843.2011.02014.x. [DOI] [PubMed] [Google Scholar]
- 41.Shaheen NJ, Crockett SD, Bright SD, Madanick RD, Buckmire R, Couch M, Dellon ES, Galanko JA, Sharpless G, Morgan DR, Spacek MB, Heidt-Davis P, Henke D. Randomised clinical trial: high-dose acid suppression for chronic cough - a double-blind, placebo-controlled study. Aliment Pharmacol Ther. 2011;33:225–234. doi: 10.1111/j.1365-2036.2010.04511.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chang AB, Lasserson TJ, Gaffney J, Connor FL, Garske LA. Gastro-oesophageal reflux treatment for prolonged non-specific cough in children and adults. Cochrane Database Syst Rev. 2005:CD004823. doi: 10.1002/14651858.CD004823.pub2. [DOI] [PubMed] [Google Scholar]
- 43.Kojima Y, Takeuchi T, Sanomura M, Higashino K, Kojima K, Fukumoto K, Takata K, Sakamoto H, Sakaguchi M, Tominaga K, Higuchi K. Does the Novel Potassium-Competitive Acid Blocker Vonoprazan Cause More Hypergastrinemia than Conventional Proton Pump Inhibitors? Digestion. 2018;97:70–75. doi: 10.1159/000484217. [DOI] [PubMed] [Google Scholar]
- 44.Lee AL, Goldstein RS. Gastroesophageal reflux disease in COPD: links and risks. Int J Chron Obstruct Pulmon Dis. 2015;10:1935–1949. doi: 10.2147/COPD.S77562. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request.