Abstract
Background
Remimazolam tosilate (RT) is a new type of γ-aminobutyric acid subtype A (GABAA) receptor agonist, having the possibility to be an ideal sedative drug for procedural sedation. At present, there are few studies on the effect of RT on respiratory depression in elderly patients. We aimed to evaluate the effect of RT on respiratory depression in elderly patients undergoing gastroscopy.
Methods
This prospective, randomized, single-blinded trial recruited patients from eight centers in China between May 2022 and July 2022. A total of 346 elderly patients undergoing gastroscopy were randomly divided into RT group (0.2 mg/kg) or propofol group (1.5 mg/kg), respectively. The primary outcome was the incidence of respiratory depression. Secondary outcomes include the incidence of sedative-related adverse events, the success rate of sedation, time to fully alert, time to loss of consciousness (LOC), time to ready for discharge, as well as the the patients, endoscopists and anethetists’ satisfaction.
Results
The incidence of respiratory depression was significantly reduced in the RT group compared with the propofol group (9.8% vs 17.9%, P=0.042). The time of LOC and fully alert in the RT group were longer than that in the propofol group (P < 0.05). The incidences of hypotention (50.9% vs 32.4%, P=0.001) and hypotension requiring treatment (5.8% vs 1.7%, P=0.031) were significantly higher in the propofol group than that in the RT group. The incidence and severity of injection pain were more frequently recorded in the propofol group than that in the RT group (40.5% vs 12.1%, P<0.05). There were no statistically significant differences between the two groups in terms of sedation success rates, time to ready for discharge, endoscopists and anethetists’ satisfaction and other sedative-related adverse events.
Conclusion
RT may be a suitable alternative sedative agent for elderly patients undergoing gastroscopy due to its safety profile.
Keywords: Remimazolam tosilate, propofol, elderly patients, gastroscopy
Introduction
Gastroscopy is one of the important means for diagnosis and treatment of upper gastrointestinal diseases. With the aging of the population and the development of digestive endoscopy technology, the number of elderly patients undergoing gastroscopy is increasing year by year.1 Although it is a non-invasive procedure, it usually causes obvious discomfort in the majority of patients, including nausea, vomiting, anxiety or pain.2 Procedural sedation during gastroscopy not only alleviates patients’ anxiety, pain and discomfort but also provides a comfortable environment for endoscopists throughout the procedure. Despite procedural sedation is generally considered safe in most patients, elderly patients undergoing procedural sedation are associated with higher risk of hemodynamic instability, respiratory depression, and delayed discharge time, especially in those with cardiopulmonary disease conditions.3,4 Therefore, it is very important for elderly patients to choose safe and effective anesthetics during gastroscopy. The ideal agent for gastroscopy should be effective in the whole process, with characteristics of rapid onset and elimination, mild respiratory and circulatory depression and less side effects. Propofol has become the most commonly used intravenous sedative agent for sedation during gastrointestinal endoscopy due to its excellent sedative properties and rapid onset profile.5 However, propofol may result in cardiovascular and respiratory depression, hypoxia or aspiration pneumonia, especially in elderly patients,6,7 which limits its application in the elderly patients undergoing gastroscopy to some extent. Consequently, an anesthetic with characteristics of mild respiratory and circulatory inhibition, rapid onset and elimination seems to be urgently needed.
Remimazolam tosilate (RT) is a new type of ultra-shorting γ-aminobutyric acid subtype A (GABAA) receptor agonist,8 a growing number studies have shown that remimazolam has the characteristics of mild respiratory depression, stable hemodynamics, rapid onset and elimination,9–11 indicating that RT may be a potential safe agent for elderly patients undergoing gastroscopy. A recent multicenter study demonstrated that RT was superior to propofol in non-elderly patients undergoing upper gastrointestinal endoscopy.12 Considering the advantages of RT as mentioned above, RT has the possibility of being a better choice during procedure sedation for elderly patients. Currently, there are few studies on the effect of RT on respiratory depression in elderly patients during a gastroscopy procedure. To the best of our knowledge, this is the first study comparing RT and propofol on respiratory depression in elderly patients during a gastroscopy procedure. Thus, the aim of the study is to compare the effect of RT and propofol on respiratory depression in elderly patients undergoing a gastroscopy procedure. This study will provide new clinical practice for evaluating the efficacy and safety of RT in elderly patients undergoing gastroscopy procedures.
