Abstract
Objective
Examine time trends in suicidal ideation in post-secondary students over the first three waves of the COVID-19 pandemic in Canada and identify subpopulations of students with increased risk.
Method
We analysed 14 months of data collected through repeated cross-sectional deployment of the World Health Organization (WHO) World Mental Health-International College Student (WMH-ICS) survey at the University of British Columbia. Estimated log odds weekly trends of 30-day suicidal ideation (yes/no) were plotted against time with adjustments for demographics using binary logistic generalized additive model (GAM). Risk factors for 30-day suicidal ideation frequency (four categories) were examined using the ordered logistic GAM, with a cubic smoothing spline for modelling time trend in obervation weeks and accounting for demographics.
Results
Nearly one-fifth (18.9%) of students experienced suicidal ideation in the previous 30 days. While the estimated log odds suggested that binary suicidal ideation was relatively stable across the course of the pandemic, an initial drop followed by an increasing trend was observed. Risk factors for suicidal ideation frequency during the pandemic included identifying as Chinese or as another non-Indigenous ethnic minority; experiencing current symptoms of depression or anxiety; having a history of suicidal planning or attempts; and feeling overwhelmed but unable to get help as a result of COVID-19. Older age was identified as a protective factor.
Conclusions
The general university student population in our study was relatively resilient with respect to suicidal ideation during the first three waves of the pandemic, but trends indicate the possibility of delayed impact. Specific sub-populations were found to be at increased risk and should be considered for targeted support. Further analyses should be undertaken to continue monitoring suicidality trends throughout the remainder of the pandemic and beyond.
Keywords: suicidal ideation, pandemic, COVID-19, student, mental health
Abrégé
Objectif
Examiner les tendances temporelles de l’idéation suicidaire chez des étudiants de niveau post-secondaire durant les trois premières vagues de la pandémie de la COVID-19 au Canada et identifier les sous-populations d’étudiants ayant un risque accru.
Méthode
Nous avons analysé 14 mois de données recueillies par le déploiement transversal répété de l’initiative des étudiants du Collège international pour la santé mentale (WMH-ICS) dans le monde de l’OMS à l’Université de la Colombie-Britannique. Les estimations des tendances hebdomadaires des probabilités logarithmiques d’idéation suicidaire de 30 jours (oui/non) étaient représentées en fonction du temps avec ajustements pour les données démographiques utilisant un modèle additif généralisé (MAG) de logistique binaire. Les facteurs de risque pour la fréquence de l’idéation suicidaire sur 30 jours (quatre catégories) ont été examinés à l’aide du MAG de logistique imposée, avec une spline de lissage cubique pour modeler la tendance temporelle des semaines de réalisation et rendre compte des données démographiques.
Résultats
Près d’un cinquième (18,9 %) des étudiants ont éprouvé une idéation suicidaire dans les 30 jours précédents. Bien que les probabilités logarithmiques estimées aient suggéré que l’idéation suicidaire binaire soit relativement stable au cours de la pandémie, une baisse initiale suivie d’une tendance à la hausse a été observée. Les facteurs de risque de la fréquence de l’idéation suicidaire durant la pandémie comprenaient s’identifier comme Chinois ou une autre minorité ethnique non-autochtone; éprouver des symptômes actuels de dépression ou d’anxiété; avoir des antécédents de planification ou de tentatives de suicide; et se sentir accablé mais incapable d’obtenir de l’aide par suite de la COVID-19. L’âge avancé était identifié comme facteur de protection.
Conclusions
La population d’étudiants d’université générale de notre étude était relativement résiliente à l’égard de l’idéation suicidaire durant les trois premières vagues de la pandémie, mais les tendances indiquent la possibilité d’une incidence différée. Les sous-populations spécifiques ont été observées être à risque accru et devraient être considérées pour un soutien ciblé. D’autres analyses devraient être entreprises pour poursuivre la surveillance des tendances à la suicidabilité durant le reste et au-delà de la pandémie.
Introduction
University is a period of substantial life changes, which, for some, may enhance stress exposure. In addition to navigating new social and academic settings, many students are away from home for the first time and experiencing stress without their prior support network. Importantly, it is also well known that university students experience a high prevalence of mental disorders and suicidal thoughts and behaviours (STBs).1–3 Although only a small minority of university students attempt suicide, there is a critical need to identify risk factors that facilitate the transition from ideation to action. This is particularly important in the context of the COVID-19 pandemic, which has led to major societal disruptions. In the university setting, schools shifted to online learning, living situations changed rapidly, job and financial security were impacted, and important life events like graduation ceremonies were cancelled. The intersection of these experiences, among others, introduced elevated stress into students’ lives,4–6 potentially increasing suicide risk.
Numerous studies have reported the prevalence of STBs among university students. A 2018 meta-analysis reported 12-month prevalence of suicidal ideation, planning, and attempts in this population as 10.6%, 3.0%, and 1.2%, respectively. 3 In the context of the COVID-19 pandemic, reported prevalences of suicidal ideation among post-secondary students have ranged from 6.7% to 19.6%.7–11 Given that global rates of STBs vary considerably across countries, 12 these wide ranges are not unexpected. Moreover, there have been marked differences in the measures undertaken (e.g., strict lockdowns) by each country to manage COVID-19, which may contribute to this variability.
Several studies conducted early in the pandemic identified a range of potential risk factors for suicidal thoughts and behaviours in post-secondary students.7,9–13 These risk factors varied considerably across studies and countries in both the types of factors selected for analysis and the identified risk factors. This lack of consistency highlights the need for additional research to improve our understanding of suicidality during the pandemic and identify individuals who may be at higher risk of being severely impacted as the world continues to grapple with COVID-19. Specifically, in this article, we examined the contributions of demographic factors, previous and current mental health history, as well as ability to access resources during COVID-19 as potential risk factors for suicidal ideation in university students. A better understanding of these subpopulations and the ways in which they are impacted will become increasingly important in managing both short- and long-term mental health consequences of the pandemic.
Initial studies on trends in STBs during COVID-19 have largely focused on the early impacts of the pandemic, despite evolving case counts and levels of imposed restrictions as the pandemic progressed. The majority of these studies are based on general population samples, without a focus on post-secondary students. There have been several general studies that use British Columbia data, and they have either not found significant increases in suicide deaths, or found reduced rates of suicide deaths in the province during the early months of the COVID-19 pandemic.14–16 One study which examined trends in suicide deaths over time showed conflicting results across different waves of the pandemic, highlighting the importance of continuing to monitor suicidality as the pandemic progresses. 17 While these data on suicide fatalities provide some indication of the impact of COVID-19, they do not necessarily generalize to all aspects of STB. Further study of suicidal ideation, especially across a longer time course, is needed to provide a more nuanced understanding of the situation and the long-term mental health impacts, particularly in the post-secondary student population. In an effort to fill these gaps, we analysed time trends in suicidal ideation in Canadian university students over approximately 14 months of the COVID-19 pandemic and identified subpopulations of students with increased risk.
Methods
Study Design
This study used data collected through repeated cross-sectional deployment of the World Health Organization (WHO) World Mental Health-International College Student (WMH-ICS) survey. It is a self-administered online survey based on the WHO World Mental Health-Composite International Diagnostic Interview (WHO WMH-CIDI). 18 The WMH-ICS initiative has been developed to help coordinate epidemiological research among university students worldwide.2,18–25 It uses validated screenings to generate estimates for a wide range of mental disorders (such as current, i.e., 30 days, and lifetime major depressive episodes [MDE] and anxiety disorders), and includes questions that probe symptom severity, help-seeking behaviours, and treatment barriers. 25
The survey was originally implemented to capture variations in symptoms in response to foreseeable and unforeseeable stressors throughout the year, such as examinations, graduation, and world events. As the COVID-19 pandemic emerged as an exposure of interest in the first week of March 2020, questions were included to assess weekly variations in the impact of COVID-19 on students (e.g., testing positive for COVID -19 or knowing someone who did). During the last week of March 2020, an additional question was included inquiring whether respondents felt emotionally affected or overwhelmed by the pandemic, and whether they had been able to access help.
