Abstract
Introduction and importance
The purpose of this study is to highlight a rare entity of unusual location and to report our therapeutic attitude in this regard, while detailing the diagnostic criteria and therapeutic management.
Case presentation
We describe the case of a 32 years old woman with a swelling of the big toe initially neglected by the patient, the evolution is marked by a discomfort when wearing shoes, it was a firm mass of 2 cm slightly painful without local inflammatory signs with bone lysis on radiography, The MRI showed an invasion of the flexor and extensor tendons of the hallux, our approach was a carcinological tumor exeresis and arthrodesis while preserving the toe since the pedicle was not invaded, the histological examination confirmed the diagnosis and the evolution is good without tumor recurrence.
Clinical discussion
A giant cell tumor of the tendon sheaths (GCTTC) usually presents as a firm slow growing mass, the radiological assessment shows bone erosions, an MRI for extension assessment and histological confirmation are mandatory, malignant degenerations are unusual but should always be investigated, treatment is based on the most complete surgical resection to avoid the risk of recurrence, adjuvant radiotherapy can be done in case of incomplete resection but it is a controversial subject.
Conclusion
GCTTC are benign tumors that may be locally malignant because of the invasion of noble structures, which makes their complete exeresis difficult. The diagnosis is based on clinical and radiological criteria and requires histological confirmation.
Keywords: Giant cell tumor, Synovial sheath, Toe, Case report
Highlights
-
•
The giant cell tumor of the synovial sheaths is a benign tumor of local malignancy.
-
•
The localization of this tumor in the toes is extremely rare.
-
•
Histological confirmation is necessary to eliminate differential diagnoses.
-
•
The surgical resection must be complete to avoid recurrence.
-
•
A complete resection is sometimes difficult because of noble structures invasion.
1. Introduction
The tendon sheath, bursa, and synovium are anatomical entities that can undergo neoplastic clonal transformations that are generally benign proliferations and rarely metastatic [1], and as tumors with a low likelihood of metastasis, the treatment is surgical, ideally a wide resection if possible. The location sometimes makes this indication not applicable.
Localization of a giant cell tumor in the toes is extremely rare [2]. They are most often observed in the hands (80 % of cases), where they represent the second soft tissue tumor after the arthrosynovial cyst [3]. They are typically single, but variable in size depending on the time of consultation of the patient. They are benign tumors and sometimes have local malignancy and frequent recurrence [4].
We report a case of a young woman diagnosed with a giant cell tumor of the hallux, we studied the diagnostic, therapeutic, and prognostic aspects.
This case report has been reported in line with the SCARE Criteria [5].
2. Case presentation
We present the case of a 32-year-old female without medical history. She complained of swelling of the big toe for 1 year, which increased gradually in size, becoming uncomfortable when putting on the shoes without any trauma or inoculation of a foreign body and without recent deterioration in general condition.
On examination, the patient was walking with a slight limp. The swelling was on the dorsal surface of the hallux across the interphalangeal joint, firm and slightly painful on palpation, with no local inflammatory signs or skin lesions, fixed in relation to the superficial and deep planes, with a long axis of 2 cm, encompassing the extensor tendon. Furthermore, there was no bone pain, no sensory-motor deficit, and immediate CRT.
The radiograph showed an osteolytic lesion in the mirror image of the interphalangeal joint, well limited without rupture of the cortex.
An MRI was performed, showing a tissue lesion encompassing the interphalangeal joint invading the overlying and underlying soft tissues, including the extensor and flexor of the hallux (Fig. 1).
Fig. 1.
MRI showing a tissue lesion encompassing the interphalangeal joint invading the overlying and underlying soft tissues, including the extensor and flexor of the hallux.
We then opted for a surgical synovial and bone biopsy by a medial approach performed by a senior surgeon. The intraoperative examination showed a whitish tissue and a fragile bone without invasion of the collateral pedicle. A capsular and cancellous sample were taken, and the anatomopathological result was doubtful between a pigmented villonodular synovitis and a giant cell tenosynovial tumor without histological signs of malignancy.
