Abstract
The world population is aging and the prevalence of noncommunicable diseases such as chronic kidney disease (CKD) will increase significantly. With advances in medical treatment and public health, the human lifespan continues to outpace the health span and the last decade of life is generally spent in poor health. In 2015, the World Health Organization defined healthy aging as ‘the process of developing and maintaining the functional ability that enables wellbeing in older age.’ CKD is increasingly being recognized as a model of accelerated aging and is associated with physical performance decline, cognitive decline, falls and fractures, poor quality of life, loss of appetite, and inflammation. Frailty and dementia are the final pathways and key determinants of disability and mortality independent of underlying disease. CKD, dementia, and frailty share a triangular relationship with synergistic actions and have common risk factors wherein CKD accelerates frailty and dementia through mechanisms such as uremic toxicity, metabolic acidosis and derangements, anorexia and malnutrition, dialysis-related hemodynamic instability, and sleep disturbance. Frailty accelerates glomerular filtration decline as well as dialysis induction in CKD and more than doubles the mortality risk. Anorexia is one of the major causes of protein-energy malnutrition, which is also prevalent in the aging population and warrants screening. Healthcare systems across the world need to have a system in place for the prevention of CKD amongst high-risk older adults, focusing on screening for poor prognostic factors amongst patients with CKD such as frailty, poor appetite, and cognitive impairment and providing necessary person-centered interventions to reverse underlying factors that may contribute to poor outcomes.
Keywords: Anorexia, Chronic kidney disease, Cognitive impairments, Frailty, Healthy aging
Introduction
The world population is aging at an exponential rate and demographic transition will have a major impact on health and social care costs. The lifespan continues to outpace healthspan, resulting in older adults spending their last decade in poor health. In the aging population, the prevalence of noncommunicable diseases such as chronic kidney disease (CKD), cardiovascular disease, diabetes, hyperlipidemia, and neurodegenerative diseases with associated frailty and dementia is expected to increase significantly. By 2040, CKD is projected to be the fifth leading cause of death across the world [1]. The world report on aging and health published by the World Health Organization (WHO) in 2015 defined ‘healthy aging’ as ‘the process of developing and maintaining the functional ability that enables wellbeing in older age’ with a particular focus on intrinsic capacities such as sensory impairment, cognition, nutrition, mobility, and depression [2,3]. The trajectory of aging is determined by multiple complex processes, including genetic susceptibility as well lifestyle, chronic diseases, behavioral, environmental, and dietary factors. Frailty and dementia are the main determinants of disability and are associated with increased morbidity and mortality independent of the underlying disease.
The current disease-centric and acute reactive healthcare model is not sustainable in countries with a fast-growing aging population and for conditions like CKD where there is a high prevalence of polypharmacy, multimorbidity, and heterogeneity. The healthcare systems of many countries are moving from a reactive state to a proactive one focusing on preventive care [4]. Redesigning of healthcare care is necessary and the WHO has published guidelines advocating on proactive assessments (e.g., comprehensive geriatric assessment) of individual impairments, slowing the decline in capacity with personalized care plans and providing interventions to improve nutrition and physical exercise and referrals to specialists for those with impairments [3,5].
With aging, the kidney undergoes functional and structural changes. Microscopic changes include glomerulosclerosis, interstitial fibrosis, thickening of the glomerular basement membrane, arteriosclerosis and tubular atrophy with a consequent decline in renal mass, glomerular filtration, and autoregulatory function [6]. In addition to the reduced functional reserve, chronic diseases such as diabetes, nephrotoxic polypharmacy, and sepsis are more prevalent in this group, and—together with underlying physiological changes such as a lack of thirst—can increase susceptibility to acute kidney injury [7]. CKD is considered a model of accelerated aging and is associated with a decline in physical performance, cognitive decline, fatigue, falls and fractures, poor quality of life (QoL), loss of appetite, and inflammation [8]. The term ‘senescent nephropathy’ is used to describe the synergistic decline in renal and physical function and is thought to be caused by increased inflammation in both aging and CKD [9]. While low-grade inflammation is not uncommon in aging, inflammation in CKD can be caused by dialysis-related factors (biocompatible membranes, dialysate [e.g., endotoxins], vascular access [e.g., prosthetic arteriovenous grafts/catheters], uremic toxicity, volume overload, subclinical infections, and alterations in the gut microbiome) [10]. Early identification of frailty and cognitive impairment in older patients with CKD will guide risk stratification and, when accompanied by personalized interventions, may promote aging free from disability as well as better self-rated health.
Frailty, cognitive impairment, and chronic kidney disease
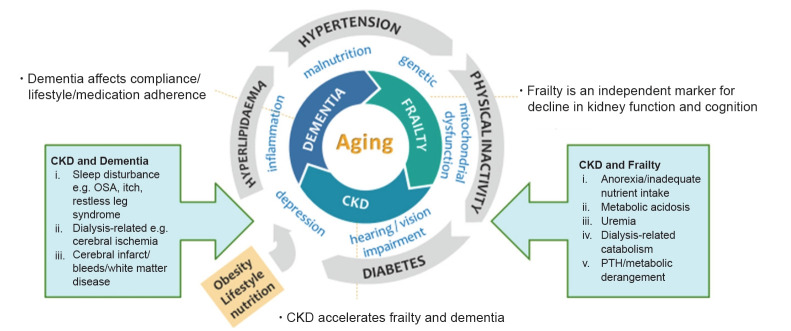
There is a triangular relationship between dementia/cognitive impairment, frailty, and CKD with aging (Fig. 1) [11,12]. The common pathophysiology and risk factors include comorbidities that often coexist in older adults, vascular risk factors such as arteriosclerosis, physical inactivity, inflammation, mitochondrial dysfunction, nutrition, depression, and impairments of the senses such as vision and hearing. Management of extrarenal complications such as frailty and cognitive impairment is a rapidly developing area in nephrology and there is lack of consensus on screening, interventions, and intended outcomes. Frailty is a dynamic, multidimensional state affecting multiple physiological systems that increases vulnerability to stressors, resulting in functional decline, falls, and increased morbidity and mortality rates [13]. The prevalence of frailty and pre-frailty in older adults worldwide varies from 43%–60% to 78% in hemodialysis (HD) patients [14]. It is an independent marker for diabetes and declines in kidney function and cognition [12,15–19]. The prevalence of frailty in pre-dialysis patients is as high as 43% and they are 2.5 times more likely to die or to begin dialysis [9,12]. Frailty may be reversible, especially before the onset of disability, with targeted interventions such as nutrition, exercise, polypharmacy, and oral health management [16,20]. However, despite its poor outcomes, frailty screening has not been incorporated into routine care by nephrologists.
Figure 1. Frailty, CKD, and dementia in the aging population.
Triangular relationship, synergistic actions, and common pathways.
CKD, chronic kidney disease; OSA, obstructive sleep apnoea; PTH, parathyroid hormone.
