Abstract
Background
Taxillus chinensis (DC.) Danser (T. chinensis), known as “Sangjisheng” in Chinese, is a member of the family Loranthaceae, with the traditional functions of “dispelling wind dampness, strengthening bones and muscles, and preventing miscarriage”. Since Eastern Han dynasty, it has been used for the treatment of rheumatoid arthritis, arthralgia, threatened abortion, and hypertension. Nowadays, T. chinensis is included in the 2020 Edition of the Chinese Pharmacopoeia as Taxilli Herba. The purpose of this review is to summarize the latest research on T. chinensis in recent years, and make critical comments, so as to provide reference for the clinical application and modern research of T. chinensis.
Main body
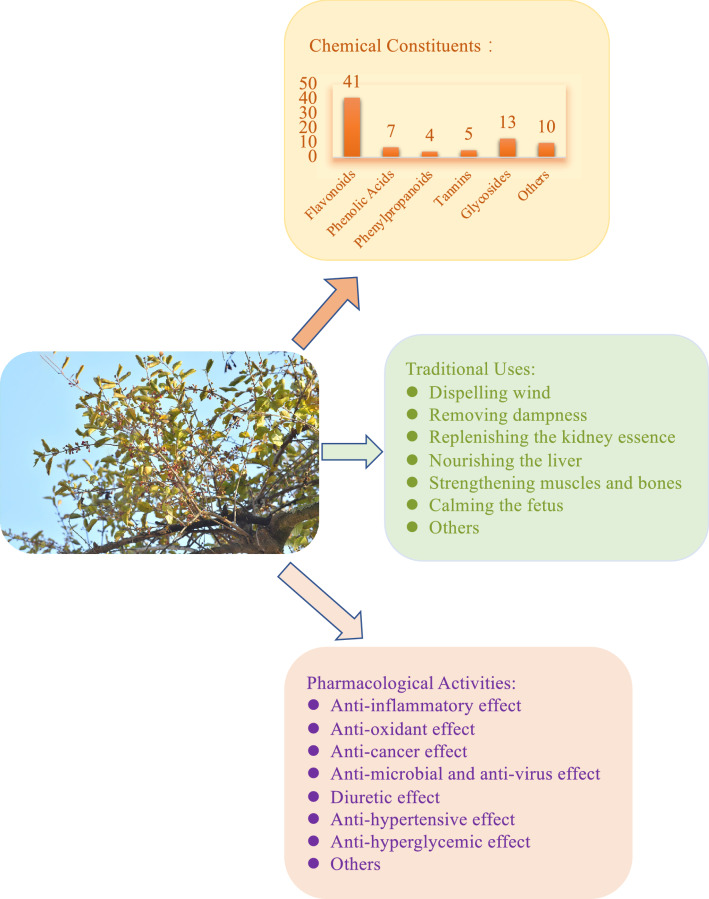
In this review, we summarize the botany, traditional uses, and research advances in the phytochemistry and pharmacological effects of T. chinensis. Its toxicity has also been discussed. The published literature on current pharmacological and toxicological data has also been assessed. To date, approximately 110 compounds, including flavonoids, phenolic acids, phenylpropanoids, tannins, glycosides, amino acids, and nucleosides, have been identified in T. chinensis. Flavonoids are considered the most vital bioactive ingredients in T. chinensis. Pharmacological studies have demonstrated that T. chinensis possesses anti-inflammatory, antioxidant, anticancer, antimicrobial, antiviral, diuretic, antihypertensive, antihyperglycemic, and other properties.
Conclusion
Currently, research on T. chinensis is in the preliminary stages, and further research is required to understand the active compounds present and mechanisms of action. We hope that this comprehensive review of T. chinensis will serve as a background for further research.
Keywords: Taxillus chinensis (DC.) Danser, Botany, Traditional uses, Phytochemistry, Pharmacology, Toxicology
Background
T. chinensis is predominantly found in East Asia, mainly in China, and belongs to the Loranthaceae species. T. chinensis is commonly found in some alpine and arid desert areas, mainly in southern and southwestern China, such as Guangxi, Fujian, Taiwan, Yunnan, Guangdong, and Hong Kong [1, 2]. In addition, it is distributed in some Southeast Asian nations, such as Malaya, Vietnam, Thailand, Laos, Cambodia, Borneo, and the Philippines (Fig. 1) [3]. T. chinensis is a hemi-parasitic plant that is more likely to be parasitic on medium and large trees, such as willow (Salix babylonica), maple poplar (Pterocarya stenoptera), and platanus (Platanus acerifolia). The parasitic position is usually at half the height of the tree or higher.
Fig. 1.
The distribution of Taxillus chinensis (DC.) Danser in the world
The chemical composition and pharmacological activity of T. chinensis vary depending on its host. In China, Taxilli Herba has been shown to “nourish the liver and kidneys, strengthen tendons and bones, expel wind and dampness, and prevent miscarriages”. It is often used for rheumatism, soreness and weakness of the waist and knees, weakness of muscles and bones, profuse menstrual bleeding, blood leakage during pregnancy, threatened abortion, and high blood pressure. For the past 300 years, people in Guangdong and Guangxi in China have used the stems and buds of T. chinensis for making tea. It helps relax muscles and improve collateral circulation. In addition, women in the Lingnan region often use T. chinensis to make soups and tea for pregnancy preservation and postpartum rehabilitation. Clinically, it is mainly used for bone and joint diseases, gynecological diseases, and cerebrovascular diseases such as rheumatoid arthritis, arthralgia, miscarriage, hypertension, and obesity [4–8]. Owing to development and improved social awareness regarding healthcare, T. chinensis has broad economic prospects in various fields.
To date, approximately 110 chemical constituents have been identified in T. chinensis, including flavonoids, phenolic acids, phenylpropanoids, tannins, glycosides, amino acids, and nucleosides. The main chemical constituents in T. chinensis are flavonoids, such as quercetin, quercitrin, rutin, avicularin, and small amounts of d-catechol, mainly dihydroflavones, flavones, and flavonolosides, which are the current research hotspots. Many studies have shown that T. chinensis exhibits many pharmacological effects, including anti-inflammatory, anticancer, antioxidant, antiviral, antimicrobial, diuretic, antihypertensive, and antihyperglycemic activities. The anti-inflammatory, antioxidant, and hypertensive pharmacological effects are closely related to traditional applications [9]. Primarily, it inhibits the production of inflammatory factors and reduces mitochondrial oxidative stress and cyclin degradation. In addition, T. chinensis exhibits both hepatotoxicity and embryotoxicity.
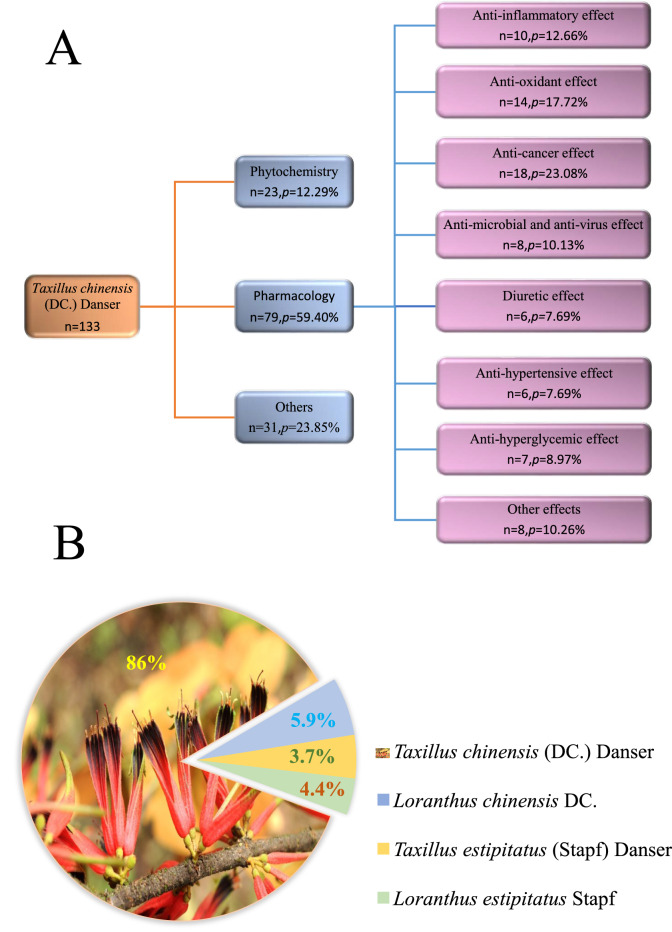
In this review, relevant studies on T. chinensis published before May 2022 were collected from online databases, and more than 360 articles were obtained using the keyword “Taxillus chinensis (DC.) Danser” on Google Scholar, of which over 70 articles contained the keyword “Sang Ji Sheng.” We analyzed the proportion and classification of the literature cited in this review (Fig. 2A). The names commonly used in the literature and data retrieval for T. chinensis are shown in Fig. 2B. At present, the literature on T. chinensis is mainly based on the identification of chemical components; however, the components have not been thoroughly analyzed, and only simple pharmacological activity studies have been performed that were mainly focused on crude extracts and their characteristic compounds, especially quercetin. Furthermore, many active components of T. chinensis have not yet been fully investigated, nor have their mechanisms of action elucidated. Moreover, bioassessments should consider the advisable effective dose, frequency of administration, and treatment duration. Reports on botany, traditional applications, or toxicology are minimal; therefore, these aspects must be reviewed, in addition to the phytochemistry and pharmacology of T. chinensis. This review summarizes the research status, prospects, and limitations of T. chinensis and summarizes its relevance to traditional uses, chemical components, and pharmacological activities. It also criticizes the shortcomings of current research. These will provide references for further research, applications, and development.
Fig. 2.
Taxillus chinensis (DC.) Danser-related articles cited in this review. A The proportion and classification of articles cited in this review. B The names commonly used in the literature and data retrieval of Taxillus chinensis (DC.) Danser
Botany
According to the Chinese Pharmacopoeia (2020 edition) and “Zhong Hua Ben Cao,” T. chinensis is a hemi-parasitic shrub that grows to a height of 0.5–1 m [10, 11]. It is usually distributed in plains or low-mountain evergreen broad-leaved forests at altitudes of 20–400 m. Branchlet and leafage: densely covered with brown or reddish-brown stellate hairs, sometimes with scattered or stacked stellate hairs. Branchlets were black and glabrous. Leaves are nearly opposite or alternate, leathery, ovate, long ovate or elliptic, 5–8 cm long, 3–4.5 cm wide, apex obtuse, base suborbicular, glabrous on top, tomentose on the bottom; lateral veins in 4–5 pairs, leaf veins are obvious; petioles 6–12 mm long, glabrous. Flowers: racemes are borne in the leaf axils or leaf axils of twigs, with 2 to 5 flowers, the inflorescence is corymbose, inflorescences and flowers are densely covered with brown stellate hairs; peduncle and rachis 1–3 mm long, pedicels 2–3 mm long; bracts ovate-triangular, 4-toothed; corolla flower bud is tube-shaped, 2.2–2.8 cm long, slightly curved, distend swollen, apically elliptic, lobes 4, lanceolate, 6–9 mm long, reflexed, sparse hair after anthesis; filaments approximately 2 mm long, anthers 3–4 mm long, another room often has a diaphragm, and the stigma is conical. Fruits: elliptical, yellow–green, with granular skin (https://www.plantplus.cn). The entire plant is shown in Fig. 3.
Fig. 3.
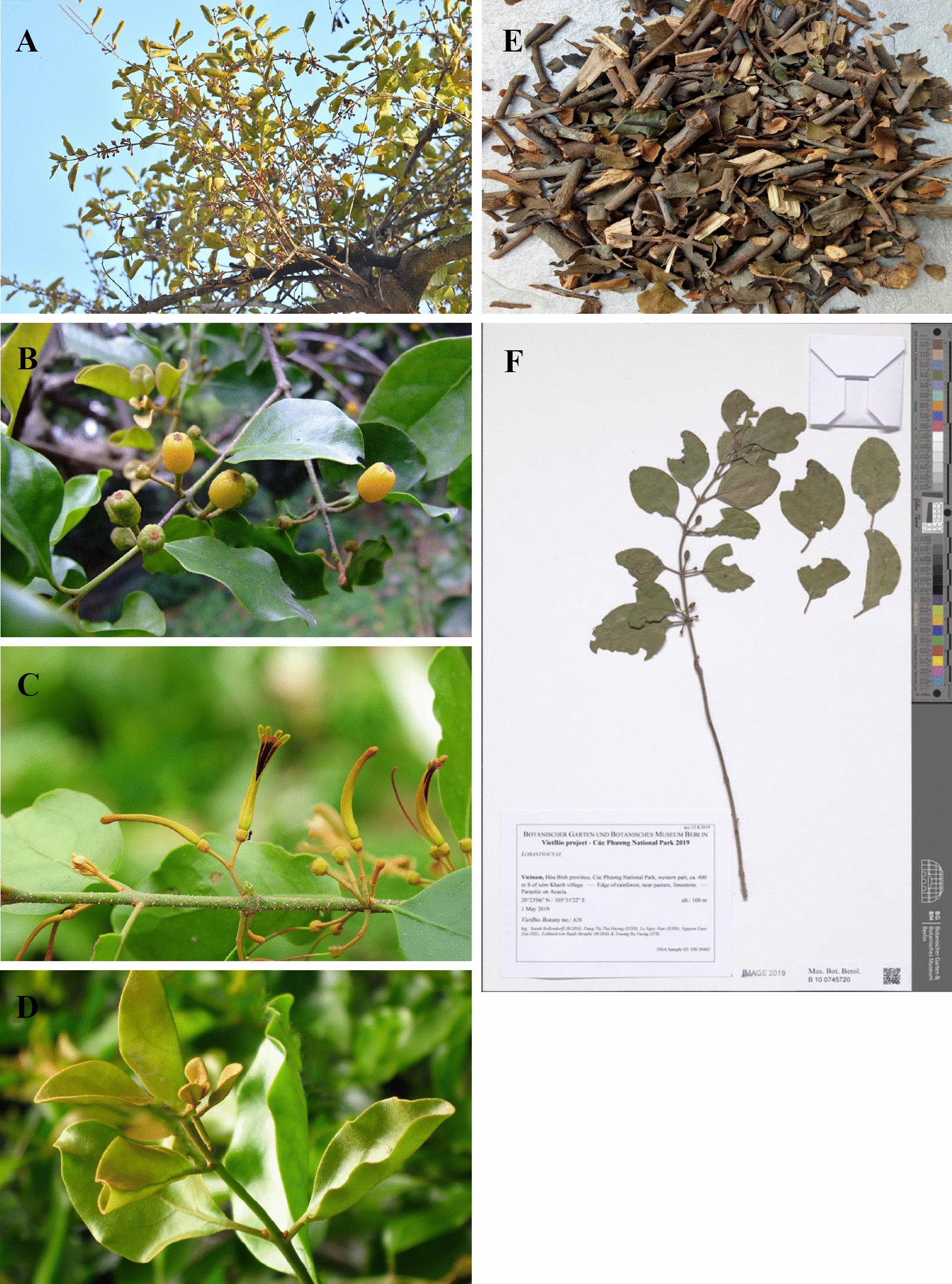
Taxillus chinensis (DC.) Danser. (Obtained from http://ppbc.iplant.cn/sp/1295). A The whole plant, B fruits, C flowers, D leaves, E Taxilli Herba, F specimen of T. chinensis (https://www.gbif.org/occurrence/3059536395)
Owing to similarities in morphology and difficulty in sample collection, T. chinensis is often confused with other plants, such as Scurrula parasitica L., Taxillus balansae (Lecomte) Danser, and Scurrula parastica var. graciliflora. In addition to macroscopic morphological identification, microscopic, physical and chemical, and secondary metabolite analyses, and genetic identification provide more accurate evidence. For example, Wu et al. used ultra-fast liquid chromatography coupled with triple quadrupole mass spectrometry (UFLC-QTRAP-MS/MS) to identify some key constituents, including isoquercitrin, catechin, proline, hyperin, quercetin, etc., to distinguish Taxilli Herba samples from different hosts. The results showed that the relative levels of these components in the M. alba sample were higher than those in other samples [12]. The quantitative analysis of these key components is not only important for identifying T. chinensis from different host sources, but also plays an important role in the safety and effectiveness of the clinical application of T. chinensis. Li et al. evaluated five candidate DNA barcodes, rbcL, matK, psbA-trnH, ITS, and ITS2 DNA, to distinguish T. chinensis from adulterants. Among the five barcodes, the amplification and sequencing efficiencies of rbcL and psbA-trnH were 100%. However, rbcL showed no interspecific discrepancy or identification efficiency. In summary, the psbA-trnH DNA barcode is of great significance for authentically identifying T. chinensis and related parasitic Loranthus [13]. Therefore, modern technology plays a significant role in the identification of medicinal materials.
T. chinensis contains chlorophyll that is connected to the host through a suction device. Owing to its hemi-parasitic characteristics, in the natural state, the spread and reproduction of T. chinensis is mainly achieved by birds pecking at the pulp of T. chinensis fruit, discarding seeds, or digesting the fruit to expel the seeds [14].
Traditional uses
The ancient pharmacological book “Shennong Bencao Jing” records T. chinensis for the first time, which was listed as “top grade” and included in the 2020 Edition of the Chinese Pharmacopoeia [10, 15]. It is bland in nature, bitter and sweet in flavor, and is attributed to the liver and kidney meridians. The medicinal value was first described in “Sheng Cao Yao Xing Bei Yao” (AD1711): “T. chinensis can nourish blood and dissipate heat and is used as a tea to relax tendons and activate collaterals” [16]. According to ancient books such as “Ben Cao Qiu Zhen” (AD1769), “Ben Jing Feng Yuan” (AD1695), and “Yao Xing Lun” (Tang Dynasty), T. chinensis can “dispel wind, remove dampness, replenish the kidney essence, nourish the liver, strengthen muscles and bones, and prevent miscarriage” [17–19]. Traditionally, it was used to treat painful disabilities caused by wind dampness, pain, and weakness in the lower back and knees, weak tendons and bones, bleeding and spotting, profuse menstruation, vaginal bleeding during pregnancy, threatened abortion, dizziness, and vertigo rheumatism (Table 1). “Classified Materia Medica” records: “When you taste the real T. chinensis plant, you can experience very good healing effects.” Among these, the application of T. chinensis in treating threatened abortion is closely related to its function of tonifying the kidney essence and nourishing the liver [20–22].
Table 1.
Traditional applications of Taxillus chinensis (DC.) Danser in classic books of herbal medicine
| Traditional uses | Plant parts | Preparations | Usage | Dosage | Classic books |
|---|---|---|---|---|---|
| Rheumatism | Branches and leaves | Decoction | Oral administration | 15–30 g | Bei Ji Qian Jin Yao Fang [121] |
| Gynecological diseases | Branches and leaves | Pill/decotion | Oral administration | 10–15 g | Yi Xue Zhong Zhong Can Xi Lu; Tai Ping Sheng Hui He Ji Ju Fang [122, 123] |
| Backache | Leaves | Tea/dispersant | Oral administration | 3–15 g | Sheng Cao Yao Xing Bei Yao; Ben Cao Gang mu [16, 124] |
| Paralysis | Branches and leaves | Pill/decoction | Oral administration | 6–30 g | Shi Yi De Xiao Fang [125] |
Owing to the parasitic characteristics of Loranthaceae plants, T. chinensis from different hosts is used to treat various diseases in folk medicine. For example, “Southern Yunnan Materia Medica” (AD1436) records that T. chinensis parasitizing Styphnolobium japonicum (L.) Schott can treat intestinal sub-wind blood syndrome, hemorrhoids, and blood leakage; T. chinensis parasitizing Morus alba L. can treat muscle and collateral obstruction and wind-cold-dampness arthralgia [23]. Its clinical applications must be specified; otherwise, it may be misused, and the desired therapeutic effect will not be achieved. To enhance efficacy, T. chinensis is often used in combination with other drugs, such as Gastrodia rhizoma, Smilacis glabrae Rhizome, Eucommiae cortex, and Polygoni multiflori Radix. Furthermore, the combined use of T. chinensis and Epimedium brevicornum Maxim. has a certain effect on the acute stage of poliomyelitis and its sequelae. However, T. chinensis may cause disease complications in some patients with liver and heart diseases; further research is required to specify the exact cause for this. In this review, we summarized the commonly used prescriptions containing T. chinensis, and their original sources, compositions, traditional effects, and indications are listed in Table 2. The extensive traditional use of T. chinensis indicates that it is safe for use in clinical practice.
Table 2.
The preparations of Taxillus chinensis (DC.) Danser in China
| Preparation name | Compositions | Traditional effects | Traditional indications | References |
|---|---|---|---|---|
|
Duohuo Jisheng pill (Bei ji qian jin yao fang) |
Angelicae sinensis (Oliv.) Diels, T. chinensis, Rehmanniae glutinosa (Gaetn.) Libosch. ex Fisch. et Mey., Achyranthes bidentata BI., Asarum sieboldii Miq., Gentiana macrophylla, Poria cocos (Schw.) Wolf, Cinnamomum cassia Presl, Saposhnikovia divaricate (Trucz.) Schishchk., Ligusticum chunxiong hort, Codonopsis Pilosula, Glycyrrhiza uralensis Fisch., Angelica sinensis (Oliv.) Diels, Cynanchum otophyllum Schneid., Eucommia Ulmoides | It has the functions of nourishing blood and relaxing muscles, dispelling wind and dampness, and replenishing liver and kidney | It is used for wind-cold-dampness arthralgia, cold pain in the waist and knees, and unfavorable flexion and extension | [126, 127] |
|
Mi Niao Ning particles (Chinese pharmacopoeia) |
Polygonum aviculare L., Phellodendron chinense Schneid., Abutilon theophrastii Medic., T. chinensis, Dipsacus asper Wall.ex Henry, Schisandra chinensis (Turcz.) Baill., Bupleurum chinense, Angelica dahurica (Fisch. Ex Hoffm.) Benth. Et Hook. f. ex Franch. et Sav, Glycyrrhiza uralensis Fisch | It has the functions of clearing heat and dredging, diuretic and pain relief, and invigorating the kidney | It is used for pyretic stranguria, urination redness and pain and urinary tract infections | [128] |
|
Zishen Yutai pill (Shang han lun) |
Rehmannia glutinosa Libosch., Panax ginseng C. A. Meyer, Eucommia ulmoides Oliver, Fallopia multiflora (Thunb.) Harald, Lycii fructus, Asini Corii Colla, Cervi cornu Degelatinatum, Morinda officinalis How, Cuscuta chinensis Lam., T. chinensis, Dipsacus asper Wall.ex Henry, Codonopsis pilosula (Franch.) Nannf., Atractylodes macrocephala Koidz, Artemisiae argri Folium, Amomum villosum Lour | It has the functions of invigorating the spleen and kidney, reinforcing qi and build up the strong constitution, nourishing blood and preventing abortion, and strengthening the body | It is used for slippery tire caused by deficiency of both spleen and kidney and insufficiency of Chong Ren | [129] |
|
Qisang Yigan pill (Compilation of national proprietary Chinese medicine) |
Astragalus membranaceus (Fisch.) Bunge, Reynoutria japonica Houtt., Sophora flavescens Ait., T. chinensis, Swertia mileensis, Cordyceps sinensis, Chinemys reevesii (Gray), Panax notoginseng (Burkill) F. H. Chen ex C. H., mel | It has the functions of invigorating the spleen and kidney, promoting blood circulation and removing blood stasis, clearing dampness and heat | It is used for chronic hepatitis B caused by damp-heat stasis, spleen and kidney deficiency | [130] |
|
Sangge Jiangzhi pill (Chinese pharmacopoeia) |
T. chinensis, Pueraria lobata (Willd.) Ohwi., Dioscorea opposita Thunb., Rhei Radix et Rhizome, Crataegus pinnatifida Bge., Salvia miltiorrhiza Bge., Carthamus tinctorius L., Alisma plantago-aquatica Linn., Artemisia capillaris Thunb., Taraxacum mongolicum Hand.-Mazz | It has the functions of invigorating the kidney and strengthening the spleen, removing blood stasis, clearing heat and removing dampness | It is used for spleen-kidney deficiency and phlegm turbidity and blood stasis type hyperlipidemia | [131] |
|
Yunkang particles (Chinese pharmacopoeia) |
Dioscorea opposita Thunb., Dipsacus asper Wall. ex Henry, Astragalus membranaceus, Angelica sinensis (Oliv.) Diels, Cibotium barometz, Cuscuta chinensis, T. chinensis, Eucommia Ulmoides, Psoralea corylifolia L., Codonopsis Pilosula, Poria cocos, Atractylodes macrocephala Koidz, Asini Corii Colla, Rehmannia glutinosa Libosch., Cornus officinalis, Lycii fructus, Mume fructus, Paeonia lactiflora Pall., Amomum villosum Lour., Alpinia oxyphylla Miq., Boehmeria nivea Roots, Scutellaria baicalensis Georgi, Artemisiae argri Folium | It has the functions of invigorating the spleen and strengthening the kidney, nourishing the blood and calming the fetus | It is used for threatened abortion and habitual abortion for kidney deficiency type and qi and blood deficiency type | [132, 133] |
Phytochemistry
The metabolic activity of the parasitic plant itself also differs depending on the diversity of the host, which produces different chemical constituents. This review summarizes approximately 110 compounds, including flavonoids, phenolic acids, phenylpropanoids, tannins, glycosides, amino acids, and nucleosides, that have been isolated and identified from T. chinensis, mainly Morus alba, Magnifera indica, and Liquidambar formosana. The components of T. chinensis are diverse. The chemical constituents and their classifications, structures, chemical formulas, extraction solvents, and parts are shown in Table 3. In the past three years, schools including Nanjing University of Chinese Medicine, Guangzhou University of Chinese Medicine, Chengdu University of Chinese Medicine and Guangxi University of Chinese Medicine have carried out the separation of T. chinensis. At present, the separation of T. chinensis components is mainly performed using ultrasonic treatment with different concentrations of methanol. In order to separate more active ingredients, more treatment methods and extraction solvents may be tried in subsequent work.
Table 3.
Chemical compounds isolated from Taxillus chinensis (DC.) Danser
| No | Chemical components | Classification | Structure | Formula | Extraction solvent and parts | References |
|---|---|---|---|---|---|---|
| Flavonoids | ||||||
| 1 | Isosakuranetin | Dihydroflavones |

