Abstract
An important step towards the development of treatments for cognitive impairment in ageing and neurodegenerative diseases is to identify genetic and environmental modifiers of cognitive function and understand the mechanism by which they exert an effect. In Huntington’s disease, the most common autosomal dominant dementia, a small number of studies have identified intellectual enrichment, i.e. a cognitively stimulating lifestyle and genetic polymorphisms as potential modifiers of cognitive function. The aim of our study was to further investigate the relationship and interaction between genetic factors and intellectual enrichment on cognitive function and brain atrophy in Huntington’s disease. For this purpose, we analysed data from Track-HD, a multi-centre longitudinal study in Huntington’s disease gene carriers and focused on the role of intellectual enrichment (estimated at baseline) and the genes FAN1, MSH3, BDNF, COMT and MAPT in predicting cognitive decline and brain atrophy. We found that carrying the 3a allele in the MSH3 gene had a positive effect on global cognitive function and brain atrophy in multiple cortical regions, such that 3a allele carriers had a slower rate of cognitive decline and atrophy compared with non-carriers, in agreement with its role in somatic instability. No other genetic predictor had a significant effect on cognitive function and the effect of MSH3 was independent of intellectual enrichment. Intellectual enrichment also had a positive effect on cognitive function; participants with higher intellectual enrichment, i.e. those who were better educated, had higher verbal intelligence and performed an occupation that was intellectually engaging, had better cognitive function overall, in agreement with previous studies in Huntington’s disease and other dementias. We also found that intellectual enrichment interacted with the BDNF gene, such that the positive effect of intellectual enrichment was greater in Met66 allele carriers than non-carriers. A similar relationship was also identified for changes in whole brain and caudate volume; the positive effect of intellectual enrichment was greater for Met66 allele carriers, rather than for non-carriers. In summary, our study provides additional evidence for the beneficial role of intellectual enrichment and carrying the 3a allele in MSH3 in cognitive function in Huntington’s disease and their effect on brain structure.
Keywords: Huntington’s disease, brain-derived neurotrophic factor, intellectual enrichment, MSH3, cognitive modifiers
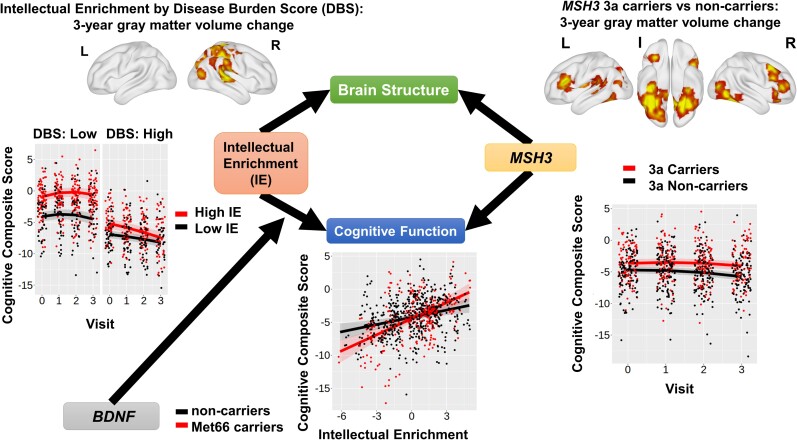
Papoutsi et al. showed that cognitive function in Huntington’s disease is affected by an interplay between genetic and environmental factors. 3a allele carriers had slower cognitive decline and cortical atrophy. In addition, high intellectual enrichment predicted slower cognitive decline and counteracted the detrimental effect of the Met66 allele in brain-derived neurotrophic factor.
See Hannan (https://doi.org/10.1093/braincomms/fcac308) for a scientific commentary on this article.
Graphical Abstract
Graphical abstract.
See Hannan (https://doi.org/10.1093/braincomms/fcac308) for a scientific commentary on this article.
Introduction
Huntington’s disease is a genetic, neurodegenerative disorder caused by an abnormal coronary artery angiography (CAG) repeat expansion in the Huntingtin (HTT)gene. It is characterized by a triad of symptoms, motor, psychiatric and cognitive. All Huntington’s disease gene carriers will eventually develop dementia,,1 but there is substantial variability in its onset and severity, which cannot be explained fully by CAG repeat length and age. Cognitive impairment is present in Huntington’s disease gene carriers many years before predicted disease onset and in the absence of motor symptoms.2 However, research on the genetic and environmental factors that contribute to this variability in cognitive impairment in Huntington’s disease is still limited.
Individual differences in cognitive function and rate of decline have been extensively studied in ageing and Alzheimer’s disease. One prominent hypothesis is that of brain maintenance,3 according to which the primary determinant of preserved cognitive function is lower levels of pathology and a slower rate of neurodegeneration. However, it has also been observed that individual differences in cognitive impairment exist despite similar levels of neurodegeneration, which led to the theory of cognitive reserve.4 Although the genetic and environmental factors that support brain maintenance and cognitive reserve in ageing and dementia are not all known, lifelong participation in intellectual activities, also known as intellectual enrichment,5 as well as genetic polymorphisms,6 have been associated with preserved cognitive function and mechanisms of brain maintenance and cognitive reserve. Genetic factors and intellectual enrichment have also been shown to interact and enhance their effects on brain structure and cognition.7–9
In Huntington’s disease, a small number of studies have so far examined the role of genetic polymorphisms and lifestyle factors on individual differences in cognitive function. More specifically, environmental enrichment,10 education and participation in lifelong intellectual activities,11–13 as well as a number of genes, including fancd2- and fanci-associated nuclease 1 (FAN1),14 catechol-O-methyl transferase (COMT),15 MutS homologue 3 (MSH3)16 and microtubule-associated protein tau (MAPT),17 predict cognitive function. Two of these studies have also provided preliminary evidence that intellectual enrichment is associated with less striatal atrophy in humans,12,13 suggesting that it supports greater brain maintenance.
The aim of our work was to provide evidence regarding the effects of intellectual enrichment and genetic factors on cognitive function and brain structure in Huntington’s disease. For this purpose, we retrospectively analysed data from a multi-centre, longitudinal study, Track-HD,18–21 that measured changes in behaviour and brain structure over 3 years in individuals with the Huntington’s disease gene mutation in pre-manifest (maximum 15 years from predicted onset) and early stages of the disease. We quantified lifetime intellectual enrichment using level of education, pre-morbid intelligence quotient (IQ) and occupational cognitive demands12 measured at baseline. In terms of genetic polymorphisms, we selected common polymorphisms that have been previously associated with cognitive function in Huntington’s disease [COMT, brain-derived neurotrophic factor (BDNF), FAN1, MSH3 and MAPT].
Materials and methods
Participants
Track-HD is a multi-centre, 4-year observational study in Huntington’s disease gene carriers and matched controls. A full description of the Track-HD study has been previously reported.18–21 In summary, 243 Huntington’s disease gene carriers (both manifest and pre-manifest) and 123 matched controls were recruited across four sites (London, UK; Paris, France; Leiden, The Netherlands and Vancouver, Canada). The participants were predominantly Caucasian (97.5%), which limits our ability to test differential effects across different populations. However, it is important to note that Huntington’s disease is predominantly found in individuals with European ancestry.22 Local ethics committees approved the study at each site and all participants provided written informed consent according to the Declaration of Helsinki.
The Track-HD study included detailed measures of brain structure, cognitive and motor function, in addition to information regarding education, pre-morbid IQ and profession. Blood for DNA analysis was also collected. Table 1 shows details of the measures that were used in this study and the number of participants included (split by visit for longitudinal measures). Data from all Huntington’s disease gene carriers with at least one follow-up visit (n = 229), irrespective of disease diagnosis, were used for the analyses. Data from the matched control group were only used to create standardized scores of cognitive performance in the gene-carrier group (demographic information on the control group is provided in Supplementary Table 1).
Table 1.
