Abstract
Introduction:
Evidence-based early stroke care as reflected by fulfillment of process performance measures, is strongly related to better patient outcomes after stroke and transient ischemic attack (TIA). Detailed data on the resilience of stroke care services during the COVID-19 pandemic are limited. We aimed to examine the quality of early stroke care at Danish hospitals during the early phases of the COVID-19 pandemic.
Materials and methods:
We extracted data from Danish national health registries in five time periods (11 March, 2020–27 January, 2021) and compared these to a baseline pre-pandemic period (13 March, 2019–10 March, 2020). Quality of early stroke care was assessed as fulfilment of individual process performance measures and as a composite measure (opportunity-based score).
Results:
A total of 23,054 patients were admitted with stroke and 8153 with a TIA diagnosis in the entire period. On a national level, the opportunity-based score (95% confidence interval [CI]) at baseline for ischemic patients was 81.1% (80.8–81.4), for intracerebral hemorrhage (ICH) 85.5% (84.3–86.6), and for TIA 96.0% (95.3–96.1). An increase of 1.1% (0.1–2.2) and 1.5% (0.3–2.7) in the opportunity-based score was observed during the first national lockdown period for AIS and TIA followed by a decline of −1.3% (−2.2 to −0.4) in the gradual reopening phase for AIS indicators. We found a significant negative association between regional incidence rates and quality-of-care in ischemic stroke patients implying that quality decreases when admission rates increase.
Conclusion:
The quality of acute stroke/TIA care in Denmark remained high during the early phases of the pandemic and only minor fluctuations occurred.
Keywords: COVID-19, stroke, transient ischemic attack, incidence, quality
Background
Since COVID-19 was declared a pandemic in March 2020 evidence suggests substantial changes in access to and quality-of-care for other major serious and life-threatening conditions, such as stroke.1,2
Stroke center admission and multidisciplinary investigations and treatment are the hallmarks of modern stroke care. Fulfillment of quality performance measures is associated with lower stroke recurrence, lower mortality, and improved functional outcome. 3 Therefore, monitoring quality-of-care using performance measures is an important part of health-care. In Denmark, it is mandatory for all stroke units providing acute stroke care to monitor the quality of the provided early care by reporting to a national clinical quality database, the Danish Stroke Registry (DSR). 4 Studies on quality of stroke care during the pandemic have been sparse and have mainly focused on changes in reperfusion therapy rates.5–7 However, in a global perspective, treatment with intravenous thrombolysis and thrombectomy are only used in 7.3% and 1.9% of cases with ischemic stroke, respectively. 8 Information about the quality of other key elements of early stroke care during the pandemic is limited and may provide insight on the resilience of every link in the “stroke chain” and help improve stroke care in the future.
We undertook a nationwide study where we examined quality-of-care for patients with acute stroke and transient ischemic attack (TIA) as reflected by care performance measures before and at different time periods during the early stages of the pandemic.
Methods
Setting and study population
In Denmark, there is equal, unrestricted, and tax-funded access to acute care. All acute stroke and TIA patients are evaluated at public hospitals and data on each event is reported to the Danish Stroke Registry (DSR). The DSR contains structured data that is collected prospectively and nationwide. It is estimated that more than 80% of all acute strokes are hospitalized at stroke units and the sensitivity and positive predictive value of registration in the DSR at the stroke units has been found to be >90%. 9
We included acute ischemic stroke (AIS), intracerebral hemorrhage (ICH), as well as TIA events. Events with missing information on residency (healthcare region) were excluded.
Stroke care performance measures
The stroke care performance measures cover acute treatment (admission to stroke unit <24 h from onset, scan <6 h from admission, revascularization offered, timing of thrombolysis, and groin puncture in case of thrombectomy), prophylactic treatment, and the timing thereof (start of antiplatelet within the second day of admission, start of oral anticoagulant <14 days for patients eligible), carotid vessel imaging, and early rehabilitation (physio- and occupational therapy evaluation, out-of-bed orders, nutrition, and swallow screening). The indicators were reported as an opportunity-based score which was calculated as the number of indicators fulfilled for a patient divided by the number of indicators estimated to be relevant for that patient. 10 In the case of missing single indicators, the opportunity based score was calculated as all relevant available and fulfilled indicators divided by all relevant available indicators. In Table 2, the indicators relevant for the subgroups are listed.