Methods
Study Design
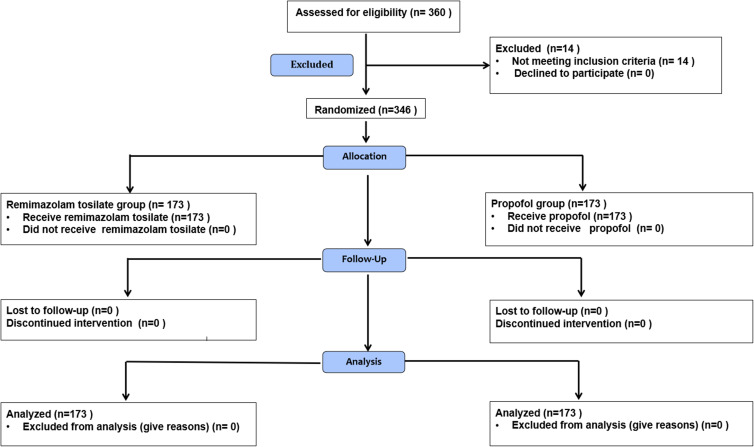
This study was a prospective, multicentered, randomized, single-blind, controlled trial comparing RT with propofol for sedation in elderly patients undergoing gastroscopy. Patients were recruited from eight centers in China between May 2022 and July 2022. The study has been approved by the Biological Medical Ethical Committee of the Affiliated Hospital of Guizhou Medical University and registered in the Chinese Clinical Trial Registry (ChiCTR2200059332). The present study was performed according to the principles of the Declaration of Helsinki. Written informed consent was obtained from all patients before the procedures. The flowchart detailing the study design is illustrated in Figure 1.
Figure 1.
Consort flow diagram of the trial design.
Patient Eligibility
Patients aged ≥65 years, American Society of Anesthesiologists (ASA) grade I–III, body mass index (BMI) between 18 and 30 kg/m2, who were scheduled for elective gastroscopy with sedation anesthesia were recruited in this study. Exclusion criteria included the following: patients had severe cardiorespiratory instability (acute heart failure, myocardial infarction, obstructive sleep apnea syndrome, acute respiratory infection, etc); required tracheal intubation (including laryngeal mask); had a history of renal or hepatic dysfunction; had neurological diseases (schizophrenia, mania, bipolar disorder, cognitive dysfunction, etc); known allergic or contraindicated to benzodiazepines, opioids, propofol, egg products or soybeans; had a history of alcohol abuse or addicted to opioids or sedative hypnotic drugs; inability to complete the survey; Patients with expected difficult airway were also excluded.
Randomization and Blinding
Randomization was performed centrally by our hospital research department with allocation concealed based on eight permuted blocks with block sizes of 60 for covering the total sample size. All selected patients were randomly divided into the RT group and propofol group using a computer-generated random number prior to gastroscopy. Opaque envelopes were made according to the randomization sequence and opened by a nurse who was blinded to the trial after patient’s arrival to the operation room. We applied the single-blind design due to different appearance of the two drugs. The endoscopists, nurses, patients and investigators were blinded to the group assignment. The randomization sequence was retained in an opaque envelope by a nurse.
Procedures
All eligible patients were fasted routinely before procedures. Routine monitoring including electrocardiography (ECG), non-invasive blood pressure (NIBP) and peripheral oxygen saturation (SpO2) were performed. Ringer lactate (5 mL/kg) was infused via a 20-gauge peripheral intravenous catheter. The average of the three vital signs of the patient at rest was recorded as the baseline data. Patients were provided oxygen (4 L/min) via a nasal cannula before induction until they were fully alert. After preoxygenation, all patients received 0.1 µg/kg sufentanil for analgesia prior to gastroscopy. Two minutes later, patients in the RT group received a dose of 0.2 mg/kg RT for induction (intravenous injection slowly over 1 minute), while patients in the propofol group received a dose of 1.5 mg/kg propofol (intravenous injection slowly over 1 minute). During the whole process, sedation level was evaluated using the Modified Observer Alert/Sedation Assessment (MOAA/S) score.13 The sedation level was evaluated every 30 seconds for the first 3 minutes, and then every 1 minute until the patient was fully awake (MOAA/S scores of 5 for three consecutive times).12,14 Gastroscopy was performed when the patient was sufficiently sedated (MOAA/S ≤3).14 If patients were deemed to be inadequate sedation (MOAA/S >3) after the initial dose, a supplemental bolus (one-third of the initial dose) of RT or propofol was added. The additional dose was one-third of the initial dose, and was allowed to add up to five times within 15 minutes. If the initial and additional doses were not enough to obtain a satisfactory sedation level for procedure within 15 minutes, propofol would be given as a rescue sedative agent.
