Abstract
Background:
During the COVID-19 pandemic lockdown, the normal daily routine activities of children were restricted as a result of the need to stay indoors. Consequently, children were forced to attend online classes provided by their educational institutions at their homes. Due to the subsequent increased screen exposure, children have started complaining of blurred vision, headache, and symptoms related to computer vision syndrome (CVS), predisposing them to myopia.
Objective:
To determine the prevalence of CVS symptoms, such as blurring of vision, headache, and watery eyes in children, due to increased screen time during the lockdown period of the COVID-19 pandemic.
Methods:
This was a non-randomized, questionnaire-based study conducted at the ophthalmology department of a tertiary care pediatric hospital. The participants were parents of children aged between 6 and 16 years attending regular school. Enrolled parents were interviewed through a Google Form after completing the online consent in English. Eligible participants were recruited by a circulation of this form through multiple groups on social media, namely, WhatsApp and email.
Results:
A total of 145 parents participated in the study. The children were classified according to the duration of exposure to digital devices ranging from less than 2 h to less than 6 h daily. There was a significant association between the increase in the number of activities and the development of CVS symptoms in children (r = 0.15; P = 0.036).
Conclusion:
COVID-19 lockdown has largely affected the lifestyle of school-going children by significantly decreasing their outdoor activities and increased online exposure to screen, thus predisposing them to myopia, ocular ill health, and increased dry eye symptoms. Increased exposure to online screen was detected during this lockdown period of the COVID-19 pandemic; this strongly supports the recommendation to decrease the number of hours of online screen exposure and encourages students to regularly get engaged in outdoor activities.
Keywords: COVID, computer vision syndrome, lockdown, online exposure
Introduction
The World Health Organization (WHO) has recently declared the coronavirus disease 2019 (COVID-19) a public health emergency of international concern.[1,2] In recent studies, the severity of COVID-19 mimicked that of SARS-CoV in some cases. Due to the rapid spread of the infection, lockdown measures were widely declared, curbing the normal daily routine activities of people outside their homes, thus restricting the free movement of children at the same time. As a result, pupils were made to study from home and attend online classes provided by their educational institution. During these times, they were involved in various indoor activities and inevitably started spending more time facing mobile phones, computers, or television screens for the purpose of either school activity or recreation. To compensate for academic activities, a new era of e-classrooms and digital education system has been introduced wherein classes are held online and students are made to attend these for a minimum of 4–5 years depending on their age to remain connected to their teachers by laptop or smartphones. This in turn made children start complaining of symptoms such as blurred vision, headache, and symptoms related to computer vision syndrome (CVS). Thus far, several studies have enumerated the role of increased screen activity in the development of dry eye disease or CVS.[3,4,5,6] Furthermore, CVS has a negative influence on lifestyle, work, and family relationships. CVS was defined by the American Optometric Association as group of symptoms that occur in response to increased exposure to digital devices, including mobile phones, computer screens in the form of laptops and other digital devices specifically when the exposure to such devices is longer than the tolerance of the user. Symptoms of CVS include dryness/grittiness in the eyes, delayed adjustment to changes of focus from distant to near vision and vice versa, teary eyes, headache, blurred vision, redness, glare/sensitivity, double vision, and changes in the perception of color. It is estimated that around 60 million people are affected by CVS globally, with about a million being added each year.[7,8,9,10,11,12] The significance of this problem prompted the present study to determine CVS symptoms in children in a targeted online questionnaire, including blurring of vision, headache, and watery eyes, due to increased screen time during the COVID-19 lockdown period, as well as to establish whether these ocular symptoms are related to the screen exposure duration. Recently, there has been a myopic pandemic globally, and India is going to be the myopic capital by 2030; this increased exposure to online classes will further increase the risk.
Materials and Methods
This was a non-randomized, questionnaire-based study conducted from July 2020 to August 2020 by the ophthalmology department of a tertiary care pediatric hospital in North India. Prior clearance was obtained from the institutional ethical committee. The inclusion criteria of the study were parents of children aged 6–16 years attending regular school. Participants were interviewed through a Google Form after giving their online consent in English. Based on the survey sample size calculation given by Moon et al.,[5] a sample size of 125 was determined for the current study.
