Abstract
The gold standard treatment for benign gallbladder disease is laparoscopic cholecystectomy (LC). LC is commonly performed using monopolar diathermy with ligation of the cystic duct and artery with clips. The aim of the current systematic review was to compare harmonic scalpel (HS) with clips in LC. Eligible studies were identified from PubMed, Cochrane library, Embase and Medline and meta-analysis was conducted using Review Manager 5.4. The primary outcome evaluated was bile leak while secondary outcomes evaluated were overall postoperative complications, operative time, conversion to open surgery and gall bladder perforation. Eight randomized control trials met the eligibility criteria which included a total of 1,205 patients. There was no statistically significant difference between the two groups in terms of bile leak (p = 0.56, I2=0%). With respect to the operative time (p = 0.004, I2=97%), conversion to open surgery (p = 0.02, I2=0%) and gall bladder perforation (p = 0.0001, I2=26%) HS was superior to clips. HS is an acceptable alternative to the use of clips when ligating the cystic duct.
Keywords: bile leak, systematic review, clips, harmonic scalpel, conventional laparoscopic cholecystectomy
Introduction and background
Laparoscopic cholecystectomy (LC) is considered to be the gold standard treatment for benign gall bladder pathologies [1]. Standard LC involves the use of metal clips to ligate the cystic duct and the cystic artery prior to division with laparoscopic scissors. In some cases, monopolar electrocautery is also used to divide the cystic artery. Monopolar electrocautery still remains the preferred energy device of choice by surgeons while performing LC [2,3]. Alternative methods of bile duct ligation include linear staplers, sutures and endoloops, but these have very seldom been used [4]. The main limitation of the use of monopolar diathermy is that there is a high risk of surrounding thermal damage. Slippage of clips off the cystic duct in relation to the gall bladder causes bile to spill into the surgical field and this invariably causes frequent instrument change which increases the risk of visceral-related injuries [5,6]. A harmonic scalpel (HS) is an energy device that makes use of ultrasound within the harmonic frequency range to coagulate and cut tissue. It is designed to be superior to monopolar diathermy and has the capability to seal vessels 5 to 7mm in diameter. Studies have also shown that thermal energy spread is less with HS as compared to monopolar diathermy [7]. The purpose of the current systematic review is to evaluate the role of HS in successfully sealing the cystic duct in LC as compared to standard clip ligation. The primary outcome evaluated was bile leak while secondary outcomes evaluated were overall postoperative complications, operative time, conversion to open surgery and inadvertent gall bladder perforation during surgery.
Review
Systematic reviews and meta-analyses were designed and reported according to Preferred Reporting Items for Systemic Reviews and Meta-Analyses (PRISMA) [8].
Search strategy
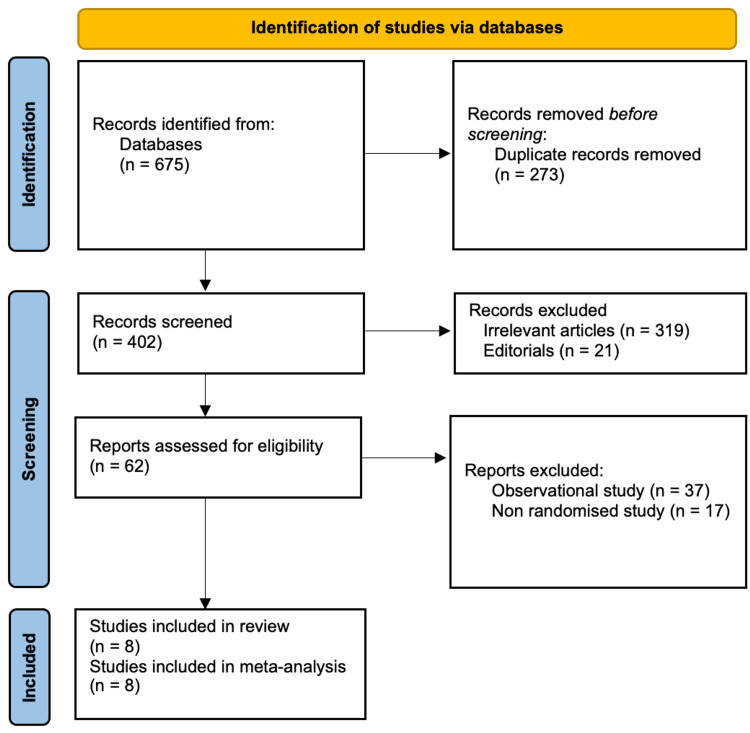
A comprehensive literature search was conducted independently by two authors from PubMed, Cochrane library, Embase and Medline. The last date of the search was September 21, 2022. There were no publication date restrictions and only human studies were included. Keywords used for electronic searches were “harmonic scalpel,” “ultrasonic device,” “clips,” “titanium clips,” “cholecystectomy,” “laparoscopy,” “laparoscopic cholecystectomy,” “cystic duct,” “bile leak” and “clipless cholecystectomy.” A flow chart of included and excluded studies is shown in Figure 1.