In view of the diagnostic doubt and because of the circumferential invasion of the hallux predicting a high chance of recurrence, a carcinological surgical excision was performed after one week. The macroscopic aspect this time showed a Chinese yellow aspect with friable bone (Fig. 2), a tumor resection taking away the bone geodes and the invaded soft parts including the flexor and extensor tendons of the hallux (Fig. 3), and an arthrodesis was subsequently performed.
Fig. 2.

Intraoperative macroscopic observation showing a Chinese yellow aspect with friable bone. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Fig. 3.
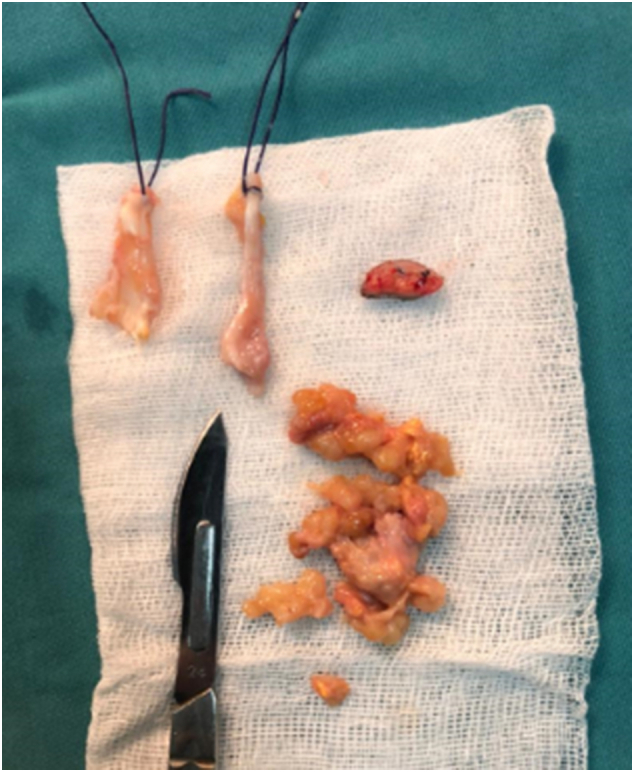
A tumor resection taking away the bone geodes and the invaded soft parts including the flexor and extensor tendons of the hallux.
Postoperatively, we recommended offloading the forefoot for 6 weeks with a Barouk shoe. At the time of the follow-up with a 2 years delay, we observed a bone consolidation without signs of local recurrence, no skin necrosis, no hypoesthesia of the pulp, and a good local condition.
3. Discussion
The giant cell tumor is a benign tumor that preferentially affects women with a sex ratio of 0.5 [6]. The age of occurrence is most often between the third and fifth decade. They present 1.6 % of all soft tissue tumors [7].
The most frequent localization of this tumor is generally the hands [4]. It's the second most common tumor of the hand following ganglion cysts [8], even when it is localized in the lower limb it often has tendency to be localized in the forefoot. The involvement of the toes is extremely rare and poorly described in the literature [9].
The lesions of the tendon sheaths can be intra or extra-articular, localized or diffuse, but the most common clinical form is a nodule in the hand, in the 3 radial fingers in 93 % of cases [1].
The clinical presentation of this tumor is very variable and non-specific due to the variety in the location and progression of the tumor [10]. In the hand, it appears as a painless, firm, slow-growing mass, sometimes associated with heat and periarticular effusion or edematous swelling [10], [11]. On the knee, it can mimic meniscal syndrome [6]. They concern mostly the small joints in the digits and especially the interphalangeal joints of the fingers near to the sheaths, usually on volar surfaces [12]. Other locations such as wrist, foot, and hip are extremely rare [10].
The diagnosis must be considered in front of the meeting of several arguments: a young patient with a typical localization like the hand, invasion of a single joint, slow evolution and after elimination of other signs of synovial pathologies (polyarthritis, gout, incipient hemophilic arthropathy…) [10].
