Abstract
Although race/ethnicity is associated with substantial differences in risk for depression and other diseases of aging in the United States, the processes underlying these health disparities remain poorly understood. We addressed this issue by examining how levels of a robust marker of inflammatory activity, C-reactive protein (CRP), and depression symptoms varied across racial/ethnic groups. Additionally, we tested whether the inflammation-depression association differed across groups. Data were drawn from the Chicago Community Adult Health Survey, an epidemiological survey examining biopsychosocial factors affecting health and well-being. Participants were 3105 Chicago community adults, of which 610 provided blood samples and were included in analyses. C-reactive protein was assayed from blood samples, and depression symptoms were assessed using the 11-item Center for Epidemiologic Studies-Depression scale. Race/ethnicity was self-reported and consisted of Black, Hispanic, White, and other racial/ethnic groups. Results revealed that these racial/ethnic groups differed in terms of both their CRP and depression levels. Specifically, Black Americans exhibited higher levels of CRP as compared to White and other race/ethnicity Americans. Moreover, Black Americans exhibited more depression symptoms than Hispanic Americans. Finally, we found that inflammatory levels were strongly related to depression symptoms but only for Black Americans, with CRP alone accounting for 8% of the variance in depression symptoms in this subgroup. These data thus point to a biological process that may help to explain disparities in mental health outcomes across race/ethnicity in the United States. At the same time, additional research is needed to understand the social and structural factors driving these effects.
Keywords: Race, Ethnicity, Inflammation, Major depressive disorder, C-reactive protein, Mental health
1. Introduction
Racial/ethnic disparities in health are one of the most costly and burdensome social and medical problems in the United States today (Williams, 2012). In particular, as compared to White Americans, Black Americans experience more major life events, financial, neighborhood, and workplace stressors, and multiple types of discrimination and adversity, which portend the emergence of several diseases of aging and, frequently, a shorter lifespan (Sternthal et al., 2011; Williams and Mohammed, 2009). Some research has also suggested that Black Americans are more likely than White Americans to have elevated levels of the key inflammatory marker C-reactive protein (CRP) (Farmer et al., 2020; Nazmi and Victora, 2007), which may increase their chronic disease and overall mortality risk (Bonaccio et al., 2016). Furthermore, these differences in inflammatory biology, which are thought to be partly driven by socially patterned stressors such as racism, discrimination, and inherited inequities (Furman et al., 2019; Slavich, 2022), might also lead to disparities in mental health outcomes including depression (Dowlati et al., 2010; Moriarity et al., 2019; Zalli et al., 2016).
In addition to affecting risk for elevated inflammation, race/ethnicity may moderate the association between CRP and depression. Supporting this possibility, Case and Stewart (2014) found that the relation between CRP and somatic (but not non-somatic) depression symptoms was stronger for non-Hispanic White Americans than for Black, Mexican, or Other Hispanic participants. Morris et al. (2011) found that CRP and depression were most strongly related for White women, as compared to White men and Black men and women. Beydoun et al. (2020) found that CRP was only associated with changes in total depression symptoms and “depressed affect” for White participants. Finally, Bey et al. (2018) found that CRP was associated with depression symptoms for White, but not Black, men and women. Conversely, Patel (2021), an unpublished dissertation, found that the relation between CRP and changes in cognitive/affective symptoms over 12 months was slightly stronger for Black as compared to White Americans. However, the main effect between CRP and change in cognitive/affective symptoms was not significant for either group, and because of the large number of coefficients tested in this study, type I error was likely to be high.
Given these racial/ethnic differences and the critical importance of better understanding biological processes affecting disparities in depression risk, we examined how race/ethnicity, inflammation, and depression symptoms were related in a diverse, community-based sample of adults. First, we investigated differences in levels of inflammation and depression symptoms across race/ethnicity. Second, we examined whether the strength of the association between inflammation and depression differed across race/ethnicity.
2. Method
2.1. Participants
Data were drawn from the Chicago Community Adult Health Study (2001–2003), archived at the Inter-University Consortium for Political and Social Research. This was an epidemiological survey investigating how psychosocial, neighborhood, and socio-economic factors affected the health and well-being of 3105 Chicago community adults (≥18 years old). A random subsample of 610 individuals provided blood samples. Participants provided informed consent for all study procedures, and the protocol was pre-approved by the Institutional Review Board.