Unlike typical surveys of university students, in collaboration with university registrars, this survey was administered to stratified random weekly samples of students (rather than, e.g., a snowball or other arbitrary sampling frame).
Outcome Measure
Our outcome measure was derived from the WHO WMH-CIDI screening question assessing 30-day suicidal ideation. Students were asked how often they had experienced suicidal ideation in the previous 30 days, which provided the following Likert-type response options: “all or almost all of the time,” “most of the time,” “some of the time,” “a little of the time,” and “none of the time.” The two response categories “all or almost all of the time” and “most of the time” were grouped together to “most of the time or all or almost all of the time” due to small cell counts, forming four ordered categories of suicidal ideation frequency for analysis. Although this grouping resulted in some loss of information, we feel that the two combined categories are very similar in terms of symptomatology.
Survey Procedure
This study utilized 59 weeks of data from 29 March 2020 to 22 May 2021, a period that encompassed three waves of the COVID-19 pandemic in Canada. Each week, the survey was sent to a new group of 350 students generated via stratified random sampling (by gender, age, degree type and year, and international student status) from currently enrolled students at the University of British Columbia (UBC), Vancouver (student population of approximately 55,000). Weekly recruitment of the initial 350 students occurred via email, and a subset of non-responders were followed-up with via phone calls and personal emails every week to minimize non-responder bias as per a specified protocol described in a previous paper. 24 The survey's adjusted response rate was 43.04% using the American Association for Public Opinion research weighted response rate 1 (RR1w) calculation for two-phase sample designs, which incorporates the initial survey response rate (27.9%) in addition to the second stage follow-up response rate for initial non-responders (24.4% for those with phone numbers on file, and 5.4% for those without phone numbers on file). 28 Further detail on the survey methodology has been published in a protocol paper in JMIR Research Protocols. 24
Ethics
The authors assert that all procedures contributing to this work complied with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human subjects were approved by the Behavioural Research Ethics Board of the University of British Columbia (H19-02538). Participants indicated their consent prior to completing the survey by reading through a consent letter and selecting a box to indicate their agreement.
Statistical Analysis
We first examined the weekly trends of the odds of having suicidal ideation (Yes/No) using the ordered binary logistic generalized additive model (GAM), with a cubic smoothing spline for modelling time trend in observation weeks and accounting for demographics (age, gender, ethnicity, student type, and international student status). The binary outcome in this GAM model was created by collapsing the four ordered categories of suicidal ideation into Yes (“all or almost all of the time,” “most of the time,” “some of the time,” and “a little of the time”) and No (“none of the time”).
In the main analysis, since the outcome was ordered, we used the GAM to perform an ordered logistic regression to analyse the original suicidal ideation outcome with four ordinal levels. More specifically, this GAM was used to examine the associations between the ordered 30-day suicidal ideation frequency variable and independent variables of interest with a nonparametric effect of survey observation week using a cubic spline.
Independent variables included as covariates in the multivariable analysis were gender, age, ethnicity, degree type and year, international student status, housing situation, type of survey communication participant responded to, survey observation week, current depression, lifetime depression, current anxiety, lifetime anxiety, lifetime suicide plan, lifetime suicide attempt, knowing someone in Vancouver who tested positive for COVID-19, and impact of the COVID-19 pandemic on emotional wellbeing. Variables involving conditions such as depression and anxiety were based on screening questions. Listwise deletion was performed so that only surveys with complete data on all variables of interest were included in the final analysis. The GAM models were conducted using R (www.r-project.org) with the mgcv package. 26
Results
This study is based on data from 4,693 respondents. The sample of respondents was primarily female (63.05%) and relatively ethnically diverse (37.55% white, 3.05% First Nations, Inuit, or Métis, 27.45% Chinese, 31.96% Non-Indigenous or Chinese visible minority). A comparison of the sample characteristics (based on stratifying variables) with those of the general student population can be found in Appendix Table 3; females and other genders, domestic students, and graduate students were overrepresented in our sample compared to the general student body.
Time Trend in Binary 30-day Suicidal Ideation (N = 4,693)
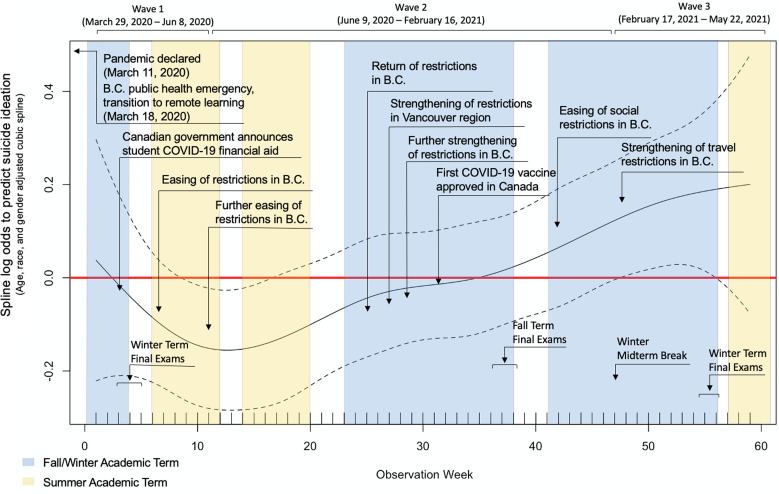
Almost one-fifth (18.9%) of students who responded to the survey experienced suicidal ideation in the previous 30 days. The weekly trend estimated log odds of 30-day suicidal ideation (yes/no) adjusted for sociodemographic variables (age, gender, and ethnicity) and survey-related variables (type of survey responded to, year of study, and whether international or not) is presented in Figure 1. The X-axis is the study observation week while the Y-axis is the estimated log odds of the contribution (effect) of spline observation week to suicidal ideation, centred on 0. If the 95% confidence intervals overlap with the zero line (dotted lines enclose the solid horizontal line) for certain values of the observation week (or throughout the entire range), this would imply a non-significant effect at those observation weeks values. From Figure 1, we observe that although, generally, a non-significant effect is observed (relatively stable) across the course of the pandemic, there is a gradual decrease in suicidal ideation from week 1, and a significant effect is observed between some range of observation weeks. The significant effects are observed around weeks 9–17 (24 May–25 July 2020) where the log odds and associated 95% confidence intervals drop below zero, and then rise above zero between weeks 48 and 56 (21 February–24 April 2021). Crude weekly suicidal ideation rates with a 4-week moving average can be found in Appendix Figure 1.
Figure 1.
Predicted weekly trend in 30-day suicidal ideation (yes/no) with adjustments for age, ethnicity, and gender (29 March 2020–22 May 2021).
Identification of Subpopulations with Increased Risk of Suicidal Ideation (N = 4,693)
Characteristics of the study sample by ordered categories of previous 30-day suicidal ideation frequency can be found in Table 1. A more detailed version is available in Appendix Table 1. Significant differences were found across groups defined by socio-demographics (gender, age, ethnicity, type of student, type of housing, and type of survey responder), mental health (lifetime history of depression without past 30-day depression, any current symptoms of depression, lifetime history of anxiety without past 30-day anxiety, any current symptoms of anxiety, lifetime history of suicide planning, and lifetime history of suicide attempts) and reported impact of COVID-19 on emotional wellbeing.
Table 1.
