Abstract
Objective:
This study was undertaken to assess the change in social contact and transmission dynamics among adults in the Puducherry district during the different phases of country-wide lockdown.
Methods:
Adults aged 18–69 years in Puducherry were assessed for frequency and duration of contacts in the following time points: prior to lockdown (March 2020), during lockdown, immediate post-lockdown (April, June 2020), and seven months post-lockdown (February 2021). Adjusted incidence rate ratios (aIRR) were obtained using a generalized estimating equation. We also assessed the exponential trajectory of the time-varying reproduction number (Rt) during and after lockdown.
Results:
Compared to pre-lockdown phase, frequency of social contacts during 1st week, 4th week of lockdown, and immediate post-lockdown were reduced by 89% (aIRR = 0.11; 95% CI: 0.09–0.13), 40% (aIRR = 0.60; 95% CI: 0.52–0.69) and 91% (aIRR = 0.09; 95% CI: 0.07–0.10) respectively. However, the decline was not statistically significant at seven months post-lockdown. Correspondingly, we observed an initial spike in Rt during the lockdown phase followed by a gradual decline during the immediate post-lockdown phase. However, seven months post-lockdown, Rt has increased again.
Conclusion:
The study showed high compliance to the lockdown measures in Puducherry during the lockdown and immediate post-lockdown periods. However, as the lockdown measures were relaxed, the contact rate returned to the pre-lockdown state.
KEY WORDS: COVID-19, infectious disease modeling, lockdown, social contact
Introduction
Respiratory infections spread mainly through close person-to-person contact. In the current pandemic of Coronavirus disease (COVID-19), the transmission of Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2) is predominantly through respiratory droplets between the close contacts.[1] As of 31 May 2021, about 170 million cases of COVID-19 and 3.5 million deaths have been reported worldwide.[2] India has recorded the second-highest burden of COVID-19, with 27.8 million cases and 0.32 million deaths occurring as two waves, one in 2020 and the other in early 2021.[3] During the waves, preventing and containing the spread of the virus has been the top public health priority for the national and state governments leading to several urgent and aggressive steps to mitigate the effect of the pandemic.[4]
Since there were no proven pharmacological interventions such as drugs or vaccines to deal with this pandemic during the first wave of COVID-19, non-pharmacological measures such as the closure of public places (workplaces, schools, colleges, etc.), and imposition of lockdown at regional or national level (regarded as the ‘social vaccine’) were resorted to.[5] Early in the pandemic, a country-wide lockdown was implemented beginning from 25 March 2020; though initially meant to last for 21 days, it was later extended with a total duration of 68 days.[6] The prime purpose of this unprecedented public health measure was to enforce a marked cessation of social contacts in the community, to break the chain of transmission.
Infectious disease modeling conducted at times of disease outbreaks help governments to prepare their health systems and mitigate the impact by predicting the morbidity and mortality over time. These predictions are based on the epidemiological concept ‘Basic Reproduction Rate (R0)’ that relies mainly on transmission coefficient, contact rates, and duration of infectiousness.[7] Predicting the spread of COVID-19 and the impact of lockdown also depend on the quantification of close contacts among the general population. Assessing the change in rate and duration of social contact will help the public health authorities to assess the effectiveness of lockdown and thereby devise/refine intervention strategies for further planning.
Self-reporting of contacts by individuals using a contact diary is a commonly used method for quantifying contact rate.[8,9] Such surveys capture the total number and duration of contacts from each individual for a given period of time. Studies from European countries have proved that the self-reported contact rate is a reliable proxy for modeling airborne/droplet-borne disease transmissions.[10] With limited availability of information on social contact rate and duration from Indian settings, especially during this COVID-19 pandemic, we undertook this study to assess the change in rate, duration of social contact, and its influence on the transmission dynamics among the adults in Puducherry during different phases of nationwide lockdown (pre-lockdown, during lockdown, and post-lockdown periods).
Methods
Study design and setting
We conducted this longitudinal study amongst adults aged 18 to 69 years in the district of Puducherry during different phases of lockdown: prior to lockdown (March 2020), during lockdown, immediate post-lockdown (April 2020 and June 2020), and seven months following the country-wide lockdown (February 2021).
Puducherry is one of the four districts of Puducherry Union Territory (UT) located along the eastern coast of Southern India. The district has a population of 950,000, with nearly 69% residing in urban areas and the rest in rural areas.[11] Population density is about 3,232 per square km[11]; adults constitute 67.8% of the population, of whom 9.6% are elderly (≥ 60 years).[12] The district has a literacy rate of 85.4%[13] and an average life expectancy of 68.3 years.[14]
Selection of participants
The sampling frame was drawn from a district-wide community-based survey on non-communicable diseases (NCDs) risk factors conducted in 2018–20.[15] The survey employed a multi-stage, stratified, cluster sampling technique using the data from Census 2011 as the baseline. In the urban area, three-stage sampling was performed, while in the rural area, two-stage sampling was performed.
Stage 1: During the first stage of sampling, 50 out of 90 wards were selected in the urban area, and 50 out of 62 revenue villages were selected in the rural area.
Stage 2: During the second stage, one census enumeration block (CEB) was selected randomly from each chosen ward in the urban area.
Stage 3: During the final stage of sampling, 36 households were selected from each of the chosen CEBs, while 16 households were selected from each of the chosen villages through a systematic random sampling technique.
In each household, one adult aged 18–69 years and residing in that particular household for the past six months at least was selected using the KISH technique. Household members with a cognitive or physical impairment to an extent at which they cannot understand and respond back to the questions were excluded. In total, 2,415 (734 in rural, 1681 in urban areas) adults were selected as per the primary objective of the large-scale survey. Amongst these participants, 550 (385 in urban and 165 in rural areas) were invited to participate in this study. They were selected by using computer-generated random numbers after an assigning identification number for each invitee in the Microsoft (MS) Excel software.
