Abstract
Background
Telelactation, a virtual lactation support platform, is a convenient and effective way of providing virtual breastfeeding support services and communicating proper breastfeeding techniques to new mothers to address any breastfeeding challenges and boost overall maternal breastfeeding confidence all from the comfort of their homes. This Ontario Health Insurance Plan (OHIP) covered service benefits more mothers in the remote areas where in-person LC service is not easily accessible.
Objective
The objective of this cross-sectional survey study is to explore the feasibility, potential benefits, and challenges, and level of patient satisfaction in virtual lactation consultation services along with virtual paediatrician consultation available in Ontario, Canada.
Method
Patient satisfaction was assessed using a structured online survey as a part of a cross-sectional observational study that asked questions relevant to several independent demographic variables as well as specific Likert type scale questions to gauge patient satisfaction with virtual lactation consultation.
Results
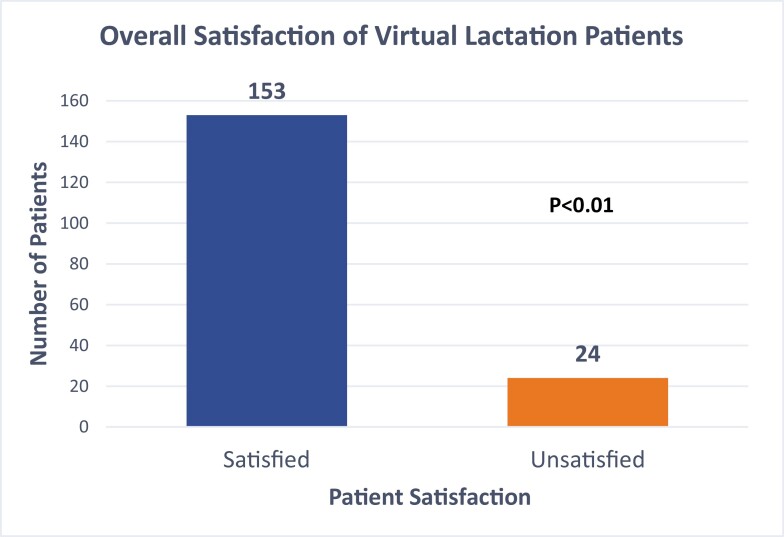
Data were analyzed from 177 survey responses (n=177), of which study revealed that 86.44% (153/177) were satisfied with the virtual lactation services they received. Patient satisfaction was found to be higher in the first-time mothers with high school or undergraduate education between the age group of 26 to 35 years living in the Greater Toronto Area (GTA). In terms of connectivity, participants from the GTA had a better experience overall compared those living outside the GTA.
Conclusion
OHIP covered telelactation with a paediatrician consultation is an innovative and feasible health care delivery platform for providing remote professional breastfeeding support to mothers of all socio-economic strata with great potential to further improve both patient experience and efficiency in patient care.
Keywords: Delivery of health care, Lactation consultation, Patient satisfaction, Remote professional support, Telelactation
Breastfeeding is generally recognized as the best diet for newborns; however, it is not without challenges. Many new mothers stop breastfeeding earlier than recommended because of inadequate guidance and professional support. Studies indicate that the primary causes of premature cessation of breastfeeding are insufficient milk production and feeding difficulties, including problems with latching, and sucking (1,2). A virtual lactation service aims to address these concerns and enhance the breastfeeding process by providing mothers with one-on-one video consultations on their personal devices (3,4). Several health care professionals can provide breastfeeding support to women, but International Board-Certified Lactation Consultants (IBCLCs) specialize in this work (1). Lactation support experts have varied levels of training and experience, topped by IBCLCs who have completed 95 hours of lactation-specific education, 14 health science courses, and over 500 clinical hours (5). However, IBCLCs are difficult to access due to a number of barriers, including limited numbers of local IBCLCs, expense, and inconvenience to both mothers and their babies. Additionally, COVID-19 social distancing restrictions further limit access to IBCLCs (2).
Telemedicine allows health care to be delivered remotely using electronic services (6). Through virtual lactation services, breastfeeding mothers can have convenient access to professional lactation support (3,4). Online video conferencing is regarded as the best form of telemedicine (3), as it is cost-effective, convenient, and allows most IBCLCs to be accessed nationally (4,7). However, online services may not be readily available in rural areas due to inadequate internet infrastructure. Additionally, individuals may find the video software difficult to use, and connectivity issues can disrupt consultations. Some patients may also not establish the same level of trust with their health care providers virtually (8), affecting patient satisfaction and the acceptability of online lactation support.
