Abstract
Although researchers have explored the link between depression and executive functioning (EF), the influence of early-life environmental and relational instability on this association has not been comprehensively assessed in adolescents. This cross-sectional study examined whether unpredictability of home environment in childhood moderated the relationship between depression and EF in adolescents. Participants were 138 adolescents aged 13 to 17 years (72% female; 47.8% White; 47.1% Hispanic). Diagnostic status (major depression versus healthy control) and depression severity were assessed using psycho-diagnostic interviews and self-reports from parents and adolescents. Participants also completed the Questionnaire of Unpredictability in Childhood (QUIC). EF was assessed using self-report (Behavior Rating Inventory of Executive Function, Second Edition; BRIEF2) and a battery of performance-based measures. Results showed that QUIC scores moderated the relationship between depression and BRIEF2 scores, such that high unpredictability was associated with poorer EF for adolescents exhibiting low depression severity. Participants with the highest levels of depression exhibited the poorest EF ratings, regardless of childhood unpredictability. Unpredictability was moderately associated with performance-based measures, but did not interact with depressive symptoms to predict complex performance-based EF. Recommendations include assessing for unpredictable childhood environment and acknowledging this risk factor for poor EF in youth with sub-threshold depression. Treatment implications are discussed with respect to family systems/parenting interventions, as mildly depressed adolescents growing up in unstable homes may be vulnerable to EF difficulties. Further, this study adds to the EF measurement literature by examining associations between self-report and performance-based EF instruments in a diverse sample of adolescents.
Keywords: childhood unpredictability, parenting, depression, executive functioning, adolescence
Extant research has explored the various factors impacting cognitive development in children and adolescents, including psychological determinants (e.g., depression), early-life influences (e.g., parenting practices), and environmental variables (e.g., socioeconomic status, chaos in the home). However, the majority of studies examining these constructs focus on young children, and none have comprehensively analyzed the relationships among depression, childhood unpredictability, and executive functioning (EF) during the vulnerable developmental period of adolescence. The present study adopts a bioecological framework to understand these complex processes, as EF has primarily been examined within biological models, which can overlook important ecological and interpersonal influences (Hughes & Ensor, 2009).
Executive Functioning and Depression
According to bioecological theory (Bronfenbrenner & Evans, 2000), cognitive processes develop in the context of proximal factors (e.g., relationships with parents, peers, and teachers) that interact with each other over time. EF, specifically, develops across childhood and adolescence and broadly captures cognitive control comprising higher-order self-regulation processes, including problem-solving, decision-making, planning, self-regulation, inhibition, cognitive flexibility, shifting, and working memory, which are managed by the prefrontal cortex (Anderson et al., 2002; Karbach & Unger, 2014). In adolescence, a period of growing independence whereby one’s behaviors have more lasting consequences, EF continues to evolve and is implicated in every-day management of emotions and behaviors, goal-setting, maintenance of relationships, and basic processing of information and attentional control (Diamond, 2013; Lezak, 2004).
This is also a period of great vulnerability whereby major depressive disorder (MDD) emerges as one of the most common mental illnesses diagnosed in adolescence (Merikangas et al., 2010). Meta-analytic data suggest that adolescents with MDD exhibit significantly poorer EF compared to their counterparts without psychiatric history, with behavioral inhibition and planning abilities strongly impacted by the disorder (Wagner et al., 2015). This association is not surprising when considering the detrimental impact that MDD symptoms, such as diminished concentration, emotional dysregulation, and slowed thinking, can have on cognitive functioning (Gonda et al., 2015). Moreover, other depressive symptoms, such as cognitive distortions, may further hinder mental flexibility and enhance cognitive difficulties. The maladaptive processes associated with depression, such as extensive negative ruminations that monopolize the central executive resources of the brain, could lead to problematic cognitive styles (e.g., perseveration) and subsequent EF deficits (Kavanaugh et al., 2019; Visted et al., 2018). Moreover, cognitive flexibility is dependent upon the development of the frontal lobe (Casey, 2000), which may be impacted by depression (Bos et al., 2018). During a time when youth depend upon EF skills to succeed academically and socially, and indeed at an age when they are primed to exert more agency and self-regulation within their environments, depression in adolescence can be particularly harmful to successful achievement trajectories and broad socioemotional adjustment (Best & Naglieri, 2011).
Executive Functioning and Environmental Influences
When examining macrosystemic influences (e.g., poverty) that interact with biological variables, the development of frontal systems and emerging EF abilities are certainly vulnerable to early-life environmental factors (Davis et al., 2017; Diamond, 2006). Growing up in institutional/transitional settings (Fisher et al., 2013; Merz et al., 2013), in families with low socioeconomic status (SES; Lawson et al., 2018) or being exposed to childhood maltreatment (Su et al., 2019) has been found to impact EF and broad cognitive abilities. Particular emphasis has also been placed on the role of parenting, attachment, and family ecology in shaping EF in children (Bernier et al., 2015; Blair et al., 2014; Zebdi et al., 2016). The limited research on the association between negative parenting practices and cognitive functioning suggests that various maladaptive parenting behaviors are linked to poor global EF and low inhibition (Valcan et al., 2018). However, there is significant measurement heterogeneity within and across studies that include negative parenting constructs, and many combine behaviors characterized as controlling and engaging (e.g., intrusiveness, harsh discipline, and hostility; e.g., Halse, 2019), as well as neglectful and disengaged (e.g., rejection and detachment; e.g., Fatima et al., 2016), which can result in diverse findings. Further, most of these studies use younger samples and more adolescent-based research is needed to distinguish these parenting dynamics at different developmental stages of the offspring.
Despite the recent focus on the complexities involved in measuring the influence of parenting on EF (Fay-Stammbach et al., 2014), there is a gap in the literature regarding the construct of unpredictability in parenting behavior. Parent-child attachment research has indicated that consistently negative/rejecting parenting, which contributes to insecure-avoidant attachment, is less detrimental than inconsistent or unpredictable parenting, which in turn contributes to insecure-ambivalent/resistant or disorganized attachment (Cassidy and Berlin, 1994; Menon et al., 2020); cognitive development is likely to be impaired when youth cannot effectively adapt to and cope with an environment and/or relationship that is constantly changing (Bronfenbrenner & Evans, 2000; Davis et al., 2019; Glynn & Baram, 2019). However, severity of negative parenting (e.g., abuse) may also be an important factor to consider when weighing the salience of consistency versus unpredictability in parenting, which is beyond the scope of the current paper. Nonetheless, the ability to foresee the potential consequences to one’s behavior, which is a core feature of EF regarding planning and organizing, is likely rooted within the consistency experienced at home through predictable patterns of rewards and punishment, and dyadic regulation (Andrews et al., 2021; Bernier et al., 2015). Indeed, predictable limit-setting with young children has been observed to lead to better effortful control (i.e., self-regulation) over time (Lengua et al., 2007), whereas inconsistent discipline has been associated with poorer EF task performance in children and younger adolescents (Sosic-Vasic et al., 2017).
In addition to unpredictability in parenting behavior, youth may be negatively impacted by uncertainty experienced in the broader home environment. From a bioecological framework, the family microsystem and associated proximal factors, such as parent-child interactions and home environment, significantly shape cognitive developmental trajectories (Bronfenbrenner & Evans, 2000). Some literature has been dedicated to the cognitive cost attached to household chaos (e.g., lack of routine, crowding, instability; Ackerman & Brown, 2010; Marsh et al., 2020), which may be considered a proxy for some aspects of childhood unpredictability. Indeed, a recent meta-analysis found robust associations between household chaos and EF problems in children (Andrews et al., 2021). Predictability in the home, such as having family meals or traditions, consistent discipline, and housing stability, is essential to the development of self-regulation and EF, as children are able to predict the consequences of their actions and begin to establish self-reliance in their abilities to contribute to the family environment in a positive way (Martin et al., 2012).
Executive Functioning, Depression, and Unpredictable Environments
Although a few studies have examined how unpredictable environments are associated with adolescent depression (e.g., Bakker et al., 2012; Fowler et al., 2015; Glynn et al., 2019), none explored how these constructs may interact to contribute to EF difficulties. Children living in unstructured home environments have a tendency to disengage from their overstimulating family interactions rather than investing adequate regulation skills to cope with unpredictability (Vernon-Feagans et al., 2016). Within the context of habitual family instability and uncertainty, depressed adolescents may be more likely to withdraw and exhibit symptoms of anhedonia compared to youth without internalizing problems faced with similar stressful situations (Glynn et al., 2019). The level of severity of the youth’s unpredictable environment (e.g., consistent instability versus sporadic disorganization in the home environment) may differentially impact the relationship between depression and EF (Andrews et al., 2021). In summary, depression can lead to and/or compound the effects of EF deficits – experiencing pervasive unpredictability in childhood (e.g., lack of routines and consistency in the home), as opposed to less severe forms of uncertainty, could further strengthen this association.