Suicidal Ideation Frequency by Sample Characteristics (N = 4,693)a.
| Characteristic | Overall Total n (% of total sample) | 30-day frequency of suicidal ideation | |||
|---|---|---|---|---|---|
| None (n = 3,807) n (row %) | A little of the time (n = 507) n (row %) | Some of the time (n = 264) n (row %) | Most of the time or all or almost all of the time (n = 115) n (row %) | ||
| Gender | *** | *** | *** | *** | |
| Male | 1,628 (34.69) | 1,385 (85.07) | 145 (8.91) | 68 (4.18) | 30 (1.84) |
| Female | 2,959 (63.05) | 2,356 (79.62) | 341 (11.52) | 182 (6.15) | 80 (2.70) |
| Otherb | 106 (2.26) | 66 (62.26) | 21 (19.81) | 14 (13.21) | 5 (4.72) |
| Age | *** | *** | *** | *** | |
| 18 or younger | 502 (10.70) | 385 (76.69) | 55 (10.96) | 37 (7.37) | 25 (4.98) |
| 19 | 609 (12.98) | 468 (76.85) | 71 (11.66) | 46 (7.55) | 24 (3.94) |
| 20 | 563 (12.00) | 447 (79.40) | 70 (12.43) | 37 (6.57) | 9 (1.60) |
| 21 | 493 (10.51) | 383 (77.69) | 62 (12.58) | 34 (6.90) | 14 (2.84) |
| 22 | 410 (8.74) | 333 (81.22) | 43 (10.49) | 27 (6.59) | 7 (1.71) |
| 23 | 298 (6.35) | 246 (82.55) | 31 (10.40) | 14 (4.70) | 7 (2.35) |
| 24 | 251 (5.35) | 197 (78.49) | 29 (11.55) | 21 (8.37) | 4 (1.59) |
| 25 or older | 1,567 (33.39) | 1,348 (86.02) | 146 (9.32) | 48 (3.06) | 25 (1.60) |
| Type of communication participant responded to | ** | ** | ** | ** | |
| Initial survey | 3,821 (81.42) | 3,056 (79.98) | 440 (11.52) | 225 (5.89) | 100 (2.62) |
| Hard to reach with phone | 750 (15.98) | 645 (86.00) | 58 (7.73) | 34 (4.53) | 13 (1.73) |
| Hard to reach without phone | 122 (2.60) | 106 (86.89) | 9 (7.38) | 5 (4.10) | 2 (1.64) |
| Lifetime depression without 30-day depression? | *** | *** | *** | *** | |
| No | 4,073 (86.79) | 3,210 (78.81) | 488 (11.98) | 260 (6.38) | 115 (2.82) |
| Yes | 620 (13.21) | 597 (96.29) | 19 (3.06) | 4 (0.65) | 0 (0.00) |
| Any current depression? | *** | *** | *** | *** | |
| No | 1,704 (36.31) | 1,659 (97.36) | 39 (2.29) | 5 (0.29) | 1 (0.06) |
| Yes | 2,989 (63.69) | 2,148 (71.86) | 468 (15.66) | 259 (8.67) | 114 (3.81) |
| Lifetime anxiety without any 30-day anxiety? | *** | *** | *** | *** | |
| No | 3,918 (83.49) | 3,078 (78.56) | 471 (12.02) | 256 (6.53) | 113 (2.88) |
| Yes | 775 (16.51) | 729 (94.06) | 36 (4.65) | 8 (1.03) | 2 (0.26) |
| Any current anxiety? | *** | *** | *** | *** | |
| No | 1,432 (30.51) | 1,360 (94.97) | 57 (3.98) | 10 (0.70) | 5 (0.35) |
| Yes | 3,261 (69.49) | 2,447 (75.04) | 450 (13.80) | 254 (7.79) | 110 (3.37) |
| Had the COVID-19 pandemic affect their emotional wellbeing? | *** | *** | *** | *** | |
| No | 729 (15.53) | 655 (89.85) | 45 (6.17) | 19 (2.61) | 10 (1.37) |
| Yes, but they were able to manage it | 2,375 (50.61) | 2,043 (86.02) | 217 (9.14) | 87 (3.66) | 28 (1.18) |
| Yes, they are overwhelmed and couldn't/can't find help | 594 (12.66) | 335 (56.40) | 110 (18.52) | 97 (16.33) | 52 (8.75) |
| Yes, they are overwhelmed but were/are able to get help | 995 (21.20) | 774 (77.79) | 135 (13.57) | 61 (6.13) | 25 (2.51) |
| Type of student | *** | *** | *** | *** | |
| 1st year undergraduate | 670 (14.28) | 518 (77.31) | 77 (11.49) | 44 (6.57) | 31 (4.63) |
| 2nd year undergraduate | 709 (15.11) | 554 (78.14) | 79 (11.14) | 53 (7.48) | 23 (3.24) |
| 3rd year undergraduate | 820 (17.47) | 644 (78.54) | 105 (12.80) | 56 (6.83) | 15 (1.83) |
| 4th year undergraduate | 655 (13.96) | 523 (79.85) | 78 (11.91) | 38 (5.80) | 16 (2.44) |
| Graduate | 1,284 (27.36) | 1,098 (85.51) | 112 (8.72) | 51 (3.97) | 23 (1.79) |
| Other | 555 (11.83) | 470 (84.68) | 56 (10.09) | 22 (3.96) | 7 (1.26) |
| Ethnicity | * | * | * | * | |
| White | 1,762 (37.55) | 1,482 (84.11) | 166 (9.42) | 79 (4.48) | 35 (1.99) |
| First Nations, Inuit or Métis | 143 (3.05) | 115 (80.42) | 20 (13.99) | 6 (4.20) | 2 (1.40) |
| Chinese | 1,288 (27.45) | 1,022 (79.35) | 152 (11.80) | 79 (6.13) | 35 (2.72) |
| Non-Indigenous or Chinese Visible Minority | 1,500 (31.96) | 1,188 (79.20) | 169 (11.27) | 100 (6.67) | 43 (2.87) |
| Housing type | ** | ** | ** | ** | |
| With parents or other relatives | 1,899 (40.46) | 1,499 (78.94) | 217 (11.43) | 128 (6.74) | 55 (2.90) |
| In their own home or apartment (owned or rented) | 1,320 (28.13) | 1,124 (85.15) | 119 (9.02) | 54 (4.09) | 23 (1.74) |
| In a university owned or operated residence or fraternity | 680 (14.49) | 542 (79.71) | 77 (11.32) | 44 (6.47) | 17 (2.50) |
| In a shared house, apartment or flat | 727 (15.49) | 584 (80.33) | 91 (12.52) | 35 (4.81) | 17 (2.34) |
| Other | 67 (1.43) | 58 (86.57) | 3 (4.48) | 3 (4.48) | 3 (4.48) |
| Lifetime suicide plan? | *** | *** | *** | *** | |
| No | 3,611 (76.94) | 3,214 (89.01) | 264 (7.31) | 101 (2.80) | 32 (0.89) |
| Yes | 1,082 (23.06) | 593 (54.81) | 243 (22.46) | 163 (15.06) | 83 (7.67) |
| Lifetime suicide attempt? | *** | *** | *** | *** | |
| No | 4,412 (94.01) | 3,673 (83.25) | 443 (10.04) | 217 (4.92) | 79 (1.79) |
| Yes | 281 (5.99) | 134 (47.69) | 64 (22.78) | 47 (16.73) | 36 (12.81) |
*p ≤ 0.05; **p ≤ 0.01; ***p ≤ 0.001; Both Chi-squared and Fisher's exact tests were used where the cell counts are small. These are testing for an overall association.
aOnly significant results are shown, see complete table in Appendix.
b“Other” gender is defined as a gender identity different than sex at birth. While there are many subgroups within this, they have been collapsed for the purpose of this analysis due to small cell counts.
