Abstract
Extant literature investigates the impact of COVID-19 on mental health outcomes, however there is a paucity of work examining mental health distress as a risk factor for COVID-19 outcomes. While systemic variables like income inequality relate to both mental health and COVID-19, more work is needed to test theoretically informed models including such variables. Using a social-ecological framework, we aimed to address these gaps in the literature by conducting a neighborhood-level analysis of potential mental health distress and systemic- (income inequality) level predictors of reported COVID-19 infection and mortality over time in Chicago. Neighborhood-level comparisons revealed differences in mental health distress, income inequality, and reported COVID-19 mortality, but not reported COVID-19 infection. Specifically, Westside and Southside neighborhoods generally reported higher levels of mental health distress and greater concentration of poverty. The Central neighborhood showed a decline in reported mortality rates over time. Multi-level negative binomial models established that Zip-codes with greater mental health distress were at increased reported COVID-19 infection risk, yet lower mortality risk; Zip-codes with more poverty were at increased reported COVID-19 infection risk, yet lower mortality risk; and Zip-codes with the highest percentage of People of Color were at decreased risk of reported COVID-19 mortality. Taken together, these findings substantiate Chicago neighborhood-level disparities in mental health distress, income inequality, and reported COVID-19 mortality; identify unique differential associations of mental health distress and income inequality to reported COVID-19 infection and reported mortality risk; and, offer an alternative lens towards understanding COVID-19 outcomes in terms of race/ethnicity.
Keywords: Income inequality, Mental health distress, COVID-19 infection, COVID-19 mortality, Neighborhood-level analysis
Highlights
-
•
Zip-codes with more mental health distress had higher infection risk
-
•
Zip-codes with more mental health distress had reduced mortality risk
-
•
Zip-codes with higher affluence showed higher infection risk
-
•
Zip-codes with higher poverty concentration showed higher mortality risk
-
•
Zip-codes with higher proportion of PoC had decreased infection risk
1. Introduction
The coronavirus disease 2019 (COVID-19) has escalated into a devastating pandemic, with over 615 million confirmed cases and over 6.5 million deaths reported to the World Health Organization as of October 4, 2022 [1]. However, it is not universal to either acquire or die from COVID-19. Variable infection and mortality rates have yielded a call to action: to better understand risk and protective factors of these COVID-19 outcomes [2]. Extant research has identified a number of risk factors for reported COVID-19 mortality, including male sex, older age, obesity, and underlying health conditions [[3], [4], [5], [6], [7]]. Communities of color are at increased risk for reported COVID-19 mortality [8,9]. At the national level, nearly 60% of COVID-19 deaths were accounted for by individuals in primarily Black U.S. counties, despite these counties representing only 20% of the sample [10].
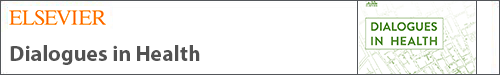
Early narratives seeking to explain these trends fail to account for some of the systemic and multi-level factors that may contribute to disparities in reported COVID-19 infection and mortality for many historically disenfranchised communities [11,12]. An adaptation of the County Health Ranking Framework offers a lens to understand the multi-level socio-systemic factors that may relate to COVID-19 outcomes, see Fig. 1. Unequal distribution of income is a specific social determinant of health (SDOH) with strong links to reported COVID-19 infection and mortality [13,14]. It is consistent with Bronfenbrenner's Social-Ecological Model [15] that individuals with low income living in high-income inequality areas would report low healthcare access and utilization [16], crowded housing, and continued in-person work as essential workers amid the COVID-19 pandemic [17,18]. Empirically, income inequality has been associated with premature mortality at multiple levels of spatial-health investigation, even after controlling for socioeconomic status, age, and sex [[19], [20], [21]]. In the context of the pandemic, income inequality has been related to increased associations with reported COVID-19 mortality, however these associations have yet to be assessed at neighborhood levels [13,14,21]. Additionally, some international research suggests that economic deprivation may be associated with COVID-19 infection, but not COVID-19 mortality [22]. Additional investigation would provide useful insight into social-ecological conditions and COVID-19 outcomes.
Fig. 1.
Adapted theoretical framework based on the county health rankings model.
While the County Health Ranking Framework [23] offers insight into health behaviors, clinical care, physical environment, and social/economic factors that relate to health outcomes, many applications of the model do not delineate an important factor highlighted in social-ecological literature – mental health [[23], [24], [25]]. Mental health distress, defined as a state of emotional suffering associated with daily stressors [26], relates to poor mental and physical health outcomes [27,28] and may be another risk of COVID-19 infection and mortality. Since the start of the pandemic, much literature has examined COVID-19's impact on mental health, [[29], [30], [31]], and generally suggests that mental health difficulties both spiked and persisted since the pandemic onset [32] – potentially exacerbating mental health difficulties for individuals with pre-existing mental illness [33]. However, much less work has examined the inverse – mental health distress as a risk factor for reported COVID-19 outcomes. Researchers theorized that individuals with serious mental illness (SMI) may be at higher risk of COVID-19 exposure, infection, and mortality due to lower health literacy, negative health-related behaviors, lower treatment adherence, and greater obstacles to quarantine adherence (e.g., homelessness) [34]. Related empirical findings are mixed, showing that having a mental illness diagnosis was not associated with likelihood of testing positive for COVID-19 [35]; however, other research suggests that communities with elevated COVID-19 infection rates also showed elevated levels of pre-pandemic mental health distress [36]. In one study, individuals with SMI were at higher risk for severe clinical outcomes of COVID-19 than those with no history of mental illness [35]. In another study, adults diagnosed with schizophrenia spectrum disorder had higher increased risk for reported COVID-19 mortality than those without such diagnosis. However, those with mood and anxiety disorders were no more at risk for reported COVID-19 mortality than those without a diagnosis [37]. Among individuals with a mental health disorder, those who were African American had higher odds of COVID-19 infection than those who were White, and women had higher odds of reported COVID-19 infection than men [38].
Together, this suggests an unclear understanding of mental health in relation to COVID-19 infection and mortality. Additionally, little work considers these associations in the context of systemic-level variables such as income inequality. Income inequality is related to reporting mental health distress, experiencing an increased risk for and incidence of mental illness, and worsening health outcomes among those affected by poor mental health. These findings have been reported at individual [39], county [40], and state levels [41]. More broadly, income inequality and mental health distress often simultaneously relate to health outcomes [[42], [43], [44]]. Despite this, investigations at the Zip-code level examining how strongly each of these factors relate to COVID-19 are only recently emerging [45]. This parallels the concept of social vulnerability, which asserts that social, economic, demographic, and geographic characteristics determine risk exposure of a community and their ability to respond to and recover from adversity [46]. That is, vulnerability is a socially constructed condition of a system that exists before it is faced with a threat that intensifies its effects [[46], [47], [48], [49], [50], [51]]. Testing models consistent with this social-ecological and social vulnerability perspective that focus on COVID-19 outcomes would make an important contribution to literature [[52], [53], [54]].
Chicago is a relevant place to investigate such socio-structural risk factors of reported COVID-19 infection and mortality. As of November 2022, Chicago had 718,355 positive COVID-19 cases, and Illinois itself had the fifth-most cases of any U.S. state [55]. Chicago also demonstrates significant racial/ethnic disparities in its COVID-19 outcomes, thus providing a location where researchers can investigate COVID-19 as a potential microcosm for broader racial/ethnic health disparities. Of all reported COVID-19 cases in Chicago, White individuals showed an infection rate of 6118.7 and death rate of 569.9 per 100,000 individuals [56]. Black individuals showed an infection rate of 6950.9 and a death rate of 1604.6 per 100,000 individuals [56]. Latino or Hispanic individuals showed an infection rate of 12,248.8 and a death rate of 1042.7 rate per 100,000 individuals [56]. These numbers starkly contrast the racial/ethnic makeup of Chicago, which is 50% White, 29.6% Black, and 28.8% Latino or Hispanic [55,57]. More broadly, Chicago has a deep history of systemic racism, making Chicago and its four prominent neighborhoods (Northside, Central or “Loop”, Westside, and Southside) some of the most racially-segregated geographic spaces in the U.S [46,58]. Racial segregation in Chicago has had long-lasting impacts, particularly on health for individuals in marginalized neighborhoods [58,59]. A recent study found that life expectancy was 90 years old for those living in Streeterville, a predominantly White neighborhood in Central Chicago, but just 60 years old for those living in Englewood, a predominantly Black community in the Southside neighborhood just nine miles away [60].
The present study aims to assess associations between these socio-structural variables in relation to COVID-19 infection and mortality in the historically segregated city of Chicago, using neighborhood-level data. First, we conduct neighborhood-level comparisons of income inequality and mental health distress, hypothesizing higher rates of each in neighborhoods that literature identifies as those occupied primarily by racial/ethnic minority individuals (i.e., Westside and Southside). Next, we conduct neighborhood-level comparisons of reported COVID-19 infection and mortality risk rates over time using multi-level linear growth modeling. We hypothesize that these same racial/ethnic-majority neighborhoods will show increased risk for these COVID outcomes. Then, we test whether Zip-code level income inequality and mental health distress serve as significant exposures to risk of reported COVID-19 infection and mortality over time, via multilevel negative binomial regression modeling, while controlling for several key covariates. We hypothesize that neighborhoods with increased mental health distress and higher concentrations of poverty experience increased risk for COVID-19 infections and mortality across neighborhoods. We also hypothesize that neighborhoods with higher proportions of people of color (PoC) will demonstrate increased risk for COVID-19 outcomes compared to neighborhoods with lower proportions of PoC within Zip-codes.
