Abstract
Background
The vaccination of children and adolescents for the prevention of Covid-19 is important to:decrease in deaths and hospitalizations, prevent multisystem inflammatory syndrome, avoid long-term complications and decrease the suspension of on-site classes. Despite of these benefits, some studies have shown that some caregivers are still hesitancy.
Methods
This is a voluntary and anonymous online survey conducted from November 17 to December 14, 2021, in Brazil, through a free-of-charge platform with a link provided on social networks. A bivariate analysis was conducted with the independent variables, with vaccine hesitancy as the outcome variable, and a multivariate logistic model was used to calculated adjusted odds ratios.
Results
The sample included 15,297 respondents. Approximately 13.3 % (2,028) of the caregivers were hesitant to vaccinate their children and adolescents against Covid-19 in at least one age group. The vaccination hesitanty rate of caregivers of children aged 0–4 years, 5–11 years and adolescents were 16 %, 13 %, 15 %, respectively. The principal factors associated with vaccine hesitancy were the following: belief that they need to wait longer, belief that children that had natural infection doesn’t need to vaccinate and belief that vaccine has long term adverse effects.
Interpretation.
The present study showed that the willingness of caregivers to have their children and adolescents vaccinated in Brazil is high compared to data from adult and pediatric international studies. This study provides a profile of the hesitant caregivers considering their perspectives and beliefs regarding vaccines that can help the elaboration of strategies to increase vaccine adherence.
Keywords: Vaccine hesitancy, Survey, Brazil, Covid-19 vaccine, Children, Adolescents
1. Introduction
Since March 11, 2020, when WHO declared Covid-19 a pandemic, global efforts have been made to control the dissemination of the new Coronavirus[1]. In this setting, vaccines against Covid-19 are critical in reducing the epidemic curve. However, although vaccines have historically been responsible for the control of a large part of the epidemics that humankind has experienced so far, representing the triumph of modern Medicine, a study conducted in emergency departments in the USA, Canada, and Israel, has shown that the number of caregivers willing to vaccinate their children against Covid-19 has been decreasing even though the pandemic still inspires concern[2]. A systematic review has found that caregivers’ willingness to vaccinate children against Covid-19 is approximately 59.3 %, which rises concern, perplexity, and the need to have a more in-depth understanding of this hesitancy[3].
Vaccination of children and adolescents is especially important due to many factors, and the major ones are the decrease in deaths and hospitalizations. The estimated effectiveness of 2 doses of Pfizer-BioNTech vaccine against severe conditions such as the multisystem inflammatory syndrome in children (MIS-C) from 12 to 18 years old was 91 % in a control case study in the USA[4]. Another potential target is to avoid long-term complications, such as long Covid, in this age group [5]. Aside from protecting children, the vaccine can reduce the number of school outbreaks, and therefore, decrease the suspension of on-site classes, avoiding disruption to in-person learning[5]. Distancing measures, particularly school closures for in-person education, which have protected children so far, have already shown damaging effects on children’s mental health, learning, and psychosocial development[6].
A study conducted to evaluate the willingness of Brazilian adults to vaccinate themselves against Covid-19 has shown vaccine hesitancy of only 10.5 %[7], suggesting that Brazilians have higher adhesion to vaccination than that observed in other countries [8], [9]. Considering that the perspectives and beliefs that caregivers have regarding vaccines are important factors to predict children immunization status[10], the aim of the present study is to evaluate the willingness of Brazilian caregivers to vaccinate their children against Covid-19 and factors associated to vaccine hesitancy.
2. Methodology
This is a voluntary and anonymous online survey conducted from November 17 to December 14, 2021, in Brazil, through a free-of-charge platform (https://www.google.com/forms/about/) with a link provided on the following social networks: WhatsApp, Telegram, Facebook, Instagram, Twitter, and LinkedIn. All participants were encouraged to share the study form through their own social media. The form link was also disclosed on the official page of Instituto Nacional de Saúde da Mulher, da Criança e do Adolescente Fernandes Figueira, FIOCRUZ (National Institute of Women, Children and Adolescents Health) (https://www.iff.fiocruz.br). The form was comprised of 33 closed questions and 2 open questions, elaborated after a literature review and a discussion with the group of experts from the research team.
2.1. Inclusion and exclusion criteria
The sample was comprised of all the questionnaires answered by participants who declared they were 18+ years old, Brazilians, residing in Brazil at the time of the survey, and caregivers of children and/or adolescents below 18 years old. The sample would exclude one of the records when all items completed in two questionnaires were identical, which reflected duplicated answers, or when the forms were sent with all items in blank. Duplicated records were excluded using SPSS, which compared the level of similarity between answers in closed variable fields, with two open fields that should have a higher level of heterogeneous answers.
2.1.1. Outcome
Study outcome is vaccine hesitancy, defined according to the criteria of the SAGE Working Group on Vaccine Hesitancy, which is delayed acceptance or complete refusal of vaccination. Caregivers were asked about their willingness to vaccinate their children in a stratified manner, according to age group: 0–4 years old, 5–11 years old, and 12 + years old. The format of the answer followed a Likert scale: very likely, likely, unlikely, very unlikely, not sure. Therefore, the study defined as vaccine hesitant those caregivers who answered the question concerning their willingness to vaccinate their children as “unlikely”, “very unlikely”, or “not sure”.
2.1.2. Variables
The following variables about the respondents were considered: 1) demographic: gender (male, female, others), age group (18–39 years old, 40–59 years old, ≥ 60 years old), self-declared ethnicity (white, brown, black, yellow, indigenous), education (completed nine-year fundamental education, High School, or Higher education), monthly income, information about respondents' vaccination against Covid-19, information about whether there was change in income during the pandemic (increased, decreased, no change), information about compliance with vaccination against other diseases other than Covid-19. Variables related to children and adolescents were: whether the child or adolescent had any physical, mental, sensory deficiency or a chronic disease that needs follow-up, whether they were attending on-site education, the perception of children and adolescents concerning loneliness, whether they felt sad or depressed due to limited social contact during the pandemic, private health insurance, information about whether the child or adolescent had had Covid-19, whether hospitalization had been required to treat Covid-19 or its complications, perception of the caregivers on the potential severity of Covid-19 in children and adolescents. Additionally, a set of sentences with options for answers was provided in likert format regarding the perception of caregivers about Covid-19 and vaccination.