Table 2.
Quality-of-care indicators for acute ischemic stroke (AIS), intracerebral hemorrhage (ICH), and transient ischemic attack (TIA) in the Danish stroke registry.
| AIS | TIA | ICH | |
|---|---|---|---|
| Reperfusion therapy | X | ||
| IVT treatment | X | ||
| EVT treatment | X | ||
| Door to needle time <45 min (IVT) | X | ||
| Door to groin puncture <180 min (EVT) | X | ||
| Admission to stroke unit admission <24 h | X | X | |
| Platelet inhibitors (AIS, TIA w/o AFIB) <48 h | X | X | |
| Anticoagulation <14 days (AIS, TIA + AFIB) | X | X | |
| CT/MRI <6 h from admission | X | X | X |
| Physiotherapy assessment <48 h of admission | X | X | |
| Occupational therapy assessment <48 h admission | X | X | |
| Out of bed orders on day of admission | X | X | |
| Nutritional screening <48 h | X | X | |
| Swallowing screen (indirect) on day of admission | X | X | |
| Swallowing screen (direct) on day of admission | X | X | |
| Carotid vessel imaging <96 h (AIS)/48 h (TIA) of admission | X | X | |
| Carotid surgery (AIS, TIA w/symptomatic stenosis) <14 days of admission | X | X |
AFIB: atrial fibrillation; AIS: acute ischemic stroke; EVT: endovascular therapy; IVT: intravenous thrombolysis; TIA: transient ischemic attack.
The presented performance measures were used by the DSR to monitor quality of Danish stroke and TIA treatment.
The quality indicators were evaluated in different time periods during the pandemic: “Baseline” was defined as 13 March, 2019–10 March, 2020 (the year prior to the lockdown.) “first national lockdown” was 11 March–15 April, 2020. “Gradual reopening” 16 April–8 June, 2020. “Few restrictions” 9 June–30 September, 2020. “Regional lockdown” 1 October–15 December, 2020. And finally, “second national lockdown” was 16 December, 2020–27 January, 2021. The first vaccine arrived in Denmark on 27th of December 2020 and did not affect admission numbers for the period studied. 11
Stroke severity was measured by the Scandinavian Stroke Scale (SSS). A mild stroke was defined as an SSS score between 45–58, moderate stroke 30–44, severe stroke as 15–29, and very severe stroke as 0–14. 12
Statistical analyses
We first compared opportunity-based scores in five time periods during the early phases of the pandemic to the baseline pre-pandemic period on a national level and stratified by diagnosis. The same analyses were then performed for each healthcare region. The Danish national health care system is divided into five regions. We extracted data for the five different regions to examine if fulfillment of quality indicators differed between regions. To account for an effect of incidence rates on quality-of-care in each region, we calculated (1) an aggregated opportunity-based scores for each healthcare region and (2) logarithmic transformed regional incidence rates. We then used random effects meta-regression analysis to investigate whether quality-of-care was affected by regional incidence rates. Regional incidence rates were calculated as number of cases in each region during the interrogated time period divided by person-time experienced for all people in Denmark in the time period. The incidence rate was measured as rate of cases per 1000 person-years. To make comparison between the five regions possible we adjusted for the regional effects by adding “region” as a covariate in the meta regression. To visualize the association graphically, we centered the regional opportunity-based scores and the log-transformed regional incidence rates and used these variables as the axes in a bubble plot with a regression line obtained from meta regression of the two variables and intercept. Logarithmic transformation of data was performed as we aimed to investigate relative differences between stroke units with different size and admission rates.
Data from OurWorldinData.org was used for national COVID-19 hospitalization rates in different countries during the pandemic (Supplemental Figure 2). 13
Data are reported by mean (95% confidence interval [CI]), median (interquartile range [IQR]), numbers, and percentages, as appropriate. The opportunity-based score is reported as means with 95% CI. All analyses were conducted using Stata version 16 (StataCorp LLC).
Research ethical approval is not required for register-based studies in Denmark. Upon approval from the Danish Data Protection Agency, pseudonymized data can be accessed through the Danish Health Data Authority and Statistics Denmark for researchers at authorized institutions.