Figure 1. PRISMA flow chart.
Preferred Reporting Items for Systemic Reviews and Meta-Analyses
Study selection
Studies eligible for inclusion were: (1) randomized controlled trials (RCTs) comparing HS with clips in LC, (2) provided information on outcome measures and (3) information on the closure of cystic ducts. Studies excluded were (1) non-RCTs, (2) studies not based on the closure of cystic duct, (3) open cholecystectomies, (4) case reports, observational studies, reviews and meta-analyses.
Data collection
The following data were extracted by two authors from each study: first author, year of publication, country of origin, number of included patients, mean age, gender distribution, operative time, intraoperative gall bladder perforation, type of cystic duct closure used, duration of surgery, postoperative complications, gall bladder perforation and conversion to open surgery.
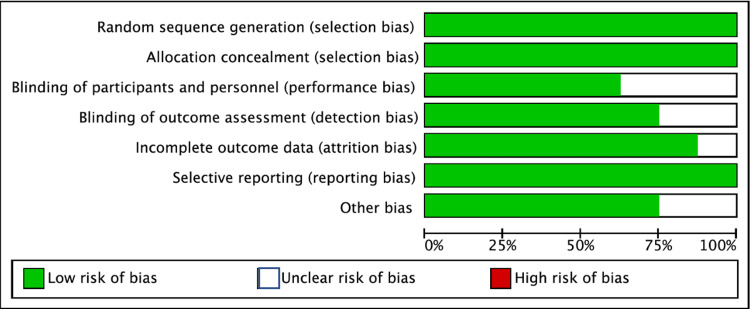
Assessment of risk of bias
The risk of bias was assessed based on the Cochrane risk of bias tool [9] by two authors. The following categories were classified as low, high or unclear: random sequence generation, allocation concealment, blinding of outcome assessment, blinding of participants and personnel, selective reporting and other sources of bias. The risk of bias was decided by discussion between all authors (Figure 2).
Figure 2. Risk of Bias among included studies.
Statistical analysis
Review manager 5.4 was used for statistical analysis. Mean difference was calculated for continuous data at 95% confidence intervals while risk ratio at 95% confidence interval was calculated for dichotomous variables. The Cochrane Q test and I2 test were used to assess heterogeneity in the included studies. 0% was considered as no heterogeneity while >50% was considered as significant heterogeneity. Random effect models and fixed effect models were used for analysis appropriately based on the calculated heterogeneity.
Results
Eight RCTs were included in our analysis comprising a total of 1205 patients. There were 547 patients that underwent LC with monopolar diathermy and clip ligation of the cystic duct while 658 patients underwent LC with HS. Characteristics of the clips group and harmonic group are shown in Table 1.
Table 1. Characteristics of included studies.