The results of the unadjusted and fully adjusted GAMs examining the association between predictors and ordered categories of 30-day suicidal ideation frequency are presented in Table 2. A more detailed version is available as Appendix Table 2. Being older appeared to be a protective factor, with those aged 20 (OR = 0.59, 95% CI = 0.32–0.86), 23 (OR = 0.55, 95% CI = 0.24–0.85), and 25 or older (OR = 0.51, 95% CI = 0.25–0.77) having lower ideation frequency compared to those aged 18 or younger. Those who reported being Chinese or another ethnic minority (excluding First Nations, Inuit, or Métis) had greater suicidal ideation frequency compared to White respondents (OR = 1.46, 95% CI = 1.13–1.79 and OR = 1.31, 95% CI = 1.03–1.59 respectively). Additional risk factors associated with significantly increased levels of suicidal ideation frequency included current symptoms of depression (OR = 7.26, 95% CI = 3.84–10.68), current symptoms of anxiety (OR = 2.28, 95% CI = 1.24–3.32), history of a suicide plan (OR = 4.82, 95% CI = 3.94–5.70) or attempt (OR = 1.70, 95% CI = 1.23–2.17), and feeling overwhelmed and unable to get help as a result of the COVID-19 pandemic (OR = 2.02, 95% CI = 1.34–2.71).
Table 2.
Suicidal Ideation Frequency GAM Ordered Regression (N = 4,693)a.
| Predictor | Unadjusted GAM cubic splinesb | Adjusted GAM cubic splinesb |
|---|---|---|
| Odds Ratio (95% CI) | Odds Ratio (95% CI) | |
| Gender | ||
| Male | Reference | Reference |
| Female | 1.46 (1.22–1.70) *** | 0.97 (0.79–1.16) |
| Otherc | 3.35 (1.97–4.73) *** | 1.23 (0.65–1.81) |
| Age | ||
| 18 or younger | Reference | Reference |
| 19 | 0.99 (0.71–1.27) | 0.78 (0.49–1.07) |
| 20 | 0.83 (0.58–1.07) | 0.59 (0.32–0.86) * |
| 21 | 0.93 (0.65–1.21) | 0.67 (0.33–1.00) |
| 22 | 0.75 (0.51–1.00) | 0.63 (0.29–0.97) |
| 23 | 0.68 (0.43–0.93) * | 0.55 (0.24–0.85) * |
| 24 | 0.89 (0.56–1.22) | 0.82 (0.34–1.29) |
| 25 or older | 0.51 (0.38–0.64) *** | 0.51 (0.25–0.77) ** |
| Type of communication participant responded to | ||
| Initial survey | Reference | Reference |
| Hard to reach with phone | 0.66 (0.51–0.81) *** | 0.79 (0.59–0.98) |
| Hard to reach without phone | 0.60 (0.27–0.92) | 0.75 (0.30–1.20) |
| Lifetime depression without 30-day depression? | ||
| No | Reference | Reference |
| Yes | 0.14 (0.08–0.20) *** | 1.03 (0.38–1.68) |
| Any current depression? | ||
| No | Reference | Reference |
| Yes | 14.56 (10.01–19.11) *** | 7.26 (3.84–10.68) *** |
| Lifetime anxiety without any 30-day anxiety? | ||
| No | Reference | Reference |
| Yes | 0.23 (0.16–0.30) *** | 1.01 (0.46–1.57) |
| Any current anxiety? | ||
| No | Reference | Reference |
| Yes | 6.38 (4.75–8.01) *** | 2.28 (1.24–3.32) *** |
| Had the COVID-19 pandemic affect their emotional wellbeing? | ||
| No | Reference | Reference |
| Yes, but they were able to manage it | 1.41 (1.03–1.80) ** | 0.78 (0.12) |
| Yes, they are overwhelmed and couldn't/can't find help | 7.18 (5.07–9.29) *** | 2.02 (1.34–2.71) *** |
| Yes, they are overwhelmed but were/are able to get help | 2.48 (1.76–3.19)*** | 0.86 (0.57–1.15) |
| Type of student | ||
| 1st year undergraduate | Reference | Reference |
| 2nd year undergraduate | 0.98 (0.73–1.23) | 1.23 (0.79–1.66) |
| 3rd year undergraduate | 0.93 (0.70–1.16) | 1.32 (0.76–1.89) |
| 4th year undergraduate | 0.87 (0.64–1.11) | 1.31 (0.68–1.94) |
| Graduate | 0.58 (0.44–0.72) *** | 1.34 (0.68–1.99) |
| Other | 0.61 (0.43–0.79) ** | 1.26 (0.61–1.91) |
| Ethnicity | ||
| White | Reference | Reference |
| First Nations, Inuit or Métis | 1.23 (0.69–1.77) | 0.82 (0.41–1.22) |
| Chinese | 1.39 (1.13–1.65) ** | 1.46 (1.13–1.79) *** |
| Non-Indigenous or Chinese Visible Minority | 1.40 (1.15–1.66) *** | 1.31 (1.03–1.59) ** |
| Housing type | ||
| With parents or other relatives | Reference | Reference |
| In their own home or apartment (owned or rented) | 0.66 (0.53–0.78) *** | 0.87 (0.65–1.10) |
| In a university owned or operated residence or fraternity | 1.00 (0.77–1.22) | 1.03 (0.76–1.31) |
| In a shared house, apartment or flat | 0.92 (0.72–1.12) | 0.96 (0.70–1.22) |
| Other | 0.61 (0.17–1.05) | 0.62 (0.11–1.14) |
| Lifetime suicide plan? | ||
| No | Reference | Reference |
| Yes | 6.91 (5.82–8.00) *** | 4.82 (3.94–5.69) *** |
| Lifetime suicide attempt? | ||
| No | Reference | Reference |
| Yes | 5.72 (4.36–7.08) *** | 1.70 (1.23–2.17)*** |
*p ≤ 0.05; **p ≤ 0.01; ***p ≤ 0.001.
aOnly significant results are shown, see complete table in Appendix Table 2.
bEach unadjusted model contains only the variable of interest. The adjusted model contains all variables in a single model.
c"Other” gender is defined as a gender identity different than sex at birth. While there are many subgroups within this, they have been collapsed for the purpose of this analysis due to small cell counts.
Discussion
The disruptive nature of the COVID-19 pandemic has brought considerable attention to the topic of mental health. The university student population has been of particular concern, and many have wondered if the upheaval of student academic and social life would have detrimental impacts on the wellbeing of this population, resulting in increased levels of suicidal thoughts and behaviours. 27 Two findings from this study stood out. First, while suicidal ideation was relatively consistent across the study period, it was significantly decreased during observation weeks 9–17 (24 May–25 July 2020) and significantly elevated during observation weeks 48–56 (21 February–24 April 2021). Second, risk factors for suicidal ideation frequency during the pandemic included identifying as Chinese or as another ethnic minority (excluding First Nations, Inuit, or Métis); experiencing current symptoms of depression or anxiety; having a history of suicidal planning or attempts; and feeling overwhelmed but unable to get help as a result of COVID-19.