Results
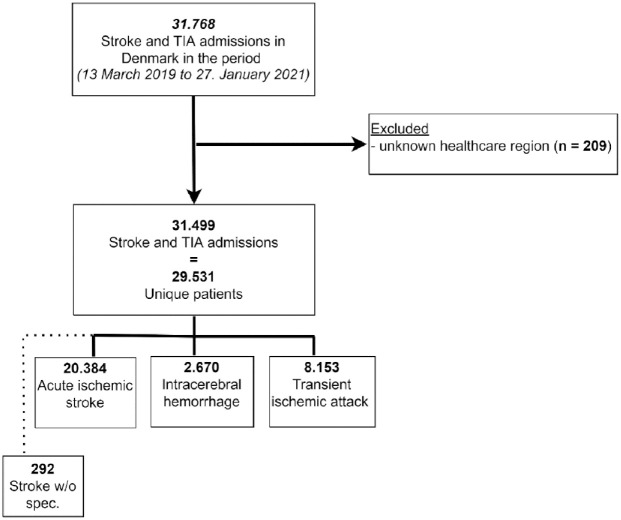
In the study period, a total of 31,499 stroke and TIA events were registered, corresponding to 23,054 cases of AIS or ICH, and 8153 cases of TIA (Figure 1). The mean age of the patients were 74.1 years and 56% were male (Table 1). Type of stroke, stroke severity, and prevalence of comorbidities (diabetes, hypertension, atrial fibrillation, prior myocardial infarction, and peripheral arterial disease) expressed as proportions was unchanged during the study period (Table 1). The number of COVID-19 hospitalizations per million inhabitants in Denmark compared to Australia, Norway, USA, and Italy during the period March 1, 2020 to January 27, 2021 is visualized in Supplement Figure 1. 13
Figure 1.
Study flowchart describing included events.
TIA: transient ischemic attack.
Stroke with-out specification (n = 292) is considered an ischemic stroke.
Table 1.
Study population characteristics, stratified by period.
| Baseline | First national lockdown | Gradual reopening | Few restrictions | Regional lockdown | Second national lockdown | |
|---|---|---|---|---|---|---|
| N = 16,519 | N = 1475 | N = 2585 | N = 5485 | N = 3580 | N = 1855 | |
| Age, median (IQR) | 74.1 (64.5–81.7) | 73.8 (65.2–81.2) | 74.3 (64.7–81.4) | 74 (64.1–81.1) | 74.4 (65.3–81.6) | 75.1 (65.8–82.4) |
| Male, % (n) | 55.8 (9212) | 56.3 (830) | 56.6 (1463) | 56.1 (3079) | 55.5 (1987) | 57.8 (1072) |
| Very severe stroke, % (n) | 5.3 (852) | 6.1 (89) | 4.3 (109) | 5.0 (266) | 5.1 (178) | 5.1 (92) |
| Severe stroke, % (n) | 6.6 (1063) | 6.9 (100) | 6.2 (157) | 5.8 (309) | 6.9 (240) | 6.6 (121) |
| Moderate stroke, % (n) | 16.0 (2593) | 16.5 (239) | 14.1 (357) | 15.7 (842) | 14.8 (519) | 17.0 (309) |
| Mild stroke, % (n) | 72.1 (11655) | 70.4 (1020) | 75.3 (1903) | 73.6 (3952) | 73.2 (2558) | 71.3 (1298) |
| SSS score, median (IQR) | 53 (43–58) | 52.5 (42–58) | 54 (45–58) | 54 (44–58) | 54 (43–58) | 53 (43–58) |
| AIS, % (n) | 64.6 (10672) | 63.9 (943) | 65.4 (1691) | 65.7 (3605) | 63.0 (2254) | 65.7 (1219) |
| ICH, % (n) | 8.5 (1397) | 10.0 (147) | 7.5 (193) | 7.7 (422) | 10.1 (362) | 8.0 (149) |
| TIA, % (n) | 25.9 (4279) | 25.3 (373) | 26.2 (676) | 25.6 (1405) | 26.3 (941) | 25.8 (479) |
| Diabetes (known/newly diagnosed), % (n) | 15.8 (2556) | 17.2 (249) | 15.8 (401) | 16.2 (867) | 15.7 (553) | 17.4 (319) |
| Hypertension (known/newly diagnosed), % (n) | 58.7 (9659) | 60.7 (892) | 58.1 (1498) | 58.7 (3203) | 59.8 (2133) | 59.7 (1102) |
| Atrial fibrillation (known/newly diagnosed), % (n) | 18.2 (3008) | 18.4 (271) | 18.5 (478) | 17.6 (959) | 19.2 (682) | 18.5 (343) |
| Acute myopcardial infarction (known/newly diagnosed), % (n) | 7.2 (1183) | 5.9 (87) | 7.6 (196) | 7.2 (392) | 6.5 (232) | 6.7 (123) |
| Peripheral artery disease (known/newly diagnosed), % (n) | 4.5 (731) | 3.3 (48) | 4.3 (108) | 4.4 (236) | 4.2 (146) | 4.9 (90) |
SSS: Scandinavian Stroke Scale.