|
C16H14O5 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 2 | Prunin | Dihydroflavones |

|
C21H22O10 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 3 | Taxifolin | Dihydroflavonols |

|
C15H12O7 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 4 | 3'-O-methyl-dihydroquercetin-7-β-D-glucoside | Dihydroflavonols |
|
C22H24O12 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 5 | Taxifolin 3'-O-β-D-glucopyranoside | Dihydroflavonols |
|
C21H22O12 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 6 | Quercetin | Flavonols |

|
C15H10O7 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 7 | 7-O-benzyl luteolin | Flavones |

|
C22H16O6 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 8 | Cosmosiin | Flavones |

|
C21H20O10 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 9 | Luteolin-7-O-glucoside | Flavones |

|
C21H20O11 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 10 | Tricetin | Flavones |

|
C15H10O7 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 11 | 5-demethylnobiletin | Flavones |

|
C20H20O8 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 12 | (+)-catechin | Flavanes |

|
C15H14O6 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 13 | Epicatechin | Flavanes |

|
C15H14O6 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 14 | Epigallocatechin | Flavanes |

|
C15H14O7 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 15 | (−)-epicatechin gallate | Flavanes |

|
C22H18O10 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 16 | Kaempferitrin | Flavonolosides |
|
C27H30O14 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 17 | Brassicin | Flavonolosides |

|
C22H22O12 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 18 | Galangin | Flavonolosides |

|
C15H10O5 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 19 | Quercetin-3-O-(6''- galloyl)-β- galactopyranside | Flavonolosides |

|
C28H24O16 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 20 | Quercetin-3-O-(6''-galloyl)-β-D-glucopyranoside | Flavonolosides |

|
C28H24O16 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 21 | Myricetrin | Flavonolosides |

|
C21H20O12 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 22 | Rutin | Flavonolosides |
|
C27H30O16 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 23 | Hyperoside | Flavonolosides |

|
C21H20O12 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 24 | Quercetin 3-O-β-D- glucuronide | Flavonolosides |

|
C21H18O13 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 25 | Isoquercitrin | Flavonolosides |

|
C21H20O12 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 26 | Avicularin | Flavonolosides |

|
C20H18O11 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 27 | Kaempferol-3-rutinoside | Flavonolosides |
|
C27H30O15 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 28 | Quercitrin | Flavonolosides |

|
C21H20O11 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 29 | Astragalin | Flavonolosides |

|
C21H20O11 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 30 | Afzelin | Flavonolosides |

|
C21H20O10 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 31 | Homomangiferin | Bisphenirone flavonoids |

|
C20H20O11 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 32 | Isochinomin | Bisphenirone flavonoids |

|
C20H20O11 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 33 | Hydrocarpin | Flavonoid lignans |

|
C25H20O9 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 34 | 8-methylretusin-7-β- glucoside | Isoflavones |

|
C23H24O10 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 35 | Cynaroside A | Flavonoids |

|
C21H32O10 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 36 | Luteolin-7,3'-di-O-β-D-glucoside | Flavonoids | not found | C27H30O16 | 70% methanol extract of the stems and leaves of T. chinensis from Morus alba L | [28] |
| 37 | Pinocembrin | Flavonoids |

