ABSTRACT
Background:
Many analgesic modalities have been investigated in pediatrics for thoracotomy. We studied the analgesic efficacy of unilateral continuous ultrasound-guided erector spinae plane block (ESPB) compared to a thoracic epidural in pediatric patients undergoing thoracotomy.
Materials and Methods:
A prospective, randomized, observer-blinded, controlled study. Pediatric patients (2–7 years) scheduled for right or left thoracotomy under general anesthesia (GA) were enrolled in the study. We randomly assigned patients into two groups: The thoracic epidural analgesia (TEA) group received GA with an epidural catheter. The ESPB group received GA with a unilateral ultrasound-guided erector spinae plane catheter. The primary outcome was postoperative cumulative opioid consumption for 24 h.
Results:
The total intraoperative fentanyl requirement was 35.4 ± 11.44 μg in the TEA group and 30.4 ± 9.08 μg in the ESPB group (t-value − 1.53013, P value: 0.134). The total postoperative fentanyl requirement was comparable in both the groups and clinically nonsignificant (44 ± 2.82 in the TEA group vs. 44.25 ± 13.72 in the ESPB group, t-value = −0.02412, P = 0.981). The median (IQR) Face, Legs, Activity, Cry, and Consolability (FLACC) score at 0, 2, 4, 8, 12, and 24 h time points in the ESPB was equivalent to the TEA group. At 6 h time point, the TEA group had a significantly lower FLACC score than the ESPB group (1[1.75, 1] in the TEA group and 2 [2, 1] in the ESPB group, P value = .02, U = 117.5, z-score = −2.218). The complications were higher in the TEA group (urine retention 20% and hypotension 40%) than in the ESPB group (0 and 0%).
Conclusions:
This study shows that the ESPB provides similar postoperative analgesia to the TEA in pediatric patients undergoing thoracotomy. The ESPB is simpler, faster, and has a lower complication rate.
Keywords: Nerve block, pediatrics, thoracic epidural, thoracotomy
INTRODUCTION
Thoracotomy is widely known to cause severe acute pain.[1] This pain can be very distressing for both children and their parents. If not treated properly, it may acutely cause ventilation-perfusion disorder and hypoxemia, together with a change in lung mechanics.[2] It may lead to a delay in recovery, with some long-term sequelae. As a part of multimodal analgesia, many regional blocks have been described.[3,4] Epidural analgesia is considered the gold standard for post-thoracotomy pain relief but may have side effects. Associated complications like hypotension, urinary retention, nausea, itching, pruritus, and malposition of the catheter can limit its utility.[5] Of note, punctures in children are usually performed after induction of general anesthesia (GA) or under sedation; these patients cannot communicate. Therefore, utmost attention has to be paid to any indirect signs of possible complications. An alternative, effective, and safer method of analgesia would be preferable. The thoracic erector spinae plane block (ESPB) seems to be the answer. In adults, there are trials reporting analgesic benefits of this block in thoracotomy.[6,7,8] The usefulness of the ESPB in children for thoracotomy has been reported in a few case reports.[9,10] There is still a paucity of evidence purporting the benefits and safety of ESPB in pediatric patients. Our study is the first prospective randomized trial to investigate the ESPB compared to the gold standard thoracic epidural for postoperative analgesia for pediatric thoracotomies. We hypothesized that ultrasound-guided ESPB performed at the level of T5, the transverse process would be equivalent to the thoracic epidural for postoperative analgesia for thoracotomies. The primary endpoint was total fentanyl consumption for 24 h in the postoperative period. The secondary endpoints were pain scores at different time points, total intraoperative fentanyl consumption, time for first rescue analgesia, and any reported complications.
MATERIALS AND METHODS
This department-supported, prospective, randomized, controlled, double-blind study was registered with the Clinical Trials Gov (CTRI/2019/04/018797) after ethical clearance by the institutional ethical committee (440/IEC/IGIMS/2018 dated 08/08/2018). The enrollment was started following these approvals. The study initiation and completion dates were May 1, 2019, and February 6, 2020, respectively.
Inclusion criteria
Any patient between 2 and 7 years posted for the right or left thoracotomy to be done under GA.
