Abstract
Objective
Postoperative delirium (POD) is a common complication, and clinical practitioners have taken measures to improve the quality of life after hip replacement surgery. We aim to establish a nomogram to predict POD in elderly patients with femoral neck fractures (FNFs) after hip replacement.
Methods
A total of 384 elderly patients (267 females) with an average age of 75.8 years who underwent hip replacement from June 2010 to May 2020 were retrospectively reviewed. Patients were divided into delirium and non‐delirium groups according to the confusion assessment method. The risk factors for POD were analyzed by multivariate logistic regression, and the nomogram was established based on the results.
Results
The incidence of POD was 33.33% (128/384). Univariate analysis showed that advanced age, diabetes, lacunar cerebral infarction, surgery type, intraoperative blood loss, electrolyte imbalance, and anemia were risk factors for POD (p < 0.05). Multivariate logistic regression revealed that the independent risk factors for POD were age (OR = 1.332, 95% CI [1.224, 1.449], p < 0.01), surgery type (OR = 0.351, 95% CI [0.137, 0.900], p = 0.029), electrolyte imbalance (OR = 4.407, 95% CI [1.947, 9.977], p< 0.01), anemia (OR = 10.819, 95% CI [4.573, 25.598], p < 0.01). The prediction equation was established; logistic (p) = −25.469 + 0.277*X1(age[value = years of age]) + 1.293*X2(surgery[value = 0 for “total hip replacement” or value = 1 for “hemiarthroplasty”]) + 1.510*X3(electrolyte imbalance[value = 0 for “no” or value = 1 for “yes”]) + 2.157*X4(anemia[value = 1 for “hemoglobin with < 120g/L in male and < 110g/L in female patients” ]) or 2.975*X5(anemia[value = 1 for “hemoglobin with <90g/L"]). The area under the curve was 0.957 (95% CI [0.938, 0.976], p < 0.01).
Conclusion
The incidence of POD in elderly patients with FNF after hip replacement is high. The nomogram incorporating age, surgery type, electrolyte imbalance, and anemia could provide an individualized prediction for POD among FNF patients after hip replacement, which may help the physician determine appropriate perioperative management.
Keywords: Femoral neck fracture, Hip replacement, Nomogram, Postoperative delirium, Risk factors
The nomogram incorporating age, surgery type, electrolyte imbalance, and anemia could provide an individualized prediction for POD among femoral neck fracture patients after hip replacement, which may help the physician determine appropriate perioperative management.

Introduction
Femoral neck fracture (FNF) is increasingly common in the elderly, mainly due to bone fragility and impaired walking ability 1 , 2 . As the global aging population increased, the number of elderly patients sustaining a hip fracture who need hip replacement has dramatically increased year by year 3 . Despite improved perioperative management, elderly patients are prone to postoperative complications owing to multiple comorbidities, leading to unsatisfying outcomes 4 .
Postoperative delirium (POD) is a common central nervous system complication in elderly patients, with an incidence of up to 50%. It is an acute and fluctuating mental state change that occurs after surgical anesthesia, accompanied by decreased consciousness, attention and psychomotor disorders, and sleep–wake cycle disturbances 5 . Once it occurs, patient compliance with treatment decreases dramatically, which increases the risk of cardiovascular events and prolongs the postoperative hospitalization, causing an increased burden on family and social medical care 6 , 7 , 8 . Therefore, clinical practitioners have been exploring the risk factors for POD and taking measures in advance to improve the quality of life after hip replacement surgery.
Due to multiple factors, the mechanism of POD is still unclear, but its risk factors can be roughly divided into two categories: susceptibility and predisposing factors. In recent years, with the continuous deepening of POD‐related research, advanced age, hypoalbuminemia, preoperative use of anticholinergic drugs, alcohol abuse, preoperative and postoperative pain, blood transfusion, and hypotension were gradually getting attention 9 . A previous study has revealed that preoperative delirium, preoperative dementia, advanced age, medical co‐management, ASA III‐V, functional dependence, smoking, systemic inflammatory response syndrome, preoperative use of mobility aid are risk factors for a hip fracture POD prediction model 10 . In the POD prediction model, however, patients with different operations were included. As internal fixation and hip replacement were two different surgeries with different surgical indications, we constructed a POD prediction model for patients undergoing hip replacement of clinical importance.