If the patient suffers from hypoxia or respiratory depression for more than 10 seconds, the following treatment measures will be taken: a) increase the inhaled oxygen flow; b) open the patient’s airway by thrusting the jaw or lifting the chin, or stretching the head; c) if the oxygen saturation does not improve, stop the gastroscopy and slightly squeeze the patient’s chest or abdomen; d) if the condition is still not improved, conduct face mask ventilation. If the above measures are not successful, endotracheal intubation shall be carried out.
Outcomes
The primary outcome was the incidence of respiratory depression, which defined as respiratory rate <8/min and/or oxygen saturation <90% lasted more than 10 seconds from drug administration to fully alert. Secondary outcomes included the following: 1) the sedation success rate, which defined as a) completion of the entire endoscopy procedure; b) no need for rescue sedative medication; and c) up to five additional doses within 15 minutes after the initial dose; 2) time to loss of consciousness (LOC), defined as the time from the initial dose to obtain sufficient sedation [the first MOAA/S score≤3]; 3) time to fully alert, defined as the time from cessation of sedative agent to fully alert [the first of three consecutive MOAA/S score of 5]; 4) time to ready for discharge [modified post-anesthesia discharge scoring system score of ≥9, with 2 points in the vital sign item]; 5) the incidence of hypotension (defined as systolic blood pressure [SBP] decreased by 20% or more than the baseline value or SBP ≤80 mmHg) from drug administration to fully alert; 6) the incidence of treatment-related hypotension (defined as hypotension occurring during sedation and requiring at least one medication); 7) the incidence of adverse events, including but not limited to apnea [absence of breathing lasting 10 seconds or more]; the abnormal SpO2 during gastroscopy; postoperative nausea and vomiting (PONV); body movement, bradycardia [defined as heart rate less than 50 beat/min], tachycardia [defined as heart rate greater than 120 beat/min], incidence and severity of injection pain,15 etc; 8) The satisfaction of anesthesiologists, doctors and patients were evaluated using a 10-point scale, which was divided into the following categories: poor, 1–4; Fairness, 5–7; Good, 8–10.2
Statistical Analysis
Sample size was calculated based on the incidence of respiratory depression. In our pilot study (unpublished), the incidence of respiratory depression in RT group and propofol group were 4.9% and 16.84%, respectively. Based on our pilot data, assuming a αlevel of 0.05 and a power of 0.90, 138 patients per group were required in our study. Considering the dropout rate was approximately 20%, we finally included 173 patients in each group.
SPSS 22.0 software (SPSS Inc, Chicago, IL, USA) was used to analyze the data. The Shapiro–Wilk test was used to test the normality of the data distribution. Data with normal distribution were presented as mean±standard deviation and compared by independent Student t-test; Data with abnormal distribution were presented as median (25th and 75th percentile) and compared using Wilcoxon signed-rank test. Categorical data were expressed as n (%) and compared using a Fisher’s exact test or Chi square test. A p value <0.05 was considered statistically significant.
Results
Patient Characteristics and Baseline Information
A total of 360 patients were recruited for study participation. Among them, three patients required trachea intubation; three patients had expected difficult airways; six patients had hemodynamic instability; and two patients had a history of sleep apnea. As a result, 346 patients were finally analyzed, as shown in Figure 1. Patients’ demographics and baseline characteristics are summarized in Table 1. There was no significant difference between the RT group and propofol group in terms of age, sex, BMI, ASA classification, procedure time, baseline SpO2, sufentanil doses, comorbidities and infusion volume (P > 0.05; Table 1).
Table 1.
Demographic and Baseline Characteristics of Patients
| Variable | Propofol Group (n=173) | RT Group (n=173) | P-value |
|---|---|---|---|
| Age (years) | 69.92±7.57 | 70.11±7.37 | 0.818 |
| Gender (male/female) | 72/101 | 69/104 | 0.743 |
| Height (cm) | 158.40±14.21 | 158.97±7.62 | 0.640 |
| Weight (kg) | 57.92±10.51 | 57.09±10.00 | 0.451 |
| BMI (kg/m2) | 22.73±3.23 | 22.75±3.15 | 0.936 |
| ASA (I/II/III) | 26/140/7 | 20/144/9 | 0.580 |
| Baseline SpO2 (%) | 98(97, 99) | 98(97, 98) | 1.000 |
| Infusion volume (mL) | 255.95±144.17 | 235.58±139.31 | 0.214 |
| Procedure times (min) | 6(4, 8) | 6(4, 8) | 0.316 |
| Sufentanil dose (µg) | 5.76±1.00 | 5.64±0.91 | 0.281 |
| Comorbidity | 0.994 | ||
| Hypertension | 53(39.8%) | 65(37.6%) | |
| Diabetes | 25(14.5%) | 30(17.3%) | |
| CHD | 7(4.0%) | 9(5.2%) | |
| COPD | 17(9.8%) | 19(20.0%) |
Notes: Variables presented as mean ±SD, median (interquartile range) or number of patients(%).