Albuminuria and CKD serve as complimentary risk factors for cognitive decline. Risk factors for cognitive decline can broadly be divided into three main groups: traditional risk factors applicable to older adults in general; dialysis-related factors; and nontraditional risk factors such as malnutrition, anemia, and inflammation [12,21].
There is a significant symptom burden among patients with CKD, some of which could be attributed to frailty and cognitive impairment, which is not often assessed in a clinical setting. In patients with CKD stage 4 to 5 managed without dialysis, weakness was found in 75%, poor mobility in 75%, poor appetite in 58%, pain in 56%, pruritus in 56%, and dyspnea in 49% [22].
Frailty and chronic kidney disease
A low estimated glomerular filtration rate (eGFR) is associated with a greater risk of frailty, and frail patients with CKD do much worse. In pre-dialysis patients, frailty is associated with a faster decline in eGFR, accelerated dialysis initiation, poor QoL, and increased mortality [9]. In dialysis patients, frailty is associated with increased risk of falls, readmission to the hospital, and more than double odds of mortality in 1 year [9,23]. Decreased energy and food intake with declining eGFR, in addition to other factors like metabolic acidosis, uremia, dialysis-related catabolism, hospital admissions, and metabolic derangement, contributes to sarcopenia and physical frailty (Fig. 1) [13,24]. Sarcopenia is a component of physical frailty defined as a progressive loss of skeletal muscle mass, quality and strength that is highly prevalent in CKD and has recently been shown to be associated with intradialytic hypotension in addition to other adverse outcomes such as mortality [25].
The operational definition of frailty is based on two principal concepts: the Fried Phenotype Model of Physical Frailty and the Cumulative Deficit Model of Frailty. The Fried Phenotype Model of Physical Frailty was validated in the Cardiovascular Health Study and is based on quantification, which requires measurements such as gait speed, handgrip strength, and physical activity in addition to weight loss and exhaustion [26]. The fatigue, resistance, ambulation, illnesses, and loss of weight (FRAIL) scale is based on a similar concept but relies on self-reported questionnaire responses pertaining to items such as fatigue, difficulty walking one block of 50 m, difficulty climbing a flight of stairs, weight loss and ≥5 illnesses [27,28]. The Rockwood Mitnitsky Frailty Index is a 70-item multi-domain frailty phenotype based on self-reported data initially validated in the Canadian study of health and aging that determines deficits in functional, cognitive, and social domains. The number of domains can be simplified and frailty is measured based on a ratio of the number of health deficits present over the number of health deficits measured [29]. The common physical function and frailty assessment tools are listed in Table 1 [3,9,26,27,29–36].
Table 1.
Physical function and frailty assessment tools
| Tool | Description | Estimated time (min) |
|---|---|---|
| Physical function assessment | ||
| Short physical performance battery test [31] | Measures the functional performance of the lower extremities using a set of 3 static balance tests, gait speed, and five times sit-to-stand test | ≤10 |
| Scoring: 4 points for each domain; a maximum score of 12 points | ||
| Gait speed (4, 6, or 10 m or 6 min) | Gait speed can be measured for 4, 6, or 10 m or 6 min. The 6-min gait speed test assesses endurance and aerobic capacity. Gait speed is also highly correlated with cognitive function [30,32]. Most sarcopenia guidelines use < 1 m/sec as a cutoff [33]. | ≤5 |
| Sit-to-stand (5 repetitions) | The time required to rise from the chair repeatedly 5 times. The measure of lower limb power and the ability to stand up after a fall. The cutoff for possible sarcopenia is ≥12 sec [33] and that for mobility limitation (ICOPE WHO) is >14 sec [3]. | ≤5 |
| Timed up and go [34] | Participants need to stand up from a chair unassisted, walk 3 m, turn, walk back to the chair, and sit down. | ≤5 |
| The test is used as a screening tool for falls and mobility. | ||
| Frailty assessment tool | ||
| FRAIL scale [27] | 5-Item scale assessing fatigue, resistance, ambulation, ≥5 illnesses, and loss of weight | ≤5 |
| Scoring: 1–2 points, pre-frail; 3–5 points, frail | ||
| Clinical Frailty Scale [35] | 9-Point scale ranging from very fit to severely frail to terminally ill | ≤5 |
| Fried’s Frailty Phenotype Scale [26] | 5-Item scale (requires physical measurement) assessing muscle strength, walking speed, physical activity, weight loss, and exhaustion | 5–10 |
| Scoring: 1–2 points, pre-frail; 3–5 points, frail | ||
| Rockwood Mitnitsky Frailty Index [29] | Cumulative deficits (pre-determined list) | 20–30 |
| Frailty index = number of health deficits present/number of health deficits measured | ||
| Groningen Frailty Indicator [9] | Includes 15 questions across 8 domains covering mobility, vision, hearing, nutrition, comorbidity, cognition, psychosocial, and physical fitness. The test has limited sensitivity, especially for physical fitness. | ≤10 |
| Edmonton Frail Scale [36] | Based on the following 9 components: cognition, general health, functional independence, social support, medication use, nutrition, mood, continence, and functional performance | ≤10 |
| Scoring: 0–5 points, not frail; 6–7 points, vulnerable; 8–9 points, mild frailty; 10–11 points, moderate frailty; 12–18 points, severe frailty |
FRAIL scale, the fatigue, resistance, ambulation, illnesses, and loss of weight scale. ICOPE, Integrated Care for Older People; WHO, World Health Organization.
The short physical performance battery test covers three domains: balance, gait speed, and sit-to-stand. The test has been shown to be associated with disease progression and increased mortality [9]. Gait speed alone has been shown to correlate with frailty and predict cognitive impairment, hospitalization, and mortality [30,37]. van Loon et al. [14] compared various frailty screening tools, including the Fried Frailty Phenotype, Groningen Frailty Indicator, Geriatric 8, the Identification of Seniors at Risk and the Hospital Safety Program, where the sensitivity ranged from 48% (Fried Frailty Phenotype) to 88% (Geriatric 8). Anderson et al. [38] compared the Frailty Index, Frailty Phenotype, Edmonton Frail Scale, and Clinical Frailty Scale in HD patients and found that agreement between different frailty tools was weak and the tools themselves were not interchangeable. The selection of an optimal frailty screening tool requires the balance between utility in decision-making, interventions or outcomes intended and ease of administration.
Cognitive impairment and chronic kidney disease
The presence of cognitive impairment in patients with CKD was first described by Dr. Thomas Addison in 1839 and, despite its significant association with poor treatment compliance, decision-making, readmissions, worsening kidney function, falls, and mortality, screening for cognitive impairment is not routinely conducted in the nephrology clinic [39]. More than half of HD patients with cognitive impairment are nonadherent to their medications [40]. It is estimated that every 10 mL/min/1.73 m2 decrease in eGFR is associated with an 11% increase in cognitive impairment prevalence amongst those aged >55 years. There is a rapid decline in cognition for those with eGFR of <30 mL/min/1.73 m2, where more than three quarters of those undergoing dialysis and up to 2/3 of pre-dialysis patients may have underlying cognitive impairment [32,39]. The initiation of dialysis can cause a stepwise decline in cognition, especially executive function [41]. Lacunar infarcts, white matter disease, and cerebrovascular disease are also common in CKD patients, especially those on dialysis, and intradialytic hemodynamic disturbances can precipitate cerebral ischemia with a cumulative impact on cognitive function [42]. Other factors often overlooked include sleep disturbance due to obstructive sleep apnea or restless leg syndrome, depression, anemia, and nutrient deficiencies [43]. While kidney transplantation is the gold standard for improvement in cognition in those with end-stage kidney disease, peritoneal dialysis (PD) also appears to be ‘protective’ in some studies [44].