Study tool and data collection
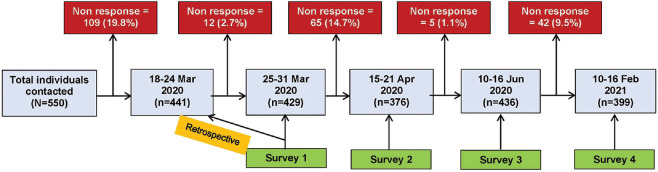
Data were collected through telephonic interviews utilizing the phone numbers from the NCD survey database. If there was no response from a household during the initial telephonic contact, repeated calls up to three times, two-three days apart, at different times were made. In case of no response at all times, they were excluded from the study. Information was collected for five data points, i.e., one week prior to the country-wide lockdown (15 to 21 March 2020), during the first week (25 to 31 March 2020), fourth week (April 2020), a week after the country-wide lockdown was withdrawn (June 2020) and seven months (February 2021) post-lockdown. Data on social contacts prior to country-wide lockdown was collected retrospectively along with the data for the first week of lockdown. Subsequent data points were collected from subsequent surveys.
Initially, informed verbal consent was obtained, following which a pre-tested semi-structured questionnaire was administered to collect the data from the selected study participants. The questionnaire consisted of two sections: the first section consisted of socio-demographic information such as age, gender, education, occupation, residence, household size, and marital status; the second section consisted of information related to the number and duration of social contacts at different social settings.
While assessing the contact pattern for a day, each participant was asked to recall information on the frequency and duration of social contacts, from the time they woke up until they went to bed (~24 hours) on the day prior to the data collection. To facilitate the recollection of information, they were first asked to list all the places visited on a particular day, followed by information on the frequency and average duration of contacts at each visited place.
Operational definitions
Social contact frequency: ‘Social contact’ is defined as a two-way conversational encounter between the participant and another person lasting for ≥5 minutes or with whom the participant had the conversation in proximity (less than one meter).[16] The number of social contacts the participant encounters per day was assessed across varied social settings such as schools, colleges, workplaces, shops or establishments, friends/relative households, etc., Contact data on multiple encounters with the same contact is considered as single social contact (as the objective is to find the difference in the number of persons coming in contact with the participant before, during, and after the lockdown). Household contacts were excluded from the analysis (as we wanted to study the impact of lockdown, which will most likely have an impact on the community contacts).
Social contact duration: Average time spent (in minutes) per day by the participant in close contact at each social setting.
Compliance to lockdown: Reduction in social contact rate of an individual by ≥75%, 25–74%, or <25% during and post lockdown periods compared to the pre-lock down period, in comparison to the pre-lockdown state were classified as high, moderate or low level of compliance respectively.
Statistical analysis
Data was entered into EpiCollect5, and analysis was performed using STATA version 14.2 software (StataCorp, CollegeStation, TX, USA). Continuous variables were summarized as mean and standard deviation (SD) or median and interquartile range (IQR) depending on the distribution of data. Categorical variables were summarized as proportions. We used the generalized estimating equation (to account for the within-subject correlation of responses on the outcome variables in a longitudinal dataset) applying negative binomial regression model (to account for overdispersion of data) to analyze the group-by-time differences in social contact rate and duration of contacts. Sociod-emographic factors such as residence, gender, age group, household size, and social settings between pre-lockdown, during the lockdown, and post-lockdown periods were considered as explanatory variables to adjust for the potential confounding. Factors significant at a P value less than 0.20 in the unadjusted analysis were considered for the multivariable model. The stepwise forward method was employed, and the significant model which had the highest adjusted R-square value was considered as the final model. Adjusted incident rate ratio (aIRR) with 95% confidence interval (CI) was reported and a P value less than 0.05 was considered statistically significant. Estimates on adherence to lockdown compliance were presented as proportion with 95% CI.
We also assessed the exponential trajectory of the time-varying reproduction number (Rt) during and after lockdown (we did not assess the trajectory before the lockdown as there were no COVID-19 cases in Puducherry during this period). Time-varying reproduction number (Rt) is referred to as the number of secondary cases expected from a typical index case in a given time point, considering that all the individuals in the community are susceptible to infection. If Rt value is more than the threshold value 1, it means that an infected individual can infect more than one individual, and the infection can more likely become an epidemic because of a sustained chain of transmission. To calculate the Rt for Puducherry, first, we obtained data on the incident number of COVID-19 cases per day starting during the lockdown period (April 2020 to June 2020), initial post-lockdown phase (July 2020 to January 2021), and late post-lockdown phase (February 2021 to April 2021). We obtained the generation time (GT) of COVID-19 for the calculation of R0. The mean and SD of GT were set at 4.8 and 2.3 days as per the available literature.[17]
The time-dependent method proposed by Wallinga and Teunis was used to compute the Rt by averaging over all the transmission networks compatible with the observations. The probability “pij” that the case “i” with onset at time “ti” was infected by case “j” with onset at time “tj” is calculated as:

The time-varying reproduction number for case “j” is, therefore, ∑ipij and the confidence interval can be obtained by simulation. All the analysis was performed in R software 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria) using the “R0” package.
Ethical statement: The study was approved by the Institutional Human Ethics Committee of JIPMER with ethical approval number JIP/IEC/2020/059.
Results
In total, 441 of 550 (80.2%) individuals participated in the survey. Figure 1 depicts the flow of participants and non-response rate throughout the study period. Table 1 shows the distribution of study participants across all the timepoints and its comparison to the demographics of the entire Puducherry district (as per census 2011 data). We did not find any significant difference in terms of any of the socio-demographic characteristics across any of the timepoints. With respect to demographics of the Puducherry district, male-female and urban-rural distribution were similar with respect to our study group, while there was a slight variation in terms of age group, education, and marital status.
Figure 1.
Flow of study participants during the study period
Table 1.