Abbreviations: RT, remimazolam tosilate; BMI, body mass index; ASA, American Society of Anaesthesiologists; CHD, coronary heart disease; COPD, chronic obstructive pulmonary disease.
Primary Outcome
The incidence of respiratory depression in the RT group was significantly lower compared with the propofol group (9.8% vs 17.9%, P=0.042). Similarly, the respiratory depression rate in patients with 18 BMI≤24 kg/m2was also lower than that in the propofol group (4.0% vs 9.2%, P=0.046), while the respiratory depression rate in patients with 24<BMI<30 kg/m2 was comparable between the two groups. Compared with the propofol group, the number of patients with oxygen saturation of 75–89% (11.6% vs 1.7%, P=0.000) as well as oxygen saturation less than 75% (0.0% vs 4.0%, P=0.015) in the RT group were significantly reduced. In addition, compared with the propofol group, the number of using airway opening maneuvers (5.2% vs 14.5%, respectively, P=0.004) as well as face mask ventilation (1.2% vs 5.8%, respectively, P = 0.019) to correct hypoxia were reduced in the RT group. None of the patients required endotracheal intubation or laryngeal mask for mechanical ventilation (Table 2).
Table 2.
Respiratory Depression and Interventions Related to Hypoxemia Between the Two Groups
| Variable | Propofol Group (n=173) | RT Group (n=173) | P-value |
|---|---|---|---|
| Total respiratory depression | 31(17.9%) | 17(9.8%) | 0.042* |
| Respiratory depression in patients with 18<BMI≤24 kg/m2 | 16(9.2%) | 7(4.0%) | 0.046* |
| Respiratory depression in patients with 24<BMI<30 kg/m2 | 15(8.7%) | 10(5.8%) | 0.505 |
| SpO2 75–89% | 20(11.6%) | 3(1.7%) | 0.000* |
| SpO2<75% | 7(4.0%) | 0(0.0%) | 0.015* |
| Airway opening maneuvers | 25(14.5%) | 9(5.2%) | 0.006* |
| Facemask ventilation | 10(5.8%) | 2(1.2%) | 0.035* |
Notes: Variables presented as number of patients(%). *P < 0.05 vs RT group.
Abbreviations: SpO2, peripheral oxygen saturation; BMI, body mass index.
Secondary Outcomes
Sedation Effectiveness Outcomes
The time to LOC (20.7 ± 6.1 vs 13.2 ± 5.2 s) as well as the time to be fully alert (15.06±4.06 s vs 13.79±4.22 s) in the RT group were longer compared with the propofol group (P < 0.05; Table 3). However, the sedation success rate and the time to ready for discharge were found no significant differences between the two groups (Table 3).
Table 3.
Comparison of Sedative Effectiveness Between Two Groups
| Variable | Propofol Group (n=173) | RT Group (n=173) | P-value |
|---|---|---|---|
| Sedation success | 173(100%) | 172(99.4%) | 1.000 |
| Time to loss of consciousness (s) | 65(50–80) | 70(58–92) | 0.020* |
| Time to fully alert (min) | 13.75±4.22 | 15.09±4.06 | 0.003* |
| Time to hospital discharge (min) | 19.55±7.60 | 19.92±6.34 | 0.623 |
Notes: Variables presented as mean ±SD, median (interquartile range) or number of patients(%). *P < 0.05 vs RT group.
Adverse Events Outcomes
The incidences of hypotention (50.9% vs 32.4%, P=0.001) and hypotension requiring treatment (5.8% vs 1.7%, P=0.031) were significant higher in the propofol group than that in the RT group (Table 4). The incidence and severity of injection pain were more frequently recorded in the propofol group than that in the RT group (40.5% vs 12.1%, P<0.05; Table 4). There were no significant differences in terms of apnea, body movement, hypertension, PONV between the two groups (P>0.05; Table 4). The endoscopists, anesthetists and patients’ satisfaction were comparable between the two groups (Table 5).
Table 4.