| Study | Country (Year of publication) | Method of randomization | Clips Group | Harmonic Group | ||||
| Number of patients | Sex Male / Female | Mean Age ± SD (Years) | Number of patients | Sex Male / Female | Mean Age ± SD (Years) | |||
| Bessa et al. [10] | Egypt (2008) | Sealed envelope | 60 | 12 / 48 | 42.5 ± 11.4 | 60 | 13 / 47 | 41.5 ± 10.3 |
| El et al. [11] | Egypt (2010) | Sealed envelope | 60 | 35 / 25 | 39.93 ± 13.82 | 60 | 42 / 18 | 41.42 ± 10.36 |
| Redwan [12] | Egypt (2010) | Not mentioned | 80 | 33 /47 | Not recorded | 80 | 27/ 53 | Not recorded |
| Kandil et al. [13] | Egypt (2010) | Sealed envelope | 70 | 30 / 40 | 41.38 ± 11.91 | 70 | 29 / 41 | 40.97 ± 11.56 |
| Jain et al [14] | India (2011) | Computer generated random numbers | 100 | 11 / 85 | 38.67 ± 11.87 | 100 | 6 / 90 | 39.55 ± 11.12 |
| Catena et al [15] | Italy (2014) | Computer generated random numbers | 21 | 10 /11 | 71.6 ± 6.2 | 21 | 11 /10 | 71.2 ± 7.1 |
| Liao et al [16] | China (2016) | Computer generated random numbers | 81 | 40/41 | 42.2 ± 10.4 | 21 | 51/66 | 43.4 ± 11.1 |
| Sanawan et al [17] | Pakistan (2017) | Sealed envelope | 75 | 7 / 68 | Not recorded | 117 | 22 / 128 | Not recorded |
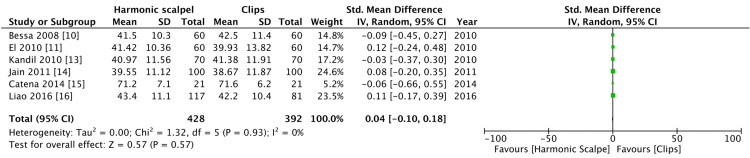
There was no significant difference in terms of age and no significant heterogeneity. Two of the included studies [12,17] did not record age as a mean and standard deviation and hence were not included in analyzing forest plots (Figure 3).
Figure 3. Comparison of age between harmonic group and clips group.
Table 2 shows the outcome of the included studies in the clips group and harmonic group.
Table 2. Outcomes of included studies.
| Study | Clips group | Harmonic Group | ||||||||
| Gall Bladder Perforation | Conversion to open | Operative time (Min) | Bile Leakage | Post op complications | Gall Bladder Perforation | Conversion to open | Operative time (Min) | Bile Leakage | Post op complications | |
| Bessa et al. [10] | 20 | 0 | Not recorded | 0 | 4 | 6 | 0 | Not recorded | 0 | 3 |
| El et al. [11] | 11 | 3 | 69.71 ± 13.01 | 2 | 9 | 6 | 2 | 45.17 ± 10.54 | 1 | 5 |
| Redwan [12] | 11 | 0 | 44.01 ± 6.47 | 0 | Not recorded | 8 | 0 | 16.8 ± 6.8 | 1 | Not recorded |
| Kandil et al. [13] | 13 | 2 | 51.7 ± 13.79 | 2 | 11 | 5 | 0 | 33.21 ± 9.62 | 0 | 3 |
| Jain et al [14] | 18 | 4 | 64.70 ± 13.74 | 0 | Not recorded | 9 | 4 | 50.0 ± 9.35 | 0 | Not recorded |
| Catena et al [15] | Not recorded | 7 | 106.4 ± 11.3 | 0 | 4 | Not recorded | 1 | 101.3 ± 10.1 | 1 | 5 |
| Liao et al [16] | 0 | 0 | 51.7 ± 9.6 | 0 | 1 | 0 | 1 | 54.9 ± 13.1 | 1 | 2 |
| Sanawan et al [17] | 16 | 0 | Not recorded | 0 | Not recorded | 5 | 0 | Not recorded | 0 | Not recorded |
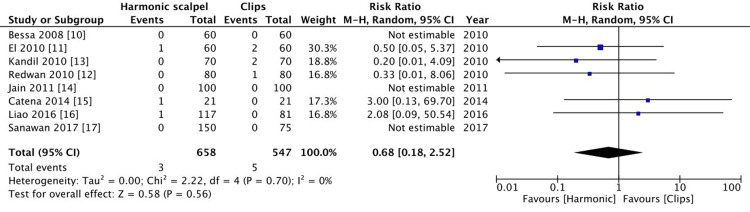
Bile leak
The primary outcome of our study was to evaluate bile leak between the harmonic group and the clips group in the early postoperative period (one week following surgery). There were three reported cases of bile leak in the harmonic group and five cases in the clips group. This failed to show a statistically significant difference (p = 0.56, I2=0%) (Figure 4).
Figure 4. Comparison of bile leak between harmonic group and clips group.
