Abstract
Background:
Data on internet utilization is needed, particularly during a time when in-person services are limited or only available virtually. The purpose of this study was to identify characteristics of internet use among persons who use drugs and assess adoption of an interactive, risk reduction informational website - WebHealth4Us.
Methods:
Participant recruitment occurred in pharmacies participating in the New York State pharmacy syringe access program (n=209). ACASI surveys were conducted on-site to ascertain internet use and related sociodemographics and risk behaviors. Internet users (use ≥ once/month) were shown a website WebHealth4Us highlighting social services and risk reduction information on 4 topic areas: mental health, HIV, HCV, and other STI; users could also sign-up for weekly text messages for any topic area. Follow-up ACASI occurred at 4-weeks to assess user experiences and website adoption.
Results:
Study sample (n=196) was mostly male (60%), average age 46, black/Latinx (76%), had a history of incarceration (79%), and reported past/current injection (53%) or non-injection (51%) drug use. Internet use was high (79%), accessed >4 times/week (60%) most commonly for: housing (61%), health issues (54%), and drug treatment (45%). Over one-third accessed WebHealth4Us during follow-up, and 35% of those opted for weekly text messages (mental health most common topic selected). After adjustment, younger age (AOR=0.96) and alcohol use (AOR=2.26) predicted WebHealth4Us access.
Conclusion:
Internet use was high with considerable WebHealth4Us access, and specifically for mental health needs. Web-based interventions warrant large-scale investigation in high-risk communities, prioritizing social determinants and behavioral health.
Keywords: mHealth, drug use, risk reduction, web-based interventions, mental health, social déterminants
Introduction
An estimated 53.2 million Americans 12 years and older (approximately 1 in 5) use illicit drugs1, and those who use injection as a route of administration experience a higher prevalence of HIV, Hepatitis (HCV), and psychiatric comorbidities2–9. Non-injection drug use also carries a higher likelihood of medical and psychiatric sequalae compared to the general population and is more common than injection drug use1,10–13. Improved access to public health services including risk reduction, primary prevention, and secondary prevention education and counseling, can help improve health outcomes among persons who use drugs (PWUD), particularly among persons who have who have been historically denied access to quality care and resources14,15. For instance, drug use-related stigma (and other intersectional stigmatizing statuses) and limited availability of behavioral health services in many U.S. communities coupled with cost of care, and lack of information about available resources persist as barriers to needed medical and social services for PWUD16–21. Web-based technologies can be utilized as a cost-effective and easily accessible means of removing some of the longstanding structural barriers to prevention and treatment resources for the most vulnerable PWUD22–26.
Mobile phone access is ubiquitous with 96% of US adults reporting ownership27. Further, most smartphone owners are comfortable using their phones to seek health information and phone-based health interventions have been shown to improve disease management, care coordination as well as motivate behavior change by facilitating affordable, accessible, and efficient delivery and utilization of healthcare28–31. Studies suggest that mobile phone access among PWUD has increased and recent data show internet utilization rates to be similar to that of the general population32–35. Many urban cities have increased internet access in communities such as New York City’s wifi access program LinkNYC providing not only smartphone charging capability, but also phone dial pad access, and touchscreen internet browsing station.
A meta-analysis of 35 internet interventions among adults reporting illicit drug use revealed that internet-based interventions demonstrated effectiveness at reducing opioid use36 among treatment seeking populations. The results of this meta-analysis also noted that high attrition rates among intervention participants remain a challenge and new strategies should be explored to retain those lost to follow-up who tend to be the most vulnerable. Finally, these web-based interventions have not been assessed for impact on other salient outcomes outside of treatment access and engagement, such as risk reduction and prevention services, and other drug use-related public health needs among PWUD (e.g., STI’s, HCV, mental health services). One notable exception are mHealth studies conducted among high risk communities with HIV and therefore, interventions were focused on treatment adherence and retention in care (e.g. sending appointment reminders via text messages), with the exception of a few case studies37,38. Investigations among PWUD and that focus on the use of technology to provide more comprehensive risk reduction information and that facilitates access to prevention resources is scant, particularly in the U.S. Thus, identifying factors associated with uptake of internet-based public health interventions among a vulnerable sample of PWUD is needed and has been suggested in previous reports. Specifically, more research is needed to not only determine efficacy, but to better understand and identify strategies related to reach, adoption, implementation, and maintenance in both clinical and community settings39.
Herein, we conducted a community-based study with PWUD to 1) document internet general use, and 2) assess feasibility and user experiences of a web-based intervention (WebHealth4Us) designed to provide HIV prevention and related risk reduction information. This website included pertinent information including where to access services for PWUD in low-income, majority Black and Latinx communities heavily burdened with HIV and street-marketed drug use. The purpose of this study was first to identify demographic, social and behavioral factors associated with internet use among PWUD. Second, after identifying and initiating active internet users to the WebHealth4Us website and a 4-week follow-up period, we aimed to assess adoption, user experience, and social and behavioral predictors of website use which included the option to ‘sign-up’ for weekly public health text messages related to mental health, HIV, HCV, and STI prevention and risk reduction.