Comparison of Adverse Events Between the Two Groups
| Variable | Propofol Group (n=173) | RT Group (n=173) | P-value |
|---|---|---|---|
| Injection pain (0/1/2/3) | 103/40/22/8 | 152/17/3/1 | <0.001* |
| Hypotension | 88(50.9%) | 56(32.4%) | 0.001* |
| Incidence of hypotension required treatment | 10(5.8%) | 3(1.7%) | 0.048* |
| Apnea | 3(1.7%) | 1(0.6%) | 0.623 |
| Hypertension | 2(1.2%) | 5(2.9%) | 0.448 |
| Body movement | 11(6.6%) | 20(11.6%) | 0.131 |
| PONV | 0(0.0%) | 1(0.6%) | 1.000 |
| Bradycardia | 3(1.7%) | 3(1.7%) | 1.000 |
| Tachycardia | 0(0.0%) | 0(0.0%) | 1.000 |
Notes: Variables presented as number of patients(%). *P < 0.05 vs RT group.
Abbreviation: PONV, postoperative nausea and vomiting.
Table 5.
Satisfactions of Physicians, Anesthetists and Patients Between the Two Groups
| Variable | Propofol Group (n=173) | RT Group (n=173) | ||||
|---|---|---|---|---|---|---|
| Good | Fair | Poor | Good | Fair | Poor | |
| Endoscopists | 158(91.3%) | 14(8.1%) | 1(0.6%) | 156(90.2%) | 14(8.1%) | 3(1.7%) |
| Anesthetists | 151(87.3%) | 19(11.0%) | 3(1.7%) | 159(91.9%) | 14(8.1%) | 0(0.0%) |
| Patients | 171(98.8%) | 2(1.2%) | 0(0.0%) | 170(98.3%) | 3(1.7%) | 0(0.0%) |
Notes: Data presented as mean ±SD, median (interquartile range) or number of patients(%).
Discussion
Our study aimed to evaluate the effect of RT and propofol on respiratory depression in elderly patients undergoing gastroscopy procedure. In our study, we found that the incidence of respiratory depression in the RT group was reduced compared with the propofol group. The incidence of sedative-related adverse events, including hypotention and injection pain, were also significant reduced in the RT group. Nevertheless, the time of LOC and the time to be fully alert in the RT group were slighter longer when compared with the propofol group. The sedation success rate, the time of ready for discharge and the patients’ satisfaction were found no significant differences between the two groups.
Since endoscopic procedures not only cause the patients anxiety, pain and discomfort but also decrease patients’ satisfaction and acceptance, sedated endoscopy has been widely used in the past decade.16,17 Propofol has been recommended by guidelines for procedural sedation due to its favorable pharmacokinetic characteristics such as rapid induction and short recovery time.18 However, respiratory depression and hypoxemia caused by propofol sedation during endoscopic procedures are particularly prominent in elderly patients.19,20 Although the respiratory depression and hypoxia caused by propofol are usually temporary, it may cause serious complications for elderly patients with poor cardiopulmonary function reserve.
RT, a new ultra-short type of GABAA receptor agonist, has been widely used in procedural sedation and general anesthesia due to its promising properties, including a rapid onset, short recovery time and stable hemodynamics.21,22 Liu et al compared the efficacy and safety between RT (0.15mg/kg) and etomidate-propofol (EP) in elderly patients undergoing colonoscopy and found that the sedation success rate was comparable between RT group and EP group, while the adverse events (myoclonus and injection pain) were recorded more frequently in the EP group.14 Similarly, Guo et al compared the use of RT (0.15mg/kg) and propofol in elderly patients undergoing gastroscopy and also demonstrated that the success rate of sedation in both RT group and propofol group was 100%, while the incidence of sedation-related side effects was reduced in the RT group.23 These studies showed that RT could be effectively used for elderly patients during procedural sedation. Despite this, both the above studies focus on the sedation success rate of RT in elderly patients, rather than on the effect of RT on respiratory depression. In addition, the sample size of these studies is relatively small and the conclusions are inconsistent. There is still uncertainty as to whether RT causes less respiratory depression than propofol, and studies with large sample are needed to address this issue.