These 610 participants were 59% female (n = 359) and 41% male (n = 251), with an average age of 43 years old (Mdn = 41) and average of 13 years of education (Mdn = 13); 33% were married (n = 203) and the median annual income was $30,000. This sample was 40% Black (n = 243), 13% Hispanic (n = 79), 43% White (n = 262), and 4.3% other (n = 26; Asian = 10, Native American = 13, Pacific Islander = 3).
2.2. Measures
2.2.1. Race/ethnicity
Race/ethnicity was self-reported and coded as Black, Hispanic, White, or other race/ethnicity.
2.2.2. C-reactive protein
CRP was assayed (mg/L) from blood samples taken by a certified phlebotomist. Following the blood draw, samples were frozen at −20 °C and delivered the same day to Quest Laboratories in Chicago. The samples were then stored at −70 °C until processing. Quest Laboratories conducts high-sensitivity CRP tests using a nephelometric method utilizing latex particles coated with CRP monoclonal antibodies. CRP tests are standardized against the International Federation of Clinical Chemistry and Laboratory Medicine/Bureau Communautaire de Référence/College of American Pathologists CRP reference preparation. This provides for an analytical sensitivity of 0.2 mg/L.
2.2.3. Depression symptoms
Depression symptoms over the past week were assessed using the well-validated, 11-item version of the Center for Epidemiologic Studies-Depression scale (CESD) (Kohout et al., 1993). Although originally designed to contain four subscales including depressed affect, lack of positive affect, somatic symptoms, and interpersonal challenges, the existence of a stable four-factor structure is questionable. In fact, 20 different factor structures have been identified for the CESD (Carleton et al., 2013). We examined the CESD total score to avoid unfounded dimensional specificity, over-interpretation, and to focus on the core broad construct of depression symptoms. An example item is “I felt depressed.” Responses were obtained on a 1 (never) to 4 (most of the time) scale. Internal consistency was α = 0.84.
2.3. Analyses
Data were examined using descriptive statistics (i.e., means, proportions, standard deviations), univariate analyses of variance, chi-square, and bivariate correlations. Ordinary least squares regression was used to examine Race/ethnicity × CRP interactions. Interaction plots display simple slopes for the association of CRP and depression symptoms by race/ethnicity. Our primary models used dummy-coded variables to compare White Americans (chosen as the reference group because it is the majority group) to Black, Hispanic, and other race/ethnicity Americans. Additional analyses compared Black Americans to Hispanic and other race/ethnicity Americans and Hispanic to other race/ethnicity Americans to investigate all possible differences between racial/ethnic groups.
Study staff cleaned, checked, and imputed data for the 610 participants with both survey and biological data. There were no missing data across any variables except income. Income data were 17.2% missing and were imputed using IVEware, which uses the sequential regression imputation method (Raghunathan et al., 2001). As compared to respondents with complete data, those with initial missing data were older (F = 6.77, p < .001, η2 = 0.03), and a greater proportion were female (χ2 = 9.14, p = .002, Cramer's V = 0.12) and married (χ2 = 5.93, p = .015, Cramer's V = 0.10). There were no differences on any other demographic variables.
Data were assessed for assumptions of parametric statistical testing and no notable violations were identified. Model residuals more closely approximated a normal distribution when CRP was log-transformed; therefore, log(CRP) was used in analyses. Descriptive statistics, univariate analyses of variance, and bivariate analyses were unweighted, and regression models were weighted so that the weighted sample matched the 2000 census population estimates for sex, age, and race/ethnicity for the city of Chicago. Statistical tests were conducted using SPSS 28. Graphics were produced with ggplot2. Statistical significance was determined at p < .05.
3. Results
3.1. Preliminary analyses
Descriptive statistics (means, proportions, and standard deviations) for all study variables by race/ethnicity are provided in Table 1. Levels of both CRP (F = 11.01, p < .001, η2 = 0.05) and depression symptoms (F = 4.21, p = .006, η2 = 0.02) differed across race/ethnicity. Pairwise comparisons revealed that Black Americans (M = 0.48, SD = 0.56) had higher CRP levels than White (M = 0.22, SD = 0.54, p < .001) and other race/ethnicity Americans (M = 0.12, SD = 0.47, p = .008), with no other groups differing from one another. Additionally, pairwise comparisons revealed that Black Americans (M = 2.00, SD = 0.54) had more depression symptoms than White Americans (M = 1.83, SD = 0.56, p = .004), with no other groups differing from one another.
Table 1.