Methods
Participant recruitment and enrollment
Between the years of 2013 – 2016, we implemented targeted street outreach in communities with high prevalence of illicit drug use in New York City (NYC), New York. Research outreach staff conducted street outreach and engaged potential participants on the streets of previously selected high risk communities in Upper Manhattan and South Bronx40, informed them of the study, and provided them with a study flyer with study information for setting up an appointment for participation, or if time permitted, scheduled an appointment at the time of engagement using a study phone. Flyers were also placed in local community organizations, pharmacies, methadone programs, and needle exchange programs. To compliment this recruitment strategy and similar to our earlier work41,42, we also trained staff at a local study-enrolled pharmacy registered with the New York State (NYS) Expanded Syringe Access Program (ESAP) to help facilitate enrollment of syringe-purchasing customers, and their peers. The pharmacy study site also provided private partitioned space for data collection activities. Use of pharmacies that participate in syringe access programs have proven to be more amenable to participant retention when implementing community studies involving follow-up since participants are accustomed to patronizing these spaces for syringe access43,44.
Potential participants were administered a 10-item screener to determine eligibility. To reduce the occurrence of false report to gain entry into the study, the screener included questions on a range of topics to mask the exact selection criteria. Individuals were considered eligible if they were 18 years of age or older, and used heroin, crack, and/or cocaine at least once in past month. After eligibility was determined, participants underwent informed consent. At the time of data collection, this study was approved by Columbia University Medical Center, Institutional Review Board for Human Subject Research. The Nathan Kline Institute for Psychiatric Research, Institutional Review Board also approved this study during the data analysis phase and manuscript development.
WebHealth4Us intervention
After consent, participants were invited to complete a baseline audio computer-assisted self-interview (ACASI) on the same day of enrollment or scheduled within one week. All active internet users (defined as participants who reported internet use at least once a month) were selected to view the WebHealth4Us website at the end of the ACASI baseline visit on the same notebook used for ACASI and were followed over time. The WebHealth4Us viewing included two components. First, the interviewer set up a secure login and a password selected by the participant. Second, the interviewer assisted the participant with the navigation of the site, highlighting each of the public health four risk topics on the site (i.e., HIV, HCV, STI’s and mental health), as well as the social services information available in their community. The WebHealth4Us site was developed by our research team in collaboration with community partners. Information for each topic included education and available resources in the community pertaining to risk reduction, prevention and treatment, as well as access information on drug treatment, housing, and food availability (e.g., green markets, food banks, food pantries). Additionally, users who visited WebHealth4Us and had access to a cell phone could click on a tab to receive text messages related to any of the four primary topic areas. This functionality was highlighted during the study visit when the interviewer and study participant were together reviewing study functionality. Those opting for text messages would receive a message consisting of an 8–12 worded risk reduction message delivered weekly, for four weeks.
At the end of the visit, participants were asked to return for follow-up in 4 weeks and given an appointment. All surveys were administered at the study pharmacy and participants were compensated for their time ($20 for the baseline and $25 for the 4-week follow-up ACASI). To further minimize attrition, research staff made at least 2 calls to participants to remind them of their follow-up appointment, with additional tracking efforts for those who missed their follow-up appointment. (see Figure 1)
Figure 1.
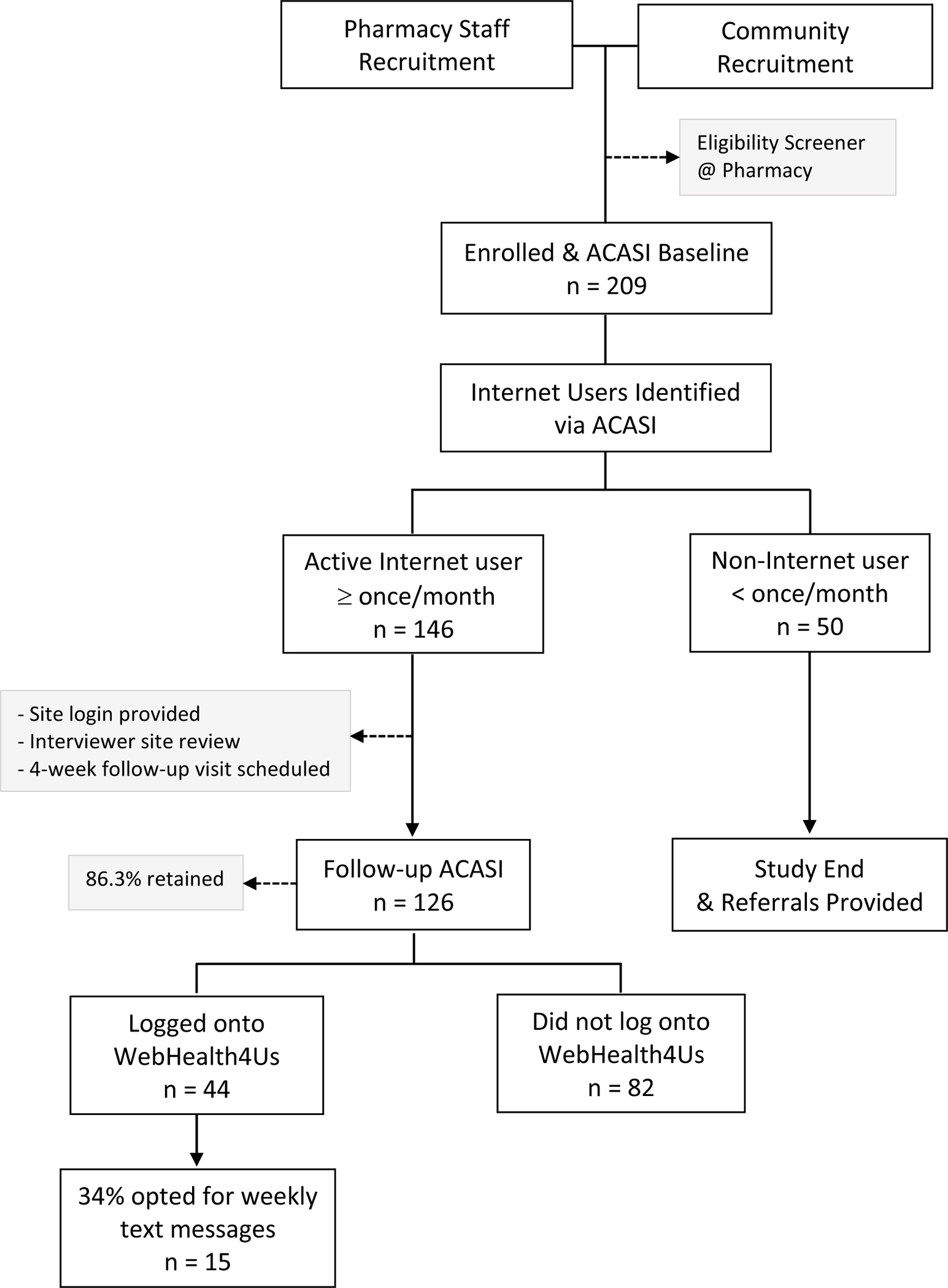
WebHealth4Us Study Flow
Measures of interest
The baseline survey ascertained participant demographic characteristics, social and health risk behaviors, device and frequency of internet use, and past internet queries related to social services and health needs. Demographic measures were collapsed into the following variables: gender (male, female), race/ethnicity (Black/Latinx, White/other), age, and sexual orientation (lesbian/gay/bisexual/other, straight). Several social factors were examined and included educational attainment (high school/GED or higher, less than high school), past year legal income ($5,000 or less, more than $5,000), recent (past 3 months) homelessness (yes, no), lifetime carceral system involvement (never, jail, prison, or jail and/or prison) and current regular doctor (yes, no).