There is still an ongoing debate about which is the best practical test to assess cognitive impairment in patients with CKD. Similar to frailty, the choice of test is dependent on its utility, time taken, threshold for intervention, and intended outcome overall. Cognitive tests (Table 2) [39,45–52] can vary from neuropsychological assessment, which takes >60 minutes in some patients and is costly to perform, to brief methods of triage, such as a single screening question or the Rapid Cognitive Screen or Mini-Cog exam [45]. Multidomain screening methods, such as the Mini-Mental State Examination and the Montreal Cognitive Assessment (which takes up to 15 minutes) are frequently used in clinical practice [39,46,47]. There are many interventions that can improve or slow down cognitive decline, requiring further validation in larger CKD populations while considering aspects such as cooled dialysis, type of dialysis, renal transplantation, anemia correction, supplements, nutrition, and exercise [39].
Table 2.
Cognition assessment tools
| Tool | Description |
|---|---|
| Triage tool | |
| Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) [47,48] | 26-Item structured informant questionnaire |
| The final score is based on the ratio of total scores (26–130 points) over the total number of completed items (1–5). It is available in multiple language translations (https://nceph.anu.edu.au/research/tools-resources/informant-questionnaire-cognitive-decline-elderly). | |
| Mini-Cog [49] | Includes 3-item recall and clock-drawing (visuospatial) |
| Rapid Cognitive Screen [45] | Includes the following three items from the Veterans Affairs SLUMS examination: i) recall of five words (testing recall), ii) a clock-drawing test (testing visuospatial function), and iii) the ability to remember a story and convert the fact (testing insight and executive function) |
| Abbreviated Mental Test Score [50] | 10-Item assessment. The test is easy to administer in the ambulatory care setting. |
| Multidomain screening tool | |
| Mini-Mental State Examination [39,51] | 30-Point assessment |
| The test evaluates attention and orientation, registration, recall, memory, calculation, language, and ability to draw a complex polygon. | |
| Montreal Cognitive Assessment [39,46] | 30-Point assessment |
| The test evaluates short-term memory, visuospatial ability, executive function, attention, concentration and working memory, language, and orientation. It is available in multiple language translations (https://www.mocatest.org/about/). | |
| Saint Louis University Mental Status (SLUMS) Examination [47,52] | 30-Point assessment |
| The test evaluates attention, immediate recall and orientation, delayed recall with interference, numeric calculation and registration, memory, digit span and visuospatial and executive function. A training video and the assessment tool are available from https://www.slu.edu/medicine/internal-medicine/geriatric-medicine/aging-successfully/assessment-tools/mental-status-exam.php. | |
| Multidomain formal assessment | |
| Neuropsychological battery | Often conducted by psychologist within an acute setting |
| The test takes > 60 min and is useful for the diagnosis of dementia and/or amnestic mild cognitive impairment. |
Anorexia of aging and chronic kidney disease
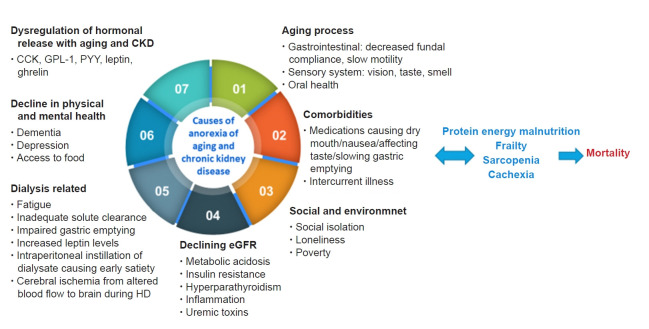
Anorexia of aging (AA) is defined as a reduced desire to eat or a loss of appetite in older adults, which is associated with weight loss, frailty, sarcopenia, hospitalization, disability, and mortality. The decrease in appetite may affect food intake and/or type of food intake, affecting overall energy intake and causing a loss of weight, which in turn is a precursor of frailty and loss of muscle mass. AA can be caused by the dysfunctional release of hormones (e.g., cholecystokinin, ghrelin, leptin), which also occurs in CKD, underlying diseases and polypharmacy, a decline in physical or mental health (including depression and dementia), a decrease in fundal compliance, poor oral health, xerostomia, and social factors such as loneliness (Fig. 2) [53,54]. In addition to the above factors, causes of anorexia in patients with CKD with/without dialysis can include a low acyl-ghrelin level, high leptin concentration, proinflammatory cytokines, metabolic acidosis, uremic toxins, changes in gut microbiomes, dialysis-related factors such as fatigue, nausea, vomiting, impaired gastric emptying and bloating, metabolic derangement, and altered taste perception [55–57]. The combination of anorexia and dietary restrictions not personalized to age, function, culture, comorbidities, or goals of treatment in the background of inflammation are major causes of protein-energy malnutrition (PEM) in CKD.
Figure 2. Causes of anorexia associated with aging or due to CKD.
CCK, cholecystokinin; CKD, chronic kidney disease; eGFR, estimated glomerular filtration rate; GLP-1, glucagon-like peptide-1; HD, hemodialysis; PYY, peptide YY.
The commonly used tools in studies and clinical practice for the evaluation of anorexia or loss of appetite are listed in Table 3 [58–64]. The Simplified Nutrition Assessment Questionnaire (SNAQ) is a simplified version of the Council on Nutrition Appetite Questionnaire that is simple to use, has been validated worldwide and was shown to be associated with depression, number of medications, poor self-rated health, and eating alone [59,60,65]. The prevalence of AA is 12% to 70% depending on the tools used and the participants studied. Among patients with CKD, the prevalence of anorexia is between 35% and 50%, and it is significantly associated with increasing age, poor QoL, and mortality [66,67].
Table 3.