A Note on EF Measurement
The Behavior Rating Inventory of Executive Function, Second Edition (BRIEF2; Gioia et al., 2015), including its previous iteration, is one of the most commonly used EF rating scales in the adolescent literature (Nyongesa, 2019). However, this measure has not strongly related to performance-based EF assessments in previous investigations (Andrews et al., 2021; Bodnar et al., 2007; Kavanaugh et al., 2019), with modest correlations reported in studies that did find associations (Miranda et al., 2015; Toplak et al., 2013). EF researchers contend that the BRIEF has greater ecological validity (i.e., responses on the rating scale have a functional resemblance to real-world behaviors, such as social adjustment), is more likely to predict future outcomes (e.g., academic functioning) and captures the wider range of broad EF abilities (Isquith et al., 2013) compared to performance-based assessments. In contrast, performance-based measures, which are collected in structured, artificial environments whereby youth are cued with detailed instructions, are more likely to capture individual cognitive components of the broader EF constructs (Isquith et al., 2013; Miranda et al., 2015). Neuroimaging studies have also differentiated brain regions implicated in predominantly cognitive aspects of EF compared to the behavioral components (Anderson et al., 2002). As these two modalities hone in on different underlying mechanisms, we used both aspects to measure EF in the current study. Prior EF research on proxies of unpredictability in childhood (Andrews et al., 2021; Marsh et al., 2020) and on depression (e.g., Wagner et al., 2015) primarily relied on performance-based measures. Studies that have used both EF modalities have shown associations between parent-rated EF and parent-rated adolescent depression scores and between youth performance on EF tasks and self-reported depression severity (Kavanaugh et al., 2019).
Current Study
The current investigation tested the hypothesis that unpredictability in the home environment would moderate the association between depression and EF difficulties, such that EF would be poorer for depressed youth who report unpredictability in their childhoods. As with the majority of samples included in the aforementioned literature on EF and depression, we utilized a convenience sample of community-recruited adolescents with varying levels of psychosocial treatment history. As the core study aimed to recruit youth with and without depression and was primarily focused on assessing outcomes (e.g., EF) for this vulnerable population, we were interested in environmental/parental factors that influence the relationship between depression and cognitive abilities. We further add to the neuropsychological assessment literature by using multi-modal EF assessments with the BRIEF2 self-report and a battery of performance-based assessments commonly used with adolescents (Nyongesa, 2019). Exploratory analyses test our hypothesis using diagnostic groups (i.e., adolescents with MDD versus healthy controls) to supplement the analyses using continuous depression measures.
Materials and Methods
Participants
Participants included 138 adolescents recruited from various community organizations and healthcare facilities throughout Southern California via advertisements and recruitment events between 2017 and 2020. Adolescents were between ages 13 and 17 years (M=15.91, SD=1.46), predominantly female (71.7%), and non-Hispanic (52.9%). Race was reported separately from ethnicity, and participants identified as White (47.8%), Multiracial (23.9%), Black (11.6%), Asian (10.2%), American Indian/Alaskan Native (5.1%), or Native Hawaiian/Pacific Islander (1.4%). Nearly half of the sample reported earning $70,000 and above in annual family income. SES, which was calculated using the Hollingshead (1957) scale based on the educational and occupational status of up to two primary caretakers, ranged from 11 to 61 (M=42.34, SD=11.94). Participants who volunteered for the study reported a wide range of treatment histories (e.g., currently in therapy, no history of psychiatric treatment). Although some participants reported having received MDD diagnoses by their mental health providers, MDD status was determined using psycho-diagnostic batteries described below.
Procedures
Adolescents were recruited as part of a larger neuroimaging study (Anonymous, 2020) and were eligible to participate if they were 13 to 17 years old at recruitment. All participants included herein represent those eligible following phone screening and recruited to-date. Exclusion criteria were based on self-report and included conditions that would affect brain development and EF performance on tasks, such as IQ below 80 and childhood neurological problems, as well as recent use of alcohol and/or drugs in the week before screening and psychotropic medications in the past three months. The protocol was approved by the Institutional Review Board. At the initial visit, youth and their parents completed informed consent/assent procedures and psycho-diagnostic interviews. Parents reported on sociodemographic factors, and youth completed self-report measures on unpredictability, depressive symptoms, and EF. At a subsequent visit shortly thereafter, youth were administered a brief neuropsychological battery (i.e., performance-based measures). Participants were compensated $50 for each of the two visits. Six adolescents who only participated in the initial visit did not complete performance-based EF measures. Three additional participants did not complete one auditory attention-based measure (i.e., Continuous Auditory Test of Attention; CATA) and one participant only completed the CATA at visit two due to equipment problems.
Measures
Appendix A provides an overview of the study measures, including the constructs captured by each score/scale/subscale used to measure EF and unpredictability, and the collection method and mode of inference.
Childhood Unpredictability
The Questionnaire of Unpredictability in Childhood (QUIC) was developed by Glynn and colleagues (2019) to comprehensively examine the impact of early-life physical, emotional, and relational unpredictability on adolescent and adult mental health. The QUIC was designed to excavate the unique influence that childhood unpredictability can have on developmental trajectories. Respondents are instructed to answer “yes” or “no” to 38 items for experiences occurring prior to age 18 (29 items) or experiences more likely to occur prior to age 12 (9 items across two subscales; e.g., parents late picking up from school), which comprise the following subscales (see Appendix A): Parental Monitoring and Involvement (9 items), Parental Predictability (12 items), Parental Environment (7 items), Physical Environment (7 items), and Safety and Security (3 items). Higher scores, which include reverse-scoring of some yes/no answers, indicate greater perceived unpredictability. The QUIC total score was used in the current study’s primary analyses and exploratory analyses examined subscale scores. The QUIC was validated in a sample of 175 adolescents, with good internal consistency reported for the total scale (α=0.84). The current sample’s Cronbach’s alpha was acceptable (α=0.72).
Depression
All psycho-diagnostic assessments were conducted by a licensed child and adolescent psychiatrist or clinical psychologists supervised by the aforementioned psychiatrist. Adolescents and a primary caregiver were separately administered the computerized Kiddie Schedule for Affective Disorders and Schizophrenia for School-Aged Children (K-SADS-COMP V2.0; Townsend et al., 2020) and consensus ratings were used to determine MDD criteria. This instrument has good psychometric properties (interrater agreement=0.94 to 0.98; and strong convergent validity with other depression scales) and was used in the current study to compare adolescents with MDD (n=63) to healthy controls (HC) with no lifetime psychiatric history (n=75) on variables of interest.
Depression severity was assessed using the 17-item Children’s Depression Rating Scale–Revised Version (CDRS-R; Poznanski, 1996), a clinician-rated, semi-structured interview used to ascertain impairment level of several domains of functioning (e.g., schoolwork, sleep disturbance, morbid ideation) over the past month, including three observational scales (i.e., depressed facial affect, listless speech, and hypoactivity). The measure was originally developed for 6-12-year-old children and was validated in an adolescent sample meeting/not meeting criteria for MDD (Cronbach’s α=0.74 to 0.94; Mayes, 2010); similarly, our sample exhibited good internal consistency (α=0.95). Total scores range from 17 to 117, with 28 or below indicating mild or minimal symptoms and 40 and above suggesting significant symptomology.
Lastly, participants completed the 21-item Beck Depression Inventory (BDI-IA; Beck, 1961) to report on depression severity over the past week using a 4-point scale (0=low to 4=extreme symptom severity). This inventory demonstrated good internal consistency in the current sample (α=0.95) as have previous validation studies (α=0.73 to 0.93; Beck, 1988). Total scores range from 0 to 63, with 16 and below indicating minimal to mild symptoms and scores 17 and above indicating moderate to severe depression.
Self-reports of Executive Functioning
Adolescents completed the 55-item BRIEF2 (Gioia et al., 2015), which assesses for problems with school- and home-based behaviors over the past six months (rated on a 3-point scale as “never, sometimes or often”). Three main EF indices are calculated, including the Behavior Regulation Index (BRI; difficulty inhibiting impulses and self-monitoring consequences of behavior on others; e.g., “I am unaware of my behavior when I am in a group”), the Cognitive Regulation Index (CRI; difficulty with planning, problem-solving, learning, task completion; e.g., “I don’t think ahead about possible problems”), and the Emotion Regulation Index (ERI; difficulty flexibly shifting emotional control; e.g. “My eyes fill with tears quickly over little things”). Higher T-scores indicate greater impairment (i.e., T=60-64 mildly elevated; T=70+ clinically elevated) and scoring protocols provide age- and sex-normed T-scores (M=50, SD=10). A Global Executive Composite (GEC) yields a summary score by incorporating all clinical scales and is the primary self-report EF measure used in the current study. The BRIEF2 was validated with a large, nationally stratified sample and displayed good internal consistency; Cronbach’s alphas in the current sample yielded similar coefficients to those found in the validation studies (GEC α=.97; BRI α=.88; CRI α=.96; ERI α=.92). The original measure and its revision have been widely used to examine associations between EF and various mental health problems, including depression, in various clinical and non-clinical adolescent samples (Kavanaugh, et al., 2019; Peters, 2019).
Performance-based Executive Functioning
The following tasks were administered by staff who were trained by clinical psychologists. The Conners’ Continuous Performance Test, 3rd edition (CPT-3; Conners, 2014a) and the Continuous Auditory Test of Attention (CATA; Conners, 2014b) are computerized, validated assessments of sustained attention used with ages 8 years and older. For the CPT-3, participants are required to respond to the letter “X” (targets) presented on a screen by pressing a button and to refrain from responding to other letters (non-targets). Each of the 360 targets are presented for 250ms with 1, 2, and 4 second interstimulus intervals. Similarly, for the CATA, respondents are asked to press a button when hearing a high-tone sound when it is preceded by a low-tone sound, and to refrain from responding to high tones when they are presented by themselves.