Huntington’s disease gene-carrier demographics and clinical characteristics
| Variable | Missing data No (% all participants) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | Visit 2 | Visit 3 | Visit 4 | |||||
| Total number of participants | 229 | – | ||||||
| Male, n (%) | 104 (45%) | 0 | ||||||
| Age at baseline, mean (SD) | 44.9 (10.2) | 0 | ||||||
| CAG, median (min–max) | 43 (39–59) | 0 | ||||||
| DBS at baseline, mean (SD) | 333.2 (74.2) | 0 | ||||||
| Clinical status at baseline, n (%) | Pre-manifest 115 (50%) | Motor manifest 114 (50%) | 0 | |||||
| Education Level, median (min—max) | 4 (1, 6) | 0 | ||||||
| Occupational cognitive demands, Mean (SD) | 3.70 (0.87) | 10 (4%) | ||||||
| Verbal IQ, median (min–max) | UK: 33 (4–47), CA: 34 (11–48) FR: 34 (19–43), NL: 39 (16–48) |
0 | ||||||
| Composite cognitive score, mean (SD) per visit | −3.85 (3.89) | −3.79 (4.42) | −4.10 (4.52) | −4.23 (4.57) | 0 | 2 (1%) | 12 (5%) | 35 (15%) |
| Total GM volume Mean (SD) per visit | 0.052 (3.9) | −0.13 (3.9) | −0.17 (3.9) | −0.30 (4.1) | 19 (8%) | 27 (12%) | 54 (24%) | 77 (34%) |
| Caudate Volume Mean (SD) per visit | −0.0012 (0.09) | −0.0070 (0.09) | −0.0114 (0.09) | −0.0231 (0.09) | 14 (6%) | 22 (10%) | 47 (21%) | 52 (23%) |
| UHDRS TMS at baseline median (min–max) | 6 (0–52) | 0 | ||||||
| Visit from baseline (years) mean (SD) | 0 | 0.96 (0.08) | 1.99 (0.08) | 3.03 (0.10) | 0 | 2 (0.9%) | 10 (4%) | 28 (12%) |
| MSH3 | Number of participants with 0 3a alleles: 126 1 3a alleles: 71 2 3a alleles: 18 | 3a allele non-carriers: 126 (55%) 3a allele carriers: 89 (39%) | 14 (6%) | |||||
| FAN1 | Number of participants with 0 G alleles: 89 1 G alleles: 107 2 G alleles: 17 | G carriers (rs2140734) Non-carriers: 89 (39%) Carriers: 124 (54%) | 16 (7%) | |||||
| BDNF | Number of participants with 0 Met66 alleles: 136 1 Met66 alleles: 73 2 Met66 alleles: 4 | Met66 Non-carriers: 136 (59%) Met66 Carriers: 77 (34%) | 16 (7%) | |||||
| COMT | Number of participants with 0 Met158 alleles: 57 1 Met158 alleles: 113 2 Met158 alleles: 43 |
Val158 carriers: 170 (74%) Met158 homozygotes: 43 (19%) | 16 (7%) | |||||
| MAPT | Number of participants with 0 H2 alleles: 120 1 H2 alleles: 78 2 H2 alleles: 15 |
H1 homozygotes: 120 (52%) H2 carriers: 93 (41%) |
16 (7%) | |||||
Global cognitive function
To quantify cognitive function and change over 3 years, we created a composite score from the available cognitive measures. This composite score represents global cognitive function and is composed of the following measures from the Track-HD cognitive battery18: number correct in 90 s from the symbol digit modality test (a measure of processing speed), number correct in 45 s from the stroop word reading test (a measure of psychomotor speed), number correct adjusted for guessing (>0 means better than chance) for the five items condition from the spot the change task (a measure of working memory), number correct for negative emotions from the emotion recognition task (a measure of facial emotion recognition) and variability in the inter-tap interval in a paced tapping task at 3 Hz (a measure of temporal precision). These tasks were included in all four visits, in addition to the circle tracing task. However, that task was excluded from the composite score because of large practice effects that persisted across all visits.23 The remaining five measures were then used to create a composite score of global cognitive function.
To calculate the composite score, raw values were transformed to Z-scores using the mean and standard deviation (SD) of the control group at baseline and then summed. In the paced tapping task, the reciprocal of the variance in the inter-tap interval was used, such that a higher value indicated better performance (i.e. lower variability), consistent with all other measures. Therefore, higher values in the composite score indicate better performance. When computing the composite score, if one or two measures were missing, they were replaced by the mean Z-score of the existing measures. This was the case for 21 participants in Visit 1, 7 participants in Visit 2, 3 participants in Visit 3 and 16 participants in Visit 4, respectively. If a participant had less than three out of five measures available for a visit, then we did not compute a composite score for that visit and therefore, this participant visit was not included in the analyses with cognitive function as a variable.
Genetic polymorphisms
Track-HD subjects were genotyped using Illumina Omni2.5v1.1 arrays24 and genotypes were extracted using PLINK software.25 Because the main outcome measure was cognitive function, we focused on single-nucleotide polymorphisms (SNPs) that had been previously associated with cognitive and psychomotor function in Huntington’s disease. Based on previous literature, we, therefore, selected the following SNPs: rs4680 on Chromosome 2215 in COMT, which relates to dopamine metabolism, rs9468 on Chromosome 1717 in MAPT, which relates to tau protein production, rs2140734 on Chromosome 15 near FAN1,14,26 which is involved in DNA repair and a polymorphic repeat expansion in Exon 1 on Chromosome 5 of MSH3,16,24,27,28 which is involved in DNA mismatch repair. In addition, we tested another polymorphism, rs6265 (Val66Met) on Chromosome 11 in BDNF, which encodes the Val66Met polymorphism and regulates BDNF expression. Although the role of the Val66Met polymorphism in Huntington’s disease remains unknown, it has been consistently associated with cognitive function in ageing and dementia6,29–31 and BNDF expression may be affected by Huntington’s disease pathology.32,33 It also interacts with intellectual enrichment factors to predict cognitive function7,34: it was therefore relevant to our research question.
A previous study showed that the gene TREM2 (rs75932628) has a role in cognitive function in Huntington’s disease.35 However, the minor allele frequency is very low in the population (0.005% in Europeans in 1000 genomes project data Phase 3) and therefore, we did not include it in our analyses.
All genetic predictors were coded as having a binary, dominant effect, similar to the approach of Vuono et al.17Supplementary Table 2 shows how each binary predictor was coded. In more detail, the MSH3 predictor was coded for the presence of the three-repeat allele (3a).27 The rs2140734 (FAN1) predictor was coded for the presence of the minor allele G. It is also important to highlight that this SNP is in complete linkage disequilibrium with minor allele C in rs3512. The latter has been more widely examined in other studies and shown to be associated with age of onset and disease progression in Huntington’s disease.24,26,36 The MAPT predictor distinguished between H1 haplotype homozygotes and H2 carriers. Carrying the minor allele C in rs9468 tags for the H2 haplotype, whereas carrying the allele T tags for the H1 haplotype.37 The COMT (rs4680) predictor variable distinguished Met158 homozygotes from carriers of the Val158 allele.15 The BDNF (rs6265) predictor variable distinguished carriers from non-carriers of the detrimental allele, Met66.
For completion, we also repeated the analyses coding the variables by the number of minor alleles for all genes except BDNF, because there was an insufficient number of cases (see Table 1 for the number of participants per minor allele).
Intellectual enrichment
Education, bilingualism, leisure and professional intellectual activities are some of the activities associated with a protective effect against cognitive decline.38 Track-HD recorded main profession, education level using the international standard classification of education scale and pre-morbid IQ using vocabulary tests. Because different tests were used in each country, pre-morbid IQ was standardized within the country (national adult reading test -2 in the UK, ANART in Canada, Dutch adult reading test in The Netherlands and Mill Hill in France). Occupational cognitive requirements39 were estimated from the main profession recorded for each participant (see Supplementary Methods). These three measures were then standardized and summed up to create a composite score of intellectual enrichment.12 A higher value in the intellectual enrichment score means a higher level of education, a more cognitively demanding profession and a higher level of estimated pre-morbid IQ.
Measures of disease pathology
Predicted disease severity at the time of recruitment was measured using the CAG by age product [disease burden score (DBS) = age × (CAG—35.5)].40 This is a commonly used model of predicted exposure to disease pathology describing the well-established relationship between age and the CAG repeat number of the longer allele. The larger the CAG repeat length, the earlier the predicted age of disease onset.41
Pathology at baseline and rate of change were quantified using structural MRI measures of caudate volume and total grey matter (GM) volume, which are robust and well-defined markers of brain atrophy in Huntington’s disease.18–21 Measures of white matter integrity using diffusion weighted imaging were only introduced at Visit 4 in Track-HD; therefore, we only focused on GM volume in our study. Whole-brain T1-weighted 3D magnetization-prepared rapid acquisition with gradient echo images were acquired at 3T at all four visits (for details of the imaging protocol see Tabrizi et al.18). Caudate volume at baseline and longitudinal change was measured using medical image display and analysis software (MIDAS)’ semi-automated segmentation and the boundary shift integral, respectively.20,42,43 Total GM volume at baseline was measured using statistical parametric mapping 12 (SPM12). Longitudinal change was measured using a non-linear fluid registration method in MIDAS, which produced whole-brain voxel compression maps measuring change from baseline.44 Voxel compression maps were then convolved with SPM-derived GM maps to generate a change in total GM over time. The measures of caudate volume and total GM volume used in all the analyses were transformed to per cent of total intracranial volume (TIV), in order to adjust for differences in brain size. TIV was measured at baseline using MIDAS.