2. Methods
All data were obtained through the City of Chicago Coronavirus Response Center Data Portal (CRCDP), City Health Dashboard (CHD), and Chicago Health Atlas (CHA). The CRCDP was created in part by the Department of Public Health and has been used in several emerging COVID-related publications in Chicago [46,61,62]. CRCDP data includes reports from the Illinois National Electronic Disease Surveillance System, Cook County Medical Examiner's Office, Illinois Vital Records, and the US Census Bureau 2018 American Community Survey (ACS). The CHD is a national data resource of health-related measures for over 750 cities across the U.S. and is a frequently cited data source in the established literature [54,63]. Similarly, the CHA is a community health data resource of aggregated data from several sources, including the ACS. Key study variables included in the CHD and CHA were obtained from the US Census Bureau 2018 ACS and the CDC's PLACES Project. Present study data were extracted from these two sources at the Zip-code level. To align with a quasi-longitudinal approach, we used mental health distress- and income inequality-predicted estimates and related estimates for our control variables for 2018 – the most recent shared year-point of all variables. Both COVID-19 infection and mortality reflect respective cumulative reported cases as of July 17, 2021.
2.1. Measures
A total of 60 Zip-codes are captured within the city of Chicago. Given that many Zip-codes are often colloquially categorized with a multi-neighborhood spatiality (e.g., Southwest, Northcenter) and data sources themselves list individual Zip-codes in multiple broader neighborhoods and higher-level amalgamations of neighborhood clusters, we categorized the data gathered from CRCDP and City Health Dashboard into four categories – Northside, Southside, Westside, and Central. This was done via comprehensive comparison of community areas identified within existing data available from the CHA [64] and 2014–2016 Community Health Needs Assessment [65]. While no method of categorization is without error, we approach this categorization through a synthetization of two existing classification systems for Chicago to achieve a more standardized categorization. Each of the following variables are aggregated and analyzed at the Zip-code level.
2.1.1. Outcomes
2.1.1.1. COVID-19 infection and mortality
Cumulative COVID-19 infection and mortality reported counts were obtained from the CRCDP. For these data, Chicago residents are included based on the home Zip-code provided by the medical provider of each reporting entity. Cases with a positive molecular or antigen test are included in this dataset and are counted based on the week in which the specimen was collected, to account for variability in testing time lapse from receiving initial COVID-19 testing. Two separate variables are included, where values represent cumulative infection cases and cumulative mortality cases in Chicago, by Zip-code, among Chicago residents. Reported COVID-19 infection and mortality variables are updated weekly on the CRCDP, and we use data gathered across 72 consecutive weeks, spanning from March 1, 2020 to July 17, 2021 to reflect initial outcomes to this public health threat.
2.2. Risk factors
2.2.1. Mental health distress
Frequency of mental health distress was obtained from the CHD, using 2018 1-year modeled estimates from the CDC PLACES project. This mental health distress frequency index was calculated as a percentage of adult respondents who reported poor mental health ≥14 days in the past month per total Zip-code level population and represents a mental health-related quality of life within each Zip-code. This operationalization is consistent with clinical criteria for select mental health disorders [66], functional impairment [67], public health surveys [64,68], and related extant research [[69], [70], [71], [72], [73], [74], [75], [76]]. With that said, this current method of assessment allows variable conceptualization of “distress” and thus may also capture distress on a broader level that is sub-clinical threshold.
2.2.2. Income inequality
The Index of Concentration at the Extremes (ICE) is a measure of income inequality obtained from the CHD and is calculated though the following formula applying income distributions for each respective geographical area or concentration [77]:
Specifically, we used the 2018 5-year ACS estimates, representing pooled estimates across multiple years of data, and scores range from −100 (all households are financially deprived) through +100 (all households are financially privileged; [59]). As such, ICE allows for a description of size and direction of income inequality within geographic areas and is argued to be a more robust measure than the popular Gini index of income inequality at the census tract [77]. While race/ethnicity itself is not explicitly measured in this variable, income inequality is often expressed as a proxy for and product of systematic racism and has racial implications. In fact, there is growing support for ICE as an indicator of historical structural racism, particularly for marginalized communities [78]. Therefore, we use and interpret findings from this variable in both the context of income inequality and race/ethnicity as a function of the city of Chicago itself, though we address race/ethnicity specifically through a designated assessment of PoC concentration.
2.3. Covariates
Other than the inclusion of Race/Ethnicity as a covariate, we focus on modifiable health behaviors available from our publicly assessable data sources as covariates for inclusion in our models. This is because health behaviors relate to health outcomes, within the context of other social determinants of health, including socio-structural and environmental drivers of health [79,80]. As such, we include health behaviors highlighted in the County Health Ranking Framework as covariates in our analyses. We also provide supporting literature surrounding their specific associations to COVID-19 below.
2.3.1. Race/Ethnicity
Race/Ethnicity are obtained from the CHA, using 2018 5-year moving averages from the ACS. Racial/ethnic categories include Non-Hispanic White, Non-Hispanic Black, Asian or Pacific Islander, Hispanic or Latino, Native American, or two or more races. Here, we obtained the total estimated number of Non-Hispanic White individuals within each respective Zip-code and created a ratio to the estimated total population within each Zip-code. We then categorized each ratio into one of three broader groupings based on the mean ratio of reported Non-Hispanic White concentration. Ratios that fell above one standard deviation of the mean represent higher concentration of Non-Hispanic White identities and were labeled “low PoC” density Zip-codes. Ratios that fell below one standard deviation of the mean represented lower concentration of Non-Hispanic White identities and were labeled “high PoC” density Zip-codes.
2.3.2. Binge drinking
Binge drinking among adults aged ≥18 years was obtained using CDC PLACES project 2018 1-year modeled estimates. Binge drinking is defined as women who reported consuming ≥ four alcoholic drinks on one occasion and men who reported consuming ≥ five alcoholic drinks on one occasion in the past 30 days [81]. These benchmarks parallel several standardized measures of hazardous drinking [82,83], a behavior known to compromise immunological functioning and place individuals at higher risk for COVID-19 [84]. Excessive alcohol use is also known to associate with lung damage and increase susceptibility to respiratory illness and COVID-19 susceptibility and severity [85]. As bring drinking is a modifiable behavior, we include neighborhood level of binge drinking as a percentage-based covariate at the Zip-code level.
2.3.3. Physical inactivity
Physical inactivity among adults aged ≥18 years was obtained using CDC PLACES project 2018 1-year modeled estimates, specifically by denying all past month physical activities or exercises such as running, calisthenics, golf, gardening, or walking for exercise [81]. Physical inactivity itself is a known correlate of increased risk for COVID-19 outcomes [86], and is a known protective factor against several other health conditions that increase risk for COVID-19 susceptibility and severity (i.e., diabetes, cardiovascular disease, obesity) [87]. As physical inactivity is a modifiable behavior, we include physical inactivity as a as percentage-based covariate at the Zip-code level.
2.3.4. Smoking
Smoking among adults aged ≥18 years was obtained using CDC PLACES project 2018 1-year modeled estimates, representing respondents reporting having smoked ≥100 cigarettes in their lifetime and current daily or near-daily smoking [81]. Smoking appears to have a somewhat paradoxical and not well understood association to severity of COVID-19 outcomes, yet is also associated with several disease factors that promote poorer COVID-19 outcomes [88,89]. As smoking is a modifiable behavior, we included smoking as a percentage-based covariate at the Zip-code level to account for potential variance explained by this construct.
2.4. Analytic plan
We used Stata version 15 for all central study analyses. All data were screened for normality. Reliability ratings for each variable are not reported due to each exposure index being a single-item, Zip-code-level index. Sample characteristics were calculated using univariate descriptive and frequency statistics. Neighborhood-level differences of the variables of interest were tested using one-way between-groups ANOVA in SPSS version 28 and multi-level linear growth models. Predictive margins were estimated to further probe differences of conditional effects. Aligning with statistical methods of existent COVID-19 literature, multi-level negative binomial regression was used to calculate incidence rate ratios to measure the effects of Zip-code level income inequality and mental health distress on reported COVID-19 infection (cumulative cases, controlling for population within Zip-code) and mortality (cumulative deaths, controlling for population within Zip-code), respectively [22,[90], [91], [92], [93]]. Negative binomial distribution was used to account for overdispersion in each dependent variable. Likelihood ratio chi-square tests were performed to test the insufficiency of a more parsimonious Poisson model.
To identify whether there is spatial variation between income inequality, people of color, and mental health distress with cumulative COVID-19 case and mortality rates, we conducted geographically weighted regression (GWR) using the final timepoint of data. The GWR model creates a separate regression equation for each identified location, allowing the association to vary across Chicago. The GWR models used the golden search neighborhood selection method to identify the optimal distance band. All GWR models were adjusted for income inequality, people of color, and mental health distress. The coefficients were mapped. Geospatial autocorrelation, geographic weighted regression, and maps were generated in ArcGIS Pro version 2.18.
3. Results
3.1. Descriptive statistics
Our sample reflects available data from Zip-codes that comprise Northside (n = 17; 15.3%), Southside (n = 19; 28.8%), Westside (n = 14; 23.7%), and Central (n = 9; 32.2%) neighborhoods. In aggregate, 12.92% (2.87) of the adults ≥ 18 years old in our sample reported ≥14 days of poor mental health within the past month prior to data collection. Our sample's level of income inequality (−5.53) showed higher concentration of poverty than the CHD average (−1.1) [94]. At the final timepoint the data used in this study, our sample had a reported average cumulative COVID-19 infection of 9841.31(SD = 2631.52) cases, and mortality of 178.05 (SD = 95.13) cases, per 100,000 residents.