Socio-demographic characteristics of study participants (N=441)
| Category | Pre-lockdown (18-24 Mar 2020) (n=441) | 1st week of lockdown (25-31 Mar 2020) (n=429) | 4th week of lockdown (15-21 Apr 2020) (n=376) | 1st week post-lockdown (10-16 Jun 2020) (n=436) | Seven months post-lockdown (10-16 Feb 2020) (n=399) | Puducherry Demographics in percentages* |
|---|---|---|---|---|---|---|
| Age group (years) | ||||||
| 18-30 | 117 (26.5) | 109 (25.4) | 108 (28.7) | 115 (26.4) | 103 (25.8) | 21.9 |
| 31-45 | 154 (34.9) | 152 (35.4) | 134 (35.6) | 153 (35.1) | 142 (35.6) | 24.7 |
| 46-59 | 107 (24.3) | 105 (24.5) | 88 (23.4) | 106 (24.3) | 100 (25.1) | 15.2 |
| ≥ 60 | 63 (14.3) | 63 (14.7) | 46 (12.2) | 62 (14.2) | 54 (13.5) | 10.1 |
| Gender | ||||||
| Males | 224 (50.8) | 221 (51.5) | 198 (52.7) | 224 (51.4) | 203 (50.9) | 49.1 |
| Females | 217 (49.2) | 208 (48.5) | 178 (47.3) | 212 (48.6) | 196 (49.1) | 50.9 |
| Residence | ||||||
| Rural | 133 (30.2) | 128 (29.8) | 118 (31.4) | 130 (29.8) | 125 (31.3) | 30.9 |
| Urban | 308 (69.8) | 301 (70.2) | 258 (68.6) | 306 (70.2) | 274 (68.7) | 69.1 |
| Household size | ||||||
| 1-2 | 136 (30.8) | 132 (30.8) | 112 (29.8) | 134 (30.7) | 124 (31.1) | NA |
| 3-4 | 245 (55.6) | 239 (55.7) | 216 (57.4) | 243 (55.8) | 219 (54.9) | NA |
| > 4 | 60 (13.6) | 58 (13.5) | 48 (12.8) | 59 (13.5) | 56 (14.0) | NA |
| Education | ||||||
| No formal education | 30 (6.8) | 30 (7.0) | 22 (5.8) | 29 (6.6) | 27 (6.8) | 14.1 |
| Primary education | 164 (37.2) | 162 (37.8) | 135 (35.9) | 162 (37.2) | 150 (37.6) | NA |
| Secondary/Higher Secondary | 145 (32.9) | 137 (31.9) | 123 (32.7) | 144 (33.0) | 132 (33.1) | NA |
| Graduation and above | 102 (23.1) | 100 (23.3) | 96 (25.6) | 101 (23.2) | 90 (22.6) | NA |
| Occupation | ||||||
| Employed | 259 (58.7) | 255 (59.4) | 228 (60.6) | 257 (58.9) | 238 (59.6) | 48.4 |
| Homemaker | 134 (30.4) | 126 (29.4) | 106 (28.2) | 131 (30.1) | 120 (30.1) | 42.3 |
| Retired/Unemployed | 48 (10.9) | 48 (11.2) | 42 (11.2) | 48 (11.0) | 41 (10.3) | 9.3 |
| Marital status | ||||||
| Never married | 68 (15.4) | 65 (15.1) | 67 (17.8) | 67 (15.4) | 61 (15.3) | 42.3 |
| Currently married | 349 (79.1) | 341 (79.5) | 290 (77.1) | 347 (79.6) | 316 (79.2) | 50.3 |
| Widowed/Divorced/Separated | 24 (5.5) | 23 (5.4) | 19 (5.1) | 22 (5.1) | 22 (5.5) | 7.4 |
NA-Not available; *Census 2011 data
Table 2 shows the change in the frequency and duration of social contact over time (from pre-lockdown to seven months post-lockdown period) after adjusting for the potential confounders. The median (IQR) number of contacts per person per day before the lockdown was 10 (5–15). However, the median number of contacts during the lockdown period reduced to 0 (0–2), and they subsequently increased to 8 (5–13) contacts per person per day at seven months post-lockdown period. Adjusted analysis showed that the incident number of social contacts during 1st week, 4th week and immediate post lockdown weeks reduced by almost 90% (aIRR = 0.11; 95% CI: 0.09–0.13), 40% (aIRR = 0.60; 95% CI: 0.52–0.69) and 91% (aIRR = 0.09; 95% CI: 0.07–0.10) respectively when compared to pre-lockdown period. These reductions were statistically significant. However, there was no significant difference in social contact rate at seven months post-lockdown period (aIRR = 0.96; 95% CI: 0.83–1.09).
Table 2.
Difference in frequency and duration of social contacts across various phases of lockdown
| Time point | Number of contacts |
Duration of contacts (in minutes) |
||||
|---|---|---|---|---|---|---|
| Median (IQR) | Adjusted IRR* (95%CI) | P | Median (IQR) | Adjusted IRR* (95% CI) | P | |
| Pre-lockdown | 10 (5-15) | Ref | Ref | 442 (243-586) | Ref | Ref |
| 1st week of lockdown | 0 (0-2) | 0.11 (0.09-0.13) | < 0.001 | 285 (180-345) | 0.64 (0.56-0.73) | < 0.001 |
| 4th week of lockdown | 3 (1-9) | 0.60 (0.52-0.69) | < 0.001 | 360 (180-540) | 0.89 (0.78-1.02) | 0.09 |
| 1st week post-lockdown | 0 (0-2) | 0.09 (0.07-0.10) | < 0.001 | 240 (180-300) | 0.61 (0.54-0.70) | < 0.001 |
| Seven months post-lockdown | 8 (5-13) | 0.96 (0.83-1.09) | 0.51 | 480 (180-600) | 0.96 (0.84-1.10) | 0.58 |
*Adjusted Incidence rate ratio derived from GEE model after adjusting for all the potential confounders; Ref - Reference category; CI - Confidence Interval; IQR - Interquartile range
At various social settings, the median (IQR) duration of social contacts prior to lockdown, during the lockdown, post-lockdown phases per participant per day were 442 (243–586), 285 (180–345), 360 (180–540), 240 (180-300), and 480 (180–600) minutes respectively. In adjusted analysis also, a similar trend was found as all the phases except seven months post-lockdown had a statistically significant reduction in the duration of social contacts when compared to the pre-lockdown period.