Behavioral risk variables included justice system involvement (never, jail only, prison), lifetime crack/cocaine, heroin, and injection drug use (yes, no), use of non-medically prescribed opioids or other pills (yes, no) past 3 months, presence of binge drinking symptomology (yes, no) measured as frequency of having ≥ 6 drinks in one occasion in past 3 months (ever vs. never) and high risk sexual behavior (yes, no) defined as self-report of multiple sex partners, sex in exchange for drugs, money, or food, and/or same sex behavior among men in past 3 months.
Current internet use (never, less than once a month, once a month, 2–3 days/month, once a week, 2–3 days/week, 4–6 days/week, or everyday) was also assessed to identify the intervention sample which was defined as using at least once a month or more. Participants reporting at least monthly internet use were asked how they accessed the internet (desktop/laptop or tablet, smartphone, at-home access), reasons for health-related internet use (e.g., communicate with a health provider, general or specific health information, find a provider, insurance information), reasons for social services-related internet use (e.g., seeking information on drug treatment or syringe exchange, resources for housing or food), and willingness to receive health-related information via mobile phone (yes, no).
The follow-up survey ascertained participant experiences using the WebHealth4Us website. This included whether they found the educational resources on the site useful (yes, no), relevancy of website by content area (e.g., HIV, HCV, STI, mental health, and other related social services including housing, food availability, and drug treatment), and because of the sensitive topic areas covered on the site, participants were asked whether reading about specific content areas (e.g., disease prevention, drug treatment, etc.) made them uncomfortable (yes, no).
Analysis plan
First, we present a descriptive summary of study participants with respect to demographics, social and behavioral characteristics, and their internet use. Using chi-squared tests of association for categorical variables and independent sample t-tests for continuous variables, we identified statistically significant correlates of internet use at baseline. Then, among study participants exposed to the website intervention, we contrasted participant characteristics and internet use behavior by WebHealth4Us access (logged onto site or not) using simple logistic regression analyses to identify characteristics with crude associations with site access. Characteristics identified in bivariate analyses were included in a multivariable regression model predicting visiting the intervention website. Finally, we summarized user experiences related to the WebHealth4Us site. All analyses were conducted using SAS v9.4 (IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY). This study was approved by Columbia University Medical Center, NYU School of Medicine, and the Nathan Kline Institute for Psychiatric Research.
Results
Table 1 provides the distribution for participant characteristics overall and by internet use. Of the 209 enrolled participants, 94% (n=196) had responses on all measures of interest. Study participants were mostly male (58.7%), Black or Latinx (76%), and 46 years of age, on average. About 18% identified as lesbian, gay, bisexual, or other sexual orientation; approximately one-third had less than a high school education (34.2%), over 70% had annual income less than $5,000, 36.7% had experienced recent homelessness, and 80% reported past carceral experience. With respect to drug use, 91% reported lifetime crack/cocaine use, 77.6% reported lifetime heroin use, 60.2% reported recent non-medically prescribed opioid use or other pill use, and one-in-three reported binge drinking (34.7%). With respect to HIV risk behaviors, over half (53.6%) reported injection drug use and one-third reported high risk sexual behavior (33.7%). Internet use was high in this study sample with over three-quarters (78%) reporting past month internet use, and fairly frequent among all reporting any internet use in past 30 days (8% used less than 1 time/month; 20% used 1–3 times/month; 21% used 1–3 days/week; 59% used 4 or more days/week). Importantly, internet use did not differ by social or risk behavior measures and younger age being the sole demographic factor that was significantly correlated with past month internet use (p<0.05).