3.2. Neighborhood-level comparison
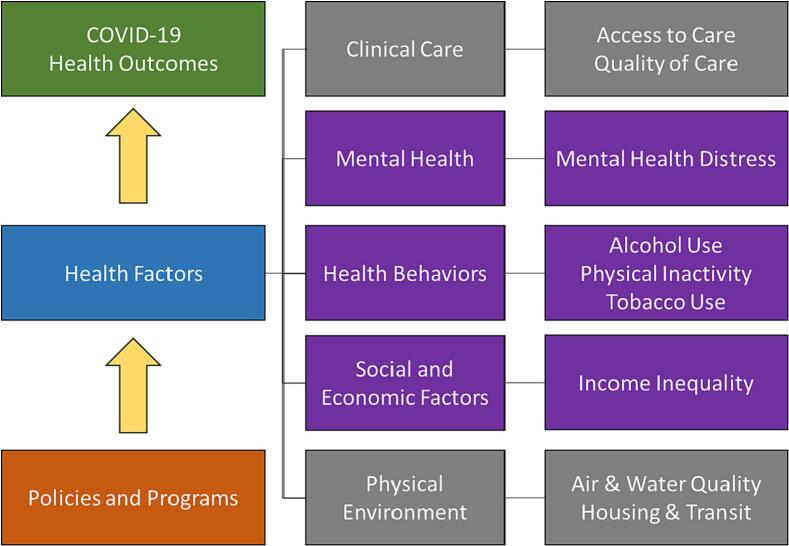
A one-way between-groups ANOVA was conducted to explore neighborhood-level differences in income inequality and mental health distress. Results indicated significant between-group differences for both variables. Levene's test for income inequality suggested that using the Tukey HSD approach was an appropriate probe for multiple post-hoc comparisons. Data for mental health distress violated the assumptions of homogeneity of variance per the Levene's test; therefore, Dunnett's T3 approach was used to probe for multiple post-hoc comparisons. Post-hoc analysis of the income inequality variable indicated that the Westside neighborhoods had a higher concentration of individuals at the lower end of the income extreme than the Central neighborhoods. Additionally, the Southside neighborhoods had a higher concentration of individuals at the lower end of the income extreme than both the Central and Northside neighborhoods. Post-hoc analysis of the mental health variable indicated that the Westside and Southside neighborhoods had more frequent days of mental health distress compared to the Central and Northside neighborhoods. Spatial autocorrelation analysis of key variables of interest revealed significant clustering similarities for Income Inequality (Moran's I = 0.47, p < .001) and Mental Health Distress (Moran's I = 0.41, p < .001) (See Fig. 2).
Fig. 2.
Neighborhood-level differences in key study predictor variables.
Logarithmic transformation of Y-axis was used to ease visual graphing interpretability of mental health distress and ICE in a single figure; however, the data themselves were not transformed. Significant differences exist between neighborhoods and mental health distress rates: F(3, 51) = 10.40, p < .001. Post-hoc comparison using Dunnet's T3 test indicated that the mean levels of mental health distress were significantly higher for both Westside (M = 13.88, SD = 3.11) and Southside (M = 14.65, SD = 2.46) when compared to Central (M = 9.93, SD = 1.98) and Northside (M = 11.23, SD = 1.20) neighborhoods independently All other mental health distress paring comparisons were non-significant, ps > 0.05. Significant differences exist between neighborhoods and income inequality: F(3, 51) = 13.56, p < .001. Post-hoc comparison using Tukey HSD test indicated that the mean ICE index was higher for Central (M = 31.18, SD = 13.12) compared to Westside (M = −9.43, SD = 16.51) and Southside (M = -24.44, SD = 20.93) neighborhoods. Additionally, Northside (M = 6.57, SD = 16.51) showed significantly higher ICE scores than Southside (M = −24.44, SD = 20.93) neighborhoods. All other ICE comparisons were non-significant, ps > 0.05 Error Bars: 95% CI.
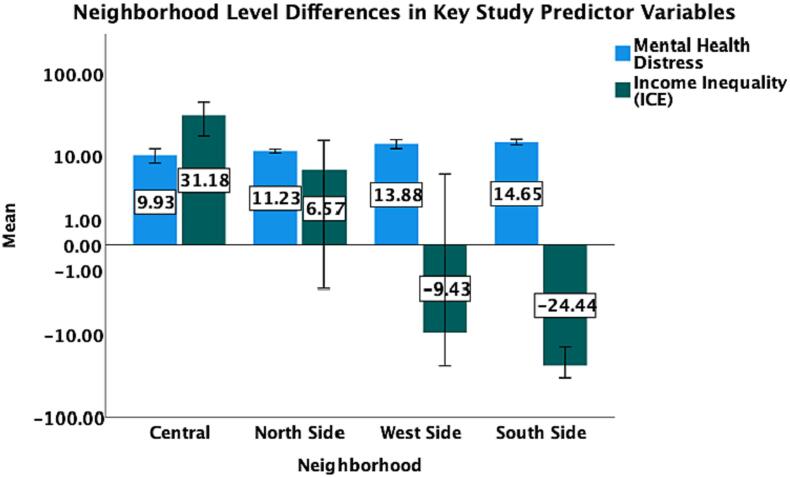
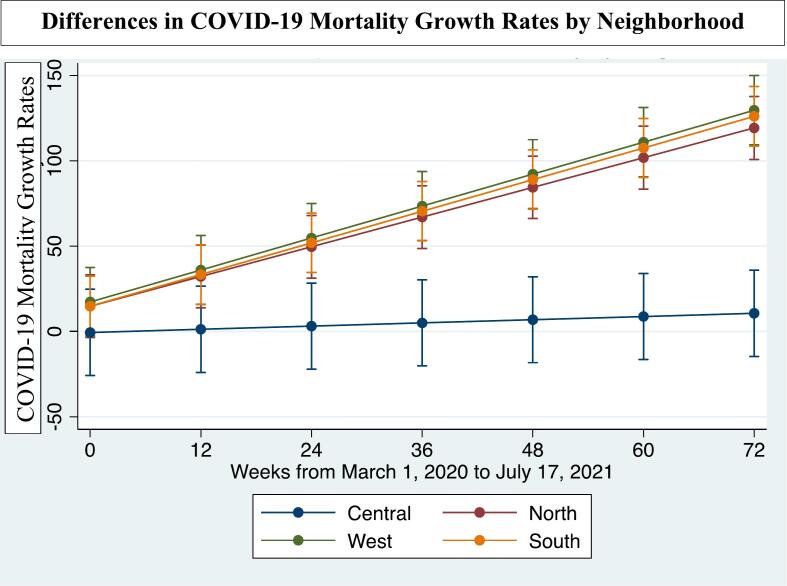
Multi-level linear growth models were conducted to explore differences at the neighborhood-level in reported COVID-19 infection and mortality, controlling for population density. For reported COVID-19 infection rates comparing the Central neighborhoods to more distal neighborhoods, differences were not significant (North: b = 12.142, SE = 6.803, p = .07; West: b = 7.182, SE = 6.976, p = .30; South: b = 6.221, SE = 6.609, p = .35). Margins analysis comparing Central neighborhoods to North, West, and South indicated that mortality rates stabilized only for the Central neighborhood (North: b = 1.294, SE = 0.348, p < .001; West: b = 1.404, SE = 0.361, p < .001; South: b = 1.388, SE = 0.342, p < .001). See Fig. 3, Fig. 4. Similarly, spatial autocorrelation analysis of variables of interest revealed clustering similarities for the most recent cumulative COVID-19 mortality rate (Moran's I = 0.30, p < .001; however, not for the most recent cumulative COVID-19 infection rate (Moran's I = −0.10, p = .15).
Fig. 3.
Differences in COVID-19 infection growth rates by neighborhood.
Margins analysis with Central neighborhood as the reference comparisons showed no significant differences between neighborhoods regarding COVID-19 infection growth rates across 72 weeks. Descending trajectories represent decline in growth rate, rather than decline in total infections.
Fig. 4.
Differences in COVID-19 mortality growth rates by neighborhood.
Margins analysis with Central neighborhood as the reference comparison showed stabilization of COVID-19 mortality growth rates for only the Central neighborhood across 72 weeks.
3.3. Geographic weighted regression
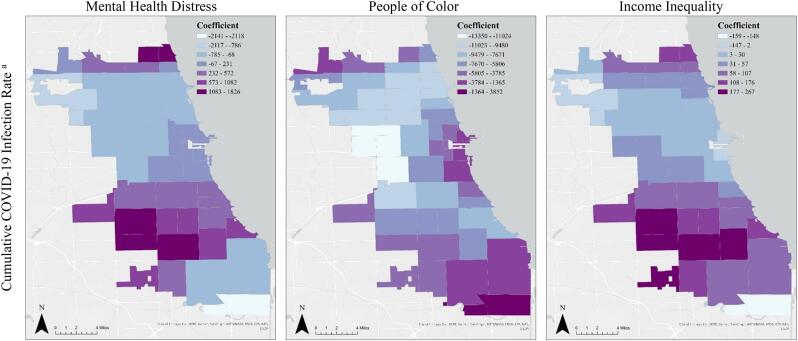
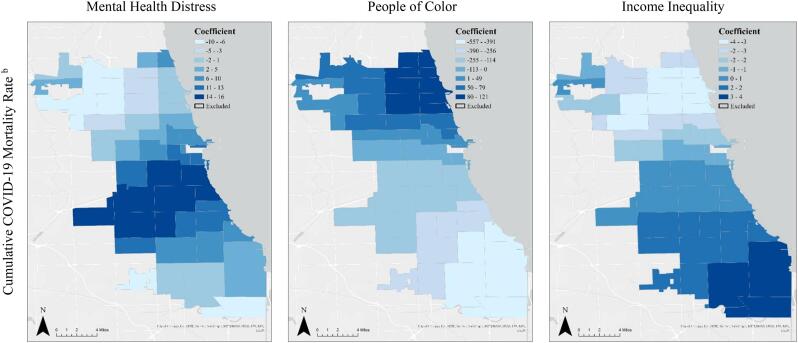
The results of the GWR can are presented in Fig. 5 and Fig. 6. Mental Health distress had the strongest, positive associations with COVID-19 infection and mortality rates predominantly in the Southside and Westside. Mental Health distress was negatively associated with both COVID-19 infection and mortality rates in the Northside of Chicago. There only were negative associations between the density of PoC and COVID-19 Infection Rates across the city. The strongest, most negative associations were identified in the Northside. While the least negative associations were identified in the Southside. COVID-19 mortality was positively associated with density of PoC in the Northside, but had strong, negative associations in the Southside. For income inequality, higher concentrations of poverty had the strongest positive associations with COVID-19 infection and mortality rates in the Southside of Chicago, with notable strengths of association in the Westside of Chicago. The strongest negative associations for infection and mortality rates were predominantly located in the Northside.