Based on our findings, the university student population appeared to be relatively resilient in the face of the pandemic, particularly during its early phases. Through our time trend analysis, we did not see prompt increases in suicidal ideation as one may anticipate. Instead, our analysis revealed relatively high initial levels which trended downwards until week 13, 21–27 June 2020 (15 weeks after the declaration of COVID-19 as a pandemic) before gradually increasing to a significant level during the period of 21 February–24 April 2021. Such initial declines in STBs have previously been referred to as the “honeymoon” effect in the literature, where an initial drop in rates is often followed by a delayed increase after community disasters. 29 In the context of COVID-19, this has been reported in a Japanese study looking at suicide rates following the pandemic, which postulated that the added support of government subsidies and reduction in commuting time and working hours may have driven this initial “honeymoon phase.” 17 These hypotheses are also plausible in the context of university students as Canadian universities transitioned to online learning and employed a variety of measures to increase support for students such as giving “pass-fail” options for grades and providing additional mental health support. Another potential explanation for this “honeymoon phase” is the sense of cohesion that resulted from the shared experience of the COVID-19 pandemic. 30
Examining the two significant periods in greater detail, the reduction in 30-day suicidal ideation (24 May–25 July 2020) encompassed a time period of summer weather in Vancouver, the summer academic term, and the easing of local COVID-19 restrictions following the first wave of cases. The significant elevation (21 February–24 April 2021) encompassed a time period of midterm and final exams, the emerging spring season, and the initial half of the third wave of the pandemic. Unfortunately, there is limited information on typical time-based variation in suicidal ideation amongst the university student population, and without these historical data it was challenging to determine if the pandemic's influence was confounded by seasonal and academic effects. It is also worth noting that at this time, there was substantial variation in the availability of vaccines, especially for young adults, who were identified as a low-priority population for vaccination. This lack of immediate access to a vaccine may have been an additional stressor.
Examining suicidal ideation frequency, certain sub-populations were at increased risk during this time period. Similar to previous studies on STB,31,32 we found that individuals with other mental health problems were at increased risk. Specifically, previous 30-day anxiety and depression, and history of previous suicide plan or attempt were all associated with an increased risk of suicidal ideation frequency. In terms of ethnicity, identifying as Chinese was associated with an increased risk of more frequent suicidal ideation. Other ethnic minority groups were also found to be at increased risk, though to a lesser degree. This is in line with a recent study on US college students which found increased odds of suicidal ideation in racial minority groups, particularly amongst Asian students, 33 which may have been compounded by the increasing reports of xenophobia directed towards Chinese populations during the pandemic.34,35
To try and more directly measure the effects of COVID-19, we specifically asked students if the pandemic had affected their emotional wellbeing. Interestingly, respondents who felt emotionally affected and even overwhelmed by COVID-19 did not experience higher suicidal ideation if they were able to manage or find help. This indicates that being overwhelmed by the pandemic itself does not increase an individual's suicidality, but lacking the resources or support to cope with it does. Although many Canadian universities tried to make academic accommodations for students and provide additional support, there was evidently a sub-population of students who were not able to access these services. This should be an important consideration for universities in planning their response to future disasters that may occur.
While our data do not allow us to directly isolate the impact of the COVID-19 pandemic, many of our findings make sense in the context of a global pandemic. Even though COVID-19 itself may not pose a large health-related threat to most students, there are many additional potential stressors which have been introduced as a result, such as academic-related concerns, general uncertainty about the pandemic, social isolation, experiences of discrimination, and mental health challenges.34–36 As the long-term impacts of the pandemic unfold, a better understanding of how high-risk students are affected will be important for managing the ongoing response by universities. These risk factors can be used to develop better screening tools, allowing for prevention and earlier intervention, especially amongst the subpopulation of individuals who were overwhelmed by the pandemic but not able to find help within the existing systems. This is particularly important given that, among respondents with suicidal ideation, 43.6% were overwhelmed and unable to get help, while only 22.2% were overwhelmed and able to get help. Given the large gap in access to mental health services for people in need, there has been a push in recent years to develop e-mental health tools which allow for increased capacity.37–39
Several strengths and limitations must also be considered in the context of this article. The weekly deployment of the survey allowed for a thorough picture of student mental health to be built throughout the first three waves of the COVID-19 pandemic. Furthermore, a robust stratified sampling strategy that included outreach to initial non-responders not only provided a representative outlook on the student population, but also allowed for an adjusted response rate higher than in most university surveys. 40 However, despite these strengths, the deployment date of our survey did limit the ability to draw conclusions regarding pre-COVID data and make direct comparisons between pre- and post-COVID-19 risk factors. In addition, our data may have been susceptible to response bias. As shown in Appendix Table 4, several sub-populations were found to differ in their likelihood of being excluded from our models due to missing data. Students aged 25 or older, graduate students, and white students were less likely to be excluded from the models, whereas students in the “other” student type category and non-Indigenous or Chinese visible minority students were more likely to be excluded from the models. It is also important to note that our outcomes could be inflated given that individuals with mental health concerns may respond to surveys with an increased rate and females are often overrepresented within this subpopulation. Despite these limitations, our sample was relatively representative of the overall student population at the University of British Columbia (see Appendix Table 3). With that said, this study was focused on this one university located in Vancouver, British Columbia, which is an important caveat when generalizing these findings to broader populations. Furthermore, while we used the increase in the frequency of suicidal thoughts as our outcome, this measure is limited in its ability to describe whether this ideation is connected to suicidal plans or intentions to act on those plans, and future research is needed to better examine this relationship.
In conclusion, our results have found that the general university student population in our study was relatively resilient with respect to suicidal ideation in the face of a global pandemic, but trends indicate the possibility of delayed impact, and certain subpopulations remain more vulnerable. Information on identified at-risk groups can offer important insight to policy and decision-makers within universities. In light of the associations found of increased suicidal ideation frequency with current symptoms of depression or anxiety, previous history of suicidal planning or attempts, identifying as Chinese or another ethnic minority (excluding First Nations or Métis), and amongst individuals who felt overwhelmed but were unable to get help as a result of COVID-19, university administrators should consider targeted interventions for at risk groups, especially during times of the year where students may be most vulnerable. Additional analyses should focus on post-pandemic suicidal ideation to further study delayed responses and establish typical annual variation amongst this population.
Acknowledgements
Thank you to Carolina Judkowicz and Gurpreet Chopra for their contributions to survey administration.
Appendix
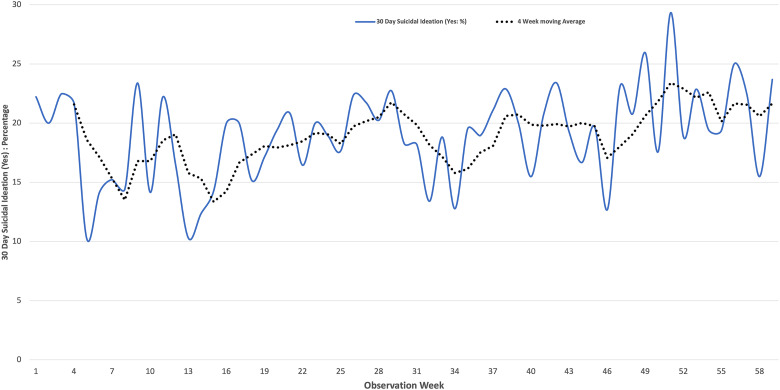
Appendix Figure 1.
Crude weekly suicidal ideation rates with a 4-week moving average.
Appendix Table 1.
Suicidal Ideation Frequency by Sample Characteristics – All Variables (N = 4,693).
