Abstract
Aim:
To evaluate the psychometric characteristics of the Perinatal Missed Care Survey and assess the prevalence of nurse-reported missed care during labor and birth.
Background:
Nursing care during labor and birth differs from other nursing care. Empirical evidence is scant regarding nursing quality and missed nursing care during labor and birth, which are important aspects of quality in maternity care.
Methods:
We conducted exploratory and confirmatory factor analysis on a previously developed perinatal missed nursing care instrument using data from 3,466 registered nurses. Measures included missed nursing care, reasons for missed nursing care, and demographic characteristics. All birth hospitals in each of 37 states were invited to distribute surveys electronically via email to their labor and delivery RN staff. The overall response rate from 277 hospitals that facilitated the survey was 35%.
Results:
Some missed care was reported for each of 25 missed care items. Labor support, intake and output, patient teaching, timely documentation, timely medication administration, and thorough review of prenatal records were missed at least occasionally by >50% respondents. Labor resources (83%), material resources (77%), and communication (60%) were reported reasons for missed nursing care. Exploratory factor analysis aligned with previous testing. Confirmatory factor analysis demonstrated good model fit.
Conclusions:
The Perinatal Missed Care Survey demonstrates good validity and reliability as a measure of missed nursing care during labor and birth. Our findings suggest missed nursing care during labor and birth is prevalent and occurs in aspects of care that could contribute to patient harm when missed.
Keywords: maternity nursing, missed nursing care, nursing care standards, psychometric, quality of health care, survey methodology
Nursing care during labor and birth is critical for patient safety, experience, and outcomes. Labor and birth comprise dynamic physiologic and psychosocial processes that require focused support. Certain complications can also develop suddenly and require quick recognition of clinical deterioration, rapid response, and mobilization of the health care team to prevent maternal or fetal injury or even death. Nurses are pivotal to both of these aspects of care, as they provide the majority of direct care management and maternal-fetal surveillance in US hospitals. Perinatal nurses complete full medical, obstetric, psychological, and social assessments; provide specialized labor support care; continuously assess and monitor maternal and fetal status during labor; administer and titrate oxytocin and other high-risk medications such as intravenous insulin and magnesium sulfate infusions; and provide recovery care for mother-baby dyads following vaginal and cesarean birth (Authors, 2012, 2016a, 2016b, 2017b). While most labors are low-risk, supportive care during labor requires dedicated time and skill and can contribute to improved maternal and infant outcomes (Bohren et al., 2017; Van der Gucht & Lewis, 2015). Pregnancy complications and other co-morbidities that require complex ongoing nursing surveillance and management are also increasing in the childbearing population (Main et al., 2020; Oot et al., 2021).
Despite the central role of nursing in hospital-based labor and birth, evidence for nursing care quality in maternity settings is exceptionally limited. This is a surprising deficiency in the quality arena. Most (>98%) of the approximately 3.75 million annual US births occur in hospitals (Martin, et al., 2021; MacDorman & Declercq, 2019), and maternal birth outcomes have been worsening (Petersen et al., 2019). Missed nursing care (defined as necessary care that is delayed, unfinished, or completely missed; also known as unfinished care and implicit rationing of care) is an error of omission and a form of medical underuse that may be an appropriate measure of nursing care quality (Kalisch, Landstrom, & Williams, 2009; Kalisch, Landstrom, & Hinshaw, 2009; VanFosson et al., 2016). Missed nursing care is a process theorized to have a negative effect on patient outcomes and to be a mechanism by which structural factors affect patient outcomes (Kalisch & Williams, 2009). Hence, missed nursing care may explain observed associations between nurse staffing and patient outcomes (Griffiths et al., 2018; Recio-Saucedo et al., 2018; Smith et al., 2020), and measurement of missed perinatal nursing care may be an important tool for assessing and improving perinatal safety and quality.
Missed nursing care, measured using several instruments, has been associated with objectively reported patient outcomes such as medication errors, nosocomial infections, falls, and readmissions, as well as patient-reported satisfaction scores (Recio-Saucedo et al., 2018); and measures of infant feeding (Tubbs-Cooley, Pickler, & Meinzen-Derr, 2015). Nursing care during labor and birth differs substantially from other forms of nursing care due to differences in the population served, the forms of care provided, and the aspects of care that may affect patient outcomes. Therefore, it is unknown whether the missed care findings from other settings are generalizable to inpatient childbirth. Conceptual exploration of missed nursing care in perinatal settings suggests that missed perinatal nursing care is consequential (Authors, 2017a, 2017b). However, empirical evidence regarding the prevalence of missed perinatal nursing care is limited (Lake et al., 2019; Lake et al., 2020; Authors, 2019).
Kalisch and colleagues developed one of the reliable and valid measures of missed nursing care, the MISSCARE survey (Kalisch & Williams, 2009), which has been used extensively in medical surgical care and has been adapted to pediatric (Bagnasco et al., 2018) and neonatal intensive care (Tubbs-Cooley, Pickler, Younger, et al., 2015). Our team previously adapted the MISSCARE Survey for the labor and birth portion of perinatal care. The resulting Perinatal Missed Care Survey incorporates nursing care and critical surveillance activities specific to labor and birth. We recently demonstrated Perinatal Missed Care Survey acceptability, reliability, and a factor structure consistent with the original instrument (Authors, 2019). The purpose of the present study was to confirm reliability and validity of the Perinatal Missed Care Survey in a large sample of nurses and hospitals, test construct validity with confirmatory factor analysis, and describe the prevalence of missed nursing care during labor and birth.
Methods
We previously used the instrument development process to modify the validated MISSCARE instrument (Kalisch, Landstrom, & Williams, 2009; Kalisch & Williams, 2009) for measurement of missed nursing care during labor and birth. An overview of the modification process is illustrated in Figure 1. Phase one has been previously reported (Authors, 2019). That phase involved a) a sequential approach to instrument development, and b) instrument testing and exploratory factor analysis with a sample of 669 labor and delivery nurses from 67 hospitals in California, Michigan, and New Jersey. In this manuscript we report findings from phase 2, including exploratory and confirmatory factor analysis and construct validation in a larger sample of nurses. Data for this phase were collected via the Nursing Care During Labor Survey as part of a larger study which ultimately aims to test associations between nursing care and patient outcomes.
Figure 1.