Fig. 5.
Geographic weighted regression of key predictors and COVID-19 infection.
aGWR model was adjusted for mental health distress, people of color, and income inequality. It used a distance band of 14,951.6 m. R2 = 0.57, Adjusted R2 = 0.38, AICc = 1055. Cumulative COVID-19 infection and mortality rates reflect rates as of the final timepoint in our data – July 17, 2021.
Fig. 6.
Geographic weighted regression of key predictors and COVID-19 mortality.
bGWR model was adjusted for mental health distress, people of color, and income inequality. It used a distance band of 18,092.1 m. R2 = 0.68, Adjusted R2 = 0.57, AICc = 628. Cumulative COVID-19 infection and mortality rates reflect rates as of the final timepoint in our data – July 17, 2021.
3.4. Multivariable models
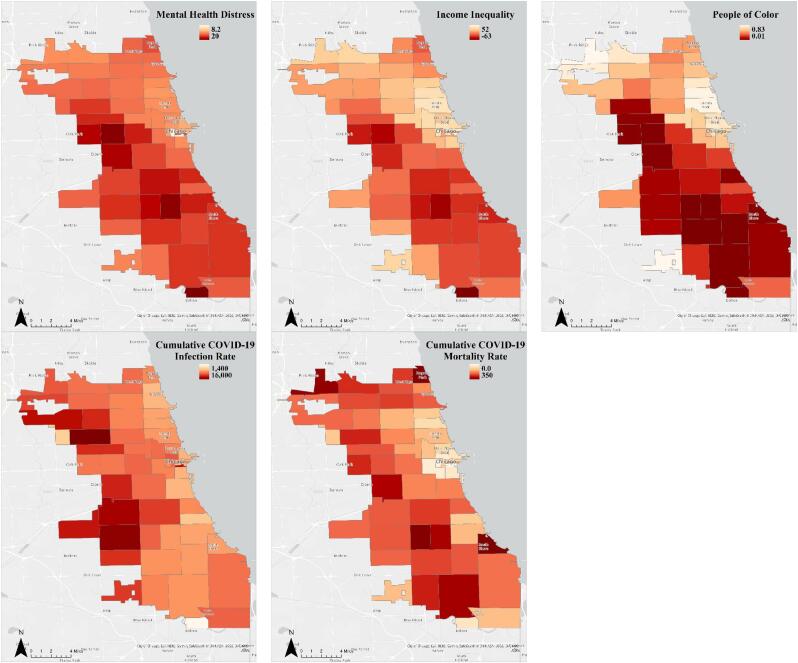
Two multi-level negative binomial regression models were conducted to evaluate whether Zip-code level determinants of income inequality, mental health distress, racial diversity, smoking status, binge drinking, physical inactivity, and time were associated with increased risk of COVID-19 infection and mortality, respectively. For the COVID-19 infection model, the likelihood ratio chi-square test indicated that the negative binomial distribution had superior fit to the Poisson model (19.95, p < .0001). There was a significant increased risk over 72 weeks for reported COVID-19 infection in Zip-codes with a greater proportion of mental health distress (IRR = 1.058, p < .01), greater concentrations of wealth (IRR = 1.006, p < .01), less reported binge drinking (IRR = 0.991, p < .01), less sedentary behavior (IRR = 0.989, p < .01), less binge drinking (IRR = 0.991, p < .01) and in Zip-codes with larger populations (IRR = 1.006, p < .001). Smoking, Zip-code density of PoC, and time did not significantly relate to risk for reported COVID-19 infection; see Table 1. For the COVID-19 mortality model, the likelihood ratio chi-square test indicated that the negative binomial distribution had superior fit to the Poisson model (3447.16, p < .0001), There was a significant increased risk over 72 weeks for reported COVID-19 mortality in Zip-codes with a lower proportion of mental health distress (IRR = 0.732, p < .05), less smoking (IRR = 0.979, p < .05), higher concentration of poverty (IRR = 0.954, p < .01), higher physical inactivity (IRR = 1.045, p < .05), and Zip-codes with larger populations (IRR = 1.029, p < .001). Additionally, Zip-codes with moderate (IRR = 0.307, p < .01) and high (IRR = 0.293, p < .05) proportions of PoC demonstrated lower risk for COVID-19 mortality, compared to Zip-codes with lower proportions of PoC. Bing drinking was not significantly associated with COVID-19 mortality risk; see Table 1. VIF = 5.1 for our multivariable model. Fig. 7 provides cross-sectional mapping of key variables at week 72.
Table 1.
Multi-level negative binomial regression models.
| Predictor | IRR (SE) | p-value | 95% CI | |
|---|---|---|---|---|
| COVID-19 Infection | Income Inequality | 0.006 (0.002) | <0.01 | (1.003, 1.010) |
| Population | 1.006 (0.001) | <0.001 | (1.003, 1.009) | |
| Binge Drinking | 0.991 (0.003) | <0.01 | (0.985, 0.996) | |
| Physical Inactivity | 0.989 (0.003) | <0.01 | (0.983, 0.995) | |
| Smoking | 1.000 (0.001) | 0.77 | (0.998, 1.003) | |
| PoC moderate PoC high |
1.083 (0.068) 1.013 (0.092) |
0.210 .89 |
(0.957, 1.226) (0.849, 1.210) |
|
| Mental Health Distress | 1.058 (0.018) | <0.01 | (1.024, 1.093) | |
| Time | 1.000 (0.001) | 0.92 | (0.999, 1.001) | |
| COVID-19 Mortality | ||||
| Income Inequality | 0.956 (0.013) | <0.01 | (0.930, 0.982) | |
| Population | 1.047 (0.010) | <0.001 | (1.027, 1.067) | |
| Binge Drinking | 1.002 (0.020) | 0.91 | (0.963, 1.043) | |
| Physical Inactivity | 1.045 (0.023) | <0.05 | (1.002, 1.090) | |
| Smoking | 0.979 (0.009) | <0.05 | (0.962, 0.996) | |
|
PoC moderate PoC high |
0.307 (0.1347)0 .293 (0.1833) |
<0.01 <0.05 |
(0.131, 0.724) (0.086, 0.995) |
|
| Mental Health Distress | 0.732 (0.089) | <0.05 | (0.577, 0.928) | |
| a | Time | 1.030 (0.004) | <0.001 | (1.029, 1.030) |
p < .05 and examination of confidence intervals was used to determine significance in our multi-level negative binomial regression models.
Fig. 7.
Spatial mapping of key variables by zip-code.
Cumulative COVID-19 infection and mortality rates reflect rates as of the final timepoint in our data – July 17, 2021. Due to the nature of the data, maps are structured with color scheme that aid in interpretive nature of variables. Specifically, Income Inequality and People of Color maps are structured in such that lower values represent higher frequency of the interpreted variable, given the nature of the data used.
4. Discussion
The present study used Chicago-based data to examine income inequality and mental health distress as risks for reported COVID-19 infection and mortality; and, to investigate differences in COVID-19 outcomes for Chicago-based communities of color. Neighborhood-level comparisons of key study variables indicated that Westside and Southside neighborhoods generally showed higher concentration of low income and higher levels of mental health distress. Zip-codes with higher pre-existing mental health distress demonstrated increased risk for reported COVID-19 infection, yet decreased risk for reported COVID-19 mortality. Income inequality was a risk factor for reported COVID-19 infection for Zip-codes with higher concentration of wealth, and also was related to a significant increase in reported COVID-19 mortality risk rates in Zip-codes with higher concentrations of poverty. While some model covariates showed paradoxical associations that are not well understood in existing literature, we included covariates in our analyses to separate covariate effects from effects of key variables that were central to this study. Using GWR, we identified that there was city-wide variability in the associations between mental health distress, people of color, and income inequality with cumulative COVID-19 infection and mortality rates. Given that GWR shows several instances of Southside and Westside neighborhoods strongly relating to neighboring Zip-code data values, we discuss these findings with a lens underscoring the phenomenological segregative nature of Chicago and abstain from discussion of endogenous control variables, as recommended by Hünermund & Louw [95].
Many of our findings substantiate earlier work indicating that broadly, Westside and Southside Chicago neighborhoods experience more systemic- and neighborhood-level distress and systemic challenges than other Chicago neighborhoods [96]. Exposure to lead, decreased healthcare access, and higher crime rates are primary examples, with highest exposure in Southside and Westside neighborhoods compared to other Chicago neighborhoods [[96], [97], [98]]. Regarding mental health, emergent research exists supporting the association of increased COVID-19 infection risk with pre-existing mental health distress [36]; however, a comprehensive understanding of mental health as a determinant of COVID-19 outcomes, particularly mortality, remains unknown. Additionally, the income inequality-mortality link is unsurprising, given that income inequality increases the prevalence of poverty, generates chronic stress, and erodes protective measures of an individual's health – each of which can both produce community-level stress and increase an individual's risk for COVID-19 death [94,99]. These multiple and interrelated disparities indicate the need for effective systemic, neighborhood-level interventions addressing such factors [100].