This survey aims to identify some of the potential benefits and challenges of online lactation consultation services. We will also explore how the presence of a paediatrician, as well as demographic factors like education, geographic location, and age can influence maternal satisfaction.
In Ontario, outpatient lactation consultation services are not publicly funded. Mothers who require consultation outside that provided shortly after delivery must pay out of pocket or use private insurance for these services, which can be up to $200 for an in-person home visit. Mothers of lower socioeconomic status with breastfeeding difficulties may therefore be reluctant to pursue these services. In response to the prevalence of breastfeeding, this virtual breastfeeding consultation service was established. This affordable virtual breastfeeding consultation service pairs a lactation consultant with a paediatrician in order to not only provide a fully OHIP covered service, but also allow for paediatrician management for complicated lactation difficulties.
METHODS
Background
Ontario residents who requires breastfeeding support can access this service without a referral. A stable internet connection and a device to run Ontario Telemedicine Network (OTN) is required to access this service. During a virtual consultation, the lactation consultant takes history, performs a breastfeeding assessment and guides mothers on breastfeeding technique and latch positions along with counselling. Paediatrician joins in during the second half of every visit, to perform a general assessment and discuss management plans. Infants are seen by the paediatrician only for that visit, they usually follow-up with their primary care physician or their paediatrician in their community for check-ups.
Design
This cross-sectional observational study conducted in Ontario, Canada uses an online survey to assess patient satisfaction with various aspects of online lactation consultations, including technical difficulties, three-way communication between a mother, a lactation consultant and a paediatrician, convenience and cost effectiveness. The Institutional Review Board’s Ethical approval was obtained through Brantford Pediatrics prior to initiating the study.
Literature review
A literature review was conducted, for which the research problem was formulated, followed by development of a review protocol. We identified relevant articles by conducting a search of PubMed, MEDLINE, Scopus, Embase (OvidSP), and Cochrane databases. We used both subject headings and text word terms for telemedicine and lactation. We excluded letters, editorials and general review articles. Only articles published within the last 10 years written in English were included, to provide up to date background information regarding virtual lactation consultations.
Sampling
Convenience sampling was employed for this study. The eligibility criteria included women who had at least one online lactation consultation visit throughout the duration of the study (October 21, 2020 to April 21, 2021), lived in Ontario, and had provided their emails. Of the 250 eligible women who were emailed the survey after their visit, 177 (71%) responded. Participants were reminded twice by email to complete the survey; 1 to 2 weeks after their appointment and during their follow-up appointment.
Sample size calculation
To test for a statistically significant difference between the proportion of satisfied and unsatisfied respondents, we used the chi-square ‘goodness of fit’ test with a significance level of 0.05 and an error margin of 8%. From these specifications, we calculated the sample size to be 152 patients.
Measurements
The demographic data collected included maternal age, highest level of education, parity, the online video application used during the consultation, any prior consultation visits, and place of residence in Ontario. Finally, data were extracted, analyzed, and synthesized to report the findings. Survey questions were developed that could appropriately assess patient satisfaction with online lactation consultations (Supplementary Appendix 1).
A 5-point Likert scale was used to record the responses of participants, in which the 5 points represented: (1) Strongly disagree; (2) Disagree; (3) Neutral; (4) Agree; and (5) Strongly agree.
Data collection
Data were collected using a secure online survey program called Cognito Forms. All participants provided informed consent prior to the completion of the survey.
Data analysis
The data were transferred to an excel spreadsheet and were analyzed using the Python3 programming language, with the Scipy package for statistical tests and the Statsmodels package for Logistic regression. For each survey question, a participant was considered satisfied if she either chose to agree (4 points) or strongly agree (5 points) on the Likert scale. Otherwise, the participant was considered unsatisfied. In terms of overall satisfaction, the sum of responses to all the questions were considered. The total score was 50, so a participant was considered satisfied if she scored 40, corresponding to answering agree (4 points) on all the questions, or higher. To evaluate the relationship between a demographic variable and the participant’s satisfaction with online lactation consultation, a logistic regression, using the software package Statsmodels, was run. If a participant’s sum of ratings on the Likert scale was >40, they were considered to have had a satisfied experience while those with a sum of ratings <40 were considered to have had an unsatisfying experience. The chi-square test was employed using a P-value <0.05 for each of the individual questions as well as for overall satisfaction to check whether the difference between the satisfied and unsatisfied groups was statistically significant.