Process performance measures for AIS, ICH, and TIA are listed in Table 2. On a national level, the opportunity-based score (95% CI) at baseline for ischemic stroke patients was 81.1% (CI: 80.8–81.4), for ICH 85.5% (84.3%–86.6%), and for TIA 96.0% (95.3%–96.12%; Table 3). A slight increase of 1.1% (CI: 0.1%–2.2%) and 1.5% (0.3%–2.7%) in the opportunity-based score was observed during the first national lockdown period for AIS and TIA compared to the baseline period. This was followed by a decline of −1.3% (−2.2% to −0.4%) for AIS indicators in the gradual reopening phase and −1.1% (−2.1% to −0.1%) during the second national lockdown. (Table 3). Regional performance measures in different time periods during the pandemic compared to the baseline period demonstrated only minor changes and followed the national trend (Supplemental Table 2).
Table 3.
National opportunity score on quality of stroke and TIA care indicators stratified by period and compared baseline (pre-pandemic period).
| Baseline (Ref), % | First national lockdown, change in % | p-Value | Gradual reopening, change in % | p-Value | Few restrictions, change in % | p-Value | Regional lockdown, change in % | p-Value | Second national lockdown, change in % | p-Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| AIS | 81.11 (80.79–81.43) | 1.14 (0.11 to 2.18) | 0.030 | −1.31 (−2.20 to −0.41) | 0.004 | −0.45 (−1.07 to 0.18) | 0.159 | −0.18 (−0.92 to 0.56) | 0.640 | −1.09 (−2.09 to −0.10) | 0.030 |
| TIA | 95.73 (95.33–96.12) | 1.46 (0.28 to 2.65) | 0.016 | −0.05 (−1.07 to 0.96) | 0.919 | 0.16 (−0.59 to 0.90) | 0.675 | −0.19 (−1.12 to 0.73) | 0.682 | 0.10 (−1.14 to 1.33) | 0.879 |
| ICH | 85.46 (84.29–86.64) | 1.62 (−2.04 to 5.28) | 0.386 | 0.73 (−2.53 to 3.98) | 0.661 | −2.15 (−4.69 to 0.39) | 0.097 | −1.33 (−4.02 to 1.36) | 0.331 | −0.89 (−4.66 to 2.89) | 0.645 |
Significant changes (p < 0.05) are marked in bold.
Regional changes in opportunity-based scores are visualized in Figure 2.
Figure 2.