X-ray is mandatory, bone abnormalities are present in 33 % of cases [10], multiple but nonspecific radiological abnormalities can be observed on standard radiographs such as bone erosions; degenerative lesions or soft tissue mass, cystic erosions are more frequent and suggestive in the hand and hip [13].
Once the diagnosis is suspected on the basis of the clinical data and the findings of X-rays, MRI must be performed. This is an effective and useful tool to characterize the tumor and estimate the extension to soft tissues. The tumor usually has decreased signal intensity at T1 and T2 [8]. De Beuckeleer et al. observed in his series that the majority of cases had an isointense signal of the muscles [14], this is not usual in extra-articular masses of soft tissues. This tumor was previously named extra-articular pigmentary villonodular synovitis (PVNS) as they share the same radiologic findings [1]. The PVNS is nowadays the first differential diagnosis to be considered before proceeding with our final diagnosis [15].
The histological study of the exerrated surgical specimen allows the retention of the diagnosis of giant cell tumors of the synovial sheaths. They correspond to a proliferation of synovial-like cells accompanied by multinucleated giant cells, inflammatory cells, siderophages, xanthoma cells and histiocytes associated with foamy macrophages, and deposits of hemosiderin [16], [17].
Metastases to lymphatic nodules and lung have been described, degeneration can be suspected clinically in front of a diffuse infiltration of soft parts; histology shows giant cells, nucleomegaly, macronucleoli, prominent nucleolus, a high nuclear cytoplasmic ratio, tumor necrosis and an important rate of mitotic count, malignant degenerations are unusual and rarely reported in the literature but should always be investigated. A malignant degeneration requires, like sarcomas, a large resection [1].
Its therapeutic principle is based on the most complete removal of the tumor to avoid the risk of local recurrence. A localized form requires a marginal excision, recurrence in these forms is also easily controlled by a reexcision. An arthroscopic resection is an excellent option in this case. It was also described that surgical management improves symptoms of these lesions [1]. Chun even recommends amputation of the finger in cases of extensive bony involvement and concern about possible recurrence from inadequate excision [18]. The use of postoperative radiotherapy is controversial in the literature; Gouin promotes the use of adjuvant radiotherapy in cases of incomplete resection or even for the prevention of recurrence [10]; Kotwal et al. recommended postoperative radiotherapy of 20 Gy in divided daily doses of 2 Gy in cases of incomplete excision or presence of mitotic figures on histological examination and involvement of bone; furthermore, they do not recommend prophylactic radiotherapy [19]. Other authors show that the risk of recurrence still exists, and the use of adjuvant radiotherapy does not change the long-term results [20].
Ushijima et al. [12] study the risk factors of tumor recurrence, a statistically significant recurrence risk exists if there is a degenerative lesion of the adjacent joint, location in the distal interphalangeal joint of the finger or interphalangeal joint of the thumb, radiographic presence of an osseous pressure erosion, anthropometric data and volar or dorsal location did not influence the recurrence risk.
Yasuyiki et al. recommend tumor resection by removing at least 1 mm of breast tissue around the tumor under the condition of careful preoperative planning and the use of a surgical microscope. Visual exploration of the surrounding soft tissue color with careful dissection is also necessary. Any doubtful tissue should be resected [21].
The prognosis of this tumor is poor in terms of function due to joint destruction and high local recurrence, which can range from 33 % to 50 % [1], [22].
The particularity of our case is the rarity of the tumor localization in the toes associated with local aggressiveness and circumferential invasion.
4. Conclusion
Giant cell tumors of the synovial sheaths are benign tumors with a slow evolution and local malignancy due to the invasion of noble structures. The localization of this tumor in the lower limb is rare, and the resection poses a therapeutic problem due to the difficulty of a complete exeresis, hence the high rate of recurrences.
Consent statement
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
The study is exempted from ethical approval.