| Characteristic | 30-day frequency of suicidal ideation | |||
|---|---|---|---|---|
| None (n = 3,807) n (row %) | A little of the time (n = 507) n (row %) | Some of the time (n = 264) n (row %) | Most of the time or all or almost all of the time (n = 115) n (row %) | |
| Gender | *** | *** | *** | *** |
| Male | 1,385 (85.07) | 145 (8.91) | 68 (4.18) | 30 (1.84) |
| Female | 2,356 (79.62) | 341 (11.52) | 182 (6.15) | 80 (2.70) |
| Othera | 66 (62.26) | 21 (19.81) | 14 (13.21) | 5 (4.72) |
| Age | *** | *** | *** | *** |
| 18 or younger | 385 (76.69) | 55 (10.96) | 37 (7.37) | 25 (4.98) |
| 19 | 468 (76.85) | 71 (11.66) | 46 (7.55) | 24 (3.94) |
| 20 | 447 (79.40) | 70 (12.43) | 37 (6.57) | 9 (1.60) |
| 21 | 383 (77.69) | 62 (12.58) | 34 (6.90) | 14 (2.84) |
| 22 | 333 (81.22) | 43 (10.49) | 27 (6.59) | 7 (1.71) |
| 23 | 246 (82.55) | 31 (10.40) | 14 (4.70) | 7 (2.35) |
| 24 | 197 (78.49) | 29 (11.55) | 21 (8.37) | 4 (1.59) |
| 25 or older | 1,348 (86.02) | 146 (9.32) | 48 (3.06) | 25 (1.60) |
| Type of communication participant responded to | ** | ** | ** | ** |
| Initial survey | 3,056 (79.98) | 440 (11.52) | 225 (5.89) | 100 (2.62) |
| Hard to reach with phone | 645 (86.00) | 58 (7.73) | 34 (4.53) | 13 (1.73) |
| Hard to reach without phone | 106 (86.89) | 9 (7.38) | 5 (4.10) | 2 (1.64) |
| Lifetime depression without 30-day depression? | *** | *** | *** | *** |
| No | 3,210 (78.81) | 488 (11.98) | 260 (6.38) | 115 (2.82) |
| Yes | 597 (96.29) | 19 (3.06) | 4 (0.65) | 0 (0.00) |
| Any current depression? | *** | *** | *** | *** |
| No | 1,659 (97.36) | 39 (2.29) | 5 (0.29) | 1 (0.06) |
| Yes | 2,148 (71.86) | 468 (15.66) | 259 (8.67) | 114 (3.81) |
| Lifetime anxiety without any 30-day anxiety? | *** | *** | *** | *** |
| No | 3,078 (78.56) | 471 (12.02) | 256 (6.53) | 113 (2.88) |
| Yes | 729 (94.06) | 36 (4.65) | 8 (1.03) | 2 (0.26) |
| Any current anxiety? | *** | *** | *** | |
| No | 1,360 (94.97) | 57 (3.98) | 5 (0.35) | |
| Yes | 2,447 (75.04) | 450 (13.80) | 110 (3.37) | |
| Knows someone in Vancouver who tested positive for COVID-19? | ||||
| No | 2,795 (80.99) | 375 (10.87) | 199 (5.77) | 82 (2.38) |
| Yes | 1,012 (81.48) | 132 (10.63) | 65 (5.23) | 33 (2.66) |
| Had the COVID-19 pandemic affect their emotional wellbeing? | *** | *** | *** | *** |
| No | 655 (89.85) | 45 (6.17) | 19 (2.61) | 10 (1.37) |
| Yes, but they were able to manage it | 2,043 (86.02) | 217 (9.14) | 87 (3.66) | 28 (1.18) |
| Yes, they are overwhelmed and couldn't/can't find help | 335 (56.40) | 110 (18.52) | 97 (16.33) | 52 (8.75) |
| Yes, they are overwhelmed but were/are able to get help | 774 (77.79) | 135 (13.57) | 61 (6.13) | 25 (2.51) |
| Type of student | *** | *** | *** | *** |
| 1st year undergraduate | 518 (77.31) | 77 (11.49) | 44 (6.57) | 31 (4.63) |
| 2nd year undergraduate | 554 (78.14) | 79 (11.14) | 53 (7.48) | 23 (3.24) |
| 3rd year undergraduate | 644 (78.54) | 105 (12.80) | 56 (6.83) | 15 (1.83) |
| 4th year undergraduate | 523 (79.85) | 78 (11.91) | 38 (5.80) | 16 (2.44) |
| Graduate | 1,098 (85.51) | 112 (8.72) | 51 (3.97) | 23 (1.79) |
| Other | 470 (84.68) | 56 (10.09) | 22 (3.96) | 7 (1.26) |
| Ethnicity | * | * | * | * |
| White | 1,482 (84.11) | 166 (9.42) | 79 (4.48) | 35 (1.99) |
| First Nations, Inuit or Métis | 115 (80.42) | 20 (13.99) | 6 (4.20) | 2 (1.40) |
| Chinese | 1,022 (79.35) | 152 (11.80) | 79 (6.13) | 35 (2.72) |
| Non-Indigenous or Chinese Visible Minority | 1,188 (79.20) | 169 (11.27) | 100 (6.67) | 43 (2.87) |
| International student? | ||||
| No | 2,999 (81.01) | 402 (10.86) | 207 (5.59) | 94 (2.54) |
| Yes | 808 (81.53) | 105 (10.60) | 57 (5.75) | 21 (2.12) |
| Housing type | ** | ** | ** | ** |
| With parents or other relatives | 1,499 (78.94) | 217 (11.43) | 128 (6.74) | 55 (2.90) |
| In their own home or apartment (owned or rented) | 1,124 (85.15) | 119 (9.02) | 54 (4.09) | 23 (1.74) |
| In a university owned or operated residence or fraternity | 542 (79.71) | 77 (11.32) | 44 (6.47) | 17 (2.50) |
| In a shared house, apartment or flat | 584 (80.33) | 91 (12.52) | 35 (4.81) | 17 (2.34) |
| Other | 58 (86.57) | 3 (4.48) | 3 (4.48) | 3 (4.48) |
| Lifetime suicide plan? | *** | *** | *** | *** |
| No | 3,214 (89.01) | 264 (7.31) | 101 (2.80) | 32 (0.89) |
| Yes | 593 (54.81) | 243 (22.46) | 163 (15.06) | 83 (7.67) |
| Lifetime suicide attempt? | *** | *** | *** | *** |
| No | 3,673 (83.25) | 443 (10.04) | 217 (4.92) | 79 (1.79) |
| Yes | 134 (47.69) | 64 (22.78) | 47 (16.73) | 36 (12.81) |
*p ≤ 0.05; **p ≤ 0.01; ***p ≤ 0.001; Both Chi-squared and Fisher's exact tests were used where the cell counts are small. These are testing for an overall association.
a“Other” gender is defined as a gender identity different than sex at birth. While there are many subgroups within this, they have been collapsed for the purpose of this analysis due to small cell counts.
Appendix Table 2.
Suicidal Ideation Frequency GAM Ordered Regression – All Variables (N = 4,693).