Procedure
An online survey (Google Forms) based on some questions from the Dry Eye Workshop (DEWS) guidelines of the McCarty questionnaire was circulated among parents during the pandemic period. All of the study subjects were invited to participate through the circulation of the Google Form through multiple groups on social media, namely WhatsApp and email. Upon receiving the link, participants were redirected to the consent form. Once the participant gave their consent, they could proceed to the Google survey, which consisted of 19 questions for parents. After answering the questions, the participant could submit the form to the investigator by clicking on the submit link. The questionnaire included questions related to the personal data and lifestyle habits of the children. To facilitate the recording and interpretation of results, questions related to screen use (daily screen hours) were included to describe the number of hours the student spent every day in front of their computer or smartphone screens. The presence of CVS symptoms was also interrogated. For the interpretation of the results, the children were divided into two groups: group I consisted of children younger than 10 years, and group II included children older than 10 years.
Statistical methods
Data were analyzed using the Statistical Package for Social Sciences (SPSS v20) software. Descriptive data were presented as percentages. The dependent variable in this study was the presence of CVS. The significance of associations was tested using Chi-square/Fisher’s exact test for categorical variables and Wilcoxon rank-sum/Kruskal–Wallis test for continuous variables. Univariate and multivariable regression analyses were carried out to find an independent factor associated with the increase in symptoms. P < 0.05 was considered as indicative of statistical significance.
Results
A total of 145 parents participated in the study. Among these, 40 parents filled the questionnaire for two children; thus, a total of 185 children were included in the study. The mean age of the children was 14.2 ± 2 years, and there were 104 (56.2%) females and 81 (43.2%) males. A total of 147 (79.5%) children were studying in classes over the 8th standard. Of all participating children, 53 (28.7%), 64 (34.6%), and 31 (16.8%) had exposure to the screen of a laptop/smartphone for more than 4 h, up to 6 h, and more than 6 h per day, respectively. Compared to the pre-pandemic era, the screen exposure duration had increased to the range of less than 1 h in 46 (24.9%), 1–2 h in 60 (32.4%), 2–3 h in 24 (13%), and more than 4 h in 25 (13.5%) children. Parents were interviewed regarding the children’s symptoms, including redness, watery eyes, scratchy eyes, headache, sore eyes, and difficulty refocusing. The number of symptoms ranged from 1 to 5 with a single symptom or five symptoms in 55 (29.9%) and 23 (12.3%) children, respectively [Tables 1 and 2]. The most common symptom reported by children was headache, followed by eye pain, scratchy eyes, and watery eyes. A total of 148 (80%) children had none of the abovementioned symptoms prior to the increased screen exposure due to online studying during lockdown period.
Table 1.
Demographic distribution of school children
| n (%) | |
|---|---|
| Age (years) | |
| 6-9 | 24 (13.0) |
| 9-10 | 26 (14.1) |
| 11-12 | 28 (15.1) |
| 13-14 | 23 (12.5) |
| 15-16 | 84 (45.4) |
| Gender | |
| Female | 104 (56.2) |
| Male | 81 (43.8) |
| Education | |
| Primary | 50 (27.1) |
| Secondary | 135 (72.9) |
| Total | 185 (100.0) |
Table 2.
Distribution of screen time among the participating school children
| n (%) | |
|---|---|
| Laptop/computer/mobile phone | |
| <1 h | 10 (5.4) |
| Up to 2 h | 27 (14.6) |
| Up to 4 h | 53 (28.7) |
| Up to 6 hours | 64 (34.6) |
| >6 h | 31 (16.7) |
| TV usage | |
| <1 h | 76 (41.1) |
| Up to 2 h | 59 (31.9) |
| Up to 4 h | 38 (20.5) |
| Up to 6 h | 12 (6.5) |
| Number of activities involving screen use | |
| One | 105 (56.7) |
| Two | 55 (29.7) |
| Three | 21 (11.3) |
| Four | 4 (2.3) |
| Number of hours of activity increase in preceding three months | |
| <1 h | 46 (24.9) |
| 1-2 h | 60 (32.4) |
| 2-3 h | 24 (13.0) |
| 3-4 h | 30 (16.2) |
| >4 h | 25 (13.5) |
| Number of symptoms | |
| None | 42 (22.7) |
| 1 | 55 (29.9) |
| 2 | 27 (14.7) |
| 3 | 16 (8.6) |
| 4 | 21 (11.3) |
| 5 | 24 (12.8) |
| Were these symptoms present before COVID? | |
| No | 148 (80.0) |
| Yes | 15 (8.1) |
| The above symptoms have increased since then* | 22 (11.9) |
| Total | 185 (100.0) |
Note: The remaining 42 children reported no symptoms
Based on classifying the symptoms according to the assumed exposure levels of children of different age groups, 135 (73%) children over 10 years of age (group II) experienced increased online screen exposure as compared to children younger than 10 years (group I) whose screen exposure was lower (P < 0.005) [Table 3, Figures 1 and 2]. The activities had no significant association with hours of exposure to screen in the form of laptops/phones (P = 0.385) in the pre-pandemic period, but this association became significant in the following 2 months (P < 0.001). Parents were also interviewed on the type of activities involving screen time, which ranged from online classes for academic purposes to recreation in the form of playing games and/or watching YouTube videos. Playing games accounted for the activity with the longest screen exposure duration in group I, while this was academic activities in group II. The number of symptoms increased along with exposure as children with more than 4 h of daily exposure had 1.2 units of more symptoms of CVS as compared to children with lower exposure (95% CI: 0.71–1.66; P < 0.005) [Tables 3 and 4].