Table 1.
Baseline demographic, social, and behavioral characteristics of internet use ≥ once per month among persons with a history of drug use in New York City (n=196), 2013–2016.
| Measures | Total | Internet Use |
|---|---|---|
| n (%) | n (%) | |
|
| ||
| All | 196 | 146 (74.5) |
| Sex | ||
| Male | 115 (58.7) | 84 (73.0) |
| Female | 81 (41.3) | 62 (76.5) |
| Race/ethnicity | ||
| Black/Latinx | 149 (76.0) | 107 (71.8) |
| White/other | 47 (24.0) | 39 (83.0) |
| Age (mean±SD) | 46.3 (±10.0) | 44.1 (±9.70)* |
| Sexual orientation | ||
| Lesbian/gay/bisexual/other | 36 (18.4) | 26 (72.2) |
| Straight | 160 (81.6) | 120 (75.0) |
| Educational attainment | ||
| High school or GED or more | 129 (65.8) | 99 (76.7) |
| Less than HS | 67 (34.2) | 47 (70.2) |
| Legal income in past year | ||
| $5000 or less | 140 (71.4) | 102 (72.9) |
| More than $5000 | 56 (28.6) | 44 (78.6) |
| Homeless in past 3 months | ||
| Yes | 72 (36.7) | 53 (73.6) |
| No | 124 (63.3) | 93 (75.0) |
| Has a regular doctor | ||
| Yes | 129 (90.3) | 129 (73.3) |
| No | 19 (9.74) | 17 (89.5) |
| Carceral involvement | ||
| Never | 39 (19.9) | 29 (74.4) |
| Jail only | 64 (32.6) | 52 (81.3) |
| Prison | 93 (47.4) | 65 (69.8) |
| Lifetime crack/cocaine use | ||
| Yes | 179 (91.3) | 133 (91.1) |
| No | 17 (8.67) | 13 (8.9) |
| Lifetime heroin use | ||
| Yes | 153 (77.6) | 114 (78.1) |
| No | 44 (22.5) | 32 (21.9) |
| NMPO/other pills in past 3 months | ||
| Yes | 118 (60.2) | 91 (77.1) |
| No | 78 (40.0) | 55 (70.5) |
| Ever had injection drug use | ||
| Yes | 105 (53.6) | 85 (81.0) |
| No | 91 (46.40 | 61 (67.0) |
| Binge drinking symptomology | ||
| Yes | 68 (34.7) | 53 (36.3) |
| No | 128 (65.3) | 93 (63.7) |
| Sexual risk behaviors | ||
| Yes | 66 (33.7) | 52 (78.8) |
| No | 130 (66.3) | 94 (72.3) |
p<0.05
Among the 146 participants who reported past month internet use, 86.3% (n= 126) returned and completed the 4-week follow-up survey (Table 2). The distribution of demographics, social, and behavioral characteristics was similar to the overall sample. With respect to internet access, 24.6% accessed the internet on a desktop, laptop, or tablet, 70.6% via smartphones, and the large majority accessed internet away from home (79.4%). The most frequently reported health or social services internet searches were to access information on housing resources (61.9%), a specific medical condition (60.3%), treatment or procedure (57.1%), and to find a doctor or other health professional (54.8%). Most respondents reported using their mobile phones for health-related purposes (66.7%), and most often for seeking health or medical information (60.6%). Importantly, nearly all study participants who reported internet use were willing to receive health information via their cell phone (84.9%). Finally, just over one-third of follow-up survey respondents (n=44) reported accessing WebHealth4Us at least once in the four-week follow-up period.
Table 2.
Internet use characteristics associated with accessing WebHealth4Us site at follow-up among persons with a history of drug use in New York City (n=126), 2013–2016.