Race/ethnicity differences for all study variables.
| Black |
Hispanic |
Other |
White |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | F or χ2 | η2 or V | p | |
| 1. Depression Symptoms | 2.00 | .54 | 1.85 | .62 | 1.92 | .71 | 1.83 | .56 | 4.21 | .02 | .006 |
| 2. C-Reactive Protein | .48 | .56 | .37 | .49 | .12 | .47 | .22 | .54 | 11.01 | .05 | .001 |
| 3. Female Proportion | .68 | .53 | .46 | .54 | 13.02 | .15 | .005 | ||||
| 4. Age | 44.48 | 15.58 | 36.49 | 13.62 | 36.5 | 13.50 | 44.30 | 16.57 | 7.33 | .04 | .001 |
| 5. Years of Education | 12.43 | 2.73 | 10.70 | 4.14 | 12.23 | 3.92 | 13.77 | 3.66 | 18.35 | .08 | .001 |
| 6. Married Proportion | .75 | .57 | .50 | .64 | 14.06 | .15 | .003 | ||||
| 7. Annual Income | 30798.83 | 27449.66 | 30974.11 | 22430.43 | 33904.15 | 30632.83 | 56317.21 | 60168.07 | 16.21 | .07 | .001 |
Differences across race/ethnicity were also observed on age (F = 7.33, p < .001, η2 = 0.04), years of education (F = 18.35, p < .001, η2 = 0.08), annual income (F = 16.21, p < .001, η2 = 0.07), proportion of females (χ2 = 13.02, p = .005, Cramer's V = 0.15), and proportion of married individuals (χ2 = 14.06, p = .003, Cramer's V = 0.15). White Americans were older than Hispanic (p < .001) and other race/ethnicity (p = .02) Americans, and Black Americans were older than Hispanic (p < .001) and other race/ethnicity Americans (p = .01) Americans. White Americans were more well-educated than Black (p < .001), Hispanic (p < .001), and other race/ethnicity (p = .03) Americans. Black Americans were more well-educated than Hispanic Americans (p < .001). Other race/ethnicity Americans were more well-educated than Hispanic Americans (p < .05). White Americans had a higher annual income that Black (p < .001), Hispanic (p < .001), and other race/ethnicity (p = .01) Americans. Black Americans had a greater proportion of females as compared to White (p = .004), Hispanic (p = .02), or other race/ethnicity (p = .04) Americans. Finally, Black Americans had a greater proportion of married individuals as compared to White (p = .01), Hispanic (p = .004), and other race/ethnicity (p = .01) Americans.
Descriptive statistics and bivariate correlations for the study variables are presented in Table 2. CRP was positively associated with depression symptoms (r = .12, p = .004). Being female, as compared to male (r = 0.19, p < .001), and being older (r = 0.19, p < .001) were also positively associated with CRP levels. In contrast, being more well-educated (r = −.18, p < .001) and having a higher annual income (r = −0.15, p < .001) were associated with lower CRP. Finally, being married, as compared to unmarried (r = −0.16, p < .001), and being more well-educated (r = −0.12, p = .004) and having a higher income (r = −0.22, p < .001) were related to reporting fewer depression symptoms.
Table 2.
Descriptive statistics and bivariate correlations.
| M or % | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|
| 1. Depression Symptoms | 1.91 | 0.57 | – | |||||
| 2. C-Reactive Protein | 0.34 | 0.55 | 0.12** | – | ||||
| 3. Female vs. Male (ref) | 59% | 0.49 | 0.05 | 0.19*** | – | |||
| 4. Age | 43.03 | 15.94 | −0.02 | 0.19*** | 0.05 | – | ||
| 5. Years of Education | 12.77 | 3.55 | −0.12** | −0.18*** | −0.02 | −0.19*** | – | |
| 6. Married vs. Not Married (ref) | 33% | 0.47 | −0.16*** | −0.01 | −0.04 | 0.09* | −0.06 | – |
| 7. Household Income | 41914 | 45942 | −0.22*** | −0.15*** | −0.12** | 0.03 | 0.39*** | 0.29*** |
Note. (ref) indicates the reference/comparison category for dummy variables.
*p < .05, **p < .01, ***p < .001.