In our study, the incidence of respiratory depression in the RT group was significantly lower compared with the propofol group. In addition, RT improved the oxygen saturation and reduced the frequency of airway opening maneuvers and face mask ventilation. These results further support that RT has potential advantages than propofol in preventing respiratory depression and hypoxia during sedative endoscopy. Previous study has reported that respiratory depression caused by propofol was closely related to the dosage and injection speed of propofol, as well as the sedation levels.24 In this study, we administered both the propofol and RT over a 1-minute period in order to avoid the injection of drugs too fast. In addition, the dose of propofol (1.5mg/kg) we selected in this study was similar to previous study,23 which was relatively appropriate for the elderly patients. Furthermore, unlike other studies maintained a deeper sedation level (MOSS/S≤1),25 the sedation level in our study was kept at the moderate-to-severe sedation level (MOSS/S ≤3) during the whole process, which could largely avoid the occurrence of deep sedation and sedative-related adverse events. Nevertheless, we did not monitor the difference of sedation level of all patients by bispectral index (BIS), which may be partially attributed to the difference in the incidence of respiratory depression.
Our investigation demonstrated that the incidences of hypotension and hypotension required treatment during sedation were both reduced in the RT group, which may be related to the following reason. Propofol has been reported to enhance parasympathetic innervation, leading to decreased heart rate and blood pressure.26,27 While RT is similar to other benzodiazepines drugs, which may stimulate sympathetic activity and avoid inhibition of cardiopulmonary function. Moreover, similar to past study,12 injection pain was significantly higher in the propofol group. As the structure of RT is different from the phenol structure of propofol, RT may have less stimulation on blood vessels.
Comparable with the previous study,12 our study revealed that RT could provide adequate sedation for elderly patients who underwent gastroscopy, which the sedation success rate was comparable with propofol (99.4% vs 100%). A previous study reported that the ED95 dose of remimazolam-induced LOC in ASA class III patients was 0.16 mg/kg.23 In our study, the dose of RT (0.2 mg/kg) was sufficient to produce adequate sedation with fewer adverse reactions in elderly patients when compared with propofol, indicating that the sedative dose range of RT is relatively wide.
Consistent with previous findings,28 our study showed that the time to LOC was slightly longer in the RT group (65 [50–80] vs 70 [58–92], P=0.020) than that in the propofol group. However, this difference does not exist much clinical significance. In contrast to the results of Chen et al,12 our results showed that the time to full alert in the RT group was relatively longer compared with the propofol group. This may be related to the fact that the dose of RT selected (0.2mg/kg) was slightly larger than that of Chen et al (0.15mg/kg). However, the time to ready for discharge was found no significant difference between the two groups, suggesting that RT has no accumulation effect in body.
However, there are several limitations in our study. First, this study is only a single-blinded trial, which may lead to observational bias. Second, the subjects of this study were elderly patients with a normal BMI. Therefore, our findings are not applicable for obese patients. Third, we did not compare the effect of different doses of RT on respiratory depression, and further studies are required to determine the optimal dose of RT for the less respiratory depressant in elderly patients. Finally, we did not monitor and compare sedation depth of all patients by specific equipment (eg, BIS, Narcotrend). Further clinical trials are needed to solve the above problems.
Strengths and Limitations of This Study
The trial is a multicentered, prospective, single-blinded, randomized, controlled trial to compare the effect of RT and propofol on respiratory depression in elderly patients undergoing gastroscopy.
Our study suggests that RT has potential advantages than propofol in reducing respiratory depression in elderly patients during procedural sedation.
This study will provide new clinical practice for evaluating the efficacy and safety of RT in the elderly patients undergoing gastroscopy procedure.
The main limitation of this study is that the participants are mainly elderly patients with a normal BMI (body mass index). Thus, our findings are not applicable for patients with an abnormal BMI.
Conclusions
Compared with propofol, the incidence of respiratory depression and other sedation-related adverse events caused by RT are significantly lower. RT may be a suitable alternative sedative agent for elderly patients undergoing gastroscopy due to its non-inferior efficacy and higher safety profile.
Funding Statement
This work was supported in part by grants from the Beijing Hongyi Medical Development Foundation (HY20210037-A-07), the Fund of Yunyan District Science and Technology department (yunkehezi[2021]10), Natural Science Foundation of China (No. 82160951, 82162024), the Science and Technology Fund of Guizhou Provincial Health Department (qiankehepingtairencai[2018]5779-52), the Fund of Guizhou Provincial Natural Science Foundation (qiankehejichu[2020]1Y298), the Cultivate project 2021 for National Natural Science Foundation of China, Affiliated Hospital of Guizhou Medical University (gyfynsfc-2021-35), the Fund of Guiyang Science and Technology department ([2019]9-1-24), the Health and Family Planning Commission of Guizhou Province (gzwkj2021-273), the Fund of Guizhou Provincial Education Department (qianjiaoheKYzi[2021]182).