Interestingly, several findings emerged that contrast existing literature. Zip-code level mental health distress was associated with reported COVID-19 mortality risk rates; however, the directionality of these associations was not fully consistent with our hypotheses. COVID-19 mortality findings are inconsistent with findings regarding other illnesses, such as cancer mortality, cardiovascular disease mortality, and other-cause mortality in extant research [101]. Psychological distress generally, largely relates to disease progression [102], however this was not the case for our sample with regard to reported COVID-19 mortality. Broadly, individuals with mental illness have greater physical health morbidity and mortality compared to general population members [103,104], which may partially explain our findings of elevated risk for COVID-19 infection in communities with elevated mental health distress. However, our findings regarding mental health and COVID-19 mortality contrast those in the existing literature and may be explained by some version of the habituation effect driven by resiliency.
The notion of psychophysiological habituation to stress parallels findings of childhood adversity and cortisol response to stress in adulthood [105], cardiovascular responses to stress [106], and amygdala response to threatening stimuli [107]. In the context of this study, it is possible that communities that experience more frequent mental health distress have developed emergent resilience, defined as an adaptation to chronic difficulties. Emergent resilience thus may contribute to an overall balanced psychophysiological response to new stressors [108]. Research shows that mental health disturbances such as anxiety, depression, and loneliness may have been experienced strongest at the start of the COVID-19 pandemic; however, symptoms either stabilized (i.e., habituated) or declined overall [109]. Symptoms among groups more vulnerable to poorer mental health during the COVID-19 pandemic experienced small decreases [109], and may suggest that on an aggregate level, communities that experienced increased mental health distress prior to COVID-19 may have habituated to the emergent stressor over time and countered the traditional associations of mental health distress and poor physical health.
That said, it is possible that pre-existing mental health distress may have manifested as anxiety or depression amid the COVID-19 pandemic. Anxiety is associated with increased healthcare utilization across multiple care settings [110], and individuals living with depression have displayed increased healthcare utilization amid the pandemic [111]. Thus, communities with pre-existing elevations in mental health distress may have increased utilization of healthcare services at the community-level in response to increased COVID-19 infections. Increased engagement in mental health services may have reduced parallel barriers towards engagement in healthcare broadly, such as though telehealth services.
However, the finding of higher concentrations of wealth positively associating to reported COVID-19 infection is unexpected, indicating that higher concentrations of lower income may disproportionately associate with COVID-19 disease progression and prognosis despite a heightened risk of reported COVID-19 infection among more affluent Zip-codes. It is possible that more affluent Zip-codes may have greater resources aiding in the ability to disperse, thus increasing exposure to COVID-19 and increased infection rates. Or those of more affluent Zip-codes may me more likely to report COVID-19 infection than their counterparts, due to increased healthcare access. Related to affluent Zip-code residents having relatively good healthcare, more affluent Zip-codes showed lower risk for COVID-19 mortality. This may be explained by increased access and ability to utilize resources in place to protect health.
The recognition that historically Black and Brown low-income neighborhoods endure a disproportionate number of physical health casualties is unfortunately familiar [97]. Social deprivation in these neighborhoods has long been an indicator of compromised health, such as low birth weight, higher rates of infant mortality, heart disease, and cancer [77,112]. One theory that may explain these findings is Massey's (2004) Biosocial Model of Stratification, particularly in that environmental stressors generated by income inequality (i.e., unequal access to resources; exposure to violence) produces allostatic load in the body [113]. This “wear and tear” associated with life in under-resourced, low-income neighborhoods, in which Black and Brown Chicagoans disproportionately reside, may elevate rates of physical and mental health problems, including reported COVID-19 related mortality [97,114]. Specific to Chicago, the Southside and Westside neighborhoods of the city endure structural barriers to healthy food [115] and quality healthcare access [116]. Similarly, due to historical redlining practices, residents of these neighborhoods are more likely to live in areas with lead poisoning [97] and toxic air pollution exposure compared to residents in the North and Central areas of Chicago [117]. The combination of these factors, among others, may both contribute to the allostatic load that neighborhood residents experience and explain the higher rates of reported COVID-19 related mortality in our findings.
However, the Cultural Armamentarium Hypothesis may also be used to explain our findings, in that individuals of specific cultures may retain culture-based practices (e.g., shared norms, family support, alcohol abstinence) that may protect these communities from negative health outcomes. These benefits may exist above and beyond the associations of mental health distress and poorer health outcomes established in research. Pertinent to this study, neighborhoods that endorsed higher rates of mental health distress in aggregate (i.e., historically Black and Brown communities) may represent cultures that possess adaptive eco-developmental and interpersonal factors that promote health despite experiencing health risk [118,119]. Given that the Zip-code level concentration of PoC was associated with decreased COVID-19 mortality rates, yet Black and Brown individuals demonstrated elevated rates COVID-19 mortality, it is likely that segregation acts synergistically with other socio-structural factors not measured in this study that may ultimately relate to race/ethnicity-based COVID-19 mortality rates [23].
4.1. Implications
Our findings have implications for future research, healthcare interventions and practice, and policy. Regarding research, while our findings provide insight into pre-existing systemic- and community-level predictors of COVID-19 outcomes, we suggest future researchers and agencies collect more recent neighborhood-level SDOH data to test for these associations. These data should include robust assessments of core constructs and allow for empirical model testing. Additionally, qualitative community-based designs will complement this quantitative work. Regarding implications for healthcare interventions, our findings suggest continued vaccine rollouts that focus on Non-Central Chicago neighborhoods may help address current COVID-19-related and broader inequities, particularly for the Southside and Westside neighborhoods. Supporting the need for such interventions, currently fewer vaccines have been sent to Southside and Westside neighborhoods because of a lack of pharmacies or physicians in areas where pharmacies have closed or don't exist, making it relatively hard for residents to adhere to medication schedules [120]. COVID-19 vaccine hesitancy, rightly rooted in the contexts of systemic racism, marginalization, and neglect, also may exist for PoC [121]. Regarding implications for healthcare practice, our findings, as well as the current and potential future resurgences of COVID-19 in Chicago, highlight the need for increased mental healthcare screening and service provision. Given the ongoing health problems of chronic/long COVID [122], the known mental health challenges experienced post COVID-19 recovery [123], the rapid national growth of the Omicron and other emergent subvariants of COVID-19 [124], we believe increased psychological screening services may be particularly timely. Finally, regarding policy implications, our findings suggest policies affecting both neighborhood and larger systemic-level factors are needed to address COVID-19 outcomes and inequities more broadly. For example, policies allocating extra funding and resources to the less affluent Chicago neighborhoods, particularly Southside and Westside neighborhoods, would likely help neighborhoods vis-à-vis infrastructure, healthcare access, public transportation, and community safety. For example, community-level psychoeducation, vaccine rollouts, COVID-19 testing, and targeted advertising related to vaccines and testing could be implemented to address neighborhood-level COVID-19 disparities. The current, relative lack of such efforts in the face of this and related study's findings reflects historical and structural inequities. Broadly, it is imperative for local-, state-, and federal-level policy to address and correct the disparities reported here and in past research.
4.2. Strengths and limitations
Our study should be interpreted in the context of its strengths and limitations. Regarding strengths, we used a creative and rigorous coding strategy to create neighborhood-level categories for analysis. Data came from Chicago – a city known for its inequities but relatively under-studied in terms of COVID-19. We also used publicly available COVID-19 data that is updated weekly, allowing us essentially real-time data for analyses. Specifically, our data represents trends across 72 weeks of time-series data, allowing for a methodologically stronger multi-level statistical approach that extends beyond the confines of simpler bivariate analyses. Use of data from the first 72 weeks of the COVID-19 pandemic allowed us to elucidate a snapshot understanding of these socio-structural associations to COVID-19 outcomes as the nation adjusted to this experience.
Regarding limitations, our pooled year-based estimates of retrospective data may be less meaningful than more recent data. Additionally, the endogeneity of mental health distress itself (e.g., mental health distress as a predictor and phenomenological outcome) was uninvestigated due to limitations of our data sources; however, such investigations may be beneficial for future investigation. Concerns exist surrounding differential neighborhood populations; however, we addressed this by including population size of each Zip-code within the multi-level analyses. Related, our sample itself (i.e., aggregated metrics for Zip-code and broader neighborhoods) did not allow us to address multi-level questions about individual or individual-by-place interactions, and thus may demonstrate ecological fallacy due to ecological regression. However, with this approach we began to address these questions through the community scope; and our findings are strengthened with time-series data. As literature suggests, likely our key variables are highly correlated. Our VIF of 5.1 indicates potential for multicollinearity concerns; however, the value is well below the VIF >10 benchmark for clear multicollinearity concerns [[125], [126], [127]]. More so, the standard errors and confidence intervals of each key predictor in the models are satisfactory – showing only a small range of uncertainty and indicating that multicollinearity is not an issue in these analyses [128]. Lastly, our data showed spatial autocorrelation for several key variables of interest and GWR showed spatially based similarities in associations. On one hand, this supports the theme of Chicago's historical and current segregation creating disenfranchised communities defined by Zip-code and larger neighborhoods. However, these approaches only allow for a cross-sectional “snapshot” understanding of our data. As such, we do advocate for additional spatial and longitudinal methods to be used to better understand these socio-structural variables regarding COVID-19. Such approaches include the use of spatial regression, Empirical Bayesian Kringing, spatial interpolation techniques, and other spatial geoprocessing tools.