Table 3.
Distribution of symptoms according to activities in different age groups
| Group I (n=50) | Group II (n=135) | Total | P | |
|---|---|---|---|---|
| Laptop/computer/smartphone | ||||
| <1 h | 3 (6.0) | 7 (5.2) | 10 (5.4) | 0.385 |
| Up to 2 h | 8 (16.0) | 19 (14.0) | 27 (14.6) | |
| Up to 4 h | 9 (18.0) | 44 (32.6) | 53 (28.5) | |
| Up to 6 h | 20 (40.0) | 44 (32.6) | 64 (35.0) | |
| >6 h | 10 (20.0) | 21 (15.6) | 31 (16.5) | |
| *Were these symptoms previously existent? | ||||
| No | 41 (82.0) | 107 (79.3) | 148 (80.0) | 0.761 |
| Yes | 3 (2.0) | 12 (9.9) | 15 (8.0) | |
| *The above symptoms have increased since | ||||
| Yes | 6 (13.6) | 16 (13.4) | 22 (13.5) | 0.975 |
| No | 38 (86.4) | 103 (86.6) | 141 (86.5) | |
| Change in power of prescription in the last 6 months | ||||
| 6/6 unaided | 17 (34.0) | 55 (40.8) | 72 (38.9) | 0.274 |
| No | 13 (26.0) | 30 (22.2) | 43 (23.2) | |
| Not checked | 15 (30.0) | 36 (26.7) | 51 (27.6) | |
| Yes | 5 (10.0) | 14 (10.3) | 19 (10.3) |
*The total is not 185 for these symptoms
Figure 1.
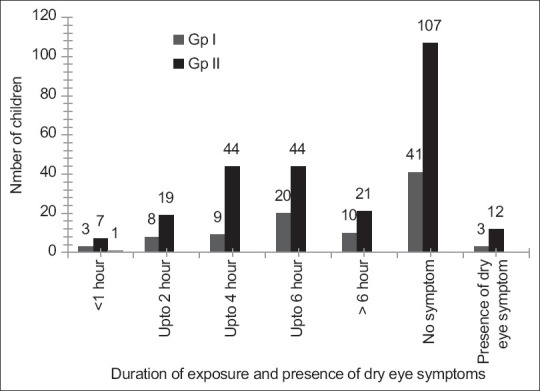
Association between hours of exposure to digital devices and dry eye symptoms in younger and older age group children
Figure 2.
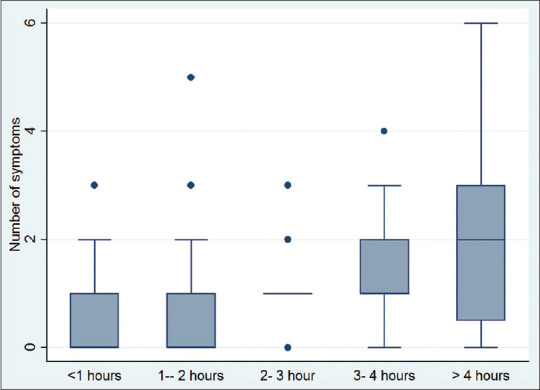
Box Whisker plot depicting the relationship between the number of hours of screen exposure and increase in symptoms Note: The remaining 42 children reported no symptoms
Table 4.