Appetite assessment tools
| Tool | Description |
|---|---|
| The Council on Nutrition Appetite Questionnaire (CNAQ) [60] | Contains 8 questions related to appetite, food intake, satiety, and number of meals consumed per day derived from the AHSPQ. The total appetite score ranges from 8 (worst appetite) to 40 points (best appetite). |
| The Simplified Nutrition Assessment Questionnaire (SNAQ) [60] | Contains four questions related to appetite, food intake, satiety, and number of meals consumed per day. A total score of ≤14 points indicates a significant risk of ≥5% weight loss in the next 6 months. |
| Appetite and Diet Assessment Tool (ADAT) [61] | 44-Item self-administered questionnaire divided into three sections about appetite and eating habits in general, on dialysis, and on non-dialysis days, respectively. It takes 10 min to complete. |
| Self-assessment of appetite changes [58] | Compares present appetite vs. appetite over the last month (increased, decreased, or unchanged). |
| Subjective assessment of appetite [58] | Compares present appetite vs. appetite last week (increased, decreased, or unchanged). The test was adapted from the ADAT. |
| Visual analogue scale (VAS) [62] | Determines present appetite indicated with a line on a scale (scale extremities: 0 mm, ‘no hunger’; 100 mm, ‘hunger’). The scale is a quantitative measure of appetite. |
| Scoring: >50 mm, good appetite | |
| FAACT-ESPEN score (based on a subset of the FAACT, in particular the AC/S [63] | 12 Questions related to appetite and food intake, each of which allows for five answers (i.e., not at all, a little bit, somewhat, quite a bit, or very much). |
| The Anorexia questionnaire (AQ) [58] | Developed for the diagnosis of anorexia associated with chronic diseases, including CKD and ESRD. |
| Appetite and Food Satisfaction Questionnaire (AFSQ) [64] | Assesses the level of appetite using a facial hedonic scale and five other questions adapted from the Buckner and Dwyer tool that assesses some aspects related to food satisfaction. |
AC/S, anorexia/cachexia subscale; AHSPQ, Appetite, Hunger and Sensory Perception Questionnaire; CKD, chronic kidney disease; ESRD, end-stage renal disease; FAACT, Functional Assessment of Anorexia/Cachexia Therapy.
Person-centered care in older patients with chronic kidney disease
With growth of the aging population, the number of older patients with CKD will continue to increase. The aging CKD population with/without dialysis will have an increased prevalence of loss of appetite, sarcopenia, frailty, cognitive impairment, and PEM, which are all associated with poor outcomes including hospitalization, disability, and mortality [11]. Healthcare systems across the world need to have systems in place for the prevention of CKD amongst high-risk older adults (e.g., diabetics), screening for poor prognostic factors amongst patients with CKD (e.g., frailty, poor appetite, cognitive impairment) and provide necessary interventions to reverse underlying factors that may contribute to poor outcomes.
Screening for frailty and cognitive impairment will enable us to manage patients with CKD better with shared decision-making where treatment options such as dialysis may prolong life but cause significant physical and psychological burdens and poor QoL. In other situations, frailty could be reversed or optimized before kidney transplantation, although this may lead to patients not being put on the transplant list. With limited numbers of geriatricians worldwide, close collaboration between geriatricians and nephrologists is required to implement assessment (e.g., comprehensive geriatric assessment) and interventions. The Rapid Geriatric Assessment tool (Fig. 3), which is available in the Epic electronic health records (https://www.epic.com/about) and as an app to screen for frailty (FRAIL), sarcopenia (SARC-F), AA (SNAQ) and cognition (Rapid Cognitive Screen) with an assisted management pathway, may be useful in centers with limited geriatric resources [45,68]. While several intervention strategies have been shown to be useful, two key approaches that warrant mention include nutrition and exercise training.
Figure 3. Rapid geriatric assessment with an assisted management pathway.
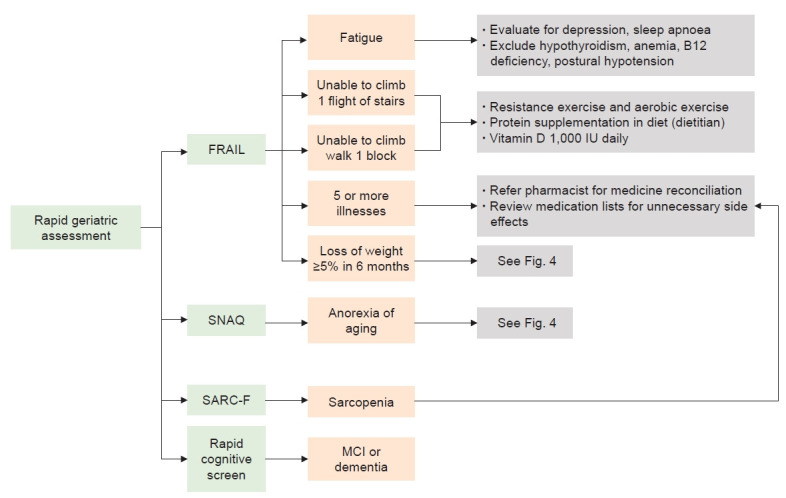
MCI, mild cognitive impairment; SARC-F, strength, ambulation, rising from a chair, climbing stairs, and falls questionnaire; SNAQ, Simplified Nutrition Assessment Questionnaire.
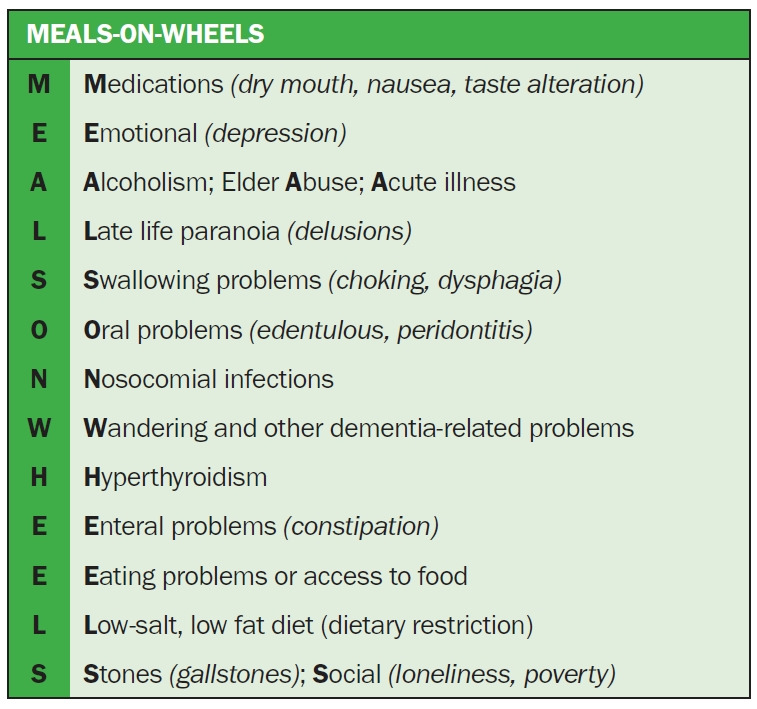
Nutrition
The National Kidney Foundation’s Kidney Disease Outcomes Quality Initiative (KDOQI) continues to revise clinical practice guidelines on the management of nutrition based on new evidence and to focus on six key areas: nutritional assessment, medical nutrition therapy, protein and energy intake, nutritional supplementation, micronutrients, and electrolytes [69]. A loss of appetite requires evaluation to exclude treatable or reversible factors based on the mnemonic ‘Meal on Wheels,’ such as medications, emotion (e.g., depression) and alcohol/substance or elder abuse, etc., as shown in Fig. 4.
Figure 4. Evaluation of loss of appetite in older adults.