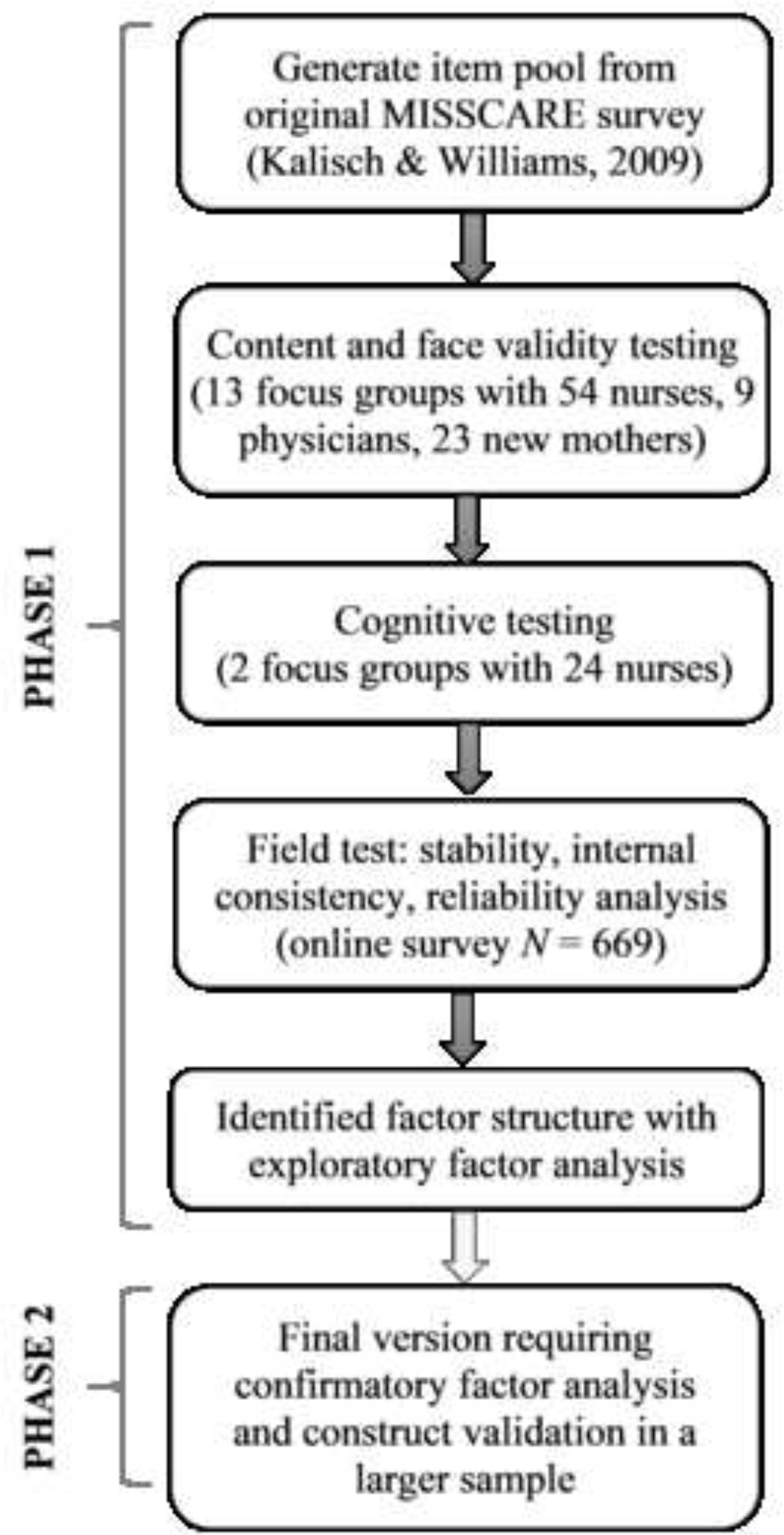
Steps in adapting the MISSCARE Survey to the maternity care setting. Authors (2019). [citation, permission]
The Nursing Care During Labor Survey comprised the Perinatal Missed Care Survey items (the focus of this manuscript), twelve items measuring demographic and professional characteristics of the nurse participants, and several other scales including a safety climate scale and a staffing scale. Demographic items included age; sex, race, and ethnicity (required elements for federal grants); highest level of education; certifications (e.g., Inpatient Obstetrics, Maternal Newborn Nurse, Electronic Fetal Monitoring); experience as a registered nurse, caring for patients during labor and birth, and working at this hospital; shift usually worked; full-time or part-time status; and role on the unit (e.g., staff nurse, charge nurse, nurse manager, clinical specialist, nurse educator). The total survey took 10–15 minutes to complete.
Participants and Settings
There are no nationally representative or comprehensive state databases through which to identify our target population of labor and delivery nurses. The membership list of the Association of Women’s Health, Obstetric, and Neonatal nurses, and the certification list from the National Certification Corporation can identify labor nurses. However, nurses in these databases are those most highly professionally engaged, and are unlikely to be representative of labor nurses nationally. Similarly, the National Database of Nursing Quality Indicators is a proprietary platform that collects voluntarily reported hospital-level perinatal indicators, nurse work environment data, and nurse satisfaction data. Therefore, we recruited RNs by inviting all birth hospitals in 36 states and the District of Columbia to facilitate survey distribution.
For this study, the target states were selected by identifying those with the availability of state inpatient data for the larger study of birth outcomes. To ensure inclusion of rural-serving and critical access hospitals, we identified all hospitals that had at least 40 births in 2016 (according to the 2016 American Hospital Association Annual Survey) in the target states. We did not recruit in Alabama, Alaska, Connecticut, Delaware, Idaho, Illinois, Indiana, Louisiana, Montana, New Hampshire, North Dakota, Ohio, Tennessee, or Wyoming due to inability to determine a path to acquisition of corresponding state inpatient data from these states at the time of survey distribution. Nurse leaders of all eligible labor and birth units (n = 2,186) in the target states were contacted by telephone and/or email and invited to facilitate the process of having the labor nurses in their hospital participate in the study.
Once the nurse leader at each hospital agreed to facilitate, we obtained the number of eligible staff for that hospital from the leader and invited labor nurses to participate in an online Qualtrics survey via email. The landing page included informed consent information. Nurses consented to participate by continuing to the survey questions. Most nurse leaders distributed the link to nurses through internal email distribution lists due to institutional preferences and firewall concerns. We provided at least three follow-up reminders for leader-distributed surveys. A smaller number of facilities provided email distribution lists for direct recruitment. These nurses received unique links and tailored reminders via Qualtrics. Six hospitals opted to administer anonymous paper surveys, which were returned by mail to the study center for data entry. Nurse leaders had no access to survey responses.
The Institutional Review Boards at University of California, San Francisco and New York University approved the study. Our study center centrally handled all recruitment and data collection so that participating hospitals were not engaged in human subjects activity. However, we also obtained local IRB approval at any of the hospitals that required it before surveying their labor nurses.