Both tasks are 14 minutes in length and scoring protocols yield age-and sex-normed T-scores (M=50, SD=10), with higher scores indicating greater impairment. The three scores used in the current study represented inattention (i.e., missed targets; Omissions), impulsivity/behavioral inhibition (i.e., incorrect responses to non-targets; Commissions), and problems with sustained attention (i.e., discrimination between targets and non-targets; Detectability). These indices are commonly selected to examine EF abilities in adolescents and young adults, have shown discriminant validity when comparing individuals with Attention-Deficit/Hyperactivity Disorder (ADHD) to the general population (Conners, 2014a and 2014b; Wang et al., 2019), and also have been used in studies examining EF in depressed adolescents (e.g., Sommerfeldt et al., 2016).
Participants also completed the Color-Word Interference (CWIT) subtest of the Delis-Kaplan Executive Function System (Delis et al., 2001), a well-validated measure commonly used to assess EF in adolescents (Nyongesa, 2019). This stroop-like task, which presents 50 stimuli of “red, blue, and green” on each of the four conditions, requires participants to name the colors of squares presented on page with speed and accuracy (Condition 1: Color Naming), read aloud “red, blue, green” words presented in black print (Condition 2: Word Reading), read aloud color-words presented in incongruent colors (e.g., “blue” printed in green; Condition 3: Inhibition), and alternate between reading the words regardless of the print color or to say the color in which that word is printed based on a predetermined rule (i.e., when there is a box around that word; Condition 4: Inhibition/Switching). Conditions 1-4 performance scores are calculated based on completion time regardless of errors and yield age-corrected standard scores (M=10, SD=3), with higher scores indicating better ability. Conditions 1 and 2 represent more basic attention and language skills, whereas Conditions 3, and particularly 4 represent higher-order cognitive flexibility and inhibition (Fatima et al., 2016). Inhibition/Switching was therefore used as the primary performance-based EF measure.
Social Functioning
The 21-item Social Adjustment Scale-Self-Report for Youth (SAS-SR-Y; Weissman et al., 1980) was administered to measure degree of functioning, communication, and support within school, friends/spare time, and family contexts. Adolescents rate items on a 5-point scale whereby higher scores indicate greater social impairment over the last two weeks. The SAS-SR-Y exhibited good psychometric properties in depressed/healthy adolescent samples (e.g., Stice et al., 2008) and the total score used in the present sample exhibited good internal consistency (α=.87). This measure was used in the current study to examine the ecological validity of scores on the BRIEF2, such that greater EF impairments were expected to coincide with greater social functioning problems.
Analytic Plan
Analyses were conducted using SPSS Version 24.0. Participants with one or more missing performance-based measures (n=10) did not significantly differ on sociodemographic variables or on primary variables of interest (i.e., CDRS, BDI, QUIC total, and BRIEF GEC) compared to participants with complete data (n=128). Further, results from Little’s MCAR test indicated that data were missing completely at random, X2(10, N=132)=8.763, p=.56 (Schlomer et al., 2010). Therefore, models were computed with all available data (FIML). Skewness and Kurtosis, which were examined by transforming coefficients to z-scores (Kim, 2013), indicated that Spearman correlations were warranted as most indices went beyond the threshold of normality (z=1.89 to 17.22); partial correlations controlled for confounding variables associated with primary outcomes. However, assumptions for linear regressions were met based on normality of variable residuals.
Our primary hypothesis was tested using hierarchical linear regressions, which included covariates (step 1), predictor variables (steps 2 and 3), and an interaction term (step 4), computed by mean centering predictor variables and multiplying the centered depression and unpredictability terms for interaction. Conditional effects were probed by calculating simple slopes at the mean, low (−1 SD of the mean), and high (+1 SD of the mean) values of the moderator. Regression models were repeated using self-reported and clinician-rated measures of depressive symptoms separately. As multiple performance-based EF indices were collected, in order to reduce multiple comparisons and limit Type-I error for our primary hypothesis, CWIT Inhibition/Switching was pre-selected as the performance-based EF index most closely representing higher-order cognitive flexibility and interpretations were limited to a more conservative threshold of significance at p<.01 based on Bonferroni correction.
Exploratory analyses included diagnostic group (MDD vs. HC) comparisons of both BRIEF GEC scores and performance-based measures, which were conducted using analysis of covariance (ANCOVA) with QUIC scores included as a predictor and a group*QUIC interaction term; covariates included SES and age. Chi-squares were also conducted to compare the groups on clinical range categories of EF measures. To explore all components of basic attention and inhibition, each performance-based measure was included as an outcome using similar regression models as primary hypothesis-testing. Lastly, associations between QUIC and BRIEF subscales were explored using partial correlations.
Results
Descriptive Statistics and Preliminary Analyses
Means, standard deviations, and correlations of demographic and outcome variables are presented in Table 1 (primary and self-report variables) and Table 2 (performance-based EF variables). Sociodemographic characteristics were examined in relation to the primary variables of interest; t-tests revealed no differences between sexes or racial groups (dichotomized as White and non-White due to small subgroup samples), and age correlated modestly with CDRS (r=.20, p<.05) and BDI scores (r=.23, p<.01). Primary variables differed by ethnicity, such that Hispanic participants exhibited poorer EF scores (e.g., BRIEF GEC: t(136)=4.57, p<.01), and higher depressive symptom (e.g., CDRS: t(136)=3.06, p<.01) and childhood unpredictability (t(135)=2.72, p<.01) scores. Hispanic families also reported significantly lower SES, t(135)=−5.38, p<.01, and SES was significantly associated with primary variables of interest (see Table 1). As ethnicity and SES co-occurred, SES, rather than ethnicity, was selected as a covariate in the analyses alongside age. Moreover, similar results yielded when replacing ethnicity for SES in our models. Given the well-established link between SES and EF (Lawson et al., 2018), and as depression and EF both vary with age, we carefully selected these two variables as covariates in all models, including all correlations. With respect to clinical range of EF abilities, adolescents in our sample predominantly exhibited average BRIEF GEC scores (62%), with the remainder scoring in the mildly elevated (20%) and clinically elevated (18%) range.
Table 1.
Descriptive Statistics, Partial Spearman Correlations Among Primary Study Variables, and Group Comparisons
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | Total (N=138) M (SD) |
MDD (n=63) |
HC (n=75) |
t |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | -- | -- | 15.91 (1.46) | 16.28 (1.40) | 15.60 (1.45) | −2.79** | ||||
| 2. SES | -- | -- | 42.34 (11.98) | 39.38 (13.15) | 44.83 (10.26) | 2.68** | ||||
| 3. CDRS | .20* | .28** | -- | 49.04 (19.36) | 68.06 (10.55) | 33.05 (5.82) | −23.51** | |||
| 4. BDI | .23** | .27** | .77** | -- | 13.43 (14.16) | 24.75 (12.840) | 3.93 (5.73) | −11.91** | ||
| 5. BRIEF | .13 | .28** | .62** | .71** | -- | -- | 57.14 (13.07) | 66.27 (11.50) | 49.47 (8.66) | −9.55** |
| 6. QUIC | .02 | .31** | .41** | .50** | .50** | .50** | 9.38 (7.23) | 12.83 (7.61) | 6.45 (5.40) | −5.57** |
| 7. SAS-SR-Y | .18* | −.32** | .73** | .88** | .74** | .57** | 42.54 (14.03) | 53.17 (12.13) | 33.60 (7.98) | −10.97** |
Note. Age and SES are included as control variables in the Spearman correlations 3-6; MDD=Major Depressive Disorder; HC=Healthy Control; t = Independent Samples t-test comparing MDD and HC participants.
SES=Socioeconomic Status using Hollingshead scale; CDRS= Children’s Depression Rating Scale–Revised Version; BDI=Beck Depression Inventory; BRIEF= Behavior Rating Inventory of Executive Function Global Executive Composite; QUIC=Questionnaire of Unpredictability in Childhood adolescent total score; SAS-SR-Y= Social Adjustment Scale-Self-Report for Youth;
p < .05.
p < .01.
Table 2.
Descriptive Statistics, Partial Spearman Correlations Among Neuropsychological Performance Scores and Primary Study Variables, and Group Comparisons
| Variable | CDRS | BDI | BRIEF | QUIC | SAS-SR-Y | M (SD) | MDD (n=61) |
HC (n=71) |
t |
|---|---|---|---|---|---|---|---|---|---|
| CPT detectability | −.04 | −.10 | −.03 | .23* | −.06 | 47.39 (9.68) | 47.13 (8.88) | 47.61 (10.37) | 0.28 |
| CPT omissions | −.05 | −.09 | −.05 | .16 | −.07 | 47.97 (8.01) | 47.28 (6.74) | 48.56 (9.07) | 0.91 |
| CPT commissions | −.03 | −.05 | .01 | .26** | .01 | 47.97 (9.23) | 48.11 (8.94) | 47.85 (9.54) | −0.17 |
| CATA detectability | .12 | .10 | .05 | .28** | .14 | 52.08 (9.06) | 53.05 (8.43) | 51.23 (9.55) | −1.14 |
| CATA omissions | .10 | .06 | .08 | .09 | .06 | 46.96 (6.19) | 47.15 (5.89) | 46.80 (6.47) | −0.32 |
| CATA commissions | .15 | .15 | .10 | .26** | .18* | 50.31 (8.62) | 50.78 (8.22) | 49.90 (8.99) | −0.58 |
| CWIT Color Naming | −.20* | −.19* | −.16 | −.25** | −.15 | 9.27 (2.82) | 8.54 (2.75) | 9.89 (2.75) | 2.80** |
| CWIT Word Reading | −.16 | −.09 | −.05 | −.16 | −.06 | 10.37 (2.46) | 9.89 (2.44) | 10.79 (2.42) | 2.13* |
| CWIT Inhibition | −.13 | −.09 | −.07 | −.21* | −.08 | 10.12 (3.11) | 9.64 (3.12) | 10.54 (3.07) | 1.66 |
| CWIT Inhibition/Switching | −.16 | −.14 | −.13 | −.16 | −.07 | 9.88 (3.12) | 9.70 (3.02) | 10.03 (3.22) | 0.59 |
Note. Age and SES are included as control variables in the Spearman correlations; Higher CPT and CATA scores indicate poorer performance and higher scores on CWIT indicate better performance; sample sizes vary for some measures.