Exclusion criteria
Children who had any coagulation abnormality, raised intracranial pressure, bilateral thoracotomy, deformity of the thoracolumbar spine, or local infection at the site of catheter placement were excluded.
Written informed consent was obtained from parents or legal guardians before study participation. The participants were randomly assigned to one of the two groups. One group was placed thoracic epidural catheter, and the other group was placed unilateral erector spinae plane catheter.
Group TEA—Thoracic epidural catheter was secured.
Group ESPB—Unilateral erector spinae plane catheter was secured.
The participants were randomly assigned to one of the two groups. The randomization was performed using computer-generated random number tables, and an open list of random numbers carried out the treatment group allocation. Preoperatively, all children were premedicated using oral midazolam (0.5 mg/kg). In the operating room, following standard monitorization with pulse oximetry, electrocardiography, and noninvasive blood pressure measurement, anesthesia was induced with 8% sevoflurane and 50% air in the oxygen. A 24/22-gauge intravenous (IV) cannula was then inserted, fentanyl 2 μg/kg, and atracurium (0.5 mg/kg) was administered for anesthesia induction. The airway was secured with a single-use endotracheal tube (Portex, Maidenhead, UK). The anesthesia maintenance was performed with sevoflurane 2% in 50% nitrous oxide and oxygen. No additional opioid or drug was used during surgeries except if the heart rate (HR) increased 15% above the baseline level. An anesthetist in the study was responsible for perioperative anesthesia management in line with the departmental guideline. At the end of the surgery, all patients received acetaminophen 15 mg/kg IV for postoperative analgesia. All blocks were performed after securing the airway, before the start of the surgery only by the consultants with adequate experience of giving these blocks in the pediatric patients. The blocks were performed using an ultrasound machine (Sonosite, Bothwell, USA) equipped with a large bandwidth, a multifrequency linear probe (6–19 MHz).
TEA technique
Ultrasound was not used for the placement of epidural catheters. Patients were placed in the lateral position for the TEA block. Following skin preparation with 10% povidone-iodine, an epidural catheter was inserted at T6-9 intervertebral space through 19 G Tuohys needle. The epidural space was identified by the loss of resistance technique. After insertion of the 22 G epidural catheter, 0.25% bupivacaine in a dose of 0.5 mL/kg was given.[4] Postoperatively, epidural analgesia was maintained by continuous infusion of 0.25% bupivacaine infused at 0.1 mL/kg/h for 24 h.
ESPB technique
The patients were placed in the lateral position for the ESPB. Following skin preparation with 10% povidone-iodine, the ultrasound probe was placed 1–2 cm lateral to the midline at the T4 level. The T5 level was identified by counting upward from the sacrum. Following identification of the erector spinae muscle (ESM) and transverse process, a 19 G Tuohys needle was inserted deep into the ESM in a craniocaudal direction, using an in-plane technique [Figure 1a]. The correct needle position was confirmed with the administration of 0.5–1 mL LA [Figure 1b]. Then a 22 G catheter was secured in the space through that needle. A precalculated dose (0.5 mL/kg) of 0.25% bupivacaine (limited to a maximum dose of 20 mL) was injected deep into the ESM for block performance. Postoperatively, analgesia was maintained by continuous infusion of 0.25% bupivacaine infused at 0.1 mL/kg/h for 24 h.
Figure 1.