Regression analysis for the association between online activities and hours in relation to screen exposure
| Variables | Median (Range) | P | Unadjusted Regression Coefficient (95% C.I.) |
P | Adjusted Regression Coefficient (95% C.I.) |
P |
|---|---|---|---|---|---|---|
| Age (years) | ||||||
| <10 | 1 (0-5) | 0.0032 | ||||
| ≥10 | 0 (0-6) | −0.4 (−0.77, −0.03) | 0.034 | |||
| Sex | ||||||
| Female | 1 (0-6) | 0.4783 | ||||
| Male | 1 (0-5) | −0.1 (−0.44, 0.22) | 0.516 | |||
| Number of hours | ||||||
| <1 | 0 (0-2) | 0.001 | ||||
| 1-2 | 0 (0-2) | 0.03 (-0.37, 0.44) | 0.841 | 0.7 (-0.33, 0.48) | 0.707 | |
| 2-3 | 1 (0-6) | 0.2 (−0.28, 0.75) | 0.368 | 0.2 (−0.30, 0.73) | 0.418 | |
| 3-4 | 1 (0-5) | 0.6 (0.07, 1.10) | 0.024 | 0.6 (0.04, 1.06) | 0.033 | |
| >5 | 2 (0-3) | 1.2 (0.71, 1.66) | 0.001 | 1.2 (0.72, 1.67) | 0.001 | |
| Number** of activities | 0.15 | 0.036 | 0.2 (0.02,0.44) | 0.2 (0.02, 0.423) | 0.032 |
** Spearman’s correlation
There was a significant association between the increase in the number of activities and the development of CVS symptoms in children (r = 0.15; P = 0.036). According to the multiple regression analysis, the number of activities and screen exposure duration were found to be independent associated factors for increased symptoms related to CVS; the regression coefficient had 0.6 units (95% CI: 0.04–1.06) of increase in these symptoms in children with screen exposure of 3–4 h to 1.2 units of increase in the above symptoms (95% CI: 0.72–1.67) in children with more than 5 h of screen exposure [Table 4].
Discussion
CVS, also known as digital eye strain (DES), occurs due to excessive exposure to computers or other digital screens that make near vision tasks more difficult than the normal capacity of the user.[4,5,6,7,8] It is characterized by symptoms related to dry eyes, such as eye discomfort, blurred vision, fatigue, headache, redness of eyes, and watery eyes. Furthermore, the blue light emitted from such screens has a short wavelength of 415–455 nm with a higher amount of energy, which has a causative role in ocular disorders such as dry eye, cataract, and age-related macular degeneration. In addition, not only does it lead to ocular health disturbances but also to sleep cycle disturbance through melatonin secretion from the pineal gland.[8,9,10,11,12] During the COVID-19 outbreak, almost all countries in the world had to adjust to a new normal in the field of education by starting online classes and electronic learning, which is also known as e-learning. This was viewed as the most ideal form of distant teaching and learning. Thus, it was important to assess whether the increased screen time during the COVID-19 lockdown period had affected the CVS-related symptoms. Numerous researches have been conducted on CVS symptoms. In a questionnaire-based study conducted by Gangamma et al.,[4] the questions related to the occurrence of pain around the eyes, headache, blurred near and distant vision, dryness/grittiness/redness of eyes, excessive tearing, double vision, twitching of eyelids, and changes in visualizing colors were considered as symptoms of CVS.