Abbreviations
RT, remimazolam tosilate; GABAA, γ-aminobutyric acid subtype A; ASA, American Society of Anesthesiologists; BMI, body mass index; NIBP, noninvasive blood pressure; ECG, electrocardiogram; HR, heart rate; SpO2, peripheral oxygen saturation; BIS, bispectral index; MOAA/S, Modified Observer’s Assessment of Alertness/Sedation; ED95, 95% effective dose; LOC, loss of consciousness; SBP, systolic blood pressure; PONV, postoperative nausea and vomiting.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are not publicly available due to the privacy policy but are available from the corresponding authors on reasonable requests.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests.
References
- 1.Meng QT, Cao C, Liu HM, et al. Safety and efficacy of etomidate and propofol anesthesia in elderly patients undergoing gastroscopy: a double-blind randomized clinical study. Exp Ther Med. 2016;12:1515–1524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shen XC, Ao X, Cao Y, et al. Etomidate-remifentanil is more suitable for monitored anesthesia care during gastroscopy in older patients than propofol-remifentanil. Med Sci Monit. 2015;21:1–8. doi: 10.12659/MSM.891183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goudra B, Nuzat A, Singh PM, et al. Association between type of sedation and the adverse events associated with gastrointestinal endoscopy: an analysis of 5 years’ data from a tertiary center in the USA. Clin Endosc. 2017;50(2):161–169. doi: 10.5946/ce.2016.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ruiz-Curiel RE, Bonilla HY, Baptista A, Bronstein M. Sedation with propofol in digestive endoscopy administered by gastroenterologists. Experience in a Venezuelan hospital. Rev Esp Enferm Dig. 2018;110:246–249. doi: 10.17235/reed.2018.5185/2017 [DOI] [PubMed] [Google Scholar]
- 5.Olofsen E, Boom M, Nieuwenhuijs D, et al. Modeling the non-steady state respiratory effects of remifentanil in awake and propofol-sedated healthy volunteers. Anesthesiology. 2010;112:1382–1395. doi: 10.1097/ALN.0b013e3181d69087 [DOI] [PubMed] [Google Scholar]
- 6.Choi GJ, Kang H, Baek CW, Jung YH, Ko JS. Etomidate versus propofol sedation for electrical external cardioversion: a meta-analysis. Curr Med Res Opin. 2018;34(11):2023–2029. doi: 10.1080/03007995.2018.1519501 [DOI] [PubMed] [Google Scholar]
- 7.Wernli KJ, Brenner AT, Rutter CM, Inadomi JM. Risks associated with anesthesia services during colonoscopy. Gastroenterology. 2016;150(4):888–894, e18. doi: 10.1053/j.gastro.2015.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Keam SJ. Remimazolam: first approval. Drugs. 2020;80(6):625–633. doi: 10.1007/s40265-020-01299-8 [DOI] [PubMed] [Google Scholar]
- 9.Chen S, Wang J, Xu X, et al. The efficacy and safety of remimazolam tosylate versus propofol in patients undergoing colonoscopy: a multicentered, randomized, positive-controlled, Phase III clinical trial. Am J Transl Res. 2020;12:4594–4603. [PMC free article] [PubMed] [Google Scholar]
- 10.Sneyd JR, Gambus PL, Rigby-Jones AE. Current status of perioperative hypnotics, role of benzodiazepines, and the case for remimazolam: a narrative review. Br J Anaesth. 2021;127(1):41–55. doi: 10.1016/j.bja.2021.03.028 [DOI] [PubMed] [Google Scholar]
- 11.Chen X, Sang N, Song K, et al. Psychomotor recovery following remimazolam-induced sedation and the effectiveness of flumazenil as an antidote. Clin Ther. 2020;42(4):614–624. doi: 10.1016/j.clinthera.2020.02.006 [DOI] [PubMed] [Google Scholar]
- 12.Chen SH, Yuan TM, Zhang J, et al. Remimazolam tosilate in upper gastrointestinal endoscopy: a multicenter, randomized, non-inferiority, phase III trial. J Gastroenterol Hepatol. 2021;36:474–481. doi: 10.1111/jgh.15188 [DOI] [PubMed] [Google Scholar]
- 13.Chernik DA, Gillings D, Laine H, et al. Validity and reliability of the observer’s assessment of alertness/sedation scale: study with intravenous midazolam. J Clin Psychopharmacol. 1990;10:244–251. [PubMed] [Google Scholar]