3.2. Primary analyses
Regression models were structured so that depression symptoms were predicted by sex, age, marital status, and race/ethnicity in Step 1; education and income in Step 2; CRP levels in Step 3; and the Race/ethnicity × CRP interaction in Step 4. Altogether, sex (B = 0.02, β = 0.02, p = .620), age (B = 0.00, β = 0.02, p = .708), marital status (B = −0.18, β = −0.15, p < .001), and Black (B = 0.15, β = 0.12, p = .004), Hispanic (B = 0.04, β = 0.02, p = .608), and other race/ethnicity (B = 0.01, β = 0.00, p = .946) Americans, as compared to White Americans, accounted for 4% of the variance in depression symptoms in Step 1 (R2 = 0.04, p < .001). Black Americans did not differ from Hispanic (B = 0.11, β = 0.06, p = .160) or other race/ethnicity Americans (B = 0.14, β = 0.06, p < .173) on depression symptoms. Hispanic as compared to other race/ethnicity Americans exhibited no differences in depression symptoms (B = 0.03, β = 0.01, p = .785). In terms of inflammation, Black (B = 0.21, β = 0.18, p < .001) and Hispanic (B = 0.21, β = 0.13, p < .002) Americans had higher CRP levels than White Americans. Additionally, Black (B = .34, β = 0.15, p < .001) and Hispanic (B = 0.34, β = 0.14, p = .001) Americans had higher CRP levels than other race/ethnicity Americans.
Adding education (B = −.02, β = −0.11, p = .014) and income (B = −0.00, β = −0.11, p < .024) in Step 2 accounted for an additional 3% of the variance in depression symptoms (R2 = 0.03, p < .001) and reduced the Black vs. White race/ethnicity effect to nonsignificant (B = 0.09, β = 0.09, p = .080). However, several race/ethnicity coefficients for CRP level remained significant after adding education and income. In particular, Black Americans still exhibited higher CRP levels than White (B = .16, β = 0.15, p < .001) and other race/ethnicity Americans (B = 0.34, β = 0.14, p < .001). Also, Hispanic Americans still had higher CRP levels than other race/ethnicity (B = 0.30, β = 0.13, p < .005) but not White Americans (B = 0.12, β = 0.11, p < .085).
CRP was significantly related to depression symptoms in Step 3 (B = 0.09, β = 0.09, p = .033; ΔR2 = 0.01, p = .033). Moreover, after accounting for the main effects of participants' demographics, race/ethnicity, and CRP levels, a significant Race/ethnicity × CRP interaction was observed in predicting depression symptoms in Step 4 (R2 = 0.02, p = .007). The association between CRP and depression symptoms was significantly stronger for Black than White (B = −.20, β = −0.14, p = .028), Hispanic (B = −0.41, β = −0.15, p = .007), and other race/ethnicity Americans (B = −0.53, β = −0.10, p = .021). Additionally, the strength of association between CRP and depression did not differ for White as compared to Hispanic (B = −.21, β = −0.08, p = .153) and other race/ethnicity Americans (B = −0.33, β = −0.06, p = .149), or for Hispanic as compared to other race/ethnicity Americans (B = −0.11, β = −0.02, p = .656). In the final model that included all variables, the total variance in depression symptoms accounted for was 10% (R2 = 0.10, p < .001).
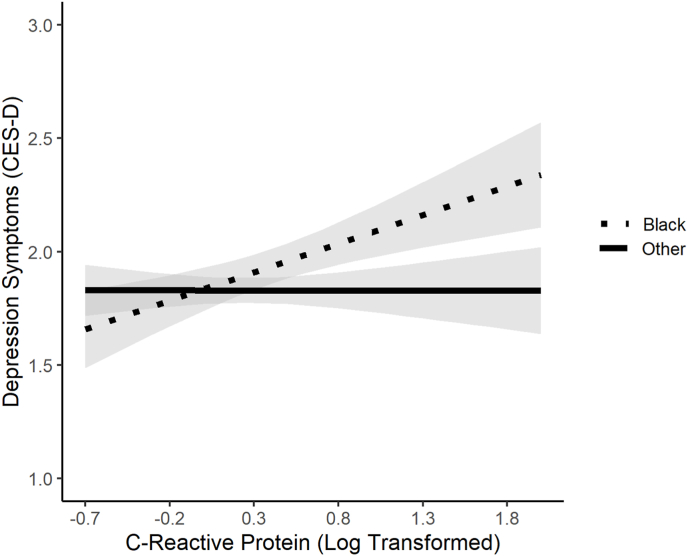
Because the association between CRP and depression symptoms was stronger for Black than White, Hispanic, or other race/ethnicity Americans, and given that the association between CRP and depression symptoms did not differ for White, Hispanic, or other race/ethnicity Americans, follow-up analyses focused on racial/ethnic differences between Black vs. all other race/ethnic groups combined (i.e., Hispanic, White, Other). Decomposing this Race/ethnicity × CRP interaction revealed that CRP was strongly, positively related to depression symptoms for Black participants (B = .30, β = 0.30, p < .001); in contrast, CRP and depression symptoms were unrelated for non-Black participants (B = −.01, β = −0.01, p = .899). Furthermore, sex, age, education, marital status, and income accounted for 11% of the total variance in depression symptoms for Black participants, with CRP alone accounting for an additional 8% of the variance in this subgroup. In contrast, for non-Black participants, sex, age, education, marital status, and income accounted for only 8% of the variance in depression symptoms, and CRP levels alone accounted for an additional 0% (see Fig. 1).