RESULTS
Demographics
Participant demographic characteristics are presented in Table 1. The majority of participants were 26 to 35 years old, with an undergraduate degree or higher, had at least one child, participated in a virtual consultation for the first time, and resided outside the Greater Toronto Area (GTA).
Table 1.
Demographic characteristics of the participants
| Characteristic | Count (n=177) |
|---|---|
| Age (years) | |
| <20 | 1 |
| 20–25 | 9 |
| 26–30 | 62 |
| 31–35 | 79 |
| >35 | 26 |
| Education level | |
| Elementary School | 0 |
| High School | 3 |
| Undergraduate | 99 |
| Graduate/Post Graduate | 75 |
| Number of children | |
| 1 | 134 |
| 2 | 33 |
| 3 | 9 |
| 4 | 1 |
| ≥5 | 0 |
| Prior virtual consultation experience | |
| Yes | 79 |
| No | 98 |
| Area of residence | |
| Within the Greater Toronto Area (GTA) | 81 |
| Outside the GTA | 96 |
| Telemedicine Application Used | |
| Ontario Telemedicine Network (OTN) Desktop | 136 |
| Infinity connect (OTN mobile app) | 30 |
| Zoom | 8 |
| Other | 3 |
Independent variables that predict participants’ satisfaction
Results of the logistic regression to predict participants’ satisfaction using their demographics are presented in Table 3. We calculated the logistic regression coefficient for the categorical variable of ‘education level’ to be 1.1589 (Table 3). This shows that only the participant’s education level has a statistically significant relationship with the level of satisfaction. Compared to participants with postgraduate education, participants with high school or undergraduate level of education showed a significantly higher level of satisfaction. The odds of a patient being satisfied increase by 3.18 times if the patient’s highest education is high school or undergraduate. The data of this survey shows that the following three factors have the greatest impact on the satisfaction levels of mothers in the two education groups: ease of making an appointment, maintenance of confidentiality, and paediatrician involvement (Figure 2). Moreover, participants living in the Greater Toronto Area and individuals in their late 20’s or early 30’s also shows higher satisfaction levels, but the relationship was not statistically significant.
Table 3.
Relationship between variables that predict lactation consult patient satisfaction
| Variable | Coefficient (Std Error) | Odds ratio | Odds ratio 95% Conf. Interval |
|---|---|---|---|
| Age | −0.4383 (0.441) | 0.6451 | [0.2718, 1.5312] |
| Education Level* | 1.1589 (0.464) | 3.1864 | [1.2833, 7.9117] |
| Number of Children | 0.0441 (0.508) | 1.0451 | [0.3861, 2.8286] |
| Prior Virtual Consultation Experience | 0.3526 (0.452) | 1.4228 | [0.5867, 3.4505] |
| Area of Residence | 0.6771 (0.446) | 1.9682 | [0.8211, 4.7174] |
P=0.05
•Education level coefficient represents effect of having highest education as High school/ Undergraduate versus having highest education as Postgraduate.
•Area of residence coefficient represents effect of residing in GTA versus residing outside the GTA.
Figure 2.
The three questions that showed highest disparity in maternal satisfaction between HS/Undergraduate education level and Graduate or above education level. The three questions from the survey: #1 Ease of making an appointment, #8 Maintenance of confidentiality, and #9 Paediatrician’s involvement.
This study found that 79% (P<0.01) of parents found paediatrician involvement during virtual consultation to be helpful (Table 4). The desktop version of the OTN application was used by 136 out of 177 (76.83%) participants for video conferencing, out of which 11% had trouble in either video, audio or both (Table 1). Zoom was used by 8 out of 177 (4.52%) participants for video conferencing, of which 25% had similar issues, while 30 out of 177 (16.95%) participants used other applications and only 6% had technical issues (Table 1). The other application as mentioned by participants is mainly Infinity Connect which is the cellular app version of OTN. Participants from outside the GTA contributed to 54.23% of the participants, in which 14.5% experienced technical difficulties (Table 1). 45.76% of the participants were from the GTA and only 8.75% experienced technical difficulties (implications of these have been discussed in the next section).
