Abstract
The coronavirus disease (COVID-19) presented a unique opportunity for the World Health Organization (WHO) to utilise public health intelligence (PHI) for pandemic response. WHO systematically captured mainly unstructured information (e.g. media articles, listservs, community-based reporting) for public health intelligence purposes. WHO used the Epidemic Intelligence from Open Sources (EIOS) system as one of the information sources for PHI. The processes and scope for PHI were adapted as the pandemic evolved and tailored to regional response needs. During the early months of the pandemic, media monitoring complemented official case and death reporting through the International Health Regulations mechanism and triggered alerts. As the pandemic evolved, PHI activities prioritised identifying epidemiological trends to supplement the information available through indicator-based surveillance reported to WHO. The PHI scope evolved over time to include vaccine introduction, emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants, unusual clinical manifestations and upsurges in cases, hospitalisation and death incidences at subnational levels. Triaging the unprecedented high volume of information challenged surveillance activities but was managed by collaborative information sharing. The evolution of PHI activities using multiple sources in WHO’s response to the COVID-19 pandemic illustrates the future directions in which PHI methodologies could be developed and used.
Keywords: event-based surveillance, COVID-19, public health intelligence, SARS-CoV-2, epidemiology, surveillance
Introduction
The World Health Organization (WHO) uses public health intelligence (PHI) as one element of its approach to improve population health. A PHI approach encompasses the detection, verification, risk assessment and investigation of events that pose a potential risk to human health, and communicating this information for effective decision making and action [1-3]. Public health intelligence requires the systematic synthesis of different types and sources of information, which are gathered through indicator-based surveillance (IBS), which includes counts of patient counts, cases, or laboratory diagnoses, and event-based surveillance (EBS) which comprises predominantly unstructured information from other sources, including from non-health sectors, that are used for public health surveillance purposes, such as media articles, listservs and community-based reporting [4-6]. We describe how the PHI activities for the coronavirus disease (COVID-19) contributed to WHO’s COVID-19 response, the evolution of PHI activities from December 2019 to December 2021, and lessons for the future.
The role of public health intelligence in the WHO response to the COVID-19 pandemic
Event-based surveillance involves the detection, triage and verification of new public health threats and changes in ongoing events. Signals, defined as raw data or information with potential acute human health risk [7], are detected, risks-assessed, documented and followed daily, based on predefined criteria.
One of the tools used by WHO for PHI to monitor all hazards, including COVID-19, is the Epidemic Intelligence from Open Sources (EIOS) system [8]. Here, publicly available online information such as media articles, government websites and social media are monitored. Between December 2019 and December 2021, the public health intelligence generated through EIOS and other sources provided important information for epidemiological interpretation and risk assessment to guide WHO’s COVID-19 response (Figure 1).
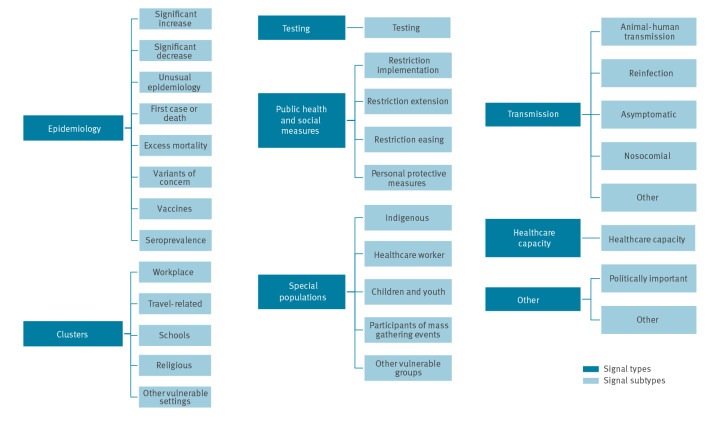
Figure 1.