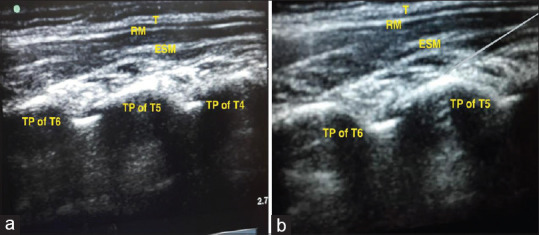
(a) Localization of the transverse process of T5 vertebrae and other structures for the erector spinae plane block. T: Trapezius, RM: Rhomboideus major, ESM: Erector spinae muscle, TP: Transverse process. (b) The tip of the needle between the erector spinae muscle and transverse process
The time for the execution of the block was noted by an independent observer. For ESPB, the execution time was the sum of the time spent in imaging (the interval between the contact of the ultrasound probe and the acquisition of satisfactory image) and the time from the needle prick on the skin to the securement of the catheter on the skin. For TEA, the execution time was the time from the needle prick on the skin to the securement of the catheter on the skin. The case was excluded if the accidental intravascular placement of the needle or catheter occurred in any patient in either group. Postoperative chest X-ray was done in all the patients to confirm or to rule out accidental pneumothorax. The success of the block was decided by an increase in the HR at the surgical incision. If the HR increased above 20 bpm, 1 μg/kg of fentanyl was given. The failed block was defined as a total intraoperative need of more than 4 μg/kg of fentanyl.[4] Hypotension, defined as a decrease in the blood pressure of more than 20% of the baseline value, was treated with intravenous fluid bolus and increments of intravenous ephedrine. Hemodynamic variables were recorded every 10 min intraoperatively and every 2 h postoperatively. Emesis was treated with IV 0.1 mg/kg ondansetron. A resident doctor (blinded to the study) performed pain evaluation using the FLACC scores in the postoperative recovery room and on the ward.
The FLACC scores were recorded at postoperative 0, 1, 3, 6, 8, 12, and 24 h. Rescue analgesia was planned based on the patients' FLACC scores. Fentanyl 1 μg/kg IV was given as rescue analgesia in the case of FLACC scores above 3. The analgesic requirements in the first 24 h postoperatively, time to first analgesic, and any reported complications were recorded.
As we could not find any previous study comparing ESPB and the pediatric patients, we decided to conduct this pilot study. Following a benchmark study published by Juliuous SA, et al.[11] we conducted a pilot study taking 22 patients in each group. We performed these two procedures as mentioned in the methodology. The post hoc analysis was performed using the total postoperative requirement obtained from the present study with an alpha error (Type 1) of 0.05 and calculated the beta error (Type II) being 80.4%.
All statistical analyses were performed using the IBM SPSS for Windows version 20.0 software (IBM Corp, Armonk, NY, USA). The Shapiro-Wilk's test was used to test the normality of data distribution. The continuous variables were expressed as mean ± standard deviation, and median values (25th–75th percentiles), and categorical variables were expressed as counts (percentages). The non-normally distributed continuous variables were compared between the groups using the Mann–Whitney U test. The categorical variables were compared between the groups using the Chi-square test or Fisher's exact test. Two-sided P values <0.05 were considered statistically significant.
RESULTS
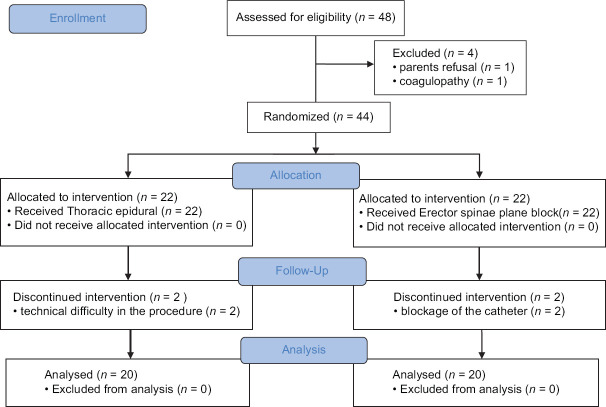
Forty-eight patients were screened for the study. Four patients were excluded; three because of parental refusal and one due to coagulopathy. Forty-four patients were randomized. Patients with failed block due to technical problems (two in the TEA group, 0 in the ESPB group) and catheter blockage (two in the ESPB group) were not included in the final analysis. None of the patients in any group required more than 4 μg/kg opioid in the intraoperative period thus indicating non-failure of the block. Thus, 40 patients completed the study and were involved in the final analysis as could be seen in the CONSORT 2010 statement [Figure 2]. Twenty patients in both groups were subjected to analysis. The patient's demographic data, type of surgery, and duration of anesthesia were comparable in both groups [Table 1].
Figure 2.
CONSORT diagram
Table 1.