Author contribution
Ahmed ZENDEOUI: original draft writing.
Mohamed GHARBI: Data analysis.
Mouadh NAFISS: Data collection.
Mohamed Hedi EZZINE: Paper editing.
Ramzi BOUZIDI: Supervision.
Anis TBORBI: Paper validation.
Guarantor
Ahmed Zendeoui/Mohamed Gharbi.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Research registration number
Not applicable.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Declaration of competing interest
The author(s) declared no potential conflicts of interest.
References
- 1.Ravi V., Wang W.-L., Lewis V.O. Treatment of tenosynovial giant cell tumor and pigmented villonodular synovitis. Curr. Opin. Oncol. 2011;23:361–366. doi: 10.1097/CCO.0b013e328347e1e3. [DOI] [PubMed] [Google Scholar]
- 2.Idrissi K.Koulali, Rafai M., Largab A., Trafeh M. Tumeur à cellules géantes des gaines des tendons extenseurs des orteils (à propos d’un cas et revue de la littérature)*. Méd. Chir. Pied. 2004;20 doi: 10.1007/s10243-004-0008-x. [DOI] [Google Scholar]
- 3.Messoudi A., Fnini S., Labsaili N., Ghrib S., Rafai M., Largab A. Les tumeurs à cellules géantes des gaines synoviales de la main: à propos de 32 cas. Chir. Main. 2007;26:165–169. doi: 10.1016/j.main.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 4.Reilly K.E., Stern P.J., Dale J.A. Recurrent giant cell tumors of the tendon sheath. J. Hand Surg. 1999;24:1298–1302. doi: 10.1053/jhsu.1999.1298. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., Thoma A., Beamish A.J., Noureldin A., Rao A., Vasudevan B., Challacombe B., Perakath B., Kirshtein B., Ekser B., Pramesh C.S., Laskin D.M., Machado-Aranda D., Miguel D., Pagano D., Millham F.H., Roy G., Kadioglu H., Nixon I.J., Mukherjee I., McCaul J.A., Chi-Yong Ngu J., Albrecht J., Rivas J.G., Raveendran K., Derbyshire L., Ather M.H., Thorat M.A., Valmasoni M., Bashashati M., Chalkoo M., Teo N.Z., Raison N., Muensterer O.J., Bradley P.J., Goel P., Pai P.S., Afifi R.Y., Rosin R.D., Coppola R., Klappenbach R., Wynn R., De Wilde R.L., Surani S., Giordano S., Massarut S., Raja S.G., Basu S., Enam S.A., Manning T.G., Cross T., Karanth V.K.L., Kasivisvanathan V., Mei Z., The S.C.A.R.E. Guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84(2020):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Monaghan H., Salter D.M., Al-Nafussi A. Giant cell tumour of tendon sheath (localised nodular tenosynovitis): clinicopathological features of 71 cases. J. Clin. Pathol. 2001;54:404–407. doi: 10.1136/jcp.54.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Occhipinti E., Heinrich S.D., Craver R. Giant cell tumor of tendon sheath arising in the toe. Fetal Pediatr. Pathol. 2004;23:171–179. doi: 10.1080/15227950490890441. [DOI] [PubMed] [Google Scholar]
- 8.Wang C., Song R.-R., Kuang P.-D., Wang L.-H., Zhang M.-M. Giant cell tumor of the tendon sheath: magnetic resonance imaging findings in 38 patients. Oncol. Lett. 2017;13:4459–4462. doi: 10.3892/ol.2017.6011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Çevik H.B., Kayahan S., Eceviz E., Gümüştaş S.A. Tenosynovial giant cell tumor in the foot and ankle. Foot Ankle Surg. 2020;26:712–716. doi: 10.1016/j.fas.2019.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Gouin F., Noailles T. Localized and diffuse forms of tenosynovial giant cell tumor (formerly giant cell tumor of the tendon sheath and pigmented villonodular synovitis) Orthop. Traumatol. Surg. Res. 2017;103:S91–S97. doi: 10.1016/j.otsr.2016.11.002. [DOI] [PubMed] [Google Scholar]