In addition to caudate and total GM volume, we also performed exploratory whole-brain analyses using voxel-based morphometry (VBM).45 The GM probability maps at baseline and voxel compression maps of change from baseline were normalized to a group template space using diffeomorphic anatomical registration through exponentiated lie algebra. Normalized images were then smoothed using an 8 mm full-width at half maximum Gaussian kernel. Full details of the MRI methods used have been published previously.46
Statistical analysis
Statistical analyses were performed using R version 3.6.3 (http://www.r-project.org/) and the packages lmertest (version 3.1-1) and lme4 (version 1.1-21).
To examine the relationship between cognitive function and brain volume with our predictors of interest, we used linear mixed models. Our predictors of interest were intellectual enrichment and genetic polymorphism. All models were fitted using maximum likelihood estimation and correlated random intercept and slope. All models included as covariates age, DBS and study site and their interaction with the visit, as well as sex (main effect only, because the sex by visit interaction term did not improve model fit and was therefore dropped). Models with cognitive function as an outcome also included the use of antipsychotic medication as a covariate (see Supplementary Methods). Time was modelled in years of follow up as approximated by the annual visit number. Based on previously published analyses of the Track-HD data,23 we included quadratic effects of time in models with cognitive function and total GM volume as the outcome. Age and DBS were mean centred (Table 1).
Our hypotheses tested whether our variables of interest significantly predicted cognitive function or brain volume at baseline and changed over time. We used likelihood ratio tests to assess the covariate-adjusted significance of predictors on the outcome variables. We also tested for the significance of the interaction of genetic predictors with intellectual enrichment in the same way. In all the analyses, we visually inspected model residual distributions to assess plausible normality. No outliers were identified. Significance was established using two-sided P-values and applying Bonferroni correction to control Type I error rate when multiple measures were used to test a hypothesis.
For VBM analyses, a binary GM mask was created using the mean normalized images from all Huntington’s disease gene carriers. This was used in all analyses. Statistical maps were thresholded at two-tailed P < 0.001 uncorrected at voxel level and P < 0.05 family-wise error corrected at cluster level.
Data availability
Track-HD data are available upon request after appropriate data use agreements are signed by the study funder, the CHDI Foundation. Please direct inquiries to info@chdifoundation.org.
Results
Intellectual enrichment
Previous research showed that participants with early stage Huntington’s disease who had higher intellectual enrichment had better cognitive performance than those with lower intellectual enrichment.13 Furthermore, among pre-manifest gene carriers who are closer to predicted disease onset, those with high intellectual enrichment have a slower rate of cognitive decline than those with low intellectual enrichment.12
In our cohort of participants with pre-manifest and early stage Huntington’s disease, intellectual enrichment predicted mean global cognitive function and there was also a significant three-way interaction between intellectual enrichment, DBS and time (i.e. annual visit number) on global cognitive function (both P < 0.001; Table 2 and Supplementary Table 3). In agreement with previous studies, the estimate for the main effect of intellectual enrichment was positive, such that participants with high intellectual enrichment had better cognitive function than those with lower intellectual enrichment. More specifically, for average DBS and age, the mean estimates [95% confidence interval (CI)] were −3.14 SD (−3.66, −2.62) and −5.57 (−6.10, −5.04) for high (1SD above mean) and low (1SD below mean) intellectual enrichment, respectively. The contrast estimate [standard error (SE)] for high versus low = 2.43 SD (0.36), t(229) = 6.744, P < 0.001.
Table 2.
Association between intellectual enrichment with cognitive function
| Model | DF | AIC | Chisq | P-value |
|---|---|---|---|---|
| Intellectual enrichment | ||||
| Null model | 20 | 3151.6 | ||
| Intellectual enrichment | 21 | 3112.3 | 41.3 | <0.001 |
| Intellectual enrichment by visit | 22 | 3113.7 | 0.6 | 0.452 |
| Intellectual enrichment by DBS | 23 | 3111.9 | 3.8 | 0.050 |
| Intellectual enrichment by DBS by visit | 24 | 3101.4 | 12.5 | <0.001 |
| Intellectual enrichment correcting for education versus education alone | ||||
| Null model | 20 | 3151.6 | ||
| Education by visit by DBS | 24 | 3133.0 | 26.5 | <0.001 |
| Intellectual enrichment by visit by DBS | 28 | 3105.3 | 35.7 | <0.001 |
| Intellectual enrichment correcting for education versus intellectual enrichment alone | ||||
| Null model | 20 | 3151.6 | ||
| Intellectual enrichment by visit by DBS | 24 | 3101.4 | 58.2 | <0.001 |
| Education by visit by DBS | 28 | 3105.3 | 4.1 | 0.397 |
The null model for intellectual enrichment included age at baseline, site (three dummy variables) and DBS at baseline with their interaction with visit and main effects of sex and use of antipsychotic medication. A quadratic term was also included for visit, as well as its interaction with DBS.
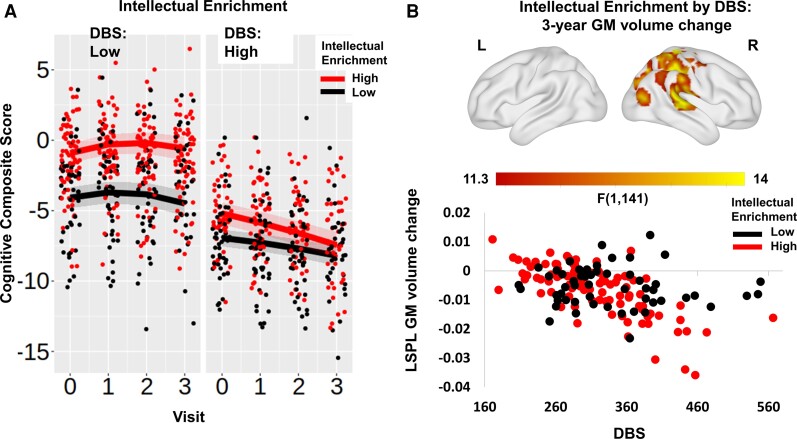
The estimate for the three-way interaction between DBS, intellectual enrichment and time were in the opposite direction from the main effect; in individuals with low DBS, those with high intellectual enrichment declined slower than those with low intellectual enrichment; however, in individuals with high DBS, those with high intellectual enrichment declined faster than those with lower intellectual enrichment, despite having better performance at baseline (Fig. 1A and Supplementary Fig. 1). More specifically, for participants with low DBS (1SD below mean) those with high intellectual enrichment declined slower than those with lower intellectual enrichment [for 258.9 DBS slope estimate (95% CI) = 0.141 (−0.007, 0.289) and −0.102 (−0.268, 0.065)] for high and low intellectual enrichment, respectively; contrast estimate (SE) for high versus low intellectual enrichment was 0.243 (0.119), t(224) = 2.043, P = 0.042). In contrast, an individual with 407.4 DBS (1SD above mean) and 1SD above mean intellectual enrichment had faster cognitive decline than an individual with the same DBS but 1SD below mean intellectual enrichment [slope estimate (95% CI) = −0.741 (−0.917, −0.565) and −0.413 (−0.556, −0.270)] for high and low intellectual enrichment, respectively; contrast estimate (SE) high versus low = −0.327 (0.110), t(247) = −2.971, P = 0.003). To aid with interpretation of this finding, we repeated the same analysis, replacing DBS with group as an ordered factor, coding for manifest and pre-manifest individuals. There was a significant main effect of intellectual enrichment; however, the group by visit by intellectual enrichment interaction was not significant in this case (Supplementary Table 4). Our results, therefore, show that there is a strong positive effect of intellectual enrichment on global cognitive function at baseline. It is unclear what is driving the significant three-way interaction between intellectual enrichment, DBS and visits and whether it is a reliable finding. The lack of a significant three-way interaction with the group suggests that it may not be driven by disease stage.
Figure 1.
Intellectual enrichment, cognitive function and brain volume. (A) Association between intellectual enrichment and DBS with global cognitive function [t(225.1) = −3.596, P < 0.001] and (B) T-map of 3-year GM volume change. In (A) regression lines are generated from a mixed linear model at high (1SD above mean; red) and low (1SD below mean; black) intellectual enrichment. For visualization purposes, results are split into high (above mean) and low (below mean) DBS. The bands around the regression lines are 95% confidence intervals. Data points show the raw data residualized against age, site, sex and use of antipsychotic medication and have been jittered to minimize overlap. In B, significant clusters are overlaid on the ICBM152 template mesh (top). Maps are thresholded at P < 0.001 uncorrected at voxel level and P < 0.05 family-wise error corrected at cluster level. Shown in a scatter plot (bottom) are the extracted values averaged across the significant cluster. For visualization purposes, data are grouped by high (above mean—red) and low (below mean—black) intellectual enrichment. Data points show the raw data residualized against age, DBS, site, sex and TIV. LSPL, left superior parietal lobe.