Table 4.
Proportion of satisfied and unsatisfied participants in responses to individual questions/statements
| Individual category | #Satisfied (%) | # Unsatisfied (%) | df | Chi-square test value | Probability |
|---|---|---|---|---|---|
| Ease of making an appointment | 166 (93.8) | 11 (6.2) | 1 | 135.734 | <0.001 |
| Waiting time | 169 (95.5) | 8 (4.5) | 1 | 146.446 | <0.001 |
| Lack of Technical Difficulties | 134 (75.6) | 43 (24.4) | 1 | 46.785 | <0.001 |
| Consultation time duration | 176 (99.4) | 1 (0.6) | 1 | 173.023 | <0.001 |
| Professionalism | 175 (98.9) | 2 (1.1) | 1 | 169.090 | <0.001 |
| Lactation Consultant Guidance | 170 (96) | 7 (4) | 1 | 150.107 | <0.001 |
| Time and cost effectiveness | 160 (90.4) | 17 (9.6) | 1 | 115.531 | <0.001 |
| Maintenance of Confidentiality | 168 (94.9) | 9 (5.1) | 1 | 142.831 | <0.001 |
| Paediatrician’s Involvement | 140 (79) | 37 (21) | 1 | 59.938 | <0.001 |
| Would Recommend Online Consultation | Likely: 149 (84.1) | Unlikely: 28 (15.9) | 1 | 82.718 | <0.001 |
With regards to feedback to further improve the online lactation consultation experience, the majority of participants (98.9%) were grateful that the lactation consultants adapted their counselling strategies with the help of visual aids like breastfeeding dolls and crochet breasts. Up to 96% of parents appreciated not only the lactation consultant’s knowledge and experience but also their patience and kindness. Overall, 101 out of 177 participants agreed that virtual consultation is an accessible form of health care, as they connected from the comfort of their own homes. Twenty out of 177 participants also stated that virtual consultation was an appropriate option to ensure safety during the COVID-19 pandemic.
DISCUSSION
This study investigated patient satisfaction by conducting a survey in a video conference-based clinic with three-way communication between mother, a lactation consultant and a paediatrician in the same visit. Parents received holistic health care from their own home, while also having the opportunity to ask questions about feeding, starting solids, bowel movements, neonatal rash, oral thrush, normal infant development, and many other topics concerning new parents. According to the results of this survey, 153 out of 177 participants (86.44%) were satisfied overall (Figure 1), based on their responses to 10 statement questions that were statistically significant for satisfaction (Table 2), correlating with Habibi et al.’s findings (9). Most in-person appointments have long wait times that can disrupt a baby’s feeding or sleeping schedule, demotivating parents to attend non-urgent care clinics. In-person clinic visits require parents to take time off from work, making the process overwhelming for sleep-deprived new parents (10). Although appointments with the lactation consultant and paediatrician pair are covered by OHIP in Ontario, the hidden cost of parking, which increases with long wait times, as well as the fear of COVID-19 exposure, can deter new mothers from utilizing in person lactation consultation services.
Figure 1.
Proportion of satisfied and unsatisfied virtual lactation patients.
Table 2.
Chi-Square relationship of satisfied and unsatisfied virtual lactation patients
| # Satisfied | # Unsatisfied | df | χ2 | P value |
|---|---|---|---|---|
| 153 | 24 | 1 | 94.02 | <0.01 |
Our study found that a fair degree of satisfaction was seen in first time mothers between age 26-35, with high school or undergraduate degree in the Greater Toronto Area (GTA), who used virtual consultations for the first time. Maternal education was the only statistically significant variable (Table 3), with higher reported satisfaction by the participants whose highest education level was high school or undergraduate degree, compared to those whose highest education was a post-graduate degree. In our study 96.08 % of mothers who completed high school and undergraduate studies are satisfied, in comparison to only 82.67% of mothers who completed post-graduate education. This study agrees with the work conducted by Wallin et al., who found that patients with university education were least satisfied, while those with compulsory education were most satisfied (11). This discrepancy may be due to the pedagogical nature of lactation consulting services; mothers with higher education may have more basic knowledge about lactation overall and hence consultation with an LC may not have as much added value to their experience compared to less educated mothers.