The level of compliance to lockdown in terms of relative reduction in social contact rate during and post lockdown periods in comparison to the pre-lockdown phase is given in [Figure 2]. Over four out of five people (82.4%) in the district of Puducherry were adherent to a high level of compliance to lockdown during the first week of lockdown. However, by the fourth week of nationwide lockdown, the population at high levels of compliance declined to less than half (45.2%), leading to a spike in the incident number of cases in Puducherry. Then, again the level of compliance has increased to more than 80% even after the withdrawal of nationwide lockdown (1st week post-lockdown). However, seven months post-lockdown, the compliance to the high level of reduction in social contact rate declined to about 11.9%.
Figure 2.
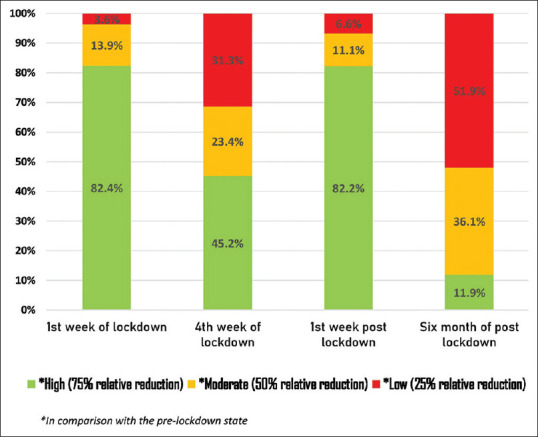
Effect of lockdown on the social contact rates on different time points of the lockdown period in comparison to the pre-lockdown phase in Puducherry, India
Table 3 shows the factors associated with social contact rate at pre-lockdown, during the lockdown, and post-lockdown periods. Males had significantly higher incident number of contacts when compared to females (aIRR = 1.48; 95% CI: 1.26–1.74). Participants who had primary education (aIRR = 0.76; 95% CI: 0.59–0.98) and secondary/higher secondary level of education (aIRR = 0.76; 95% CI: 0.59–0.99) had fewer incident number of contacts compared to those with no formal education. Table 4 shows the factors associated with the duration of social contacts at pre-lockdown, during the lockdown, and post-lockdown period. Participants aged 18–30 years had a significantly higher duration of social contacts (aIRR = 1.25; 95% CI: 1.01–1.54) when compared to those elderly participants. Men had a significantly higher duration of social contacts (aIRR = 1.32; 95% CI: 1.16–1.50) when compared to women.
Table 3.
Factors associated with the social contact rate prior to, during and post-lockdown periods in Puducherry, India
| Category | Total n (%) | Median number of Social Contacts (IQR) |
Adjusted IRR (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| Pre-lockdown (18-24 Mar 2020) (n=441) | 1st week of lockdown (25-31 Mar 2020) (n=429) | 4th week of lockdown (15-21 Apr 2020) (n=376) | 1st week post-lockdown (10-16 Jun 2020) (n=436) | Seven months post-lockdown (10-16 Feb 2020) (n=399) | |||
| Total sample | 441 (100) | 10 (5-15) | 0 (0-2) | 3 (1-9) | 0 (0-2) | 8 (5-13) | - |
| Gender | |||||||
| Male | 224 (50.8) | 13 (8-21) | 0 (0-2) | 4 (1-13) | 0 (0-2) | 8 (6-12)* | 1.48 (1.26-1.74)* |
| Female | 217 (49.2) | 6 (3-11) | 0 (0-2) | 2 (1-6) | 0 (0-2) | 7 (5-14) | Ref |
| Age group (years) | |||||||
| 18-30 | 117 (26.5) | 10 (5-15) | 0 (0-2) | 4 (1-12) | 0 (0-2) | 10 (5-16) | 1.23 (0.94-1.60) |
| 31-45 | 154 (34.9) | 9 (5-16) | 0 (0-2) | 3 (1-12) | 0 (0-2) | 7 (5-13) | 1.24 (0.99-1.54) |
| 46-59 | 107 (24.3) | 9 (5-13) | 0 (0-2) | 2 (0-6) | 0 (0–2) | 7 (5–11) | 1.10 (0.89-1.36) |
| ≥ 60 | 63 (14.3) | 10 (5-16) | 0 (0-1) | 3 (1-6) | 0 (0-2) | 10 (5-11) | Ref |
| Residence | |||||||
| Rural | 133 (30.2) | 10 (5-17) | 0 (0-3) | 3 (0-7) | 0 (0-2) | 6 (4-8) | Ref |
| Urban |
308 (69.8) |
11 (5-15) | 0 (0-2) | 3 (1-12) | 0 (0-2) | 9 (6-15) | 1.02 (0.90-1.17) |
| Household size | |||||||
| 1-2 | 136 (30.8) | 8 (4-15) | 0 (0–2) | 3 (1–8) | 0 (0–2) | 7 (5–12) | Ref |
| 3-4 | 245 (55.6) | 10 (5-16) | 0 (0–2) | 3 (1–11) | 0 (0–2) | 8 (5–13) | 1.10 (0.96-1.25) |
| > 4 | 60 (13.6) | 10 (5-15) | 0 (0–2) | 3 (1–8) | 0 (0–2) | 7 (6–14) | 1.10 (0.91-1.34) |
| Education | |||||||
| No formal education | 30 (6.8) | 10 (4-17) | 0 (0-2) | 2 (0-9) | 0 (0-1) | 6 (5-15) | Ref |
| Primary education | 164 (37.2) | 9 (5-15) | 0 (0-2) | 3 (1-7) | 0 (0-2) | 7 (5-12) | 0.76 (0.59-0.98)* |
| Secondary/Higher Secondary | 145 (32.9) | 10 (5-15) | 0 (0-1) | 3 (1-8) | 0 (0-2) | 8 (5-12) | 0.76 (0.59-0.99)* |
| Graduation and above | 102 (23.1) | 10 (5-16) | 0 (0-2) | 4 (4-17) | 0 (0-2) | 8 (5-15) | 0.96 (0.72-1.28) |
| Occupation | |||||||
| Employed | 259 (58.7) | 12 (7-17) | 0 (0-2) | 3 (1-12) | 0 (0-2) | 8 (6-13) | 0.99 (0.83-1.17) |
| Homemaker | 134 (30.4) | 5 (2-10) | 0 (0-2) | 2 (1-7) | 0 (0-2) | 6 (4-14) | Ref |
| Retired/Unemployed | 48 (10.9) | 12 (8-21) | 0 (0-1) | 4 (2-8) | 0 (0-2) | 6 (3-11) | 0.93 (0.73-1.19) |
| Marital status | |||||||
| Never married | 68 (15.4) | 11 (8-17) | 0 (0-2) | 4 (1-11) | 0 (0-2) | 12 (7-17) | 0.92 (0.65-1.36) |
| Currently married | 349 (79.1) | 10 (5-16) | 0 (0-2) | 3 (1-10) | 0 (0-2) | 7 (5-12) | 0.95 (0.71-1.26) |