Measures
The Perinatal Missed Care Survey is an adaptation for the perinatal setting of the valid and reliable MISSCARE Survey (Kalisch & Williams, 2009). In preliminary psychometric testing the Perinatal Missed Care Survey performed similarly to the original MISSCARE instrument (Authors., 2019). The Perinatal Missed Care Survey consists of two parts. Part 1, Aspects of Required Nursing Care (Aspects; comparable to MISSCARE Part A), consists of 25 items assessing the frequency at which required aspects of basic labor nursing care are delayed, unfinished, or completely missed on a 4-point Likert scale with options 1=Rarely delayed/unfinished/missed, 2 = occasionally delayed/unfinished/missed, 3 = Frequently delayed/unfinished/missed, and 4=Always delayed/unfinished/missed, or “Not applicable.” Part 2, Reasons for Missing Required Nursing Care (Reasons; comparable to MISSCARE Part B) consists of 16 items assessing potential reasons that nursing care was delayed, unfinished, or missed using a 4-point Likert scale from 1=Not a reason to 4=Significant factor. Surveillance is a recently proposed addition to the MISSCARE survey (Dabney et al., 2019). The Perinatal Missed Care instrument already includes surveillance items, such as “Recognize and respond to indeterminate (Category II) or abnormal (Category III) FHR changes within 15 minutes,” “Recognize and respond to excessive uterine activity within 20 minutes,” and “recognize and respond to new maternal complications within 10 minutes (e.g. hypertension, bleeding)” (Authors, 2019).
Hospital characteristics, including annual birth volume, ownership, AHA level of obstetrics and neonatal care, teaching status, rurality, and critical access and sole community provider status, were obtained from the 2018 American Hospital Association Survey.
Data Analysis
Characteristics of the responding hospitals were compared to all other hospitals in the AHA survey with ≥40 births using unequal variance t-tests or Fisher’s Exact test as appropriate. Nurses’ responses were analyzed first at the item level to assess missing data, response distribution, frequency of reporting any missed care (rarely, occasionally, frequently, or always) and degree to which reasons for missed care were endorsed (minor to significant reason). We then followed the methods described by Kalisch & Williams (2009) and conducted factor analyses of the Aspects and Reasons item sets.
The study sample was randomly split into two equal sized groups for the purpose of conducting exploratory factor analysis on a development sample and confirmatory factor analysis on a validation sample. These groups did not differ in terms of demographics, nursing experience, or work characteristics, indicating adequacy of the random split. To account for the ordinal nature of the data (4-point Likert scales) and non-normal distributions of responses, factor analyses were conducted on matrices of polychoric correlations between items.
For the exploratory factor analysis (EFA), Horn’s parallel analysis was used to identify the number of factors to retain. Parallel analysis uses simulation to identify the optimal number of factors to retain (Hayton et al., 2004). Factors were extracted using principal components methods, and Varimax rotation was used to generate uncorrelated factors and produce simple structure.
The identified solution was reviewed using multiple criteria: factors with eigenvalues > 1, amount of variance explained, items with factor loadings exceeding 0.32 (corresponding to approximately 10% overlapping variance between item and the factor) (Tabachnick, 2001), minimal cross loadings, and factors having at least 4 items with their primary loading on them. Confirmatory factor analysis (CFA) was conducted on data from the validation sample to evaluate the factor structure identified by the EFA. Adequacy of model fit was determined using multiple fit indices (root mean square error of approximation [RMSEA], standardized root mean square residual [SRMR], confirmatory factor index [CFI], Tucker Lewis Index [TLI]). Reliability for subscales of the reasons for missed care identified by the EFA was assessed using Cronbach’s alpha. Following exclusions, missingness was below the suggested threshold for applying missing data techniques (<5%), so complete case analyses were conducted (Schafer, 1999). Construct validity was first established using the described CFA to replicate the factor structure identified in the exploratory factor analyses and by the original authors, and then using a convergent/discriminant validity framework to determine the pattern of associations between the scales and factors hypothesized to be associated or not associated with missed care.
Distributions of a mean score and a count score for Aspects items were explored and tested for convergent validity with measures of safety climate and nurse-reported staffing, which we hypothesized would be negatively correlated with aspects of and reasons for missed care. Discriminant validity for aspects of missed care was measured by testing for associations with hospital ownership, shift worked, and full- vs part-time work, which have been shown not to be associated with missed care in prior studies. Reasons for missed care scales were also hypothesized to be associated with safety climate and nurse-reported staffing, and hypothesized to not be associated with full-time employment status and core based statistical area (CBSA: metropolitan, micropolitan, rural). All analyses were conducted using Stata/SE v14.2
Results
Data were collected from February 2018 through July 2019. Four percent of contacted hospitals were ineligible due to hospital closure (n=10) or discontinuation of labor and delivery services (n=87). Of the remaining 2,089 hospitals, 202 (10%) declined to participate and 1,610 (77%) did not respond to repeated study center outreach. Nurse leader turnover and firewall issues accounted for about 20% of hospital non-response. Leaders from 277 hospitals (12.7%) in 34 states agreed to facilitate survey distribution, and the Nursing Care During Labor Survey was distributed to 10,630 nurses. No hospital partners responded, hence no surveys were distributed in the District of Columbia, Rhode Island, or South Carolina (Figure 2).
Figure 2.
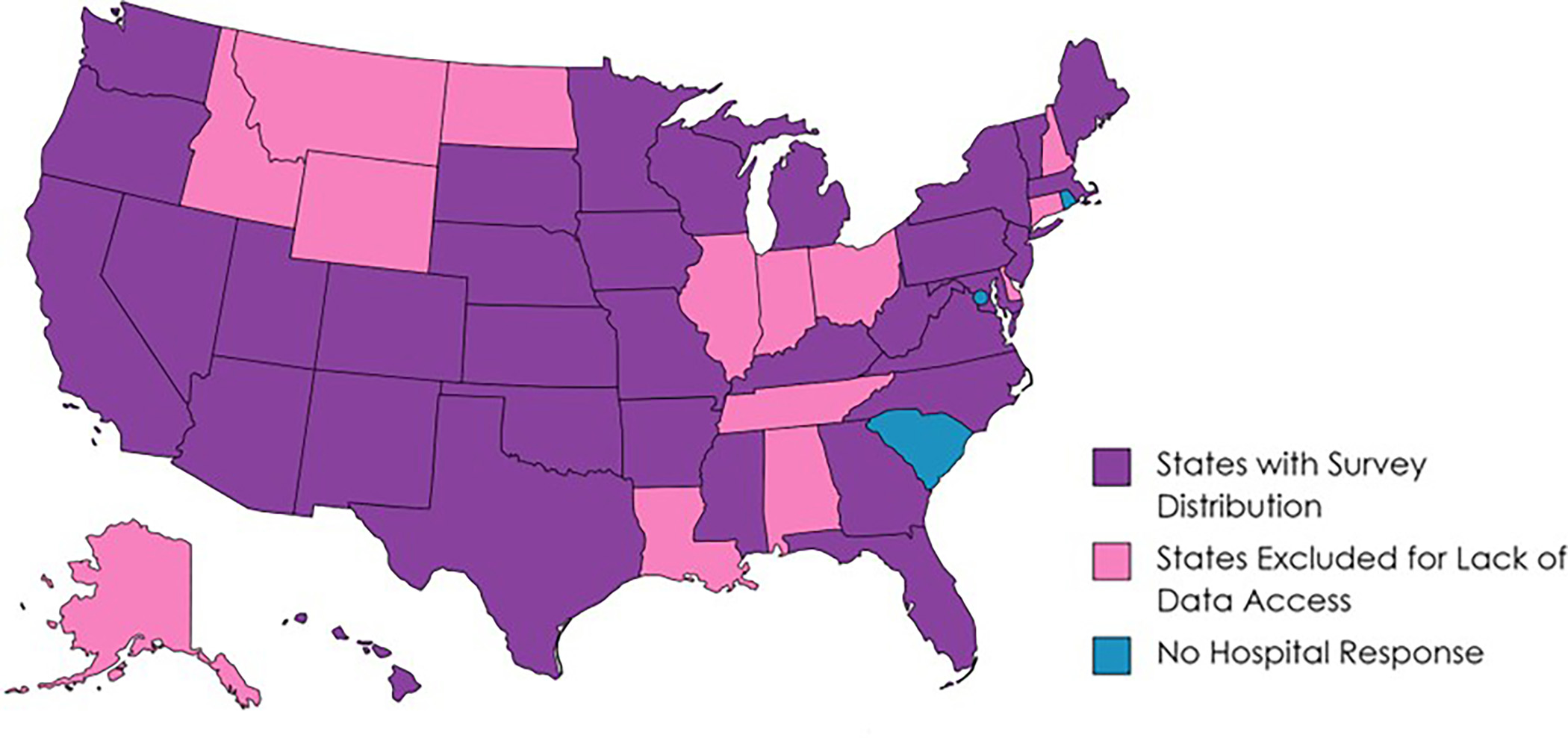
Survey Distribution by State
The nurse response rate was 35% (n=3,676) after excluding 568 surveys that were either blank (500) or ineligible (68). An additional 199 surveys (5.4%) were excluded for exceeding a missing data threshold that accounted for both the absolute number of questions unanswered (40% or ~30 items) and the number of invalid scale scores per participant due to unanswered questions (≥3 scale scores). Finally, 11 surveys were excluded because participants reported a role that did not meet inclusion criteria (e.g., certified nurse midwife, patient care technician).