Categorisation of COVID-19 Public Health Intelligence activities, as of December 2021a
a These are the types and subtypes of categories detected by the Global team within the WHO headquarters COVID-19 Incident Management Support Team, and do not represent all types of PHI information detected by WHO. The scope of signals is adapted based on the evolution of the pandemic, and additional signal types may be monitored and detected based on surveillance and response needs.
With the emergence of COVID-19, additional event-specific criteria were established and adapted over time to reflect the pandemic’s evolution and the evolving response needs. These additional criteria were determined as a result of a discussion between a team of WHO epidemiologists who took into account surveillance objectives and scope, the epidemiological context in which the pandemic took place, and available human resources. The criteria were continuously reassessed every several months, or when the characteristics of the pandemic changed. COVID-19 PHI provided a more complete understanding of disease dynamics rather than relying on IBS alone.
Epidemic Intelligence from Open Sources system
The EIOS system was one component key for WHO PHI activities during the COVID-19 pandemic. EIOS is an adaptable, user-oriented and constantly evolving web-based system designed to support, augment and accelerate PHI activities. It is used by communities and organisations from national to international levels [9-11]. The EIOS system is one of the tool to monitor open-source information in emergencies. PHI teams across WHO offices use the system to detect unusual or unexpected signals at various geographic levels. The system gathers pieces of information in multiple languages on a near real-time basis from over 13,000 sources. To improve geographical and thematic coverage, information sources are continuously reviewed and added, in collaboration with user communities such as national health authorities and partner organisations. Individuals and user communities can tailor the system by defining selection criteria based on parameters which include potential health threats, time, country, locations, sources and language. Furthermore, users can pin, flag and export selected articles to collaborate and communicate with stakeholders according to their data sharing needs. Users can also provide input to add new categories of interest, modify the category definitions and add sources as emergencies evolve.
Evolution of public health intelligence activities during different stages of the COVID-19 pandemic
Prior to the detection of COVID-19, the WHO was conducting standardised EBS daily, employing an all-hazards approach and using official government reports, EIOS and other sources of information. Building on this established mechanism at the onset of the pandemic, the WHO intensified EBS to track initial cases and deaths from COVID-19 while an IBS system was being established to complement International Health Regulations (2005) reporting mechanisms. Due to the volume of information, the number of analysts dedicated to screening for COVID-19-related events was increased. In addition, a separate set of filter criteria was created within the EIOS system exclusively for monitoring information related to COVID-19, which reduced the volume of articles on the routine EBS boards. Systematic information sharing for COVID-19-related signals and events was put in place among WHO country offices, Regional offices and headquarters.
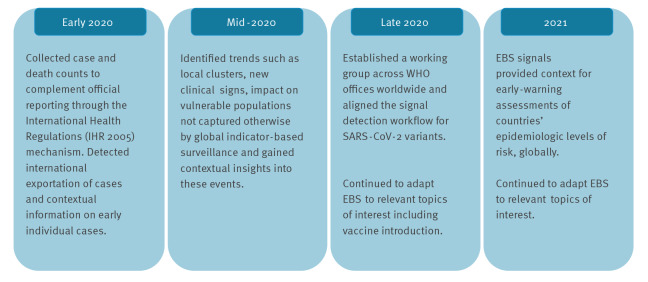
Since the first detection of COVID-19 cases, the processes and scope for COVID-19 EBS activities have evolved to reflect changing response priorities. During the early months of the pandemic, EBS complemented official COVID-19 case and death reporting according to the International Health Regulations (2005) [3] and triggered verification processes and responses. As the pandemic evolved, PHI activities evolved to provide a more comprehensive understanding of the pandemic that was not readily captured by one type of surveillance alone (Figure 2).
Figure 2.
The adaptation of the World Health Organization’s public health intelligence activities for COVID-19, 2020–2021
COVID-19: coronavirus disease; PHI: public health intelligence; SARS-CoV-2: severe acute respiratory syndrome coronavirus 2; WHO: World Health Organization.