Demographic data of the studied groups
| Thoracic epidural analgesia (TEA) n=20 | Erector spinae plane block (ESPB) n=20 | |
|---|---|---|
| Age (years) | 4.45±0.9 | 4.4±1.35 |
| Gender (M/F) | 15/5 | 15/5 |
| Weight (kg) | 15.6±3.6 | 14.7±3.2 |
| Duration of surgery (min) | 168.3±28.3 | 172.0±26.8 |
| Type of surgery, n (%) | ||
| 13 (65%) | 14 (70%) | |
| Lobectomy segmentectomy | 7 (35%) | 6 (30%) |
Data presented as mean±SD or patient’s number or number (percentage)
The total intraoperative fentanyl requirement was 35.4 ± 11.44 μg in the TEA group and 30.4 ± 9.08 μg in the ESPB group (t-value − 1.53013, P value 0.134). The total postoperative fentanyl requirement was comparable in both the groups and clinically nonsignificant (44 ± 2.82 μg in the TEA group vs. 44.25 ± 13.72 μg in the ESPB group, t-value = −0.02412 P = 0.981) [Table 2]. The number of patients requiring rescue analgesic was comparable in both the groups (10% vs. 20%, respectively, in the TEA and ESPB groups, P = 0.3899, 95% CI (0.4119–9.7119)] [Table 2]. The pain scores were comparable in both the groups except at 6 h time point. At 0-2-4-8-12-24 h postoperative time, only minor statistically insignificant differences were found between the TEA and ESPB groups (P = 0.105, 0.218, 0.081, 0.091, 0.250, and 0.060, respectively). At 6 h postoperative period, only clinically difference in the FLACC score was found (U = 117.5 z-score = −2.21811, P = 0.026) [Table 3].
Table 2.
Perioperative analgesia consumption in the study groups
| Thoracic epidural analgesia (TEA) n=20 | Erector spinae plane block group (ESPB) n=20 | Relative risk | t-Statistic and P value (95% confidence limit) | |
|---|---|---|---|---|
| Total intraoperative fentanyl (µg) | 35.4±11.44 | 30.4±9.08 | t-value -1.530, P value- 0.134 | |
| Postoperative fentanyl consumption (µg) | 44±2.82 | 44.25±13.72 |
t-value -0.02412 P-value -0.981 |
|
| Number of patients who required fentanyl (%) | 2 (10%) | 4 (20%) | 2.000 | P-value- 0.3899 (0.4119-9.7119) |
Data presented as mean±SD or number (percentage)
Table 3.
Comparison of FLACC scores in the studied group in median and interquartile range
| Time points | Thoracic epidural analgesia (TEA) n=20 | Erector spinae plane block Group (ESPB) n=20 | U-value and z-score | P-value |
|---|---|---|---|---|
| 0 h | 1 [2, 1] | 2 [2, 1] | 139.5 | 0.105 |
| -1.62301 | ||||
| 2 h | 1 [2, 1] | 2 [2, 1] | 154 | 0.218 |
| -1.23078 | ||||
| 4 h | 1 [1.75, 1] | 2 [2, 1] | 135 | 0.081 |
| -1.74473 | ||||
| 6 h | 1 [1.75, 1] | 2 [2, 1] | 117.5 | 0.026* |
| -2.21811 | ||||
| 8 h | 1 [1.75, 1] | 2 [2, 1] | 137 | 0.091 |
| -1.69063 | ||||
| 12 h | 1 [1.75, 1] | 1.5 [2, 1] | 157 | 0.250 |
| -1.14963 | ||||
| 24 h | 1 [1, 1] | 1.5 [2, 1] | 130 | 0.060 |
| -1.87998 |
*P-value<0.05 is significant. Mann–Whitney U test applied
The block execution time was 7.14 ± 1.007 min in the TEA group and 4.43 ± 0.69 min in the ESPB group and the difference was significant (t-value − 12.913, P < 0.00001). The complications were higher in the TEA group (urine retention 20% and hypotension 40%) than in the ESPB group (0 and 0%) [Table 4]. There were no ESPB-related adverse events, including pneumothorax, bleeding, motor-power weakness, or local anesthetic (LA) toxicity.
Table 4.