Fig. 1.
The association between C-reactive protein and depression symptoms was moderated by race/ethnicity. CRP was strongly, positively related to depression symptoms for Black participants (B = .30, β = 0.30, p < .001, R2 = 0.08); in contrast, CRP and depression symptoms were unrelated for non-Black participants (B = −.01, β = −0.01, p = .899, R2 = 0.00).
4. Discussion
The goal of this study was to advance research on the possible biological roots of mental health disparities by examining associations between race/ethnicity, CRP, and depression symptoms. In univariate analyses, Black Americans exhibited higher CRP levels than White or other race/ethnicity Americans. Multivariate models that controlled for sex, age, and marital status before investigating the effects of race/ethnicity revealed that Black and Hispanic Americans had higher CRP levels than White or other race/ethnicity Americans, and that these differences largely persisted after controlling for education and income. In univariate analyses, Black Americans exhibited more depression symptoms than White Americans. In multivariate models that controlled for sex, age, and marital status, Black Americans no longer differed from White Americans on depression symptoms, and this remained true after controlling for education and income.
The finding that Black Americans have higher CRP levels as compared to White and other race/ethnicity groups is consistent with existing national and meta-analytic research (Farmer et al., 2020; Nazmi and Victora, 2007). Similarly, higher rates of distress for Black as compared to White Americans that disappear after other socio-demographic variables are controlled has also been frequently documented in prior research, but the pattern is not uniform (Menselson et al., 2008; Williams et al., 2010a). It is unclear if this pattern is due to differences in the specific symptoms used in measures assessing depression symptoms or psychological distress. At the same time, studies using a diagnosis of major depression have reported that Black Americans have lower rates of depression that White Americans. For example, analyses of national data showed that Black Americans had lower rates of current and lifetime major depression than White Americans, but that once depressed, Black Americans were more likely than White Americans to be chronically depressed, have more severe symptoms and impairment, and to not receive treatment (Williams et al., 2007).
There is much more we need to learn about how adverse living conditions in segregated neighborhoods combine with psychosocial resources such as religious engagement and social support, along with potential variations in the presentation of depression across race/ethnicity, may affect patterns of the distribution of depression symptoms and the diagnosis of major depression (Bailey et al., 2019; Williams et al., 2010a). Furthermore, like other studies, our assessment of depression was symptom-based, whereas many population studies use screening measures of depression diagnosis. Nevertheless, Black Americans in this study also exhibited higher depression symptom levels than Hispanic Americans after controlling for socio-demographic factors. Although it is common to compare White Americans to Black, Hispanic, and a variety of other minority Americans (Menselson et al., 2008), it is less common to make comparisons across the minority groups themselves (i.e., Black vs. Hispanic; Black vs. other race/ethnicity; Hispanic vs. other race/ethnicity) as we have done here. Nevertheless, one prior study reported that Hispanics (10.8%) have a slightly higher prevalence of depression than Blacks (8.9%), but this difference was not tested with inferential statistics (Dunlop et al., 2003).
Race/ethnicity moderated the association between CRP and depression symptoms in this sample, and this finding is consistent with prior research (Beydoun et al., 2020; Case and Stewart, 2014; Morris et al., 2011; Patel, 2021). However, most prior research suggests that the CRP-depression link is stronger for White Americans than for other race/ethnicities. To the contrary, we found clear evidence that CRP and depression were strongly related for Black Americans, with no effect evident for other racial/ethnic groups. Prior studies have examined population-based samples from Atlanta (Morris et al., 2011), Baltimore (Beydoun et al., 2020), Indiana (Patel, 2021), and the entire United States (Morris et al., 2011) using the longer version of the depression measure used here (Beydoun et al., 2020) as well as the Beck Depression Inventory-II (Morris et al., 2011) and Patient Health Questionnaire-9 (Case and Stewart, 2014; Patel, 2021). These differences in the assessment of depression may partly explain these mixed results. Moreover, it is possible that these differences in how race/ethnicity is associated with the CRP-depression link are affected by factors such as discrimination; interpersonal racism; cultural, institutional, or structural racism; exposure to stressful life events; blocked opportunities; heightened vigilance; and racialized incarceration, all of which can differ across samples and communities (Williams and Etkins, 2021). Additional research is thus needed to determine to what extent race/ethnicity is a proxy variable for these, or other, explanatory variables.