|
C15H12O4 | 70% methanol extract of the stems and leaves of T. chinensis from Morus alba L | [28] |
| 38 | Nigrasins A | Flavonoids |

|
C25H26O8 | 70% methanol extract of the stems and leaves of T. chinensis from Morus alba L | [28] |
| 39 | Artonin E2 | Flavonoids |

|
C25H24O7 | 70% methanol extract of the stems and leaves of T. chinensis from Morus alba L | [28] |
| 40 | Luteolin 8-C-hexosyl-O-hexoside | Flavonoids | not found | C27H30O16 | 70% methanol extract of the stems and leaves of T. chinensis from Morus alba L | [28] |
| 41 | Sanggenon F/H | Flavonoids |
|
C20H18O6 | 70% methanol extract of the stems and leaves of T. chinensis from Morus alba L | [28] |
| 42 | Kuwanon S2 | Flavonoids |
|
C25H26O5 | 70% methanol extract of the stems and leaves of T. chinensis from Morus alba L | [28] |
| 43 | Sanggenon M | Flavonoids |
|
C25H24O7 | 70% methanol extract of the stems and leaves of T. chinensis from Morus alba L | [28] |
| 44 | Kuwanon D | Flavonoids |
|
C25H26O6 | 70% methanol extract of the stems and leaves of T. chinensis from Morus alba L | [28] |
| 45 | Sanggenol L | Flavonoids |

|
C25H26O6 | 70% methanol extract of the stems and leaves of T. chinensis from Morus alba L | [28] |
| 46 | Mangiferin | Flavonoids |

|
C19H18O11 | 40% methanol extract of the branches and leaves of T. chinensis from Mangifera indica | [29] |
| 47 | Quercetin-3-O-β-D-glucuronide | Flavonoids |

|
C21H18O13 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 48 | Hyperin | Flavonoids |

|
C21H20O12 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 49 |
Kaempferol-3,7- bisrhamnoside |
Flavonoids |
|
C27H30O14 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| Phenolic acids | ||||||
| 50 | Quinic acid | Phenolic acids |
|
C7H12O6 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 51 | Shikimic acid | Phenolic acids |
|
C7H10O5 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 52 | Malic acid | Phenolic acids |

|
C4H6O5 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 53 | Citric acid | Phenolic acids |

|
C6H8O7 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 54 | Gallic acid | Phenolic acids |
|
C7H6O5 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 55 | Protocatechuic acid | Phenolic acids |
|
C7H6O4 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 56 | 4-hydroxybenzoic acid | Phenolic acids |
|
C7H6O3 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 57 | Coniferic acid | Phenolic acids |
|
C10H10O4 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| Phenylpropanoids | ||||||
| 58 | Toddacoumaquinone | Phenylpropanoids |

|
C23H18O7 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 59 | p-coumaric acid | Phenylpropanoids |
|
C9H8O3 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 60 | Caffeic acid | Phenylpropanoids |
|
C9H8O4 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 61 | Chlorogenic acid | Phenylpropanoids |

|
C16H18O9 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| Tannins | ||||||
| 62 | Glucogallin | Hydrolysable tannins |

|
C13H16O10 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 63 | Procyanidin B2 | Condensed tannins |

|
C30H26O12 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 64 | Procyanidin B1 | Condensed tannins |

|
C30H26O12 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 65 | Procyanidin C1 | Condensed tannins |

|
C45H38O18 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 66 | Procyanidin B2 3'-O-gallate | Condensed tannins |

|
C37H30O16 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| Glycosides | ||||||
| 67 | Taxilluside A | Ester glycosides |

|
C18H24O10 | 60% aqueous ethanol extract of the branches and leaves of T. chinensis | [40] |
| 68 | Taxilluside B | Ester glycosides |

|
C18H24O10 | 60% aqueous ethanol extract of the branches and leaves of T. chinensis | [40] |
| 69 | Taxilluside C | Ester glycosides |
|
C25H28O14 | 60% aqueous ethanol extract of the branches and leaves of T. chinensis | [40] |
| 70 | Taxilluside D | Ester glycosides |
|
C18H25O10 | 60% aqueous ethanol extract of the branches and leaves of T. chinensis | [40] |
| 71 | Hydroxybenzoic acid β-D-glucose ester | Ester glycosides |

|
C13H16O8 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 72 | Tachioside | Phenol glycosides |
|
C13H18O8 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 73 | (1S)-2(acetyloxy)-1-(hydroxymethy)ethyl-β-D-glucopyranoside | Phenol glycosides |
|
C11H20O9 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 74 | Gallic acid 3-O-β-D-glucopyranoside | Phenol glycosides |

|
C13H16O10 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 75 | 2,6-dihydroxyphenyl-β-D-glucopyranosiduronic acid | Phenol glycosides |

|
C12H14O9 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 76 | Glucosyringic acid | Phenol glycosides |
|
C15H20O10 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 77 | Methyl-4-(β-D-glucopyranosyloxy)-3-methoxybenzoate | Phenol glycosides |
|
C15H20O9 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 78 | Ethyl 3-(β-D-glucopyranosyloxy) butanoate | Phenol glycosides |
|
C12H22O8 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 79 | Hexyl 6-O-β-D-xylopyranosyl-β-D-glucopyranoside | Phenol glycosides |
|
C17H32O10 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 80 | Diyhdromelilotoside | Phenol glycosides |

|
C15H20O8 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 81 | Androsin | Phenol glycosides |
|
C15H20O8 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 82 | Phloracetophenone 4'-O-glucoside | Phenol glycosides |
|
C14H18O9 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 83 | Salicin | Phenol glycosides |

|
C13H18O7 | methanol extract of the branches and leaves of T. chinensis from Willow | [41] |
| 84 | Mulberroside F | Stibene glucosides |

|
C26H30O14 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| Amino acids | ||||||
| 85 | Glutamine | Amino acids |

|
C5H10N2O3 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 86 | Lysine | Amino acids |
|
C6H14N2O2 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 87 | Histidine | Amino acids |
|
C6H9N3O2 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 88 | Argnine | Amino acids |
|
C6H14N4O2 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 89 | Serine | Amino acids |

|
C3H7NO3 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 90 | Threonine | Amino acids |

|
C4H9NO3 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 91 | Glutamic acid | Amino acids |

|
C5H9NO4 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 92 | Proline | Amino acids |

|
C5H9NO2 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 93 | Valine | Amino acids |

|
C5H11NO2 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 94 | Tyrosine | Amino acids |
|
C9H11NO3 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 95 | Isoleucine | Amino acids |

|
C6H13NO2 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 96 | Leucine | Amino acids |

|
C6H13NO2 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 97 | Phenylalanine | Amino acids |
|
C9H11NO2 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| Nucleotides | ||||||
| 98 | 2'-deoxyadenosine | Nucleotides |
|
C10H13N5O3 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 99 | Inosine | Nucleotides |
|
C10H12N4O5 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 100 | Guanosine | Nucleotides |

|
C10H13N5O5 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 101 | 2'-deoxyguanosine | Nucleotides |

|
C10H13N5O4 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| 102 | Adenosine | Nucleotides |
|
C10H13N5O4 | 70% methanol extract of the stems, branches and leaves of T. chinensis from 45 hosts | [12] |
| Others | ||||||
| 103 | Glucose | Polyhydroxy aldehydes |

|
C6H12O6 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 104 | Primeverose | Carbohydrates |
|
C11H20O10 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 105 | Bisdemethoxycurcumin | Diphenylheptane |
|
C19H16O4 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 106 | Fluorescein-β-D-galactopyranoside | Galactosides |
|
C26H22O10 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 107 | Artonol B | Phenols |
|
C24H20O7 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 108 | Swertiamarin | Liridoid |
|
C16H22O10 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
| 109 | Emodin | Anthraquinones |