The mean age of participants was 40.7±11.8 years. Participants were experienced (median 10 years in labor and delivery, interquartile range 3.5–19, range 1–49), identified as female (99.5%), not Hispanic/Latino (94.3%), and white (92.2%). The majority worked as full-time (75%) as staff nurses (64%) or both staff and charge (26%). Most participants worked day shift (53%) or night shift (35%) as opposed to evening (3.5%) or rotating shifts (8.2%). For highest degree, almost two-thirds of the sample held a bachelor’s degree (61.7%) and nearly one-third held an associate’s degree (27.5%). The number of labor and delivery nurses employed by hospitals represented in this study, as reported by nurse leaders, ranged from 2–200 (mean 38.7; standard deviation 30.9; median 28, interquartile range 17–51). The mean labor and delivery unit response rate was 38.2% (standard deviation 20.4; median 36.6, interquartile range 23.7–48.1).
Of the 277 hospitals that facilitated survey distribution, 271 had valid 2018 AHA survey data. Compared to all hospitals reporting ≥ 40 annual births (n=2705), study hospitals had higher mean annual births (1,621.2±1,986.1, median 895, range 49–14,334 vs. 1,243.3±1,457.1, median 748, range 40–16,829; p=0.002). They also differed in birthrates, with a lower proportion of hospitals with <500 births (30.3% vs. 38.1%) and a higher proportion of hospitals with ≥2500 births (20.7% vs. 14.%), p=0.009; in ownership, with study hospitals less likely to be government (17% vs 19.6%) or investor-owned (10% vs. 15.7%) and more likely to be church operated (14.8% vs 11.1%) or other non-profit (57.9% vs 53.6%), p=0.022. Study hospitals were more likely to have neonatal intensive care (48.1% vs 36.1%), p<0.001. There were no statistically significant differences in teaching status, rurality (metropolitan, micropolitan, or rural), critical access status, or sole community provider status.
Construct Validity
Aspects of Required Nursing Care & Frequency of Missed Care.
The proportions of nurses reporting that specified aspects of care were occasionally, frequently, or always missed are shown in Table 1. Most aspects of care were reported rarely delayed, missed, or incomplete (~40 to 80% of respondents), although some degree of missed nursing care was reported for each of the 25 aspects, and 6.7% of respondents reported missing care on all 25 aspects. Ten aspects were reported as missed at least occasionally by more than half of respondents, and more than 75% of respondents reported two aspects (real or near-time documentation and monitoring intake and output) missed at least occasionally. Among the least missed aspects of care (≤ 30% of respondents reporting as missed occasionally or more frequently) were four safety items: recognize and respond to fetal heart rate changes, recognize and respond to excessive uterine activity, recognize and respond to new maternal complications, and timely notification of physician/midwife to attend birth. Horn’s parallel analysis of the Aspects items identified a single factor solution. Despite the single factor having a large adjusted eigenvalue (15.1), all factor loadings were <0.23 indicating the single factor explained little of the variability in items’ responses (loadings correspond to <5.3% of variability in responses). This did not meet the criteria for a strong solution, thus no further psychometric analysis was performed.
Table 1.