One possible explanation for the observed association between CRP and depression in Black Americans, but not Hispanics could involve the distinctiveness of the history of Black Americans in the United States, who have experienced severe economic and social adversity, including long-standing racism and discrimination (Williams, 2018). For example, although Hispanic Americans have less income and wealth and experience more discrimination than White Americans, they have lower poverty rates, higher median income, and greater wealth than Black Americans (Williams et al., 2010b). In short, Black Americans experience more racism, stress, and social and economic disadvantage than Hispanic Americans who experience more of these adversities than White Americans. Native Americans appear to be the only group that experiences similar, if not higher, levels of racial discrimination than Black Americans (American Psychological Association, 2016). If the association between CRP and depression resembles a threshold effect, then perhaps only at the highest levels of race-related stressor exposure does the effect become apparent. Alternatively, perhaps the association is curvilinear in nature, and individuals at the lowest and highest ends of the racism spectrum exhibit the CRP-depression association, whereas those in the middle of the racism continuum do not. Additional research is needed to model these effects.
An additional point in considering the results of this study involves the intersectionality of multiple social strata (e.g., race, sex, class). Future research could investigate how different combinations of race and sex, race and class, and race, sex, and class might assist in better understanding how CRP and depression are related across groups. At present, the existing literature examining race differences in associations between CRP and depression has not found a consistent moderating effect of sex (Bey et al., 2018; Beydoun et al., 2020; Case and Stewart, 2014). That is, in analyses where race and sex have been examined together, race differences appear to be more prominent, and when sex differences do appear, they have not been robust and have been explained by other confounding variables (Morris et al., 2011). This is not to say that issues of intersectionality should not be further considered. The literature on race and its effects on the CRP-depression association is quite small, and several conceptual and empirical issues remain unresolved. For instance, research has yet to seriously examine how race and class, and race and aging, interact in this context (Straka et al., 2021).
4.1. Limitations
Several study limitations should be noted. First, this was a population-based study of adults in Chicago, a large metropolitan city in the upper Midwest United States, and the generalizability of these results to other populations requires investigation, particularly because geopolitical forces affecting race/ethnicity, racism, and health differ substantially across U.S. communities. Second, these results are based on one inflammatory protein, and although CRP is a robust marker of systematic inflammation, other analytes should be investigated. Third, although these data were drawn from a large population-based study, the subsample with both survey and biological data available was smaller, leading to a limited sample of Hispanic and other race/ethnicity Americans. Smaller samples of Hispanic and other race/ethnicity groups limits power to detect differences in levels and associations of CRP and depression. Fourth, we did not examine any depression symptom clusters (e.g., negative affect, positive affect, interpersonal, and somatic) because the CESD dimensional structure is not robust and two-item subscale reliabilities were unacceptable, ranging from .57 to .65. Fifth, these data were collected from 2001 to 2003. The psychoneuroimmunological mechanisms linking inflammation and depression are unlikely to have changed since then, but changes may have occurred in other social factors. For instance, 75% of Black Americans and 60% of Hispanic Americans perceived that racism got worse after president Donald Trump was elected (Ballard, 2019). Therefore, the present data may not reflect the current socio-political landscape of America or potential subcultural differences across the U.S. Finally, the present data do not speak to the drivers of these race/ethnicity-related effects, which likely include a confluence of social, environmental, and other factors that require investigation.
5. Conclusions
In conclusion, these data support prior research suggesting that Black American adults have higher CRP levels than adults from other racial/ethnic backgrounds. Moreover, this study focuses on an important question regarding CRP levels and depression, and the extent to which this association varies by race/ethnicity. Given the paucity of research on this topic, additional studies are needed to investigate the robustness and generalizability of these findings to other geographic regions, racial/ethnic groups, and communities. Research is also needed to understand the social and structural drivers of these differences in inflammation and depression to help improve mental health outcomes for those experiencing the greatest disadvantage and burden.