|
C15H10O5 | 50% methanol extract of the dried stems and branches with leaves of T. chinensis from Morus alba L | [27] |
In addition, researchers have determined the chemical components and their variation laws with significant differences through core means, such as similarity evaluation, cluster analysis, and principal component analysis. Upon analysing these studies, we found that the chemical compositions of T. chinensis samples from different hosts were roughly similar, but were clearly different in the contents of flavonoids. Yuan et al. identified 19 different chemical components, including proanthocyanidin B2, proanthocyanidin B1, proanthocyanidin C1, isosakuranetin, and kaempferitrin, in T. chinensis from 10 host plants. Among them, ( +)-catechin, hyperoside, quercetin 3-O-β-D-glucuronide, and quercetin were common chemical components. These four compounds were all flavonoids, but their content differed significantly in T. chinensis from different hosts. The relative contents of these four compounds in T. chinensis from Morus alba L. were higher than those in the other nine hosts, followed by Clausena lansium (Lour.) skeels and Diospyros kaki Thunb. The quercetin 3-O-β-D-glucuronide and hyperoside contents were the lowest in T. chinensis from Sapindus saponaria Linnaeus [24, 25].
Flavonoids
Flavonoids are widespread throughout the plant kingdom and are considered the main chemical constituents of T. chinensis [26]. To date, 49 flavonoids have been identified in T. chinensis, including dihydroflavones, flavonols, dihydroflavonols, isoflavones, flavones, and flavanes. A study conducted on a 50% methanol extract of Taxilli Herba from Morus alba L. has reported the isolation of 34 flavonoid compounds including isosakuranetin (1), prunin (2), taxifolin (3), 3'-O-methyl-dihydroquercetin-7-β-D-glucoside (4), taxifolin 3'-O-β-D-glucopyranoside (5), quercetin (6), 7-O-benzyl luteolin (7), cosmosiin (8), luteolin-7-O-glucoside (9), tricetin (10), 5-demethylnobiletin (11), ( +)-catechin (12), epicatechin (13), epigallocatechin (14), (-)-epicatechin gallate (15), kaempferitrin (16), brassicin (17), galangin (18), quercetin-3-O-(6''-galloyl)-β-galactopyranside (19), myricetrin (21), rutin (22), hyperoside (23), quercetin 3-O-β-D-glucuronide (24), isoquercitrin (25), avicularin (26), kaempferol-3-rutinoside (27), quercitrin (28), astragalin (29), afzelin (30), homomangiferin (31), isochinomin (32), hydrocarpin (33), 8-methylretusin-7-β-glucoside (34), and cynaroside A (35) [27]. The 70% methanol extract of Taxilli Herba from 45 hosts by UFLC-QTRAP-MS/MS revealed the presence of flavonoids such as quercetin-3-O-(6''-galloyl)-β-D-glucopyranoside (20), quercetin-3-O-β-D-glucuronide (47), hyperin (48), and kaempferol-3,7-bisrhamnoside (49) [12]. Ten flavonoid compounds reported using UPLC-MS analysis of the 70% methanol extract of the stems and leaves of T. chinensis from Morus alba L. were luteolin-7,3'-di-O-β-D-glucoside (36), pinocembrin (37), nigrasins A (38), artonin E2 (39), luteolin 8-C-hexosyl-O-hexoside (40), sanggenon F/H (41), kuwanon S2 (42), sanggenon M (43), kuwanon D (44), and sanggenol L (45) [28]. Similarly, mangiferin was found in a 40% methanol extract of branches and leaves of T. chinensis from Mangifera indica revealed the presence of mangiferin (46) [29]. Different extraction sites can have different effects on the content of the active ingredients. The total flavonoid content in the leaves of T. chinensis was approximately four times higher than that in the stems and branches [30]. Flavonoids have anti-inflammatory properties and are potent antioxidants [31]. Quercetin 3-O-β-D-glucuronide, isoquercitrin, catechin, hyperin, hyperoside, quercetin, avicularin, and quercitrin are the main flavonoids in T. chinensis and may be the active ingredients in T. chinensis that exert anti-inflammatory and antioxidant effects. Of these, quercetin is often sold as a dietary supplement. In Canada, quercetin can be used as a “natural health product” with two different benefits: “antioxidant” or “used in herbal medicine as a capillary or blood vessel protectant” [32]. Rutin is a unique antioxidant flavonoid that is abundant in plants [33]. Isoquercitrin has a variety of protective roles in vitro and in vivo, particularly against oxidative stress, cancer, cardiovascular disease, diabetes, and allergic reactions [34]. Although flavonoids are the hot spots of current research, their structure–activity relationship, activity mechanism, absorption, and metabolism mechanism remain to be understood, which limits their development and utilization. In the future, these aspects of flavonoids should be further studied, as they will have a significant impact on the development of new drugs.
Phenolic acids
The term “phenolic acids” generally refers to phenols with a single carboxylic acid functionality, and can be categorized into three main subclasses, including hydroxybenzoic acid, hydroxycinnamic acid, and hydroxyphenylacetic acid [35]. At present, 8 phenolic acids have been found in Taxilli Herba, including quinic acid (50), shikimic acid (51), malic acid (52), citric acid (53), gallic acid (54), protocatechuic acid (55), 4-hydroxybenzoic acid (56), and coniferic acid (57) [12, 27]. Phenolic acids are receiving increasing attention because of their high antioxidant activity and other antibacterial, dietary, and health benefits [36]. However, the proportion of phenolic acids in T. chinensis remains unclear; therefore, their biological activity requires further verification. Plant phenolic acids also face problems of low extraction efficiency and low purity, and extraction technology must be continuously improved.
Phenylpropanoids
Phenylpropanoids are usually a type C6-C3 compound as the basic unit, typically including simple phenylpropanoids, coumarins, and lignans. To date, four phenylpropanoids have been isolated from a 50% methanol extract of Taxilli Herba, including p-coumaric acid (59), caffeic acid (60), and chlorogenic acid (61), which are classified as simple phenylpropanoids, and toddacoumaquinone (58), which is a coumarin [27]. Among them, caffeic acid and chlorogenic acid have broad-spectrum antibacterial and antiviral effects, and may be effective components of T. chinensis. In the future, the phenylpropane components of T. chinensis must be analyzed quantitively and its antiviral activity verified.
Tannins
A study conducted on a 50% methanol extract of Taxilli Herba from Morus alba L. revealed the presence of five tannins, including glucogallin (62), procyanidin B2 (63), procyanidin B1 (64), procyanidin C1 (65), and procyanidin B2-3'-O-gallate (66) [27]. Among them, glucogallin is a hydrolyzable tannin, and the remainder is condensed tannins. Procyanidins are the main components of T. chinensis tannins and have various pharmacological activities, including antioxidant, anticancer, and hyperglycemic activities [37–39]. According to current experimental research, they may be the active ingredients responsible for the anticancer activity of T. chinensis.
Glycosides
Glycosides are compounds in which sugars or glycoside saccharides are attached to form another non-sugar substance by carbon atoms at the end of the sugar. To date, 18 glycosides have been isolated and identified from T. chinensis. Phytochemical research on the branches and leaves of T. chinensis led to the isolation of taxilluside A-D (67–70) [40]. Similarly, a study conducted on a 50% methanol extract of Taxilli Herba from Morus alba L. reported the isolation of 13 glycoside compounds, including hydroxybenzoic acid β-D-glucose ester (71), tachioside (72), (1S)-2(acetyloxy)-1-(hydroxymethy)ethyl-β-D-glucopyranoside (73), gallic acid 3-O-β-D-glucopyranoside (74), 2,6-dihydroxyphenyl-β-D-glucopyranosiduronic acid (75), glucosyringic acid (76), methyl-4-(β-D-glucopyranosyloxy)-3-methoxybenzoate (77), ethyl 3-(β-D-glucopyranosyloxy) butanoate (78), hexyl 6-O-β-D-xylopyranosyl-β-D-glucopyranoside (79), diyhdromelilotoside (80), androsin (81), phloracetophenone 4'-O-glucoside (82), and mulberroside F (84) [27]. Additionally, salicin (83) was isolated from the methanol extract of the branches and leaves of T. chinensis in willow [41]. Taxilluside C and taxilluside D from T. chinensis exhibited inhibitory activity against calcium concentration in myocardial cells, which was observed by measuring the change in fluorescence signal using laser scanning confocal microscopy [40]. This suggests that T. chinensis might have a protective effect on cardiomyocytes. Furthermore, the ion channel regulatory activities of these compounds must be explored further. The activity of other glycosides in T. chinensis have not been studied, and will be a future research direction.
Amino acids
Amino acids are not only used in protein biosynthesis, but also serve as the building blocks of several other biosynthetic pathways and play key roles in signaling processes and plant stress responses [42]. To date, only 13 amino acids have been identified in T. chinensis. Glutamine (85) was detected in a 50% methanol extract of Taxilli Herba from Morus alba L. [27]. A UFLC-QTRAP-MS/MS study conducted on a 70% methanol extract of Taxilli Herba from 45 hosts reported 12 amino acids, including lysine (86), histidine (87), arginine (88), serine (89), threonine (90), glutamic acid (91), proline (92), valine (93), tyrosine (94), isoleucine (95), leucine (96), and phenylalanine (97) [12]. Glutamic acid, arginine, glutamine, and other amino acids can be used alone for treating certain diseases, such as liver, digestive tract, and respiratory diseases [43–45]. Hence, the discovery of amino acids in T. chinensis may lead to further research on its potential pharmacological activities.
Nucleotides
Nucleotides fulfill many essential functions in plants, such as promoting growth, development, and delaying senescence. Five nucleotides, namely 2'-deoxyadenosine (98), inosine (99), guanosine (100), 2'-deoxyguanosine (101), and adenosine (102), were isolated from a 70% methanol extract of Taxilli Herba from 45 hosts [12]. The nucleotide content of T. chinensis plants is unknown. Primarily, it regulates plant growth and development and has little value in terms of pharmacological activity.
Others
Several other compounds have been isolated from the 50% methanol extract of Taxilli Herba from Morus alba L., such as glucose (103), primeverose (104), bisdemethoxycurcumin (105), fluorescein-β-D-galactopyranoside (106), artonol B (107), swertiamarin (108), and emodin (109) [27].
Pharmacology
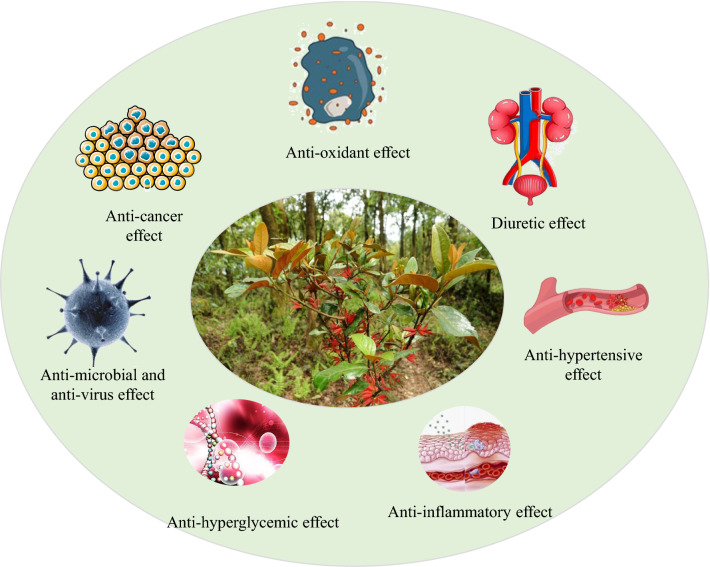
T. chinensis is a well-known Chinese medicine widely used to treat viral hepatitis, splenic asthenia, liver cancer, and renal toxicity [46]. Studies have shown that it has anti-inflammatory, antioxidant, anticancer, antimicrobial, antiviral, diuretic, antihypertensive, antihyperglycemic, and other properties (Fig. 4). The bioactivities are summarized in Table 4. T. chinensis “tonifying the liver and kidneys, strengthening muscles and bones” mainly involves biological processes such as cell proliferation, metabolic processes, biosynthesis processes, and inflammatory reactions by regulating thyroid hormone, osteoclast differentiation, HIF-1, TNF, NF-κB, and estrogen [47]. This process is closely related to the antioxidant, anti-inflammatory, antitumor, and cardiovascular protective activities of T. chinensis.
Fig. 4.
Summary of pharmacological effects of Taxillus chinensis (DC.) Danser
Table 4.
Modern pharmacological studies of Taxillus chinensis (DC.) Danser
| Bioactivities | Model | Extracts or compound | Method of administration | Dosage | Mechanism | References |
|---|---|---|---|---|---|---|
| Anti-inflammatory | RAW 264.7 macrophages | The whole dried plant/water/ethanol extracts | / | 60 mg/mL | Inhibiting NO and TNF-α production | [52] |
| RAW 264.7 macrophages | The whole plant/quercetin | / | 2.5, 5, 10, 20 μg/ml | Inhibiting NO production and the protein expression of iNOS and COX-2 in a dose-dependent manner | [7] | |
| Xylene-induced ear edema mice | The whole plant/water extracts | Intragastric administration | 0.5, 1.0 mg/kg b/w | Reducing the extent of ear edema | [55] | |
| Collagen-induced arthritis mice | The whole plant/quercetin | Intragastric administration | 50, 100 mg/kg b/w | Inhibiting ankle mitochondrial dysfunction and mitochondrial oxidative stress | [4] | |
| Antioxidant | DPPH radical | The whole dried plant/water/ethanol extracts | / | 60 mg/mL | Exhibiting good free radical scavenging ability | [52] |
| yeast model | The whole dried plant/water/ethanol extracts | / | 60 mg/mL | Showing higher survival rates | [52] | |
| DPPH radical | Dried stem/the crude polysaccharide extract | / | 10 mg/mL | Exhibiting significant scavenging ability, with scavenging capacities more than 400 µM ascorbate equiv/g | [68] | |
| Saccharomyces cerevisiae BY4734 | Dried stem/the purified polysaccharide | / | 10 mg/mL | TCP-2, TCP-3, UC-1 and UC-2 displaying significant antioxidant activity | [68] | |
| Anticancer | Human colorectal cancer cell lines HCT116 and SW480 | The whole plant/70% ethanol extracts | / | 25, 50, 100 μg/ml | Inhibiting human colorectal cancer cells through GSK3β-dependent cyclin D1 degradation | [73] |
| Human colon cancer HT-29 cells | Taxilli heba/water extracts | / | 0, 0.5, 1, 2, 4, 8 g/mL | Inhibiting the proliferation, invasion, and migration of human colon cancer cells via the PI3K/AKT signaling pathway | [74] | |
| Human leukemia cell lines HL-60 and K562 | The whole plant/extracts | / | 50, 100, 200, 400 μg/ml | Inhibiting cell proliferation | [75] | |
| Human leukemia U937 cells | Quercetin | / | 10, 20 μM | Promoting the reversible G2/M phase arrest of U937 cells | [80] | |
| Myeloid cell line P39 | Quercetin | / | 10, 50, 100 μM | Decreasing expression of BcL2, BcL-xL and McL-1 expression, increasing Bax expression | [81] | |
| Liver cancer cells (HuH-7 cells, HepG-2 cells) | Procyanidin B1 | / | 0, 5, 50, 500 μM | Inhibiting the Kv10.1 channel in a concentration-dependent manner | [82] | |
| Xenograft mice | Procyanidin B1 | Subcutaneous injection | 15 mg/kg b/w | Inhibiting the growth of the tumor | [82] | |
| MCF-7 and MDA-MB-231 breast cancer cell lines | Procyanidin C1 | / | 6.25 ~ 100 μg/mL | Inducing DNA damage, arresting the cell cycle, Decreasing Bcl-2 levels, and increasing the expression of BAX, caspase 3 and 9 in cells | [83] | |
| Human liver cancer cells Bel-7402 and human stomach cancer cells MGC-823 | Lectins | / | 6.25, 12.5, 25, 50, 100, 200 μg/mL | Inhibiting the growth of cells | [86] | |
| Antimicrobial and anti-virus | Vero E6 cells | The dried stem, with leave of the plant/water–ethanol extracts | / | 0, 25, 50, 100, 200 μg/mL | Inhibiting SARS-CoV 3CL protease activity | [87] |
| HBsAg | The whole plant/10% water extract | / | 20, 40, 80, 150, 300, 600, 1200, 2500 μg/50 μL | Exhibiting good inhibitory effect on HbsAg | [88] | |
| DHBV-infected ducklings | Chlorogenic acid, caffeic acid, quinic acid | Intragastric administration | 100 mg/kg b/w | Reducing the DHBV viremia | [89] | |
| Diuretic | Anesthetized dogs | Avicularin | Intravenous injection | 0.5 mg/kg b/w | Exhibiting diuresis | [95, 96] |
| Rats | Avicularin | Intragastric administration or injection | 34 mg/kg b/w | Exhibiting significant diuretic effect | [95, 96] | |
| Anti-hypertensive | Spontaneously hypertensive rats | Taxilli herba | Intragastric administration | 1.48, 5.90 g/kg b/w | Increasing SOD activity, increasing NO release in serum, and decreasing AngII and ET-1 levels in plasma | [102] |