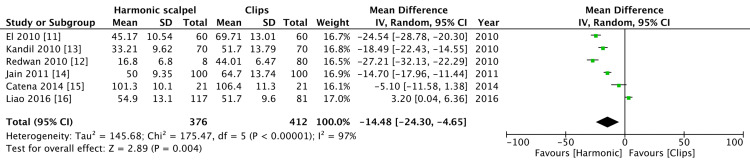
Operative time
Operative time was recorded by six studies. Operative time with the harmonic group was shorter as compared to the clips group and this was statistically significant. There was a high level of heterogeneity in regard to operative time (p = 0.004, I2=97%) (Figure 5).
Figure 5. Comparison of operative time between harmonic group and clips group.
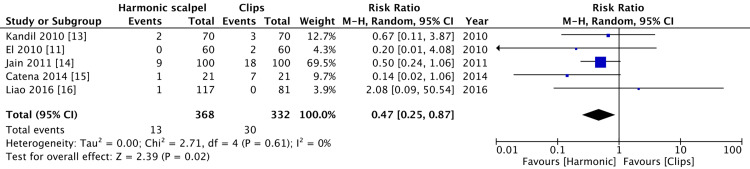
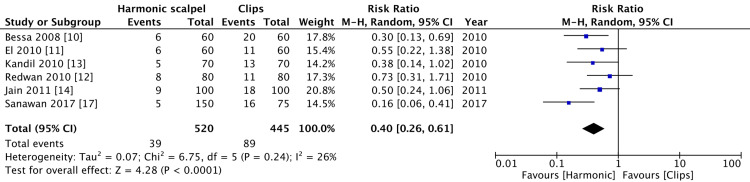
Conversion to open surgery and gall bladder perforation
In three of the included studies [10,12,17], there was no conversion of open surgery in either of the groups. There were 13 cases in the harmonic group and 81 cases in the clips group that was converted to open surgery. This was statistically significant with low heterogeneity (p = 0.02, I2=0%) (Figure 6).
Figure 6. Comparison of conversion to open surgery between harmonic group and clips group.
Liao et al. [16] did not have any gall bladder perforation during surgery and Catena et al. [15] had not recorded gall bladder perforation in their study. There were 39 cases of gall bladder perforation in the harmonic group and 89 in the clips group which was statistically significant. There was a low level of heterogeneity (p = 0.0001, I2=26%) (Figure 7).
Figure 7. Comparison of gall bladder perforation between harmonic group and clips group.
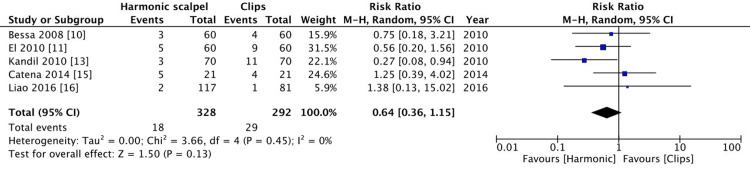
Postoperative complications
Five studies reported post-operative complications. Since the primary outcome was to evaluate bile leak this has not been included in the analysis as part of post-operative complications. There was no significant difference between the two groups (p=0.13, I2=0%) (Figure 8).
Figure 8. Comparison of operative complications between harmonic group and clips group.
Discussion
HS works on the principle of generating high-frequency ultrasound which when applied to tissue produces three main effects of cavitation, coagulation and lastly cutting [18]. Due to these effects, it limits the number of instruments required to perform a safe cholecystectomy. A standard cholecystectomy includes the use of monopolar cautery for dissection, clips for ligation of cystic artery and duct and laparoscopic scissors for division [19]. Since HS can overcome the use of multiple instrumentations, it invariably reduces the chance of intraoperative tissue injury [20]. The heat generated from HS ranges between 60 to 90 degrees Celsius, which is lower as compared to monopolar diathermy which is 150 degrees Celsius [21]. Hence the degree of thermal damage by HS is less as compared to monopolar diathermy.
The main outcome of our systematic review was to evaluate bile leaks following the application of clips versus the use of HS. Although there were a greater number of bile leaks with clip application it was not significant. The most common cause of bile leak is from cystic duct stumps and secondly from inadvertent injury to the biliary tree [22]. Another reason for bile leak is the accessory duct of Lushka, which can leak bile during gall bladder separation from the liver bed [23]. In these situations, HS proves to be quite beneficial.
The main advantage of harmonic seen in this review was that operative time was significantly shorter as compared to the use of clips. When clips are being used in cholecystectomy, it often involves the use of multiple instruments to be taken in and out which adds to the operative time. HS on the other hand acts as a sole instrument to cut and seals tissue at the same time achieving hemostasis [24].