2.1.3. Context/Background
Until the collection of data, Brazil had had a total of 616,251 accumulated deaths since the beginning of the pandemic. The number of new cases was 10,055. Vaccination against Covid-19 in adolescents aged 12 years or older had been authorized by ANVISA and the Pfizer vaccine (Cominarty) had been provided by the Ministry of Health of Brazil on August 23, 2021. Study recruitment was completed on December 14, the authorization was extended to Comirnarty at a dosage of 10mcg against Covid-19 for children aged 5–11 years on December 16, 2021, and Coronavac was approved for children aged 6–11 years on January 20, 2022. Authorization for vaccination against Covid-19 had not been provided for children aged 0–4 years until April 2022.
2.1.4. Statistical analysis
Data were coded and analyzed using the SPSS software. All variables were analyzed according to their absolute and relative frequencies. Bivariate analysis was performed with vaccine hesitancy as the outcome. This analysis used the chi-square test, and statistical significance of differences was set at a p-value < 0.05. A multivariate logistic model was used to calculate adjusted odds ratios with the respective 95 % confidence intervals for the set of statistically significant variables in the bivariate analysis.
3. Results
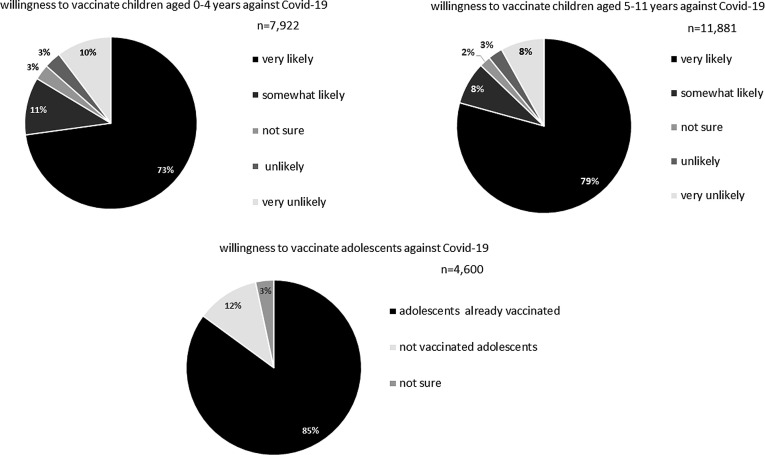
After the exclusions (268 reports), a total of 15,297 respondents were included in the analysis. Approximately 13.3 % (2,028) of the caregivers were hesitant to vaccinate their children and adolescents against Covid-19 in at least one age group. The caregivers of children aged 0–4 years had the highest vaccination hesitancy rate, 16 %; The vaccination hesitancy rate of caregivers of children aged 5–11 years and caregivers of adolescents younger than 18 years old were 13 % and 15 %, respectively (Fig. 1 ).
Fig. 1.
The graphs show the distribution of answers about willingness to vaccinate children aged 0–4 years (graph a) and children aged 5–11 years (graph b) with the following options: very likely, somewhat likely, not sure, unlikely, very unlikely. Graph c shows the distribution of answers about the intention of vaccinating adolescents (vaccines already available) with the options: vaccinated, not vaccinated, not sure.
All five macro-regions in Brazil were represented in this study although there was predominance of answers from the southeastern region (northern region, n = 368; northeastern region, n = 1,266; mid-western region, n = 1,167; southern region, n = 1,703; southeastern region, n = 10,793).
Socio-demographic variables and variables related to vaccination were stratified according to vaccine hesitancy and are available in Table 1 . Higher vaccination hesitancy rates against Covid-19 in children and adolescents were observed among caregivers who had not vaccinated against Covid-19. However, it was also observed among caregivers that had only received the first dose, which means this reflects the standpoint of caregivers, either those who did not complete or who are delaying their own vaccination. Approximately 46.7 % of caregivers believed that children have little or no chance of developing the severe form when infected by SARS-CoV-2.
Table 1.
Socio-demographic and vaccine characteristics of the study participants and the children/adolescents they care for stratified by vaccine hesitancy.
| Variables | Hesitant | Not Hesitant | p-value |
|---|---|---|---|
| Age group | |||
| 18–39 years old | 789 (11.7 %) | 5,959 (88.3 %) | <0.001 |
| 40–59 years old | 1,181 (14.3 %) | 7,090 (85.7 %) | |
| 60–74 years old | 58 (21.7 %) | 209 (78.3 %) | |
| ≥ 75 years old | 0 (0 %) | 11 (100 %) | |
| Ethnicity | |||
| White | 1,515 (13.6 %) | 9,622 (86.4 %) | <0.001 |
| Black | 63 (8.1 %) | 716 (91.9 %) | |
| Brown | 413 (13.4 %) | 2,671 (86.6 %) | |
| Yellow | 29 (12.6 %) | 202 (87.4 %) | |
| Indigenous | 2 (8 %) | 23 (92 %) | |
| Gender | |||
| Female | 1,535 (12 %) | 11,284 (88 %) | <0.001 |
| Male | 479 (19.9 %) | 1927 (80.1 %) | |
| Other/I'd rather not inform | 10 (21,7%) | 36 (78.3 %) | |
| Schooling | |||
| Incomplete Fundamental Education | 10 (24.4 %) | 31 (75.6 %) | <0.001 |
| Completed Fundamental Education | 22 (14.28 %) | 132 (85.7 %) | |
| Completed High School | 248 (12.42 %) | 1,748 (87.57 %) | |
| Completed Higher Education | 1,740 (13.3 %) | 11,313 (86.6 %) | |
| Monthly Income | |||
| No income | 41 (14.2 %) | 248 (85.8 %) | |
| Up to US$ 641 | 176 (9.8 %) | 1,615 (90.2 %) | <0.001 |
| US$ 642–855 | 275 (11 %) | 2,222 (89.0 %) | |
| US$ 856–2,137 | 491 (11.70 %) | 3,705 (88.3 %) | |
| >2138 | 936 (16.3 %) | 4,791 (83.7 %) | |
| Change of income during the pandemic | |||
| No income change | 876 (12.2 %) | 6,323 (87.8 %) | <0.001 |
| Increased income | 89 (12.3 %) | 632 (87.7 %) | |
| Decreased income | 1,048 (14.4 %) | 6,244 (85.6 %) | |
| Complete vaccination of caregivers against Covid-19 | |||
| Yes | 1,476 (10.1 %) | 13,163 (89.9 %) | |
| No, only the 1st dose | 154 (64.7 %) | 84 (36.3 %) | |