5. Conclusions
In Chicago – a city with historical segregation and related long-lasting impacts on the health of individuals in marginalized neighborhoods – Westside and Southside neighborhoods generally showed higher levels of poverty and mental health distress. Reported mortality rates stabilized only for the Central neighborhood, with no differences in reported infection rates across time. There was a significant increased risk of reported COVID-19 infection in Zip-codes with more mental health distress, but reduced risk for reported COVID-19 mortality in these Zip-codes. There was a significant increased risk of reported COVID-19 infection in Zip-codes with higher concentrations of wealth; however, increased risk of reported COVID-19 mortality emerged for Zip-codes with higher concentration of poverty. When compared to Zip-codes with higher concentration of Non-Hispanic White individuals, Zip-codes with higher proportion of PoC demonstrated decreased risk for COVID-19 infection. More work is needed to test theoretically- and empirically-informed models including individual, neighborhood, and systemic-level variables. These models can best capture the complexity of health phenomenon related to COVID-19, spatial location, and mental health. We advocate for the simultaneous investigation of all social-ecological levels (i.e., individual, interpersonal, community, organizational, and policy) to better understand the potential inter-level associations of SDOH to COVID-19 outcomes.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
S.D. Ramos was supported by NIDA grant T32 DA 023356 B.N.C. Chronister was supported by NIMH grant T32 MH122376.
References
- 1.World Health Organization WHO Coronavirus (COVID-19) Dashboard|WHO Coronavirus (COVID-19) Dashboard With Vaccination Data. https://covid19.who.int/?adgroupsurvey={adgroupsurvey}&gclid=Cj0KCQjwg7KJBhDyARIsAHrAXaF-zXrGTVSEehtUUqzaa25Da-srVMf7qW7QWm2Ev_j_6mWlJ7Y0cXcaAiABEALw_wcB (accessed Aug. 30, 2021)
- 2.Zhang X.-B., et al. Risk factors for mortality of coronavirus disease-2019 (COVID-19) patients in two centers of Hubei province, China: a retrospective analysis. PLoS One. Jan. 2021;16(1) doi: 10.1371/journal.pone.0246030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grasselli G., et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. Apr. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. Jama. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 5.Yang J., et al. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis. 2020;10(10):1016. [Google Scholar]
- 6.Zhou F., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jordan R.E., Adab P., Cheng K.K. Covid-19: risk factors for severe disease and death. BMJ. Mar. 2020;368 doi: 10.1136/bmj.m1198. [DOI] [PubMed] [Google Scholar]
- 8.Laurencin C.T., McClinton A. The COVID-19 pandemic: a call to action to identify and address racial and ethnic disparities. J Racial Ethn Health Disparities. 2020;7(3):398–402. doi: 10.1007/s40615-020-00756-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sáenz R., Garcia M.A. The disproportionate impact of COVID-19 on older Latino mortality: the rapidly diminishing Latino paradox. J Gerontol Ser B. 2021;76(3):e81–e87. doi: 10.1093/geronb/gbaa158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Millett G.A., et al. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol. 2020;47:37–44. doi: 10.1016/j.annepidem.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Freese K.E., Vega A., Lawrence J.J., Documet P.I. Social vulnerability is associated with risk of COVID-19 related mortality in US counties with confirmed cases. J Health Care Poor Underserved. 2021;32(1):245–257. doi: 10.1353/hpu.2021.0022. [DOI] [PubMed] [Google Scholar]
- 12.US Department of Health and Human Services Social Determinants of Health - Healthy People 2030|health.gov. https://health.gov/healthypeople/objectives-and-data/social-determinants-health (accessed Aug. 30, 2021)
- 13.Elgar F.J., Stefaniak A., Wohl M.J. The trouble with trust: time-series analysis of social capital, income inequality, and COVID-19 deaths in 84 countries. Soc Sci Med. 2020;263 doi: 10.1016/j.socscimed.2020.113365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Raifman M.A., Raifman J.R. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59(1):137–139. doi: 10.1016/j.amepre.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bronfenbrenner U. Harvard University Press; 1979. The ecology of human development: Experiments by nature and design. [Google Scholar]
- 16.Tumin D., Menegay M., Shrider E.A., Nau M., Tumin R. Local income inequality, individual socioeconomic status, and unmet healthcare needs in Ohio, USA. Health Equity. 2018;2(1):37–44. doi: 10.1089/heq.2017.0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De P.K., Price T. Pre-existing economic conditions and COVID-19 infections and mortality in new York City. J Health Care Poor Underserved. 2021;32(4):1978–1994. doi: 10.1353/hpu.2021.0177. [DOI] [PubMed] [Google Scholar]
- 18.Hawkins D. Differential occupational risk for COVID-19 and other infection exposure according to race and ethnicity. Am J Ind Med. 2020;63(9):817–820. doi: 10.1002/ajim.23145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kondo N., van Dam R.M., Sembajwe G., Subramanian S.V., Kawachi I., Yamagata Z. Income inequality and health: the role of population size, inequality threshold, period effects and lag effects. J Epidemiol Community Health. 2012;66(6):1–6. doi: 10.1136/jech-2011-200321. [DOI] [PubMed] [Google Scholar]
- 20.Kondo N., Sembajwe G., Kawachi I., Van Dam R.M., Subramanian S.V., Yamagata Z. Income inequality, mortality, and self rated health: meta-analysis of multilevel studies. Bmj. 2009;339 doi: 10.1136/bmj.b4471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oronce C.I.A., Scannell C.A., Kawachi I., Tsugawa Y. Association between state-level income inequality and COVID-19 cases and mortality in the USA. J Gen Intern Med. 2020;35(9):2791–2793. doi: 10.1007/s11606-020-05971-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mateo-Urdiales A., et al. Socioeconomic patterns and COVID-19 outcomes before, during and after the lockdown in Italy (2020) Health Place. Sep. 2021;71 doi: 10.1016/j.healthplace.2021.102642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kathe N.J., Wani R.J. Determinants of COVID-19 case fatality rate in the United States: spatial analysis over one year of the pandemic. J Health Econ Outcomes Res. 2021;8(1):51. doi: 10.36469/jheor.2021.22978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li D., et al. Identifying US County-level characteristics associated with high COVID-19 burden. BMC Public Health. May 2021;21(1):1007. doi: 10.1186/s12889-021-11060-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pro G., Gilbert P.A., Baldwin J.A., Brown C.C., Young S., Zaller N. Multilevel modeling of county-level excessive alcohol use, rurality, and COVID-19 case fatality rates in the US. PLoS One. Jun. 2021;16(6) doi: 10.1371/journal.pone.0253466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arvidsdotter T., Marklund B., Kylén S., Taft C., Ekman I. Understanding persons with psychological distress in primary health care. Scand J Caring Sci. 2016;30(4):687–694. doi: 10.1111/scs.12289. [DOI] [PubMed] [Google Scholar]
- 27.McLachlan K.J., Gale C.R. The effects of psychological distress and its interaction with socioeconomic position on risk of developing four chronic diseases. J Psychosom Res. 2018;109:79–85. doi: 10.1016/j.jpsychores.2018.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rasul F., Stansfeld S.A., Hart C.L., Smith G.D. Psychological distress, physical illness, and risk of coronary heart disease. J Epidemiol Community Health. 2005;59(2):140–145. doi: 10.1136/jech.2004.019786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cao W., et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33(2) doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–542. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Haucke M., Liu S., Heinzel S. The persistence of the impact of COVID-19–related distress, mood inertia, and loneliness on mental health during a postlockdown period in Germany: an ecological momentary assessment study. JMIR Ment Health. 2021;8(8) doi: 10.2196/29419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Neelam K., Duddu V., Anyim N., Neelam J., Lewis S. Pandemics and pre-existing mental illness: a systematic review and meta-analysis. Brain Behav Immun - Health. Nov. 2020;10 doi: 10.1016/j.bbih.2020.100177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shinn A.K., Viron M. Perspectives on the COVID-19 pandemic and individuals with serious mental illness. J Clin Psychiatry. 2020;81(3) doi: 10.4088/JCP.20com13412. [DOI] [PubMed] [Google Scholar]
- 35.Lee S.W., et al. Association between mental illness and COVID-19 susceptibility and clinical outcomes in South Korea: a nationwide cohort study. Lancet Psychiatry. 2020;7(12):1025–1031. doi: 10.1016/S2215-0366(20)30421-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee J., Ramírez I.J. Geography of disparity: connecting COVID-19 vulnerability and social determinants of health in Colorado. Behav Med. 2022;48(2):72–84. doi: 10.1080/08964289.2021.2021382. [DOI] [PubMed] [Google Scholar]
- 37.Nemani K., et al. Association of psychiatric disorders with mortality among patients with COVID-19. JAMA Psychiat. 2021;78(4):380–386. doi: 10.1001/jamapsychiatry.2020.4442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang Q., Xu R., Volkow N.D. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. 2021;20(1):124–130. doi: 10.1002/wps.20806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Compton M.T., Shim R.S. The social determinants of mental health. Focus. 2015;13(4):419–425. [Google Scholar]