For protein intake in metabolically stable CKD stage 3 to 5 patients, the KDOQI recommends a low-protein (0.55–0.60 g of dietary protein/kg body weight/day) or very-low-protein (0.28–0.43 g of dietary protein/kg body weight/day) diet with additional keto acid/amino acid analogs to meet protein intake needs. A protein intake of 0.6 to 0.8 g/kg body weight per day is recommended for CKD stage 3 to 5 patients with diabetes. For those on dialysis, regardless of diabetes, a dietary protein intake of 1.0 to 1.2 g/kg body weight per day is recommended [69]. A prescription of energy intake of 25 to 35 kcal/kg body weight per day is recommended in CKD stage 1 to 5D to maintain nutritional status [69]. Oral nutritional solutions in non-dialysis and dialysis patients with CKD have been shown to improve nutrition and inflammation [70,71]. The KDOQI recommends a minimum of a 3-month trial of oral nutritional supplements to improve dietary status in those who failed to respond to dietary counseling to meet nutritional requirements.
The role of appetite stimulants like megestrol acetate requires further evaluation in larger randomized control trials [72]. As the aging population and those with CKD are very heterogeneous, personalized assessments, which assess psychosocial aspects, environment, comorbidities with associated polypharmacy, frailty, and dementia, are necessary before providing intervention for loss of appetite, malnutrition, and/or PEM. Poor dietary compliance is often caused by contradictory and complicated dietary regimes without taking personal preference into account [73]. For those in a hypercatabolic state, malnourished and/or frail, there should be some flexibility in dietary recommendations.
Exercise
Exercise is considered a poly-pill for primary prevention and a multitude of medical diagnoses, including frailty and dementia, where no cure is available [20]. Older patients with CKD have multimorbidity’s, poor effort tolerance, fatigue, poor QoL, and poor appetite and are at increased risk of social isolation. While renal rehabilitation includes recommendations on diet and water management, pharmacotherapy, education, and psychological support, exercise is a core tenet of renal rehabilitation [74]. Insufficient physical activity increased with disease progression and increasing age in CKD patients [75]. While 34% of CKD stage 1 to 2 patients were physically active, only 11% of CKD stage 5, 6% of HD patients, and 8% of PD patients were physically active in the same study [75]. Physical inactivity is one of the causes of a high symptom burden and leads to a loss of muscle mass and strength with a consequent functional decline, disability, poor QoL, and mortality [76].
Exercise is beneficial in both CKD non-dialysis and CKD dialysis patients, being partially possibly mediated through a muscle-bone crosstalk mechanism [77]. The DOPPS (Dialysis Outcomes and Practice Pattern Study) showed that CKD patients on maintenance HD who participated in aerobic physical activity had better QoL, survival and fewer depression symptoms [78]. Moraes et al. [79] found that 6 months of resistance exercise increased physical function (as assessed by the 36-Item Short Form Survey), plasma concentrations of appetite hormones (acyl-ghrelin), body composition, and nutritional status in HD patients. Intradialytic exercise (Fig. 5) is increasingly encouraged in dialysis centers worldwide as it is associated with increased dialysis efficacy, better QoL, and improved physical function [80,81]. Specific exercises need to be prescribed and must include aerobic, strength, and flexibility exercises performed 2 to 3 days/wk. Each exercise should have ≤2 sets of 12 to 15 reps, and common modalities include cycle ergometer, weights/resistance bands, and static stretching [82].
Figure 5. Intradialytic exercise.

Photo courtesy of the National Kidney Foundation Singapore.
Systematic reviews on the benefits of exercise in pre-dialysis patients showed that it improved eGFR, blood pressure, body mass index, inflammatory markers, maximal oxygen uptake peak, and QoL [83–85]. A lower decline in glomerular filtration and improvements in muscle strength were reported in a 12-week randomized study combining resistance exercise with a low-protein diet by Castaneda et al. [86]. While there is limited evidence for dual-task exercise in CKD patients, it has been shown to improve gait speed, cognition, pain, and perceived health in at-risk community-dwelling older adults [87].
Future studies
The literature on frailty in older patients with CKD has increased significantly in the last 5 years, but significant gaps remain, which warrants further research. Despite a large number of frailty screening tools, there is still a lack of optimal screening tools in patients with CKD. Most researchers and dialysis centers worldwide are using physical performance tools, such as the sit-to-stand test or the gait speed test, which allow objective comparisons across different time points. Given the reversibility of frailty and pre-frailty in the general population, it remains unclear whether interventions to alter the trajectory of frailty, such as nutrition and exercise, will help to slow CKD progression. Future studies should focus on the role of various different types of intervention in delaying the onset of frailty in pre-dialysis or dialysis patients. There is very little literature on the impact of frequency or dosage of dialysis and reducing HD complications on frailty and cognitive impairment trajectory. Lastly, we do not know if physical activity and nutrition intervention in the peri-dialysis initiation period will have an overall impact on outcomes like mortality and functional decline after the initiation of dialysis.
Conclusion
CKD is a model for accelerated aging and is significantly associated with frailty, cognitive impairment, and loss of appetite. Early screening with necessary interventions, such as exercise and nutrition interventions, may help to modify the trajectory of CKD and improve physical function, cognition, and perceived health.
Footnotes
Conflicts of interest
All authors have no conflicts of interest to declare.
Authors’ contributions
Conceptualization: RAM, AV
Writing–original draft: RAM
Writing–review & editing: RAM, AV
All authors read and approved the final manuscript.