| Not vaccinated | 392 (96.8 %) | 13 (3.2 %) | <0.001 |
| Routine vaccines | |||
| Vaccinates their children with all vaccines | 1,878 (12.29 %) | 13,080 (85.5 %) | <0.001 |
| Refuses some vaccines | 135 (44.7 %) | 167 (55.3 %) | |
| Does not vaccinate | 11 (84.6 %) | 2 (15.4 %) | |
| Any child with deficiency or chronic disease | |||
| Yes | 212 (11.5 %) | 1,625 (88.5 %) | 0.01 |
| No | 1,813 (13.5 %) | 11,618 (86.5 %) | |
| Children attending on-site education | |||
| Yes (some/all of them) | 1,787 (11.68 %) | 10,832 (70.81 %) | <0.001 |
| No | 116 (6.8 %) | 1600 (93.2 %) | |
| Any child feeling lonely, sadness, depression, anxiety due to social distancing | |||
| Yes | 668 (10.1 %) | 5,936 (89.9 %) | <0.001 |
| No | 1,355 (15.7 %) | 7,299 (84.3 %) | |
| Any children who have had Covid | |||
| Yes | 502 (19.6 %) | 2,057 (80.4 %) | <0.001 |
| No | 1,523 (12 %) | 11,195 (88 %) | |
Table 2 shows some beliefs, fears, and perceptions related to Covid-19 and vaccination, stratified by vaccine hesitancy. Most participants (89.1 %) do not believe that natural immunity is a better protection measure than vaccination, disagree that natural products are more valuable than vaccines (90 %), and believe in the severity of the pandemic (91.3 %). The fear of long-term adverse reactions resulting from vaccination was only reported by approximately 12.9 % of caregivers. The vaccine is also seen as important for a safer return to school by 88.1 % of the caregivers. Higher vaccination hesitancy rates were observed among those who believe that vaccines are safer for adults than for children, who believe vaccines have long-term adverse effects, who feel they need more time to feel safer to have their children vaccinated, who believe that those who have already had Covid-19 do not need vaccination, who believe natural immunity is better than vaccination, that natural products are preferable rather than vaccines, and that the pandemic is not as severe as the press has claimed. Those who disagree that vaccines might ensure a safer return to school also showed higher vaccine hesitancy rates.
Table 2.
Beliefs, fears, and perceptions related to Covid-19 and vaccination, stratified by vaccine hesitancy.
| Variables | Hesitancy yes | Hesitancy no | p-value |
|---|---|---|---|
| Afraid that the son/daughter has an adverse reaction resulting from the vaccine | |||
| Very afraid | 1,399 (75.3 %) | 460 (24.7 %) | <0.001 |
| Somewhat afraid | 451 (13 %) | 3,022 (87 %) | |
| Indifferent | 31 (9 %) | 314 (91 %) | |
| Slightly afraid | 103 (1.9 %) | 5,437 (98.1 %) | |
| Not afraid | 41 (1 %) | 4,022 (99 %) | |
| What is the chance of the child/adolescent having serious Covid-19? | |||
| High chance | 44 (4.3 %) | 990 (95.7 %) | <0.001 |
| Some chance | 244 (5.2 %) | 4,465 (94.8 %) | |
| Not sure | 187 (7.8 %) | 2,197 (92.2 %) | |
| Low chance | 1,345 (19.6 %) | 5,514 (80.4 %) | |
| No chance | 207 (70.6 %) | 86 (29.4 %) | |
| Vaccines are safer for adults than for children and adolescents | |||
| Completely agree | 523 (61.3 %) | 330 (38.7 %) | <0.001 |
| Agree | 585 (41.8 %) | 814 (58.2 %) | |
| Not sure | 513 (11.1 %) | 4,115 (88.9 %) | |
| Disagree | 223 (4.4 %) | 4,894 (95.6 %) | |
| Completely disagree | 178 (5.4 %) | 3,104 (94.6 %) | |
| Vaccines have long-term adverse effects | |||
| Completely agree | 1,054 (93.2 %) | 77 (6.8 %) | <0.001 |
| Agree | 465 (55.4 %) | 375 (44.6 %) | |
| Not sure | 424 (7.7 %) | 5091 (92.3 %) | |
| Disagree | 66 (1.4 %) | 4,570 (98.6 %) | |
| Completely disagree | 18 (0.6 %) | 3,140 (99.4 %) | |
| I need more time to feel safe | |||
| Completely agree | 1334 (86.9 %) | 201 (13.1 %) | <0.001 |
| Agree | 422 (26.2 %) | 1,186 (73.8 %) | |
| Not sure | 107 (9.3 %) | 1,040 (90.7 %) | |
| Disagree | 110 (1.7 %) | 6,235 (98.3 %) | |
| Completely disagree | 55 (1.2 %) | 4,590 (98.8 %) | |
| Vaccines ensure a safer return to on-site education | |||
| Completely agree | 176 (1.7 %) | 10,060 (98.3 %) | <0.001 |
| Agree | 283 (8.8 %) | 2,934 (91.2 %) | |
| Not sure | 263 (70.7 %) | 109 (29.3 %) | |
| Disagree | 540 (82.2 %) | 117 (17.8 %) | |
| Completely disagree | 764 (95.6 %) | 35 (4.8 %) | |
| People who have had Covid-19 do not need to vaccinate | |||
| Completely agree | 832 (91 %) | 82 (9 %) | <0.001 |
| Agree | 427 (75.4 %) | 139 (24.6 %) | |
| Not sure | 319 (43.2 %) | 419 (56.8 %) | |
| Disagree | 305 (6.5 %) | 4,366 (93.5 %) | |
| Completely disagree | 144 (1.7 %) | 8,249 (98.3 %) | |
| Natural immunity is a better solution than vaccination | |||
| Agree | 484 (90.5 %) | 51 (9.5 %) | <0.001 |
| Agree | 408 (85.4 %) | 70 (14.6 %) | |
| Not sure | 369 (56.3 %) | 286 (43.7 %) | |
| Disagree | 496 (16.5 %) | 2,514 (83.5 %) | |
| Completely disagree | 266 (13.2 %) | 10,329 (97.5 %) | |
| The pandemic is not as severe as the media claims | |||
| Completely agree | 326 (82.3 %) | 70 (17.7 %) | <0.001 |
| Agree | 424 (71.5 %) | 169 (28.5 %) | |
| Not sure | 216 (60.7 %) | 140 (39.3 %) | |
| Disagree | 612 (25.1 %) | 1,827 (74.9 %) | |