The scope of PHI evolved over time to include vaccine introduction, emergence of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) variants, unusual clinical manifestations, upsurges in cases, hospitalisations and deaths at subnational level. Granular information collected through PHI provided valuable contextual information, which is not always available through IBS sources alone, including the burden on the health system and at-risk and vulnerable groups such as healthcare workers, rapid response teams, indigenous populations, children, pregnant women, elderly people and refugees.
The PHI approach combined signals detected via EBS and IBS along with contextual information which provided WHO response teams that supported the assessment and interpretation of COVID-19 epidemiological situations at national and subnational level. Analysts working on COVID-19 PHI activities validated and risk-assessed relevant signals, and communicated them through internal and external information products, including WHO Regional weekly briefing documents and the WHO’s weekly epidemiological update on COVID-19 [12]. In addition, PHI supported the interpretation of epidemiological trends collected through IBS which were shared publicly on the global COVID-19 dashboard [13], as well as other reports and dashboards.
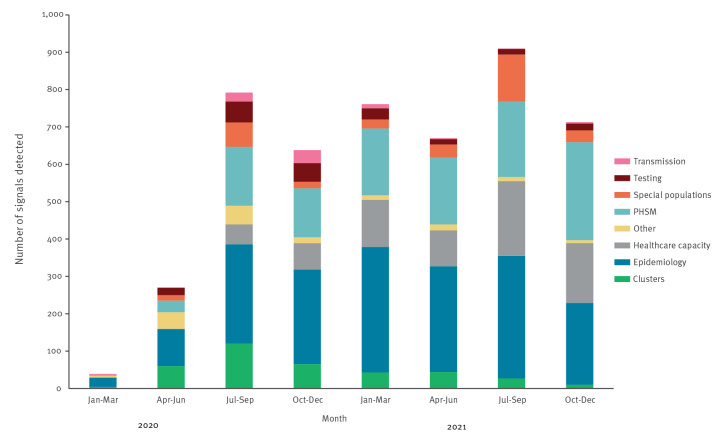
Between 31 December 2019 and 31 December 2021, 4,794 COVID-19 signals were detected and followed up by the WHO at the global level using the EIOS system (Figure 3).
Figure 3.
COVID-19 public health intelligence detected by the World Health Organization at global level by category type, as of December 2021
COVID-19: coronavirus disease; PHI: public health intelligence; PHSM: public health and social measures; WHO: World Health Organization.
In May 2021, the WHO developed a situational alert system to support the early detection of countries where immediate action may help to mitigate the impact of a COVID-19 surge on morbidity and/or mortality. From May 2021 to June 2022, a collaborative, multi-disciplinary, mixed-methods process took place weekly, integrating information and input from teams across the three levels of the organisation. The first stage of the situational alert system employed an automated statistical risk assessment algorithm, based on daily incidence of cases and deaths, to predict COVID-19 disease severity within the near future. This produced an initial alert level for each country. The second stage integrated a PHI-based qualitative context assessment, which provided important information including pressure on the healthcare system; the impact of other concerning epidemiological signals such as concurrent outbreaks and large changes in circulating variants of concern; and the impact of factors affecting response activities such as acute events resulting in insecurity, or mass gatherings and population movement. This was combined with information on vaccination coverage, public health and social measures, and an assessment of the trust in available data for each indicator to produce a standardised recommendation for whether a country should be maintained at the initial alert level, or whether it should be updated. Based on this, teams at WHO global and regional levels jointly agreed on a final classification where the process supported a shared understanding of risk and operational priorities across the COVID-19 incident management teams at different levels of the organisation and, for specific contexts, the rapid release of response funds, distribution of oxygen, distribution of testing supplies, and technical support.