Frequency of Missed Nursing Care Reported by Respondents
| Proportion Reporting > Rarely Missed |
||||
|---|---|---|---|---|
| Aspects of Required Nursing Care | Occasionally | Frequently | Always | Total |
|
| ||||
| 1. Provide labor support (peanut ball, hydrotherapy, etc) | 33.1 | 18.3 | 2.5 | 54.0 |
| 2. Assess effectiveness of medications | 32.3 | 14.8 | 2.3 | 49.4 |
| 3. Check bladder status/voiding needs every 2 hours | 37.0 | 16.4 | 2.2 | 55.6 |
| 4. Assess pain status every hour | 35.3 | 19.4 | 2.9 | 57.5 |
| 5. Thorough review of prenatal records | 39.4 | 20.5 | 3.2 | 63.0 |
| 6. Patient teaching about procedures, tests, and diagnostic studies | 35.1 | 14.3 | 2.6 | 52.1 |
| 7. Medications administered within 30 minutes of scheduled time | 38.9 | 11.9 | 1.9 | 52.8 |
| 8. Administer oxytocin as per orders or protocol | 25.1 | 11.6 | 2.3 | 39.1 |
| 9. Response to call light is initiated within 5 minutes | 18.7 | 9.7 | 2.4 | 30.8 |
| 10. Emotional support to patient and/or family | 28.7 | 13.2 | 2.4 | 44.4 |
| 11. Patient bathing, skin care, or pericare | 37.4 | 13.7 | 2.4 | 53.9 |
| 12. Recognize & respond to indeterminate (Category II) or abnormal (Category III) FHR changes within 15 minutes | 12.3 | 7.1 | 2.4 | 21.9 |
| 13. Recognize & respond to excessive uterine activity within 20 minutes | 15.9 | 7.7 | 2.2 | 26.0 |
| 14. Recognize & respond to new maternal complications within 10 minutes | 19.7 | 7.7 | 2.4 | 30.0 |
| 15. Focused reassessments according to patient condition | 28.0 | 11.3 | 3.0 | 42.7 |
| 16. Real/near-time documentation of maternal-fetal assessments | 37.2 | 35.1 | 6.3 | 78.9 |
| 17. Patient teaching about signs/symptoms, when to call, etc | 22.9 | 9.4 | 2.4 | 35.7 |
| 18. Monitor intake and output | 45.5 | 28.6 | 3.9 | 78.4 |
| 19. Provide skin-to-skin mother-baby care immediately after birth | 13.8 | 8.6 | 2.0 | 24.4 |
| 20. Assess vital signs as ordered, or per protocol | 31.6 | 10.6 | 2.3 | 44.8 |
| 21. Provide thorough patient handoff | 30.8 | 10.9 | 2.3 | 44.3 |
| 22. Hand washing | 18.2 | 8.0 | 2.4 | 28.8 |
| 23. Breastfeeding within 1 hour of birth for breastfeeding women | 26.0 | 9.5 | 1.8 | 37.6 |
| 24. Recovery care - 2 hours of every 15-minute mom & every 30-minute baby assessments | 24.7 | 13.0 | 4.3 | 43.2 |
| 25. Timely notification of physician/nurse-midwife to attend birth | 13.9 | 6.4 | 2.4 | 22.7 |
Items were dichotomized (rarely = 0, occasionally/frequently/always = 1), and the distribution of the count of missed aspects compared to the distribution of mean scores. The count scores were more normally distributed, exhibited greater variability (possible score 0–25, mean 11.03±7.03, median 10, interquartile range 5–16), and are more easily interpretable. For convergent validity, as we hypothesized, there were significant moderate negative correlations with safety climate and nurse-reported staffing guideline adherence (r = −0.298 and −0.273 respectively, p<0.05) and for discriminant validity there were no significant differences between count scores and hospital ownership, shift worked, or part-time vs. full-time status (Table 2).
Table 2.
Tests of Convergent/Discriminant Validity for Aspects Count and Reasons Scales
| Characteristic | Aspects Count | Reasons Communication | Reasons Materiel | Reasons Labor | |||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Hospital ownership | n | m | sd | m | sd | m | sd | m | sd |
|
| |||||||||
| Governmen | 557 | 10.7 | 7.0 | ||||||
| Church | 564 | 11.4 | 7.2 | ||||||
| Other non-profit | 2,055 | 10.9 | 6.9 | ||||||
| Investor | 219 | 12.1 | 7.6 | ||||||
| Core-based statistical area | n | m | sd | m | sd | m | sd | m | sd |
|
| |||||||||
| Metroa | 2,761 | 1.84b,c | 0.56 | 2.30b,c | 0.81 | 2.61b,c | 0.80 | ||
| Microb | 436 | 1.69a | 0.52 | 1.95a,c | 0.75 | 2.33a,c | 0.70 | ||
| Ruralc | 198 | 1.65a | 0.47 | 1.72a,b | 0.62 | 2.11a,b | 0.66 | ||
| Shift type | n | m | sd | m | sd | m | sd | m | sd |
|
| |||||||||
| Daysa | 1,789 | 11.1 | 7.0 | ||||||
| Eveningsb | 119 | 11.6 | 7.1 | ||||||
| Nightsc | 1,176 | 11.2 | 6.9 | ||||||
| Rotatingd | 275 | 10.5 | 6.7 | ||||||
| Employment | n | m | sd | m | sd | m | sd | m | sd |
|
| |||||||||
| Full-time | 2,523 | 11.0 | 7.0 | 1.8 | 0.6 | 2.2 | 0.8 | 2.6 | 0.8 |
| Part-time | 835 | 11.3 | 7.0 | 1.8 | 0.5 | 2.2 | 0.8 | 2.5 | 0.8 |
Superscript notations identify which groups differed significantly on MISSCARE scales– e.g. For Reasons-Communication, rural hospitals differed from metro hospitals; while for Reasons-Materiel, rural hospitals differed from both metro and micro hospitals.
Reasons for Missing Required Nursing Care.
The proportion of respondents who reported each reason as a factor in missed nursing care are shown in Table 3. The Kaiser-Meyer-Olkin measure of sampling adequacy was 0.9178, indicating suitability for factor analysis.
Table 3.
Reasons for Missing Required Aspects of Care
| Reason | Minor Factor % | Moderate Factor % | Significant Factor % | Total %a |
|---|---|---|---|---|
|
| ||||
| Tension or communication breakdowns within nursing team | 47.2 | 13.2 | 3.4 | 63.9 |
| Lack of backup support from team members | 41.3 | 15.9 | 5.9 | 63.3 |
| Colleague/assistant/OB tech did not communicate that care was not done | 47.2 | 11.6 | 2.5 | 61.6 |
| Caregiver is off unit or unavailable (including: nurse/assistant/OB tech) | 35.0 | 7.3 | 2.4 | 44.9 |
| Tension or communication breakdowns with medical or midwifery staff | 44.5 | 15.1 | 4.8 | 64.5 |
| Tension or communication breakdowns with other support departments | 43.9 | 16.8 | 4.6 | 65.5 |
| Other departments did not provide the care needed | 37.6 | 10.8 | 3.0 | 51.6 |
| Inadequate handoff from previous shift or sending unit | 53.6 | 12.0 | 2.7 | 68.5 |
| Supplies/equipment not available when needed | 41.9 | 22.4 | 11.3 | 76.0 |
| Supplies/equipment not functioning properly when needed | 42.6 | 21.4 | 10.8 | 74.9 |
| Medications not available when needed | 44.1 | 25.8 | 10.1 | 80.2 |
| Unexpected rise in patient volume or patient acuity on the unit | 26.9 | 32.5 | 32.6 | 92.6 |
| Urgent patient situations (worsening condition, emergent cesarean) | 38.6 | 30.6 | 17.2 | 86.6 |
| Inadequate number of staff (patient assignments >recommended ratios) | 30.5 | 27.6 | 28.3 | 86.7 |
| Inadequate number of assistive personnel (assistants, OB techs) | 33.7 | 22.4 | 19.5 | 76.0 |
| Unbalanced patient assignments | 39.9 | 20.4 | 13.0 | 73.5 |
Horn’s parallel analysis identified a 3-factor solution explaining 66.7% of item variance. This solution satisfied multiple criteria, including factors comprised of three or more items with loadings >0.32 and no cross-loadings >0.32 between factors. Rotated factor loadings, eigenvalues, variance explained, and scales’ reliability are displayed in Table 4.
Table 4.