| Completely disagree | 446 (3.9 %) | 11,045 (96.1 %) | |
| I prefer to use natural products than vaccine | |||
| Completely agree | 495 (95.7 %) | 33 (4.3 %) | <0.001 |
| Agree | 488 (80.7 %) | 117 (19.3 %) | |
| Not sure | 237 (57.1 %) | 178 (42.9 %) | |
| Disagree | 503 (14.2 %) | 3,037 (85.8 %) | |
| Completely disagree | 299 (2.9 %) | 9,896 (97.1 %) | |
A logistic regression was performed to evaluate the variables that were more related to vaccine hesitancy and it is available in Table 3 . Variables with the highest value were the perception that more time is required (OR = 6.80), the perception that it is not necessary to vaccinate those who have already had the infection (OR = 5.37), and the belief that vaccines might have long-term adverse reactions (OR = 5.06).
Table 3.
Multivariate logistic regression to evaluate factors associated to vaccine hesitancy of those responsible for vaccinating children and adolescents.
| Logistic regression for overall hesitancy | ||||
|---|---|---|---|---|
| variables | β | Wald | p-value | AOR (95 %CI) |
| Sex (male × others) | 0.315 | 6.802 | 0.009 | 1.37 (1.08–1.73) |
| Children attending on-site education | 0.397 | 5.634 | 0.018 | 1.48 (1.07–2.06) |
| Fear of adverse reactions | 1.303 | 138.28 | <0.001 | 3.68 (2.96–4.57) |
| Belief that children might develop the severe form of Covid-19 | −0.596 | 34.166 | <0.001 | 0.55 (0.45–0.67) |
| Belief that vaccines are safer for adults than for children | 0.655 | 40.182 | <0.001 | 1.92 (1.57–2.35) |
| Belief that the vaccine has long-term adverse effects | 1.622 | 219.20 | <0.001 | 5.06 (4.08–6.27) |
| Belief that they need to wait longer to vaccinate | 1.918 | 361.06 | <0.001 | 6.80 (5.58–8.29) |
| Belief that the child who has had Covid-19 does not need vaccination | 1.682 | 148.69 | <0.001 | 5.37 (4.10–7.04) |
| Belief that natural immunity is better than vaccination | 0.749 | 15.879 | <0.001 | 2.11 (1.46–3.05) |
| Belief that the pandemic is not as severe | 0.433 | 6.201 | 0.013 | 1.54 (1.09–2.17) |
| Preference for using natural products to increase immunity rather than the vaccine | 1.313 | 67.290 | <0.001 | 3.71 (2.71–5.08) |
| Constant | −4.800 | 358.63 | <0.001 | |
4. Discussion
The present study gathered the opinion of 15,297 caregivers from all regions of the country and shows that 13.3 % of caregivers are hesitant to vaccinate children and adolescents against Covid-19, a number higher than that observed in the study on the willingness of Brazilian adults to vaccinate[7]. In Brazil, a study with 501 caregivers of children and adolescents residing in São Paulo, conducted between May and June 2021, showed vaccine hesitancy of only 2.5 %[11]. International studies have shown a higher hesitancy profile. In December to March 2021, a study from USA, Canada and Israel showed a drop in the willingness of caregivers to have their children vaccinated against Covid-19 [2]. In Saudi Arabia, the parental acceptability of vaccination was 53.7 %[12]. A Chinese study recruited 2,026 caregivers between May 1 and 19, 2020, and showed that 22.3 % were hesitant to have their children vaccinated[10]. A systematic review found a median rate of only 59.3 % of caregivers willing to have their children vaccinated against Covid-19 [3]. These differences in willingness to vaccinate between Brazilians and individuals from other countries shows the importance of understanding the beliefs that support the higher adhesion in Brazil. The present study helps build this knowledge that might provide a better understanding about vaccine hesitancy, which is important both at a national level and as a key factor in devising potential vaccine adhesion strategies in other countries. The strong will of Brazilian parents to vaccinate their children against covid-19 is even more valuable if we understand that they are part of a population that went through the pandemic under the aegis of a president with science-denying behavior, discrediting vaccines and encouraging ineffective treatments such as use of hydroxychloroquine[13]. Furthermore, a large amount of disinformation was spread through social media as showed in a study that evaluated messages from more than 500 public political groups in Brazil finding a conection between disinformation on WhatsApp and a far-right political discourse[14].
The data in the present study clearly show higher hesitancy in having children aged 0–4 years vaccinated, which might be associated to the absence of available studies that ensure the efficacy and safety for this age group so far. Although the vaccine against Covid-19 for children aged 5–11 years has not been approved, yet, and was not available in Brazil at the time of this study, it has already been approved in the USA and in other countries since November 2021. This was the group with the lowest vaccine hesitancy, even lower than the willingness to have adolescents vaccinated, for whom Comirnaty has been already available and approved for use in Brazil since mid-September 2021.