| Measures | Total | Logged on to WebHealth4Us | ||
|---|---|---|---|---|
| n (%) | n (%) | Crude OR (95% CI) | Adj OR (95% CI) | |
|
| ||||
| Total Sample | 126 | 44 (34.9) | -- | -- |
| Demographics | ||||
| Sex | ||||
| Male | 74 (58.7) | 24 (54.6) | ||
| Female | 52 (41.3) | 20 (45.5) | ||
| Race/ethnicity | ||||
| Black/Latinx | 94 (74.6) | 31 (70.5) | ||
| White/other | 32 (25.4) | 13 (29.6) | ||
| Age (mean±SD) | 44.0 (±9.87) | 40.5 (±9.90)** | 0.94 (0.91 – 0.98)** | 0.94 (0.91 – 0.98) ** |
| Sexual orientation | ||||
| Lesbian/gay/bisexual/other | 26 (20.6) | 12 (27.3) | ||
| Straight | 100 (79.4) | 32 (72.7) | ||
| Educational attainment | ||||
| Less than HS | 38 (30.2) | 12 (27.3) | ||
| High school or GED or more | 88 (69.8) | 32 (72.7) | ||
| Annual legal income | ||||
| $5000 or less | 82 (66.7) | 32 (76.2) | ||
| More than $5000 | 41 (33.3) | 10 (23.8) | ||
| Homeless (past 3 months) | ||||
| Yes | 44 (34.9) | 14 (31.1) | ||
| No | 82 (65.1) | 30 (68.2) | ||
| Carceral involvement | ||||
| Never | 26 (20.6) | 9 (34.6) | ||
| Jail only | 40 (31.8) | 17 (42.5) | ||
| Prison | 60 (47.6) | 18 (30.0) | ||
| Internet use | ||||
| Access using desktop/laptop or tablet | ||||
| Yes | 31 (24.6) | 8 (18.2) | ||
| No | 95 (75.4) | 36 (81.8) | ||
| Access using smartphone | ||||
| Yes | 89 (70.6) | 32 (72.7) | ||
| No | 37 (29.4) | 12 (27.3) | ||
| Has internet access at home | ||||
| Yes | 26 (20.6) | 16 (36.4) | ||
| No | 100 (79.4) | 28 (63.6) | ||
| Health-related internet usea | ||||
| Receive medical test results | 21 (16.7) | 10 (47.6) | ||
| Communicate with provider | 42 (33.3) | 18 (42.9) | ||
| General health issues | 52 (41.3) | 16 (30.8) | ||
| Specific disease or condition | 76 (60.3) | 28 (36.8) | ||
| Certain treatment or procedure | 72 (57.1) | 28 (38.9) | ||
| Find a doctor or other professional | 69 (54.8) | 30 (43.5) | ||
| HIV-related information | 38 (30.2) | 11 (28.9) | ||
| Health insurance | 56 (44.4) | 22 (39.3) | ||
| Social services related internet usea | ||||
| Housing | 78 (61.9) | 29 (37.2) | ||
| Drug treatment | 59 (46.8) | 24 (40.7) | ||
| Places to get free food | 51 (40.5) | 23 (45.1) | 2.11 (1.00 – 4.46)** | 2.14 (0.97 – 4.71)* |
| Safe injection sites | 26 (20.6) | 8 (30.8) | ||
| Use mobile phone for health-related purposes | ||||
| Yes | 84 (66.7) | 31 (36.9) | ||
| No | 42 (33.3) | 13 (31.0) | ||
| Health-related mobile phone internet usea | ||||
| Health or medical information | 60 (60.6) | 27 (45.0) | ||
| Track or manage health via applications | 32 (26.9) | 14 (43.8) | ||
| Communicate with health care providers | 40 (31.8) | 17 (42.5) | ||
| Willing to receive health information via cell phoneb | ||||
| Yes | 107 (84.9) | 40 (37.4) | ||
| No | 19 (15.1) | 4 (21.1) | ||
| Drug use and risk behaviors | ||||
| Lifetime crack/cocaine use | ||||
| Yes | 115 (91.3) | 38 (33.0) | ||
| No | 11 (8.73) | 6 (54.5) | ||
| Lifetime heroin use | ||||
| Yes | 99 (78.6) | 32 (32.3) | ||
| No | 27 (21.4) | 12 (44.4) | ||
| Ever had injection drug use | ||||
| Yes | 77 (61.1) | 24 (31.2) | ||
| No | 49 (38.9) | 20 (40.8) | ||
| NMPO/other pills (past 3 months) | ||||
| Yes | 76 (60.3) | 28 (36.8) | ||
| No | 50 (39.7) | 16 (32.0) | ||
| Binge drinking (past 3 months) | ||||
| Yes | 43 (34.1) | 21 (48.8) | 2.49 (1.16 – 5.36)** | 2.26 (1.01 – 5.05) ** |
| No | 83 (65.9) | 23 (27.7) | ||
| High risk sexual behavior (past 3 months) | ||||
| Yes | 46 (36.5) | 15 (32.6) | ||
| No | 80 (63.5) | 29 (36.3) | ||
p<0.05
p<0.10
categories not mutually exclusive
Table 2 also provides regression analysis results of significant predictors of WebHealth4Us access. After adjustment, older pharmacy customers had lower odds of accessing site with each year increase in age estimated to be associated with a 6% decrease in the odds of accessing the site (AOR=0.94, p<0.05). Participants who used the internet for social services related to places to get free food were twice as likely to log on to WebHealth4Us as compared to participants who did not use the internet for this purpose (AOR=2.14; p<0.06). Participants with binge drinking symptomology had more than 2-fold increase in the odds of accessing WebHealth4Us as compared to those who did not report binge drinking symptomology (AOR=2.26, p<0.05).
In Table 3, user satisfaction metrics for the WebHealth4Us site for pharmacy customers who logged onto the site are presented. In general, users found the website information useful and nearly all (93.2%) reported that they would revisit the site or recommend it to others. Further, despite its focus on sensitive topics, only one participant felt uncomfortable or offended by the website content, namely social services resources information, and none felt uncomfortable with the disease prevention information provided. Finally, among those who reported logging onto the WebHealth4Us website, 34% (n=15) clicked on the sign-up tab and entered their cell phone number to receive health-related text messages: 8 signed up for mental health messages, 6 for HIV prevention messages, 6 for STI messages, and 5 for HCV prevention messages.
Table 3.