Comparison of complication in the studied group
| Thoracic epidural analgesia (TEA) n=20 | Erector spinae plane block group (ESPB) n=20 | Relative risk | t-Statistic and P value (95% confidence limit) | |
|---|---|---|---|---|
| Urinary retention | 4 (10%) | 0 (0%) | 5.0000 | 1.060 P=0.2891 0.2551 to 98.0032 |
| Hypotension | 8 (40%) | 0 (0%) | 17.0000 | 1.992 P=0.0463 (1.0469 to 276.0432) |
Data presented as number (percentage)
DISCUSSION
The finding of this study showed a comparable postoperative opioid-sparing effect of the TEA and ESPB in pediatric thoracotomy. The total intraoperative fentanyl requirement was 35.4 ± 11.44 μg in the TEA group and 30.4 ± 9.08 μg in the ESPB group and the total cumulative postoperative fentanyl requirement was 30.4 ± 9.08 μg in the ESPB group and 35.4 ± 11.44 μg in the TEA group. During the intraoperative period, all 40 patients in both groups required supplemental opioids but the total dose was not above 4 μg/kg in any patient. The pain scores at most time points were also comparable in both groups. The children requiring rescue analgesia were, respectively, 2 (TEA group) and 4 (ESPB group) in both the study groups and the difference was again clinically insignificant. In thoracotomy, if regional analgesia is not adequate, the opioid becomes the mainstay for pain management. The use of opioids would be accompanied by opioid-related side effects, such as respiratory depression, nausea and vomiting, pruritus, and delayed bowel emptying. Thus, whenever possible, the use of opioids should be minimized. The use of thoracic epidural is already established for its opioid-sparing analgesia in thoracotomy, ESPB has shown promising results in the present study.
The time required for the execution of the block was faster in the ESPB group (4.43 ± 0.69 min) compared to the TEA which nearly took double time to secure the thoracic epidural catheter (7.14 ± 1.007 min). The incidence of hypotension and urinary retention was seen in a higher percentage of patients in the TEA group. Though the analgesia was comparable in both the groups, the presence of these complications in the TEA group made it a less favorable block in our study.
The ESPB has garnered an enormous interest in regional anesthesia practice. The use of this block has involved both adults and pediatrics. Forero et al.[12] proposed this block in which LA is deposited in the fascial plane deep to the ESM and just superficial to the tip of the transverse process. It achieves an extensive multi-dermatomal sensory block of the posterior, lateral, and anterior thoracic walls.[13,14,15] Its analgesic effect appears due to LA diffusion into the paravertebral space, affecting both the dorsal and ventral rami of the thoracic spinal nerves and the rami communicantes that supply the sympathetic chain.
There are a few randomized control trials done in adults evaluating the efficacy of the ESPB for post-sternotomy pain and finding it equivalent to the TEA[16] and superior to systemic analgesia.[17] Most of the published reports of this block, both as a continuous and single-shot technique for thoracic surgery in the pediatric age group are restricted to case reports/series. There are multiple reports of the successful use of single-shot ESPB with LA alone or with an adjuvant to prolong analgesia for thoracotomy in pediatric patients.[18,19,20]
Continuous ESPB technique was reported in a 7-month-old infant by Kaplan et al.[21] for providing perioperative analgesia in a thoracotomy surgery. They inserted a catheter in ESP at the T5 level with LA (0.2% ropivacaine) with an approximate 0.3 mL/kg bolus and 0.15 mL/kg/h infusion and maintained excellent analgesia. A similar report of the use of block by continuous technique for thoracotomy in a 7-year-old was published by Patel et al.[22] The dose of LA given by them was similar as we used in our study (0.5 mL/kg 0.5% Ropivacaine and 0.2 mg/kg/h). They also achieved adequate analgesia with no reported complications. In another report on continuous ESPB in a 3-year-old for thoracotomy, the block was performed at a T9 level requiring a higher volume of LA both as a bolus and continuous infusion.[23] We inserted the ESP catheter at the T5 level. This level provides adequate analgesia with less volume of LA infusion, and has been used in most reported cases of ESPB for adult and pediatric thoracotomy.