The intellectual enrichment score is a composite measure comprised of education, verbal IQ and occupational cognitive requirements. Education alone is a well-known predictor of cognitive function.47 We next wanted to understand whether the effect captured by intellectual enrichment on cognitive function is primarily due to the contribution of education or is incremental to the effect of education. To address this question, we compared a model including all education and intellectual enrichment terms against two different models, one with only the education terms and another with only the intellectual enrichment terms (Table 2; Supplementary Table 5). We found that intellectual enrichment contributed highly significant information to the model above and beyond education alone.
To confirm that the relationship between intellectual enrichment and cognitive function is not driven by motor or neuropsychiatric symptoms, we re-estimated the models, adding unified Huntington’s disease rating scale total motor score (TMS) at baseline and the presence of depressive symptoms at baseline with their interactions with visit as confounds. Adding these factors did not alter the results, both the main effect of intellectual enrichment and the three-way interaction between intellectual enrichment, DBS and visit remained significant (Supplementary Table 6).
To further understand the mechanism by which intellectual enrichment influences global cognitive function, we next examined its relationship with brain volume, measured by caudate and total GM volume over 3 years. There was a significant interaction between intellectual enrichment and DBS on caudate volume at baseline (pbon = 0.024; Supplementary Tables 7 and 8), such that intellectual enrichment had a positive association with caudate volume in Huntington’s disease gene carriers far from predicted disease onset (i.e. low DBS), but this effect was attenuated or reversed as the disease progressed (Supplementary Fig. 2A). More specifically, a participant with 258.9 DBS (1SD below mean) and high intellectual enrichment had larger caudate volume at baseline compared with a participant with the same DBS, but low intellectual enrichment [mean estimate (95% CI) = 0.0645 (0.0464, 0.0826) and 0.0291 (0.0097, 0.0486)] for high and low intellectual enrichment, respectively; contrast estimate (SE) high versus low = 0.0354 (0.0139), t(215) = 2.534, P = 0.012). However, there was no difference in participants with high DBS (for 407.4 DBS contrast estimate (SE) for high versus low intellectual enrichment was −0.0141 (0.135), t(215) = −1.044, P = 0.298). As previously, we repeated the same analysis, replacing DBS with the group as an ordered factor, coding for manifest versus pre-manifest individuals. There was no significant group by intellectual enrichment interaction on caudate volume at baseline (Supplementary Table 9). It is therefore unclear what is driving the intellectual enrichment by DBS interaction and whether it is reliable. There were no significant main effects or interactions with total GM volume (all pbon > 0.1; Supplementary Table 7 and Fig. 2B).
Lastly, we performed exploratory, whole-brain analyses using VBM to identify whether there were specific brain regions that showed an effect of intellectual enrichment or an interaction between intellectual enrichment and DBS. There was no significant main effect of intellectual enrichment on volume or volume change anywhere in the brain, but there was a significant interaction with DBS. Participants with low DBS and high intellectual enrichment had larger GM volume at baseline in the right putamen, the thalamus and the right superior temporal gyrus compared with individuals with similar DBS but low intellectual enrichment (Supplementary Table 10 and Fig. 3). In addition, the rate of GM atrophy over 3 years was faster in individuals with high intellectual enrichment and high DBS in a cluster extending from the right post-central gyrus to the right superior temporal gyrus ventrally and to the superior parietal lobe and the right precuneus caudally (Fig. 1B and Supplementary Table 10). As previously, we repeated the same analyses, replacing DBS with a group. There were no brain regions that showed a significant interaction between intellectual enrichment and group for baseline volume or 3 year change.
Genetic polymorphisms
We next examined the relationship between cognitive function and five genetic polymorphisms linked to genes known to affect cognitive function in Huntington’s disease: MSH3, FAN1, MAPT, BDNF and COMT. We did not find a significant association between FAN1, MAPT, BDNF and COMT variants and global cognitive function at baseline or change over time after Bonferroni correction for five multiple comparisons (all pbon > 0.068; Table 3). In agreement with previous analyses of disease progression in the same cohort27 and recent research,16MSH3 was a significant predictor of global cognitive function at baseline and change (both pbon = 0.045; Table 3 and Supplementary Table 11). More specifically, participants with one or more 3a alleles in MSH3 had a better cognitive function at baseline and slower cognitive decline compared with non-carriers of 3a alleles [for average age and DBS slope (95% CI) = −0.329 (−0.434, −0.223) and −0.118 (−0.241, 0.004)] for non-carriers and carriers, respectively; contrast estimate (SE) non-carriers versus carriers = −0.21 (0.081), t(213) = −2.587, P = 0.010; Fig. 2A and Supplementary Fig. 4). We repeated the analyses coding for the number of alleles in the genes MSH3, FAN1, COMT and MAPT. There was no change in the results (see Supplementary Table 12), i.e. only MSH3 was a significant predictor of cognitive function at baseline and change over time.
Table 3.
Association between genetic polymorphisms and cognitive function
| Model | DF | AIC | χ2 | P-value | P-value Bonferroni cor. |
|---|---|---|---|---|---|
| MSH3 | |||||
| Null model | 20 | 3139.0 | |||
| MSH3 | 21 | 3134.2 | 6.8 | 0.009 | 0.045 |
| MSH3 by visit | 22 | 3129.3 | 6.8 | 0.009 | 0.045 |
| MSH3 by DBS | 23 | 3131.1 | 0.2 | 0.649 | 1 |
| MSH3 by DBS by visit | 24 | 3133.1 | 0.0 | 0.850 | 1 |
| FAN1 | |||||
| Null model | 20 | 3109.3 | |||
| FAN1 | 21 | 3110.7 | 0.6 | 0.4223 | 1 |
| FAN1 by visit | 22 | 3112.6 | 0.0 | 0.895 | 1 |
| FAN1 by DBS | 23 | 3113.1 | 1.6 | 0.213 | 1 |
| FAN1 by DBS by visit | 24 | 3113.4 | 1.7 | 0.193 | 0.964 |
| MAPT | |||||
| Null model | 20 | 3109.3 | |||
| MAPT | 21 | 3108.8 | 2.6 | 0.110 | 0.550 |
| MAPT by visit | 22 | 3110.8 | 0.0 | 0.988 | 1 |
| MAPT by DBS | 23 | 3107.2 | 5.5 | 0.019 | 0.094 |
| MAPT by DBS by visit | 24 | 3109.2 | 0.0 | 0.947 | 1 |
| COMT | |||||
| Null model | 20 | 3109.3 | |||
| COMT | 21 | 3110.8 | 0.5 | 0.488 | 1 |
| COMT by visit | 22 | 3111.2 | 1.6 | 0.201 | 1 |
| COMT by DBS | 23 | 3112.6 | 0.5 | 0.462 | 1 |
| COMT by DBS by visit | 24 | 3112.2 | 2.4 | 0.120 | 0.601 |
| BDNF | |||||
| Null model | 20 | 3109.3 | |||
| BDNF | 21 | 3111.2 | 0.1 | 0.706 | 1 |
| BDNF by visit | 22 | 3107.1 | 6.1 | 0.014 | 0.068 |
| BDNF by DBS | 23 | 3109.0 | 0 | 0.889 | 1 |
| BDNF by DBS by visit | 24 | 3110.9 | 0.1 | 0.741 | 1 |
The null model included age at baseline, site (three dummy variables), DBS at baseline with their interaction with visit, sex and use of antipsychotic medication. A quadratic term was also included for visit, as well as its interaction with DBS. P-values were corrected for five independent comparisons using Bonferroni correction.
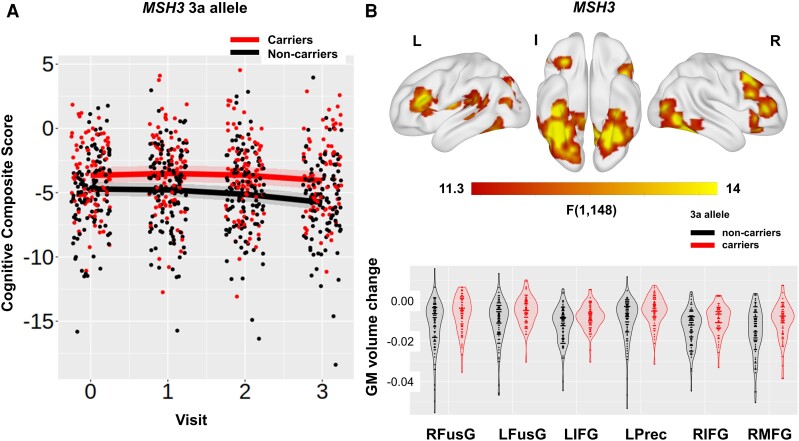
Figure 2.