On acceptance of technology, a study conducted by Ifinedo found an association between higher educational attainment and acceptance of technology in a health care setting (12). In another study by Mlikotic et al., women with higher educational levels participated more in website platform questionnaires (13). Maternal education level plays a crucial role in how clients comprehend advice given through a relatively new form of counselling platform.
The following three aspects of online consultation had the greatest disparity in satisfaction across education levels: ease of making an appointment, maintenance of confidentiality, and paediatrician’s involvement (Figure 2). Few mothers felt they did not need to see paediatricians at a follow-up appointment; they did not know that the virtual lactation framework at this clinic requires a paediatric consult at every visit to provide OHIP covered service. Therefore, the structure of the visit should be well outlined to the mothers, highlighting that a paediatrician will be joining the call during every single visit. Effective measures can improve communication, like giving an advance notice just prior to the appointment or a quick reminder before a paediatrician joins the call, especially if a male paediatrician is about to join the appointment if the mother is still practicing breastfeeding. In terms of confidentiality, participants should sign an online consent form detailing the privacy policies prior to their virtual online sessions and are therefore aware about operating platform’s security. However, a few mothers still felt uncomfortable breastfeeding in front of the camera. A verbal reassurance about confidentiality and the internet security of the application at the beginning of the consultation would strengthen their sense of safety and help them better understand privacy. Another recommended measure is to reduce the burden on the already overwhelmed mothers by simplifying the appointment booking process.
The unique aspect of this study is the collaboration between a paediatrician and a lactation consultant for a virtual lactation appointment. Parents often kept a list of questions ready for the paediatrician, mainly related to baby’s feed, reflux, sleep, bowel frequency or color, rash, teething, weight gain concerns, starting solids and readiness, growth and development. Getting their questions answered by a paediatrician not only gave reassurance, especially to concerned first time parents, but also makes this service completely OHIP covered. Affordability plays an important role for new parents who are already spending a significant amount of money on newborn care. The subject of reimbursement challenges with remote monitoring has been addressed in study by Serper et al. (14). Mothers are encouraged to attend OHIP covered follow-up sessions to continue practicing breastfeeding and get an assessment done at each visit along with seeing a paediatrician for baby related queries. Often, if requested, these services are made available over the weekends and statutory holidays, giving much needed support with lactation, as well as a paediatric consult, which otherwise may not be accessible. Lactation consultants in our setting typically get referrals from their community and the majority of LCs who distributed surveys to their clients were from outside GTA. Therefore, most of the participants in our study were from suburban and rural areas of Ontario who have relatively lesser access to in-person LC services. Hence our OHIP covered service serves the less privileged people the most.
Many mothers felt that the virtual consultation provided them with the same experience as an in-person consultation as they received one-on-one professional support. In contrast to Hale et al., who states that concerns about privacy and security of telehealth system may adversely affect people’s trust in telehealth and threaten the ability of effectiveness of health care, our study found that participants were able to establish a good rapport with their lactation consultant (8). Participants’ satisfaction was evident by the positive 5-star reviews given on social media platforms for their respective lactation consultant and adherence to their service through follow-up appointments. Following the pattern found in Boudreaux et al., parents felts more satisfied with efficient empathetic communication too in our study by LCs and paediatricians (15). While 84.1% of participants said they would recommend virtual consultation visits to family and friends, further research is needed to elucidate how regular follow-ups affect the duration and willingness of mothers to breastfeed (Table 4).
Many participants were glad that they could save time with virtual consultations as they could avoid travel to the health care clinic, traffic, wait times, and parking costs. These results are supported by an article by JM Kahn, who states that telemedicine reduces travel expenses and costs associated with obtaining care, such as missed hours or days of work (10). A recent study by Tenforde et al. found a high level of patient satisfaction during telehealth visits during the COVID-19 pandemic since female caregivers, who balance work and childcare, had shorter wait times (16).