| Renal hypertensive rats | Quercetin | Intragastric administration | 30 mg/kg b/w | Decreasing blood pressure, reducing the concentration of free calcium ions in renal artery smooth muscle cells | [103] | |
| Anti-hyperglycemic | Hyperglycemia mice induced by streptozotocin | Total flavonoids | Intragastric administration | 100, 200, 400 mg/kg b/w | Reducing the serum TC and TG levels and increase the serum HDL-G content of mice | [107] |
| Diabetic mice induced by streptozotocin (STZ) | Total flavonoids | Intragastric administration | 150, 300, 600 mg/kg b/w | Inhibiting lipid peroxidation in mice, protecting thymus atrophy and improving insulin resistance in diabetic mice | [108] | |
| HepG 2 cells | Taxilli herba | / | 0.1, 0.01, 0.001 mg/mL | Promoting the metabolism of peripheral tissues and improving the sensitivity of liver cells to insulin | [109] | |
| Type 2 diabetes mellitus (T2DM) model mice | The dried plant/Ethanol extract | Intragastric administration | 7.5, 15, 30 g/kg b/w | Improving high blood glucose level, liver and kidney complications, and protecting liver and kidney function | [110] |
Anti-inflammatory effect
T. chinensis can treat multiple inflammatory diseases, including osteoarthritis, chronic pelvic inflammation, chronic kidney disease, and rheumatoid arthritis [48–51]. The anti-inflammatory activity of T. chinensis is closely related to its traditional rheumatism-dispelling effect. Zhang et al. used RAW264.7 cells to test the anti-inflammatory activity of the water-alcohol extract of T. chinensis. They found that T. chinensis extract had significant anti-inflammatory activity by restraining the generation of NO (IC50 = 0.05 mg/mL) and TNF-α (IC50 = 0.14 mg/mL), and did not significantly affect cell viability [52]. TNF-α can activate the expression of nicotinamide adenine dinucleotide phosphate (NADPH) oxygenase, thereby promoting the synthesis of reactive oxygen species (ROS) by NADPH and further aggravating the inflammatory response of the body [53]. It can be speculated that T. chinensis extract exerts its anti-inflammatory effect mainly by reducing the oxidative stress state of the body. A lipopolysaccharide-induced cellular inflammation model was also used to evaluate the anti-inflammatory activity of T. chinensis. Liu et al. found that RAW264.7 macrophages cultured with quercetin (5, 10, and 20 μg/mL) and LPS (100 ng/mL) for 24 h exhibited no changes in cell viability. Compared with LPS alone, 10 and 20 μg/mL quercetin significantly inhibited NO generation. Meanwhile, quercetin dose-dependent inhibition of iNOS and COX-2 protein expression was observed in LPS-treated Raw264.7 cells [7]. The two aforementioned studies were conducted on RAW264.7 cells to study their anti-inflammatory activity. However, one cell model is not convincing enough and should be further validated in other cell lines, such as the J774A.1 and BMDM cell models. The anti-inflammatory mechanism of quercetin may be related to the reduction of inflammatory cytokines TNF-α, IL-1, and IL-6 by inhibiting LPS-induced activation and nuclear translocation of NF-κB and phosphorylation of extracellular signal-regulated kinase 1/2 (ERK1/2) and c-Jun N-terminal kinase [54]. In a subsequent study, the regulatory effect of T. chinensis on the above inflammatory factors was detected to reveal its possible mechanistic pathway, which represents significant progress in the study of the anti-inflammatory effects of T. chinensis.
In addition, the water extract of T. chinensis reduced the extent of ear edema in mice, which was induced by the proinflammatory agent xylene, and accelerated the dissipation of inflammation, and its therapeutic effect was equal to that of the positive control drug aspirin [55]. Shen et al. found that quercetin treatment significantly attenuated the inflammatory response and inhibited ankle mitochondrial dysfunction and mitochondrial oxidative stress in collagen-induced arthritis (CIA) mice [4]. The afore-mentioned studies have verified the in vivo anti-inflammatory effect and provided a scientific basis for the folk use of T. chinensis to treat various inflammatory diseases, especially rheumatoid arthritis; however, these studies are still in the initial stages, and clinical experimental data are lacking. Further research is required to validate these results.
Antioxidant effect
Free radicals and ROS generated during human metabolism cause severe oxidative damage to large molecules, such as proteins, DNA, and lipids, which have been linked to heart disease, cancer, and atherosclerosis [56–59]. For example, ROS accumulation occurs during lung tumorigenesis. To maintain oxidative homeostasis, BACH1, Nrf2, and Maf transcription factors regulate the expression of antioxidant genes such as heme oxygenase-1 (HO-1) [60]. T. chinensis contains a variety of flavonoids. Flavonols are one of the most common classes of flavonoids in the diet and exhibit strong lipid peroxidation-inhibitory activity [61]. Some flavones prevent amplification and damage to other biomolecules, such as lipids, proteins, and DNA, by directly decreasing the levels of free radicals (hydroxyl, superoxide, and nitric oxide) and/or reactive species (such as hydrogen peroxide, peroxynitrite, and hypochlorous acid) in cells, thereby interfering with various oxidative stress-related events [62]. The antioxidant activity of T. chinensis was studied using the 2,2-diphenyl-1-pyridine hydrazide (DPPH) free-radical scavenging method and a yeast model. Ascorbate (vitamin C) was used as a positive control. Notably, T. chinensis showed significant activity in both the DPPH and yeast models. The scavenging capacity of the water extract was 152.4 μM ascorbate equiv/g, whereas that of the ethanol extract was 91.36 μM ascorbate equiv/g. Moreover, the correlation between total phenolic and flavonoid content and antioxidant properties was significant for aqueous and ethanolic extracts [52]. The antioxidant activity of the extracts prepared using different solvents was significantly different, primarily due to the polarity of the extraction agent. Moreover, the antioxidant capacities of T. chinensis differ significantly among different hosts. For example, the ethyl acetate and n-butanol extracts of T. chinensis from Clausena lansium (Lour.) Skeels showed good antioxidant activity, and 80% acetone extracts of T. chinensis from Nerium indicum showed the best antioxidant activity [63, 64].
Recently, the separation, characterization, and activity of polysaccharides in oriental medicine have become research hotspots due to their antitumor, antioxidative, antidiabetic, hypolipidemic, and immunoregulatory activities [65–67]. The antioxidant activity of T. chinensis polysaccharides was studied by DPPH and yeast assays for the first time. All polysaccharide fractions of T. chinensis had significant scavenging ability, ranging from 207 to 662 μM ascorbate equiv/g. Among them, TCP-2 and TCP-3 showed significant antioxidant activity, with scavenging capacities greater than 400 μM ascorbate equiv/g. Saccharomyces cerevisiae BY4743 was used to determine the antioxidant capacity of the purified polysaccharides in vivo using a high-throughput assay. They demonstrated the in vivo antioxidant activity of fractions, including TCP-2, TCP-3, UC-1, and UC-2. However, TCP-1 was toxic at high concentrations and exhibited no significant antioxidant activity in vivo. Therefore, no further studies on TCP-1 were conducted. These results suggest the potential of polysaccharides isolated from T. chinensis as natural antitumor agents [68]. In summary, phenols, flavonoids, and polysaccharides from T. chinensis have clear antioxidant effects. The presence of other antioxidant active components in T. chinensis must be investigated further. Owing to its potent antioxidant activity, T. chinensis is expected to become a natural antioxidant that can be used to prevent or treat diseases related to oxidative damage.
Anticancer effect
Most traditional chemotherapy and radiotherapy focus on antiproliferative treatment [69]. The antiproliferative activity of herbal medicines provides hope for treating cancer, tumors, and other malignant diseases. T. chinensis contains various anticancer compounds such as rutin, quercetin, and phlorin [70–72]. Park et al. found that 70% ethanol extracts of T. chinensis (25–100 μg/mL) inhibited human colorectal cancer cell growth in a dose-dependent manner. The potential molecular mechanism involves the inhibition of the proliferation of human colorectal cancer cells through GSK3β-dependent degradation of cyclin D1 [73]. Feng et al. explored the effects of T. chinensis extract on the proliferation, invasion, and migration of human colon cancer HT-29 cells. The relative protein expression levels of p-PI3K and p-AKT were significantly decreased following treatment with T. chinensis extract, suggesting that T. chinensis extract inhibited proliferation, invasion, and migration through the PI3K/AKT signaling pathway [74]. These findings provide evidence for the development of T. chinensis as a chemopreventive or therapeutic drug for human colorectal cancer. However, cell invasion and migration are complex processes involving various signaling pathways, genes and cytokines. It is not rigorous to determine the mechanism of action solely based on the decreased relative expression levels of p-PI3K and p-AKT in cells, and more indicators need to be measured for verification. It is also necessary to obtain additional cell lines from colorectal cancer and xenografted mice to confirm their anticancer activity. The results showed that the extract of T. chinensis from Casuarina equisetifolia Forst had inhibitory effect on the proliferation of HL-60 and K562 cells, and the diethyl ether, ethyl acetate, and n-butanol fractions were identified as the active fractions of T. chinensis against leukemia cells in vitro for the first time. However, the active ingredient and its mechanism of action need to be further studied [75].
The components of T. chinensis have also shown anticancer activity. For example, several studies have confirmed that quercetin inhibits the growth and proliferation of different cell lines, such as lung, colon, breast, and prostate cancer cell lines [76–79]. In addition, quercetin promoted reversible G2/M phase arrest in U937 cells by decreasing cyclin D, E, E2F1, and E2F2, and increasing cyclin B [80]. Quercetin induced apoptosis and autophagy in P39 cells and increased cell blocks in the G1 phase. Quercetin treatment in vivo significantly reduced the tumor volume in P39 xenografts and verified the aforementioned in vitro findings [81]. These studies revealed the antitumor activity of quercetin, indicating that it is an attractive antitumor drug. Procyanidin B1 (64) was identified as an effective specific inhibitor that inhibits the Kv10.1 pathway in a concentration-dependent manner, thereby inhibiting HuH-7 and HepG2 cell migration and proliferation. In vivo, 15 mg/kg procyanidin B1 significantly inhibited tumor growth, with an inhibition rate of approximately 60.25%. Moreover, compared with cisplatin, procyanidin B1 has no side effects on normal metabolism in mice [82]. Therefore, procyanidin B1 is a promising anti-tumor drug. Procyanidin B1 is a tannin component in T. chinensis, but its content has not been quantitatively analyzed. Further research is required to determine whether it is an anti-tumor active component of T. chinensis. Procyanidin C1(65), another tannin in T. chinensis, promotes apoptosis in MCF-7 and MDA-MB-231 breast cancer cells by inducing DNA damage, arresting the cell cycle, reducing Bcl-2 levels, and increasing the expression of BAX and caspases 3 and 9 [83]. Glycosides in different plants were highly cytotoxic to different cancer cell lines in early preclinical studies [84]. Studies on the anticancer activity of glycosides isolated from T. chinensis will be of great value; however, whether they will affect normal cells and verify their safety for normal cells remains to be determined. At present, research on the anti-tumor properties of T. chinensis mainly focuses on small molecular substances such as flavonoids, alkaloids, and other compounds, whereas research on macromolecular substances such as toxic proteins and lectins is limited. Studies have confirmed that lectins from T. chinensis have anti-tumor effects. The MTT method showed that the IC50 values of lectins in BEL-7402 liver cancer cells and MGC-823 gastric cancer cells were 24.2 μg/mL and 20.9 μg/mL, respectively. The inhibitory rate of lectin on liver and gastric cancer cells increases with increasing drug concentration within a certain range [85, 86]. In this experiment, the lectins from T. chinensis were believed to have a certain anti-tumor effect, but the lectins used were of low purity and needed to be further separated and purified to detect a single component. In addition, this study was carried out in a cell model, and the detailed mechanism of the anti-tumor effect of lectins from T. chinensis remains to be investigated further in vivo. In conclusion, flavonoids, tannins, and lectins in T. chinensis have anti-tumor effects, and their mechanism is mainly related to the degradation of cell cycle proteins and the inhibition of cell proliferation and migration through certain signaling pathways.
Antimicrobial and antiviral effects
The T. chinensis extract has antiviral effects. Wen et al. evaluated the anti-SARS-CoV activity of T. chinensis in Vero E6 cells. The effective concentration of the T. chinensis extract for inhibiting the SARS coronavirus was between 25 and 200 μg/ml. Although the EC50 values of the T. chinensis extract (EC50 = 5.39 μg/ml) were approximately three times higher than those of valinomycin (VAL) (EC50 = 1.87 μg/ml), the significantly lower EC50 value (< 10 μg/ml) is interesting. Moreover, the potential toxicity of T. chinensis extract to Vero E6 cells was evaluated using the MTT assay with the CC50 value as an evaluation index. The CC50 value of the T. chinensis extract (CC50 > 500 μg/ml) was even higher than that of the positive control valinomycin (CC50 = 75.01 μg/ml), indicating that the T. chinensis extract did not interfere with cell growth and was generally safe for host cells [87]. Therefore, T. chinensis extract can inhibit the replication of SARS coronavirus with no or low toxicity to Vero E6 cells; therefore, it may be a useful candidate for future anti-SARS therapy. Moreover, a total of 150 μg/50 μL of T. chinensis aqueous extract treated with eight hemagglutination units of HBsAg for 4 h had an eightfold inhibitory effect on HbsAg. The results showed that T. chinensis was a natural inhibitor of the hepatitis B virus [88].
Various chemical constituents of T. chinensis exhibit antimicrobial and antiviral activities. In a duck hepatitis B virus (DHBV) model, chlorogenic acid (61) significantly reduced DHBV viremia in DHBV-infected ducklings, and its inhibitory efficacy was superior to that of lamivudine. Caffeic acid (60) also reduced DHBV viremia, but quinic acid (50) only slightly altered it. In a cellular model, all three compounds inhibited HBV DNA replication and HBsAg production [89]. The results showed that the three compounds can potentially inhibit the hepatitis B virus; however, further research is required to explore its mechanism of action. Studies have confirmed that toddacoumaquinone (58) is a potential inhibitor of the SARS coronavirus protease. It has a significant inhibitory effect on the main protease of SARS-CoV with a binding energy of − 7.8 kcal/mol [90]. Caffeic acid (60) is widely used to combat chronic infections induced by fungi, bacteria, and viruses [91, 92]. Current studies have mainly focused on in vitro models, and the antimicrobial and antiviral effects and their mechanisms in in vivo models must be evaluated further.