Another finding was the association between the belief that children and adolescents are low risk for Covid-19 and higher vaccine hesitancy. It is important to understand that although this age group shows asymptomatic or light infection compared to adults, this does not mean there are no cases that evolve to more severe conditions, including death. Underestimating the severity in children and adolescents is considered a cognitive illusion created by the direct comparison with the much more significant number of cases of hospitalization and deaths in adults[15]. In Brazil, data reported until December 2021 showed 19,900 confirmed Covid-19 cases in people below 19 years old, who were hospitalized due to severe acute respiratory syndrome (SARS), resulting in 1,422 deaths[16]. In Brazil, 1,412 cases of multisystemic inflammatory syndrome in children have been notified, with 85 deaths[17], while 6,431 MIS-C cases have been notified in the United States, resulting in 55 deaths. Hence, although the severity of Covid-19 in children is a fact regardless of the country, a higher risk profile has been observed in continents with high burden of infectious diseases, such as Latin America and Africa, due to comorbidities and to the poor healthcare system in these regions[18]. This shows that conditions of socioeconomic vulnerability might be a risk factor for the severity of Covid-19[19], which renders vaccination in children even more important in Brazil.
Underestimating Covid-19 severity seems to be as harmful as overestimating the ability of children and adolescents who are deprived of social contact to maintain their mental health. Approximately 43.1 % of caregivers mentioned feelings of loneliness, sadness, depression, or anxiety by their children caused by social distancing; among these caregivers, vaccine hesitancy was lower. Over 13 % of boys and girls aged between 10 and 19 years were estimated to have some type of mental disorder in 2019, prior to the Covid-19 pandemic, with an incidence of 6/100,000 suicide cases in the population between 15 and 19 years old, i.e. the fourth cause of death in this age group[20]. UNICEF has alerted to the fact that the Covid-19 pandemic has worsened the mental health of children and adolescents[20]. A systematic review gathered 36 studies from 11 countries involving a total of 79,781 children and adolescents and showed that 18 to 60 % of the children and adolescents scored above risk thresholds for distress, particularly anxiety and depressive symptoms [21]. Therefore, it is already clear that the taboo mentioned previously must be overcome regarding mental health issues in childhood and adolescence[22] and measures must be taken to remediate knowledge gaps related to how to approach this issue by teachers, healthcare professionals, or caregivers. What is more, it is time to stop the damage, prioritizing the reopening of schools, which can only be safely performed by having children and adolescents vaccinated.
Hesitancy to have children and adolescents vaccinated has also been associated with beliefs related to concerns with vaccine safety. The belief that vaccines against Covid-19 are safer for adults than for children has also been associated with vaccine hesitancy and this might explain why<5 % of the caregivers has not received at least two doses of vaccine, while 13.3 % showed vaccine hesitancy for children and adolescents on average. This also explains why a lower rate was found in a previous study evaluating the willingness of Brazilian adults to vaccinate, only 10.5 %[7]. Apprehension with both short- and long-term adverse reactions are at the forefront of their concerns. However, Cominarty has been approved at all clinical trial phases, for children aged 5 to 11 years[23] and 12 to 17 years[24], which ensures its efficacy and safety for these age groups. Most of the post-vaccine adverse reactions observed in both age groups were light to moderate, similar to those caused by other vaccines with which the public are quite familiar, and with which caregivers usually deal quite confidently, such as fever, headache, myalgia, and pain at the injection site. No cases of myocarditis (a rare adverse effect feared by caregivers) were observed in the clinical trials. This rare event was observed only as the vaccine started being used at a large scale. The U.S. Vaccine Adverse Event Reporting System (VAERS) reported 11 cases of myocarditis in 8.7 million doses of Pfizer vaccine in children aged 5–11 years [25] and 397 cases of myocarditis were reported in 8.9 million doses of Pfizer vaccine in adolescents aged 12 to 17 years[26]. The occurrence of myocarditis after the vaccination with Pfizer-BioNTech vaccine is a rare post-vaccine event; it was also a complication with mild course and possible to treat with only anti-inflammatory medication and rest. No deaths from post-vaccine myocarditis were observed[25], [26]. The fear of myocarditis after the vaccination with Pfizer-BioNTech vaccine should not be a reason for delayed vaccination, since it is an extremely rare event, which is self-limited and treatable with no after-effects. On the other hand, myocarditis caused by SARS-CoV-2 infection, either isolated or within the spectrum of multisystemic inflammatory syndrome, is much more frequent and usually has a more severe course, and might even cause death. Up until late January 2022, 6,581 cases of multisystemic inflammatory syndrome in children had been reported in the United States[27] and 1,412 cases had been reported in Brazil until December 2021, with 85 deaths [17]. A study evaluated the incidence of myocarditis based on notifications by the vaccine adverse event reporting system (VAERS) in the period ranging from December 2020 to August 2021 in the USA and it showed that 1,626 reports of myocarditis were identified among 354,100,845 doses applied with RNA-base vaccines, which means a rate of 0.0000045 %, thus confirming that it is a rare event [34]. Myocarditis rates were higher after the second dose of vaccine in male adolescents aged 12–15 years (70.7 per million doses of Pfizer vaccine) and in adolescents aged 16–17 years (105.9 per million doses of Pfizer vaccine)[28]. A study conducted in England with people older than 16 years old from December 2020 to August 2021 showed that the extra risk of myocarditis was 1 event per 1 million vaccinated and one extra risk of 40 events per 1 million people infected by SARS-CoV-2, which shows that vaccination could be a beneficial option particularly to those people concerned with the risk of having this pathology[29].
Believing that vaccines might have long-term adverse effects was also identified as a factor associated with higher vaccine hesitancy in the logistic regression. This highlights the important fact that there is an information gap about how these new vaccination platforms actually work. Educational activities that explain that RNA-messenger vaccines constitute temporary fragments that allow the reproduction of viral proteins as a training strategy for the immune system that will be responsible for our defense against diseases might help in the process to convince caregivers[30]. The vaccine against Covid-19 that uses this platform does not blend into our genetic material or remain in the organisms of people who take it. After the body produces an immune response triggered by the RNA messenger vaccine, it eliminates even other cells that might occasionally have viral proteins being produced, either via natural infection or by additional doses that some people might receive [31]. Therefore, vaccines are unlikely to have long-term adverse reactions. On the other hand, there is evidence that long Covid-19 has already been observed in adults and in children and adolescents who had MIS-C, with a mean recovery period of 3–6 months of cardiological, neurological, and laboratory changes, although some changes persist for a longer period of time[32], [33], [34]. Data from the Centers for Disease Control (CDC) show that the chance of children and adolescents being diagnosed with diabetes is 2.5 times higher 30 days or more after being infected by Covid-19 [35].