Nomograms had a wide application in oncology to quantify risks by incorporating variables. It could be used to calculate the probability of any events based on multivariable analysis. The purpose of the study was: (i) to identify the risk factors for POD among patients with hip replacement; (ii) to construct a corresponding clinical nomogram to predict high‐risk ones.
Methods
Study Population
We included elderly patients (>65 years of age) with FNFs who underwent hip replacement surgery in our center from June 2010 to May 2020. The electronic medical record was reviewed by two independent reviewers. One surgeon preformed all hip replacement surgeries in our center.
Exclusion criteria: (1) pathological fractures; (2) multiple trauma; (3) patients with preoperative delirium, cognitive impairment, and confusion; (4) previous history of mental illness; (5) aphasia and hearing impairment. This study was reviewed and approved by the Peking University People's Hospital Ethics Committee (2021phb190‐01).
Delirium Assessment
Postoperative delirium refers to the occurrence of delusion within 72 h after surgery. Delirium was evaluated according to the confusion assessment method (CAM). The diagnostic criteria of CAM include four items: (1) acute onset and fluctuating course, (2) inattention, and either (3) disorganized thinking, or (4) altered level of consciousness. Delirium can be diagnosed when (1) + (2) + (3) or (1) + (2) + (4) appears 11 .
Model Development
We evaluated 14 variables with the potential to predict the POD. The variables consisted of patient demographic characteristics, chronic coexisting conditions at admission, surgery and anesthesia type, and preoperative laboratory test results. Anemia was defined as hemoglobin <120g/L in male and <110g/L in female patients. The moderate and severe anima was defined as hemoglobin <90g/L and <60g/L, respectively. Electrolyte imbalance was defined as the concentration of potassium, sodium, and calcium beyond the normal range over 24 h after treatment.
The prediction model was established using variable screening. Firstly, the univariate analysis of the included factors was performed. Multivariate logistic regression was then performed on seven variables selected from the univariate analysis and relative weights were assigned to them. A nomogram was then drawn to present these variables and corresponding scores for the risk of POD.
Statistical Analysis
SPSS 25.0 software (IBM, USA) was used for statistical processing. The categorical variables were expressed as the number and percentages, using the χ2 of Fisher exact test to verify the differences between the groups; the continuous variables were expressed as the mean and standard deviation, and the independent sample t‐test was used for the comparison between groups. The related risk factors of POD were analyzed by the multivariate logistic regression method. p < 0.05 indicated that the difference was statistically significant. The mathematical formula of the model was generated and drawn using the nomogram package in R software (version 3.6.3; R Foundation for Statistical Computing, Vienna, Austria). The model was then validated for discrimination and calibration abilities, using the rms package in R software. The calibration curve, with the Hosmer–Lemeshow χ2 test, was used to evaluate the agreement between the predicted probability and the actual events.
Ethics Statement
This study was reviewed and approved by the Peking University People's Hospital Ethics Committee (2021phb190‐01). Written informed consent was obtained from all participants. All clinical investigations conformed to the provisions of the Declaration of Helsinki.
Results
Risk Factors
A total of 384 patients were included in the study. The age range was 65–103 years old, with an average of (75.78 ± 11.62) years old. There were 267 females and 117 males. POD occurred in 128 of the 384 patients, with an incidence rate of 33.33%. The differences between the two groups of patients in terms of age, previous diabetes, lacunar infarction, surgery type, intraoperative blood loss, electrolyte imbalance, and anemia were statistically significant (p < 0.05) (Table 1).
TABLE 1.