| Widowed/Divorced | 24 (5.5) | 8 (4-12) | 0 (0-2) | 2 (0-6) | 0 (0-1) | 6 (4-11) | Ref |
| Day of week | |||||||
| Weekday | 375 (85.0) | 10 (5-15) | 0 (0-2) | 3 (1-10) | 0 (0-2) | 8 (5-14) | {Not included in the model} |
| Weekend | 66 (15.0) | 9 (6-16) | 0 (0-2) | 3 (0-7) | 0 (0-1) | 6 (4-8) | |
*P-value less than 0.05 – statistically significant; IRR-Incidence rate ratio; Ref-Reference category; IQR-Interquartile range
Table 4.
Factors associated with the duration of social contacts prior to, during lockdown, and post-lockdown periods in Puducherry, India (N=441)
| Category | Total n (%) | Median duration of Social Contacts (IQR) (in minutes) |
Adjusted IRR (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| Pre-lockdown (18-24 Mar 2020) (n=441) | 1st week of lockdown (25-31 Mar 2020) (n=429) | 4th week of lockdown (15-21 Apr 2020) (n=376) | 1st week post-lockdown (10-16 Jun 2020) (n=436) | Seven months post-lockdown (10-16 Feb 2020) (n=399) | |||
| Total sample | 441 (100) | 442 (243-586) | 285 (180-345) | 360 (180-540) | 240 (180-300) | 480 (180-600) | - |
| Gender | |||||||
| Male | 224 (50.8) | 570 (461-633) | 335 (240-360) | 445 (240-660) | 270 (225-330) | 540 (330-600) | 1.32* (1.16-1.50) |
| Female | 217 (49.2) | 272 (190-420) | 225 (160-300) | 300 (150-420) | 240 (180-300) | 305 (120-550) | Ref |
| Age group (years) | |||||||
| 18-30 | 117 (26.5) | 483 (249-630) | 285 (180-360) | 480 (240-660) | 245 (180-315) | 540 (348-600) | 1.25* (1.01-1.54) |
| 31-45 | 154 (34.9) | 422 (236-600) | 270 (180-340) | 360 (180-600) | 240 (180-300) | 480 (180-570) | 1.13 (0.95-1.35) |
| 46-59 | 107 (24.3) | 480 (250–565) | 300 (183-342) | 360 (180-480) | 252 (180-303) | 480 (180–600) | 1.10 (0.93-1.31) |
| ≥ 60 | 63 (14.3) | 411 (272–576) | 270 (180-345) | 240 (120-300) | 255 (202-325) | 225 (120-540) | Ref |
| Residence | |||||||
| Rural | 133 (30.2) | 444 (300–571) | 255 (180-360) | 330 (157-607) | 240 (180-300) | 360 (120-540) | {Not included in the model} |
| Urban | 308 (69.8) | 436 (221–600) | 292 (180-345) | 360 (180–540) | 250 (192-330) | 540 (240-600) | |
| Household size | |||||||
| 1-2 | 136 (30.8) | 422 (254–582) | 300 (180-345) | 300 (150-600) | 240 (190-315) | 480 (180-570) | {Not included in the model} |
| 3-4 | 245 (55.6) | 461 (251–575) | 270 (180-345) | 360 (180-540) | 240 (180-312) | 438 (180-600) | |
| > 4 | 60 (13.6) | 425 (210–604) | 285 (165-345) | 382 (172-540) | 240 (180-300) | 540 (378-600) | |
| Education | |||||||
| No formal education | 30 (6.8) | 375 (218–570) | 240 (180-348) | 345 (232-435) | 255 (187-315) | 429 (120-600) | Ref |
| Primary education | 164 (37.2) | 439 (254–571) | 255 (180–342) | 300 (150–540) | 240 (180-300) | 420 (157-570) | 0.98 (0.79-1.20) |
| Secondary/Higher Secondary | 145 (32.9) | 480 (258–618) | 300 (180–352) | 360 (180–540) | 250 (180-313) | 540 (250-570) | 0.99 (0.80-1.20) |
| Graduation and above | 102 (23.1) | 488 (220-600) | 300 (180-345) | 420 (240–600) | 250 (195-320) | 480 (240-600) | 0.95 (0.75-1.20) |
| Occupation | |||||||
| Employed | 259 (58.7) | 543 (330-630) | 300 (195-360) | 420 (180-600) | 255 (195-317) | 540 (300-600) | 1.10 (0.96-1.27) |
| Homemaker | 134 (30.4) | 241 (181-366) | 180 (134-300) | 300 (165-420) | 240 (180-300) | 305 (120-540) | Ref |
| Retired/Unemployed | 48 (10.9) | 542 (301-629) | 300 (225-348) | 300 (127-675) | 240 (180-315) | 330 (120-540) | 1.03 (0.85-1.27) |
| Marital status | |||||||
| Never married | 68 (15.4) | 569 (338-647) | 315 (204-370) | 480 (240-660) | 250 (210-315) | 540 (480-611) | 0.93 (0.69-1.25) |
| Currently married | 349 (79.1) | 423 (241-573) | 270 (180–343) | 330 (180–540) | 240 (180–300) | 460 (180-570) | 0.94 (0.74-1.18) |
| Widowed/Divorced | 24 (5.5) | 333 (221-420) | 255 (180-345) | 180 (97-315) | 240 (180-337) | 215 (120-555) | Ref |
| Day of week | |||||||
| Weekday | 375 (85.0) | 484 (250-600) | 285 (180-345) | 360 (180-540) | 240 (180-300) | 510 (240-600) | {Not included in the model} |
| Weekend | 66 (15.0) | 304 (240-451) | 240 (180-345) | 270 (135-585) | 240 (196-319) | 258 (120-540) | |
*P-value less than 0.05 - statistically significant; IRR-Incidence rate ratio; Ref-Reference category; IQR-Interquartile range
The change in time-varying reproduction number (Rt) and total burden of COVID-19 during the study period is presented in [Figure 3]. There was an initial spike in the Rt during the lockdown phase followed by a gradual decline with Rt consistently less than one during the immediate post-lockdown phase. However, seven months after lockdown, Rt increased again and is consistently present over the threshold value of 1.