User experiences among study participants who logged onto WebHealth4Us4Us site in New York City (n=44), 2013–2016.
| Measures | n (%) |
|---|---|
|
| |
| All | 44 (100) |
| Found disease prevention educational resources useful | 42 (95.5) |
| Disease prevention resources by topic (categories not mutually exclusive) | |
| HIV | 41 (95.4) |
| Hepatitis C | 37 (90.2) |
| Other sexually transmitted diseases | 40 (95.2) |
| Found social services informational resources useful | 41 (93.2) |
| Social services resources by topic (categories not mutually exclusive) | |
| Mental Health Resources | 36 (97.3) |
| Drug treatment | 40 (90.9) |
| Felt uncomfortable or offended by disease prevention information | |
| Yes | 0 |
| No | 44 (100) |
| Felt uncomfortable or offended by social services resources | |
| Yes | 1 (2.3) |
| No | 42 (97.7) |
| Would recommend WebHealth4Us to others | |
| Yes | 41 (93.2) |
| No | 3 (6.8) |
| Will revisit WebHealth4Us site after the end of the study | |
| Yes | 41 (93.2) |
| No | 3 (6.8) |
Discussion
Among a majority Black and Latinx community-based sample, heavily burdened with street-marketed illicit drug use, we highlight a noticeably high proportion of internet use, typically through the use of a smartphone as opposed to a desktop, laptop or tablet. This rate of internet access was similar to the national averages during the time of the study (2013–2016), for persons with income less than $30,000 (72%–79%), and among general populations of Black (79%–88%), and Latinx populations (80%–88%), respectively45. Interestingly, there were no significant differences with respect to social and behavioral risk characteristics when comparing those who used the internet (at least once/month) vs. those who did not. Additionally, after 4-week follow-up among active internet users, slightly more than one-third logged onto the WebHealth4Us intervention, and a third of those individuals opted for weekly risk reduction text messages. To our knowledge, internet use, type, and frequency among a socioeconomically vulnerable community sample of persons actively using heroin, crack and/or cocaine has not been previously reported. The only exceptions are study samples from substance abuse treatment settings and/or persons with HIV infection, both of which have a connection to social and/or medical services and does not reflect the social condition of the current study population. Thus, documenting internet use and adoption of a web-based intervention in this community has high public health significance for this vulnerable, high-need population of PWUD.
Those who logged onto the intervention website were characterized by heavier polydrug use as indicated by binge drinking symptomology (i.e., alcohol use in addition heroin, crack and/or cocaine use), and a tendency to have greater social needs as indicated by reporting internet use to contend with food insecurity as opposed to risk reduction/prevention, treatment or other health-related information. While this relationship carried a strong crude association, it dampened statistically after adjustment; however, the clinical and public health value of this relationship elevates it’s significance and warrants further study, particularly among highly vulnerable populations. While uptake of the intervention was modest, this study revealed a highly successful community-based recruitment strategy, namely the use of community pharmacies who participate in a public health syringe access program, and located in low-income, high risk neighborhoods coupled with community outreach. Furthermore, while retention of participants actively using street-marketed drugs is typically challenging, we observed a relatively high follow-up rate (86.3%) which is also largely due to the use of community pharmacies for recruitment and data collection activities, and known to have trusting ties with the community.46,47
WebHealth4Us and interactive option to receive text messaging
Those who visited WebHealth4Us expressed high satisfaction with the behavioral health, risk reduction and social services content available, indicated they would recommend the website to peers, and revisit the site after study end. However, it is unknown if those who did not log onto the site felt similarly. Low uptake by more than half the sample could be due to a lack of prioritizing risk reduction, prevention, and other health-related services above attending to basic daily needs which was a significant challenge for this population. In fact, among the 35% who were able to access the site, seeking information on access to food pantry’s suggests extreme social disadvantage. This suggests it may be unrealistic to expect higher uptake of risk reduction, prevention and treatment for HIV, HCV, STI’s and/or mental health when basic social needs are unmet. While content on the availability of social services was a component of WebHealth4Us, the focus of the intervention content was risk reduction information, infectious disease prevention, and mental health services access. It still remains a possibility that study participants did not log onto WebHealth4HUs because the site may not have been appealing or useful. These data support investigation of a web-based intervention that emphasizes social determinants of health as a primary public health strategy which may, in turn, result in greater public health impact.
Characteristics of internet use and WebHealth4Us
Internet access was also fairly frequent, with the majority of participants (80%) accessing the internet at least weekly. This result also aligns with prior studies during the same study period (2013–2016) and highlights high and frequent access among adults with substance use disorders22,34, reinforces the need to enhance access to devices with web-browsing capabilities, and to eliminate costs through free wifi access points. In this study, it is important to note that those who did not report internet use (or use less than once per month) were not targeted for the WebHealth4Us intervention due to the time constraints of study funding and the need to recruit a sizable population for feedback on user experiences. For this reason, our findings only reflect active internet users, however, it is unlikely that a website would significantly increase website adoption in this study population. Instead, before assessing adoption of a website among infrequent/never internet users, social and structural barriers to internet use should be addressed and considered as either a primary focus of a separate intervention or in combination with a website such as WebHealth4Us and is currently underway.
Additional unexpected and encouraging findings of this study was the more common use of mobile phone platforms to access the internet than computers, and that internet use and WebHealth4Us adoption was not differentiated by high risk behavior or demographics (with the exception of younger age for website adoption). This could be beneficial when designing intervention studies which could show potential effectiveness more broadly among this population.
Conclusion
These promising findings underscore the importance of harnessing web-based interventions targeting PWUD to address social and economic disparities that have persisted in low-income Black and Latinx urban communities. These data provide successful strategies for community-based study recruitment and retention, which can directly inform large-scale studies involving web-based services or interventions in low-income heavy drug-involved communities. However, web-based public health strategies to address inequities in prevention and treatment access warrant investigations that prioritize social and structural determinants of health instead of expending resources on strategies that solely focus upon or prioritize individual risk behavior.