Tailoring to Regional response needs
WHO was able to effectively adapt its PHI processes and systems including EIOS to align with surveillance strategies across different WHO offices as the pandemic evolved. An example of the unique adaptations implemented at the regional level was seen in the Western Pacific Region. Here, a media statement on cases of ‘unknown viral pneumonia’ in China (the first detection of COVID-19 cases) was detected through routine EBS processes on 31 December 2019 [14]. EIOS picked up a media report on this same signal in the Programme for Monitoring Emerging Diseases [15] on the same day. Subsequently, WHO rapidly established COVID-19-specific global surveillance activities to detect other related signals, focusing PHI to the needs and perceived risks within each Region. In the African Region, PHI was crucial in detecting signals of countries’ first cases and checking official statements for cases reported in the media. In the Region of the Americas, PHI was useful in detecting and contextualising outbreaks in cross-border areas, among cruise ship passengers and in congregate care settings and schools. The Eastern Mediterranean Region conducted PHI to detect upsurges in case or death incidence, track public health and social measures, particularly for schools, and later monitor vaccine roll-out. In the European Region, PHI activities focused on special populations and potential super-spreading events, and monitored subnational trends. The South-East Asia Region used PHI to monitor health systems capacities and reports of overwhelmed mortuaries and burial grounds during upsurges in the number of deaths.
Additionally, the WHO and partners conducted PHI for mass gathering events from December 2019 to December 2021, including the Union of European Football Associations championship that took place in 11 countries in Europe, the Tokyo Olympic and Paralympic Games in Japan, Hajj in Saudi Arabia, Al-Arbaeiin in Iraq and the World Handball Championship in Spain.
Identifying strengths and weaknesses and addressing challenges
There are many strengths to the COVID-19 PHI activities implemented by WHO during the pandemic. WHO was able to develop a PHI approach throughout the course of the pandemic, used the findings to guide response activities and later to contextualise and supplement information derived from EBS and IBS as processes were established. The WHO’s PHI activities have remained flexible, scalable and resilient, adapting to the changing epidemiological context and availability of the WHO and partners’ person-time. Furthermore, the location of COVID-19 PHI activities within WHO’s Health Emergencies Programme and the Incident Management Support team structure was essential for coordinating and collaborating with key technical experts, ensuring relevancy and usefulness of information gathered, in order to better support Member States.
While the WHO’s experience with PHI during the COVID-19 pandemic illustrates its value for the timely detection of health threats [16] using multiple sources, there remain some limitations and challenges. Amid the rapid evolution of response needs, it was not possible to detect every potentially relevant piece of information across the range of topics of interest, particularly given the unprecedentedly high volume of information requiring triaging. This high volume of information necessitated an increase in the amount of person-time dedicated to COVID-19 PHI activities, while continuing to ensure sufficient resources for monitoring and detecting other public health events. Finding this balance with resource constraints proved challenging during several different phases of the pandemic. This suggests the need for continued improvement in response activities that enable public health intelligence teams to rapidly surge resources for PHI in future emergencies. While the evolving methods of PHI within the COVID-19 response are an operational strength, it also means that the type and volume of information varies throughout the course of a public health event WHO identified new technical challenges, including managing the different languages in which the information was written, their translation, identification of appropriate keywords for signal detection and the need for enhanced system support to improve signal detection. Signal detection could be improved by developing more targeted categories, and further addition of local or emerging key sources.
In response to these limitations and challenges, several initiatives have been developed to improve EBS activities for COVID-19 and other public health events. WHO offices established a COVID-19 PHI working group to strengthen collaboration, maximise resources and brainstorm solutions. From 31 March 2020 to 31 December 2021, the working group initiated a collaborative use of the EIOS system as one tool for detecting relevant information. The working group also provided regular feedback to further improve the process, including enhanced signal detection and verification, broadening of source types, geographical and language coverage and the use of tools to optimise shared workflows in rapid signal detection and monitoring. In addition to establishing the working group, WHO increased the number of personnel working on PHI, added and formalised trainings on PHI activities for COVID-19 and conducted a survey-based assessment of the system to further understand its strengths and weaknesses.