Although there have been numerous studies related to the excessive usage of computers in adults, recently, a few studies have been conducted in children due to sudden changes in their lifestyle due to increased online exposure due to changed education mode during the COVID-19 pandemic, even though their increased screen exposure in the form of online classes and games is a component of the new normal during COVID times. All these symptoms and behavioral modifications have them predisposed to myopic changes as stated in different studies.[13,14,15,16,17,18]
According to the American Academy of Ophthalmology, prolonged screen exposure with great concentration can lead to a reduced blink rate and difficulty in eye accommodation with a poor distribution of tears. Computer-based learning, also known as e-learning, is part of school education in certain developed nations, whereas it is an entirely new concept in developing nations like India, especially for completing a normal school curriculum. E-learning is associated with various barriers as the eyes are normally adjusted to seeing farther than 6 m; therefore, viewing at a computer screen or mobile phone is an outwardly visual task compared to a printed page. Digital prints have smaller print sizes and glimmering and pixelated images. The mixture of different digital components hampers smooth reading and leads to the CVS symptoms of eye strain. A further significant concern is the background illumination level of cellular phones. The current study indicated an increase in CVS symptoms following the higher use of computers and mobile phones. Moreover, parents reported that such ocular symptoms were not present before the online classes started, and the range of symptoms increased with the duration of online exposure. These findings are in agreement with those of studies conducted on e-learning in developed nations. For example, Kozeis et al.[12] reported that viewing online screens can lead to development of symptoms such as blurred vision, fatigue, headache, and other symptoms. Our results are similar to the recent study conducted by Saxena et al.;[19] and Wong et al.;[20] they reported an increased risk of developing myopia due to increased online excessive screen exposure during the COVID-19 pandemic. Another study conducted by Mohan et al.[21] on the impact of the online teaching environment on students’ vision emphasized the need to improve the classroom teaching efficiency. The American Academy of Ophthalmology has provided some guidelines, for example, for an ideal posture, the display should be at a minimum distance of 25 inches away or at arm’s length following the 20-20-20 rule; and the child is advised to look at a distant object 20 feet away for 20 s every 20 min.[16,17,18,19,22] Along with the usage of matte screen filters, children should be encouraged to wear glasses if required along with frequent blinking instead of simply wearing protective glasses. At the same time, parents should be made to understand that they need to discourage their children from viewing screens 2–3 h before bedtime.[21,23,24,25,26,27,28]
The limitation of the current study is that as it is an online study, where objective tests, such as Schirmer’s test, Fluorescein dye disappearance test, and Ocular Surface Disease Index (OSDI), could not be conducted. Also, we could not compare the pre-COVID outdoor activity hours in these children. A further study in the same cross-section of the population to assess the onset of refractive error after shifting to conventional classroom teaching is recommended.
Conclusion
There was an increased exposure to digital screens for online activities during the lockdown period of the COVID-19 pandemic, leading to increased symptoms of dry eye due to the changed education mode from conventional classroom teaching to digitalization, thus strongly supporting the suggestion to decrease the number of hours of daily screen exposure during online activities and encouraging students to get involved in outdoor activities. Moreover, to alleviate the problems of eye strain and other dry eye symptoms, students should adjust their background illumination appropriately, and teachers can help by providing breaks in their learning to avoid long periods of continuous online screen exposure. The American Academy of Ophthalmology and the World Health Organization recommends that besides refraction and routine ophthalmic examination, certain eye exercises that include up-and-down and side-to-side eye-tracking movements should also be carried out.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet. 2020;395:565–74. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Optometric Association. Guide to the Clinical Aspects of Computer Vision Syndrome. St. Louis: American Optometric Association; 2017. [Last accessed on 2020]. [Google Scholar]
