1. PATIENT PRESENTATION
A 56‐year‐old previously healthy man presented to the emergency department with worsening exertional dyspnea, lower extremity weakness, bilateral periorbital edema (Figure 1), and hyperkeratosis of both palms (Figure 2). These symptoms started only 5 months earlier. On blood tests, there was a marked elevation of creatine kinase (CK:4103 U/L) and mild elevation of C‐reactive protein (CRP: 3.8 mg/dL). On chest computed tomography scan, there was an interstitial lung disease pattern with ground‐glass opacities and traction bronchiectasis (Figure 3); on echocardiography, there was only increased pulmonary artery pressure (42 mmHg) with no left ventricular dysfunction.
FIGURE 1.

Bilateral periorbital edema
FIGURE 2.

Right‐hand palm hyperkeratosis
FIGURE 3.
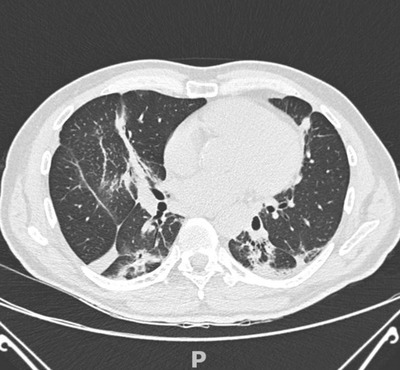
Chest high‐resolution computed tomography scan: interstitial lung disease
2. DIAGNOSIS
2.1. Jo‐1 antisynthetase syndrome with pulmonary, muscle, and dermatologic involvement
Given antisynthetase syndrome clinical suspicion (mechanic's hands, interstitial lung disease, CK and CRP elevation), 1 the patient was admitted to the pulmonary unit. Immunologic tests, including myositis‐specific, myositis‐associated, and anti‐aminoacyl‐tRNA synthetase antibodies 1 , 2 showed anti‐Jo‐1 and anti‐Ro52 positivity. The latter is also a predictor of increased severity of pulmonary manifestations and lower response to immunosuppressive treatment. 3 Clinical suspicion in the emergency department led us to exclude myocardial involvement early (8% of Jo‐1 antisynthetase syndrome) with troponin I, B‐type natriuretic peptide, and echocardiography 2 and start methylprednisolone boluses (1 g daily for 3 consecutive days) early. Rheumatologists then started immunosuppressive therapy with cyclosporine 100 mg twice a day and follow‐up with the patient. 4 The patient's symptoms improved during hospitalization, and he was discharged with an outpatient follow‐up program.
Finazzi A, Cosentini R. Man with periorbital edema, palms hyperkeratosis, and exertional dyspnea. JACEP Open. 2022;3:e12835. 10.1002/emp2.12835
REFERENCES
- 1. Katzap E, Barilla‐Labarca ML, Marder G. Antisynthetase syndrome. Curr Rheumatol Rep. 2011;13:175‐181. [DOI] [PubMed] [Google Scholar]
- 2. Masiak A, Marzec M, Kulczycka J, Zdrojewski Z. The clinical phenotype associated with antisynthetase autoantibodies. Reumatologia. 2020;58:4‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bauhammer J, Blank N, Max R, et al. Rituximab in the treatment of jo1 antibody‐associated antisynthetase syndrome: anti‐Ro52 positivity as a marker for severity and treatment response. J Rheumatol. 2016;43:1566‐1574. [DOI] [PubMed] [Google Scholar]
- 4. Witt LJ, Curran JJ, Strek ME. The diagnosis and treatment of antisynthetase syndrome. Clin Pulm Med. 2016;23:218‐226. [DOI] [PMC free article] [PubMed] [Google Scholar]