Univariate analysis of POD in elderly patients with femoral neck fracture after hip arthroplasty
| Factors | With delirium (128) | Without delirium (256) | Χ2/T | p |
|---|---|---|---|---|
| Age | 84.601 ± 5.255 | 71.039 ± 8.733 | 18.923 | <0.001 |
| Gender | 0.885 | 0.347 | ||
| Male | 35 | 82 | ||
| Female | 93 | 174 | ||
| Comorbidity | 2.798 | 0.094 | ||
| Yes | 124 | 237 | ||
| No | 4 | 19 | ||
| Hypertension | 0.005 | 0.942 | ||
| Yes | 69 | 137 | ||
| No | 59 | 119 | ||
| Diabetes | 6.752 | 0.009 | ||
| Yes | 26 | 82 | ||
| No | 102 | 174 | ||
| Coronary heart disease | 2.169 | 0.141 | ||
| Yes | 19 | 25 | ||
| No | 109 | 231 | ||
| Lacunar Infarction | 4.995 | 0.025 | ||
| Yes | 9 | 6 | ||
| No | 119 | 250 | ||
| Chronic stroke | 2.04 | 0.153 | ||
| Yes | 10 | 11 | ||
| No | 118 | 245 | ||
| Surgery type | 108.63 | <0.001 | ||
| Hemiarthroplasty | 113 | 82 | ||
| Total hip arthroplasty | 15 | 174 | ||
| Blood loss(ml) | 154.609 ± 130.739 | 205.75 ± 166.616 | −3.288 | 0.001 |
| Length of hospital stay (Day) | 16.234 ± 16.048 | 15.973 ± 7.930 | 0.174 | 0.862 |
| Anesthesia | 0.464 | 0.464 | ||
| General | 34 | 46 | ||
| Spinal | 132 | 212 | ||
| Electrolyte imbalance | 56.593 | <0.001 | ||
| Yes | 103 | 102 | ||
| No | 25 | 154 | ||
| Anemia | 47.068 | <0.001 | ||
| Yes | 98 | 101 | ||
| No | 30 | 155 |
After the multivariate logistic regression, it was concluded that age (advanced), surgery type (hemiarthroplasty), electrolyte imbalance, and anemia were independent risk factors for POD in elderly patients’ hip fracture after a hip replacement (p < 0.05) (Table 2).
TABLE 2.
Multivariate analysis of POD in elderly patients with femoral neck fracture after hip arthroplasty
| Factor | B | ST | Wald χ2 | p | OR | 95%CI | |
|---|---|---|---|---|---|---|---|
| lower | upper | ||||||
| Age | 0.277 | 0.042 | 42.990 | 0.000 | 1.319 | 1.214 | 1.433 |
| Diabetes | −0.308 | 0.470 | 0.517 | 0.472 | 0.735 | 0.317 | 1.703 |
| Lacunar infarction | 1.737 | 1.109 | 2.453 | 0.117 | 5.679 | 0.646 | 49.908 |
| Surgery type | 1.293 | 0.470 | 7.579 | 0.006 | 3.644 | 1.451 | 9.150 |
| Blood loss | −0.001 | 0.001 | 0.814 | 0.367 | 0.999 | 0.997 | 1.001 |
| Electrolyte Imbalance | 1.510 | 0.410 | 13.566 | 0.000 | 4.528 | 2.207 | 10.114 |
| Anemia | |||||||
| mild | 2.157 | 0.431 | 25.002 | 0.000 | 8.648 | 3.712 | 20.145 |
| Moderate | 2.975 | 0.811 | 13.456 | 0.000 | 19.598 | 3.997 | 96.085 |
Abbreviations: OR, odds ratio; ST, standard deviation.
Model Development
The derived nomogram to predict POD was shown in Figure 1. The mathematical equation for calculating admission risk could be divided into three following steps. Step 1: calculate Y1, Y1 = −25.469 + 0.277*X1(age[value = years of age]) + 1.293*X2(surgery[value = 0 for “total hip replacement” or value = 1 for “hemiarthroplasty”]) + 1.510*X3(electrolyte imbalance[value = 0 for “no” or value = 1 for “yes”]) + 2.157*X4(anemia[value = 1 for “hemoglobin with < 120g/L in male and < 110g/L in female patients”]) or 2.975*X5(anemia[value = 1 for “hemoglobin with <90g/L"]). Step 2: calculate Y2 where Y2 = ey1. Step 3: calculate probability of readmission, where Probability = Y2/(1 + Y2).
Fig. 1.

Nomogram predicting POD in elderly patients with FNF after hip replacement. To calculate a patient's possibility of POD, points for each parameter can be identified from corresponding values on the points axis and sum of the points was plotted on total points axis. The patient's possibility of POD is the value at a vertical line from the corresponding total points. POD = postoperative delirium.
Model Validation
The receiver operating characteristic curve was used to evaluate the discrimination of the regression equation. The area under the curve was 0.957, the 95% confidence interval was (0.938, 0.976), and p < 0.001. The calibration curve showed good agreement between the predictive risk and the actual probability (Figure 2). The Hosmer–Lemeshow x2 statistics was 11.13 (p = 0.195), suggesting there was no significant deviation.