- 4.Gangamma M, Rajagopala M. A clinical study on “computer vision syndrome” and its management with Triphala eye drops and Saptamrita Lauha. Ayu. 2010;31:236–9. doi: 10.4103/0974-8520.72407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moon JH, Kim KW, Moon NJ. Smartphone use is a risk factor for pediatric dry eye disease according to region and age: A case control study. BMC Ophthalmol. 2016;16:188. doi: 10.1186/s12886-016-0364-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The definition and classification of dry eye disease: Report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop. Ocul Surf. 2007;5:75–92. doi: 10.1016/s1542-0124(12)70081-2. [DOI] [PubMed] [Google Scholar]
- 7.Iqbal M, Massry AE, Elagouz M, Elzembely H. Computer vision syndrome survey among medical students in Sohag University hospital, Egypt. Ophthalmic Res. 2018;8:1–8. [Google Scholar]
- 8.Zhao ZC, Zhou Y, Tan G, Li J. Research progress about the effect and prevention of blue light on eyes. Int J Ophthalmol. 2018;11:1999–2003. doi: 10.18240/ijo.2018.12.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bhola R. The Effects of Too Much Screen Time on Children's Vision. [Last accessed on 2020 Jul 13];CHOCChildren'sBlog. 2017 Available from: https: //blog.chocchildrens.org/effects-of-screen-time-on-childrens-vision/ [Google Scholar]
- 10.Gudgel D. Screen Use for Kids. [Last accessed on 2020 Jul 13];American Academy of Ophthalmology. 2020 Available from: https: //www.aao.org/eye-health/tips-prevention/screen-use-kids . [Google Scholar]
- 11.Tosini G, Ferguson I, Tsubota K. Effects of blue light on the circadian system and eye physiology. Mol Vis. 2016;22:61–72. [PMC free article] [PubMed] [Google Scholar]
- 12.Kozeis N. Impact of computer use on children's vision. Hippokratia. 2009;13:230–1. [PMC free article] [PubMed] [Google Scholar]
- 13. [Last accessed on 2021 Aug 12];Digital guidelines: Promoting healthy technology use for children. APA. 2019 Available from: https: //www.apa.org/topics/healthy-technology-use-children/ [Google Scholar]
- 14. [Last accessed on 2021 Aug 12];WFH, online classes led increase in Computer Vision Syndrome amid pandemic. ET HealthWorld.com2020. https: //health.economictimes.indiatimes.com/news/industry/wfh-nlineclasses-led-increase-in-computer-vision-syndrome-amid-pandemic/78725729/ [Google Scholar]
- 15.Munshi S, Varghese A, Dhar-Munshi S. Computer vision syndrome-A common cause of unexplained visual symptoms in the modern era. Int J Clin Pract. 2017;71 doi: 10.1111/ijcp.12962. doi: 10.1111/ijcp.12962. [DOI] [PubMed] [Google Scholar]
- 16.Ku PW, Steptoe A, Lai YJ, Hu H-Y, Chu D, Yen Y-F, et al. The associations between near visual activity and incident myopia in children: A nationwide 4-year follow-up study. Ophthalmology. 2019;126:214–20. doi: 10.1016/j.ophtha.2018.05.010. [DOI] [PubMed] [Google Scholar]
- 17.Muhamedagic L, Muhamedagic B, Halilovic EA, Halimic JA, Stankovic A, Muracevic B. Relation between near work and myopia progression in student population. Mater Sociomed. 2014;26:100–3. doi: 10.5455/msm.2014.26.100-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lanca C, Saw SM. The association between digital screen time and myopia: A systematic review. Ophthalmic Physiol Opt. 2020;40:216–29. doi: 10.1111/opo.12657. [DOI] [PubMed] [Google Scholar]
- 19.Saxena R, Gupta V, Rakheja V, Dhiman R, Bhardawaj A, Vashist P. Lifestyle modification in school-going children before and after COVID-19 lockdown. Indian J Ophthalmol. 2021;69:3623–9. doi: 10.4103/ijo.IJO_2096_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wong CW, Tsai A, Jonas JB, Ohno-Matsui K, Chen J, Ang M, et al. Digital screen time during the COVID-19 pandemic: Risk for a further myopia boom? Am J Ophthalmol. 2021;223:333–7. doi: 10.1016/j.ajo.2020.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohan A, Sen P, Shah C, Jain E, Jain S. Prevalence and risk factor assessment of digital eye strain among children using online e-learning during the COVID-19 pandemic: Digital eye strain among kids (DESK study-1) Indian J Ophthalmol. 2021;69:140–4. doi: 10.4103/ijo.IJO_2535_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dirani M, Tong L, Gazzard G, Zhang X, Chia A, Young TL, et al. Outdoor activity and myopia in Singapore teenage children. Br J Ophthalmol. 2009;93:997–1000. doi: 10.1136/bjo.2008.150979. [DOI] [PubMed] [Google Scholar]
- 23.Jha N, Shenoy V. Digitization of Indian education process: A hope or hype. IOSR J Bus Manag. 2016;18:131–9. [Google Scholar]
- 24.Bhattacharya S, Saleem SM, Singh A. Digital eye strain in the era of COVID-19 pandemic: An emerging public health threat. Indian J Ophthalmol. 2020;68:1709–10. doi: 10.4103/ijo.IJO_1782_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ganne P, Najeeb S, Chaitanya G, Sharma A, Krishnappa NC. Digital eye strain epidemic amid COVID-19 pandemic-A cross-sectional survey. Ophthalmic Epidemiol. 2021;28:285–92. doi: 10.1080/09286586.2020.1862243. [DOI] [PubMed] [Google Scholar]
- 26.Narinasamy I. The Need to Care: Students'Perceptions of Teacher's Caring Behaviour. Conference: Asia-Pacific Network for Moral Education, At Kaohsiung Normal University, Taiwan. 2018 [Google Scholar]
- 27.Garza R, Alejandro E A, Blythe T, Fite K. Caring for Students: What Teachers Have to Say. ISRN Education. 2014 [Google Scholar]
- 28.Radesky J, Christakis D. Media and young minds. Pediatrics. 2016;138:e20162591. doi: 10.1542/peds.2016-2591. [DOI] [PubMed] [Google Scholar]