Diuretic effect
Diuretics are one of the most commonly used drugs that increase urine flow and induce urinary sodium loss, and are used to treat hypertension, congestive heart failure, and edema [93]. However, the long-term use of diuretics has shown toxic effects on the human body. Contrastingly, the diuretic effect of traditional Chinese medicine is obvious, lasts longer, and does not cause electrolyte disorders; therefore, traditional Chinese medicines and Chinese medicine compound preparations with diuretic effects must be developed [94]. T. chinensis is mostly used to dispel wind dampness in clinical settings. Therefore, it has the potential to promote diuresis. Avicularin is a flavonoid isolated from Taxilli Herba, with confirmed diuretic effect. Intravenous injection of 0.5 mg/kg avicularin to anesthetized dogs can cause diuresis, and the diuretic effect becomes more significant as the dose increases. Gavage or injection of 34 mg/kg avicularin in rats also has a significant diuretic effect [95, 96]. Aldosterone, angiotensin II, antidiuretic hormone, and atrial natriuretic hormone are the four hormones in the renin-angiotensin system that are closely linked to fluid balance. Many diuretic experiments will measure these indices, so they can provide a reference for subsequently studying the diuretic mechanism of T. chinensis. Triterpenoids and polyphenols have been clinically proven to have diuretic effects and have certain reference values for research on the diuretic effect of T. chinensis [97, 98]. Polyphenols, including flavonoids and phenolic acids, are abundant in T. chinensis and are associated with antioxidant, anti-inflammatory, and anti-tumor effects. In the future, experimental studies of these polyphenols in T. chinensis should be conducted to determine whether they also have diuretic effects. Although only few studies have been conducted on the diuretic properties of T. chinensis, its potential is worth exploring.
Antihypertensive effect
Millions of people have been estimated to die annually from cardiovascular diseases, particularly myocardial infarction and stroke [99]. Population growth and aging have led to a gradual increase in cardiovascular morbidity and mortality [100]. In clinical practice, T. chinensis is often used in combination to treat hypertension due to hyperactivity of the “liver yang type” with dizziness, tinnitus, anorexia, and dreaminess as the main symptoms, based on the traditional efficacy of “nourishing the liver and kidney, regulating blood vessels, and expelling wind” [101]. Recently, the pharmacological effects of T. chinensis in lowering blood pressure have been investigated. Zhang et al. investigated the antihypertensive activity of T. chinensis from six different hosts in spontaneously hypertensive rats (SHRs). Taxilli Herba from five hosts can reduce blood pressure; however, the effect varies depending on the host. The antihypertensive effects of these five hosts were as follows: Salix babylonica L., Liquidambar formosana Hance, Morus alba L., Castanea mollissima Bl., and Camellia oleifera Abel. The high-dose (5.9 g/kg body weight) and low-dose (1.48 g/kg body weight) Taxilli Herba extract from Morus alba L. showed a significant antihypertensive effect similar to that of captopril on SHRs, and the molecular mechanism may be related to increased SOD activity, increased serum NO release, and decreased plasma Ang II and ET-1 levels [102]. T. chinensis from Camellia oleifera Abel. and Nerium oleander L. showed obvious toxicity, which may cause damage to the body of SHR rats, resulting in no antihypertensive effect. Therefore, the relationship between blood pressure reduction and toxicity requires further study. Quercetin also had an obvious antihypertensive effect on renal hypertensive rats, and the effect was approximately equivalent to that of verapamil. Quercetin-treated rats had a decreased fluorescence density ratio of free calcium ions in the renal artery vascular ring smooth muscle cells, suggesting that the hypotensive mechanism is related to a reduction in the concentration of free calcium ions in renal artery smooth muscle cells. To further explore its in-depth antihypertensive mechanism, the whole-cell patch-clamp technique was used to observe the effect of quercetin on the relevant channel currents on the membrane of rat renal artery smooth muscle cells [103]. Furthermore, the antihypertensive effect mediated by quercetin is related to the regulation of renal arachidonic acid metabolism. In the future, it may be used as an independent and cost-effective complementary approach to treat hypertension and prevent organ damage caused by uncontrolled hypertension [104].
Antihyperglycemic effect
Diabetes is a serious, chronic disease that develops when the pancreas does not produce enough insulin or when the body does not utilize insulin effectively [105]. The vast majority of patients with metabolic hyperglycemic diseases have type 2 diabetes [106]. Chen et al. applied total flavonoids (100, 200, and 400 mg/kg body weight) from T. chinensis to a streptozotocin (STZ)-induced hyperglycemia mouse model, and the results showed that 200 and 400 mg/kg total flavonoids reduced serum TC and TG levels and increased serum HDL-G levels in mice. The hypoglycemic effect of the total flavonoids (400 mg/kg body weight) was similar to that of metformin (60 mg/kg body weight), a known hypoglycemic compound. The results suggested that T. chinensis prevented and treated hyperglycemia and its complications, which provided a new idea for preventing and treating hyperglycemia using traditional Chinese medicine [107]. However, the mechanism of hypoglycemic activity is not fully understood, nor does it demonstrate the potential of T. chinensis as a new therapeutic drug. Meng et al. then studied the mechanism through which the total flavonoids from T. chinensis decrease blood sugar levels in STZ-induced diabetic mice. In vitro experiments revealed that total flavonoids inhibited the activity of α-glucosidase and α-amylase in a dose-dependent manner. The inhibition rate of total flavonoids on α-glucosidase was similar to that of acarbose, but the inhibition rate of α-amylase was much lower than that of acarbose, a well-known α-glucosidase inhibitor. Therefore, total flavonoids are strong α-glucosidase inhibitors and weaker α-amylase inhibitors. After four weeks of treatment with total flavonoids (150, 300, and 600 mg/kg body weight) in the STZ-induced hyperglycemia mouse model, the blood glucose content of mice in the high-dose group (600 mg/kg body weight) was close to that of mice in the metformin (60 mg/kg body weight) group. Total flavonoids significantly reduced blood sugar levels and enhanced glucose tolerance, indicating that insulin resistance in diabetic mice was enhanced. Simultaneously, after administration, the liver glycogen content, SOD activity, and thymus index increased, while MDA content decreased, suggesting that the hypoglycemic mechanism of total flavonoids in T. chinensis may be related to the inhibition of lipid peroxidation in mice, protection of thymus atrophy, and improvement of insulin resistance in diabetic mice [108]. The authors verified the hypoglycemic effect of T. chinensis using in vitro and in vivo experiments and clarified the potential of T. chinensis as an antidiabetic drug, pointing out directions for future experimental research. T. chinensis can also increase glucose consumption in human HepG2 cells by promoting the metabolism of peripheral tissues and improving the sensitivity of liver cells to insulin [109]. Luo et al. identified that the alcoholic extract of T. chinensis (30, 15, 7.5 g/kg body weight) treatment significantly ameliorated hyperglycemia and liver and kidney complications and protected liver and kidney function in an STZ-induced hyperglycemia mouse model. The mechanism may be related to the improvement of immune function, upregulation of anti-apoptotic factors, and downregulation of apoptosis-promoting and inflammation-promoting factor expression to maintain the functional state of hepatocytes and decrease the degree of renal cell injury [110]. Although this experiment showed the hypoglycemic effect and possible mechanism of action of T. chinensis, its dosage is relatively large, and high-dose medication may cause toxicity and side effects. It cannot reflect the real situation of a drug in the human body, and its clinical reference value is low. The antioxidant and antihyperglycemic effects of caffeic acid (60) have been demonstrated in STZ-induced mouse models of diabetes, and in the future, it could be considered a dietary supplement for diabetes [111].
Other effects
In addition, T. chinensis was found to inhibit fatty acid synthase and decrease weight in rats in a preliminary study; the pharmacologically active ingredient was avicularin [8]. Therefore, avicularin may act as an anti-obesity and anti-dietary flavonoid. In future studies, avicularin should be assessed in vivo, and its mechanism of action should be investigated [112]. Recently, catechins (12) and their derivatives have attracted public attention because of their anti-tumor, antioxidative, and antimicrobial activities, in addition to easy availability, few toxic effects, and low cost [76, 113, 114]. Catechins have been shown to have nephroprotective activity and can prevent kidney damage caused by nephrotoxic drugs [115, 116]. In future studies, the safety and efficacy of catechins in treating acute kidney injury should be further explored to provide reference values for clinical treatment. Previously, T. chinensis was shown to reverse scopolamine-induced memory impairment in mice [117]. It is speculated to protect the nerves and enhance memory. However, no relevant research has been conducted in recent years. Therefore, further experiments are urgently required to clarify the mechanisms of action.
Toxicology
To date, reports on T. chinensis toxicity are mainly related to liver and embryo toxicity. In the process of growth and development, the host transfers its characteristic components to T. chinensis, and if these components are toxic, they will affect the safety of T. chinensis, so the toxicity of T. chinensis is closely related to the host. Xia et al. investigated the acute toxicity and liver damage caused by water extracts of T. chinensis from six different hosts in zebrafish. The results showed that T. chinensis from M. alba was not hepatotoxic to zebrafish, whereas T. trichocarpum, C. oleifera, S. babylonica, M. azedarach, and N. indicum showed a certain degree of liver damage in zebrafish [118]. The dosage of drugs for the safe treatment of pregnant women and safe clinical use of T. chinensis have been investigated [119]. T. chinensis has certain genetic toxicity when the dosage is 20 g/kg body weight, and it has potential embryonic development toxicity when it reaches 40 g/kg body weight. In addition, no teratogenic effect was observed in rat embryos, but high-dose decoction showed embryo toxicity [120]. Since few studies have analyzed the toxicological data of T. chinensis, a thorough evaluation of the toxicological performance of this plant is needed.
Conclusion and perspectives
As a traditional Chinese medicine, T. chinensis is abundantly available, contains various chemical components, and shows important pharmacological activities (Fig. 5). This paper summarizes the published research results on T. chinensis and reviews the botany, traditional uses, phytochemistry, pharmacology, and toxicity. The plant has been used in clinical practice since the reign of the Eastern Han dynasty. T. chinensis is traditionally used to treat various diseases, including joint swelling and pain, rheumatism, threatened abortion, stroke, and hypertension. The Duhuo Jisheng, Qisang Yigan, and Sangge Jiangzhi pills, among other preparations, have been widely used in traditional prescriptions and have shown good clinical effects. Phytochemical composition is an important factor in determining biological activity and traditional uses. Recently, researchers have isolated a variety of compounds from T. chinensis, among which quercetin has been widely studied, and it is the quality control index stipulated by the pharmacopoeia. T. chinensis has now been shown to possess various pharmacological activities, including anti-inflammatory, antioxidant, anticancer, antiviral, antimicrobial, antihypertensive, and antihyperglycemic activities.
Fig. 5.
Traditional uses, chemical constituents, and pharmacological activities of Taxillus chinensis (DC.) Danser
To date, T. chinensis has been extensively investigated in various fields, and their phytochemical and pharmacological activities studied. However, further work on T. chinensis should focus on the following aspects. First, T. chinensis has a long history of application in China, and classic prescriptions with significant curative effects are available that are widely circulated and can treat various diseases. However, the relationship between traditional applications and modern pharmacological activities has not been sufficiently studied. Therefore, more experiments are required to elucidate the relationship between these compounds and to further discover their potential pharmacological activities. Second, approximately 110 compounds were identified in T. chinensis. However, most of the current studies are qualitative analysis of the compounds, and the exact content of each component in T. chinensis is not clear, which may be one of the future research focuses. Previous research has mainly focused on flavonoids; however, the pharmacological activities and targets of other components remain to be studied. Further exploration of the chemical components of T. chinensis is required to identify additional active components. What’s more, in practice, T. chinensis is often confused with mistletoe, resulting in market confusion and poor drug effect. In order to better control the quality of T. chinensis, it is necessary to establish a standardized fingerprint in the future. Third, although several pharmacological actions of T. chinensis have been reported, its exact active components and mechanisms are not clear, and pharmacological analysis is sometimes inconsistent with clinical application, resulting in confusion. Therefore, exploring the pharmacological action and mechanism of a single bioactive component will be the focus of future research. Finally, toxicological studies should be conducted to determine the safe dose of T. chinensis for clinical use, and clinical trials should be conducted to evaluate the efficacy of pharmacological actions in humans. Although this paper reviewed the botany, traditional application, phytochemistry, pharmacological activity and toxicity of T. chinensis, it lacked a summary of the pharmacokinetic research and clinical application. Clinical trials are essential to verify the safety and efficacy of drugs. In the future, clinical trials are necessary to develop more preparations related to T. chinensis. With the development of pharmaceutical chemistry and the improvement of human health level, the requirement of pharmacokinetics is increasingly high. In order to expand the market prospect of T. chinensis, future research can focus on the pharmacokinetics of the main active ingredients.