Acknowledgement:
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute on Drug Abuse [R21DA049166, K23DA042140-01A1].
REFERENCES
- 1.Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2018 National Survey on Drug Use and Health.; 2019. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHNationalFindingsReport2018/NSDUHNationalFindingsReport2018.pdf.
- 2.Mackesy-Amiti ME, Donenberg GR, Ouellet LJ. Psychiatric correlates of injection risk behavior among young people who inject drugs. Psychol Addict Behav. 2014;28(4):1089–1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pilowsky DJ, Wu L-T, Burchett B, Blazer DG, Ling W. Depressive Symptoms, Substance Use and HIV-Related High Risk Behaviors among Opioid-Dependent Individuals: Results from the Clinical Trials Network. Subst Use Misuse. 2011;46(14):1716–1725. doi: 10.3109/10826084.2011.611960.Depressive [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Degenhardt L, Hall W, Warner-Smith M. Using cohort studies to estimate mortality among injecting drug users that is not attributable to AIDS. Sex Transm Infect. 2006;82:iii56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cornford C, Close H. The physical health of people who inject drugs: complexities, challenges, and continuity. Br J Gen Pr. 2016;66(647):286–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Winkelman TN, Chang VW, Binswanger IA. Health, polysubstance use, and criminal justice involvement among adults with varying levels of opioid use. JAMA Netw open. 2018;1(3):e180558–e180558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Degenhardt L, Peacock A, Colledge S, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Heal. 2017;5(12):e1192–e1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mathers BM, Degenhardt L, Phillips B, et al. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. The Lancet. Lancet. 2008;372(9651):1733–1745. [DOI] [PubMed] [Google Scholar]
- 9.Roth AM, Aumaier BL, Felsher MA, et al. An exploration of factors impacting preexposure prophylaxis eligibility and access among syringe exchange users. Sex Transm Dis. 2018;45(4):217–221. doi: 10.1097/OLQ.0000000000000728 [DOI] [PubMed] [Google Scholar]
- 10.Volkow ND, Baler RD, Compton WM, Weiss SRB. Adverse Health Effects of Marijuana Use. N Engl J Med. 2014;370:2219–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Azofeifa A, Mattson ME, Schauer G, McAfee T, Grant A, Lyerla R. National Estimates of Marijuana Use and Related Indicators — National Survey on Drug Use and Health, United States, 2002–2014. Morb Mortal Wkly Rep Surveill Summ. 2016;65(11):1–25. [DOI] [PubMed] [Google Scholar]
- 12.Witkiewitz K, Vowles KE. Alcohol and opioid use, co-use, and chronic pain in the context of the opioid epidemic: A critical review. Alcohol Clin Exp Res. 2018;42(3):478–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Substance Abuse and Mental Health Services Administration. Results from the 2011 National Survey on Drug Use and Health: Mental Health Findings. Rockville, MD; 2012. [Google Scholar]
- 14.Yearby R Racial Disparities in Health Status and Access to Healthcare: The Continuation of Inequality in the United States Due to Structural Racism: Continuing Racial Health Disparities. Am J Econ Sociol. 2018;77(3–4):1113–1152. [Google Scholar]
- 15.Johnson T Intersection of Bias, Structural Racism, and Social Determinants With Health Care Inequities. Pediatrics. 2020;146(2). [DOI] [PubMed] [Google Scholar]
- 16.Neale J, Tompkins C, Sheard L. Barriers to accessing generic health and social care services: a qualitative study of injecting drug users. Heal Soc Care Community. 2008;16(2):147–154. [DOI] [PubMed] [Google Scholar]
- 17.Ahern J, Stuber J, Galea S. Stigma, discrimination and the health of illicit drug users. Drug Alcohol Depend. 2007;88(2–3):188–196. [DOI] [PubMed] [Google Scholar]
- 18.Schmitt MT, Branscombe NR, Postmes T, Garcia A. The consequences of perceived discrimination for psychological well-being: A meta-analytic review. Psychol Bull. 2014;140(4):921–948. [DOI] [PubMed] [Google Scholar]
- 19.Pascoe EA, Smart Richman L. Perceived discrimination and health: A meta-analytic review. Psychol Bull. 2009;135(4):531–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guerrero EG, Marsh JC, Duan L, Oh C, Perron B, Lee B. Disparities in completion of substance abuse treatment between and within racial and ethnic groups. Health Serv Res. 2013;48(4):1450–1467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Laine C, Lin YT, Hauck WW, Turner BJ. Availability of medical care services in drug treatment clinics associated with lower repeated emergency department use. Med Care. 2005:985–995. [DOI] [PubMed] [Google Scholar]
- 22.Tofighi B, Leonard N, Greco P, Hadavand A, Acosta MC, Lee JD. Technology use patterns among patients enrolled in inpatient detoxification treatment. J Addict Med. 2019;13(4):279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brettle RP. HIV and harm reduction for injection drug users. Aids. 1991;5(2):125–136. [DOI] [PubMed] [Google Scholar]
- 24.Horvath KJ, Lammert S, LeGrand S, Muessig KE, Bauermeister JA. Using technology to assess and intervene with illicit drug-using persons at risk for HIV. Curr Opin HIV AIDS. 2017;12(5):458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zlotorzynska M, Sullivan P, Sanchez T. The Annual American Men’s Internet Survey of Behaviors of Men Who Have Sex With Men in the United States: 2015 Key Indicators Report. JMIR Public Heal Surveill. 2017;3(1):e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Downing M Jr., Chiasson M, Hirshfield S. Recent anxiety symptoms and drug use associated with sexually transmitted infection diagnosis among an online US sample of men who have sex with men. J Heal Psychol. 2016;21(12):2799–2812. [DOI] [PubMed] [Google Scholar]
- 27.Center PR. Mobile Fact Sheet. https://www.pewresearch.org/internet/fact-sheet/mobile/#mobile-phone-ownership-over-time. Published 2019.