| Predictor | Unadjusted GAM cubic splinesa | Adjusted GAM cubic splinesa |
|---|---|---|
| Odds ratio (robust SE) | Odds ratio (robust SE) | |
| Gender | ||
| Male | Reference | Reference |
| Female | 1.46 (1.22–1.70) *** | 0.97 (0.79–1.16) |
| Otherb | 3.35 (1.97–4.73) *** | 1.23 (0.65–1.81) |
| Age | ||
| 18 or younger | Reference | Reference |
| 19 | 0.99 (0.71–1.27) | 0.78 (0.49–1.07) |
| 20 | 0.83 (0.58–1.07) | 0.59 (0.32–0.86) * |
| 21 | 0.93 (0.65–1.21) | 0.67 (0.33–1.00) |
| 22 | 0.75 (0.51–1.00) | 0.63 (0.29–0.97) |
| 23 | 0.68 (0.43–0.93) * | 0.55 (0.24–0.85) * |
| 24 | 0.89 (0.56–1.22) | 0.82 (0.34–1.29) |
| 25 or older | 0.51 (0.38–0.64) *** | 0.51 (0.25–0.77) ** |
| Type of communication participant responded to | ||
| Initial survey | Reference | Reference |
| Hard to reach with phone | 0.66 (0.51–0.81) *** | 0.79 (0.59–0.98) |
| Hard to reach without phone | 0.60 (0.27–0.92) | 0.75 (0.30–1.20) |
| Lifetime depression without 30-day depression? | ||
| No | Reference | Reference |
| Yes | 0.14 (0.08–0.20) *** | 1.03 (0.38–1.68) |
| Any current depression? | ||
| No | Reference | Reference |
| Yes | 14.56 (10.01–19.11) *** | 7.26 (3.84–10.68) *** |
| Lifetime anxiety without any 30-day anxiety? | ||
| No | Reference | Reference |
| Yes | 0.23 (0.16–0.30) *** | 1.01 (0.46–1.57) |
| Any current anxiety? | ||
| No | Reference | Reference |
| Yes | 6.38 (4.75–8.01)*** | 2.28 (1.24–3.32) *** |
| Knows someone in Vancouver who tested positive for COVID-19? | ||
| No | Reference | Reference |
| Yes | 0.90 (0.74–1.06) | 0.83 (0.66–1.00) |
| Had the COVID-19 pandemic affect their emotional wellbeing? | ||
| No | Reference | Reference |
| Yes, but they were able to manage it | 1.41 (1.03–1.80) ** | 0.78 (0.12) |
| Yes, they are overwhelmed and couldn't/can't find help | 7.18 (5.07–9.29) *** | 2.02 (1.34–2.71) *** |
| Yes, they are overwhelmed but were/are able to get help | 2.48 (1.76–3.19)*** | 0.86 (0.57–1.15) |
| Type of student | ||
| 1st year undergraduate | Reference | Reference |
| 2nd year undergraduate | 0.98 (0.73–1.23) | 1.23 (0.79–1.66) |
| 3rd year undergraduate | 0.93 (0.70–1.16) | 1.32 (0.76–1.89) |
| 4th year undergraduate | 0.87 (0.64–1.11) | 1.31 (0.68–1.94) |
| Graduate | 0.58 (0.44–0.72) *** | 1.34 (0.68–1.99) |
| Other | 0.61 (0.43–0.79) ** | 1.26 (0.61–1.91) |
| Ethnicity | ||
| White | Reference | Reference |
| First Nations, Inuit or Métis | 1.23 (0.69–1.77) | 0.82 (0.41–1.22) |
| Chinese | 1.39 (1.13–1.65) ** | 1.46 (1.13–1.79) *** |
| Non-Indigenous or Chinese Visible Minority | 1.40 (1.15–1.66) *** | 1.31 (1.03–1.59) ** |
| International student? | ||
| No | Reference | Reference |
| Yes | 0.97 (0.79–1.15) | 0.99 (0.76–1.22) |
| Housing type | ||
| With parents or other relatives | Reference | Reference |
| In their own home or apartment (owned or rented) | 0.66 (0.53–0.78) *** | 0.87 (0.65–1.10) |
| In a university owned or operated residence or fraternity | 1.00 (0.77–1.22) | 1.03 (0.76–1.31) |
| In a shared house, apartment or flat | 0.92 (0.72–1.12) | 0.96 (0.70–1.22) |
| Other | 0.61 (0.17–1.05) | 0.62 (0.11–1.14) |
| Lifetime suicide plan? | ||
| No | Reference | Reference |
| Yes | 6.91 (5.82–8.00) *** | 4.82 (3.94–5.69) *** |
| Lifetime suicide attempt? | ||
| No | Reference | Reference |
| Yes | 5.72 (4.36–7.08) *** | 1.70 (1.23–2.17)*** |
*p ≤ 0.05; **p ≤ 0.01; **p ≤ 0.001; ***p ≤ 0.001.
aEach unadjusted model contains only the variable of interest. The adjusted model contains all variables in a single model.
b"Other” gender is defined as a gender identity different than sex at birth. While there are many subgroups within this, they have been collapsed for the purpose of this analysis due to small cell counts.
Appendix Table 3.
Comparing Respondent and Population Demographics (N = 4,693).
| Respondent demographics (column %) | Population demographics (column %) | Absolute percent difference | |
|---|---|---|---|
| Gender | |||
| Male | 34.69 | 43.74 | 9.05 |
| Female | 63.05 | 56.23 | 6.82 |
| Othera | 2.26 | 0.02 | 2.24 |
| Age median (IQR) | 22 (20–26) | 22 (20–26) | - |
| Student status | |||
| International | 21.12 | 27.4 | 6.28 |
| Domestic | 78.88 | 72.6 | 6.28 |
| Year of study | |||
| 1 | 14.28 | 17.74 | 3.46 |
| 2 | 15.11 | 15.06 | 0.05 |
| 3 | 17.48 | 18.57 | 1.09 |
| 4 | 13.96 | 18.32 | 4.36 |
| Graduate | 27.37 | 18.77 | 8.6 |
| Others | 11.8 | 11.54 | 0.26 |
a“Other” gender is defined as a gender identity different than sex at birth. While there are many subgroups within this, they have been collapsed for the purpose of this analysis due to small cell counts.
Appendix Table 4.
Comparison of the Demographic Characteristics of Respondents Included and Excluded from the Models.
| Characteristic | Excluded from models (column %) (n = 2,351) | Included in models (column %) (n = 4,693) |
|---|---|---|
| Gender | ||
| Male | 812 (37.33) | 1,628 (34.69) |
| Female | 1,321 (60.74) | 2,959 (63.05) |
| Othera | 42 (1.93) | 106 (2.26) |
| Age | *** | *** |
| 18 or younger | 265 (12.24) | 502 (10.70) |
| 19 | 301 (13.90) | 609 (12.98) |
| 20 | 250 (11.55) | 563 (12.00) |
| 21 | 229 (10.58) | 493 (10.51) |
| 22 | 236 (10.90) | 410 (8.74) |
| 23 | 159 (7.34) | 298 (6.35) |
| 24 | 117 (5.40) | 251 (5.35) |
| 25 or older | 608 (28.08) | 1,567 (33.39) |
| Type of student | *** | *** |
| 1st year undergraduate | 376 (15.99) | 670 (14.28) |
| 2nd year undergraduate | 350 (14.89) | 709 (15.11) |
| 3rd year undergraduate | 340 (14.46) | 820 (17.47) |
| 4th year undergraduate | 234 (9.95) | 655 (13.96) |
| Graduate | 343 (14.59) | 1,284 (27.36) |
| Other | 708 (30.11) | 555 (11.83) |
| Ethnicity | *** | *** |
| White | 537 (24.88) | 1,762 (37.55) |
| First Nations, Inuit or Métis | 22 (1.02) | 143 (3.05) |
| Chinese | 667 (30.91) | 1,288 (27.45) |
| Non-Indigenous or Chinese Visible Minority | 932 (43.19) | 1,500 (31.96) |
| Housing type | ||
| With parents or other relatives | 869 (41.38) | 1,899 (40.46) |
| In their own home or apartment (owned or rented) | 524 (24.95) | 1,320 (28.13) |
| In a university owned or operated residence or fraternity | 329 (15.67) | 680 (14.49) |
| In a shared house, apartment or flat | 343 (16.33) | 727 (15.49) |
| Other | 35 (1.67) | 67 (1.43) |
*p ≤ 0.05; **p ≤ 0.01; ***p ≤ 0.001; Both Chi-squared and Fisher's exact tests were used where the cell counts are small. These are testing for an overall association.
a“Other” gender is defined as a gender identity different than sex at birth. While there are many subgroups within this, they have been collapsed for the purpose of this analysis due to small cell counts.
Footnotes
Data Access: Anonymous survey response data can be requested from the corresponding author from investigators at academic institutions with research ethics board approval.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Yatham reports personal fees from Canadian Network for Mood & Anxiety Treatments, personal fees from Gedeon Richter, grants and personal fees from DSP, personal fees from Sanofi, other from CANMAT, personal fees from Intracellular Therapies, personal fees from Merck, grants and personal fees from Abbvie, other from Alkermes, personal fees from GSK, outside the submitted work.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Health Canada (grant number 1920-HQ-000069).