References
- 1.Foreman KJ, Marquez N, Dolgert A, et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet. 2018;392:2052–2090. doi: 10.1016/S0140-6736(18)31694-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Beard JR, Officer A, de Carvalho IA, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387:2145–2154. doi: 10.1016/S0140-6736(15)00516-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) Geneva: World Health Organization; c2019. Integrated Care for Older People (ICOPE) handbook: guidance on person-centred assessment and pathways in primary care [Internet] [cited 2022 May 26]. Available from: https://www.afro.who.int/publications/handbook-guidance-person-centred-assessment-and-pathways-primary-care. [Google Scholar]
- 4.Cesari M, Araujo de Carvalho I, Amuthavalli Thiyagarajan J, et al. Evidence for the domains supporting the construct of intrinsic capacity. J Gerontol A Biol Sci Med Sci. 2018;73:1653–1660. doi: 10.1093/gerona/gly011. [DOI] [PubMed] [Google Scholar]
- 5.Thiyagarajan JA, Araujo de Carvalho I, Peña-Rosas JP, et al. Redesigning care for older people to preserve physical and mental capacity: WHO guidelines on community-level interventions in integrated care. PLoS Med. 2019;16:e1002948. doi: 10.1371/journal.pmed.1002948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Sullivan ED, Hughes J, Ferenbach DA. Renal aging: causes and consequences. J Am Soc Nephrol. 2017;28:407–420. doi: 10.1681/ASN.2015121308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson S, Eldadah B, Halter JB, et al. Acute kidney injury in older adults. J Am Soc Nephrol. 2011;22:28–38. doi: 10.1681/ASN.2010090934. [DOI] [PubMed] [Google Scholar]
- 8.Wang XH, Mitch WE. Mechanisms of muscle wasting in chronic kidney disease. Nat Rev Nephrol. 2014;10:504–516. doi: 10.1038/nrneph.2014.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Worthen G, Tennankore K. Frailty screening in chronic kidney disease: current perspectives. Int J Nephrol Renovasc Dis. 2019;12:229–239. doi: 10.2147/IJNRD.S228956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mehrotra R, Kopple JD. Nutritional management of maintenance dialysis patients: why aren’t we doing better? Annu Rev Nutr. 2001;21:343–379. doi: 10.1146/annurev.nutr.21.1.343. [DOI] [PubMed] [Google Scholar]
- 11.Wong L, Duque G, McMahon LP. Sarcopenia and frailty: challenges in mainstream nephrology practice. Kidney Int Rep. 2021;6:2554–2564. doi: 10.1016/j.ekir.2021.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shen Z, Ruan Q, Yu Z, Sun Z. Chronic kidney disease-related physical frailty and cognitive impairment: a systemic review. Geriatr Gerontol Int. 2017;17:529–544. doi: 10.1111/ggi.12758. [DOI] [PubMed] [Google Scholar]
- 13.Mei F, Gao Q, Chen F, et al. Frailty as a predictor of negative health outcomes in chronic kidney disease: a systematic review and meta-analysis. J Am Med Dir Assoc. 2021;22:535–543. doi: 10.1016/j.jamda.2020.09.033. [DOI] [PubMed] [Google Scholar]
- 14.van Loon IN, Goto NA, Boereboom FT, Bots ML, Verhaar MC, Hamaker ME. Frailty screening tools for elderly patients incident to dialysis. Clin J Am Soc Nephrol. 2017;12:1480–1488. doi: 10.2215/CJN.11801116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Merchant RA, Chen MZ, Tan LW, Lim MY, Ho HK, van Dam RM. Singapore Healthy Older People Everyday (HOPE) Study: prevalence of frailty and associated factors in older adults. J Am Med Dir Assoc. 2017;18:734. doi: 10.1016/j.jamda.2017.04.020. [DOI] [PubMed] [Google Scholar]
- 16.Dent E, Morley JE, Cruz-Jentoft AJ, et al. Physical frailty: ICFSR International Clinical Practice Guidelines for identification and management. J Nutr Health Aging. 2019;23:771–787. doi: 10.1007/s12603-019-1273-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Veronese N, Stubbs B, Fontana L, et al. Frailty is associated with an increased risk of incident type 2 diabetes in the elderly. J Am Med Dir Assoc. 2016;17:902–907. doi: 10.1016/j.jamda.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 18.Strain WD, Down S, Brown P, Puttanna A, Sinclair A. Diabetes and frailty: an expert consensus statement on the management of older adults with type 2 diabetes. Diabetes Ther. 2021;12:1227–1247. doi: 10.1007/s13300-021-01035-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.O’Caoimh R, Sezgin D, O’Donovan MR, et al. Prevalence of frailty in 62 countries across the world: a systematic review and meta-analysis of population-level studies. Age Ageing. 2021;50:96–104. doi: 10.1093/ageing/afaa219. [DOI] [PubMed] [Google Scholar]
- 20.Izquierdo M, Merchant RA, Morley JE, et al. International Exercise Recommendations in Older Adults (ICFSR): expert consensus guidelines. J Nutr Health Aging. 2021;25:824–853. doi: 10.1007/s12603-021-1665-8. [DOI] [PubMed] [Google Scholar]
- 21.Olczyk P, Kusztal M, Gołębiowski T, Letachowicz K, Krajewska M. Cognitive impairment in end stage renal disease patients undergoing hemodialysis: markers and risk factors. Int J Environ Res Public Health. 2022;19:2389. doi: 10.3390/ijerph19042389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murphy EL, Murtagh FE, Carey I, Sheerin NS. Understanding symptoms in patients with advanced chronic kidney disease managed without dialysis: use of a short patient-completed assessment tool. Nephron Clin Pract. 2009;111:c74–c80. doi: 10.1159/000183177. [DOI] [PubMed] [Google Scholar]
- 23.Guo Y, Tian R, Ye P, Luo Y. Frailty in older patients undergoing hemodialysis and its association with all-cause mortality: a prospective cohort study. Clin Interv Aging. 2022;17:265–275. doi: 10.2147/CIA.S357582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chan GC, Ng JK, Chow KM, et al. Progression in physical frailty in peritoneal dialysis patients. Kidney Blood Press Res. 2021;46:342–351. doi: 10.1159/000515635. [DOI] [PubMed] [Google Scholar]
- 25.Son HE, Ryu JY, Lee K, et al. The importance of muscle mass in predicting intradialytic hypotension in patients undergoing maintenance hemodialysis. Kidney Res Clin Pract. 2022;41:611–622. doi: 10.23876/j.krcp.21.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 27.Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16:601–608. doi: 10.1007/s12603-012-0084-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nitta K, Hanafusa N, Tsuchiya K. Frailty and mortality among dialysis patients. Ren Replace Ther. 2017;3:41. [Google Scholar]
- 29.Rockwood K, Mitnitski A. Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clin Geriatr Med. 2011;27:17–26. doi: 10.1016/j.cger.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 30.Merchant RA, Goh J, Chan YH, Lim JY, Vellas B. Slow gait, subjective cognitive decline and motoric cognitive RISK syndrome: prevalence and associated factors in community dwelling older adults. J Nutr Health Aging. 2021;25:48–56. doi: 10.1007/s12603-020-1525-y. [DOI] [PubMed] [Google Scholar]
- 31.Reese PP, Cappola AR, Shults J, et al. Physical performance and frailty in chronic kidney disease. Am J Nephrol. 2013;38:307–315. doi: 10.1159/000355568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Otobe Y, Hiraki K, Hotta C, et al. Mild cognitive impairment in older adults with pre-dialysis patients with chronic kidney disease: prevalence and association with physical function. Nephrology (Carlton) 2019;24:50–55. doi: 10.1111/nep.13173. [DOI] [PubMed] [Google Scholar]