CPT=Continuous Performance Test; CATA=Continuous Auditory Test of Attention; CWIT=Color-Word Interference; CDRS= Children’s Depression Rating Scale–Revised Version; BDI=Beck Depression Inventory; BRIEF=Behavior Rating Inventory of Executive Function Global Executive Composite; QUIC=Questionnaire of Unpredictability in Childhood adolescent total score; SAS-SR-Y= Social Adjustment Scale-Self-Report for Youth; MDD=Major Depressive Disorder; HC=Healthy Control; t = Independent Samples t-test comparing MDD and HC participants.
p < .05.
p < .01.
Associations between Study Variables
All primary study variables were moderately to strongly associated with each other after accounting for age and SES (Table 1). Expectedly, the clinician-rated and self-reported depression measures were highly correlated, and greater childhood unpredictability was associated with greater depression severity. As expected, poorer self-reported EF on the BRIEF was associated with poorer social adjustment on the SAS. Partial correlations controlling for age and SES showed strong associations between depression scores and the BRIEF. Further, greater childhood unpredictability was associated with poorer EF on the BRIEF.
No associations were found between performance-based and self-report EF measures, nor between depression and EF task performance (Table 2). QUIC scores yielded associations with some performance-based measures, with coefficients ranging from .21 to .28. Specifically, greater childhood unpredictability was associated with poorer visual and auditory attention skills (CATA Detectability; CWIT Color Naming), and poorer impulse-control on visual and auditory attention tasks (CPT and CATA Commissions).
Hypothesis Testing
Hierarchical linear regressions showed that childhood unpredictability significantly moderated the association between depression and self-reported global EF (Table 3, step 4). Graphical representations of the data demonstrate that a high depression score was significantly linked to greater EF difficulties (i.e., exhibiting the worst BRIEF scores within the sample) regardless of QUIC scores (Figures 1a & b). Decomposition of the simple slopes indicated that increases in childhood unpredictability led to increases in EF difficulties for adolescents exhibiting low symptoms of depression for both CDRS (Figure 1a) and BDI (Figure 1b), although only the BDI was significant at the p<.01 level. QUIC scores did not significantly interact with either self-reported or clinician-rated depression scores when testing moderation with the same hierarchical models for performance-based EF, using CWIT Inhibition/Switching as an outcome (Table 4, step 4).
Table 3.
Hierarchical Linear Regressions Examining Childhood Unpredictability as a Moderator of the Effect of Depression Severity (Model 1: CDRS; Model 2: BDI) on Self-Reported Executive Functioning
| Outcome: BRIEF GEC | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable CDRS |
Step 1 | Step 2 | Step 3 | Step 4 | ||||||||
| B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI | |
| SES | −0.34** | 0.09 | −0.52, −0.16 | −0.14 | 0.07 | −0.28, 0.01 | −0.09 | 0.07 | −0.24, 0.05 | −0.09 | 0.07 | −0.23, 0.05 |
| Age | 1.54* | 0.73 | 0.10, 2.98 | 0.20 | 0.59 | −0.96, 1.36 | 0.23 | 0.56 | −0.88, 1.35 | 0.22 | 0.55 | −0.88, 1.32 |
| CDRS | 0.43** | 0.05 | 0.34, 0.52 | 0.36** | 0.05 | 0.27, 0.46 | 0.36** | 0.05 | 0.26, 0.45 | |||
| QUIC | 0.43** | 0.13 | 0.18, 0.67 | 0.52** | 0.13 | 0.26, 0.77 | ||||||
| CDRS x QUIC | −0.02* | 0.01 | −0.03, −0.01 | |||||||||
| Adj. R2 | .10 | .45 | .49 | .51 | ||||||||
| ΔF | 8.71** | 87.42** | 11.52** | 5.87* | ||||||||
| BDI | ||||||||||||
| SES | −0.34** | 0.09 | −0.52, −0.16 | −0.13 | 0.07 | −0.27, 0.01 | −0.10 | 0.07 | −0.24, 0.04 | −0.08 | 0.07 | −0.22, 0.05 |
| Age | 1.54* | 0.73 | 0.10, 2.98 | 0.20 | 0.57 | −0.93, 1.33 | 0.25 | 0.56 | −0.86, 1.35 | 0.23 | 0.54 | −0.85, 1.30 |
| BDI | 0.60** | 0.06 | 0.48, 0.72 | 0.52** | 0.07 | 0.39, 0.65 | 0.54** | 0.07 | 0.41, 0.67 | |||
| QUIC | 0.35** | 0.13 | 0.10, 0.60 | 0.46** | 0.13 | 0.21, 0.72 | ||||||
| BDI x QUIC | −0.02** | 0.01 | −0.04, −0.01 | |||||||||
| Adj. R2 | .10 | .48 | .50 | .53 | ||||||||
| ΔF | 8.71** | 97.77** | 7.56** | 8.83** | ||||||||
Note. QUIC, CDRS, and BDI are mean-centered.
BRIEF= Behavior Rating Inventory of Executive Function; GEC=Global Executive Composite; SES = socioeconomic status; CDRS=Children’s Depression Rating Scale–Revised; BDI = Beck Depression Inventory; QUIC = Questionnaire of Unpredictability in Childhood (Total Score).
p < .05.
p < .01.
Figure 1a. The Interaction Between Depression (CDRS) and Unpredictability (QUIC) Predicts BRIEF GEC Scores.
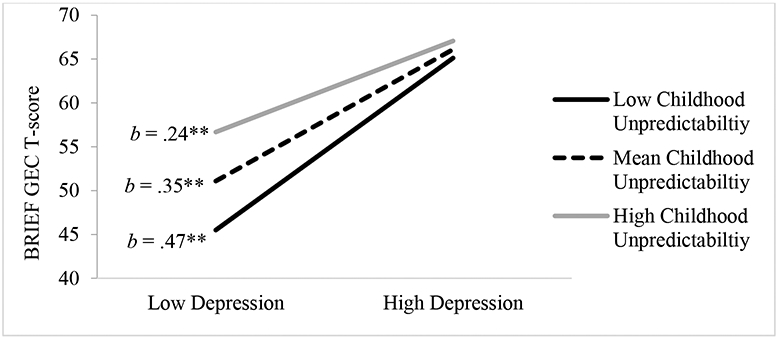
Note. QUIC low score=2.15, mean score=9.38, high score=16.61; CDRS low score=29.67 and high score=68.40; CDRS ≤ 27 indicate minimal/mild depression and ≥ 41 indicate severe depression; Higher BRIEF scores indicate poorer EF
**p < .01
Figure 1b. The Interaction Between Depression (BDI) and Unpredictability (QUIC) Predicts BRIEF Scores.
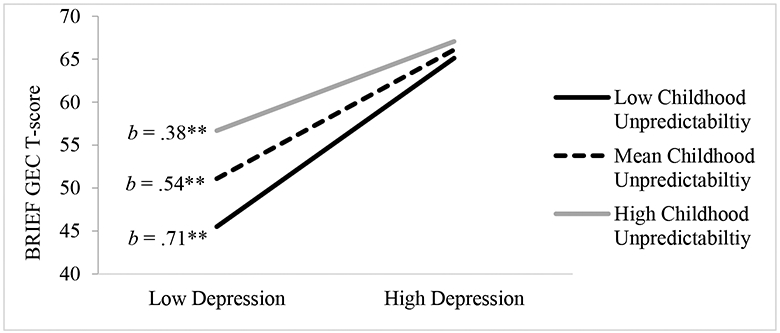
Note. QUIC low score=2.15, mean score=9.38, high score=16.61; BDI low score=1.16 and high score=27.60; BDI ≤ 16 indicate mild/minimal depression and ≥ 17 indicate moderate to severe depression; Higher BRIEF scores indicate poorer EF.
**p < .01
Table 4.