Failure to understand clearly how vaccines actually work might be at the root of another belief associated to higher vaccine hesitancy, which is that natural immunity is better than vaccines. Building immunity using vaccination provides several benefits compared with natural immunity, since it is possible to avoid becoming sick, risk their lives, and even having long Covid-19. A study evaluated that individuals that had recovered from Covid-19 previously had increased immune responses after vaccination (hybrid or heterologous immunity) compared to their vaccinated peers who had not been infected[36]. This emphasizes the value of vaccination for those who already had the disease. It is important to bolster an important notion with caregivers, that natural immunity cannot be separated from vaccine immunity; in fact, the vaccine is created to enhance natural immunity and not to replace it, as already observed in an American study[30]. Brazil has one of the highest rates of cases and deaths attributed to Covid-19 in the world[13]. One of the worst moments of the pandemic in Brazil occurred during the second wave of infection in Manaus in late 2020 and early 2021, driven by the spread of the Gamma variant. The Brazilian population watched perplexed the news of the collapse of the health system with dramatic reports of people dying of asphyxia in the “Earths lungs” due to lack of oxygen in hospitals [37]. The experience of Manaus was a clear example of how assumptions of reaching herd immunity in the absence of vaccination can turn into a tragedy[37].
A study that evaluated beliefs associated with vaccine hesitancy showed that some people understand that good health is the absence of disease, and thus, they infer that this is the standard human condition what make the effect of the vaccine imperceptible[30]. This study also showed that the understanding of the American public of natural immunity of the human body lies across a spectrum of strength and weaknesses, which leads to the conclusion that not everybody needs vaccination [30]. This type of belief can also explain another belief shown by Brazilian caregivers with high vaccine hesitancy rate: that it is preferable to use natural products to increase immunity than to be vaccinated.
Vaccination of children and adolescents is important because although Covid-19 affects adults more severely than children, it cannot be considered a benign disease as the pandemic has had a significant impact on the health of this age group.[38]. We identified 5 key points to recommend vaccination for children and adolescents: 1) Reduction of hospitalization for Covid-19. 2) Reduction of MIS-c cases. 3) Reduce deaths. 4) Reduction of the risk of post-acute sequelae. 5) It is a right of children and adolescents to be healthy. Access to vaccination for protection against disease is in line with the WHO concept of health, which defines it as a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.[39].
The present study is the most comprehensive survey regarding the willingness of caregivers to have their children and adolescents vaccinated in Brazil so far, and it provides important information on which factors are related to vaccine hesitancy. It is also aligned with the five-year strategy (“Gavi 5.0”) developed by GAVI which has as its vision of “Leaving no one behind with immunisation”, in which one of the principles focus on community owned that should ensure community trust and confidence in vaccines by engaging communities[40]. This study aimed not to label parents pejoratively as anti-vaxx but to understand the concerns since according to anthropologist Heidi Larson to build trust in vaccines this must be done through listening and engagement rather than creating a polarized debate[41]. According to the Vaccine messaging guide of Unicef, we see what we believe instead of believing what we see[42]. Thus, knowing the beliefs and feelings of Brazilian parents may help design campaigns and strategies to immunize against disinformation through critical thinking that enable better decisions by families. This study has some limitations that must be addressed.The most important limitations are those already reported in other similar websurvey studies, such as higher recruitment of women, individuals with higher socio-economic status and higher education, which comprise the subgroups that most frequently answer online surveys. This means that hesitancy in the general population may be slightly higher, since those with low monthly income and low education were underrepresented as in most of websurveys[7]. In the present study, there was also a preferential recruitment from the southeastern regions. The choice of the sample for this study by convenience (not probabilistic) was made due to the difficulties imposed by the pandemic, and because it is an urgent context, this fact has demonstrated acceptability among the population. The fact that the form was made online restricts the participation of people who do not have internet. Access to the internet grows every day, in Brazil, in 2019, three out of four Brazilians had access to the internet, which is equivalent to 134 million internet users [43]. In view of these limitations future campaign validation studies should focus especially on the portion of the population with low education and low income that are usually underrepresented in websurvey-type studies.
5. Conclusion
The present study showed that the willingness of caregivers to have their children and adolescents vaccinated in Brazil is high compared to data from international studies. Underestimating the risk of death and complications due to Covid-19 infection in children and adolescents was one of the major factors associated to hesitancy, as well as the fear of adverse reactions. Believing that natural immunity is better than vaccination might lead to vaccine hesitancy and to risky behaviors with unpredictable outcomes.. It is important to understand that it is not about changing the campaigns that are being done, as there is a lot of good work being done and the result of this is that most choose to vaccinate their children but understand the challenges we are facing. In the age of the internet and post modernity, fake news has to be seen as a virus and every effort to stop them must be made. But to defend against the virus of misinformation, it will be necessary to immunize hesitant people against them through critical thinking tools.
Funding
The funding information for this paper is : PPGPASCM-IFF/Fiocruz-FAPERJ (E-29/2021).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2022.11.077.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
The authors do not have permission to share data.