Figure 3.

Time-varying reproduction number (Rt) and the total number of reported cases of COVID-19 in Puducherry, India (April 2020 – April 2021)
Discussion
The current study showed that there was a significant reduction in both social contact rate and duration of contacts during and immediate post-lockdown phases in comparison to the pre-lockdown phase. In our study, the median number of social contacts prior to lockdown was 10, with an IQR of 5 to 15. This number was higher than the previous studies conducted in Hong Kong,[18] Vietnam,[19] and Germany.[20] However, a study in North India on social mixing patterns found that the median number of contacts was 17 (IQR 12-25).[21] The observed differences across various studies could be attributed to the various key factors such as the definition adopted for the ‘social contacts,’ as studies have regarded the casual contacts, any social interaction as social contact, and the inherent variations in the nature of social interactions across the geographical regions.[22] Substantiating the observed difference, studies have shown that the social contacts rate varies across geographic regions due to various factors such as population density, household size, weather/time of the year, and local activities carried out in the region.[10,23,24] But, while studying the dynamics of disease transmission, evidence suggests that counting the close contacts is more critical than the casual contacts or interactions.[10]
An assumption behind lockdown measures is that the reduction in contact rates will reduce the rate of infection, and this is confirmed by most of the model simulations.[25] This can be corroborated by looking at the doubling time of this pandemic in India in comparison to the United States of America (USA). In India, it took a doubling time of eight days to reach 32,000 cases, whereas it was only two days to reach the same range in the USA. This difference may be attributed to less rigorous lockdown implementation in the USA.[26]
Over 80% of the study participants adhered to limiting their social contacts during the first week of nationwide lockdown. Four weeks into the lockdown, there was a considerable increase in both social contact rate and duration, which was met with the rise in the number of cases and Rt, and the people again started adhering to the lockdown restrictions, which lasted even during the immediate post-lockdown phase (as revealed by the June 2020 survey in our study). Once the lockdown restrictions were removed/relaxed, there was a considerable increase in both social contact rate and its duration, as revealed by post lockdown surveys conducted in February 2021. The increase indicated a decline in the COVID-19 appropriate behavior in terms of social contacts and duration of contacts per person per day, implying the population approaching towards the pre-COVID contact behaviors. The change in reproduction number in our study also showed that though there was an initial spike (during the fourth week of lockdown as suggested by an increase in social contact rate and duration in our survey), there was a gradual decline with the Rt staying consistently less than 1 for a considerable period of time (even after the lockdown relaxations), indicating the impact of lockdown on social contact rate and duration, thereby reducing the transmission rate of COVID-19. However, seven months following the lockdown, the social contact rate was almost similar to the pre-lockdown phase, thereby increasing the Rt more than the threshold value of one. This indicates a lack of adherence to COVID appropriate behavior in the population with the ease of lockdown measures, heading towards the pre-COVID social contact behaviors.
Substantiating this phenomenon, India has faced the second wave COVID-19 with a surge in the number of cases since March 2021. Presently, we are in the third wave of COVID-19, with almost all states in the country having a reproduction number greater than one, implying a significant increase in the infection rate throughout the country. In this scenario, COVID-19 appropriate behaviors such as limiting the number and duration of social contacts, universal masking, hand hygiene, and maintaining physical distancing are crucial in preventing the COVID-19 spread. With COVID-19 vaccines in place, people need to be encouraged to take the vaccine at the earliest and also follow the above indicated COVID-19 preventive behaviors even after taking the shots in order to break the chain of infection.