Hierarchical Linear Regressions Examining Childhood Unpredictability as a Moderator of the Effect of Depression Severity (Model 1: CDRS; Model 2: BDI) on Performance-Based Executive Functioning
| Outcome: CWIT Inhibition/Switching | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable CDRS |
Step 1 | Step 2 | Step 3 | Step 4 | ||||||||
| B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI | B | SE | 95% CI | |
| SES | 0.04 | 0.02 | −0.01, 0.08 | 0.03 | 0.02 | −0.02, 0.08 | 0.03 | 0.02 | −0.02, 0.07 | 0.03 | 0.02 | −0.02, 0.07 |
| Age | 0.28 | 0.18 | −0.08, 0.65 | 0.35 | 0.19 | −0.02, 0.73 | 0.35 | 0.19 | −0.02, 0.73 | 0.35 | 0.19 | −0.03, 0.73 |
| CDRS | −0.02 | 0.02 | −0.05, 0.01 | −0.02 | 0.02 | −0.05, 0.01 | −0.02 | 0.02 | −0.05, 0.01 | |||
| QUIC | −0.02 | 0.04 | −0.10, 0.07 | −0.02 | 0.05 | −0.11, 0.07 | ||||||
| CDRS x QUIC | 0.01 | 0.01 | −0.01, 0.01 | |||||||||
| Adj. R2 | 0.03 | 0.03 | .03 | 0.02 | ||||||||
| ΔF | 2.95 | 0.90 | 1.40 | 0.01 | ||||||||
| BDI | ||||||||||||
| SES | 0.04 | 0.02 | −0.01, 0.08 | 0.03 | 0.02 | −0.01, 0.08 | 0.03 | 0.02 | −0.02, 0.08 | 0.03 | 0.02 | −0.02, 0.08 |
| Age | 0.28 | 0.18 | −0.08, 0.65 | 0.31 | 0.19 | −0.07, 0.69 | 0.31 | 0.19 | −0.07, 0.69 | 0.30 | 0.19 | −0.07, 0.68 |
| BDI | −0.01 | 0.02 | −0.05, 0.03 | −0.01 | 0.02 | −0.05, 0.04 | −0.01 | 0.02 | −0.05, 0.04 | |||
| QUIC | −0.04 | 0.04 | −0.12, 0.05 | −0.05 | 0.05 | −0.14, 0.04 | ||||||
| BDI x QUIC | 0.01 | 0.01 | −0.01, 0.01 | |||||||||
| Adj. R2 | 0.03 | 0.02 | 0.02 | 0.03 | ||||||||
| ΔF | 2.95 | 0.30 | 0.62 | 2.04 | ||||||||
Note: QUIC, CDRS, and BDI are mean-centered.
CWIT=Color-Word Interference; SES = socioeconomic status; CDRS=Children’s Depression Rating Scale–Revised; BDI = Beck Depression Inventory; QUIC = Questionnaire of Unpredictability in Childhood (Total Score).
p < .05.
p < .01.
Exploratory Analyses
Diagnostic Group Comparisons
Tables 1 and 2 present means, standard deviations, and t-test comparison results of all study variables for the MDD and HC groups. Consistent with the associations observed between sociodemographic factors and continuous depression measures, participants diagnosed with MDD were older, came from lower SES backgrounds, and were more likely to be Hispanic (62%) compared to HC (35%), X2=10.20, p<.01. Further, the groups differed on one performance-based measure of basic attention (CWIT Color Naming; Table 2).
After adjusting for age and SES, there was a main effect of diagnostic status on BRIEF scores, F(3,134)=76.53, p<.01, indicating significantly poorer self-reported EF in depressed adolescents (M=65.74, SD=1.30) compared to HC (M=49.92, SD=1.18). An additional ANCOVA was conducted to examine whether unpredictability moderated the effect of depression diagnosis on EF, and no moderating effect was found for either the BRIEF, F(5,131)=1.76, p=.19, or CWIT Inhibition/Switching, F(5,126)=0.03, p=.85. Table 5 presents group comparisons on BRIEF clinical range categories, which revealed that MDD participants were significantly more likely to score in the mildly-to-clinically elevated ranges on all BRIEF subscales compared to HC. Of note, all 25 adolescents scoring in the clinically elevated range on the BRIEF GEC were diagnosed with MDD.
Table 5.
Descriptive Statistics and Group Comparisons on Clinical Range Categories for BRIEF Scores
| Variable | MDD (n=63) | HC (n=75) | X 2 | ||
|---|---|---|---|---|---|
| n | % | n | % | ||
| GEC Average | 22 | 34.9 | 63 | 84.0 | 44.64** |
| GEC Mild | 16 | 25.4 | 12 | 16.0 | |
| GEC Elevated | 25 | 39.7 | 0 | 0 | |
| BRI Average | 30 | 47.6 | 68 | 90.7 | 31.13** |
| BRI Mild | 24 | 38.1 | 6 | 8.0 | |
| BRI Elevated | 9 | 14.3 | 1 | 1.3 | |
| CRI Average | 19 | 30.2 | 61 | 81.3 | 46.81** |
| CRI Mild | 16 | 25.4 | 13 | 17.3 | |
| CRI Elevated | 28 | 44.4 | 1 | 1.3 | |
| ERI Average | 16 | 25.4 | 64 | 85.3 | 52.61** |
| ERI Mild | 24 | 38.1 | 9 | 12.0 | |
| ERI Elevated | 23 | 36.5 | 2 | 2.7 | |
Note. MDD=Major Depressive Disorder; HC=Healthy Control; BRIEF= Behavior Rating Inventory of Executive Function; GEC=Global Executive Composite; BRI=Behavioral Regulation Index; CRI=Cognitive Regulation Index; ERI=Emotional Regulation Index; Average=T-scores below 59; Mild=T-scores 60-64; Elevated=T-scores 70 and above.
p < .01.
When exploring other performance-based measures as outcomes using this model, there were no main effects of diagnostic status, but diagnosis and unpredictability interacted to predict CPT Omissions scores, F(5,126)=7.87, p<.01, such that MDD participants exhibited lower scores (i.e., better performance; M=47.15, SD=1.10) than did HC youth (M=50.43, SD=1.05) when accounting for unpredictability. However, these scores do not denote clinically significant differences in visual attention, as both groups performed in the average range (i.e., normative sample T-scores M=50, SD=10). Additionally, chi-square analyses, whereby T-scores were categorized as average (<60) or elevated (≥60), revealed no group differences for CPT Omission scores (X2=1.73, p>.05). No main effects of unpredictability were observed for these measures, and depression diagnosis and unpredictability did not interact to predict other performance-based EF.
Performance-based EF Regressions
As with the models conducted for our primary hypothesis testing, hierarchical linear regressions were conducted with each of the other nine performance-based EF measures as outcomes and with BDI and CDRS included as interaction terms with childhood unpredictability in separate models. Tasks that did not meet regression assumptions (i.e., non-normality of variable residuals) were winsorized; namely, CPT Omissions and CATA Omissions and Commissions. Although no significant interactions were found, marginal findings show that youth with low depression, but not high depression severity, performed worse on visual attention tasks when they reported greater levels of childhood unpredictability. Similar to patterns observed using the BRIEF, adolescents with high depression severity performed poorly on performance-based EF measures regardless of unpredictability level, although mean EF scores were not in the impairment range. Decomposition of the simple slopes graphs for marginal findings at p<.05 are included in Appendix B and the exploratory regression tables are included in Appendix C.
Associations between BRIEF and QUIC subscales
Correlation results for all BRIEF and QUIC subscales revealed similar patterns to those found with total scores for each index in relation to depression ratings. All BRIEF and QUIC subscale associations yielded significant values (p<.01) ranging from .21 to .48, with the QUIC Parental Predictability subscale showing the strongest correlations and Parental Environment exhibiting the smallest associations. The BRIEF Emotional Regulation Index, expectedly, exhibited the strongest correlation with self-reported depression ratings (r=.73). Most QUIC subscales yielded small to moderate correlation values with depression scores (r=.24 to .47).
Discussion
The present study explored the complex relationships between executive functioning and depression, and the systemic influence of home environment unpredictability from a bioecological perspective. We hypothesized that EF would be poorer for adolescents with depression and unpredictable childhoods. Results showed that unpredictability in childhood may incur risk for poorer broad EF abilities for adolescents reporting milder symptomology. However, for youth reporting high levels of depression in the current sample, broad EF deficits were observed regardless of childhood unpredictability, which suggests that biological influences may overshadow ecological risk factors that exist beyond individual-level variables. No such interaction between depression and childhood unpredictability was observed for the more specific cognitive components measured by performance-based EF tests, and visual attention diagnostic group differences did not denote clinically significant distinctions (i.e., scores for both groups did not significantly differ from average scores in the normative population used in standardization samples).
When examining relationships between pairs of key constructs, depression and unpredictability were individually associated with youth EF ratings after accounting for the influence of age and SES. The diagnostic groups differed on all BRIEF indices with respect to clinical range categories, with greater EF impairment found in adolescents meeting MDD criteria compared to healthy controls. These results correspond to findings from a recent study by Kavanaugh and colleagues (2019), which found some associations between BRIEF2 parent ratings and both depressive symptoms and diagnosis in a clinical sample of youth spanning childhood and adolescence.
The domain of unpredictability in the home environment measured in the current study has not been previously explored in the literature in a comprehensive manner; however, household chaos and inconsistent parenting behaviors/relationships can be considered adequate proxies for the various uncertainties experienced in early life. The relationship between QUIC scores and EF observed herein is generally consistent with research on household chaos and young children’s cognitive development (Andrews et al., 2021; Marsh et al., 2020), as well as emerging work on perceived low maternal care and poor parent-child relationships predicting EF difficulties in adolescent boys (Harwood-Gross et al., 2020). When examining relationships between specific QUIC subscales in the current study, exploratory analyses revealed that poorer Parental Predictability (e.g., inconsistent punishment, parent mood lability, uncertainty of parental presence, lack of family activities) showed the highest correlation with all BRIEF indices. Indeed, bioecological theory eloquently explains this association, with unpredictability (i.e., interruption of important environmental patterns) contributing to developmentally-disruptive cognitive outcomes (Bronfenbrenner & Evans, 2000).