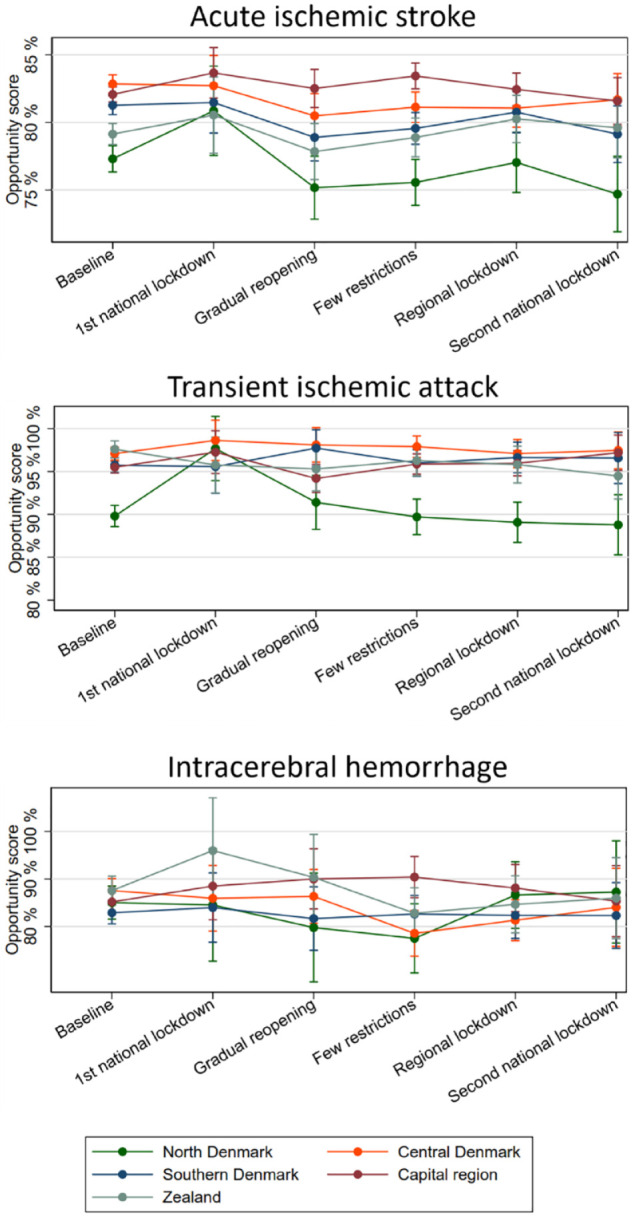
Margins-plot on process performance measures for acute ischemic stroke, transient ischemic attack, and intracerebral hemorrhage (opportunity score) by health care region.
All process performance measures for AIS patients before and during the pandemic are available in Supplemental Table 1. Performance measures stratified by whether patients with ischemic stroke were admitted directly to a stroke unit or not are available in Supplemental Table 3. Overall, quality-of-care were lower in patients not directly admitted to a stroke unit.
The proportion of patients with at least one missing process performance indicator for acute ischemic stroke (0%–2%) was low in all healthcare regions (Supplemental Figure 2).
To account for an effect of different regional incidence rates of quality of stroke care, we calculated an aggregated opportunity-based scores per healthcare region and used logarithmic transformed regional incidence rates. We found a significant negative association between regional incidence rates and opportunity-based scores in patients with AIS implying that quality decreases when admission rates increase (Figure 3), Coef. = −15.3% (−22.8 to −7.8), p < 0.001. No significant effect of admission rates on the opportunity score were found for ICH and TIA patients (data not shown).
Figure 3.
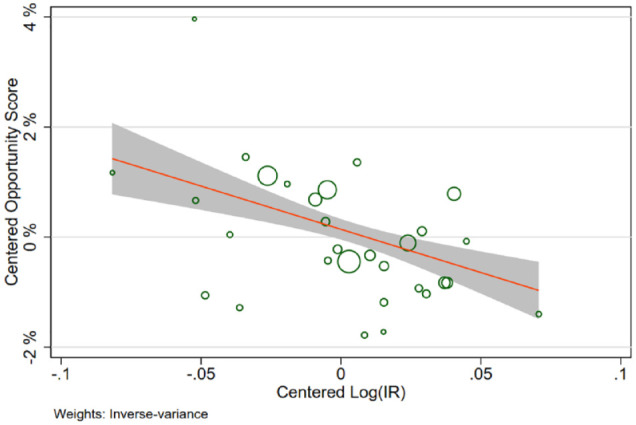
Association of opportunity scores to regional incidence rates (log) for ischemic stroke.
Bubble-plot. Centered opportunity scores and centered logarithmically transformed incidence rates stratified by region and time period are plotted against each other with a regression line obtained from fixed-effects meta regression. The sizes of the circles reflect the number of observations, with larger circles corresponding to greater precision of the estimates and greater weight in the analysis.
Discussion
We found that the quality of acute stroke (AIS, ICH) and TIA care in Denmark during the start of the pandemic remained high with only minor fluctuations. During the first national lockdown a slight increase in stroke care quality was observed. This was followed by a decline during reopening phase and second national lockdown, however, the magnitudes of all changes were minimal. The observed change in acute stroke care quality and regional differences may be explained by increased regional incidence rates/admission rates of stroke following the first national lockdown. Our study provides in depth details on fulfillment of different acute stroke and TIA care quality indicators during the pandemic.