Measures such as isolation can result in the reduction of contacts in the symptomatic population, while quarantine can reduce the contacts among asymptomatic unvaccinated high-risk COVID-19 contacts. Similarly, lockdown is based on the fact that the reduction of contacts in the general population can reduce the incidence of infection, thus buying time for strengthening the health system infrastructure.[27,28,29] However, limiting social contacts beyond lockdown by behavior change communication efforts, limiting movement by multiple strategies like enforcing time restrictions, and continued physical distancing are required to keep the number of infections down.[30] This is mainly because the lockdown has serious negative impacts in terms of human rights issues, freedom restrictions, economic issues, mental health issues, marginalized groups, and eclipses the care for all other diseases. Hence, measures alternative to lockdown for limiting the social contacts are important to limit the transmission and prevent the surge in the cases.[31,32,33]
We attempted to define compliance to lockdown in terms of reduction of social contacts, which may be useful to inform the effectiveness of non-pharmacological intervention (NPI) models for infection transmission in the region. Four out of five participants reduced their contact rates to at least 75%, while the majority had reduced their contacts by half during the lockdown period. Further, this significant reduction in the social contact rate was observed across all co-variates, including high-risk groups like the elderly, day of the week, and place of residence. This can be attributed to the fact that Puducherry having one of the highest proportions of literates in the country, observed Government protocols on lockdown to a great extent. The health literacy among the study participants might have played a prominent role in the adherence to the COVID-19 preventive behaviors during the lockdown.[34] The lockdown in the Puducherry district was relaxed during the third phase, which started on 4 May 2020. Shops, business establishments, industries, and government offices in the territory were allowed to function while abiding by the social distancing norms.[35] From the study, it is important to note that during the lockdown period, although the median contact rates reached zero, the contact duration remained high at 285 minutes, but now it is raised to 480 minutes. This raises concerns as contact duration is one of the key contributors to the transmission of infectious diseases.
Strengths and Limitations
This study had certain strengths. To our knowledge, this study is one of the first attempts in India to assess the effectiveness of country-wide lockdown in reducing the social contact rates among the general population. Importantly, at a time when countries are implementing regional or nationwide lockdown, the study findings would provide key information for predicting the spread and trajectories of COVID-19 over time.
However, there were certain limitations in our study, such as the telephonic nature of the survey, the inherent social desirability bias in responses towards adherence to lockdown and recall bias in remembering the number and duration of social contacts (as there was no pre-specified date arranged for data collection, no prior provision of contact diary to record that information and retrospective nature of data collection for the first time point). We studied only the socio-demographic factors associated with contact patter and did not study certain geographical, meteorological, and biological characteristics that can affect the contact rate due to feasibility constraints. The study did not assess the contact patterns that occurred with mask use (which might influence the transmission dynamics) and household members of participants with whom the contact rate and duration are expected to be the maximum. Irrespective of the lockdown, the contact rate at the households would remain constant between the periods, but the higher duration of contacts expected with the household members during lockdown would skew the overall contact duration assessed in our study at various social settings. Future surveys shall also assess the mixing patterns and tracing of social contacts (verification of survey findings) using traditional methods, and triangulation of data can be done using several data collection methods such as telephonic interviews, online questionnaires, and mobile applications. Future research can focus on performing a follow-up study to identify and explore the possible risks and benefits associated with such reduction in the social contacts and its impact during any similar catastrophic events.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. Modes of transmission of virus causing COVID-19: Implications for IPC precaution recommendations. Available from: https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations . [Last accessed on 2020 May 06]
- 2.Weekly operational update on COVID-19-31 May. 2021. Available from: https://www.who.int/publications/m/item/weekly-operational-update-on-covid-19-26-april-2021 . [Last accessed on 2021 May 31]
- 3.MoHFW. COVID-19 INDIA. Ministry of Health and Family Welfare. Available from: https://www.mohfw.gov.in/index.php . [Last accessed on 2020 May 01]
- 4.Steps taken by countries in fighting COVID-19 pandemic. Available from: https://www.aa.com.tr/en/health/steps-taken-by-countries-in-fighting-covid-19-pandemic/1812009 . [Last accessed on 2020 May 06]
- 5.Herren CM, Brownwright TK, Liu EY, El Amiri N, Majumder MS. Democracy and mobility: A preliminary analysis of global adherence to non-pharmaceutical interventions for COVID-19. Rochester, NY: Social Science Research Network; 2020. Report No.: ID 3570206. Available from: https://papers.ssrn.com/abstract=3570206 . [Last accessed on 2020 May 06] [Google Scholar]
- 6.COVID-19: Lockdown across India, in line with WHO guidance. UN News. 2020. Mar 24. Available from: https://news.un.org/en/story/2020/03/1060132 . [Last accessed on 2020 May 06]
- 7.Dietz K. The estimation of the basic reproduction number for infectious diseases. Stat Methods Med Res. 1993;2:23–41. doi: 10.1177/096228029300200103. [DOI] [PubMed] [Google Scholar]
- 8.Fu Y. Contact diaries: Building archives of actual and comprehensive personal networks. Field Methods. 2007;19:194–217. [Google Scholar]
- 9.Read JM, Edmunds WJ, Riley S, Lessler J, Cummings DA. Close encounters of the infectious kind: Methods to measure social mixing behaviour. Epidemiol Infect. 2012;140:2117–30. doi: 10.1017/S0950268812000842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Melegaro A, Jit M, Gay N, Zagheni E, Edmunds WJ. What types of contacts are important for the spread of infections?: using contact survey data to explore European mixing patterns. Epidemics. 2011;3:143–51. doi: 10.1016/j.epidem.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 11.Census of India Website: Office of the Registrar General & Census Commissioner, India. Available from: http://www.censusindia.gov.in/2011-Common/CensusData2011.html . [Last accessed on 2019 Apr 21]
- 12.Statistics Times. Population of Puducherry (Census 2011) Available from: http://statisticstimes.com/demographics/population-of-puducherry.php . [Last accessed on 2020 May 07]
- 13.Census of India. Puducherry District Population Religion - Puducherry Literacy, Sex Ratio - Census India 2011 [Internet] www.censusindia.co.in. [cited 2022 Apr 29]. Available from: https://www.censusindia.co.in/district/puducherry-district-puducherry-635 .