ORCID iDs: Laura B. Jones https://orcid.org/0000-0002-6387-7542
Angel Y. Wang https://orcid.org/0000-0003-2001-2220
Daniel V. Vigo https://orcid.org/0000-0002-4445-4122
References
- 1.Auerbach RP, Alonso J, Axinn WG, et al. Mental disorders among college students in the World Health Organization world mental health surveys. Psychol Med. 2016; 46: 2955‐2970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Auerbach RP, Mortier P, Bruffaerts R, et al. WHO World mental health surveys international college student project: prevalence and distribution of mental disorders. J Abnorm Psychol. 2018; 127: 623‐638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mortier P, Cuijpers P, Kiekens G, et al. The prevalence of suicidal thoughts and behaviours among college students: a meta-analysis. Psychol Med. 2018; 48(4): 554‐565. [DOI] [PubMed] [Google Scholar]
- 4.Bourion-Bédès S, Tarquinio C, Batt M, et al. Stress and associated factors among French university students under the COVID-19 lockdown: the results of the PIMS-CoV 19 study. J Affect Disord. 2021; 283: 108‐114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Son C, Hegde S, Smith A, Wang X, Sasangohar F. Effects of COVID-19 on college students’ mental health in the United States: interview survey study. J Med Internet Res. 2020; 22(9): e21279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Keyserlingk L, Yamaguchi-Pedroza K, Arum R, Eccles JS. Stress of university students before and after campus closure in response to COVID-19. J Community Psychol. 2022; 50(1):285‐301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wathelet M, Duhem S, Vaiva G, et al. Factors associated with mental health disorders among university students in France confined during the COVID-19 pandemic. JAMA Netw Open. 2020; 3: e2025591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim H, Rackoff GN, Fitzsimmons-Craft EE, et al. College mental health before and during the COVID-19 pandemic: results from a nationwide survey. Cognit Ther Res. 2022; 46(1): 1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tasnim R, Islam MS, Sujan MSH, Sikder MT, Potenza MN. Suicidal ideation among Bangladeshi university students early during the COVID-19 pandemic: prevalence estimates and correlates. Child Youth Serv Rev. 2020; 119: 105703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nomura K, Minamizono S, Maeda E, et al. Cross-sectional survey of depressive symptoms and suicide-related ideation at a Japanese national university during the COVID-19 stay-home order. Environ Health Prev Med. 2021; 26(1): 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun S, Goldberg S B, Lin D, Qiao S, Operario D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Global Health. 2021; 17(1): 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Naghavi M. Global, regional, and national burden of suicide mortality 1990 to 2016: systematic analysis for the Global Burden of Disease Study 2016. Br Med J. 2019; 364: l94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pramukti I, Strong C, Sitthimongkol Y, et al. Anxiety and suicidal thoughts during the COVID-19 pandemic: cross-country comparative study among Indonesian, Taiwanese, and Thai university students. J Med Internet Res. 2020; 22(12): e24487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pirkis J, John A, Shin S, et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. The Lancet Psychiatry. 2021; 8(7): 579‐588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barbic D, Scheuermeyer FX, Barbic SP, Honer WG. Suicide deaths in British Columbia during the first wave of the COVID-19 pandemic. Can J Psychiatry. 2021; 66(9): 830‐831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pirkis J, John A, Shin S, et al. Did suicide numbers diverge from pre-existing trends during the first 9-15 months of the COVID-19 pandemic? Interrupted time series analyses of total and sex- and age-specific suicide counts in 33 countries. Preprint available at SSRN: https://ssrn.com/abstract=4066503 or 10.2139/ssrn.4066503 [DOI]
- 17.Tanaka T, Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat Hum Behav. 2021; 5: 229‐238. [DOI] [PubMed] [Google Scholar]
- 18.Kessler RC, Üstün BB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res. 2004; 13: 93‐121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mortier P, Auerbach RP, Alonso J, et al. Suicidal thoughts and behaviors among first-year college students: results from the WMH-ICS project. J Am Acad Child Adolesc Psychiatry. 2018; 57: 263‐273.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bruffaerts R, Mortier P, Auerbach RP, et al. Lifetime and 12-month treatment for mental disorders and suicidal thoughts and behaviors among first year college students. Int J Methods Psychiatr Res. 2019; 28: e1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ballester L, Alayo I, Vilagut G, et al. Accuracy of online survey assessment of mental disorders and suicidal thoughts and behaviors in Spanish university students. Results of the WHO world mental health-international college student initiative. PLoS One. 2019; 14: e0221529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ebert DD, Mortier P, Kaehlke F, et al. Barriers of mental health treatment utilization among first-year college students: first cross-national results from the WHO world mental health international college student initiative. Int J Methods Psychiatr Res. 2019; 28: e1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vigo D, Jones L, Munthali R, et al. Investigating the effect of COVID-19 dissemination on symptoms of anxiety and depression among university students. BJPsych Open. 2021; 7: e69. 10.1192/bjo.2021.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jones LB, Judkowicz C, Hudec KL, et al. The world mental health international college student survey in Canada: protocol for a mental health and substance use trend study. JMIR Res Protoc. 2022; 11(7): e35168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cuijpers P, Auerbach RP, Benjet C, et al. The world health organization world mental health international college student initiative: an overview. Int J Methods Psychiatr Res. 2019; 28: e1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wood SN. Generalized additive models: an introduction with R. 2nd ed. Boca Raton, FL: CRC Press; 2017. doi: 10.1201/9781315370279. [DOI] [Google Scholar]
- 27.Gunnell D, Appleby L, Arensman E, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020; 7: 468‐471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.The American Association for Public Opinion Research. Standard definitions: final dispositions of case codes and outcome rates for surveys. 9th ed. AAPOR; 2016. [Google Scholar]
- 29.Morganstein JC, Ursano RJ. Ecological disasters and mental health: causes, consequences, and interventions. Front Psychiatry. 2020; 11: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bowe M, Wakefield JRH, Kellezi B, et al. The mental health benefits of community helping during crisis: coordinated helping, community identification and sense of unity during the COVID-19 pandemic. J Community Appl Soc Psychol. 2022; 32: 521‐535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Garlow SJ, Rosenberg J, Moore JD, et al. Depression, desperation, and suicidal ideation in college students: results from the American Foundation for Suicide Prevention College Screening Project at Emory University. Depress Anxiety. 2008; 25(6): 482‐488. [DOI] [PubMed] [Google Scholar]
- 32.Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: results from the national comorbidity survey replication. Mol Psychiatry. 2010; 15(8): 868‐876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sa J, Choe S, Cho BY, Chaput JP, Lee J, Hwang S. Sex and racial/ethnic differences in suicidal consideration and suicide attempts among US college students, 2011-2015. Am J Health Behav. 2020; 44(2): 214‐231. [DOI] [PubMed] [Google Scholar]
- 34.Cheah CSL, Wang C, Ren H, Zong X, Cho HS, Xue X. COVID-19 racism and mental health in Chinese American families. Pediatrics. 2020; 146(5): e2020021816. [DOI] [PubMed] [Google Scholar]
- 35.Lou NM, Noels KA, Kurl S, Zhang YSD, Young-Leslie H. Chinese Canadians’ experiences of the dual pandemics of COVID-19 and racism: implications for identity, negative emotion, and anti-racism incident reporting. Can Psychol. 2022; 63(3): 279‐297. [Google Scholar]
- 36.Wang C, Pan R, Wan X, et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020; 87: 40‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lal S, Adair CE. E-mental health: a rapid review of the literature. Psychiatr Serv. 2014; 65(1): 24‐32. [DOI] [PubMed] [Google Scholar]
- 38.Lal S. E-mental health: promising advancements in policy, research, and practice. Healthc Manag Forum. 2019; 32(2): 56‐62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gratzer D, Torous J, Lam RW, et al. Our digital moment: innovations and opportunities in digital mental health care. Can J Psychiatry. 2021; 66(1): 5‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nair CS, Adams P, Mertova P. Student engagement: the key to improving survey response rates. Qual High Educ. 2008; 14(3): 225‐232. [Google Scholar]