In our review, there were a greater number of cases in the clips group that converted to open surgery as compared to the harmonic group and this was found to be statistically significant and consistent with already published literature [16]. In reference to gall bladder perforation, there were more cases in the clips group where monopolar diathermy was used, and this was consistent with published literature [12-14]. This is most likely to be due to the precision by which HS can be used laparoscopically as compared to monopolar diathermy. Another factor can also be the greater thermal damage caused by monopolar diathermy as compared to HS. Factors such as gall bladder inflammation, operative technique, surgeons' experience, and patient factors such as cirrhosis and obesity will also affect the outcome of open conversion and gall bladder perforation [25].
Limitations to the current review are a smaller size of the included cohort and this can result in a potential publication bias. However, we have chosen to include only RCTs to minimize bias. Data with respect to postoperative complications and gall bladder perforation were not recorded in all studies and this will affect the overall analysis. Studies have not taken patient-related factors into consideration such as but not limited to gall bladder inflammation, obesity, and liver cirrhosis which can potentially affect outcome measures.
Conclusions
The current systematic review demonstrated that HS has certain advantages over the use of clips and monopolar diathermy used in conventional LC. With respect to operative time, conversion to open surgery and gall bladder perforation HS proved to be more useful. There was no difference in terms of postoperative bile leak or general postoperative complications. Hence, we conclude that HS is an acceptable alternative to the use of clips when ligating the cystic duct.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
Footnotes
The authors have declared that no competing interests exist.
References
- 1.WSES guidelines on acute calculous cholecystitis. Ansaloni L, Pisano M, Coccolini F, et al. World J Emerg Surg. 2016;11:25. doi: 10.1186/s13017-016-0082-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Laparoscopic cholecystectomy with Harmonic scalpel. Gelmini R, Franzoni C, Zona S, Andreotti A, Saviano M. JSLS. 2010;14:14–19. doi: 10.4293/108680810X12674612014301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Using a standardized method for laparoscopic cholecystectomy to create a concept operation-specific checklist. Connor SJ, Perry W, Nathanson L, Hugh TB, Hugh TJ. HPB (Oxford) 2014;16:422–429. doi: 10.1111/hpb.12161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ligation of the structures of the cystic pedicle during laparoscopic cholecystectomy. Nathanson LK, Easter DW, Cuschieri A. Am J Surg. 1991;161:350–354. doi: 10.1016/0002-9610(91)90596-6. [DOI] [PubMed] [Google Scholar]
- 5.Injuries during laparoscopic cholecystectomy: a scoping review of the claims and civil action judgements. Cirocchi R, Panata L, Griffiths EA, et al. J Clin Med. 2021;10:5238. doi: 10.3390/jcm10225238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bile leakage resulting from clip displacement of the cystic duct stump: a potential pitfall of laparoscopic cholecystectomy. Hanazaki K, Igarashi J, Sodeyama H, Matsuda Y. Surg Endosc. 1999;13:168–171. doi: 10.1007/s004649900932. [DOI] [PubMed] [Google Scholar]
- 7.Comparison of lateral thermal damage of the human peritoneum using monopolar diathermy, harmonic scalpel and LigaSure. Družijanić N, Pogorelić Z, Perko Z, Mrklić I, Tomić S. Can J Surg. 2012;55:317–321. doi: 10.1503/cjs.000711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cochrane handbook for systematic reviews of interventions. [ Oct; 2022 ]. 2022. https://training.cochrane.org/handbook/current https://training.cochrane.org/handbook/current