The application Infinity Connect mentioned by the participants seems to have better customer satisfaction in terms of audio, video, and connectivity. Results of our study suggest that urban centres had better connectivity when compared to regions outside the GTA. This is an issue for suburban and rural areas as poor network connectivity can cause audio or video issues, which are some of the technical issues encountered by mothers of these geographical areas (17). For these reasons, many participants in rural regions must use their limited cellular data for these appointments. Having an application which can function as effectively in rural areas of Ontario as other applications do in the GTA/urban areas will encourage participants from all regions of Ontario to benefit from online lactation counselling.
In our study, 56 participants felt no improvement is needed to the current consultation practice, confirming that the online consultation platform is satisfactory. As observed in other literature, such as in a study by Habibi et al., use of technology such as virtual consultation for lactation support was found to be satisfactory to mothers (18). However, there were 18 participants who preferred other platforms for video conferencing due to connection issues while 17 participants expressed that the audio-video quality could have been better. There were eight mothers who identified limitations to virtual consultations. Firstly, an online consultation limits the hands-on aspect of the demonstration of breastfeeding techniques, which could appear complex to first time mothers. An increased reliance on verbal explanations have been noted during online consultations, which may not be adequate to demonstrate latching techniques to first-time parents. Another challenge is a mother’s ability to angle the camera while practicing latching techniques so that the LC can see the latch properly to guide accordingly, especially if she is alone with her baby for her appointment. A few participants stated that thorough communication prior to an online session would have prepared them better: perhaps by receiving written instructions to go over beforehand. Eight mothers stated that they benefited from the online virtual consultation but felt the need for longer initial appointments along with more time for questions at the end of the session, with frequent follow-ups.
Virtual consultation can be made accessible to patients in lower socio-economical demographics by collaborating with a local public health care centre, where patients can have access to a device with stable internet to have a virtual breastfeeding consultation. Patients who either do not have access to internet or literacy to use a required device can be helped by a community family physician who can have clinic hours in their office for mothers to access a device for these consultations. This study brings up the question of effectiveness of virtual breastfeeding services. Further study is required to compare this with in-person consultation to measure its effectiveness. Moreover, data can be collected by follow-ups to find out the percentage of mothers benefiting from the lactation consultation and a comparison can be done to understand to what degree their breastfeeding experience improved after lactation consultation.
CONCLUSION
Virtual lactation consultation is an innovation in the delivery of professional breastfeeding support. This research validates a positive experience with virtual consultation for lactation in the presence of a paediatrician for expert opinions, alongside an IBCLC. Maternal educational level indicated the strongest predictive value for patient satisfaction, with higher patient satisfaction being associated with a lower education level. First time mothers in their late 20s and early 30s were more inclined to invest in breastfeeding support through virtual platforms. While better connectivity in urban areas facilitated parents to enjoy the full duration of their virtual lactation consultation session without any technical interference, we recommend simpler web application that runs efficiently on lower internet bandwidth so that similar access to care could be offered to parents living in suburban and rural areas of Ontario who have relatively lesser access to in-person LC services. Since OHIP covered virtual lactation service provides breastfeeding support to mothers of lower socio-economic demographics who would otherwise not be able to access in-person LC service due to affordability, we propose an increase in such platforms to be considered.
Supplementary Material
ACKNOWLEDGEMENTS
The authors gratefully thank Lactation Consultants at the Ontario Breastfeeding Network who helped in survey distribution.
Contributor Information
Muhammad Akhter Hamid, Assistant Professor, Department of Pediatrics, University of Toronto, Toronto, Ontario, Canada.
Anubha Kumar, Research Director, Ontario Breastfeeding Clinic, Ontario, Canada.
Luxhman Gunaseelan, Saba University School of Medicine, Toronto, Ontario, Canada.
Atchaya Arulchelvan, Medical Student, University of Buckingham, Buckingham, UK.
Abhinav Sinha, Decision, Risk, and Operations (DRO) Division, Graduate School of Business, Columbia University, New York, USA.
Sidra Razi, Xavier School of Medicine, Oranjestad, Aruba.
Muzhda Subhan, Department of Internal Medicine, Washington University in Saint Louis, St Louis, Missouri, USA.
Sarah Subhan, Department of Internal Medicine, Westchester Medical Center, Valhalla, New York, USA.
Suruchi Kapoor, Government Medical College Kozhikode, Kozhikode, India.
Asim Salim, Assistant Professor, Department of Pediatrics, McMaster University, Hamilton, Ontario, Canada.
FUNDING
There are no funders to report.