Factor Loadings and Reliability for Exploratory Factor Analysis with Varimax Rotation of Reasons for Missing Required Nursing Care
| Factor Loadings |
|||
|---|---|---|---|
| 1 | 2 | 3 | |
|
| |||
| Factor 1 Communication: Eigenvalue = 7.98; Variance = 49.9%; α =.85 | |||
| Tension or communication breakdowns w/in nursing team | 0.4649 | ||
| Lack of backup support from team members | 0.3282 | ||
| Colleague/assistant/OB tech did not communicate that care was not done | 0.3974 | ||
| Caregiver is off unit or unavailable (including nurse/assistant/OB tech) | 0.2166a | ||
| Tension or communication breakdowns with medical or midwifery staff | 0.3787 | ||
| Tension or communication breakdowns with other support departments | 0.3358 | ||
| Other departments did not provide the care needed | 0.2922a | ||
| Inadequate handoff from previous shift or sending unit | 0.3495 | ||
| Factor 2 Material Resources: Eigenvalue = 1.54; Variance = 9.7%; α =.86 | |||
| Supplies/equipment not available when needed | 0.5483 | ||
| Supplies/equipment not functioning properly when needed | 0.5394 | ||
| Medications not available when needed | 0.5155 | ||
| Factor 3 Labor Resources: Eigenvalue = 1.13; Variance = 7.1%; α =.87 | |||
| Unexpected rise in patient volume or patient acuity on the unit | 0.4417 | ||
| Urgent patient situations (worsening condition, emergent cesarean) | 0.3781 | ||
| Inadequate number of staff (patient assignments >recommended ratios) | 0.4758 | ||
| Inadequate number of assistive personnel (assistants, OB techs) | 0.4187 | ||
| Unbalanced patient assignments | 0.4015 | ||
Note: values <|0.32| suppressed
Primary loadings included for items that do not have loadings >0.32 on any factor.
Two items (reasons 4, caregiver off unit or unavailable and 7, other departments did not provide the care needed) did not load >0.32 on any factor, though their primary loadings were on the initial factor. All remaining items loaded above this threshold on a single factor each.
The factor structure identified was largely consistent with that identified by Kalisch and Williams (Kalisch & Williams, 2009), and we retained their naming conventions (Communication, Materiel and Labor Resources). Confirmatory factor analysis indicated that the factor structure identified by the EFA is an adequate fit for the data (RMSEA = .08, SRMR .051, CFI = .92, TLI = .90), and examination of modification indices did not identify any theoretically plausible changes that could improve model fit. Reliability was strong (Cronbach’s α ≥ .85) for corresponding subscales.
There was evidence supporting convergent validity of reasons scales with significant negative correlations between these scales and with safety climate (Communications r = −0.388, Material r = −0.317, Labor r = −0.391) and nurse-reported staffing guideline adherence (Communications r = −0.273, Material r = −0.294, Labor r = −0.402). Evidence for discriminant validity was mixed, with small but significant differences in all reasons scales by geographic region type (CBSA), ownership (reasons were more highly endorsed for RNs in metropolitan regions compared to micro and rural), and no significant differences on any reasons scales by part-time vs. full-time status (see Table 2).
Discussion
Our findings on the frequency of nurse-reported missed care are concerning in their own right, and doubly so in light of worsening childbirth outcomes in the United States. The three aspects of care reported missed by the largest proportions of nurses can all contribute to serious failures in care. Thorough review of prenatal records was missed at least occasionally by 63% of respondents. This represents a missed opportunity to identify social, medical, and obstetric factors that may increase a person’s risk for serious morbidity and contribute to failure to recognize emerging complications or clinical deterioration. Missed timely documentation of maternal-fetal assessments may limit other team members’ understanding of a birthing person’s clinical status. This parameter was reported missed at least occasionally by 78% of participants, and could result in failure of other team members to recognize and respond to clinical deterioration in a timely fashion. When the nurse’s assessments and reasoning are not visible to the rest of the clinical team, the nurse remains isolated from contributing substantively to team decisions. Finally, failure to monitor intake and output (reported missed by 78% of participants) can result in conditions of fluid overload and in clinicians’ failure to recognize conditions where decreased urine output is sign of serious trouble (e.g. worsening preeclampsia, shock, sepsis). As much as 60% of maternal morbidity and mortality is potentially preventable, and often involves failure to recognize and act upon signs and symptoms of clinical deterioration (Guglielminotti et al., 2021; Lappen, et al; 2021:Petersen et al., 2019). Thus, these three sources of missed nursing care may be contributing to serious and potentially preventable harm.
Aspects of care that were reported missed by smaller proportions of respondents also have serious implications. Frequent maternal and infant assessments for the first two hours after birth are crucial during a critical time of physiological transition for both patients. This period of care requires continuous nursing attendance at the bedside for ongoing surveillance of both patients, and interventions to support physiologic stability. Patient teaching, emotional support, and assistance with breastfeeding are highly valued by patients (Authors, 2017a). Missing these aspects of care may result in poor physical and emotional outcomes for childbearing families.
The five Labor Resources items and three Material Resources items were endorsed as minor, moderate, or significant factors contributing to missed nursing care by >70% of participants, and inadequate staffing was endorsed as a significant factor by 28% of participants. Six Communication items were endorsed as minor, moderate, or significant factors by >60% of participants. All items on the Reasons section of the survey represent system-level responsibility and accountability. Adequate staffing, assistive personnel, ability to respond to acuity, availability of supplies and equipment, and the communication culture within organizations are driven by executive-level decisions and priorities. Systems of care that do not provide adequate resources create an environment in which nurses are not able to perform all essential aspects of care and must prioritize or ration the care that gets delivered. The resulting omissions of essential nursing care reduce the quality and safety of patient care. Childbirth is a critical juncture affecting maternal, infant, and family health with potential long-range consequences. Systems and policies should be in place at the institutional and societal level to provide adequate essential care during this pivotal time.
Conclusions
The Perinatal Missed Care Survey is specific to the basic aspects of nursing care which are essential during labor and birth. In this study we found the survey to be a valid and reliable adaptation of the original MISSCARE instrument. The lack of a factor solution for the Aspects of Required Nursing Care (corresponding to MISSCARE Part A) is similar to previously reported findings and may be explained by the items representing a list of nursing actions that may not be related to each other (Bagnasco et al., 2018; Kalisch & Williams, 2009; Authors, 2019). Confirmatory factor analysis supported the three-factor solution for the Reasons for Missed Care. The Reasons subscales were consistent with those reported for MISSCARE Part B, and demonstrated good reliability (Cronbach’s α 0.85–0.87). Convergent and divergent validity were demonstrated for both Aspects count and Reasons scales. The Perinatal Missed Care Survey could potentially be used to measure nursing care quality, and to assess the effectiveness of structural interventions to improve quality and safety.