MSH3, cognitive function and brain volume. (A) Association between the MSH3 predictor and global cognitive function [t(198.7) = 2.637, P = 0.009] and (B) T-map of 3-year GM volume change. In A, regression lines show the predicted effect of carrying (red) and not carrying (black) the 3a allele from a mixed linear model. The bands around the regression lines are 95% confidence intervals. Data points show the raw data residualized against age, site, sex and use of antipsychotic medication and have been jittered to minimize overlap. In B, significant clusters are overlaid on the ICBM152 template mesh (top). Maps are thresholded at P < 0.001 uncorrected at voxel level and P < 0.05 family-wise error corrected at cluster level. Shown in violin plots (bottom) are the extracted values averaged across the significant clusters for carriers (red) and non-carriers (black) of the 3a allele. Individual data points are shown in black dots. Data points show the raw data residualized against age, DBS, site, sex and TIV. RFusG and LFusG, right and left fusiform gyrus; LIFG and RIFG, left and right inferior frontal gyrus; LPrec, left precuneus; RMFG, right middle frontal gyrus.
We next examined the relationship between MSH3 polymorphisms and brain volume to further understand the mechanism by which MSH3 may influence global cognitive function. MSH3 had a significant effect on the total GM volume rate of change (i.e. MSH3 by visit interaction; pbon = 0.001; Supplementary Tables 7, 13 and Fig. 5). Huntington’s disease gene carriers with one or more 3a alleles in MSH3 had a slower rate of total GM atrophy over 3 years compared with non-carriers [for average age and DBS slope (95% CI) = −0.181 (−0.202, −0.160) and −0.122 (−0.148, −0.097)] for non-carriers and carriers, respectively; contrast estimate (SE) for non-carriers versus carriers = −0.0586 (0.0168), t(196) = −3.486, P < 0.001).
Exploratory VBM analyses examined the main effect of MSH3 on GM volume across the whole brain. There was a significant effect of MSH3 on GM volume at baseline in the right middle temporal gyrus, the right inferior occipital gyrus and the left post-central gyrus (Supplementary Table 10 and Fig. 6). There was also a significant effect of MSH3 on GM volume change in the fusiform gyrus bilaterally, the inferior frontal gyrus bilaterally, the right middle frontal gyrus and the left precuneus (Supplementary Table 10 and Fig. 2B). Lastly, there was an interaction between MSH3 and DBS on GM volume change in the left inferior frontal gyrus, the left supplementary motor area and the right superior temporal gyrus (Supplementary Table 10 and Fig. 7). The effect of MSH3 was positive in all cases, such that 3a allele carriers (across all participants or for those with high DBS) had higher volume and a slower rate of GM atrophy compared with non-carriers. Our results therefore suggest that carrying the 3a allele in MSH3 supported preserved cognitive function and was associated with a slower rate of neurodegeneration.
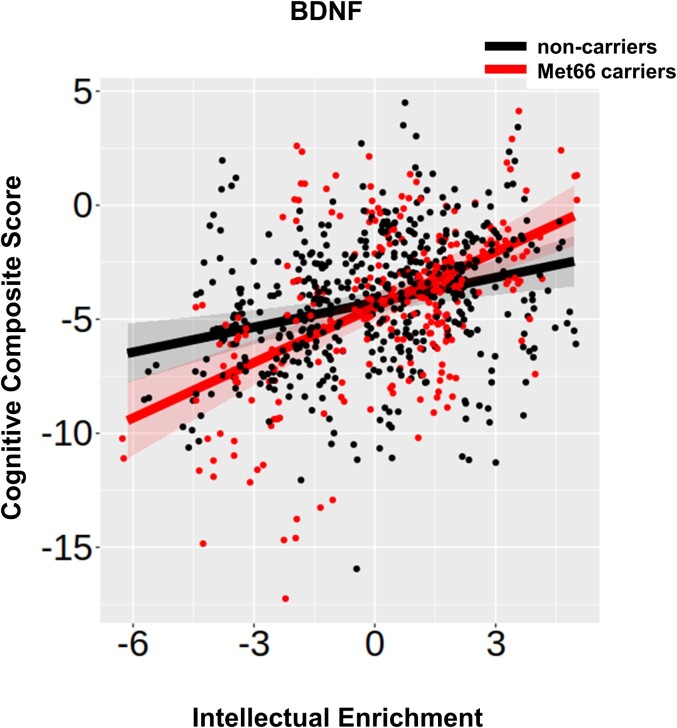
Gene–environment interaction
Previous research in ageing and dementia has shown that environmental factors, including intellectual enrichment, interact with genetic polymorphisms in order to predict cognitive function.7,8 To test this hypothesis in our study, we examined the interaction between all five genetic polymorphisms and intellectual enrichment on cognitive function and decline. BDNF was the only gene that significantly interacted with intellectual enrichment to predict global cognitive function at baseline (pbon = 0.031 corrected for five tests; Table 4 and Supplementary Table 14). There was a positive interaction between BDNF and intellectual enrichment on global cognitive function at baseline, such that the effect of intellectual enrichment on cognitive function was stronger for Met66 allele carriers than for non-carriers. More specifically, the estimates for Met66 allele carriers with low (1SD below mean) and high intellectual enrichment (1SD above mean) were: estimates (95% CI) = −6.31 (−7.20, −5.42) and −2.57 (−3.41, −1.73), respectively; contrast estimate (SE) for high versus low intellectual enrichment = 3.74 (0.598), t(216) = 6.249, P < 0.001. Similarly, for Met66 allele non-carriers, with low (1SD below mean) and high intellectual enrichment (1SD above mean) estimate (95% CI) = −5.08 (−5.75, −4.42) and −3.40 (−4.10, −2.71), respectively; contrast estimate (SE) for high versus low intellectual enrichment = 1.68 (0.483), t(214) = 3.486, P < 0.001. The difference between high and low intellectual enrichment was greater for Met66 allele carriers than for non-carriers, suggesting that the Met66 allele moderates the effect of intellectual enrichment on cognitive function [contrast estimate (SE) = −2.06 (0.768), t(215) = −2.678, P = 0.008; Fig. 3].
Table 4.
Interaction between intellectual enrichment and genetic polymorphisms on cognitive function
| Model | DF | AIC | χ2 | P-value | P-value Bonferroni cor. |
|---|---|---|---|---|---|
| MSH3 | |||||
| Null model | 24 | 2931.8 | |||
| MSH3 by intellectual enrichment | 25 | 2933.1 | 0.7 | 0.404 | 1 |
| MSH3 by intellectual enrichment by visit | 26 | 2933.9 | 1.1 | 0.286 | 1 |
| FAN1 | |||||
| Null model | 24 | 2910.6 | |||
| FAN1 by intellectual enrichment | 25 | 2912.4 | 0.2 | 0.679 | 1 |
| FAN1 by intellectual enrichment by visit | 26 | 2914.4 | 0.0 | 0.833 | 1 |
| MAPT | |||||
| Null model | 24 | 2911.5 | |||
| MAPT by intellectual enrichment | 25 | 2913.5 | 0.0 | 0.895 | 1 |
| MAPT by intellectual enrichment by visit | 26 | 2915.5 | 0.0 | 0.894 | 1 |
| COMT | |||||
| Null model | 24 | 2910.2 | |||
| COMT by intellectual enrichment | 25 | 2912.2 | 0.0 | 0.960 | 1 |
| COMT by intellectual enrichment by visit | 26 | 2914.0 | 0.2 | 0.630 | 1 |
| BDNF | |||||
| Null model | 24 | 2907.6 | |||
| BDNF by intellectual enrichment | 25 | 2902.1 | 7.5 | 0.006 | 0.031 |
| BDNF by intellectual enrichment by visit | 26 | 2903.8 | 0.2 | 0.627 | 1 |
The null model included intellectual enrichment, the genetic polymorphism, age at baseline, site (three dummy variables), DBS at baseline with their interaction with visit, sex and use of antipsychotic medication. A quadratic term was also included for visit, as well as its interaction with DBS. P-values were corrected for five independent comparisons using Bonferroni correction.
Figure 3.
BDNF, intellectual enrichment and cognitive function. Association between the BDNF predictor and intellectual enrichment with global cognitive function [t(203.5) = 2.760, P = 0.006]. Regression lines show the predicted effect of carrying (red) and not carrying (black) the Met66 allele. The bands around the regression lines are 95% confidence intervals. Data points show the raw data residualized against age, site, sex and use of antipsychotic medication.