- 33.Chen LK, Woo J, Assantachai P, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21:300–307. doi: 10.1016/j.jamda.2019.12.012. [DOI] [PubMed] [Google Scholar]
- 34.Mesquita R, Janssen DJ, Wouters EF, Schols JM, Pitta F, Spruit MA. Within-day test-retest reliability of the Timed Up & Go test in patients with advanced chronic organ failure. Arch Phys Med Rehabil. 2013;94:2131–2138. doi: 10.1016/j.apmr.2013.03.024. [DOI] [PubMed] [Google Scholar]
- 35.Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rolfson DB, Majumdar SR, Tsuyuki RT, Tahir A, Rockwood K. Validity and reliability of the Edmonton Frail Scale. Age Ageing. 2006;35:526–529. doi: 10.1093/ageing/afl041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zanotto T, Mercer TH, van der Linden ML, Koufaki P. Screening tools to expedite assessment of frailty in people receiving haemodialysis: a diagnostic accuracy study. BMC Geriatr. 2021;21:411. doi: 10.1186/s12877-021-02356-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Anderson BM, Qasim M, Correa G, et al. Correlations, agreement and utility of frailty instruments in prevalent haemodialysis patients: baseline cohort data from the FITNESS study. Clin Kidney J. 2021;15:145–152. doi: 10.1093/ckj/sfab137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Crowe K, Quinn TJ, Mark PB, Findlay MD. “Is it removed during dialysis?”: cognitive dysfunction in advanced kidney failure: a review article. Front Neurol. 2021;12:787370. doi: 10.3389/fneur.2021.787370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hain DJ. Cognitive function and adherence of older adults undergoing hemodialysis. Nephrol Nurs J. 2008;35:23–29. [PubMed] [Google Scholar]
- 41.Drew DA, Weiner DE, Tighiouart H, et al. Cognitive decline and its risk factors in prevalent hemodialysis patients. Am J Kidney Dis. 2017;69:780–787. doi: 10.1053/j.ajkd.2016.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Findlay MD, Dawson J, Dickie DA, et al. Investigating the relationship between cerebral blood flow and cognitive function in hemodialysis patients. J Am Soc Nephrol. 2019;30:147–158. doi: 10.1681/ASN.2018050462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kelly DM, Rothwell PM. Disentangling the relationship between chronic kidney disease and cognitive disorders. Front Neurol. 2022;13:830064. doi: 10.3389/fneur.2022.830064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Neumann D, Mau W, Wienke A, Girndt M. Peritoneal dialysis is associated with better cognitive function than hemodialysis over a one-year course. Kidney Int. 2018;93:430–438. doi: 10.1016/j.kint.2017.07.022. [DOI] [PubMed] [Google Scholar]
- 45.Chen MZ, Chan YH, Wong MW, Merchant RA. Comparison of Rapid Cognitive Screen against Montreal Cognitive Assessment in screening for cognitive impairment in the old and old-old. Psychogeriatrics. 2022;22:460–468. doi: 10.1111/psyg.12841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dong Y, Lee WY, Basri NA, et al. The Montreal Cognitive Assessment is superior to the Mini-Mental State Examination in detecting patients at higher risk of dementia. Int Psychogeriatr. 2012;24:1749–1755. doi: 10.1017/S1041610212001068. [DOI] [PubMed] [Google Scholar]
- 47.Patnode CD, Perdue LA, Rossom RC, et al. Screening for cognitive impairment in older adults: an evidence update for the U.S. Preventive Services Task Force. Evidence synthesis No. 189. Rockville (MD): Agency for Healthcare Research and Quality; 2019. [PubMed] [Google Scholar]
- 48.Harrison JK, Stott DJ, McShane R, Noel-Storr AH, Swann-Price RS, Quinn TJ. Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE) for the early diagnosis of dementia across a variety of healthcare settings. Cochrane Database Syst Rev. 2016;11:CD011333. doi: 10.1002/14651858.CD011333.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Seitz DP, Chan CC, Newton HT, et al. Mini-Cog for the diagnosis of Alzheimer’s disease dementia and other dementias within a primary care setting. Cochrane Database Syst Rev. 2018;2:CD011415. doi: 10.1002/14651858.CD011415.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pendlebury ST, Klaus SP, Mather M, de Brito M, Wharton RM. Routine cognitive screening in older patients admitted to acute medicine: abbreviated mental test score (AMTS) and subjective memory complaint versus Montreal Cognitive Assessment and IQCODE. Age Ageing. 2015;44:1000–1005. doi: 10.1093/ageing/afv134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Arevalo-Rodriguez I, Smailagic N, Roqué I Figuls M, et al. Mini-Mental State Examination (MMSE) for the detection of Alzheimer’s disease and other dementias in people with mild cognitive impairment (MCI) Cochrane Database Syst Rev. 2015;2015:CD010783. doi: 10.1002/14651858.CD010783.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Feliciano L, Horning SM, Klebe KJ, Anderson SL, Cornwell RE, Davis HP. Utility of the SLUMS as a cognitive screening tool among a nonveteran sample of older adults. Am J Geriatr Psychiatry. 2013;21:623–630. doi: 10.1016/j.jagp.2013.01.024. [DOI] [PubMed] [Google Scholar]
- 53.Merchant RA, Woo J, Morley JE. Editorial: anorexia of ageing: pathway to frailty and sarcopenia. J Nutr Health Aging. 2022;26:3–5. doi: 10.1007/s12603-021-1703-6. [DOI] [PubMed] [Google Scholar]
- 54.Bossola M, Di Stasio E, Giungi S, et al. Xerostomia is associated with old age and poor appetite in patients on chronic hemodialysis. J Ren Nutr. 2013;23:432–437. doi: 10.1053/j.jrn.2013.05.002. [DOI] [PubMed] [Google Scholar]
- 55.Oner-Iyidogan Y, Gurdol F, Kocak H, et al. Appetite-regulating hormones in chronic kidney disease patients. J Ren Nutr. 2011;21:316–321. doi: 10.1053/j.jrn.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 56.Setyapranata S, Holt SG. The gut in older patients on peritoneal dialysis. Perit Dial Int. 2015;35:650–654. doi: 10.3747/pdi.2014.00341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Carrero JJ. Mechanisms of altered regulation of food intake in chronic kidney disease. J Ren Nutr. 2011;21:7–11. doi: 10.1053/j.jrn.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 58.Molfino A, Kaysen GA, Chertow GM, et al. Validating appetite assessment tools among patients receiving hemodialysis. J Ren Nutr. 2016;26:103–110. doi: 10.1053/j.jrn.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hanisah R, Suzana S, Lee FS. Validation of screening tools to assess appetite among geriatric patients. J Nutr Health Aging. 2012;16:660–665. doi: 10.1007/s12603-012-0056-6. [DOI] [PubMed] [Google Scholar]
- 60.Wilson MM, Thomas DR, Rubenstein LZ, et al. Appetite assessment: simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residents. Am J Clin Nutr. 2005;82:1074–1081. doi: 10.1093/ajcn/82.5.1074. [DOI] [PubMed] [Google Scholar]
- 61.Burrowes JD, Powers SN, Cockram DB, et al. Use of an appetite and diet assessment tool in the pilot phase of a hemodialysis clinical trial: mortality and morbidity in hemodialysis study. J Ren Nutr. 1996;6:229–232. [Google Scholar]