POTENTIAL CONFLICTS OF INTEREST
All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
REFERENCES
- 1. Weltgesundheitsorganisation, ed. Global Strategy for Infant and Young Child Feeding. WHO; 2003. [Google Scholar]
- 2. Canada PHA. Chapter 6: Breastfeeding. aem. Published October 5, 2018. Accessed October 31, 2020. https://www.canada.ca/en/public-health/services/publications/healthy-living/maternity-newborn-care-guidelines-chapter-6.html [Google Scholar]
- 3. DaMota K, Bañuelos J, Goldbronn J, Vera-Beccera LE, Heinig MJ.. Maternal request for in-hospital supplementation of healthy breastfed infants among low-income women. J Hum Lact 2012;28:476–82. [DOI] [PubMed] [Google Scholar]
- 4. Uscher-Pines L, Mehrotra A, Bogen DL.. The emergence and promise of telelactation. Am J Obstet Gynecol 2017;217:176–8.e1. [DOI] [PubMed] [Google Scholar]
- 5. Feinstein J, Eric JS, Henry HB.. Telehealth can promote breastfeeding during the Covid-19 pandemic. NEJM Catalyst Innovations in Care Delivery. doi: 10.1056/CAT.21.0076 [DOI] [Google Scholar]
- 6. Ahluwalia IB, Morrow B, Hsia J.. Why do women stop breastfeeding? Findings from the pregnancy risk assessment and monitoring system. Pediatrics 2005;116:1408–12. [DOI] [PubMed] [Google Scholar]
- 7. Morris CA, Gutowski JL.. The effect of an international board certified lactation consultant in the pediatric primary care setting on breastfeeding duration and exclusivity during the first year of life. Clinical Lactation. 2015;6:109–16. [Google Scholar]
- 8. Hale TM, Kvedar JC.. Privacy and security concerns in telehealth. Virtual Mentor. 2014;16(12):981–5. [DOI] [PubMed] [Google Scholar]
- 9. Habibi MF, Springer CM, Spence ML, Hansen-Petrik MB, Kavanagh KF.. Use of videoconferencing for lactation consultation: An online cross-sectional survey of mothers’ acceptance in the United States. J Hum Lact. 2018;34:313–21. [DOI] [PubMed] [Google Scholar]
- 10. Kahn JM. Virtual visits--confronting the challenges of telemedicine. N Engl J Med 2015;372:1684–5. [DOI] [PubMed] [Google Scholar]
- 11. Wallin E, Lundgren P-O, Ulander K, Staël von Holstein C.. Does age, gender or educational background effect patient satisfaction with short stay surgery? Ambulatory Surgery. 2000;8:79–88. [Google Scholar]
- 12. Ifinedo P. The moderating effects of demographic and individual characteristics on nurses’ acceptance of information systems: A Canadian study. Int J Med Inform 2016;87:27–35. [DOI] [PubMed] [Google Scholar]
- 13. Mlikotic R, Parker B, Rajapakshe R.. Assessing the effects of participant preference and demographics in the usage of web-based survey questionnaires by women attending screening mammography in British Columbia. J Med Internet Res 2016;18(3):e70. doi: 10.2196/jmir.5068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Serper M, Volk ML.. Current and future applications of telemedicine to optimize the delivery of care in chronic liver disease. Clin Gastroenterol Hepatol 2018;16:157–61.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Boudreaux ED, Ary RD, Mandry CV, McCabe B.. Determinants of patient satisfaction in a large, municipal ED: The role of demographic variables, visit characteristics, and patient perceptions. Am J Emerg Med 2000;18:394–400. [DOI] [PubMed] [Google Scholar]
- 16. Tenforde AS, Borgstrom H, Polich G, et al. Outpatient physical, occupational, and speech therapy synchronous telemedicine. Am J Phys Med & Rehabil. 2020;99(11):977–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Demirci J, Kotzias V, Bogen DL, Ray KN, Uscher-Pines L.. Telelactation via mobile app: Perspectives of rural mothers, their care providers, and lactation consultants. Telemed J E Health 2019;25:853–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Habibi MF, Nicklas J, Spence M, Hedberg S, Magnuson E, Kavanagh KF.. Remote lactation consultation: A qualitative study of maternal response to experience and recommendations for survey development. J Hum Lact 2012;28:211–7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.