Acknowledgements
Not applicable.
Abbreviations
- T. chinensis
Taxillus chinensis (DC.) Danser
- HIF-1
Hypoxia inducible factor-1
- TNF
Tumor necrosis factor
- NF-κB
Nuclear factor kappa-B
- BACH1
Basic leucine zipper transcription factor 1
- MAF
Minor allele frequency
- Nrf2
Nuclear factor erythroid-2 related factor 2
- HO-1
Heme oxygenase-1
- DPPH
1,1-Diphenyl-2-picrylhydrazyl
- Bcl-2
B-cell lymphoma-2
- MTT
3-(4,5-Dimethyl-2-thiazolyl)-2,5-diphenyl tetrazolium bromide
- DHBV
Duck hepatitis B virus
- SHRs
Spontaneously hypertensive rats
- STZ
Streptozotocin
- iNOS
Inducible nitric oxide synthase
- CC50
The half-maximal cytotoxic concentration
- EC50
Concentration for 50% of maximal effect
- IC50
The half maximal inhibitory concentration
- LPS
Lipopolysaccharide
- COX-2
Cyclooxygenase 2
- p-PI3K
Phosphorylated phosphatidylinositol 3 kinase
- p-AKT
Phosphorylated AKT
Author contributions
MQ, JW, AW, LW, QH and XY contributed to the study conception and design. Conceptualization, material preparation, data collection and analysis were performed by MQ, QH, XY, LY, YT, JD, JL and HH. The draft of the manuscript was written by MQ, QH and XY. CZ, DQ, WZ, LW, AW and JW revised the manuscript. All authors read and approved the final manuscript.
Funding
This research was funded by grants from the National Natural Science Foundation of China [Grant Nos. 82074129, 81903829, and 81804221], the Science and Technology Planning Project of Sichuan Province, China [Grant Nos. 2022YFS0620, 2022JDJQ0061, 2019YJ0484, and 2019YJ0473], Science and Technology Program of Luzhou, China [Grant Nos. 2019LZXNYD-J11, 2019LZXNYDJ05, 2020LZXNYDZ03 and 2020LZXNYDP01]. Southwest Medical University (Nos. 2021ZKZD015, 2021ZKZD018, and 2021ZKMS046).
Availability of data and materials
All data generated or analyzed during this study are included in this published article [and its additional files].
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The manuscript has been approved by all authors for publication.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Mi Qin, Qianqian Huang, and Xin Yang are contributed equally to this work
Contributor Information
Long Wang, Email: wanglongsdu1226@163.com.
Anguo Wu, Email: wag1114@foxmail.com.
Jianming Wu, Email: jianmingwu@swmu.edu.cn.
References
- 1.Wagner H, Püls S, Barghouti T, et al. Herba Taxilli-Sangjisheng. Chromatographic fingerprint analysis of herbal medicines. Springer; 2017. pp. 63–70. [Google Scholar]
- 2.Zhao ZZ. An illustrated Chinese materia medica in Hong Kong. World Scientific; 2004. [Google Scholar]
- 3.Liu B, Zhang Y, Shi Y. Complete chloroplast genome sequence of Taxillus chinensis (Loranthaceae): a hemiparasitic shrub in South China. Mitochondrial DNA B Resour. 2019;4(2):3077–3078. doi: 10.1080/23802359.2019.1666680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shen P, Lin W, Ba X, et al. Quercetin-mediated SIRT1 activation attenuates collagen-induced mice arthritis. J Ethnopharmacol. 2021;279:114213. doi: 10.1016/j.jep.2021.114213. [DOI] [PubMed] [Google Scholar]
- 5.Yang M, Luo J, Li Y, et al. Systems pharmacology-based research on the mechanism of Tusizi-Sangjisheng herb pair in the treatment of threatened abortion. Biomed Res Int. 2020;2020:4748264. doi: 10.1155/2020/4748264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang Y, Deng M, Zhang SY, et al. Parasitic loranthus from Loranthaceae rather than Viscaceae potently inhibits fatty acid synthase and reduces body weight in mice. J Ethnopharmacol. 2008;118(3):473–478. doi: 10.1016/j.jep.2008.05.016. [DOI] [PubMed] [Google Scholar]
- 7.Liu CY, Lin YC, Deng JS, et al. Antioxidant, anti-inflammatory, and antiproliferative activities of Taxillus sutchuenensis. Am J Chin Med. 2012;40(2):335–348. doi: 10.1142/S0192415X12500267. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y, Zhang SY, Ma XF, et al. Potent inhibition of fatty acid synthase by parasitic loranthus [Taxillus chinensis (DC.) Danser] and its constituent avicularin. J Enzyme Inhib Med Chem. 2006;21(1):87–93. doi: 10.1080/14756360500472829. [DOI] [PubMed] [Google Scholar]
- 9.Zhu KX, Su BW, Zhao MH, et al. Research progress on the Taxilli Herba to strengthen muscles and bones. J China Prescr Drug. 2018;16(07):25–26. [Google Scholar]
- 10.Commission CP. Chinese pharmacopoeia. Beijing: People’s Medical Publishing House; 2020
- 11.Hu XM, Zhang WK, Zhu QS. Zhonghua Bencao. Shanghai: Shanghai Science and Technology Publications; 1998. pp. 225–226. [Google Scholar]
- 12.Wu N, Li L, Cai ZC, et al. Quality evaluation of Taxilli Herba from different hosts based on simultaneous determination of multiple bioactive constituents combined with multivariate statistical analysis. Molecules. 2021;26(24):7490. doi: 10.3390/molecules26247490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li YH, Ruan JL, Chen SL, et al. Authentication of Taxillus chinensis using DNA barcoding technique. J Med Plants Res. 2010;4(24):2706–2709. doi: 10.5897/JMPR09.677. [DOI] [Google Scholar]
- 14.Wei SG, Pan LM, He LL, et al. Study on the breeding technique of Taxillus chinensis (DC.) Danser. J Guangxi Academy Sci. 2019;35(01):51–55. doi: 10.13657/j.cnki.gxkxyxb.20190123.006. [DOI] [Google Scholar]
- 15.Wu P, Sun X, Sun F. Shen nong ben cao jing: Shang wu yin shu guan; 1955.
- 16.He J. Sheng Cao Yao Xing Bei Yao: Huaxia Publishing House. Beijing; 1999.
- 17.Huang GX, Wang SM. Ben cao qiu zhen: Zhongguo Zhong yi yao chu ban she; 1997.
- 18.Zhang L, Zhao XQ, Pei XF. Ben jing feng yuan: Zhongguo Zhong yi yao chu ban she; 1996.
- 19.Zhen Q, Shang ZJ. Yao Xing Lun. Heifei: Anhui Science and Technology Publishing House; 2006. p. 79. [Google Scholar]
- 20.Qu F, Zhou J. Treating threatened abortion with Chinese herbs: a case report. Phytother Res. 2006;20(10):915–916. doi: 10.1002/ptr.1979. [DOI] [PubMed] [Google Scholar]
- 21.Ding J, Tan X, Song K, et al. Bushen Huoxue Recipe alleviates implantation loss in mice by enhancing estrogen-progesterone signals and promoting decidual angiogenesis through FGF2 during early pregnancy. Front Pharmacol. 2018;9:437. doi: 10.3389/fphar.2018.00437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou J, Li LS, Zhou Q, et al. The role of quercetin in the treatment of spontaneous abortion and its molecular mechanism. J Tradit China Med. 2020;61(13):1188–1193. doi: 10.13288/j.11-2166/r.2020.13.016. [DOI] [Google Scholar]
- 23.Lan M. Southern Yunnan Materia Medica. Kunming: Yunnan’s Medical Publishing House; 2000. p. 13. [Google Scholar]
- 24.Yuan JH, Wu N, Wang WX, et al. Analysis on the difference of chemical constituents in Taxilli Herba from different host plants. Nat Prod Res Dev. 2022;33(07):1119–1128. doi: 10.16333/j.1001-6880.2022.7.004. [DOI] [Google Scholar]
- 25.Lu SH, Gan YY, Tang L, et al. Evaluation of the quality of Taxillus chinensis from different hosts sources by HPLC fingerprint combined with chemometrics. China Pharm. 2020;31(07):794–799. doi: 10.6039/j.issn.1001-0408.2020.07.06. [DOI] [Google Scholar]
- 26.Hostetler GL, Ralston RA, Schwartz SJ. Flavones: food sources, bioavailability, metabolism, and bioactivity. Adv Nutr. 2017;8(3):423–435. doi: 10.3945/an.116.012948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yuan J, Li L, Cai Z, et al. Qualitative analysis and componential differences of chemical constituents in Taxilli Herba from different hosts by UFLC-Triple TOF-MS/MS. Molecules. 2021 doi: 10.3390/molecules26216373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li L, Teng J, Zhu Y, et al. Metabolomics study of flavonoids of Taxillus chinensis on different hosts using UPLC-ESI-MS/MS. Molecules. 2021;26(24):7681. doi: 10.3390/molecules26247681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhang X, Liu C, Nepal S, et al. A hybrid approach for scalable sub-tree anonymization over big data using MapReduce on cloud. J Comput Syst Sci. 2014;80(5):1008–1020. doi: 10.1016/j.jcss.2014.02.007. [DOI] [Google Scholar]
- 30.Maleki SJ, Crespo JF, Cabanillas B. Anti-inflammatory effects of flavonoids. Food Chem. 2019;299:125124. doi: 10.1016/j.foodchem.2019.125124. [DOI] [PubMed] [Google Scholar]
- 31.Liu SS, Liu Q, He CN, et al. Application history and modern research progress of Taxillus chinensis herb tea. Mod Chin Med. 2019;21(02):147–153. doi: 10.13313/j.issn.1673-4890.20180920006. [DOI] [Google Scholar]
- 32.Andres S, Pevny S, Ziegenhagen R, et al. Safety aspects of the use of quercetin as a dietary supplement. Mol Nutr Food Res. 2018;62(1):1700447. doi: 10.1002/mnfr.201700447. [DOI] [PubMed] [Google Scholar]
- 33.Satari A, Ghasemi S, Habtemariam S, et al. Rutin: a flavonoid as an effective sensitizer for anticancer therapy; insights into multifaceted mechanisms and applicability for combination therapy. Evid Based Complement Altern Med. 2021;2021:9913179. doi: 10.1155/2021/9913179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Valentova K, Vrba J, Bancirova M, et al. Isoquercitrin: pharmacology, toxicology, and metabolism. Food Chem Toxicol. 2014;68:267–282. doi: 10.1016/j.fct.2014.03.018. [DOI] [PubMed] [Google Scholar]
- 35.Bialecka-Florjanczyk E, Fabiszewska A, Zieniuk B. Phenolic acids derivatives - biotechnological methods of synthesis and bioactivity. Curr Pharm Biotechnol. 2018;19(14):1098–1113. doi: 10.2174/1389201020666181217142051. [DOI] [PubMed] [Google Scholar]
- 36.Valanciene E, Jonuskiene I, Syrpas M, et al. Advances and prospects of phenolic acids production, biorefinery and analysis. Biomolecules. 2020;10(6):874. doi: 10.3390/biom10060874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li S, Xu M, Niu Q, et al. Efficacy of procyanidins against in vivo cellular oxidative damage: a systematic review and meta-analysis. PLoS ONE. 2015;10(10):e139455. doi: 10.1371/journal.pone.0139455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee Y. Cancer chemopreventive potential of procyanidin. Toxicol Res. 2017;33(4):273–282. doi: 10.5487/TR.2017.33.4.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gonzalez-Abuin N, Pinent M, Casanova-Marti A, et al. Procyanidins and their healthy protective effects against type 2 diabetes. Curr Med Chem. 2015;22(1):39–50. doi: 10.2174/0929867321666140916115519. [DOI] [PubMed] [Google Scholar]
- 40.Ding B, Dai Y, Hou YL, et al. Four new hemiterpenoid derivatives from Taxillus chinensis. Fitoterapia. 2013;86:1–5. doi: 10.1016/j.fitote.2013.01.017. [DOI] [PubMed] [Google Scholar]
- 41.Dong L. Study on salicin content correlation between Taxilli Herba and their willow host plants. J Med Plants Res. 2012;6(12):2474–2477. doi: 10.5897/JMPR11.1735. [DOI] [Google Scholar]
- 42.Hildebrandt TM, Nunes NA, Araujo WL, et al. Amino acid catabolism in plants. Mol Plant. 2015;8(11):1563–1579. doi: 10.1016/j.molp.2015.09.005. [DOI] [PubMed] [Google Scholar]
- 43.Yamaguchi Y, Yamamoto K, Sato Y, et al. Combination of aspartic acid and glutamic acid inhibits tumor cell proliferation. Biomed Res. 2016;37(2):153–159. doi: 10.2220/biomedres.37.153. [DOI] [PubMed] [Google Scholar]
- 44.Oliveira GP, de Abreu MG, Pelosi P, et al. Exogenous glutamine in respiratory diseases: myth or reality? Nutrients. 2016;8(2):76. doi: 10.3390/nu8020076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ren W, Bin P, Yin Y, et al. Impacts of amino acids on the intestinal defensive system. Adv Exp Med Biol. 2020;1265:133–151. doi: 10.1007/978-3-030-45328-2_8. [DOI] [PubMed] [Google Scholar]
- 46.Moghadamtousi SZ, Kamarudin MN, Chan CK, et al. Phytochemistry and biology of Loranthus parasiticus Merr, a commonly used herbal medicine. Am J Chin Med. 2014;42(1):23–35. doi: 10.1142/S0192415X14500025. [DOI] [PubMed] [Google Scholar]
- 47.Li XF, Fang RZ, Feng H, et al. Study on the mechanism of Taxillus chinensis (DC.) Danser of tonifying liver and kidney, strengthening muscles and bones based on network pharmacology. Chin J Ethnomed Ethnophar. 2021;30(06):16–26. [Google Scholar]
- 48.Wang W, Zheng H, Zheng M, et al. Protective effect of avicularin on rheumatoid arthritis and its associated mechanisms. Exp Ther Med. 2018;16(6):5343–5349. doi: 10.3892/etm.2018.6872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhuo ZM, Fan ZC, Guo X. Effect of herba taxilli extracts combined with miR-375 on viability and apoptosis of osteoarthritic chondrocytes. Chin J Pathophysiol. 2020;36(06):1082–1088. doi: 10.3969/j.issn.1000-4718.2020.06.017. [DOI] [Google Scholar]
- 50.Zhao Y. Observation of the clinical efficacy of renal and hepatic thinning in the treatment of chronic pelvic inflammatory disease. Aisa-Pac Tradit Med. 2015;11(01):84–85. doi: 10.11954/ytctyy.201501041. [DOI] [Google Scholar]
- 51.Wu JY, Zhang W, Lei Q. Experience in the treatment of chronic glomerulonephritis. Henan Tradit Med. 2012;32(2):182–183. doi: 10.16367/j.issn.1003-5028.2012.02.031. [DOI] [Google Scholar]
- 52.Zhang L, Ravipati AS, Koyyalamudi SR, et al. Antioxidant and anti-inflammatory activities of selected medicinal plants containing phenolic and flavonoid compounds. J Agric Food Chem. 2011;59(23):12361–12367. doi: 10.1021/jf203146e. [DOI] [PubMed] [Google Scholar]
- 53.Blaser H, Dostert C, Mak TW, et al. TNF and ROS crosstalk in inflammation. Trends Cell Biol. 2016;26(4):249–261. doi: 10.1016/j.tcb.2015.12.002. [DOI] [PubMed] [Google Scholar]
- 54.Lee HN, Shin SA, Choo GS, et al. Anti-inflammatory effect of quercetin and galangin in LPS-stimulated RAW264.7 macrophages and DNCB-induced atopic dermatitis animal models. Int J Mol Med. 2018;41(2):888–898. doi: 10.3892/ijmm.2017.3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Guan Q, Zhang H. Study on anti-inflammatory action and analgesic effect of single antirheumatic Chinese Medicine. J Clin Ration Drug Use. 2012;5(19):6–7. doi: 10.15887/j.cnki.13-1389/r.2012.19.020. [DOI] [Google Scholar]
- 56.Palace VP, Khaper N, Qin Q, et al. Antioxidant potentials of vitamin A and carotenoids and their relevance to heart disease. Free Radic Biol Med. 1999;26(5–6):746–761. doi: 10.1016/s0891-5849(98)00266-4. [DOI] [PubMed] [Google Scholar]
- 57.Ozben T. Antioxidant supplementation on cancer risk and during cancer therapy: an update. Curr Top Med Chem. 2015;15(2):170–178. doi: 10.2174/1568026615666141209160918. [DOI] [PubMed] [Google Scholar]
- 58.Kattoor AJ, Pothineni N, Palagiri D, et al. Oxidative stress in atherosclerosis. Curr Atheroscler Rep. 2017;19(11):42. doi: 10.1007/s11883-017-0678-6. [DOI] [PubMed] [Google Scholar]
- 59.Xu X, Jin K, Bais AS, et al. Uncompensated mitochondrial oxidative stress underlies heart failure in an iPSC-derived model of congenital heart disease. Cell Stem Cell. 2022;29(5):840–855. doi: 10.1016/j.stem.2022.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lignitto L, LeBoeuf SE, Homer H, et al. Nrf2 activation promotes lung cancer metastasis by inhibiting the degradation of bach1. Cell. 2019;178(2):316–329. doi: 10.1016/j.cell.2019.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Saha S, Panieri E, Suzen S, et al. The interaction of flavonols with membrane components: potential effect on antioxidant activity. J Membr Biol. 2020;253(1):57–71. doi: 10.1007/s00232-019-00105-1. [DOI] [PubMed] [Google Scholar]
- 62.Catarino MD, Alves-Silva JM, Pereira OR, et al. Antioxidant capacities of flavones and benefits in oxidative-stress related diseases. Curr Top Med Chem. 2015;15(2):105–119. doi: 10.2174/1568026615666141209144506. [DOI] [PubMed] [Google Scholar]
- 63.Huo LN, Chen R, Liao YF, et al. Antioxidant activity of the extract from Taxillus chinensis parasitized on Clausena lansium (Lour.) Skeels. Hubei Agric Sci. 2014;53(11):2631–2633. doi: 10.14088/j.cnki.issn0439-8114.2014.11.003. [DOI] [Google Scholar]