Overall, our results suggest that adolescents who report milder depressive symptoms and who report childhoods marked by uncertainty, such as tenuous parental relationships (e.g., inconsistent punishment), may struggle to regulate their behaviors and emotions across several settings. This is consistent with meta-analysis findings showing links between disorganized attachment and internalizing and externalizing behaviors throughout childhood for community samples of adolescents (Madigan et al., 2016). In addition to the influence of distal and proximal factors such as genetics and early-life attachment, it may be that youth who have been habitually exposed to uncertainty within their environments, perhaps observing and learning from mercurial parental figures, may essentially begin to emulate those maladaptive behaviors (Bandura, 1977), thus placing them at risk for depression and cognitive difficulties. Further, these individuals may not have had the opportunity to benefit from parent-child co-regulation and may now be inefficient at coping with the stress of unpredictable environments (Vernon-Feagans et al., 2016), thereby compounding the effect of depressive symptoms on EF. Ample research shows the link between depression and broad cognitive difficulties, but less is known about adolescents exhibiting milder symptoms, as studies tend to solely focus on diagnostic categories or may overlook gradations in symptoms (e.g., Wagner et al., 2015). Indeed, one of the strengths of the current study is our inclusion of diagnostic distinctions in addition to continuous measurements of depression, without which we would not have observed how unpredictability significantly changes the relationship between depression and EF. Youth who do not meet full MDD criteria may be vulnerable to negative outcomes due to high familial/socioecological risk factors, such as living in chaotic homes. These environmental stressors should not be overlooked as they are an essential component contributing to the bioecological framework.
Clinical Implications
Our findings have some potential assessment and treatment implications. First, given the link between high levels of depression and EF difficulties, evidence-based psychosocial and pharmacological treatments for depression may improve EF through symptom reduction (Biringer et al., 2005; Gonda et al., 2015). Second, as youth exhibiting more severe symptomology are more likely to seek treatment and receive a higher level of care compared to those with milder symptoms (Mendenhall et al., 2012), adolescents with sub-threshold depression may not be referred for mental health services or neglected in this system if they are referred. Therefore, providers based in schools or primary care may be more optimally slated to intervene. Living in a chaotic versus stable environment appears to matter greatly to the cognitive functioning of youth experiencing low levels of depressive symptomology. Hence, care providers working with adolescents seeking help for broad EF-related problems (e.g., academic and/or social adjustment problems) may consider systematically assessing for key ecological factors, such as early-life environment and parent-child relationships. As early-life stress has been linked to myriad negative outcomes in childhood (Oh et al., 2018), healthcare best practices and recommendations are emerging which include screening pediatric populations for adverse childhood experiences (ACEs; Shonkoff & Garner, 2012), using a measure which taps into some constructs of unpredictability (Felliti et al., 1998).
To the best of our knowledge, no interventions have been identified for specifically addressing household chaos, as also recognized by others (Marsh et al., 2020). However, speaking to the more nuanced construct of unpredictability of the home environment, most family-centered adolescent therapies target various aspects of unpredictable parenting, such as helping caregivers implement routines and use consistent contingencies (e.g., Multisystemic Therapy: Henggeler & Schaeffer, 2016; behavioral management strategies: Johnson et al., 2014). For adolescents with subthreshold depression living in unstable environments, increasing consistency in the home may yield the greatest positive change on broad EF skills. Establishing daily routines has the potential to significantly improve self-regulation in younger children (Martin et al., 2012); such approaches may also be beneficial to adolescents, particularly those who may have disengaged from the family system due to unpredictability.
With respect to addressing the link between depression and unpredictability, some interventions aiming to enhance family cohesiveness and routines by increasing meals eaten together have led to reductions in adolescent depression (Fulkerson et al., 2009). Moreover, a systematic review of the depression intervention literature indicates that targeting both symptom reduction and the parent-adolescent relationship by methodically involving parents in treatment maximize positive outcomes (Dardas et al., 2018). Stability in the home environment, including financial stability, as well as family cohesion, belonging, and supportive parent-child relationships, have been highlighted as protective factors leading to positive adolescent outcomes (Murray & Monson, 2013).
Intervening in chaotic households may be most impactful earlier in development for youth exhibiting early signs of internalizing problems (Bakker et al., 2012). The influence of specific parenting behaviors on child EF, such as scaffolding and sensitivity, has been comprehensively studied in younger samples (e.g., Fay-Stammbach et al., 2014), and has been identified as the primary focus of parenting interventions. For example, Parent-Child Interaction Therapy (McNeil & Hembree-Kigin, 1995), which was developed from attachment and social learning theories, promotes consistent communication, and targets parent-child co-regulation, has been effective in enhancing consistency in discipline for families living in unstable environments (e.g., Herschell et al., 2017). In summary, strengthening parent-child/adolescent relationships and increasing consistency in the home through behavior management approaches may be the best course of treatment to strengthen cognitive functioning for mildly depressed youth reporting unpredictable childhoods and interrupt the vicious cycle of worsening depressive symptoms, EF deficits and parent-child relationship.
Contribution to the EF Measurement Literature
This study adds to the body of literature utilizing the BRIEF to measure EF with adolescents diagnosed with MDD in addition to examining depressive symptoms and, to the best of our knowledge, this is the first investigation to implement the revised BRIEF2 self-report measure in this manner. Our correlations showed no uniform associations between depression severity/diagnostic status and performance-based measures, which captured basic attention, inhibition, and cognitive flexibility (i.e., CPT, CATA, or CWIT scores). With the exception of converging evidence on basic/selective attention remaining equal among adolescents with and without depression (Baune et al., 2014; Vilgis et al., 2013; Wagner et al., 2015), the literature on this topic is mixed. When parsing out the specific domains measured with various performance-based tasks, some large-scale reviews failed to find differences in set shifting abilities and inhibition when comparing adolescents and young adults with and without MDD (Baune et al., 2014; Vilgis et al., 2013), whereas meta-analytic data with children and adolescents showed opposite results (Wagner et al., 2015). Contradictory findings are likely, in part, due to sample heterogeneity, such that both clinical and community samples of youth with varying levels of depression and diagnostic comorbidity are often included, as well as the confounding impact of medication on neuropsychological functioning. Lastly, when comparing findings from previous literature using heterogenous age groups, we should note the unique characteristics of our participants, as adolescents may be markedly more self-aware of their emotional states and exhibit greater cognitive self-regulation than do younger children and may exhibit less cognitive control compared to young adult samples (e.g., Casey et al., 2019).
Additionally, we did not find any associations between our EF rating scale (BRIEF2) and performance-based measures, which is generally consistent with the literature (e.g., Bodnar et al., 2007; Stichter et al., 2016) – however, most rating scales examined have typically been limited to parent reports (Kavanaugh et al., 2019) and studies have primarily used ADHD samples (Isquith et al., 2013). Although some researchers have noted a few relationships between the BRIEF and stroop-like tasks (e.g., Anderson et al., 2002), again, parent reports of EF were typically used; adolescents’ perceptions of their own behavioral problems likely capture more socially-based, goal-directed regulation, whereas parent observations may converge more strongly with performance-based tasks of behavioral inhibition. Even investigators finding small correlations between the two types of measures have noted salient differences in the two constructs (Miranda et al., 2015; Toplak et al., 2013), noting that broad EF is a more nuanced estimate of emotional and behavioral responses (Anderson et al., 2002). Indeed, BRIEF scores were strongly associated with social adjustment scores in the current sample, which further supports the ecological validity of the BRIEF and bases the functioning captured in the measure within real-world domains.
Limitations and Future Directions
The primary limitation of the current study is the use of a cross-sectional design, which restricts the predictive interpretation of the results. We conceptualized EF as a functional outcome of depression based on prior literature (e.g., Jeon & Kim, 2015) and we were interested in EF outcomes within our recruited sample of adolescents with depression. Further, notwithstanding that one of the study strengths is the inclusion of a medication-naïve, racially/ethnically diverse sample of adolescents, it should be noted that youth volunteered to participate in a study focusing on depression. A further limit to generalizability, stringent diagnostic and exclusion criteria were implemented, thereby excluding adolescents with ADHD, a condition that has significant overlap with EF difficulties, and those engaging in substance use. Further, participants were not generally representative of the surrounding urban setting, and included significantly more female, Black, and Multiracial adolescents than the general population of Orange County, California (e.g., U.S. Census Bureau, 2019). Comparable to other studies on EF and depression, our convenience sample of community-based participants included youth with varying levels of treatment/diagnostic history for depression. Also, important developmental differences should be considered across the age group of the current sample (13-17 years old); to address this limitation, age was included as a covariate in all models.
Although we conceptualize unpredictability of the home environment as being linked to the development of EF difficulties in adolescence, it is important to note that most QUIC items inquired about experiences occurring throughout childhood, past and present, reports of which may have been influenced by the presence of depressive symptoms. Indeed, variations in how childhood unpredictability is measured, and from whom reports on adolescent problems are obtained, may lead to divergent findings. For instance, such differences in reporters have been found in the literature linking attachment to internalizing behaviors (Madigan et al., 2016). It is also important to account for potential shared-informant bias when interpreting results herein, which were mostly based on self-reports measures (with the exception of clinician-rated depression). Similarly, although QUIC parent unpredictability and BRIEF indices were highly correlated, the specific nature of this link is not well understood, as youth with various dysregulation behaviors may engender poor parenting practices, and vice versa (Halse, 2019). Future investigations should consider implementing longitudinal designs to examine causal relationships and the temporal presentation of symptomology, environmental factors and EF, and simultaneously consider implementing multi-modal assessments to comprehensively capture these interconnected constructs. With respect to additional environmental variables to consider, exploring educational contexts would further our understanding of how supportive or hostile school environments may play a role in the development of EF for these adolescents (e.g., teacher support enhancing student emotional regulation; see Romano et al., 2021). Lastly, as home environment unpredictability and associated internalizing and externalizing problems are overrepresented in adolescent populations with a history of out-of-home placements (e.g., residential care; Muzi & Pace, 2020), who are already vulnerable to disruptions in EF development (Carrera et al., 2019), future research should expand to such high-risk samples.