Funding
D.P.M. and G.M.S. were supported by grant #OPR21101 from the California Governor's Office of Planning and Research/California Initiative to Advance Precision Medicine. Additionally, D.P.M. was supported by an American Psychological Foundation Visionary Grant. These organizations had no role in designing or planning this study; in collecting, analyzing, or interpreting the data; in writing the article; or in deciding to submit this article for publication.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Loren L. Toussaint, Email: touslo01@luther.edu.
George M. Slavich, Email: gslavich@mednet.ucla.edu.
Data availability
Data can be requested directly from the Chicago Community Adult Health Survey Data Center (see https://www.isr.umich.edu/ccahs/data.html).
References
- American Psychological Association . 2016. Stress in America: the Impact of Discrimination. Stress in America Survey.https://www.apa.org/news/press/releases/stress/2015/impact-of-discrimination.pdf [Google Scholar]
- Bailey R.K., Mokonogho J., Kumar A. Racial and ethnic differences in depression: current perspectives. Neuropsychiatric Dis. Treat. 2019;15:603–609. doi: 10.2147/NDT.S128584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ballard J. 2019. A Majority of Black Americans Say Racism in the US Has Gotten Worse under Trump.https://today.yougov.com/topics/politics/articles-reports/2019/02/19/black-history-month-trump-racism-education [Google Scholar]
- Bey G.S., Jesdale B.M., Ulbricht C.M., Mick E.O., Person S.D. Allostatic load biomarker associations with depressive symptoms vary among US black and white women and men. Healthcare. 2018;6(3):105. doi: 10.3390/healthcare6030105. https://www.mdpi.com/2227-9032/6/3/105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beydoun M.A., Obhi H.K., Weiss J., Canas J.A., Beydoun H.A., Evans M.K., Zonderman A.B. Systemic inflammation is associated with depressive symptoms differentially by sex and race: a longitudinal study of urban adults. Mol. Psychiatr. 2020;25(6):1286–1300. doi: 10.1038/s41380-019-0408-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonaccio M., Di Castelnuovo A., Pounis G., De Curtis A., Costanzo S., Persichillo M., Cerletti C., Donati M.B., de Gaetano G., Iacoviello L. A score of low-grade inflammation and risk of mortality: prospective findings from the Moli-sani study. Haematologica. 2016;101(11):1434–1441. doi: 10.3324/haematol.2016.144055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carleton R.N., Thibodeau M.A., Teale M.J.N., Welch P.G., Abrams M.P., Robinson T., Asmundson G.J.G. The Center for Epidemiologic Studies Depression Scale: a review with a theoretical and empirical examination of item content and factor structure. PLoS One. 2013;8(3) doi: 10.1371/journal.pone.0058067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case S.M., Stewart J.C. Race/ethnicity moderates the relationship between depressive symptom severity and C-reactive protein: 2005–2010 NHANES data. Brain Behav. Immun. 2014;41:101–108. doi: 10.1016/j.bbi.2014.04.004. [DOI] [PubMed] [Google Scholar]
- Dowlati Y., Herrmann N., Swardfager W., Liu H., Sham L., Reim E.K., Lanctôt K.L. A meta-analysis of cytokines in major depression. Biol. Psychiatr. 2010;67(5):446–457. doi: 10.1016/j.biopsych.2009.09.033. [DOI] [PubMed] [Google Scholar]
- Dunlop D.D., Song J., Lyons J.S., Manheim L.M., Chang R.W. Racial/ethnic differences in rates of depression among preretirement adults. Am. J. Publ. Health. 2003;93(11):1945–1952. doi: 10.2105/ajph.93.11.1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer H.R., Wray L.A., Xian Y., Xu H., Pagidipati N., Peterson E.D., Dupre M.E. Racial differences in elevated C-reactive protein among us older adults. J. Am. Geriatr. Soc. 2020;68(2):362–369. doi: 10.1111/jgs.16187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furman D., Campisi J., Verdin E., Carrera-Bastos P., Targ S., Franceschi C., Ferrucci L., Gilroy D.W., Fasano A., Miller G.W., Miller A.H., Mantovani A., Weyand C.M., Barzilai N., Goronzy J.J., Rando T.A., Effros R.B., Lucia A., Kleinstreuer N., Slavich G.M. Chronic inflammation in the etiology of disease across the life span. Nat. Med. 2019;25(12):1822–1832. doi: 10.1038/s41591-019-0675-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohout F.J., Berkman L.F., Evans D.A., Cornoni-Huntley J. Two shorter forms of the CES-D depression symptoms index. J. Aging Health. 1993;5(2):179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- Menselson T., Rehkopf D.H., Kubzansky L.D. Depression among Latinos in the United States: a meta-analytic review. J. Consult. Clin. Psychol. 2008;76(3):355–366. doi: 10.1037/0022-006X.76.3.355. [DOI] [PubMed] [Google Scholar]