Early in the pandemic, direct and indirect consequences on the quality of global stroke care were observed, as lower stroke admission rates, increased prehospital delay, and declining rates of reperfusion therapy were observed. 14 In one of the first published studies, massive decreases in stroke admissions and thrombolysis and thrombectomy rates were reported among 280 surveyed Chinese hospitals in February 2020. 15 Later reports on the overall incidence and admission rates for stroke have reported more varied results.7,16–20 In a recent nationwide study we found only relatively small changes of admission rates for stroke and TIA with a decrease of 7% during the first lockdown and an increase of 5%–7% in the following periods of the pandemic. 11 Prehospital and in-hospital workflow metrics have been reported to be affected during the pandemic in previous studies, resulting in decreased utilization of reperfusion treatment.5–7 In this study, 24.6% received IVT and/or EVT before the pandemic and 21.7%–27.1% during different phases of the pandemic. Only minor changes in in-hospital workflow occurred measured as treatment with IVT within 45 min of arrival (84.1% before and 80.3%–84.8% during) and neuroimaging performed within 6 h of stroke center admission (91.6% before and 90.4%–93.9% during) were observed (Supplemental Table 1). Door to groin puncture and rate of stroke center admission <24 h from onset was also largely unchanged in this study. By comparison, in a study from Australia using a national stroke registry, a decreased stroke unit access as well as fewer stroke patients admitted in stroke center beds was observed. This translated into a decline in quality-of-care, and prolonged door-to-needle times during the first months of the pandemic. 21 In a French study, carotid endarterectomy procedures for symptomatic carotid stenosis decreased during the first peak (March to May 2020) of the pandemic with a later increase. 22 Finally, a large registry-based cohort study from United Kingdom found preserved stroke quality-of-care measures and improvement in some (direct access to stroke unit care, 1-h brain imaging, and swallow screening) during the lockdown. Only the period before and during the first lockdown (March 23–April 30, 2020) was investigated. 23
Stroke care is multidisciplinary and includes assessment of physiotherapy, mobilization, occupational therapy needs as well as nutritional, and dysphagia screening. 3 We found only smaller changes on several quality-of-care indicators, without obvious large declines in a single factor. The impact of the pandemic on stroke care is likely to affect multiple areas of care and thus an aggregated opportunity-based score was selected.2,23 Despite some changes being significant in this study, it is important to emphasize that the magnitude of these changes was minimal (e.g. for AIS, −2.2% to −0.4%). These results are line with results from UK during the first lockdown. 23 Provision of stroke care has likely been heterogenous in different countries, depending on pandemic control/hospitalization burden, differences in health care systems and pre-pandemic organization of stroke care. 24 Further, there may have been regional changes in transportation protocols/triage processes, reallocation of neurology and stroke beds and staff to COVID-19 patients or departments. 15 We found regional differences in quality care following the first national lock down which may be a reflection of regional increases in incidence/admission rates and increased patient flow at the stroke wards. A similar picture with increased admission rates following the first lockdown has recently been reported.11,25
From an organizational point of view, stroke care remained unchanged in Denmark and only a small proportion of stroke personnel was reallocated to staff COVID-19 departments. Denmark enacted strict and early government regulations, including stay-at-home orders, and early mass scale up testing. The healthcare system was never overwhelmed and experienced lower COVID-19 hospitalization rates compared to many other countries. 26 During the first national lockdown outpatients clinics were closed, freeing healthcare workers to man the wards, which may explain the minor increase in quality-of-care during the first national lockdown.
The main strength of this study is the use of a compulsory, nationwide stroke registry with individual patient data on quality-of-care indicators from all Danish stroke units, both comprehensive and non-comprehensive centers. Further, we were able to perform aggregated quality-of-care scores for each healthcare region and compare it to the regional stroke/TIA incidence rates, highlighting the association of stroke incidence rates, and quality-of-care. There are, however, limitations: Not all stroke patients are admitted to a stroke unit and no stroke care performance measures are available for these. The proportion of patients not admitted to a stroke unit at all and thus not registered in the DSR have been estimated to be 6% in 2020 (6%) and 8% in 2021.27,28 These patients are often elderly nursing home residents for whom there are no treatment or rehabilitation consequences. Quality-of-care were lower in patients not directly admitted to a stroke unit. The quality-of-care indicators for stroke/TIA do not include information on COVID-19 infection status and we do not have information on whether quality-of-care remained high from a patient/relative perspective (support, level of information, and involvement of the relatives).