- 14.Liu X, Ding B, Shi F, et al. The efficacy and safety of remimazolam tosilate versus etomidate-propofol in elderly outpatients undergoing colonoscopy: a prospective, randomized, single-blind, non-inferiority trial. Drug Des Devel Ther. 2021;15:4675–4685. doi: 10.2147/DDDT.S339535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Guan X, Jiao Z, Gong X, et al. Efficacy of pre-treatment with remimazolam on prevention of propofol-induced injection pain in patients undergoing abortion or curettage: a prospective, double-blinded, randomized and placebo-controlled clinical trial. Drug Des Devel Ther. 2021;15:4551–4558. doi: 10.2147/DDDT.S334100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chung JW, Kim N, Wee JH, et al. Clinical features of snoring patients during sedative endoscopy. Korean J Intern Med. 2019;34(2):305–314. doi: 10.3904/kjim.2017.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim DK. Nonoperating room anaesthesia for elderly patients. Curr Opin Anaesthesiol. 2020;33(4):589–593. doi: 10.1097/ACO.0000000000000883 [DOI] [PubMed] [Google Scholar]
- 18.Riphaus A, Wehrmann T, Hausmann J, et al. Update S3-guideline: “sedation for gastrointestinal endoscopy” 2014 (AWMF-register-no. 021/014). Z Gastroenterol. 2016;54:58–95. doi: 10.1055/s-0041-109680 [DOI] [PubMed] [Google Scholar]
- 19.Shao LJ, Zou Y, Liu FK, et al. Comparison of two supplemental oxygen methods during gastroscopy with propofol mono-sedation in patients with a normal body mass index. World J Gastroenterol. 2020;26:6867–6879. doi: 10.3748/wjg.v26.i43.6867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gouda B, Gouda G, Borle A, et al. Safety of non-anesthesia provider administered propofol sedation in non-advanced gastrointestinal endoscopic procedures: a meta-analysis. Saudi J Gastroenterol. 2017;23(3):133–143. doi: 10.4103/sjg.SJG_501_16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Antonik LJ, Goldwater DR, Kilpatrick GJ, Tilbrook GS, Borkett KM. A placebo- and midazolam-controlled Phase I single ascending-dose study evaluating the safety, pharmacokinetics, and pharmacodynamics of remimazolam (CNS 7056): part I. Safety, efficacy, and basic pharmacokinetics. Anesth Analg. 2012;115(2):274–283. doi: 10.1213/ANE.0b013e31823f0c28 [DOI] [PubMed] [Google Scholar]
- 22.Sheng XY, Liang Y, Yang XY, et al. Safety, pharmacokinetic and pharmacodynamic properties of single ascending dose and continuous infusion of remimazolam besylate in healthy Chinese volunteers. Eur J Clin Pharmacol. 2020;76:383–391. doi: 10.1007/s00228-019-02800-3 [DOI] [PubMed] [Google Scholar]
- 23.Guo J, Qian Y, Zhang X, et al. Remimazolam tosilate compared with propofol for gastrointestinal endoscopy in elderly patients: a prospective, randomized and controlled study. BMC Anesthesiol. 2022;22(1):180. doi: 10.1186/s12871-022-01713-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shimizu H, Homma Y, Norii T. Incidence of adverse events among elderly vs non-elderly patients during procedural sedation and analgesia with propofol. Am J Emerg Med. 2021;44:411–414. doi: 10.1016/j.ajem.2020.04.094 [DOI] [PubMed] [Google Scholar]
- 25.Ki S, Cho Y, Choi Y, et al. Effect of chemotherapy on effect-site concentration of propofol for loss of consciousness in patients with colorectal cancer. Korean J Anesthesiol. 2022;75(2):160–167. doi: 10.4097/kja.21327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Amornyotin S. Sedation-related complications in gastrointestinal endoscopy. World J Gastrointest Endosc. 2013;5:527–533. doi: 10.4253/wjge.v5.i11.527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Win NN, Fukayama H, Kohase H, Umino M. The different effects of intravenous propofol and midazolam sedation on hemodynamic and heart rate variability. Anesth Analg. 2005;101(1):97–102. doi: 10.1213/01.ANE.0000156204.89879.5C [DOI] [PubMed] [Google Scholar]
- 28.Cao Y, Chi P, Zhou C, et al. Remimazolam tosilate sedation with adjuvant sufentanil in Chinese patients with liver cirrhosis undergoing gastroscopy: a randomized controlled study. Med Sci Monit. 2022;28:e936580. doi: 10.12659/MSM.936580 [DOI] [PMC free article] [PubMed] [Google Scholar]