The thoracic epidural is nowadays considered safe in pediatric practice, but being close to vital structures can be associated with fatal complications.[24] Its use in infants and young children should be restricted to those experienced in the technique. The procedure should be abandoned if difficulties are encountered. We think the ESPB is a technically more straightforward fascial plane block which can be given unilaterally in thoracotomies. The other good thing about the block is that complications are less because the injection site is far from the pleura, major blood vessels, and spinal cord. The erector spinae plane is relatively avascular, so there is less risk of immediate intravascular absorption of LA. This block can be safely given even in patients with coagulation disorders/patients on anticoagulants being relatively superficial block.[22]
Our study had a few limitations; the sample size was small. The sensory assessment of the ESPB block was not possible as we performed it under GA. Since there is no previous similar study, the dose of LAs used through the ESPB catheters was based on our experience (single-center), and a few case reports. Another limitation was that all the ESP blocks were given under ultrasound, but in the TEA group, we did not use ultrasound or any other method for confirming the right placement of the epidural catheters.
Thus, we conclude that the continuous ESPB provides adequate opioid-sparing perioperative analgesia in pediatric thoracotomy. The analgesic efficacy of the ESPB is comparable to the TEA, an established technique. The execution of the ESPB is faster and simpler compared to the securement of a thoracic epidural catheter. The ESPB also has a lesser incidence of complications. More studies are further warranted to establish the ESPB for thoracotomy and also for establishing a required dose of LAs to achieve optimal analgesia.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.McGovern I, Walkar C, Cox F. Pain relief after thoracotomy. Br J Anaesth. 2007;98:844–5. doi: 10.1093/bja/aem112. author reply 844. [DOI] [PubMed] [Google Scholar]
- 2.Ochroch EA, Gottschalk A. Impact of acute pain and its management for thoracic surgical patients. Thorac Surg clin. 2005;15:105–21. doi: 10.1016/j.thorsurg.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 3.Dabir S, Parsa T, Radpay B, Padyab M. Interpleural morphine vs bupivacaine for post thoracotomy pain relief. Asian Cardiovasc Thorac Ann. 2008;16:370–4. doi: 10.1177/021849230801600506. [DOI] [PubMed] [Google Scholar]
- 4.El-Morsy GZ, El-Deeb A, El-Desouky T, Elsharkawy AA, Elgamal MA. Can thoracic paravertebral block replace thoracic epidural block in pediatric cardiac surgery? A randomized blinded study. Ann Card Anaesth. 2012;15:259–63. doi: 10.4103/0971-9784.101848. [DOI] [PubMed] [Google Scholar]
- 5.Kotzé A, Hinton W, Crabbe DC, Carrigan BJ. Audit of epidural analgesia in children undergoing thoracotomy for decortication of empyema. Br J Anaesth. 2007;98:662–6. doi: 10.1093/bja/aem065. [DOI] [PubMed] [Google Scholar]
- 6.Fang B, Wang Z, Huang X. Ultrasound-guided preoperative single-dose erector spinae plane block provides comparable analgesia to thoracic paravertebral block following thoracotomy: A single center randomized controlled double-blind study. Ann Transl Med. 2019;7:174. doi: 10.21037/atm.2019.03.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forero M, Rajarathinam M, Adhikary S, Chin KJ. Continuous erector spinae plane block for rescue analgesia in thoracotomy after epidural failure: A case report. A Case Rep. 2017;8:254–6. doi: 10.1213/XAA.0000000000000478. [DOI] [PubMed] [Google Scholar]
- 8.Forero M, Rajarathinam M, Adhikary S, Chin KJ. Erector spinae plane (ESP) block in the management of post thoracotomy pain syndrome: A case series. Scand J Pain. 2017;17:325–9. doi: 10.1016/j.sjpain.2017.08.013. [DOI] [PubMed] [Google Scholar]