- 14.Sarala G National Commission for Women. A Situational Analysis of Women and Girls in Pondicherry. New Delhi: National Commission for Women; 2005. p. 96. Available from: http://ncwapps.nic.in/pdfReports/Gender_Profile_Pondicherry.pdf . [Google Scholar]
- 15.Sivanantham P, Sahoo J, Lakshminarayanan S, Bobby Z, Kar SS. Profile of risk factors for Non-Communicable Diseases (NCDs) in a highly urbanized district of India: Findings from Puducherry district-wide STEPS Survey, 2019-20. PloS One. 2021;16:e0245254. doi: 10.1371/journal.pone.0245254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hoang T, Coletti P, Melegaro A, Wallinga J, Grijalva CG, Edmunds JW, et al. A systematic review of social contact surveys to inform transmission models of close-contact infections. Epidemiology. 2019;30:723–36. doi: 10.1097/EDE.0000000000001047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nishiura H, Linton NM, Akhmetzhanov AR. Serial interval of novel coronavirus (COVID-19) infections. Int J Infect Dis. 2020;93:284–6. doi: 10.1016/j.ijid.2020.02.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Leung K, Jit M, Lau EHY, Wu JT. Social contact patterns relevant to the spread of respiratory infectious diseases in Hong Kong. Sci Rep. 2017;7:1–12. doi: 10.1038/s41598-017-08241-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Horby P, Thai PQ, Hens N, Yen NTT, Mai LQ, Dang DT, et al. Social contact patterns in Vietnam and implications for the control of infectious diseases. PLoS One. 2011;6:e16965. doi: 10.1371/journal.pone.0016965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mossong J, Hens N, Jit M, Beutels P, Auranen K, Mikolajczyk R, et al. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. 2008;5:e74. doi: 10.1371/journal.pmed.0050074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kumar S, Gosain M, Sharma H, Swetts E, Amarchand R, Kumar R, et al. Who interacts with whom? Social mixing insights from a rural population in India. PLoS One. 2018;13:e0209039. doi: 10.1371/journal.pone.0209039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bolton KJ, McCaw JM, Forbes K, Nathan P, Robins G, Pattison P, et al. Influence of contact definitions in assessment of the relative importance of social settings in disease transmission risk. PLoS One. 2012;7:e30893. doi: 10.1371/journal.pone.0030893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kretzschmar M, Mikolajczyk RT. Contact profiles in eight European countries and implications for modelling the spread of airborne infectious diseases. PloS One. 2009;4:e5931. doi: 10.1371/journal.pone.0005931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Edmunds WJ, O'Callaghan CJ, Nokes DJ. Who mixes with whom? A method to determine the contact patterns of adults that may lead to the spread of airborne infections. Proc Biol Sci. 1997;264:949–57. doi: 10.1098/rspb.1997.0131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vega DI. Lockdown, one, two, none, or smart. Modeling containing covid-19 infection. A conceptual model. Sci Total Environ. 2020;730:138917. doi: 10.1016/j.scitotenv.2020.138917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The Economic Times. India's COVID-19 doubling rate slower, mortality rate lower than US, Italy, Spain, UK. Available from: https://economictimes.indiatimes.com/industry/healthcare/biotech/healthcare/indias-covid-19-doubling-rate-slower-mortality-rate-lower-than-us-italy-spain-uk/articleshow/75471247.cms?from=mdr .
- 27.Teslya A, Pham TM, Godijk NG, Kretzschmar ME, Bootsma MCJ, Rozhnova G. Impact of self-imposed prevention measures and short-term government-imposed social distancing on mitigating and delaying a COVID-19 epidemic: A modelling study. PLoS Med. 2020;17:e1003166. doi: 10.1371/journal.pmed.1003166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jarvis CI, Van Zandvoort K, Gimma A, Prem K, Auzenbergs M, O'Reilly K, et al. Quantifying the impact of physical distance measures on the transmission of COVID-19 in the UK. BMC Med. 2020;18:124. doi: 10.1186/s12916-020-01597-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lonergan M, Chalmers JD. Estimates of the ongoing need for social distancing and control measures post-“lockdown” from trajectories of COVID-19 cases and mortality. Eur Respir J. 2020;56:2001483. doi: 10.1183/13993003.01483-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schueller E, Lin G, Tseng K, Balasubramanian R, Kapoor G, Joshi J, et al. COVID-19 in India: Potential impact of the lockdown and other longer-term policies. The Center for disease dynamics, economics & policy. Available from: https://cddep.org/wp-content/uploads/2020/04/India-Shutdown-Modeling-Slides-Final-2.pdf .
- 31.Burlacu A, Crisan-Dabija R, Covic A, Raiu C, Mavrichi I, Popa IV, et al. Pandemic lockdown, healthcare policies and human rights: Integrating opposed views on COVID-19 public health mitigation measures. Rev Cardiovasc Med. 2020;21:509–16. doi: 10.31083/j.rcm.2020.04.274. [DOI] [PubMed] [Google Scholar]
- 32.Chowdhury R, Luhar S, Khan N, Choudhury SR, Matin I, Franco OH. Long-term strategies to control COVID-19 in low and middle-income countries: An options overview of community-based, non-pharmacological interventions. Eur J Epidemiol. 2020;35:743–8. doi: 10.1007/s10654-020-00660-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Niedzwiedz CL, Green MJ, Benzeval M, Campbell D, Craig P, Demou E, et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: Longitudinal analyses of the UK Household Longitudinal Study. J Epidemiol Community Health. 2021;75:224–31. doi: 10.1136/jech-2020-215060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gautam V, S D, Rustagi N, Mittal A, Patel M, Shafi S, et al. Health literacy, preventive COVID 19 behaviour and adherence to chronic disease treatment during lockdown among patients registered at primary health facility in urban Jodhpur, Rajasthan. Diabetes Metab Syndr. 2021;15:205–11. doi: 10.1016/j.dsx.2020.12.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liquor shops to remain shut as Puducherry to relax lockdown rules from May 4. The New Indian Express. Available from: https://www.newindianexpress.com/states/tamil-nadu/2020/may/04/liquor-shops-to-remain-shut-as-puducherry-to-relax-lockdown-rules-from-may-4-2138768.html . [Last accessed on 2020 May 06]