- Moriarity D.P., Mac Giollabhui N., Ellman L.M., Klugman J., Coe C.L., Abramson L.Y., Alloy L.B. Inflammatory proteins predict change in depressive symptoms in male and female adolescents. Clin. Psychol. Sci. 2019;7(4):754–767. doi: 10.1177/2167702619826586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris A.A., Zhao L., Ahmed Y., Stoyanova N., De Staercke C., Hooper W.C., Gibbons G., Din-Dzietham R., Quyyumi A., Vaccarino V. Association between depression and inflammation--differences by race and sex: the META-Health study. Psychosom. Med. 2011;73(6):462–468. doi: 10.1097/PSY.0b013e318222379c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nazmi A., Victora C.G. Socioeconomic and racial/ethnic differentials of C-reactive protein levels: a systematic review of population-based studies. BMC Publ. Health. 2007;7(1):212. doi: 10.1186/1471-2458-7-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel J.S. Indiana University Purdue University Indianapolis ScholarWorks Repository; 2021. Longitudinal Relationships between Depressive Symptom Clusters and Inflammatory Biomarkers Implicated in Cardiovascular Disease in People with Depression [Doctoral Dissertation, Purdue University.https://scholarworks.iupui.edu/handle/1805/27378 [Google Scholar]
- Raghunathan T.E., Lepkowski J.M., Van Hoewyk J., Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv. Methodol. 2001;27(1):85–96. [Google Scholar]
- Slavich G.M. Social Safety Theory: understanding social stress, disease risk, resilience, and behavior during the COVID-19 pandemic and beyond. Current Opinion in Psychology. 2022;45 doi: 10.1016/j.copsyc.2022.101299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sternthal M.J., Slopen N., Williams D.R. Racial disparities in health: how much does stress really matter? Du. Bois Rev.: Social Science Research on Race. 2011;8(1):95–113. doi: 10.1017/S1742058X11000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straka K., Tran M.-L., Millwood S., Swanson J., Kuhlman K.R. Aging as a context for the role of inflammation in depressive symptoms. Front. Psychiatr. 2021;11 doi: 10.3389/fpsyt.2020.605347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R. Miles to go before we sleep: racial inequities in health. J. Health Soc. Behav. 2012;53(3):279–295. doi: 10.1177/0022146512455804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R. Stress and the mental health of populations of color: advancing our understanding of race-related stressors. J. Health Soc. Behav. 2018;59(4):466–485. doi: 10.1177/0022146518814251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Costa M., Leavell J.P. In: A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems. Scheid T.L., Brown T.N., editors. Cambridge University Press; 2010. Race and mental health: patterns and challenges; pp. 268–290. [Google Scholar]
- Williams D.R., Etkins O.S. Racism and mental health. World Psychiatr. 2021;20(2):194–195. doi: 10.1002/wps.20845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., González H.M., Neighbors H., Nesse R., Abelson J.M., Sweetman J., Jackson J.S. Prevalence and distribution of major depressive disorder in african Americans, caribbean Blacks, and non-hispanic whites: results from the national survey of American life. Arch. Gen. Psychiatr. 2007;64(3):305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- Williams D.R., Mohammed S.A. Discrimination and racial disparities in health: evidence and needed research. J. Behav. Med. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Mohammed S.A., Leavell J., Collins C. Race, socioeconomic status, and health: complexities, ongoing challenges, and research opportunities. Ann. N. Y. Acad. Sci. 2010;1186(1):69–101. doi: 10.1111/j.1749-6632.2009.05339.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalli A., Jovanova O., Hoogendijk W.J.G., Tiemeier H., Carvalho L.A. Low-grade inflammation predicts persistence of depressive symptoms. Psychopharmacology. 2016;233(9):1669–1678. doi: 10.1007/s00213-015-3919-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data can be requested directly from the Chicago Community Adult Health Survey Data Center (see https://www.isr.umich.edu/ccahs/data.html).