References
- 1.WHO Director-General’s opening remarks at the media briefing on COVID-19 - 11 March 2020 [Internet]. [citado 20 de março de 2021]. Disponível em: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 2.Goldman RD, Krupik D, Ali S, Mater A, Hall JE, Bone JN, et al. Caregiver Willingness to Vaccinate Their Children against COVID-19 after Adult Vaccine Approval. Int J Environ Res Public Health. 28 de setembro de 2021;18(19):10224. [DOI] [PMC free article] [PubMed]
- 3.Pan F, Zhao H, Nicholas S, Maitland E, Liu R, Hou Q. Parents’ Decisions to Vaccinate Children against COVID-19: A Scoping Review. Vaccines (Basel). 14 de dezembro de 2021;9(12):1476. [DOI] [PMC free article] [PubMed]
- 4.Zambrano LD, Newhams MM, Olson SM, Halasa NB, Price AM, Boom JA, et al. Effectiveness of BNT162b2 (Pfizer-BioNTech) mRNA Vaccination Against Multisystem Inflammatory Syndrome in Children Among Persons Aged 12–18 Years — United States, July–December 2021. MMWR Morb Mortal Wkly Rep. 14 de janeiro de 2022;71(2):52–8. [DOI] [PMC free article] [PubMed]
- 5.CDC. CDC Recommends Pediatric COVID-19 Vaccine for Children 5 to 11 Years [Internet]. Centers for Disease Control and Prevention. 2021 [citado 13 de janeiro de 2022]. Disponível em: https://www.cdc.gov/media/releases/2021/s1102-PediatricCOVID-19Vaccine.html.
- 6.Fegert J.M., Vitiello B., Plener P.L., Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health. 2020;14:20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moore DCBC, Nehab MF, Camacho KG, Reis AT, Junqueira-Marinho M de F, Abramov DM, et al. Low COVID-19 vaccine hesitancy in Brazil. Vaccine. 8 de outubro de 2021;39(42):6262–8. [DOI] [PMC free article] [PubMed]
- 8.Khubchandani J., Sharma S., Price J.H., Wiblishauser M.J., Sharma M., Webb F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J Community Health abril de. 2021;46(2):270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wong MCS, Wong ELY, Huang J, Cheung AWL, Law K, Chong MKC, et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine. 12 de fevereiro de 2021;39(7):1148–56. [DOI] [PMC free article] [PubMed]
- 10.Lin Y, Hu Z, Zhao Q, Alias H, Danaee M, Wong LP. Chinese parents’ intentions to vaccinate their children against SARS-CoV-2 infection and vaccine preferences. Hum Vaccin Immunother. 10 de dezembro de 2021;1–10. [DOI] [PMC free article] [PubMed]
- 11.Bagateli LE, Saeki EY, Fadda M, Agostoni C, Marchisio P, Milani GP. COVID-19 Vaccine Hesitancy among Parents of Children and Adolescents Living in Brazil. Vaccines (Basel). 30 de setembro de 2021;9(10):1115. [DOI] [PMC free article] [PubMed]
- 12.Altulaihi BA, Alaboodi T, Alharbi KG, Alajmi MS, Alkanhal H, Alshehri A. Perception of Parents Towards COVID-19 Vaccine for Children in Saudi Population. Cureus. 13(9):e18342. [DOI] [PMC free article] [PubMed]
- 13.Silva H.M. The Brazilian Scientific Denialism Through The American Journal of Medicine. Am J Med. 2021;134(4):415–416. doi: 10.1016/j.amjmed.2021.01.003. 1o de abril de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Soares FB, Recuero R, Volcan T, Fagundes G, Sodré G. Research note: Bolsonaro’s firehose: How Covid-19 disinformation on WhatsApp was used to fight a government political crisis in Brazil. Harvard Kennedy School Misinformation Review [Internet]. 29 de janeiro de 2021 [citado 8 de setembro de 2022]; Disponível em: https://misinforeview.hks.harvard.edu/article/research-note-bolsonaros-firehose-how-covid-19-disinformation-on-whatsapp-was-used-to-fight-a-government-political-crisis-in-brazil/.
- 15.Cognitive Illusions and How Not to Write About COVID-19 and Children | Science-Based Medicine [Internet]. 2021 [citado 10 de janeiro de 2022]. Disponível em: https://sciencebasedmedicine.org/cognitive-illusions-and-how-not-to-write-about-covid-19-and-children/.
- 16.Boletim Epidemiológico No 92 - Boletim COE Coronavírus — Português (Brasil) [Internet]. [citado 10 de janeiro de 2022]. Disponível em: https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/boletins/boletins-epidemiologicos/covid-19/2021/boletim_epidemiologico_covid_92_10dez21.pdf/view.
- 17.Boletim Epidemiológico No 91 - Boletim COE Coronavírus — Português (Brasil) [Internet]. [citado 10 de janeiro de 2022]. Disponível em: https://www.gov.br/saude/pt-br/centrais-de-conteudo/publicacoes/boletins/boletins-epidemiologicos/covid-19/2021/boletim_epidemiologico_covid_91_6dez21_final6dez.pdf/view.
- 18.Nepomuceno, M. R. Vulnerable groups at increased risk of COVID-19 in sub-Saharan Africa: the case of the HIV population [Internet]. Max Planck Institute for Demographic Research. [citado 13 de janeiro de 2022]. Disponível em: https://www.demogr.mpg.de/en/publications_databases_6118/publications_1904/preprints/vulnerable_groups_at_increased_risk_of_covid_19_in_sub_saharan_africa_the_case_of_the_hiv_population_6780.
- 19.Rocha R., Atun R., Massuda A., Rache B., Spinola P., Nunes L., et al. Effect of socioeconomic inequalities and vulnerabilities on health-system preparedness and response to COVID-19 in Brazil: a comprehensive analysis. The Lancet. Global Health. 2021;9(6):e782–e792. doi: 10.1016/S2214-109X(21)00081-4. 1o de junho de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The State of the World’s Children 2021 | UNICEF [Internet]. [citado 17 de janeiro de 2022]. Disponível em: https://www.unicef.org/reports/state-worlds-children-2021.