- 64.Chen BH, Lai JJ, Zheng Q, et al. Effects of different extraction solvents on the antioxidant activities of leaves extracts of Scurrula parasitica. J Fujian Norm Univ. 2010;26(1):86–90. [Google Scholar]
- 65.Jiao R, Liu Y, Gao H, et al. The anti-oxidant and antitumor properties of plant polysaccharides. Am J Chin Med. 2016;44(3):463–488. doi: 10.1142/S0192415X16500269. [DOI] [PubMed] [Google Scholar]
- 66.Luo Y, Peng B, Wei W, et al. Antioxidant and anti-diabetic activities of polysaccharides from guava leaves. Molecules. 2019;24(7):1343. doi: 10.3390/molecules24071343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zeng P, Li J, Chen Y, et al. The structures and biological functions of polysaccharides from traditional Chinese herbs. Prog Mol Biol Transl Sci. 2019;163:423–444. doi: 10.1016/bs.pmbts.2019.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zhang L, Koyyalamudi SR, Jeong SC, et al. Immunomodulatory activities of polysaccharides isolated from Taxillus chinensis and Uncaria rhyncophylla. Carbohydr Polym. 2013;98(2):1458–1465. doi: 10.1016/j.carbpol.2013.07.060. [DOI] [PubMed] [Google Scholar]
- 69.Bar J, Onn A. Combined anti-proliferative and anti-angiogenic strategies for cancer. Expert Opin Pharmacother. 2008;9(5):701–715. doi: 10.1517/14656566.9.5.701. [DOI] [PubMed] [Google Scholar]
- 70.Barros PP, Eisinger A, GonCalves G, et al. Oral rutin suspension intervene in hepatic hyperplasia in rats. Arq Gastroenterol. 2020;57(3):296–299. doi: 10.1590/S0004-2803.202000000-54. [DOI] [PubMed] [Google Scholar]
- 71.Ezzati M, Yousefi B, Velaei K, et al. A review on anti-cancer properties of quercetin in breast cancer. Life Sci. 2020;248:117463. doi: 10.1016/j.lfs.2020.117463. [DOI] [PubMed] [Google Scholar]
- 72.Choi BY. Biochemical basis of anti-cancer-effects of phloretin-A natural dihydrochalcone. Molecules. 2019;24(2):278. doi: 10.3390/molecules24020278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Park GH, Song HM, Park SB, et al. Anti-proliferative activity of ethanol extracts from Taxilli Ramulus (Taxillus chinensis (DC.) Danser) through cyclin D1 proteasomal degradation in human colorectal cancer cells. Korean J Plant Res. 2017;30(6):640–646. doi: 10.7732/kjpr.2017.30.6.640. [DOI] [Google Scholar]
- 74.Feng HY, Liu Z, Fu ZX. Mechanism and effect of water extract from herba taxilli on the invasion and migration of human colorectal cancer HT-29 cells. Zhejiang Med J. 2020;42(07):666–669. doi: 10.12056/j.issn.1006-2785.2020.42.7.2019-2962. [DOI] [Google Scholar]
- 75.Zhang J, Zhou XX, Liang Y, et al. Study on the anti-leukemia effect of Taxillus chinensis (DC.) Danser in different extraction sites. Lishizhen Med Mater Med Res. 2011;22(10):2452–2454. doi: 10.3969/j.issn.1008-0805.2011.10.059. [DOI] [Google Scholar]
- 76.Yang JH, Hsia TC, Kuo HM, et al. Inhibition of lung cancer cell growth by quercetin glucuronides via G2/M arrest and induction of apoptosis. Drug Metab Dispos. 2006;34(2):296–304. doi: 10.1124/dmd.105.005280. [DOI] [PubMed] [Google Scholar]
- 77.Choi JA, Kim JY, Lee JY, et al. Induction of cell cycle arrest and apoptosis in human breast cancer cells by quercetin. Int J Oncol. 2001;19(4):837–844. doi: 10.3892/ijo.19.4.837. [DOI] [PubMed] [Google Scholar]
- 78.Zizkova P, Stefek M, Rackova L, et al. Novel quercetin derivatives: from redox properties to promising treatment of oxidative stress related diseases. Chem Biol Interact. 2017;265:36–46. doi: 10.1016/j.cbi.2017.01.019. [DOI] [PubMed] [Google Scholar]
- 79.Ghafouri-Fard S, Shabestari FA, Vaezi S, et al. Emerging impact of quercetin in the treatment of prostate cancer. Biomed Pharmacother. 2021;138:111548. doi: 10.1016/j.biopha.2021.111548. [DOI] [PubMed] [Google Scholar]
- 80.Lee TJ, Kim OH, Kim YH, et al. Quercetin arrests G2/M phase and induces caspase-dependent cell death in U937 cells. Cancer Lett. 2006;240(2):234–242. doi: 10.1016/j.canlet.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 81.Maso V, Calgarotto AK, Franchi GJ, et al. Multitarget effects of quercetin in leukemia. Cancer Prev Res (Phila) 2014;7(12):1240–1250. doi: 10.1158/1940-6207.CAPR-13-0383. [DOI] [PubMed] [Google Scholar]
- 82.Na W, Ma B, Shi S, et al. Procyanidin B1, a novel and specific inhibitor of Kv10.1 channel, suppresses the evolution of hepatoma. Biochem Pharmacol. 2020;178:114089. doi: 10.1016/j.bcp.2020.114089. [DOI] [PubMed] [Google Scholar]
- 83.Koteswari LL, Kumari S, Kumar AB, et al. A comparative anticancer study on procyanidin C1 against receptor positive and receptor negative breast cancer. Nat Prod Res. 2020;34(22):3267–3274. doi: 10.1080/14786419.2018.1557173. [DOI] [PubMed] [Google Scholar]
- 84.Khan H, Saeedi M, Nabavi SM, et al. Glycosides from medicinal plants as potential anticancer agents: emerging trends towards future drugs. Curr Med Chem. 2019;26(13):2389–2406. doi: 10.2174/0929867325666180403145137. [DOI] [PubMed] [Google Scholar]
- 85.Zhang LS, Liu SL. Isolation of anti-cancer proteins from Lorathlorace and part property studying. Nat Prod Res Dev. 2006;18(01):43–46. doi: 10.16333/j.1001-6880.2006.01.011. [DOI] [Google Scholar]
- 86.Pan X, Liu SL. Isolation and characterization of antitumor lectins from Chinese herbs Loranthaceae. Nat Prod Res Dev. 2006;18(02):210–213. doi: 10.16333/j.1001-6880.2006.02.007. [DOI] [Google Scholar]
- 87.Wen CC, Shyur LF, Jan JT, et al. Traditional Chinese medicine herbal extracts of Cibotium barometz, Gentiana scabra, Dioscorea batatas, Cassia tora, and Taxillus chinensis inhibit SARS-CoV replication. J Tradit Complement Med. 2011;1(1):41–50. doi: 10.1016/s2225-4110(16)30055-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zheng MS, Zheng YF. Experimental study on the inhibition of hepatitis B virus surface antigen by 1000 kinds of Chinese herbal medicine. J Tradit Chin Med. 1989;11:47–48. doi: 10.13288/j.11-2166/r.1989.11.023. [DOI] [Google Scholar]
- 89.Wang GF, Shi LP, Ren YD, et al. Anti-hepatitis B virus activity of chlorogenic acid, quinic acid and caffeic acid in vivo and in vitro. Antiviral Res. 2009;83(2):186–190. doi: 10.1016/j.antiviral.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 90.Chidambaram SK, Ali D, Alarifi S, et al. In silico molecular docking: evaluation of coumarin based derivatives against SARS-CoV-2. J Infect Public Health. 2020;13(11):1671–1677. doi: 10.1016/j.jiph.2020.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Touaibia M, Jean-Francois J, Doiron J. Caffeic acid, a versatile pharmacophore: an overview. Mini Rev Med Chem. 2011;11(8):695–713. doi: 10.2174/138955711796268750. [DOI] [PubMed] [Google Scholar]
- 92.Khan F, Bamunuarachchi NI, Tabassum N, et al. Caffeic acid and its derivatives: antimicrobial drugs toward microbial pathogens. J Agric Food Chem. 2021;69(10):2979–3004. doi: 10.1021/acs.jafc.0c07579. [DOI] [PubMed] [Google Scholar]
- 93.Buttner S, Koch A, Pfeilschifter J. Diuretic therapy. Dtsch Med Wochenschr. 2019;144(6):387–392. doi: 10.1055/a-0661-4426. [DOI] [PubMed] [Google Scholar]
- 94.Liu WF, Huang XJ, Xia LX, et al. Research progress on functional mechanisms of diuretic antihypertensive herbs. SH J TCM. 2011;45(09):73–78. doi: 10.16305/j.1007-1334.2011.09.031. [DOI] [Google Scholar]
- 95.Wang J. Sang parasitic research overview. J Pract Tradit Chin Intern Med. 2018;32(01):74–77. doi: 10.13729/j.issn.1671-7813.Z20170473. [DOI] [Google Scholar]
- 96.Chen LS. Pharmacological research on Loranthus parasiticus (L.) Merr. Shanxi J Tradit Chin Med. 2000;21(11):520–521. [Google Scholar]
- 97.Christie S, Walker AF, Lewith GT. Flavonoids–a new direction for the treatment of fluid retention? Phytother Res. 2001;15(6):467–475. doi: 10.1002/ptr.1011. [DOI] [PubMed] [Google Scholar]
- 98.Somova LO, Nadar A, Rammanan P, et al. Cardiovascular, antihyperlipidemic and antioxidant effects of oleanolic and ursolic acids in experimental hypertension. Phytomedicine. 2003;10(2–3):115–121. doi: 10.1078/094471103321659807. [DOI] [PubMed] [Google Scholar]
- 99.Layne K, Ferro A. Traditional Chinese medicines in the management of cardiovascular diseases: a comprehensive systematic review. Br J Clin Pharmacol. 2017;83(1):20–32. doi: 10.1111/bcp.13013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Roth GA, Forouzanfar MH, Moran AE, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015;372(14):1333–1341. doi: 10.1056/NEJMoa1406656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Yin P, Li YM, Li XW, et al. Clinical analysis of Liver-Yang hyperactivity type hypertension treatment by Tianma Gouteng Decoction. China Contin Med Educ. 2016;8(16):179–180. doi: 10.3969/j.issn.1674-9308.2016.16.127. [DOI] [Google Scholar]
- 102.Zhang H, Huang FY, Liu RY, et al. Effects of Taxilli Herba from different hosts on lowering blood pressure of spontaneously hypertensive rats. Chin Tradit Pat Med. 2018;40(02):249–254. doi: 10.3969/j.issn.1001-1528.2018.02.001. [DOI] [Google Scholar]
- 103.Hou GJ, Qin XJ, Hou XM, et al. Study on the hypotensive effect and mechanism of quercetin on rats with renal hypertension. Chin J Integr Med Cerebrovasc Dis. 2016;14(02):137–139. doi: 10.3969/j.issn.1672-1349.2016.02.009. [DOI] [Google Scholar]
- 104.Elbarbry F, Abdelkawy K, Moshirian N, et al. The antihypertensive effect of quercetin in young spontaneously hypertensive rats; role of arachidonic acid metabolism. Int J Mol Sci. 2020;21(18):6554. doi: 10.3390/ijms21186554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Campbell JE, Newgard CB. Mechanisms controlling pancreatic islet cell function in insulin secretion. Nat Rev Mol Cell Biol. 2021;22(2):142–158. doi: 10.1038/s41580-020-00317-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tuomilehto J. Definitions of intermediate hyperglycaemia and progression to type 2 diabetes. Lancet Diabetes Endocrinol. 2019;7(4):243–245. doi: 10.1016/S2213-8587(19)30064-6. [DOI] [PubMed] [Google Scholar]
- 107.Chen XQ, Meng TX, Fang ZW, et al. Preliminary study on hypoglycemic effect of total flavonoids from Loranthus parasiticus. Strait Pharm J. 2020;32(07):25–26. [Google Scholar]
- 108.Meng TX, Yuan XL, Liang F, et al. Hypoglycemic effect of total flavonoids from mistletoe on diabetic mice induced by streptozotocin. J Shanxi Univ Chin Med. 2021;44(06):55–60. doi: 10.13424/j.cnki.jsctcm.2021.06.013. [DOI] [Google Scholar]
- 109.Wang N, Zhu Q, Zhou YW, et al. Effects of extract of Herba Taxlli on glucose comsumption in cultured HepG2 cells of human. Chin Arch Tradit Chin Med. 2006;24(03):442–443. doi: 10.13193/j.archtcm.2006.03.60.wangn.028. [DOI] [Google Scholar]
- 110.Luo ZP, Li L, Pan WL, et al. Improvement effects of ethanol extract from Taxillus sutchuenensis on blood glucose level, liver and renal complications in type 2 diabetes mellitus model mice and its mechanism. China Pharm. 2019;30(06):796–801. doi: 10.6039/j.issn.1001-0408.2019.06.16. [DOI] [Google Scholar]
- 111.Orsolic N, Sirovina D, Odeh D, et al. Efficacy of caffeic acid on diabetes and its complications in the mouse. Molecules. 2021;26(11):3262. doi: 10.3390/molecules26113262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Fujimori K. Avicularin, a plant flavonoid, suppresses lipid accumulation through repression of C/EBP alpha-activated GLUT4-mediated glucose uptake in 3T3-L1 cells. J Agric Food Chem. 2013;61(21):5139–5147. doi: 10.1021/jf401154c. [DOI] [PubMed] [Google Scholar]
- 113.Braicu C, Pilecki V, Balacescu O, et al. The relationships between biological activities and structure of flavan-3-ols. Int J Mol Sci. 2011;12(12):9342–9353. doi: 10.3390/ijms12129342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chacko SM, Thambi PT, Kuttan R, et al. Beneficial effects of green tea: a literature review. Chin Med. 2010;5:13. doi: 10.1186/1749-8546-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Diniz L, Elshabrawy HA, Souza M, et al. Catechins: therapeutic perspectives in COVID-19-associated acute kidney injury. Molecules. 2021;26(19):5951. doi: 10.3390/molecules26195951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Khalatbary AR, Khademi E. The green tea polyphenolic catechin epigallocatechin gallate and neuroprotection. Nutr Neurosci. 2020;23(4):281–294. doi: 10.1080/1028415X.2018.1500124. [DOI] [PubMed] [Google Scholar]
- 117.Weon JB, Lee J, Eom MR, et al. The effects of loranthus parasiticus on scopolamine-induced memory impairment in mice. Evid Based Complement Altern Med. 2014;2014:860180. doi: 10.1155/2014/860180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Xia YP, He CH, Chai ZS, et al. Acute toxicity and hepatotoxicity of aqueous extracts of taxilli herba from different hosts in zebrafish model. Chin J Exp Tradit Med Formulas. 2021;27(21):91–97. doi: 10.13422/j.cnki.syfjx.20212125. [DOI] [Google Scholar]
- 119.Liu X, Li LJ, Xu XY, et al. Effects of Morus vulgaris decoction on the growth and development of mouse embryo limb buds and the expression of Tbx2 and BMP-2 genes. J Health Toxicol. 2017;31(02):109–114. doi: 10.16421/j.cnki.1002-3127.2017.02.007. [DOI] [Google Scholar]
- 120.Liu MS, Li XH, Zhang H, et al. Effects of Sangjisheng detection on SD pregnant mice and embryonic development. Chin J Eugen Genet. 2013;21(11):105–107. doi: 10.13404/j.cnki.cjbhh.2013.11.056. [DOI] [Google Scholar]
- 121.Sun SM. Bei Ji Qian Jin Yao Fang. Beijing: People’s Medical Publishing House; 1997. [Google Scholar]
- 122.Zhang XC. Yi Xue Zhong Zhong Can Xi Lu.: Tian Jin Xin Hua Yin Shu Ju. Tian Jin; 1909.
- 123.Liu JYC. Tai Ping Sheng Hui He Ji Ju Fang. People's Medical Publishing House; 2007.
- 124.Li SZ. Bencao gangmu. ZBG. 1995
- 125.Yi LW. Shi Yi De Xiao Fang, vol 266. Seoul: Yŏgang Chulpansa; 1987. p. 317–8.
- 126.Zheng YH. Effects of Duhuo Jisheng Pills combined with celecoxib on inflammatory factors, endothelial function and knee function in elderly patients with knee osteoarthritis. Chin J Gerontol. 2017;37(10):2513–2515. doi: 10.3969/j.issn.1005-9202.2017.10.074. [DOI] [Google Scholar]
- 127.Ji DG, Zhang GQ, Zhang W. Observation of glucosamine hydrochloride combined with Duhuo Jisheng Pill in the treatment of knee osteoarthritis. Chin Foreign Med Res. 2014;12(31):10–12. doi: 10.14033/j.cnki.cfmr.2014.31.085. [DOI] [Google Scholar]
- 128.Zeng FB, Cui XR, Yu ZM, et al. Experimental study on the pharmacodynamics of Miniaoning Granules. Chin J Tradit Med Sci Technol. 2002;9(01):15–16. [Google Scholar]
- 129.Maharajan K, Xia Q, Duan X, et al. Therapeutic importance of Zishen Yutai Pill on the female reproductive health: a review. J Ethnopharmacol. 2021;281:114523. doi: 10.1016/j.jep.2021.114523. [DOI] [PubMed] [Google Scholar]
- 130.Fan D. Clinical observation on 156 cases of chronic hepatitis B treated by Yigan Pill. Hunan J Tradit Chin Med. 2005;21(05):26–27. doi: 10.16808/j.cnki.issn1003-7705.2005.05.012. [DOI] [Google Scholar]
- 131.Du X, Chen XQ, Yang Y, et al. Observation on lipid-lowering effect of Sangge Jiangzhi Pill and Dantian Jiangzhi Pill. Chin J Integr Tradit West Med. 1994;14(01):41–42. [Google Scholar]
- 132.Yang CR, Hu H, Yan J, et al. Clinical study on Yunkang Granules combined with chorionic gonadotrophin in treatment of habitual abortion. Drugs Clin. 2019;34(09):2717–2719. doi: 10.7501/j.issn.1674-5515.2019.09.031. [DOI] [Google Scholar]
- 133.Zhang ZG, Yang SH, Zheng PP. Clinical observation of Yunkang granules combined with dydrogesterone in the treatment of early threatened abortion. Chin Tradit Pat Med. 2016; 27(23): 3229–31. 10.6039/j.issn.1001-0408.2016.23.21.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article [and its additional files].