Conclusion
Public health intelligence is a rapidly evolving approach that is necessary for WHO and Member States [17]. The COVID-19 pandemic presented a unique and challenging opportunity to develop PHI approaches for pandemic monitoring and response. WHO’s experience with PHI during the pandemic illustrate as the need for continuous development of PHI approaches for effective decision making to support Member States and inform response to a public health event. It also suggests that key future improvements should include greater automation tools that enable analysts to handle large quantities of information, additional training for personnel undertaking PHI and increased PHI capacity building within Member States and WHO. This would facilitate surge capacity in the future, further methodological development for systematic filtering of relevant information and establish evaluation processes for the PHI system. Building Member States and partners’ capacities to implement PHI approaches, in addition to IBS, for new and future public health threats has already begun, and it is important to continue developing these activities. Public health professionals and institutions dedicated to strengthening PHI capacity, including WHO’s recently established Hub for Pandemic and Epidemic Intelligence, can catalyse this change and build on the momentum created by the response to the COVID-19 pandemic.
Acknowledgements
We thank Member States for their dedication to public health intelligence activities during the COVID-19 pandemic, as well as timely information sharing and collaboration with WHO. This work would not have been possible without the efforts of officers in the Health Emergencies Programme across WHO offices, including the public health intelligence team and the event-based surveillance working group.
WHO African Region Health Emergency Information and Risk Management team:
Valerie Mize, Tamayi Mlanda, Muhammad Arish Salam Bukhari, Opeayo Ogundiran, Freddy Kambale Kavoga, Jean Paul Kimenyi, Mangosa Zaza Ramazani, George Sie Williams and Dabwitso Jezreel Banda.
Funding statement
The development of this manuscript was carried out as part of work for the WHO. Funders of the WHO had no role in the design of the study, the collection, analysis, and interpretation of data and in writing the manuscript.
Conflict of interest: None declared.
Authors’ contributions: Eri Togami conducted the initial conception and design of the work, conducted all coordination of the manuscript; conducted data collection through event-based surveillance (EBS), contributed to defining signal definition and scope, conducted the analysis and produced figures, interpreted data; led the drafting, revising, finalizing of the manuscript.
Bridget Griffith conducted to the initial conception and design of the work; conducted data collection through event-based surveillance, defined EBS detection categories, interpreted the data; co-led the drafting, revising, and finalizing of all sections of the manuscript, provided technical input on evaluating the strengths and challenges of the EBS system.
Mostafa Mahran contributed to the initial conception of the project; developed the draft particularly providing technical input on daily EBS processes at WHO both from the perspectives of Regional Office and headquarters, as well as the background and rationale for conducting EBS.
Ingrid H Nezu collected, cleaned and analysed data for the EBS signal database, created figure 3; developed the draft, in particular, providing input for daily EBS processes, and details related to WHO’s epidemiologic level of risk.
Bernadette B Mirembe collected data on EBS signals during the study period; drafted and revised the manuscript, including the section on the introduction section, how EBS is conducted in the global EBS team, and related pandemic response which were triggered from improved detection of signals.
Kaja Kaasik-Aaslav and Lidia Alexandrova-Ezerska contributed to the initial set up of the EBS system, including at the onset of the pandemic and collected EBS signal data; drafted the section about EBS activities conducted routinely at WHO.
Amarnath Babu and Tika Ram Sedai contributed to the initial conception of the project; developed and revised the draft, including the section on EBS supported the COVID-19 response in the WHO South-East Asia Region.
Masaya Kato guided the design of the project; developed and revised the draft, including the section on EBS supported the COVID-19 response in the WHO South-East Asia Region.
Heidi Abbas and Mahmoud Sadek contributed to the initial conception of the project; developed and revised the draft, including the section on EBS supported the COVID-19 response in the WHO Eastern Mediterranean Region.
Pierre Nabeth guided the design of the project; developed and revised the draft, including the section on EBS supported the COVID-19 response in the WHO Eastern Mediterranean Region.