Conclusion
The quality of acute stroke/TIA care in Denmark remained high during the early stages of the pandemic and only minor fluctuations occurred. During the first national lockdown, a small increase in stroke care performance measures was observed, followed by a decline in the gradual reopening phase and second national lockdown. Denmark experienced lower COVID-19 hospitalization rates compared to many other countries.
Supplemental Material
Supplemental material, sj-docx-1-eso-10.1177_23969873221139695 for Quality in stroke care during the early phases of the COVID-19 pandemic: A nationwide study by Rolf A Blauenfeldt, Jakob N Hedegaard, Christina Kruuse, David Gaist, Troels Wienecke, Boris Modrau, Dorte Damgaard, Søren P Johnsen, Grethe Andersen and Claus Z Simonsen in European Stroke Journal
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: RAB is supported by National Institute of Health (1R01NS112511-01A1). CK is supported from Novo Nordisk Foundation (NNF18OC0031840). DG is supported by Novo Nordisk Foundation (NNF20OC0064637). GA is supported by Novo Nordisk Foundation (NNF18OC0052924, NNF20OC0060998) Trygfoundation (120636), Lundbeck Foundation (349-2020-907), and National Institute of Health (1R01NS112511-01A1). CZS is supported by a research grant from Novo Nordisk Foundation (NNF17OC0029520) and Health Research Foundation of Central Denmark Region. Authors DD, TWS, JNH, BM, and SPJ reports no conflict of interest.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study is supported by a research grant from Lundbeck foundation (349-2020-907).
Ethical approval: Ethical approval is not required for register-based studies in Denmark. Data can be accessed through the Danish Health Data Authority and Statistics Denmark for researchers at authorized institutions.
Guarantor: CZS.
Author contributions: RAB, CZS, GA, and SPJ researched literature and conceived the study. JNH, SPJ, and RAB performed the data analysis, and all authors were involved in critical interpretation of data. RAB wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
ORCID iDs: Rolf A Blauenfeldt  https://orcid.org/0000-0002-4846-9516
https://orcid.org/0000-0002-4846-9516
Christina Kruuse  https://orcid.org/0000-0002-4210-0523
https://orcid.org/0000-0002-4210-0523
Supplemental material: Supplemental material for this article is available online.
References
- 1. Markus HS, Brainin M. Leading opinion COVID-19 and stroke-a global world stroke organization perspective. Int J Stroke 2020; 15(4): 361–364. [DOI] [PubMed] [Google Scholar]
- 2. Dengler J, Prass K, Palm F, et al. Changes in nationwide in-hospital stroke care during the first four waves of COVID-19 in Germany. Eur Stroke J 2022; 2022(2): 166–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Winstein CJ, Stein J, Arena R, et al. Guidelines for adult stroke rehabilitation and recovery: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2016; 47(6): e98–e169. [DOI] [PubMed] [Google Scholar]
- 4. Paaske Johnsen S, Ingeman A, Hundborg HH, et al. The Danish stroke registry. Clin Epidemiol 2016; 8: 697–6702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ramos-Pachón A, García-Tornel Á, Millán M, et al. Bottlenecks in the acute stroke care system during the COVID-19 pandemic in Catalonia. Cerebrovasc Dis 2021; 50(5): 551–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pop R, Quenardelle V, Hasiu A, et al. Impact of the COVID-19 outbreak on acute stroke pathways: insights from the Alsace region in France. Eur J Neurol 2020; 27(9): 1783–1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kerleroux B, Fabacher T, Bricout N, et al. Mechanical thrombectomy for acute ischemic stroke amid the COVID-19 outbreak: decreased activity, and increased care delays. Stroke 2020; 51: 2012–2017. [DOI] [PubMed] [Google Scholar]
- 8. Norrving B, Barrick J, Davalos A, et al. Action plan for stroke in Europe 2018-2030. Eur Stroke J 2018; 3(4): 309–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wildenschild C, Mehnert F, Wernich Thomsen R, et al. Registration of acute stroke: validity in the Danish stroke registry and the Danish national registry of patients. Clin Epidemiol 2014; 6(1): 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kara P, Valentin JB, Mainz J, et al. Composite measures of quality of health care: evidence mapping of methodology and reporting. PLoS One 2022; 17(5): e0268320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Simonsen CZ, Blauenfeldt RA, Hedegaard JN, et al. COVID-19 did not result in increased hospitalization for stroke and transient ischemic attack: a nationwide study. Eur J Neurol 2022; 29(8): 2269–2274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vinding NE, Kristensen SL, Rørth R, et al. Ischemic stroke severity and mortality in patients with and without atrial fibrillation. J Am Heart Assoc 2022; 11(4): 22638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ritchie H, Mathieu E, Rodés-Guirao L, et al. Coronavirus pandemic (COVID-19), https://ourworldindata.org/coronavirus (2020, accessed 4 October 2022).