To understand the mechanism by which BDNF interacts with intellectual enrichment to impact cognitive function, we examined the interaction between BDNF and intellectual enrichment on brain volume. The effect of the interaction of BDNF with intellectual enrichment was significant but small on both caudate and total GM volume rate of change (both pbon < 0.03 corrected for two tests; Supplementary Tables 15–17). The difference in the rate of volume change between individuals with high and low intellectual enrichment was positive in Met66 allele carriers but negative for non-carriers. In more detail, Met66 allele carriers with high (1SD above mean) and low intellectual enrichment (1SD below mean) estimate (95% CI) = −0.0094 (−0.0105, −0.0082) and −0.0110 (−0.0123, −0.0097), respectively; contrast estimate (SE) = 0.0017 (0.0009), t(228) = 1.900, P = 0.059. Met66 allele non-carriers with high (1SD above mean) and low intellectual enrichment (1SD below mean) estimate (95% CI) = −0.0103 (−0.0112, −0.0094) and −0.0094 (−0.0102, −0.0085), respectively; contrast estimate (SE) = −0.0010 (0.0007), t(205) = −1.480, P = 0.140. The difference between high and low intellectual enrichment was positive for Met66 allele carriers, but negative for non-carriers, suggesting that the Met66 allele moderates the effect of intellectual enrichment on caudate atrophy rate [contrast estimate (SE) = −0.0026 (0.0011), t(221) = −2.406, P = 0.017; Supplementary Fig. 8].
This was similar to total GM volume. Met66 allele carriers with high (1SD above mean) and low intellectual enrichment (1SD below mean) estimate (95% CI) = −0.129 (−0.167, −0.090) and −0.206 (−0.248, −0.1635), respectively; contrast estimate (SE) = 0.0769 (0.0289), t(214) = 2.658, P = 0.008. Met66 allele non-carriers with high (1SD above mean) and low intellectual enrichment (1SD below mean) estimate (95% CI) = −0.179 (−0.209, −0.1484) and −0.132 (−0.161, −0.1020), respectively; contrast estimate (SE) = −0.0469 (0.0218), t(192) = −2.154, P = 0.0324. The difference between high and low intellectual enrichment was positive for Met66 allele carriers but negative for non-carriers, suggesting that the Met66 allele moderates the effect of intellectual enrichment on total GM atrophy rate [contrast estimate (SE) = −0.124 (0.0362), t(207) = −3.421, P = 0.008; Supplementary Fig. 9].
Exploratory whole-brain VBM analyses examined the interaction between BDNF and intellectual enrichment on GM volume at baseline and change over time, but we did not identify any significant clusters.
Discussion
The aim of our study was to examine the role of intellectual enrichment and genetic polymorphisms on cognitive function and brain structure in Huntington’s disease. Our results highlight the complexity of the interplay between environmental and genetic factors on behaviour and brain structure. Intellectual enrichment and genetic variation in MSH3 are independently associated with global cognitive function and brain structure, whereas intellectual enrichment interacts with BDNF to attenuate the deleterious effect of the Met66 polymorphism.
In more detail, we replicated previous findings showing that intellectual enrichment was associated with better global cognitive function at earlier (pre-manifest) stages of the disease.12 In the present work, we further show that the composite intellectual enrichment score explains additional variance in education. We also show that in participants with high DBS (in our study, mean DBS was 333.2), those with high intellectual enrichment had a faster rate of decline over 3 years (0.36 SD annualized change in global cognitive function) than those with lower intellectual enrichment (Fig. 1A). The faster rate of decline in participants with high DBS narrowed the difference in baseline cognitive performance between individuals with low and high intellectual enrichment. Similarly, we found that high intellectual enrichment predicted accelerated atrophy in the posterior cortical regions of the right hemisphere in participants with high DBS. Therefore, it appears that as DBS increases, the protective effect of intellectual enrichment on cognition decreases. However, when replacing DBS with group, the three-way interaction between intellectual enrichment, group and visit was not significant in relation to cognitive function or brain volume. Given the very strong association between DBS and group, it is therefore unclear what is driving the significant interaction between intellectual enrichment and DBS and whether it is a reliable finding.
Further insights regarding the mechanism by which intellectual enrichment affects cognitive function are provided by the interaction between intellectual enrichment and BDNF gene variation. The difference in cognitive function between individuals with low and high intellectual enrichment was greater in Met66 allele carriers than in non-carriers. Previously, comparing the blood expression levels of BDNF between 22 controls and 62 manifest gene carriers from this cohort using RNAseq, we found that Huntington’s disease gene carriers had lower levels of BDNF expression than controls (P = 0.04266).48 Post-mortem studies have also identified reduced BDNF levels in the striatum of Huntington’s disease patients. However, it is unclear whether this is due to defects in the delivery of cortical BDNF49 or to the response in the striatum.33 It is possible that carrying the Met66 allele exacerbates existing defects in the BDNF pathway. Previous research in animal models of Huntington’s disease showed that such defects can be rescued by environmental enrichment.50 Our results are in broad agreement with these findings and suggest that intellectual enrichment potentially counteracts the detrimental effect of the Met66 allele in both cognitive function and brain structure (striatum and total GM). Our findings are also in agreement with previous studies in ageing showing a significant interaction between intellectual enrichment and BDNF to predict cognitive function and decline in healthy older adults.7,34
Intellectual enrichment did not interact with any of the other genetic polymorphisms we examined, whereas the only genetic predictor with a significant effect on cognitive function was variation in MSH3. A recent study16 has identified MSH3 as a modifier of cognitive function in Huntington’s disease rather than motor function, while we have previously shown in this cohort that variation in MSH3, specifically carrying a 3a allele, has a protective effect on a composite score of disease progression, which included cognitive and psychomotor function.24,27 It is currently hypothesized that MSH3 is introducing an expansion of the HTT CAG repeat in the process of repair. Greater expansion is associated with earlier disease onset and faster progression,51,52 whereas carrying the 3a allele is associated with reduced expression of MSH3 and therefore reduced somatic expansion and slower progression.27 In agreement with this finding, in the present work, we further show that carrying the 3a allele in MSH3 was associated with slower GM atrophy across different regions in the cortex, including the inferior temporal and inferior frontal gyri. The absence of a significant effect in the striatum is notable given previous work, which showed that there is large somatic expansion in both the cortex (temporal, occipital and prefrontal cortex) and the striatum.53 This finding could be explained by the fact that all analyses were adjusted for differences in DBS and suggests that carrying the 3a allele does not explain additional variance in striatal atrophy. Lastly, it is important to note that the protective effect of carrying the 3a allele in MSH3 is a result of reducing the expression of MSH3 and there is no evidence that it supports neuroprotective mechanisms. The effect of MSH3 on cognitive function and brain volume cannot therefore be interpreted as brain maintenance.
Similar to MSH3, variation in FAN1 (rs3512) has also been implicated in somaticinstability52 and has been previously shown to predict delayed age of onset in Huntington’s disease.26,36FAN1 overexpression reduces CAG repeat expansion in human cell modes54; however, in our study, there was no significant effect of rs2140734 (or rs3512) on cognitive function. The reason for the contradictory findings is unclear. It could be due to a lack of statistical power given the relatively small sample size, but recent work suggests a differential effect of FAN1 on motor rather than cognitive function.16
Lastly, in contrast to previous studies in Huntington’s disease, we did not find any evidence for an association between the genes COMT and MAPT and cognitive function. A previous study15 showed that COMT Val158 allele carriers had slower cognitive decline compared with Met158 homozygotes in manifest Huntington’s disease patients. The number of Met158 homozygotes was low in our cohort (43 out of 229; 19%) and our cohort included both pre-manifest and patients at early stages of the disease, which could explain the contradictory findings. Variation in the MAPT gene has also been previously shown to predict cognitive decline in Huntington’s disease,17 such that H1 homozygotes had a slower decline in cognitive function compared with H2 carriers. However, this effect was the opposite to what has been previously reported for Parkinson’s disease,55 and had a small effect size (r = −0.14). In our study, we did not find strong evidence for an association between MAPT and cognitive function; it is therefore currently unclear whether MAPT plays a role in cognitive function in Huntington’s disease.
Conclusion
In summary, we have shown that cognitive function in Huntington’s disease is affected by an interplay between genetic and environmental factors. We have replicated previous findings that cognitive decline is slower in carriers of the 3a allele in the gene MSH3, and further showed that slower cognitive decline is supported by the slowing of GM volume atrophy in the cortex, in agreement with the role of MSH3 in somatic instability. Intellectual enrichment also appears to have a protective effect on cognitive function at pre-manifest stages of the disease, but as the disease progresses, this effect is attenuated and there is faster neurodegeneration and cognitive decline. Importantly, we also observed a significant interaction between intellectual enrichment and the BDNF gene, whereby intellectual enrichment counteracted the detrimental effect of carrying the Met66 allele on cognitive function and brain structure, in agreement with the role of intellectual enrichment in enhancing brain trophic support. Future research is now needed to develop and evaluate intellectual enrichment interventions in Huntington’s disease and measure their impact on both behaviour and brain structure.