- 9.Muñoz F, Cubillos J, Bonilla AJ, Chin KJ. Erector spinae plane block for postoperative analgesia in pediatric oncological thoracic surgery. Can J Anesth. 2017;64:880–2. doi: 10.1007/s12630-017-0894-0. [DOI] [PubMed] [Google Scholar]
- 10.De La Cuadra-Fontaine JC, Concha M, Vuletin F, Arancibia H. Continuous erector spinae plane block for thoracic surgery in a pediatric patient. Paediatr Anaesth. 2017;28:74–5. doi: 10.1111/pan.13277. [DOI] [PubMed] [Google Scholar]
- 11.Juliuous SA, Patterson SD. Sample sizes for estimation in clinical research. Phamaceut Stat. 2004;3:213–5. [Google Scholar]
- 12.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: Anovelanalgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–7. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 13.Schwartzmann A, Peng P, Maciel MA, Forero M. Mechanism of the erector spinaeplaneblock: Insights from a magnetic resonance imaging study. Can J Anaesth. 2018;65:1165–6. doi: 10.1007/s12630-018-1187-y. [DOI] [PubMed] [Google Scholar]
- 14.Adhikary SD, Bernard S, Lopez H, Chin KJ. Erector spinae plane block versusretrolaminarblock: A magnetic resonance imaging and anatomical study. Reg Anesth Pain Med. 2018;43:756–62. doi: 10.1097/AAP.0000000000000798. [DOI] [PubMed] [Google Scholar]
- 15.Ivanusic J, Konishi Y, Barrington MJ. A cadaveric study investigating the mechanismofaction of erector spinae blockade. Reg Anesth Pain Med. 2018;43:567–71. doi: 10.1097/AAP.0000000000000789. [DOI] [PubMed] [Google Scholar]
- 16.Krishna SN, Chauhan S, Bhoi D, Kaushal B, Hasija S, Sangdup T, et al. Bilateral erector spinae plane block for acute post-surgical pain in adult cardiac surgical patients: A randomized controlled trial. J Cardiothorac Vasc Anesth. 2019;33:368–75. doi: 10.1053/j.jvca.2018.05.050. [DOI] [PubMed] [Google Scholar]
- 17.Nagaraja PS, Ragavendran S, Singh NG, Asai O, Bhavya G, Manjunath N, et al. Comparison of continuous thoracic epidural analgesia with bilateral erector spinae plane block for perioperative pain management in cardiac surgery. Ann Card Anaesth. 2018;21:323–7. doi: 10.4103/aca.ACA_16_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hernandez MA, Palazzi L, Lapalma J, Forero M, Chin KJ. Erector spinae plane block for surgery of the posterior thoracic wall in a pediatric patient. Reg Anesth Pain Med. 2018;43:217–9. doi: 10.1097/AAP.0000000000000716. [DOI] [PubMed] [Google Scholar]
- 19.Nardiello MA, Herlitz M. Bilateral single shot erector spinae plane block for pectus excavatum and pectus carinatum surgery in 2 pediatric patients. Rev Esp Anestesiol Reanim (Engl Ed) 2018;65:530–3. doi: 10.1016/j.redar.2018.04.006. [DOI] [PubMed] [Google Scholar]
- 20.Wyatt K, Elattary T. The erector spinae plane block in a high-risk Ehlers-Danlos syndrome pediatric patient for vascular ring repair. J Clin Anesth. 2019;54:39–40. doi: 10.1016/j.jclinane.2018.10.031. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan I, Jiao Y, AuBuchon JD, Moore RP. Continuous erector spinae plane catheter for analgesia after infant thoracotomy: A case report. A Pract. 2018;11:250–2. doi: 10.1213/XAA.0000000000000799. [DOI] [PubMed] [Google Scholar]
- 22.Patel NV, Glover C, Adler AC. Erector spinae plane catheter for postoperative analgesia after thoracotomy in a pediatric patient: A case report. A Pract. 2019;12:299–301. doi: 10.1213/XAA.0000000000000914. [DOI] [PubMed] [Google Scholar]
- 23.Gaio-Lima C, Costa CC, Moreira JB, Lemos TS, Trindade HL. Continuous erector spinae plane block for analgesia in pediatric thoracic surgery: A case report. Rev Esp Anestesiol Reanim. 2018;65:287–90. doi: 10.1016/j.redar.2017.11.010. [DOI] [PubMed] [Google Scholar]
- 24.Wong GK, Arab AA, Chew SC, Naser B, Crawford MW. Major complications related to epidural analgesia in children: A 15-year audit of 3,152 epidurals. Can J Anesth. 2013;60:355–63. doi: 10.1007/s12630-012-9877-3. [DOI] [PubMed] [Google Scholar]