Our prior preliminary study (Authors, 2019) and one other study (Lake et al., 2019) have evaluated the frequency and prevalence of missed nursing care during labor and birth. A third study assessed the association between nurse burnout and missed care among labor nurses (Clark & Lake, 2020). Our findings are consistent with prior data, although nurses reported a lower prevalence of missed care in this study than in our preliminary study, and in both nurses report a higher prevalence than recorded by Lake et al. (2019; Clarke & Lake, 2020). While Lake and colleagues removed items that were not considered relevant to labor and birth (such as oral care) from the instrument they used, the tasks identified remain generic to nursing care across settings. The Perinatal Missed Care Survey is tailored to specific basic nursing actions during labor and following birth. These differences in instrument specification could account for the differences in our findings.
Overall, our findings on the frequency of missed nursing care and the factor structure of the Perinatal Missed Care Survey are consistent with the literature on missed nursing care in other settings. Across types of care, systematic reviews have found at that nurses consistently report missing at least one aspect of basic care on their last shift or that aspects of basic nursing care are missed more than occasionally on their units, depending on the instrument and instructions used (Jones et al., 2015; Mandal et al., 2020).
The self-reported nature of missed nursing care and the response rate are study limitations. Self-report is the primary approach used internationally in the missed nursing care literature, and it is substantially more feasible to implement than direct observation or patient reporting. Although we invited all hospitals in target states that had >40 annual births, there may be differences the quality of nursing care between hospitals that agreed to facilitate recruitment and those that did not. The directionality of such potential self-selection bias is unknown, however hospitals in this study were relatively similar to other birth hospitals in the 2018 AHA Annual Survey, and while missed nursing care is conceptualized as a unit- or hospital-level quality measure, prior studies describing missed nursing care in specialty settings have included units with ≥3 individual responses (Lake et al., 2017; Lake et al., 2019). Our approach and response rate are consistent with these prior studies. Finally, we did not specify a time frame for the assessment of missed nursing care. Recent pediatric and neonatal adaptations of the MISSCARE Survey have specified the last shift worked as the time frame, as do other instruments measuring missed care (Bagnasco et al., 2018; Mandal et al., 2020; Tubbs-Cooley, Pickler, Younger, et al., 2015). Using a standardized time frame of last shift worked for future investigations would enhance cross-study comparisons. A strength of this study is inclusion of items representing critical aspects of maternal and fetal surveillance that are consistent with the surveillance question in the Tasks Undone measure (Aiken et al., 2013) and the recent addition of surveillance to the revised MISSCARE survey (Dabney et al., 2019). The Perinatal Missed Care Survey items are more direct and relevant to basic nursing care during labor and birth.
Substantial additional research is needed to develop a robust set of nurse-sensitive indicators for the care of childbearing families. Childbearing people, nurses, and physicians alike believe that nursing care during labor and birth influences patient outcomes: there is consensus among these groups that nursing care contributes to cesarean birth rates, breastfeeding rates, and patient satisfaction (Authors, 2017a). Nurses also identify multiple pathways for nursing care to influence other perinatal patient safety and quality outcomes (Authors, 2017b). However, measures to demonstrate these linkages are scarce and difficult to delineate. Additional validation work on missed care during labor and birth could include work cross-validating nurse- and patient-reported missed care together, and more real-time shift-based assessments of missed nursing care (Tubbs-Cooley et al., 2019). Measures specific to postpartum and well newborn care have yet to be defined. Additional work on families’ perspectives on missed nursing care and nursing care quality before, during, and after birth is needed.
Highlights.
Nursing quality measures need to be developed for perinatal care
This cross-sectional survey included 3676 Labor & Delivery RNs from 271 US hospitals
The Perinatal Missed Care Survey is a valid and reliable adaptation of MISSCARE
Missing aspects of care reported by 63–78% of nurses can undermine patient safety
Acknowledgments:
This project was supported by grant number R01 HS025715 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. The authors acknowledge support from the Association of Women’s Health, Obstetric, and Neonatal Nurses (AWHONN) for previous instrument development by the AWHONN Staffing Research Team (Author, PI), and non-financial sponsorship of the present study.
References
- Aiken LH, Sloane DM, Bruyneel L, Van den Heede K, Sermeus W, & Consortium RC (2013). Nurses’ reports of working conditions and hospital quality of care in 12 countries in Europe. International Journal of Nursing Studies, 50(2), 143–153. 10.1016/j.ijnurstu.2012.11.009 [DOI] [PubMed] [Google Scholar]
- Authors (2012). Nurses’ perceptions of critical issues requiring consideration in the development of guidelines for professional registered nurse staffing for perinatal units. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 41(4), 474–482. 10.1111/j.1552-6909.2012.01383.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Authors (2016a). Labor Nurses’ Views of their Influence on Cesarean Birth. MCN: American Journal of Maternal Child Nursing. 10.1097/NMC.0000000000000308 [DOI] [PubMed] [Google Scholar]
- Authors (2016b). Consequences of Inadequate Staffing Include Missed Care, Potential Failure to Rescue, and Job Stress and Dissatisfaction. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 45(4), 481–490. 10.1016/j.jogn.2016.02.011 [DOI] [PubMed] [Google Scholar]
- Authors (2017a). Thematic analysis of US stakeholder views on the influence of labour nurses’ care on birth outcomes. BMJ Quality & Safety, 26(10), 824–831. 10.1136/bmjqs-2016-005859 [DOI] [PubMed] [Google Scholar]
- Authors (2017b). Consequences of Delayed, Unfinished, or Missed Nursing Care During Labor and Birth. Journal of Perinatal and Neonatal Nursing, 31(1), 32–40. 10.1097/JPN.0000000000000203 [DOI] [PubMed] [Google Scholar]
- Authors (2019). Adaptation of the MISSCARE Survey to the Maternity Care Setting. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 48(4), 456–467. 10.1016/j.jogn.2019.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagnasco A, Zanini M, Aleo G, Catania G, Kalisch BJ, & Sasso L (2018). Development and validation of the MISSCARE survey - Pediatric version. Journal of Advanced Nursing, 74(12), 2922–2934. 10.1111/jan.13837 [DOI] [PubMed] [Google Scholar]