- 40.Muramatsu N. County-level income inequality and depression among older Americans. Health Serv Res. 2003;38(6p2):1863–1884. doi: 10.1111/j.1475-6773.2003.00206.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Messias E., Eaton W.W., Grooms A.N. Economic grand rounds: income inequality and depression prevalence across the United States: an ecological study. Psychiatr Serv. 2011;62(7):710–712. doi: 10.1176/ps.62.7.pss6207_0710. [DOI] [PubMed] [Google Scholar]
- 42.Kim D., Kawachi I. US state-level social capital and health-related quality of life: multilevel evidence of main, mediating, and modifying effects. Ann Epidemiol. 2007;17(4):258–269. doi: 10.1016/j.annepidem.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 43.Mishra S., Carleton R.N. Subjective relative deprivation is associated with poorer physical and mental health. Soc Sci Med. 2015;147:144–149. doi: 10.1016/j.socscimed.2015.10.030. [DOI] [PubMed] [Google Scholar]
- 44.Sommet N., Morselli D., Spini D. Income inequality affects the psychological health of only the people facing scarcity. Psychol Sci. 2018;29(12):1911–1921. doi: 10.1177/0956797618798620. [DOI] [PubMed] [Google Scholar]
- 45.Scott J.L., Lee-Johnson N.M., Danos D. Place, race, and case: examining racialized economic segregation and COVID-19 in Louisiana. J Racial Ethn Health Disparities. 2022:1–13. doi: 10.1007/s40615-022-01265-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim S.J., Bostwick W. <?covid19?> social vulnerability and racial inequality in COVID-19 deaths in Chicago. Health Educ Behav. 2020;47(4):509–513. doi: 10.1177/1090198120929677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bergstrand K., Mayer B., Brumback B., Zhang Y. Assessing the relationship between social vulnerability and community resilience to hazards. Soc Indic Res. Jun. 2015;122(2):391–409. doi: 10.1007/s11205-014-0698-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ge Y., Dou W., Zhang H. A new framework for understanding urban social vulnerability from a network perspective. Sustainability. Oct. 2017;9(10) doi: 10.3390/su9101723. [DOI] [Google Scholar]
- 49.Burton C., Rufat S., Tate E. Social vulnerability. Vulnerabil Resil Nat Hazards. 2018:53–81. [Google Scholar]
- 50.Cutter S.L. Vulnerability to environmental hazards. Prog Hum Geogr. 1996;20(4):529–539. [Google Scholar]
- 51.Pelling M. Routledge; 2012. The vulnerability of cities: Natural disasters and social resilience. [Google Scholar]
- 52.Gonzalez R., Fuentes A., Muñoz E. On social capital and health: the moderating role of income inequality in comparative perspective. Int J Sociol. 2020;50(1):68–85. [Google Scholar]
- 53.Hamouche S. COVID-19 and employees’ mental health: stressors, moderators and agenda for organizational actions. Emerald Open Res. 2020;2 [Google Scholar]
- 54.Spoer B.R., et al. Peer reviewed: health and health determinant metrics for cities: a comparison of county and City-level data. Prev Chronic Dis. 2020;17 doi: 10.5888/pcd17.200125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chicago.gov City of Chicago COVID Dashboard. https://www.chicago.gov/city/en/sites/covid-19/home/covid-dashboard.html (accessed Aug. 30, 2021)
- 56.Chicago Department of Public Health Protecting Chicago: Phase IV Re-Opening Metrics Summary. Jul. 2021. https://www.chicago.gov/content/dam/city/sites/covid/reports/CDPH-COVID-Reopening-metrics_070221.pdf Accessed: Nov. 06, 2022. [Online]. Available:
- 57.Bryan M.S., et al. Coronavirus disease 2019 (COVID-19) mortality and neighborhood characteristics in Chicago. Ann Epidemiol. 2021;56:47–54. doi: 10.1016/j.annepidem.2020.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bertocchi G., Dimico A. 2020. COVID-19, race, and redlining. [Google Scholar]
- 59.Laurence J. Wider-community segregation and the effect of neighbourhood ethnic diversity on social capital: an investigation into intra-neighbourhood trust in Great Britain and London. Sociology. 2017;51(5):1011–1033. doi: 10.1177/0038038516641867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.NYU Langone Health Chicago, IL - City Overview | City Health Dashboard. https://www.cityhealthdashboard.com/il/chicago/city-overview (accessed Aug. 30, 2021)
- 61.Hooper M.W., Nápoles A.M., Pérez-Stable E.J. COVID-19 and racial/ethnic disparities. Jama. 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Buhimschi C.S., et al. Prevalence and neighborhood geomapping of COVID-19 in an underserved Chicago pregnant population. Am J Perinatol Rep. 2020;10(04):e413–e416. doi: 10.1055/s-0040-1721416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gourevitch M.N., Athens J.K., Levine S.E., Kleiman N., Thorpe L.E. City-level measures of health, health determinants, and equity to foster population health improvement: the City health dashboard. Am J Public Health. 2019;109(4):585–592. doi: 10.2105/AJPH.2018.304903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chicago Health Atlas Places|Chicago Health Atlas. https://chicagohealthatlas.org/neighborhood (accessed Aug. 30, 2021)
- 65.Cohen S., Prachand N., Bocskay K., Sayer J., Schuh T. 2016. Healthy Chicago 2.0 community health assessment: Informing efforts to achieve health equity. Retrived from https://www.cityofchicago.org/content/dam/city/depts/cdph…. [Google Scholar]
- 66.“Psychiatry Online,” DSM Library 10.1176/appi.books.9780890425596 (accessed Dec. 19, 2021). [DOI]
- 67.Cree R.A., Okoro C.A., Zack M.M., Carbone E. Frequent mental distress among adults, by disability status, disability type, and selected characteristics—United States, 2018. Morb Mortal Wkly Rep. 2020;69(36):1238. doi: 10.15585/mmwr.mm6936a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Moriarty D.G., Zack M.M., Kobau R. The centers for disease control and prevention’s healthy days measures–Population tracking of perceived physical and mental health over time. Health Qual Life Outcomes. 2003;1(1):1–8. doi: 10.1186/1477-7525-1-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Thurston-Hicks A., Paine S., Hollifield M. Rural psychiatry: functional impairment associated with psychological distress and medical severity in rural primary care patients. Psychiatr Serv. 1998;49(7):951–955. doi: 10.1176/ps.49.7.951. [DOI] [PubMed] [Google Scholar]
- 70.Moriarty D.G., Zack M.M., Holt J.B., Chapman D.P., Safran M.A. Geographic patterns of frequent mental distress: US adults, 1993–2001 and 2003–2006. Am J Prev Med. 2009;36(6):497–505. doi: 10.1016/j.amepre.2009.01.038. [DOI] [PubMed] [Google Scholar]
- 71.Liu Y., et al. Association between perceived insufficient sleep, frequent mental distress, obesity and chronic diseases among US adults, 2009 behavioral risk factor surveillance system. BMC Public Health. 2013;13(1):1–8. doi: 10.1186/1471-2458-13-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Strine T.W., Balluz L., Chapman D.P., Moriarty D.G., Owens M., Mokdad A.H. Risk behaviors and healthcare coverage among adults by frequent mental distress status, 2001. Am J Prev Med. 2004;26(3):213–216. doi: 10.1016/j.amepre.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 73.Dominick K.L., Ahern F.M., Gold C.H., Heller D.A. Relationship of health-related quality of life to health care utilization and mortality among older adults. Aging Clin Exp Res. 2002;14(6):499–508. doi: 10.1007/BF03327351. [DOI] [PubMed] [Google Scholar]
- 74.Taylor R.M., Gibson F., Franck L.S. A concept analysis of health-related quality of life in young people with chronic illness. J Clin Nurs. 2008;17(14):1823–1833. doi: 10.1111/j.1365-2702.2008.02379.x. [DOI] [PubMed] [Google Scholar]
- 75.Chen H.-Y., Baumgardner D.J., Rice J.P. Peer reviewed: health-related quality of life among adults with multiple chronic conditions in the United States, behavioral risk factor surveillance system, 2007. Prev Chronic Dis. 2011;8(1) [PMC free article] [PubMed] [Google Scholar]
- 76.Doll H.A., Petersen S.E., Stewart-Brown S.L. Obesity and physical and emotional well-being: associations between body mass index, chronic illness, and the physical and mental components of the SF-36 questionnaire. Obes Res. 2000;8(2):160–170. doi: 10.1038/oby.2000.17. [DOI] [PubMed] [Google Scholar]
- 77.Krieger N., Waterman P.D., Spasojevic J., Li W., Maduro G., Van Wye G. Public health monitoring of privilege and deprivation with the index of concentration at the extremes. Am J Public Health. 2016;106(2):256–263. doi: 10.2105/AJPH.2015.302955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bishop-Royse J., Lange-Maia B., Murray L., Shah R.C., DeMaio F. Structural racism, socio-economic marginalization, and infant mortality. Public Health. 2021;190:55–61. doi: 10.1016/j.puhe.2020.10.027. [DOI] [PubMed] [Google Scholar]
- 79.Short S.E., Mollborn S. Social determinants and health Behaviors: conceptual frames and empirical advances. Curr Opin Psychol. Oct. 2015;5:78–84. doi: 10.1016/j.copsyc.2015.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.N. R. Council (US), I. of Medicine (US), Woolf S.H., Aron L. National Academies Press (US); 2013. Physical and Social Environmental Factors.https://www.ncbi.nlm.nih.gov/books/NBK154491/ Accessed: Dec. 02, 2022. [Online]. Available: [PubMed] [Google Scholar]
- 81.CDC . Centers for Disease Control and Prevention; Oct. 20, 2021. Unhealthy behaviors measure definitions.https://www.cdc.gov/places/measure-definitions/unhealthy-behaviors/index.html (accessed Dec. 19, 2021) [Google Scholar]
- 82.Centers for Disease Control and Prevention Alcohol Screening and Brief Intervention Before Prescribing Opioids. Jan. 02, 2020. https://www.cdc.gov/alcohol/fact-sheets/alcohol-screening.html (accessed Dec. 19, 2021)
- 83.National Institute on Alcohol Abuse and Alcoholism Understanding Binge Drinking. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/binge-drinking (accessed Dec. 19, 2021)
- 84.World Health Organization Alcohol and COVID-19: what you need to know. 2020. https://www.euro.who.int/__data/assets/pdf_file/0010/437608/Alcohol-and-COVID-19-what-you-need-to-know.pdf (accessed Dec. 19, 2021)