- 9.The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. Higgins JP, Altman DG, Gøtzsche PC, et al. BMJ. 2011;343:0. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clipless laparoscopic cholecystectomy by ultrasonic dissection. Bessa SS, Al-Fayoumi TA, Katri KM, Awad AT. J Laparoendosc Adv Surg Tech A. 2008;18:593–598. doi: 10.1089/lap.2007.0227. [DOI] [PubMed] [Google Scholar]
- 11.Clipless laparoscopic cholecystectomy using the Harmonic scalpel for cirrhotic patients: a prospective randomized study. El Nakeeb A, Askar W, El Lithy R, Farid M. Surg Endosc. 2010;24:2536–2541. doi: 10.1007/s00464-010-0999-9. [DOI] [PubMed] [Google Scholar]
- 12.Single-working-instrument, double-trocar, clipless cholecystectomy using harmonic scalpel: a feasible, safe, and less invasive technique. Redwan AA. J Laparoendosc Adv Surg Tech A. 2010;20:597–603. doi: 10.1089/lap.2009.0375. [DOI] [PubMed] [Google Scholar]
- 13.Comparative study between clipless laparoscopic cholecystectomy by harmonic scalpel versus conventional method: a prospective randomized study. Kandil T, El Nakeeb A, El Hefnawy E. J Gastrointest Surg. 2010;14:323–328. doi: 10.1007/s11605-009-1039-8. [DOI] [PubMed] [Google Scholar]
- 14.A prospective, randomized study of comparison of clipless cholecystectomy with conventional laparoscopic cholecystectomy. Jain SK, Tanwar R, Kaza RC, Agarwal PN. J Laparoendosc Adv Surg Tech A. 2011;21:203–208. doi: 10.1089/lap.2010.0455. [DOI] [PubMed] [Google Scholar]
- 15.The HAC trial (harmonic for acute cholecystitis): a randomized, double-blind, controlled trial comparing the use of harmonic scalpel to monopolar diathermy for laparoscopic cholecystectomy in cases of acute cholecystitis. Catena F, Di Saverio S, Ansaloni L, et al. World J Emerg Surg. 2014;9:53. doi: 10.1186/1749-7922-9-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harmonic scalpel versus monopolar Electrocauterization in cholecystectomy. Liao G, Wen S, Xie X, Wu Q. JSLS. 2016;20:0. doi: 10.4293/JSLS.2016.00037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Effectiveness of ultrasound shear for clipless laparoscopic cholecystectomy versus conventional unipolar electrocautery in patients with cholelithiasis. Sanawan E, Qureshi AU, Qureshi SS, Cheema KM, Cheema MA. http://chrome-extension://efaidnbmnnnibpcajpcglclefindmkaj/https://jcpsp.pk/archive/2017/Oct2017/05.pdf. J Coll Physicians Surg Pak. 2017;27:611–615. [PubMed] [Google Scholar]
- 18.The harmonic scalpel. Dutta DK, Dutta I. J Obstet Gynaecol India. 2016;66:209–210. doi: 10.1007/s13224-016-0850-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.The standard of laparoscopic cholecystectomy. Bittner R. Langenbecks Arch Surg. 2004;389:157–163. doi: 10.1007/s00423-004-0471-1. [DOI] [PubMed] [Google Scholar]
- 20.Three-port laparoscopic cholecystectomy by harmonic dissection without cystic duct and artery clipping. Tebala GD. Am J Surg. 2006;191:718–720. doi: 10.1016/j.amjsurg.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 21.Determination of temperature elevation in tissue during the application of the harmonic scalpel. Koch C, Friedrich T, Metternich F, Tannapfel A, Reimann HP, Eichfeld U. Ultrasound Med Biol. 2003;29:301–309. doi: 10.1016/s0301-5629(02)00727-5. [DOI] [PubMed] [Google Scholar]
- 22.Clipless minilaparoscopic cholecystectomy: a study of 1,096 cases. Suo G, Xu A. J Laparoendosc Adv Surg Tech A. 2013;23:849–854. doi: 10.1089/lap.2012.0561. [DOI] [PubMed] [Google Scholar]
- 23.Bile leaks from the duct of Luschka (subvesical duct): a review. Spanos CP, Syrakos T. Langenbecks Arch Surg. 2006;391:441–447. doi: 10.1007/s00423-006-0078-9. [DOI] [PubMed] [Google Scholar]
- 24.A comparative study of ultrasonic scalpel (US) versus conventional metal clips for closure of the cystic duct in laparoscopic cholecystectomy (LC): a meta-analysis. Ai XM, Ho LC, Yang NY, Han LL, Lu JJ, Yue X. Medicine (Baltimore) 2018;97:0. doi: 10.1097/MD.0000000000013735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Evaluation of affecting factors for conversion to open cholecystectomy in acute cholecystitis. Oymaci E, Ucar AD, Aydogan S, Sari E, Erkan N, Yildirim M. Prz Gastroenterol. 2014;9:336–341. doi: 10.5114/pg.2014.45491. [DOI] [PMC free article] [PubMed] [Google Scholar]