Supplementary Material
Highlights.
First investigation to examine how unpredictability of home environment moderates the link between depression and executive functioning (EF) in adolescents.
High scores on childhood unpredictability were associated with poor EF for adolescents exhibiting low scores on depression severity.
Adolescents with high depression scores exhibited poor EF regardless of childhood unpredictability.
Methodology contributions include examining associations between self-report and performance-based EF measures.
Early-life environment and parent-child relationships should be assessed to help guide clinical assessment and treatment.
Funding:
This work was supported in part by grants from the National Institutes of Health (NIH) under Grants R01 MH108155, R01 DA040966, and R01 MD010757. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- Ackerman BP, & Brown ED (2010). Physical and psychosocial turmoil in the home and cognitive development. In Evans GW & Wachs TD (Eds.), Decade of behavior (science conference). Chaos and its influence on children's development: An ecological perspective (p. 35–47). American Psychological Association. 10.1037/12057-003 [DOI] [Google Scholar]
- Anderson VA, Anderson P, Northam E, Jacobs R, & Mikiewicz O (2002). Relationships between cognitive and behavioral measures of executive function in children with brain disease. Child Neuropsychology, 8(4), 231–240. 10.1076/chin.8.4.231.13509 [DOI] [PubMed] [Google Scholar]
- Andrews K, Atkinson L, Harris M, & Gonzalez A (2021). Examining the effects of household chaos on child executive functions: A meta-analysis. Psychological Bulletin, 147(1), 16–32. 10.1037/bul0000311 [DOI] [PubMed] [Google Scholar]
- Anonymous (2020). Details omitted for double-blind reviewing.
- Bakker MP, Ormel J, Verhulst FC, & Oldehinkel AJ (2012). Childhood family instability and mental health problems during late adolescence: a test of two mediation models--the TRAILS study. Journal of Clinical Child and Adolescent Psychology, 41(2), 166–176. 10.1080/15374416.2012.651990 [DOI] [PubMed] [Google Scholar]
- Bandura A (1977). Social learning theory. Englewood Cliffs: Prentice-Hall [Google Scholar]
- Baune BT, Fuhr M, Air T, & Hering C (2014). Neuropsychological functioning in adolescents and young adults with major depressive disorder--a review. Psychiatry Research, 218(3), 261–271. 10.1016/j.psychres.2014.04.052 [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, & Erbaugh J (1961). An inventory for measuring depression. Archives of General Psychiatry, 4, 561–571. doi.org/ 10.1001/archpsyc.1961.01710120031004 [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Carbin MG (1988) Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review, 8(1), 77–100. 10.1016/0272-7358(88)90050-5 [DOI] [Google Scholar]
- Bernier A, Beauchamp MH, Carlson SM, & Lalonde G (2015). A secure base from which to regulate: Attachment security in toddlerhood as a predictor of executive functioning at school entry. Developmental Psychology, 51(9), 1177–1189. 10.1037/dev0000032 [DOI] [PubMed] [Google Scholar]
- Best JR, Miller PH, & Naglieri JA (2011). Relations between Executive Function and Academic Achievement from Ages 5 to 17 in a Large, Representative National Sample. Learning and Individual Differences, 21(4), 327–336. 10.1016/j.lindif.2011.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biringer E, Lundervold A, Stordal K, Mykletun A, Egeland J, Bottlender R, & Lund A (2005). Executive function improvement upon remission of recurrent unipolar depression. European Archives of Psychiatry and Clinical Neuroscience, 255(6), 373–380. 10.1007/s00406-005-0577-7 [DOI] [PubMed] [Google Scholar]
- Blair C, Raver CC, Berry DJ, & Family Life Project Investigators (2014). Two approaches to estimating the effect of parenting on the development of executive function in early childhood. Developmental Psychology, 50(2), 554–565. 10.1037/a0033647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodnar LE, Prahme MC, Cutting LE, Denckla MB, & Mahone EM (2007). Construct validity of parent ratings of inhibitory control. Child Neuropsychology, 13(4), 345–362. doi.org/ 10.1080/09297040600899867 [DOI] [PubMed] [Google Scholar]
- Bos M, Peters S, van de Kamp FC, Crone EA, & Tamnes CK (2018). Emerging depression in adolescence coincides with accelerated frontal cortical thinning. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 59(9), 994–1002. 10.1111/jcpp.12895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U, & Evans GW (2000). Developmental science in the 21st century: Emerging questions, theoretical models, research designs and empirical findings. Social Development, 9, 115–125. 10.1111/1467-9507.00114 [DOI] [Google Scholar]
- Carrera P, Jiménez-Morago JM, Román M, & León E (2019). Caregiver ratings of executive functions among foster children in middle childhood: Associations with early adversity and school adjustment. Children and Youth Services Review, 106, 1. 10.1016/j.childyouth.2019.104495 [DOI] [Google Scholar]
- Casey BJ, Giedd JN, & Thomas KM (2000). Structural and functional brain development and its relation to cognitive development. Biological Psychology, 54(1-3), 241–257. 10.1016/s0301-0511(00)00058-2 [DOI] [PubMed] [Google Scholar]
- Casey BJ, Heller AS, Gee DG, & Cohen AO (2019). Development of the emotional brain. Neuroscience letters, 693, 29–34. 10.1016/j.neulet.2017.11.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy J, & Berlin LJ (1994). The insecure/ambivalent pattern of attachment: Theory and research. Child Development, 65(4), 971–981. 10.2307/1131298 [DOI] [PubMed] [Google Scholar]
- Conners CK (2014a). Conners CPT 3 – Conners CATA Manual. Multi-Health Systems: Toronto. [Google Scholar]
- Conners CK (2014b). Conners Continuous Auditory Test of Attention. North Tonawanda, NY: Multi-Health Systems. [Google Scholar]
- Dardas LA, van de Water B, & Simmons LA (2018). Parental involvement in adolescent depression interventions: A systematic review of randomized clinical trials. International Journal of Mental Health Nursing, 27(2), 555–570. 10.1111/inm.12429 [DOI] [PubMed] [Google Scholar]
- Davis EP, Korja R, Karlsson L, Glynn LM, Sandman CA, Vegetabile B, Kataja EL, Nolvi S, Sinervä E, Pelto J, Karlsson H, Stern HS, & Baram TZ (2019). Across continents and demographics, unpredictable maternal signals are associated with children's cognitive function. EBioMedicine, 46, 256–263. 10.1016/j.ebiom.2019.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis EP, Stout SA, Molet J, Vegetabile B, Glynn LM, Sandman CA, Heins K, Stern H, & Baram TZ (2017). Exposure to unpredictable maternal sensory signals influences cognitive development across species. Proceedings of the National Academy of Sciences of the United States of America, 114(39), 10390–10395. 10.1073/pnas.1703444114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delis DC, Kaplan E, and Kramer JH (2001). Delis-Kaplan Executive Function System (DKEFS). San Antonio, TX: The Psychological Corporation. [Google Scholar]
- Diamond A (2006). The early development of executive functions. In Bialystock E & Craik FIM (Eds.), Lifespan Cognition: Mechanisms of change (pp. 70–95). Oxford University Press. [Google Scholar]
- Diamond A (2013). Executive functions. Annual Review of Psychology, 64, 135–168. 10.1146/annurev-psych-113011-143750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatima S, Sheikh H, & Ardila A (2016). Association of parent–child relationships and executive functioning in south Asian adolescents. Neuropsychology, 30(1), 65–74. 10.1037/neu0000216 [DOI] [PubMed] [Google Scholar]
- Fay-Stammbach T, Hawes DJ, & Meredith P (2014). Parenting influences on executive function in early childhood: A review. Child Development Perspectives, 8, 258–264. 10.1111/cdep.12095 [DOI] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. 10.1016/s0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- Fisher PA, Mannering AM, Van Scoyoc A, Graham AM (2013). A translational neuroscience perspective on the importance of reducing placement instability among foster children. Child Welfare, 92(5), 9–36. [PMC free article] [PubMed] [Google Scholar]
- Fowler PJ, Henry DB, & Marcal KE (2015). Family and housing instability: Longitudinal impact on adolescent emotional and behavioral well-being. Social Science Research, 53, 364–374. 10.1016/j.ssresearch.2015.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fulkerson JA, Kubik MY, Story M, Lytle L, & Arcan C (2009). Are there nutritional and other benefits associated with family meals among at-risk youth?. The Journal of Adolescent Health: Official Publication of the Society for Adolescent Medicine, 45(4), 389–395. 10.1016/j.jadohealth.2009.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gioia G, Isquith PK, Guy SC, & Kenworthy L (2015). Behavior rating inventory of executive function, second edition, professional manual. Lutz, FL: Psychological Assessment Resources. [Google Scholar]
- Glynn LM, & Baram TZ (2019). The influence of unpredictable, fragmented parental signals on the developing brain. Frontiers in Neuroendocrinology, 53, 100736. 10.1016/j.yfrne.2019.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glynn LM, Stern HS, Howland MA, Risbrough VB, Baker DG, Nievergelt CM, Baram TZ, & Davis EP (2019). Measuring novel antecedents of mental illness: The Questionnaire of Unpredictability in Childhood. Neuropsychopharmacology, 44(5), 876–882. 10.1038/s41386-018-0280-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonda X, Pompili M, Serafini G, Carvalho AF, Rihmer Z, & Dome P (2015). The role of cognitive dysfunction in the symptoms and remission from depression. Annals of General Psychiatry, 14, 27. 10.1186/s12991-015-0068-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halse M, Steinsbekk S, Hammar Å, Belsky J, & Wichstrøm L (2019). Parental predictors of children's executive functioning from ages 6 to 10. British Journal of Developmental Psychology, 37(3), 410–426. 10.1111/bjdp.12282 [DOI] [PubMed] [Google Scholar]