Fig. 2.
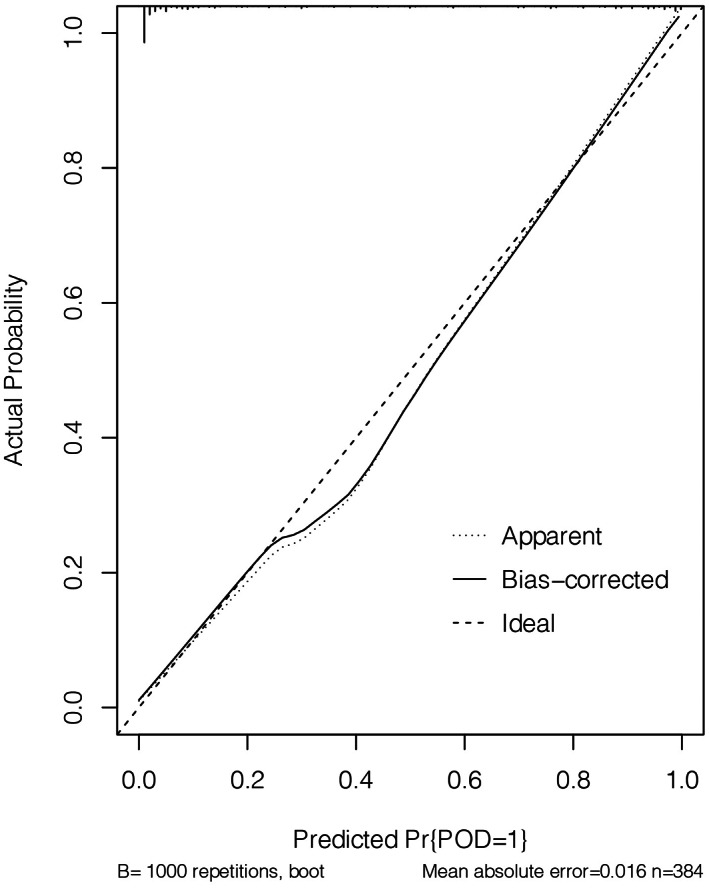
The calibration curve for the predicted probability of POD. A plot along the 45° line represents a perfect calibration model. The predicted probability is identical to the actual outcome. POD = postoperative delirium.
Discussion
Risk Factors for POD
FNF accounts for about 3.6% of the total body fracture, and its incidence is still increasing year by year 12 . For elderly patients with an obviously displaced FNF (Garden III and IV), the optimal procedure is hip replacement. POD is a common complication after FNF in elderly patients. Once it occurs, it can seriously affect the prognosis of patients. At present, the pathogenesis of POD is not yet clear. Related studies have shown that its pathophysiological mechanisms mainly include blood–brain barrier damage, vascular endothelial cell damage, reduction of cholinergic receptors, neuroinflammatory response, neurotransmitter disorders, and so forth 13 , 14 . This study showed that the incidence of POD in elderly patients with hip fracture was 33.33%, which was similar to the results reported by a previous study 9 .
In a National Inpatient Sample study, Yang et al 15 . demonstrated that independent risk factors of delirium following total joint arthroplasty included advanced age, neurological disorder, alcohol and drug abuse, depression, psychoses, fluid and electrolyte disorders, diabetes, weight loss, deficiency or chronic blood loss anemia, coagulopathy, metastatic cancer, hypertension, congestive heart failure, pulmonary circulation disorders, valvular disease, peripheral vascular disorders, and renal failure. The database only recorded patients before discharge, which may lead to bias in the assessment of postoperative delirium. Besides, only the variables provided in the NIS database could be included in the risk factor analysis, while the possible influencing factors such as anesthesia mode, perioperative drug use (opioids, benzodiazepines, and so forth), operation duration, preoperative hypoxemia, and blood transfusion volume could not be analyzed.