Lauren E. MacDonald and Lucía Hernández-García contributed to the initial conception of the project, collected data on SARS-CoV-2 variants of concern which was shared across WHO offices; developed and revised the draft, including the section on EBS supported the COVID-19 response in the WHO European Region.
Jeffrey Pires contributed to the initial conception of the project; developed and revised the draft, including the section on EBS supported the COVID-19 response in the WHO European Region.
Stefany Ildefonso contributed to the initial conception of the project, collected data on SARS-CoV-2 variants of concern which was shared across WHO offices; developed and revised the draft, including the section on EBS supported the COVID-19 response in the WHO Region of the Americas.
Mary Stephen, Theresa Min-Hyung Lee and Benido Impouma on behalf of the AFRO Health Emergency Information and Risk Management (HIM) team contributed to the initial conception of the project; developed and revised the draft, including the section on EBS supported the COVID-19 response in the WHO African Region.
Johannes Schnitzler supported the conception the project through discussions among members of the COVID-19 EBS working group; collected information and provided technical input on the EIOS platform; drafted the manuscript, in particular the technical characteristics of the EIOS system, such as languages, categories, number of sources that feed into the system.
Julie Fontaine supported the conception the project through discussions among members of the COVID-19 EBS working group; collected information and provided technical input on the EIOS platform; drafted the manuscript, in particular, the EIOS background and details of its use for COVID-19 EBS, and coordinated and prepared figure 1.
Tamano Matsui, Sangjun Moon, Manilay Phenxay, Viema Biaukula and Ariuntuya Ochirpure contributed to the initial conception of the project; developed and revised the draft, including the section on EBS supported the COVID-19 response in the WHO Region of the Western Pacific.
Irena Djordjevic, Hannah Brindle, Jessica Kolmer and Martina McMenamin contributed to the collection and interpretation of data, with particular focus on WHO’s situation alert system and risk assessment; drafted and reviewed the section related to WHO’s response following signal detection.
Emilie Peron contributed to the initial set up of the EBS system, including at the onset of the pandemic and collected EBS signal data; provided critical review with focus on routine EBS activities conducted at WHO before COVID-19 was detected, as well as in the acute phase of the pandemic.
Zyleen Kassamali guided the design of the project with insight from managing and leading the EBS team within the COVID-19 intelligence team; critically reviewed the draft and suggestions pertaining to resources required for conducting EBS during the pandemic response.
Blanche Greene-Cramer led the initial conception and design of the projects; co-led all coordination activities for the manuscript; managed and led the EBS team within the COVID-19 intelligence team, interpreted the data; led the drafting, revising, finalizing of all sections of the manuscript.
Esther Hamblion guided the design of the project and the manuscript, supported the interpretation of EBS signal data in line with WHO’s public health intelligence approach; reviewed and revised the manuscript critically and provided suggestions.
Philip Abdelmalik guided the design of the project and manuscript, supported the interpretation of EBS signal data and the in line with WHO’s initiative for the use of Epidemic Intelligence from Open Sources; revised the manuscript critically and provided suggestions.
Boris Pavlin guided the design of the project and manuscript in line with response activities of the epidemiology pillar of the COVID-19 incident management support team; revised the manuscript critically and provided suggestions.
Abdi Rahman Mahamud guided the design of the manuscript in line with WHO’s response to, and coordination for acute health emergencies; revised the manuscript critically and provided suggestions especially for response activities that followed signal detection.
Oliver Morgan guided the design of the project and manuscript, supported interpretation of EBS signal data and in line with WHO’s public health intelligence approach and activities for the wider health emergency information management and response; revised the manuscript critically and provided suggestions.