- 62.Zabel R, Ash S, King N, Bauer J. The relationship between subjective appetite sensations, markers of inflammation and appetite in dialysis patients. J Hum Nutr Diet. 2009;22:343–350. doi: 10.1111/j.1365-277X.2009.00968.x. [DOI] [PubMed] [Google Scholar]
- 63.Yang Z, Luo Y, Lu H, et al. Validation of the functional assessment of anorexia/cachexia therapy instrument to assess quality of life in maintenance hemodialysis patients with cachexia. Semin Dial. 2022;35:330–336. doi: 10.1111/sdi.13053. [DOI] [PubMed] [Google Scholar]
- 64.Melo TL, Meireles MS, Kamimura MA, Cuppari L. Concurrent validity of an appetite questionnaire in peritoneal dialysis. Perit Dial Int. 2020;40:41–46. doi: 10.1177/0896860819879878. [DOI] [PubMed] [Google Scholar]
- 65.Mikami Y, Motokawa K, Shirobe M, et al. Relationship between eating alone and poor appetite using the simplified nutritional appetite questionnaire. Nutrients. 2022;14:337. doi: 10.3390/nu14020337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Arezzo di Trifiletti A, Misino P, Giannantoni P, et al. Comparison of the performance of four different tools in diagnosing disease-associated anorexia and their relationship with nutritional, functional and clinical outcome measures in hospitalized patients. Clin Nutr. 2013;32:527–532. doi: 10.1016/j.clnu.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 67.Grove BE, Schougaard LM, Hjollund NH, Ivarsen P. Self-rated health, quality of life and appetite as predictors of initiation of dialysis and mortality in patients with chronic kidney disease stages 4-5: a prospective cohort study. BMC Res Notes. 2018;11:371. doi: 10.1186/s13104-018-3472-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Merchant RA, Hui RJ, Kwek SC, et al. Rapid geriatric assessment using mobile app in primary care: prevalence of geriatric syndromes and review of its feasibility. Front Med (Lausanne) 2020;7:261. doi: 10.3389/fmed.2020.00261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ikizler TA, Cuppari L. The 2020 updated KDOQI clinical practice guidelines for nutrition in chronic kidney disease. Blood Purif. 2021;50:667–671. doi: 10.1159/000513698. [DOI] [PubMed] [Google Scholar]
- 70.Wong MM, Zheng Y, Renouf D, Sheriff Z, Levin A. Trajectories of nutritional parameters before and after prescribed oral nutritional supplements: a longitudinal cohort study of patients with chronic kidney disease not requiring dialysis. Can J Kidney Health Dis. 2022;9:20543581211069008. doi: 10.1177/20543581211069008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Caglar K, Fedje L, Dimmitt R, Hakim RM, Shyr Y, Ikizler TA. Therapeutic effects of oral nutritional supplementation during hemodialysis. Kidney Int. 2002;62:1054–1059. doi: 10.1046/j.1523-1755.2002.00530.x. [DOI] [PubMed] [Google Scholar]
- 72.Wazny LD, Nadurak S, Orsulak C, Giles-Smith L, Tangri N. The efficacy and safety of megestrol acetate in protein-energy wasting due to chronic kidney disease: a systematic review. J Ren Nutr. 2016;26:168–176. doi: 10.1053/j.jrn.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 73.Stevenson J, Tong A, Gutman T, et al. Experiences and perspectives of dietary management among patients on hemodialysis: an interview study. J Ren Nutr. 2018;28:411–421. doi: 10.1053/j.jrn.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 74.Zhang F, Ye J, Bai Y, Wang H, Wang W. Exercise-based renal rehabilitation: a bibliometric analysis from 1969 to 2021. Front Med (Lausanne) 2022;9:842919. doi: 10.3389/fmed.2022.842919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wilkinson TJ, Clarke AL, Nixon DG, et al. Prevalence and correlates of physical activity across kidney disease stages: an observational multicentre study. Nephrol Dial Transplant. 2021;36:641–649. doi: 10.1093/ndt/gfz235. [DOI] [PubMed] [Google Scholar]
- 76.Baker LA, March DS, Wilkinson TJ, et al. Clinical practice guideline exercise and lifestyle in chronic kidney disease. BMC Nephrol. 2022;23:75. doi: 10.1186/s12882-021-02618-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Leal DV, Ferreira A, Watson EL, Wilund KR, Viana JL. Muscle-bone crosstalk in chronic kidney disease: the potential modulatory effects of exercise. Calcif Tissue Int. 2021;108:461–475. doi: 10.1007/s00223-020-00782-4. [DOI] [PubMed] [Google Scholar]
- 78.Lopes AA, Lantz B, Morgenstern H, et al. Associations of self-reported physical activity types and levels with quality of life, depression symptoms, and mortality in hemodialysis patients: the DOPPS. Clin J Am Soc Nephrol. 2014;9:1702–1712. doi: 10.2215/CJN.12371213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Moraes C, Marinho S, Lobo JC, et al. Effects of resistance exercise training on acyl-ghrelin and obestatin levels in hemodialysis patients. Ren Fail. 2015;37:851–857. doi: 10.3109/0886022X.2015.1033634. [DOI] [PubMed] [Google Scholar]
- 80.Kim S, Park HJ, Yang DH. An intradialytic aerobic exercise program ameliorates frailty and improves dialysis adequacy and quality of life among hemodialysis patients: a randomized controlled trial. Kidney Res Clin Pract. 2022;41:462–472. doi: 10.23876/j.krcp.21.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Parent-Roberge H, Deshayes TA, Fortier C, et al. Feasibility of an intradialytic combined exercise program targeting older adults with end-stage renal disease. J Aging Phys Act. 2021;29:905–914. doi: 10.1123/japa.2020-0359. [DOI] [PubMed] [Google Scholar]
- 82.Müller-Ortiz H, Moscoso-Aguayo P, Troncoso-Riquelme J, et al. Recommendations for implementation of physical training guidelines for patients undergoing chronic hemodialysis. J Hum Sport Exerc. 2021;16:S1732–S1745. [Google Scholar]
- 83.Mallamaci F, Pisano A, Tripepi G. Physical activity in chronic kidney disease and the EXerCise Introduction To Enhance trial. Nephrol Dial Transplant. 2020;35:ii18–ii22. doi: 10.1093/ndt/gfaa012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang L, Wang Y, Xiong L, Luo Y, Huang Z, Yi B. Exercise therapy improves eGFR, and reduces blood pressure and BMI in non-dialysis CKD patients: evidence from a meta-analysis. BMC Nephrol. 2019;20:398. doi: 10.1186/s12882-019-1586-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Barcellos FC, Santos IS, Umpierre D, Bohlke M, Hallal PC. Effects of exercise in the whole spectrum of chronic kidney disease: a systematic review. Clin Kidney J. 2015;8:753–765. doi: 10.1093/ckj/sfv099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Castaneda C, Gordon PL, Uhlin KL, et al. Resistance training to counteract the catabolism of a low-protein diet in patients with chronic renal insufficiency: a randomized, controlled trial. Ann Intern Med. 2001;135:965–976. doi: 10.7326/0003-4819-135-11-200112040-00008. [DOI] [PubMed] [Google Scholar]
- 87.Merchant RA, Chan YH, Hui RJ, et al. Possible sarcopenia and impact of dual-task exercise on gait speed, handgrip strength, falls, and perceived health. Front Med (Lausanne) 2021;8:660463. doi: 10.3389/fmed.2021.660463. [DOI] [PMC free article] [PubMed] [Google Scholar]