Advanced Age Increased the Risk of POD
Our study showed that advanced age, hemiarthroplasty, electrolyte imbalance, and anemia were risk factors for postoperative POD in elderly patients with hip fracture. Previous studies have pointed out that advanced age was considered a risk factor for delirium after hip replacement 9 , 10 , which was consistent with the results of this study. Analyzing the reasons, the increase of age could gradually reduce the synthesis of central acetylcholine, and the decrease of cholinergic neurotransmitters reserved in the central nervous system and the relative excess of dopaminergic neurotransmitters could cause delirium 16 . In addition, this may also be related to the fact that elderly patients often had more comorbidities, and compensatory ability and metabolic function remarkably declined.
Hemiarthroplasty Increased the Risk of POD
Patients who underwent hemiarthroplasty had a greater risk of delirium than those who underwent total hip arthroplasty. Elderly patients with FNFs who had a long life expectancy and a large amount of activity often underwent total hip replacement. Because the femoral head prosthesis cannot be completely matched with the bony acetabulum, the hemiarthroplasty was likely to cause acetabular wear, and postoperative pain was easy to appear after walking for a long time 17 . However, hemiarthroplasty was simple, with small surgical trauma and short surgical time, and the elderly patients in poor physical condition with low requirements for postoperative activities usually underwent this operation 18 , while those patients were high risk ones for POD. Therefore, hemiarthroplasty appeared to be an independent risk factor for POD.
Malnutrition and Anemia Increased the Risk of POD
Preoperative nutritional status was related to the occurrence of POD 19 . This study showed that patients with perioperative electrolyte imbalance and anemia were at greater risk of POD. Analysis of the reasons showed that electrolyte imbalance could easily cause central nervous system dysfunction. Some studies have pointed out that patients with electrolyte imbalance were prone to delirium. Sim et al. showed that preoperative anemia was associated with poorer physical function and quality of life after hip fracture surgery 20 . When complicated with anemia, the blood oxygenation and oxygen transport capacity decreased, so that the cerebral blood oxygen saturation was reduced, with decreased acetylcholine in the brain, and the incidence of POD increased 21 .
Limitations
Therefore, the establishment of a simple and effective scoring model to predict the risk of POD in elderly patients with FNFs was clinically meaningful. This study analyzed several factors that may be related to the occurrence of POD in elderly patients with FNFs, established a risk prediction equation, and proved that the model fits well through the ROC curve. The study still had some limitations. To begin with, its retrospective design and date retrieving may have led to bias. The study was conducted in a trauma center with strong academic background, conclusions derived from a single center may not apply to other hospitals, so a wide application of the model to different care settings should be validated. Moreover, temporal and geographical validation was further needed to warrant its practicality.
Conclusions
In conclusion, we developed and validated a nomogram incorporating age, surgery type, preoperative electrolyte condition, and hemoglobin level to predict the probability of POD in FNF patients after hip replacement. This nomogram included easily accessible demographics and clinical parameters and may facilitate enhanced recovery after surgery among FNF patients.
Author Contributions
Bingbing Li and Jiabao Ju processed the data and wrote the manuscript. Jiaying Zhao and Ying Qin collected data and reviewed the manuscript. Yan Zhang designed the study and revised the manuscript.
Funding Information
This work was supported by National Center for Trauma Medicine and Key Laboratory of Trauma and Neural Regeneration, Ministry of Education.
Conflict of Interest
None declared.
Bingbing Li and Jiabao Ju are Co‐first authors
Authorship declaration: All authors listed meet the authorship criteria and are in agreement with the manuscript.