- 85.Director's Blog: Alcohol poses different challenges during the COVID-19 pandemic|National Institute on Alcohol Abuse and Alcoholism (NIAAA) https://www.niaaa.nih.gov/directors-blog-alcohol-poses-different-challenges-during-covid-19-pandemic
- 86.Sallis R., Young D.R., Tartof S.Y., Sallis J.F., Sall J., Li Q.…Cohen D.A. Physical inactivity is associated with a higher risk for severe COVID-19 outcomes: a study in 48 440 adult patients. British journal of sports medicine. 2021;55(19):1099–1105. doi: 10.1136/bjsports-2021-104080. [DOI] [PubMed] [Google Scholar]
- 87.CDC People with certain medical conditions. Ctr Dis Control Prev. Nov. 22, 2022 https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html [accessed Dec. 02, 2022] [Google Scholar]
- 88.Haddad C., Bou Malhab S., Sacre H., Salameh P. Smoking and COVID-19: a scoping review. Tob Use Insights. 2021;14 doi: 10.1177/1179173X21994612. p. 1179173X21994612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Usman M.S., et al. Is there a smoker’s paradox in COVID-19? BMJ Evid-Based Med. 2021;26(6):279–284. doi: 10.1136/bmjebm-2020-111492. [DOI] [PubMed] [Google Scholar]
- 90.Fernández-Niño J.A., Peña-Maldonado C., Rojas-Botero M., Rodriguez-Villamizar L.A. Effectiveness of contact tracing to reduce fatality from COVID-19: preliminary evidence from Colombia. Public Health. 2021;198:123–128. doi: 10.1016/j.puhe.2021.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kumar A., et al. Global impact of environmental temperature and BCG vaccination coverage on the transmissibility and fatality rate of COVID-19. PLoS One. 2020;15(10) doi: 10.1371/journal.pone.0240710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Strully K., Yang T.-C., Liu H. Regional variation in COVID-19 disparities: connections with immigrant and Latinx communities in U.S. counties. Ann Epidemiol. Jan. 2021;53:56–62.e2. doi: 10.1016/j.annepidem.2020.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bagshaw S.M., et al. Association between pandemic coronavirus disease 2019 public health measures and reduction in critical care utilization across ICUs in Alberta, Canada. Crit Care Med. 2022;50(3):353. doi: 10.1097/CCM.0000000000005275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Finch W.H., Hernández Finch M.E. Poverty and Covid-19: rates of incidence and deaths in the United States during the first 10 weeks of the pandemic. Front Sociol. 2020;5:47. doi: 10.3389/fsoc.2020.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hünermund P., Louw B. On the nuisance of control variables in regression analysis. ArXiv Prepr. 2020:1–22. ArXiv200510314. [Google Scholar]
- 96.Tung E.L., Johnson T.A., O’Neal Y., Steenes A.M., Caraballo G., Peek M.E. Experiences of community violence among adults with chronic conditions: qualitative findings from Chicago. J Gen Intern Med. 2018;33(11):1913–1920. doi: 10.1007/s11606-018-4607-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Sampson R.J., Winter A.S. The racial ecology of lead poisoning: toxic inequality in Chicago neighborhoods, 1995-2013. Bois Rev Soc Sci Res Race. 2016;13(2):261–283. [Google Scholar]
- 98.Yonek J., Hasnain-Wynia R. A profile of health and health resources within Chicago’s 77 communities. Northwest Univ Inst Healthc Stud. 2011;14 [Google Scholar]
- 99.American Public Health Association Reducing Income Inequality to Advance Health. https://www.apha.org/Policies-and-Advocacy/Public-Health-Policy-Statements/Policy-Database/2018/01/18/Reducing-Income-Inequality-to-Advance-Health (accessed Aug. 30, 2021)
- 100.Kondo M.C., Andreyeva E., South E.C., MacDonald J.M., Branas C.C. Neighborhood interventions to reduce violence. Annu Rev Public Health. 2018;39:253–271. doi: 10.1146/annurev-publhealth-040617-014600. [DOI] [PubMed] [Google Scholar]
- 101.Russ T.C., Stamatakis E., Hamer M., Starr J.M., Kivimäki M., Batty G.D. Association between psychological distress and mortality: individual participant pooled analysis of 10 prospective cohort studies. Bmj. 2012;345 doi: 10.1136/bmj.e4933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Greeson J.M., Hurwitz B.E., Llabre M.M., Schneiderman N., Penedo F.J., Klimas N.G. Psychological distress, killer lymphocytes and disease severity in HIV/AIDS. Brain Behav Immun. 2008;22(6):901–911. doi: 10.1016/j.bbi.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 103.Latoo J., Mistry M., Dunne F.J. Physical morbidity and mortality in people with mental illness. Br J Med Pr. 2013;6(3):621–623. [Google Scholar]
- 104.Walker E.R., McGee R.E., Druss B.G. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiat. 2015;72(4):334–341. doi: 10.1001/jamapsychiatry.2014.2502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Appelmann H.M., Manigault A.W., Shorey R.C., Zoccola P.M. Childhood adversity and cortisol habituation to repeated stress in adulthood. Psychoneuroendocrinology. Mar. 2021;125 doi: 10.1016/j.psyneuen.2020.105118. [DOI] [PubMed] [Google Scholar]
- 106.Tyra A.T., et al. Adverse childhood experiences, sex, and cardiovascular habituation to repeated stress. Biol Psychol. Oct. 2021;165 doi: 10.1016/j.biopsycho.2021.108175. [DOI] [PubMed] [Google Scholar]
- 107.Bilek E., et al. Deficient amygdala habituation to threatening stimuli in borderline personality disorder relates to adverse childhood experiences. Biol Psychiatry. Dec. 2019;86(12):930–938. doi: 10.1016/j.biopsych.2019.06.008. [DOI] [PubMed] [Google Scholar]
- 108.Bennett J.M., Rohleder N., Sturmberg J.P. Biopsychosocial approach to understanding resilience: stress habituation and where to intervene. J Eval Clin Pract. 2018;24(6):1339–1346. doi: 10.1111/jep.13052. [DOI] [PubMed] [Google Scholar]
- 109.Mata J., Wenz A., Rettig T., Reifenscheid M., Möhring K., Krieger U.…Naumann E. Health behaviors and mental health during the COVID-19 pandemic: A longitudinal population-based survey in Germany. Social Science & Medicine. 2021;287:1–9. doi: 10.1016/j.socscimed.2021.114333. 114333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Horenstein A., Heimberg R.G. Anxiety disorders and healthcare utilization: a systematic review. Clin Psychol Rev. Nov. 2020;81 doi: 10.1016/j.cpr.2020.101894. [DOI] [PubMed] [Google Scholar]
- 111.Liberman J.N., et al. Impact of the COVID-19 pandemic on healthcare resource utilization in individuals with major depressive disorder. Health Serv Res Manag Epidemiol. Jan. 2022;9 doi: 10.1177/23333928221111864. p. 23333928221111864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Williams D.R., Collins C. SAGE PublicationsSage CA; Los Angeles, CA: 2001. Racial residential segregation: A fundamental cause of racial disparities in health public health reports. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Massey D.S. Segregation and stratification: a biosocial perspective. Bois Rev Soc Sci Res Race. 2004;1(1):7–25. [Google Scholar]
- 114.Sharkey P., Sampson R.J. Social Neuroscience. Harvard University Press; 2015. 13. Violence, cognition, and Neighborhood inequality in America; pp. 320–339. [Google Scholar]
- 115.Kolak M., et al. Urban foodscape trends: disparities in healthy food access in Chicago, 2007–2014. Health Place. 2018;52:231–239. doi: 10.1016/j.healthplace.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 116.West Side Health Equity Collaborative Application for Funding - Healthcare Transformation Collaboratives. https://www2.illinois.gov/hfs/Documents/West%20Side%20Health%20Equity%20Collaborative_Application.pdf [Online]. Available:
- 117.Interactive Map: Pollution Hits Chicago's West, South Sides Hardest | Better Government Association. https://www.bettergov.org/news/interactive-map-pollution-hits-chicagos-west-south-sides-hardest/
- 118.Alamilla S.G., et al. Explaining the immigrant paradox: the influence of acculturation, enculturation, and acculturative stress on problematic alcohol consumption. Behav Med. 2020;46(1):21–33. doi: 10.1080/08964289.2018.1539945. [DOI] [PubMed] [Google Scholar]
- 119.Salas-Wright C.P., Vaughn M.G., Schwartz S.J., Córdova D. An ‘immigrant paradox’ for adolescent externalizing behavior? Evidence from a national sample. Soc Psychiatry Psychiatr Epidemiol. 2016;51(1):27–37. doi: 10.1007/s00127-015-1115-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Health Care Council of Chicago Event Recap|The Challenging Future of the Chicago Safety Net White Paper Release|03.18.2021. https://www.hc3.health/post/event-recap-the-challenging-future-of-the-chicago-safety-net-white-paper-release-03-18-2021 (accessed Aug. 30, 2021)
- 121.Quinn S.C., Andrasik M.P. Addressing vaccine hesitancy in BIPOC communities—toward trustworthiness, partnership, and reciprocity. New England Journal of Medicine. 2021;385(2):97–100. doi: 10.1056/NEJMp2103104. [DOI] [PubMed] [Google Scholar]
- 122.Raveendran A.V., Jayadevan R., Sashidharan S. Long COVID: an overview. Diabetes Metab Syndr Clin Res Rev. May 2021;15(3):869–875. doi: 10.1016/j.dsx.2021.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.M. M. Hossain et al., “Epidemiology of mental health problems in COVID-19: a review,” F1000Research, vol. 9, p. 636, Jun. 2020 10.12688/f1000research.24457.1. [DOI] [PMC free article] [PubMed]
- 124.Lyngse F.P., et al. MedRxiv; 2022. Transmission of SARS-CoV-2 omicron VOC subvariants BA. 1 and BA. 2: Evidence from Danish households. [Google Scholar]
- 125.Vittinghoff E., editor. Regression methods in biostatistics: Linear, logistic, survival, and repeated measures models. Springer; New York: 2005. [Google Scholar]
- 126.Gareth J., Daniela W., Trevor H., Robert T. Spinger; 2013. An introduction to statistical learning: With applications in R. [Google Scholar]
- 127.Menard S. Sage; 2002. Applied logistic regression analysis. [Google Scholar]
- 128.Goldberger A.S., Goldberger A.S.G. Harvard University Press; 1991. A course in econometrics. [Google Scholar]