Supplementary Material
Abbreviations
- BDNF =
brain-derived neurotrophic factor
- CAG =
coronary artery angiography
- CI =
confidence interval
- COMT =
catechol-O-methyl transferase
- DBS =
disease burden score
- DF =
degrees of freedom
- FAN1 =
fancd2- and fanci-associated nuclease 1
- GM =
grey matter
- HTT =
Huntingtin
- IQ =
intelligence quotient
- MAPT =
microtubule-associated protein tau
- MIDAS =
medical image display and analysis software
- MSH3 =
MutS homologue 3
- SD =
standard deviation
- SE =
standard error
- SEM =
structural equation modelling
- SNP =
single-nucleotide polymorphism
- SPM =
statistical parametric mapping
- TIV =
total intracranial volume
- UHDRS TMS =
unified Huntington’s disease rating scale total motor score
- VBM =
voxel-based morphometry
Appendix
Track-HD investigators
Peter Kraus, Rainer Hoffman, Alan Tobin, Beth Borowsky, S. Keenan, Kathryn B. Whitlock, Sarah Queller, Colin Campbell, Chiachi Wang, Eric Axelson, Hans Johnson, Tanka Acharya, Dave M. Cash, Chris Frost, Rebecca Jones, Caroline Jurgens, Ellen P. ‘t Hart, Jeroen van der Grond, Marie-Noelle N. Witjes-Ane, Raymund A.C. Roos, Eve M. Dumas, Simon J.A. van den Bogaard, Cheryl Stopford, David Craufurd, Jenny Callaghan, Natalie Arran, Diana D. Rosas, S. Lee, W Monaco, Alison O’Regan, Cassie Milchman, Ellen Frajman, Izelle Labuschagne, Julie Stout, Melissa Campbell, Sophie C. Andrews, Natalie Bechtel, Ralf Reilmann, Stefan Bohlen, Chris Kennard, Claire Berna, Stephen Hicks, Alexandra Durr, Cristophe Pourchot, Eric Bardinet, Kevin Nigaud, Romain Valabrègue, Stephane Lehericy, Cecilia Marelli, Celine Jauffret, Damian Justo, Blair Leavitt, Joji Decolongon, Aaron Sturrock, Alison Coleman, Rachelle Dar Santos, Aakta Patel, Claire Gibbard, Daisy Whitehead, Ed Wild, Gail Owen, Helen Crawford, Ian Malone, Nayana Lahiri, Nick C. Fox, Nicola Z. Hobbs, Roger Ordidge, Tracey Pepple, Joy Read, Miranda J. Say, Bernhard Landwehrmeyer.
Contributor Information
Marina Papoutsi, UCL Huntington’s Disease Centre, Queen Square Institute of Neurology, University College London, London, UK; Ixico plc, London, UK.
Michael Flower, UCL Huntington’s Disease Centre, Queen Square Institute of Neurology, University College London, London, UK.
Davina J Hensman Moss, UCL Huntington’s Disease Centre, Queen Square Institute of Neurology, University College London, London, UK.
Peter Holmans, MRC Centre for Neuropsychiatric Genetics and Genomics, Cardiff University, Cardiff, UK.
Carlos Estevez-Fraga, UCL Huntington’s Disease Centre, Queen Square Institute of Neurology, University College London, London, UK.
Eileanoir B Johnson, UCL Huntington’s Disease Centre, Queen Square Institute of Neurology, University College London, London, UK.
Rachael I Scahill, UCL Huntington’s Disease Centre, Queen Square Institute of Neurology, University College London, London, UK.
Geraint Rees, Wellcome Centre for Human Neuroimaging, Queen Square Institute of Neurology, University College London, London, UK; Institute of Cognitive Neuroscience, University College London, London, UK.
Douglas Langbehn, Carver College of Medicine, University of Iowa, Iowa City, IA, USA.
Sarah J Tabrizi, UCL Huntington’s Disease Centre, Queen Square Institute of Neurology, University College London, London, UK; UK Dementia Research Institute at University College London, London, UK.
Track-HD Investigators:
Peter Kraus, Rainer Hoffman, Alan Tobin, Beth Borowsky, S Keenan, Kathryn B Whitlock, Sarah Queller, Colin Campbell, Chiachi Wang, Eric Axelson, Hans Johnson, Tanka Acharya, Dave M Cash, Chris Frost, Rebecca Jones, Caroline Jurgens, Ellen P ‘t Hart, Jeroen van der Grond, Marie-Noelle N Witjes-Ane, Raymund AC Roos, Eve M Dumas, Simon JA van den Bogaard, Cheryl Stopford, David Craufurd, Jenny Callaghan, Natalie Arran, Diana D Rosas, S Lee, W Monaco, Alison O’Regan, Cassie Milchman, Ellen Frajman, Izelle Labuschagne, Julie Stout, Melissa Campbell, Sophie C Andrews, Natalie Bechtel, Ralf Reilmann, Stefan Bohlen, Chris Kennard, Claire Berna, Stephen Hicks, Alexandra Durr, Cristophe Pourchot, Eric Bardinet, Kevin Nigaud, Romain Valabrègue, Stephane Lehericy, Cecilia Marelli, Celine Jauffret, Damian Justo, Blair Leavitt, Joji Decolongon, Aaron Sturrock, Alison Coleman, Rachelle Dar Santos, Aakta Patel, Claire Gibbard, Daisy Whitehead, Ed Wild, Gail Owen, Helen Crawford, Ian Malone, Nayana Lahiri, Nick C Fox, Nicola Z Hobbs, Roger Ordidge, Tracey Pepple, Joy Read, Miranda J Say, and Bernhard Landwehrmeyer
Funding
This work was supported by a Huntington’s Disease Society of America (HDSA) Human Biology fellowship award to M.P. S.J.T.’s work is supported by the UK Dementia Research Institute (DRI) which receives its funding from DRI Ltd, funded by the UK Medical Research Council, Alzheimer’s Society and Alzheimer’s Research UK. The Track-HD study was funded by the CHDI Foundation.
Competing interests
MP is an employ of IXICO plc. All other authors report no competing interests.
Supplementary material
Supplementary material is available at Brain Communications online.
References
- 1. Snowden JS. The neuropsychology of Huntington’s disease. Arch Clin Neuropsychol. 2017;32(7):876–887. [DOI] [PubMed] [Google Scholar]
- 2. Duff K, Paulsen J, Mills J, et al. Mild cognitive impairment in prediagnosed Huntington disease. Neurology. 2010;75(6):500–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Nyberg L, Lövdén M, Riklund K, Lindenberger U, Bäckman L. Memory aging and brain maintenance. Trends Cogn Sci. 2012;16(5):292–305. [DOI] [PubMed] [Google Scholar]
- 4. Stern Y. Cognitive reserve. Neuropsychologia. 2009;47(10):2015–2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vemuri P, Lesnick TG, Przybelski SA, et al. Association of lifetime intellectual enrichment with cognitive decline in the older population. JAMA Neurol. 2014;71(8):1017–1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Harris SE, Deary IJ. The genetics of cognitive ability and cognitive ageing in healthy older people. Trends Cogn Sci. 2011;15(9):388–394. [DOI] [PubMed] [Google Scholar]
- 7. Ward DD, Summers MJ, Saunders NL, Ritchie K, Summers JJ, Vickers JC. The BDNF Val66Met polymorphism moderates the relationship between cognitive reserve and executive function. Transl Psychiatry. 2015;5(6):e590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Premi E, Grassi M, van Swieten J, et al. Cognitive reserve and TMEM106B genotype modulate brain damage in presymptomatic frontotemporal dementia: A GENFI study. Brain. 2017;140(6):1784–1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Gazzina S, Grassi M, Premi E, et al. Education modulates brain maintenance in presymptomatic frontotemporal dementia. J Neurol Neurosurg Psychiatry. 2019;90(10):1124–1130. [DOI] [PubMed] [Google Scholar]
- 10. van Dellen A, Blakemore C, Deacon R, York D, Hannan AJ. Delaying the onset of Huntington’s in mice. Nature. 2000;404(6779):721–722. [DOI] [PubMed] [Google Scholar]
- 11. Trembath MK, Horton ZA, Tippett L, et al. A retrospective study of the impact of lifestyle on age at onset of Huntington disease. Mov Disord. 2010;25(10):1444–1450. [DOI] [PubMed] [Google Scholar]
- 12. Bonner-Jackson A, Long JD, Westervelt H, Tremont G, Aylward E, Paulsen JS. Cognitive reserve and brain reserve in prodromal Huntington’s disease. J Int Neuropsychol Soc. 2013;19(7):739–750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Garcia-Gorro C, Garau-Rolandi M, Escrichs A, et al. An active cognitive lifestyle as a potential neuroprotective factor in Huntington’s disease. Neuropsychologia. 2019;122:116–124. [DOI] [PubMed] [Google Scholar]
- 14. Long JD, Lee JM, Aylward EH, et al. Genetic modification of Huntington disease acts early in the prediagnosis phase. Am J Hum Genet. 2018;103(3):349–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. De Diego-Balaguer R, Schramm C, Rebeix I, et al. COMT Val158met polymorphism modulates Huntington’s disease progression. PLoS One. 2016;11(9):e0161106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lee JM, Huang Y, Orth M, et al. Genetic modifiers of Huntington’s disease differentially influence motor and cognitive domains. Am J Hum Genet. 2022;109(5):885–899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vuono R, Winder-Rhodes S, de Silva R, et al. The role of tau in the pathological process and clinical expression of Huntington’s disease. Brain. 2015;138(7):1907–1918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tabrizi SJ, Langbehn DR, Leavitt BR, et al. Biological and clinical manifestations of Huntington’s disease in the longitudinal TRACK-HD study: Cross-sectional analysis of baseline data. Lancet Neurol. 2009;8(9):791–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tabrizi SJ, Scahill RI, Durr A, et al. Biological and clinical changes in premanifest and early stage Huntington’s disease in the TRACK-HD study: The 12-month longitudinal analysis. Lancet Neurol. 2011;10:31–42. [DOI] [PubMed] [Google Scholar]