References
- 1. Jianbo J, Ying J, Xinxin L, Lianghao W, Baoqing Y, Rongguang A. Hip hemiarthroplasty for senile femoral neck fractures: minimally invasive SuperPath approach versus traditional posterior approach[J]. Injury. 2019;50(8):1452–9. [DOI] [PubMed] [Google Scholar]
- 2. Miller BJ, Callaghan JJ, Cram P, Karam M, Marsh JL, Noiseux NO. Changing trends in the treatment of femoral neck fractures: a review of the american board of orthopaedic surgery database[J]. J Bone Joint Surg Am. 2014;96(17):e149. [DOI] [PubMed] [Google Scholar]
- 3. Greenstein AS, Gorczyca JT. Orthopedic surgery and the geriatric patient[J]. Clin Geriatr Med. 2019;35(1):65–92. [DOI] [PubMed] [Google Scholar]
- 4. Pincus D, Ravi B, Wasserstein D, Huang A, Paterson JM, Nathens AB, et al. Association between wait time and 30‐day mortality in adults undergoing hip fracture surgery[J]. Jama. 2017;318(20):1994–2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jin Z, Hu J, Ma D. Postoperative delirium: perioperative assessment, risk reduction, and management[J]. Br J Anaesth. 2020;125(4):492–504. [DOI] [PubMed] [Google Scholar]
- 6. Marcantonio ER. Delirium in Hospitalized Older Adults[J]. N Engl J Med. 2017;377(15):1456–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Reddy SV, Irkal JN, Srinivasamurthy A. Postoperative delirium in elderly citizens and current practice[J]. J Anaesthesiol Clin Pharmacol. 2017;33(3):291–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zywiel MG, Hurley RT, Perruccio AV, Hancock‐Howard RL, Coyte PC, Rampersaud YR. Health economic implications of perioperative delirium in older patients after surgery for a fragility hip fracture[J]. J Bone Joint Surg Am. 2015;97(10):829–36. [DOI] [PubMed] [Google Scholar]
- 9. Yang Y, Zhao X, Dong T, Yang Z, Zhang Q, Zhang Y. Risk factors for postoperative delirium following hip fracture repair in elderly patients: a systematic review and meta‐analysis[J]. Aging Clin Exp Res. 2017;29(2):115–26. [DOI] [PubMed] [Google Scholar]
- 10. Kim EM, Li G, Kim M. Development of a risk score to predict postoperative delirium in patients with hip fracture[J]. Anesth Analg. 2020;130(1):79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The confusion assessment method: a systematic review of current usage[J]. J Am Geriatr Soc. 2008;56(5):823–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Florschutz AV, Langford JR, Haidukewych GJ, Koval KJ. Femoral neck fractures: current management[J]. J Orthop Trauma. 2015;29(3):121–9. [DOI] [PubMed] [Google Scholar]
- 13. Hshieh TT, Inouye SK, Oh ES. Delirium in the elderly[J]. Clin Geriatr Med. 2020;36(2):183–99. [DOI] [PubMed] [Google Scholar]
- 14. Lakstygal AM, Kolesnikova TO, Khatsko SL, Zabegalov KN, Volgin AD, Demin KA, et al. DARK classics in chemical neuroscience: atropine, scopolamine, and other anticholinergic Deliriant hallucinogens[J]. ACS Chem Nerosci. 2019;10(5):2144–59. [DOI] [PubMed] [Google Scholar]
- 15. Qinfeng Y, Jian W, Yang Z, et al. Incidence and risk factors of postoperative delirium following total joint arthroplasty based on USA Nationwide inpatient sample[J]. Chin J Joint Surg(Electronic Edition). 2021;15(1):57–63. [Google Scholar]
- 16. Wang Y, Shen X. Postoperative delirium in the elderly: the potential neuropathogenesis[J]. Aging Clin Exp Res. 2018;30(11):1287–95. [DOI] [PubMed] [Google Scholar]
- 17. Rogmark C, Leonardsson O. Hip arthroplasty for the treatment of displaced fractures of the femoral neck in elderly patients[J]. Bone Joint J. 2016;98:291–7. [DOI] [PubMed] [Google Scholar]
- 18. Liu Y, Chen X, Zhang P, Jiang B. Comparing total hip arthroplasty and hemiarthroplasty for the treatment of displaced femoral neck fracture in the active elderly over 75 years old: a systematic review and meta‐analysis of randomized control trials[J]. J Orthop Surg Res. 2020;15(1):215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Huisman MG, Veronese G, Audisio RA, Ugolini G, Montroni I, de Bock GH, et al. Poor nutritional status is associated with other geriatric domain impairments and adverse postoperative outcomes in onco‐geriatric surgical patients–a multicentre cohort study[J]. Eur J Surg Oncol. 2016;42(7):1009–17. [DOI] [PubMed] [Google Scholar]
- 20. Sim YE, Sim SD, Seng C, Howe TS, Koh SB, Abdullah HR. Preoperative anemia, functional outcomes, and quality of life after hip fracture surgery[J]. J Am Geriatr Soc. 2018;66(8):1524–31. [DOI] [PubMed] [Google Scholar]
- 21. European Society of Anaesthesiology evidence‐based and consensus‐based guideline on postoperative delirium: erratum[J]. Eur J Anaesthesiol. 2018;35(9):718–9. [DOI] [PubMed] [Google Scholar]