- 14. Nogueira RG, Abdalkader M, Qureshi MM, et al. Global impact of COVID-19 on stroke care. Int J Stroke 2021; 16(5): 573–584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhao J, Li H, Kung D, et al. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke 2020; 51: 1996–2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jasne AS, Chojecka P, Maran I, et al. Stroke code presentations, interventions, and outcomes before and during the COVID-19 pandemic. Stroke 2020; 51: 2664–2673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chamorro Á, Rudilosso S, Laredo C, et al. Experience at a comprehensive stroke center in Barcelona. Stroke 2020; 51(7): 1991–1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nguyen-Huynh MN, Xian M, Tang N, et al. Acute stroke presentation, care, and outcomes in community hospitals in Northern California during the COVID-19 pandemic. Stroke 2020; 51(7): 2224–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Meza HT, Lvaro A, Gil L, et al. Impact of COVID-19 outbreak on ischemic stroke admissions and in-hospital mortality in North-West Spain. Int J Stroke 2020; 15(7): 755–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Paolucci M, Biguzzi S, Cordici F, et al. Impact of COVID-19 pandemic on acute stroke care: facing an epidemiological paradox with a paradigm shift. Neurol Sci 2021; 42(2): 399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cadilhac DA, Kim J, Cloud G, et al. Effect of the coronavirus disease 2019 pandemic on the quality of stroke care in stroke units and alternative wards: a national comparative analysis. J Stroke 2022; 24(1): 79–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Crespy V, Benzenine E, Mariet AS, et al. Impact of the first COVID-19 pandemic peak and lockdown on the interventional management of carotid artery stenosis in France. J Vasc Surg 2022; 75(5): 1670–1678.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Douiri A, Muruet W, Bhalla A, et al. Stroke care in the United Kingdom during the COVID-19 pandemic. Stroke 2021; 52: 2125–2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Burns SP, Fleming TK, Webb SS, et al. Stroke recovery during the COVID-19 pandemic: a position paper on recommendations for rehabilitation. Arch Phys Med Rehabil 2022; 103(9): 1874–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Drenck N, Grundtvig J, Christensen T, et al. Stroke admissions and revascularization treatments in Denmark during COVID-19. Acta Neurol Scand 2022; 145(2): 160–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yarmol-Matusiak EA, Cipriano LE, Stranges S. A comparison of COVID-19 epidemiological indicators in Sweden, Norway, Denmark, and Finland. Scand J Public Health 2021; 49(1): 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. RKKP. Regionernes Kliniske Kvalitetsudviklingsprogram, https://www.sundhed.dk/content/cms/69/4669_dap_aarsrapport-2020_240621.pdf (2021, accessed 4 October 2022).
- 28. RKKP. Regionernes Kliniske Kvalitetsudviklingsprogram, https://www.sundhed.dk/content/cms/69/4669_dap_aarsrapport-2021_270622.pdf (2022, accessed 4 October 2022).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-eso-10.1177_23969873221139695 for Quality in stroke care during the early phases of the COVID-19 pandemic: A nationwide study by Rolf A Blauenfeldt, Jakob N Hedegaard, Christina Kruuse, David Gaist, Troels Wienecke, Boris Modrau, Dorte Damgaard, Søren P Johnsen, Grethe Andersen and Claus Z Simonsen in European Stroke Journal