- Bohren MA, Hofmeyr GJ, Sakala C, Fukuzawa RK, & Cuthbert A (2017). Continuous support for women during childbirth. Cochrane Database of Systematic Reviews(7). 10.1002/14651858.CD003766.pub6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark RRS, & Lake E (2020). Burnout, job dissatisfaction and missed care among maternity nurses. Journal of Nursing Management, 28(8), 2001–2006. 10.1111/jonm.13037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dabney BW, Kalisch BJ, & Clark M (2019). A revised MISSCARE survey: Results from pilot testing. Applied Nursing Research, 50, 151202. 10.1016/j.apnr.2019.151202 [DOI] [PubMed] [Google Scholar]
- Griffiths P, Recio-Saucedo A, Dall’Ora C, Briggs J, Maruotti A, Meredith P, Smith GB, Ball J, & Missed Care Study G (2018). The association between nurse staffing and omissions in nursing care: A systematic review. Journal of Advanced Nursing, 74(7), 1474–1487. 10.1111/jan.13564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guglielminotti J, Wong CA, Friedman AM, & Li G (2021). Racial and Ethnic Disparities in Death Associated With Severe Maternal Morbidity in the United States: Failure to Rescue. Obstetrics and Gynecology, 137(5), 791–800. 10.1097/AOG.0000000000004362 [DOI] [PubMed] [Google Scholar]
- Hamilton B, Martin J, & Osterman M (2020). Births: Provisional data for 2019. Vital Statistics Rapid Release, 8. https://www.cdc.gov/nchs/data/vsrr/vsrr-8-508.pdf [Google Scholar]
- Hayton JC, Allen DG, & Scarpello V (2004). Factor Retention Decisions in Exploratory Factor Analysis: a Tutorial on Parallel Analysis. Organizational Research Methods, 7(2), 191–205. 10.1177/1094428104263675 [DOI] [Google Scholar]
- Jones TL, Hamilton P, & Murry N (2015). Unfinished nursing care, missed care, and implicitly rationed care: State of the science review. International Journal of Nursing Studies, 52(6), 1121–1137. 10.1016/j.ijnurstu.2015.02.012 [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Landstrom G, & Williams RA (2009). Missed nursing care: errors of omission. Nursing Outlook, 57(1), 3–9. 10.1016/j.outlook.2008.05.007 [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Landstrom GL, & Hinshaw AS (2009). Missed nursing care: a concept analysis. Journal of Advanced Nursing, 65(7), 1509–1517. 10.1111/j.1365-2648.2009.05027.x [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, & Williams RA (2009). Development and psychometric testing of a tool to measure missed nursing care. Journal of Nursing Administration, 39(5), 211–219. 10.1097/NNA.0b013e3181a23cf5 [DOI] [PubMed] [Google Scholar]
- Lake ET, de Cordova PB, Barton S, Singh S, Agosto PD, Ely B, Roberts KE, & Aiken LH (2017). Missed Nursing Care in Pediatrics. Hospital Pediatrics, 7(7), 378–384. 10.1542/hpeds.2016-0141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake ET, French R, O’Rourke K, Sanders J, & Srinivas SK (2019). Linking the work environment to missed nursing care in labour and delivery. Journal of Nursing Management. 10.1111/jonm.12856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lappen JR, Pettker CM, & Louis JM (2021). Society for Maternal-Fetal Medicine Consult Series #54: Assessing the risk of maternal morbidity and mortality. American Journal of Obstetrics and Gynecology, 224(4), B2–B15. 10.1016/j.ajog.2020.12.006 [DOI] [PubMed] [Google Scholar]
- MacDorman MF, & Declercq E (2019). Trends and state variations in out-of-hospital births in the United States, 2004–2017. Birth, 46(2), 279–288. 10.1111/birt.12411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Main EK, Leonard SA, & Menard MK (2020). Association of Maternal Comorbidity With Severe Maternal Morbidity: A Cohort Study of California Mothers Delivering Between 1997 and 2014. Annals of Internal Medicine, 173(11 Suppl), S11–s18. 10.7326/m19-3253 [DOI] [PubMed] [Google Scholar]
- Mandal L, Seethalakshmi A, & Rajendrababu A (2020). Rationing of nursing care, a deviation from holistic nursing: A systematic review. Nursing Philosophy, 21(1), e12257. 10.1111/nup.12257 [DOI] [PubMed] [Google Scholar]
- Martin JA, Hamilton BE, Osterman MJK, & Driscoll AK (2021). Births: Final Data for 2019. National Vital Statistics Reports, 70(2), 1–51. https://www.ncbi.nlm.nih.gov/pubmed/33814033 [PubMed] [Google Scholar]
- Oot A, Huennekens K, Yee L, & Feinglass J (2021). Trends and Risk Markers for Severe Maternal Morbidity and Other Obstetric Complications. Journal of Women’s Health (Larchmt), 30(7), 964–971. 10.1089/jwh.2020.8821 [DOI] [PubMed] [Google Scholar]
- Petersen EE, Davis NL, Goodman D, Cox S, Mayes N, Johnston E, Syverson C, Seed K, Shapiro-Mendoza CK, Callaghan WM, & Barfield W (2019). Vital Signs: Pregnancy-Related Deaths, United States, 2011–2015, and Strategies for Prevention, 13 States, 2013–2017. MMWR: Morbidity and Mortality Weekly Report, 68(18), 423–429. 10.15585/mmwr.mm6818e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Recio-Saucedo A, Dall’Ora C, Maruotti A, Ball J, Briggs J, Meredith P, Redfern OC, Kovacs C, Prytherch D, Smith GB, & Griffiths P (2018). What impact does nursing care left undone have on patient outcomes? Review of the literature. Journal of Clinical Nursing, 27(11–12), 2248–2259. 10.1111/jocn.14058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL (1999). Multiple imputation: a primer. Statistical Methods in Medical Research, 8(1), 3–15. 10.1177/096228029900800102 [DOI] [PubMed] [Google Scholar]
- Smith GB, Redfern O, Maruotti A, Recio-Saucedo A, Griffiths P, & The Missed Care Study, G. (2020). The association between nurse staffing levels and a failure to respond to patients with deranged physiology: A retrospective observational study in the UK. Resuscitation. 10.1016/j.resuscitation.2020.01.001 [DOI] [PubMed] [Google Scholar]
- StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP. [Google Scholar]; Tabachnick BG (2001). Using multivariate statistics. Allyn and Bacon. [Google Scholar]
- Tabachnick BG (2001). Using multivariate statistics. Allyn and Bacon. [Google Scholar]
- Tubbs-Cooley HL, Mara CA, Carle AC, Mark BA, & Pickler RH (2019). Association of Nurse Workload With Missed Nursing Care in the Neonatal Intensive Care Unit. JAMA Pediatrics, 173(1), 44–51. 10.1001/jamapediatrics.2018.3619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tubbs-Cooley HL, Pickler RH, & Meinzen-Derr JK (2015). Missed oral feeding opportunities and preterm infants’ time to achieve full oral feedings and neonatal intensive care unit discharge. American Journal of Perinatology, 32(1), 1–8. 10.1055/s-0034-1372426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tubbs-Cooley HL, Pickler RH, Younger JB, & Mark BA (2015). A descriptive study of nurse-reported missed care in neonatal intensive care units. Journal of Advanced Nursing, 71(4), 813–824. 10.1111/jan.12578 [DOI] [PubMed] [Google Scholar]
- Van der Gucht N, & Lewis K (2015). Women’s experiences of coping with pain during childbirth: A critical review of qualitative research. Midwifery, 31(3), 349–358. 10.1016/j.midw.2014.12.005 [DOI] [PubMed] [Google Scholar]
- VanFosson CA, Jones TL, & Yoder LH (2016). Unfinished nursing care: An important performance measure for nursing care systems. Nursing Outlook, 64(2), 124–136. 10.1016/j.outlook.2015.12.010 [DOI] [PubMed] [Google Scholar]