- 21.Viner R, Russell S, Saulle R, Croker H, Stansfield C, Packer J, et al. School Closures During Social Lockdown and Mental Health, Health Behaviors, and Well-being Among Children and Adolescents During the First COVID-19 Wave: A Systematic Review. JAMA Pediatr. 18 de janeiro de 2022; [DOI] [PubMed]
- 22.Silva Filho O.C., da, Minayo MC de S. Triple taboo: considerations about suicide among children and adolescents. Cien Saude Colet julho de. 2021;26(7):2693–2698. doi: 10.1590/1413-81232021267.07302021. [DOI] [PubMed] [Google Scholar]
- 23.Walter EB, Talaat KR, Sabharwal C, Gurtman A, Lockhart S, Paulsen GC, et al. Evaluation of the BNT162b2 Covid-19 Vaccine in Children 5 to 11 Years of Age. N Engl J Med. 6 de janeiro de 2022;386(1):35–46. [DOI] [PMC free article] [PubMed]
- 24.Ali K, Berman G, Zhou H, Deng W, Faughnan V, Coronado-Voges M, et al. Evaluation of mRNA-1273 SARS-CoV-2 Vaccine in Adolescents. New England Journal of Medicine. 9 de dezembro de 2021;385(24):2241–51. [DOI] [PMC free article] [PubMed]
- 25.Hause AM, Baggs J, Marquez P, Myers TR, Gee J, Su JR, et al. COVID-19 Vaccine Safety in Children Aged 5-11 Years - United States, November 3-December 19, 2021. MMWR Morb Mortal Wkly Rep. 31 de dezembro de 2021;70(5152):1755–60. [DOI] [PMC free article] [PubMed]
- 26.Hause AM, Gee J, Baggs J, Abara WE, Marquez P, Thompson D, et al. COVID-19 Vaccine Safety in Adolescents Aged 12-17 Years - United States, December 14, 2020-July 16, 2021. MMWR Morb Mortal Wkly Rep. 6 de agosto de 2021;70(31):1053–8. [DOI] [PMC free article] [PubMed]
- 27.CDC. COVID Data Tracker [Internet]. Centers for Disease Control and Prevention. 2020 [citado 7 de fevereiro de 2022]. Disponível em: https://covid.cdc.gov/covid-data-tracker.
- 28.Oster M.E., Shay D.K., Su J.R., Gee J., Creech C.B., Broder K.R., et al. Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From. 2022;327(4):331–340. doi: 10.1001/jama.2021.24110. December 2020 to August 2021. JAMA. 25 de janeiro de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patone M, Mei XW, Handunnetthi L, Dixon S, Zaccardi F, Shankar-Hari M, et al. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat Med. 14 de dezembro de 2021;1–13. [DOI] [PMC free article] [PubMed]
- 30.O’Shea P, L’Hôte E, Aassar M, Hestres L, Rochman A. Communicating About Vaccination in the United States: A FrameWorks Strategic Brief [Internet]. 2021 [citado 5 de maio de 2022]. Disponível em: https://www.frameworksinstitute.org/publication/communicating-about-vaccination-in-the-united-states-a-frameworks-strategic-brief/.
- 31.CDC. COVID-19 Vaccine Facts [Internet]. Centers for Disease Control and Prevention. 2021 [citado 5 de maio de 2022]. Disponível em: https://www.cdc.gov/coronavirus/2019-ncov/vaccines/facts.html.
- 32.Penner J., Abdel-Mannan O., Grant K., Maillard S., Kucera F., Hassell J., et al. 6-month multidisciplinary follow-up and outcomes of patients with paediatric inflammatory multisystem syndrome (PIMS-TS) at a UK tertiary paediatric hospital: a retrospective cohort study. The Lancet Child & Adolescent. Health. 2021;5(7):473–482. doi: 10.1016/S2352-4642(21)00138-3. 1o de julho de. [DOI] [PubMed] [Google Scholar]
- 33.Farooqi KM, Chan A, Weller RJ, Mi J, Jiang P, Abrahams E, et al. Longitudinal Outcomes for Multisystem Inflammatory Syndrome in Children. Pediatrics. agosto de 2021;148(2):e2021051155. [DOI] [PubMed]
- 34.Capone CA, Misra N, Ganigara M, Epstein S, Rajan S, Acharya SS, et al. Six Month Follow-up of Patients With Multisystem Inflammatory Syndrome in Children. Pediatrics. 29 de julho de 2021;e2021050973. [DOI] [PubMed]
- 35.Barrett CE. Risk for Newly Diagnosed Diabetes 30 Days After SARS-CoV-2 Infection Among Persons Aged 18 Years — United States, March 1, 2020–June 28, 2021. MMWR Morb Mortal Wkly Rep [Internet]. 2022 [citado 31 de janeiro de 2022];71. Disponível em: https://www.cdc.gov/mmwr/volumes/71/wr/mm7102e2.htm. [DOI] [PMC free article] [PubMed]
- 36.Bates TA, McBride SK, Leier HC, Guzman G, Lyski ZL, Schoen D, et al. Vaccination before or after SARS-CoV-2 infection leads to robust humoral response and antibodies that effectively neutralize variants. Sci Immunol. 25 de janeiro de 2022;eabn8014. [DOI] [PMC free article] [PubMed]
- 37.Malta M., Strathdee S.A., Garcia P.J. The brazilian tragedy: Where patients living at the “Earth’s lungs” die of asphyxia, and the fallacy of herd immunity is killing people. EClinicalMedicine fevereiro de. 2021;32 doi: 10.1016/j.eclinm.2021.100757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Why COVID-19 Vaccines are Important for Children [Internet]. [citado 16 de setembro de 2022]. Disponível em: https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/covid-19-vaccine-for-children/why-covid-19-vaccines-are-important-for-children/.
- 39.Constitution of the World Health Organization [Internet]. [citado 16 de setembro de 2022]. Disponível em: https://www.who.int/about/governance/constitution.
- 40.Phase 5 (2021–2025) [Internet]. [citado 10 de novembro de 2022]. Disponível em: https://www.gavi.org/our-alliance/strategy/phase-5-2021-2025.
- 41.Larson HJ, Gakidou E, Murray CJL. The Vaccine-Hesitant Moment. N Engl J Med. 7 de julho de 2022;387(1):58–65. [DOI] [PMC free article] [PubMed]
- 42.Vaccine messaging guide | UNICEF [Internet]. [citado 10 de novembro de 2022]. Disponível em: https://www.unicef.org/documents/vaccine-messaging-guide.
- 43.Cetic.br - Centro Regional para o Desenvolvimento da Sociedade da Informação [Internet]. Cetic.br - Centro Regional para o Desenvolvimento da Sociedade da Informação. [citado 31 de outubro de 2022]. Disponível em: https://cetic.br.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors do not have permission to share data.