- 28.Krishna S, Boren SA, Balas EA. Healthcare via cell phones: A systematic review. Telemed e-Health. 2009;15(3):231–240. [DOI] [PubMed] [Google Scholar]
- 29.Fox S Mobile Health 2010.; 2010. https://www.pewresearch.org/internet/wp-content/uploads/sites/9/media/Files/Reports/2010/PIP_Mobile_Health_2010.pdf.
- 30.Fjeldsoe BS, Marshall AL, Miller YD. Behavior Change Interventions Delivered by Mobile Telephone Short-Message Service. Am J Prev Med. 2009;36:165–173. [DOI] [PubMed] [Google Scholar]
- 31.Downer S, Meara JG, Da Costa A. Use of SMS text messaging to improve outpatient attendance. Med J Aust. 2005;183:366–368. [DOI] [PubMed] [Google Scholar]
- 32.Tofighi B, Nicholson JM, McNeely J, Muench F, Lee JD. Mobile phone messaging for illicit drug and alcohol dependence: a systematic review of the literature. Drug Alcohol Rev. 2017;36(4):477–491. [DOI] [PubMed] [Google Scholar]
- 33.Collins KM, Armenta RF, Cuevas-Mota J, Liu L, Strathdee SA, Garfein RS. Factors associated with patterns of mobile technology use among persons who inject drugs. Subst Abus. 2016;37(4):606–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tofighi B, Campbell ANC, Pavlicova M, Hu MC, Lee JD, Nunes EV. Recent internet use and associations with clinical outcomes among patients entering addiction treatment involved in a web-delivered psychosocial intervention study. J Urban Heal. 2016;93(5):871–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ranjit YS, Shrestha R, Copenhaver M, Altice FL. Online HIV information seeking and pre-exposure prophylaxis awareness among people who use drugs. J Subst Abuse Treat. 2020;111:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boumparis N, Karyotaki E, Schaub MP, Cuijpers P, Riper H. Internet interventions for adult illicit substance users: A meta-analysis. Addiction. 2017;112(9):1521–1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Krishnan A, Cravero C. A multipronged evidence-based approach to implement mHealth for underserved HIV-infected populations. Mob Media Commun. 2017;5(2):194–211. [Google Scholar]
- 38.Thompson MA, Mugavero MJ, Amico KR, et al. Guidelines for improving entry into and retention in care and antiretroviral adherence for persons with HIV: evidence-based recommendations from an International Association of Physicians in AIDS Care panel. Ann Intern Med. 2012;156(11):817–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Noar S Computer technology-based interventions in HIV prevention: state of the evidence and future directions for research. AIDS Care. 2011;23(5):525–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lewis CF, Lekas HM, Rivera A, et al. Pharmacy PEP Access Intervention Among Persons Who Use Drugs in New York City: iPEPcare Study—Rethinking Biomedical HIV Prevention Strategies. AIDS Behav. 2020;24:1–11. [DOI] [PubMed] [Google Scholar]
- 41.Crawford ND, Amesty S, Rivera AV, Harripersaud K, Turner A, Fuller CM. Randomized, community-based pharmacy intervention to expand services beyond sale of sterile syringes to injection drug users in pharmacies in New York City. Am J Public Health. 2013;103(9):1579–1582. doi: 10.2105/AJPH.2012.301178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Crawford ND, Dean T, Rivera AV, et al. Pharmacy Intervention to Improve HIV Testing Uptake Using a Comprehensive Health Screening Approach. Public Health Rep. 2015;131 Suppl(1468–2877 (Electronic)):139–146. http://www.ncbi.nlm.nih.gov/pubmed/26862239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lewis CF, Rivera AV, Crawford ND, DeCuir J, Amesty S. Pharmacy-randomized intervention delivering HIV prevention services during the syringe sale to people who inject drugs in New York City. Drug Alcohol Depend. 2015;153:72–77. doi: 10.1016/j.physbeh.2017.03.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lewis CF, Lekas H-M, Rivera A, et al. Pharmacy PEP Access Intervention Among Persons Who Use Drugs in New York City: iPEPcare Study—Rethinking Biomedical HIV Prevention Strategies. AIDS Behav. 2020:1–11. [DOI] [PubMed] [Google Scholar]
- 45.Center PR. Internet/Broadband Fact Sheet. https://www.pewresearch.org/internet/fact-sheet/internet-broadband/. Published 2019. Accessed January 10, 2020.
- 46.Strand MA, Bratberg J, Eukel H, Hardy M, Williams C. Community Pharmacists’ Contributions to Disease Management During the COVID-19 Pandemic. Prev Chronic Dis. 2020;17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Goode JV, Owen J, Page A, Gatewood S. Community-based pharmacy practice innovation and the role of the community-based pharmacist practitioner in the United States. Pharmacy. 2019;7(3):106. [DOI] [PMC free article] [PubMed] [Google Scholar]