- 11.Lucas D.R. Tenosynovial giant cell tumor: case report and review. Arch. Pathol. Lab. Med. 2012;136:901–906. doi: 10.5858/arpa.2012-0165-CR. [DOI] [PubMed] [Google Scholar]
- 12.Ushijima M., Hashimoto H., Tsuneyoshi M., Enjoji M. Giant cell tumor of the tendon sheath (nodular tenosynovitis): a study of 207 cases to compare the large joint group with the common digit group. Cancer. 1986;57:875–884. doi: 10.1002/1097-0142(19860215)57:4<875::AID-CNCR2820570432>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 13.Lowyck H., De Smet L. Recurrence rate of giant cell tumors of the tendon sheath. Eur. J. Plast. Surg. 2006;28:385–388. doi: 10.1007/s00238-005-0791-6. [DOI] [Google Scholar]
- 14.Beuckeleer L.D., Schepper A.D., Belder F.D., Goethem J.V., Marques M.C.B., Broeckx J., Verstraete K., Vermaut F. Magnetic resonance imaging of localized giant cell tumour of the tendon sheath (MRI of localized GCTTS) Eur. Radiol. 1997;7:198–201. doi: 10.1007/s003300050134. [DOI] [PubMed] [Google Scholar]
- 15.Jelinek J.S., Kransdorf M.J., Shmookler B.M., Aboulafia A.A., Malawer M.M. Giant cell tumor of the tendon sheath: MR findings in nine cases. Am. J. Roentgenol. 1994;162:919–922. doi: 10.2214/ajr.162.4.8141018. [DOI] [PubMed] [Google Scholar]
- 16.D. Jeddi M.O. Lamrani A.E. Bardouni Y. Bjijou M.S. Berrada , Tumeur à Cellules Géantes des Gaines Tendineuses du gros orteil à propos d’un cas et revue de la littérature, (n.d.) 3.
- 17.Gholve P.A., Hosalkar H.S., Kreiger P.A., Dormans J.P. Giant cell tumor of tendon sheath: largest single series in children. J. Pediatr. Orthop. 2007;27:67–74. doi: 10.1097/01.bpo.0000242380.95348.8b. [DOI] [PubMed] [Google Scholar]
- 18.Lu C.-T., Chen H.-C., Coskunfirat O.K. Immediate toe transfer following index finger amputation for extensive giant cell tumor of the tendon sheath with intraosseous invasion. Chang Gung Med. J. 2004;27:312–317. [PubMed] [Google Scholar]
- 19.P K.P. Giant-cell tumour of the tendon sheath. J. Bone Joint Surg. Br. 2000;Vol. 82-B:No. 4. doi: 10.1302/0301-620X.82B4.0820571. https://online.boneandjoint.org.uk/doi/abs/10.1302/0301-620X.82B4.0820571 [DOI] [PubMed] [Google Scholar]
- 20.Garg B., Kotwal P.P. Giant cell tumour of the tendon sheath of the hand. J. Orthop. Surg. 2011;19:218–220. doi: 10.1177/230949901101900218. [DOI] [PubMed] [Google Scholar]
- 21.Kitagawa Y., Takai S. Optimal treatment for tenosynovial giant cell tumor of the hand. J. Nippon Med. Sch. Nippon Ika Daigaku Zasshi. 2020;87:184–190. doi: 10.1272/jnms.JNMS.2020_87-408. [DOI] [PubMed] [Google Scholar]
- 22.de Saint Aubain Somerhausen N., Fletcher C.D.M. Diffuse-type giant cell tumor: clinicopathologic and immunohistochemical analysis of 50 cases with extraarticular disease. Am. J. Surg. Pathol. 2000;24:479–492. doi: 10.1097/00000478-200004000-00002. [DOI] [PubMed] [Google Scholar]