References
- 1.World Health Organization (WHO). Mitigating the spread of global public health threats: a review of WHO public health intelligence activities, 2018–2020. Geneva: WHO; Jul 2021. Available from: https://apps.who.int/iris/handle/10665/342528
- 2.United Nations. The United Nations Terminology Database. Public Health Intelligence. New York: United Nations. [Accessed: 7 Jan 2022]. Available from: https://unterm.un.org/unterm/display/record/who/na/2b406931-845d-4e66-a6fe-b464ee3d6573
- 3.World Health Organization (WHO). International Health Regulations (2005). Geneva: WHO; Jan 2008. Available from: https://www.who.int/publications-detail-redirect/9789241580410.
- 4.Joint Research Centre. Institute for the Protection and the Security of the Citizen. Linge J, Belyaeva J, Mantero J. How to maximise event-based surveillance web-systems: the example of ECDC/JRC collaboration to improve the performance of MedISys. Luxembourg: Publications Office of the European Union; May 2011. Available from: https://data.europa.eu/doi/10.2788/69804
- 5.Centers for Disease Control and Prevention (CDC). Event-based Surveillance. Atlanta: CDC. [Accessed: 14 Jan 2022]. Available from: https://www.cdc.gov/globalhealth/healthprotection/gddopscenter/how.html
- 6. Barboza P, Vaillant L, Le Strat Y, Hartley DM, Nelson NP, Mawudeku A, et al. Factors influencing performance of internet-based biosurveillance systems used in epidemic intelligence for early detection of infectious diseases outbreaks. PLoS One. 2014;9(3):e90536. 10.1371/journal.pone.0090536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization (WHO). Early detection, assessment and response to acute public health events: implementation of early warning and response with a focus on event-based surveillance, interim version. Geneva: WHO; 2014. Available from: http://apps.who.int/iris/bitstream/handle/10665/112667/WHO_HSE_GCR_LYO_2014.4_eng.pdf;jsessionid=1603103B3B719CFC0A03F6B985D9BA01?sequence=1
- 8.World Health Organization (WHO). Weekly epidemiological update on COVID-19 - 15 June 2021. Geneva: WHO; Jun 2021. Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---15-june-2021
- 9.World Health Organization (WHO). Epidemic Intelligence from Open Sources (EIOS). Geneva: WHO. [Accessed: 26 Aug 2021]. Available from: https://www.who.int/initiatives/eios
- 10.World Health Organization (WHO). Epidemic Intelligence from Open Sources Newsletter. Geneva: WHO; April 2021. Available from: https://www.who.int/publications/m/item/eios-newsletter-april-2021
- 11.World Health Organization (WHO). Epidemic Intelligence from Open Sources Newsletter. Geneva: WHO; Jul 2021. Available from: https://www.who.int/publications/m/item/eios-newsletter-july-2021
- 12.World Health Organization (WHO). Coronavirus Disease (COVID-19) Situation Reports. Geneva: WHO. [Accessed: 2 Dec 2021]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
- 13.World Health Organization (WH0). WHO Coronavirus (COVID-19) Dashboard. Geneva: WHO. [Accessed: 15 Dec 2021]. Available from: https://covid19.who.int/
- 14.World Health Organization (WHO). Timeline: WHO’s COVID-19 response. Geneva: WHO. [Accessed: 17 Dec 2021] Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline
- 15.International Society for Infectious Diseases (ISID). Program for Monitoring Emerging Diseases (ProMED). Massachusetts: ISID. [Accessed: 24 Jun 2022]. Available from: https://promedmail.org/
- 16. Yan SJ, Chughtai AA, Macintyre CR. Utility and potential of rapid epidemic intelligence from internet-based sources. Int J Infect Dis. 2017;63:77-87. 10.1016/j.ijid.2017.07.020 [DOI] [PubMed] [Google Scholar]
- 17. Morgan OW, Abdelmalik P, Perez-Gutierrez E, Fall IS, Kato M, Hamblion E, et al. How better pandemic and epidemic intelligence will prepare the world for future threats. Nat Med. 2022;28(8):1526-8. 10.1038/s41591-022-01900-5 [DOI] [PMC free article] [PubMed] [Google Scholar]