- 20. Tabrizi SJ, Reilmann R, Roos RA, et al. Potential endpoints for clinical trials in premanifest and early Huntington’s disease in the TRACK-HD study: Analysis of 24 month observational data. Lancet Neurol. 2012;11(1):42–53. [DOI] [PubMed] [Google Scholar]
- 21. Tabrizi SJ, Scahill RI, Owen G, et al. Predictors of phenotypic progression and disease onset in premanifest and early-stage Huntington’s disease in the TRACK-HD study: Analysis of 36-month observational data. Lancet Neurol. 2013;12(7):637–649. [DOI] [PubMed] [Google Scholar]
- 22. Bates GP, Dorsey R, Gusella JF, et al. Huntington disease. Nat Rev Dis Primer. 2015;1:15005. [DOI] [PubMed] [Google Scholar]
- 23. Langbehn DR, Stout JC, Gregory S, et al. Association of CAG repeats with long-term progression in Huntington disease. JAMA Neurol. 2019;76:1375–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Moss DJH, Pardiñas AF, Langbehn D, et al. Identification of genetic variants associated with Huntington’s disease progression: A genome-wide association study. Lancet Neurol. 2017;16(9):701–711. [DOI] [PubMed] [Google Scholar]
- 25. Purcell S, Neale B, Todd-Brown K, et al. PLINK: A tool set for whole-genome association and population-based linkage analyses. Am J Hum Genet. 2007;81(3):559–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Genetic Modifiers of Huntington’s Disease (GeM-HD) Consortium . Identification of genetic factors that modify clinical onset of Huntington’s disease. Cell. 2015;162(3):516–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Flower M, Lomeikaite V, Ciosi M, et al. MSH3 Modifies somatic instability and disease severity in Huntington’s and myotonic dystrophy type 1. Brain. 2019;142(7):1876–1886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Genetic Modifiers of Huntington’s Disease (GeM-HD) Consortium . CAG Repeat not polyglutamine length determines timing of Huntington’s disease onset. Cell. 2019;178(4):887–900.e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Buchman AS, Yu L, Boyle PA, Schneider JA, De Jager PL, Bennett DA. Higher brain BDNF gene expression is associated with slower cognitive decline in older adults. Neurology. 2016;86(8):735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lim YY, Hassenstab J, Cruchaga C, et al. BDNF Val66met moderates memory impairment, hippocampal function and tau in preclinical autosomal dominant Alzheimer’s disease. Brain. 2016;139(10):2766–2777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lim YY, Hassenstab J, Goate A, et al. Effect of BDNFVal66Met on disease markers in dominantly inherited Alzheimer’s disease. Ann Neurol. 2018;84(3):424–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Zuccato C, Cattaneo E. Role of brain-derived neurotrophic factor in Huntington’s disease. Prog Neurobiol. 2007;81(5):294–330. [DOI] [PubMed] [Google Scholar]
- 33. Plotkin JL, Day M, Peterson JD, et al. Impaired TrkB receptor signaling underlies corticostriatal dysfunction in Huntington’s disease. Neuron. 2014;83(1):178–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ward DD, Andel R, Saunders NL, et al. The BDNF Val66Met polymorphism moderates the effect of cognitive reserve on 36-month cognitive change in healthy older adults. Alzheimers Dement Transl Res Clin Interv. 2017;3(3):323–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Vuono R, Kouli A, Legault EM, et al. Association between toll-like receptor 4 (TLR4) and triggering receptor expressed on myeloid cells 2 (TREM2) genetic variants and clinical progression of Huntington’s disease. Mov Disord. 2020;35(3):401–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bettencourt C, Hensman-Moss D, Flower M, et al. DNA repair pathways underlie a common genetic mechanism modulating onset in polyglutamine diseases. Ann Neurol. 2016;79(6):983–990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Stefansson H, Helgason A, Thorleifsson G, et al. A common inversion under selection in Europeans. Nat Genet. 2005;37(2):129–137. [DOI] [PubMed] [Google Scholar]
- 38. Valenzuela MJ, Sachdev P. Brain reserve and dementia: A systematic review. Psychol Med. 2006;36(4):441–454. [DOI] [PubMed] [Google Scholar]
- 39. Pool LR, Weuve J, Wilson RS, Bültmann U, Evans DA, Mendes de Leon CF. Occupational cognitive requirements and late-life cognitive aging. Neurology. 2016;86(15):1386–1392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Penney JB, Vonsattel JP, Macdonald ME, Gusella JF, Myers RH. CAG repeat number governs the development rate of pathology in Huntington’s disease. Ann Neurol. 1997;41(5):689–692. [DOI] [PubMed] [Google Scholar]
- 41. Langbehn D, Brinkman R, Falush D, Paulsen J, Hayden M, on behalf of an International Huntington’s Disease Collaborative Group . A new model for prediction of the age of onset and penetrance for Huntington’s disease based on CAG length. Clin Genet. 2004;65(4):267–277. [DOI] [PubMed] [Google Scholar]
- 42. Freeborough PA, Fox NC, Kitney RI. Interactive algorithms for the segmentation and quantitation of 3-D MRI brain scans. Comput Methods Programs Biomed. 1997;53(1):15–25. [DOI] [PubMed] [Google Scholar]
- 43. Hobbs NZ, Henley SMD, Wild EJ, et al. Automated quantification of caudate atrophy by local registration of serial MRI: Evaluation and application in Huntington’s disease. NeuroImage. 2009;47(4):1659–1665. [DOI] [PubMed] [Google Scholar]
- 44. Freeborough PA, Fox NC. Modeling brain deformations in Alzheimer disease by fluid registration of serial 3D MR images. J Comput Assist Tomogr. 1998;22(5):838–843. [DOI] [PubMed] [Google Scholar]
- 45. Ashburner J, Friston KJ. Voxel-based morphometry—The methods. NeuroImage. 2000;11(6):805–821. [DOI] [PubMed] [Google Scholar]
- 46. Johnson EB, Byrne LM, Gregory S, et al. Neurofilament light protein in blood predicts regional atrophy in Huntington disease. Neurology. 2018;90(8):e717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Stern Y. Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol. 2012;11(11):1006–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Hensman Moss DJ, Flower MD, Lo KK, et al. Huntington’s disease blood and brain show a common gene expression pattern and share an immune signature with Alzheimer’s disease. Sci Rep. 2017;7(1):44849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Zuccato C, Cattaneo E. Brain-derived neurotrophic factor in neurodegenerative diseases. Nat Rev Neurol. 2009;5(6):311–322. [DOI] [PubMed] [Google Scholar]
- 50. Spires TL, Grote HE, Varshney NK, et al. Environmental enrichment rescues protein deficits in a mouse model of Huntington’s disease, indicating a possible disease mechanism. J Neurosci. 2004;24(9):2270–2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Swami M, Hendricks AE, Gillis T, et al. Somatic expansion of the Huntington’s disease CAG repeat in the brain is associated with an earlier age of disease onset. Hum Mol Genet. 2009;18(16):3039–3047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Ciosi M, Maxwell A, Cumming SA, et al. A genetic association study of glutamine-encoding DNA sequence structures, somatic CAG expansion, and DNA repair gene variants, with Huntington disease clinical outcomes. EBioMedicine. 2019;48:568–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mouro Pinto RM, Arning L, Giordano JV, et al. Patterns of CAG repeat instability in the central nervous system and periphery in Huntington’s disease and in spinocerebellar ataxia type 1. Hum Mol Genet. 2020;29(15):2551–2567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Goold R, Flower M, Moss DH, et al. FAN1 modifies Huntington’s disease progression by stabilizing the expanded HTT CAG repeat. Hum Mol Genet. 2019;28(4):650–661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Williams-Gray CH, Evans JR, Goris A, et al. The distinct cognitive syndromes of Parkinson’s disease: 5 year follow-up of the CamPaIGN cohort. Brain. 2009;132(11):2958–2969. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Track-HD data are available upon request after appropriate data use agreements are signed by the study funder, the CHDI Foundation. Please direct inquiries to info@chdifoundation.org.