- Harwood-Gross A, Lambez B, Feldman R, & Rassovsky Y (2020). Perception of caregiving during childhood is related to later executive functions and antisocial behavior in at-risk boys. Frontiers in Psychiatry, 11, 10. 10.3389/fpsyt.2020.00037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henggeler SW, & Schaeffer CM (2016). Multisystemic therapy: Clinical overview, outcomes, and implementation research. Family Process, 55(3), 514–528. 10.1111/famp.12232 [DOI] [PubMed] [Google Scholar]
- Herschell AD, Scudder AB, Schaffner KF, & Slagel LA (2017). Feasibility and effectiveness of parent-child interaction therapy with victims of domestic violence: A pilot study. Journal of Child and Family Studies, 26(1), 271–283. 10.1007/s10826-016-0546-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB (1957). Two Factor Index of Social Position. New Haven, Conn.: Yale University [Google Scholar]
- Hughes CH, & Ensor RA (2009). How do families help or hinder the emergence of early executive function? In Lewis C & Carpendale JIM (Eds.), Social interaction and the development of executive function. New Directions in Child and Adolescent Development, 123, 35–50. [DOI] [PubMed] [Google Scholar]
- Isquith PK, Roth RM, & Gioia G (2013). Contribution of rating scales to the assessment of executive functions. Applied Neuropsychology. Child, 2(2), 125–132. 10.1080/21622965.2013.748389 [DOI] [PubMed] [Google Scholar]
- Jeon SW, & Kim Y (2015). Cognitive impairment in depression. Current Psychiatry Reviews, 11(4), 280–289. 10.2174/1573400511666150831201635 [DOI] [Google Scholar]
- Johnson MH, George P, Armstrong MI, Lyman DR, Dougherty RH, Daniels AS, Ghose SS, & Delphin-Rittmon ME (2014). Behavioral management for children and adolescents: assessing the evidence. Psychiatric Services (Washington, D.C.), 65(5), 580–590. 10.1176/appi.ps.201300253 [DOI] [PubMed] [Google Scholar]
- Kaiser RH, Andrews-Hanna JR, Wager TD, & Pizzagalli DA (2015). Large-scale network dysfunction in major depressive disorder: A meta-analysis of resting-state functional connectivity. JAMA Psychiatry, 72(6), 603–611. doi: 10.1001/jamapsychiatry.2015.0071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karbach J, & Unger K (2014). Executive control training from middle childhood to adolescence. Frontiers in Psychology, 5, 390. 10.3389/fpsyg.2014.00390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend L, Kobak K, Kearney C, Milham M, Andreotti C, Escalera J, … Kaufman, J. (2020). Development of three web-based computerized versions of the kiddie schedule for affective disorders and schizophrenia child psychiatric diagnostic interview: Preliminary validity data. Journal of the American Academy of Child & Adolescent Psychiatry, 59(2), 309–325. 10.1016/j.jaac.2019.05.009 [DOI] [PubMed] [Google Scholar]
- Kavanaugh BC, Cancilliere MK, Fryc A, Tirrell E, Oliveira J, Oberman LM, Wexler BE, Carpenter LL, & Spirito A (2019). Measurement of executive functioning with the national institute of health toolbox and the association to anxiety/depressive symptomatology in childhood/adolescence. Child Neuropsychology, 26(6), 754–769. 10.1080/09297049.2019.1708295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HY (2013). Statistical notes for clinical researchers: Assessing normal distribution (2) using skewness and kurtosis. Restorative Dentistry & Endodontics, 38(1), 52–54. 10.5395/rde.2013.38.1.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson GM, Hook CJ, & Farah MJ (2018). A meta-analysis of the relationship between socioeconomic status and executive function performance among children. Developmental Science, 21(2), 10.1111/desc.12529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lengua LJ, Honorado E, & Bush NR (2007). Contextual risk and parenting as predictors of effortful control and social competence in preschool children. Journal of Applied Developmental Psychology, 28(1), 40–55. 10.1016/j.appdev.2006.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lezak MD, Howieson DB, Loring DW, and Fischer JS (2004). Neuropsychological assessment. New York, NY: Oxford University Press. [Google Scholar]
- Madigan S, Brumariu LE, Villani V, Atkinson L, & Lyons-Ruth K (2016). Representational and questionnaire measures of attachment: A meta-analysis of relations to child internalizing and externalizing problems. Psychological Bulletin, 142(4), 367–399. 10.1037/bul0000029 [DOI] [PubMed] [Google Scholar]
- Marsh S, Dobson R & Maddison R (2020). The relationship between household chaos and child, parent, and family outcomes: a systematic scoping review. BMC Public Health 20(1), 513. 10.1186/s12889-020-08587-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin A, Razza RP, & Brooks-Gunn J (2012). Specifying the links between household chaos and preschool children's development. Early Child Development and Care, 182(10), 1247–1263. 10.1080/03004430.2011.605522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayes TL, Bernstein IH, Haley CL, Kennard BD, & Emslie GJ (2010). Psychometric properties of the Children’s Depression Rating Scale-Revised in adolescents. Journal of Child and Adolescent Psychopharmacology, 20(6), 513–516. 10.1089/cap.2010.0063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNeil CB & Hembree-Kigin TL (2011) Parent-Child Interaction Therapy. 2nd ed. New York, NY: Springer. [Google Scholar]
- Mendenhall AN (2012). Predictors of service utilization among youth diagnosed with mood disorders. Journal of Child and Family Studies, 21(4), 603–611. 10.1007/s10826-011-9512-x [DOI] [Google Scholar]
- Menon M, Katz RC, & Easterbrooks MA (2020). Linking attachment and executive function systems: Exploring associations in a sample of children of young mothers. Journal of Child and Family Studies, 29, 2314–2329. 10.1007/s10826-020-01759-5 [DOI] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, & Swendsen J (2010). Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 49(10), 980–989. 10.1016/j.jaac.2010.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merz EC, McCall RB, & Groza V (2013). Parent-reported executive functioning in postinstitutionalized children: a follow-up study. Journal of Clinical Child and Adolescent Psychology, 42(5), 726–733. 10.1080/15374416.2013.764826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda A, Colomer C, Mercader J, Fernández MI, & Presentación MJ (2015). Performance-based tests versus behavioral ratings in the assessment of executive functioning in preschoolers: associations with ADHD symptoms and reading achievement. Frontiers in Psychology, 6, 545. 10.3389/fpsyg.2015.00545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray L, & Monson K (2013). Youth health, mental health and well-being. In Connolly M & Harms L (Eds.), Social work: Contexts and practice (3rd ed.). Oxford University Press. [Google Scholar]
- Muzi S, & Pace CS (2020). Adolescents in residential-care. Relations among internalizing and externalizing symptoms, attachment, emotion regulation and alexithymia. Psicologia Clinica Dello Sviluppo, 24(1), 117–126. DOI: 10.1449/95801 [DOI] [Google Scholar]
- Niendam TA, Laird AR, Ray KL, Dean YM, Glahn DC, & Carter CS (2012). Meta-analytic evidence for a superordinate cognitive control network subserving diverse executive functions. Cognitive, Affective & Behavioral Neuroscience, 12(2), 241–268. 10.3758/s13415-011-0083-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyongesa MK, Ssewanyana D, Mutua AM, Chongwo E, Scerif G, Newton C, & Abubakar A (2019). Assessing Executive Function in Adolescence: A Scoping Review of Existing Measures and Their Psychometric Robustness. Frontiers in Psychology, 10, 311. 10.3389/fpsyg.2019.00311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh DL, Jerman P, Silvério Marques S, Koita K, Purewal Boparai SK, Burke Harris N, & Bucci M (2018). Systematic review of pediatric health outcomes associated with childhood adversity. BMC Pediatrics, 18(1), 83. 10.1186/s12887-018-1037-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters AT, Ren X, Bessette KL, Goldstein BI, West AE, Langenecker SA, & Pandey GN (2019). Interplay between pro-inflammatory cytokines, childhood trauma, and executive function in depressed adolescents. Journal of Psychiatric Research, 114, 1–10. 10.1016/j.jpsychires.2019.03.030 [DOI] [PubMed] [Google Scholar]
- Poznanski EO & Mokros HB (1996). Children's Depression Rating Scale, Revised (CDRS-R). Western Psychological Services; Los Angeles. [Google Scholar]
- Romano L, Angelini G, Consiglio P, & Fiorilli C (2021). The effect of students’ perception of teachers’ emotional support on school burnout dimensions: Longitudinal findings. International Journal of Environmental Research and Public Health, 18(4), 1922. 10.3390/ijerph18041922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schlomer GL, Bauman S, & Card NA (2010). Best practices for missing data management in counseling psychology. Journal of Counseling Psychology, 57(1), 1–10. 10.1037/a0018082 [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS, Committee on Psychosocial Aspects of Child and Family Health, Committee on Early Childhood, Adoption, and Dependent Care, & Section on Developmental and Behavioral Pediatrics (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232–e246. 10.1542/peds.2011-2663 [DOI] [PubMed] [Google Scholar]
- Sommerfeldt SL, Cullen KR, Han G, Fryza BJ, Houri AK, & Klimes-Dougan B (2016). Executive Attention Impairment in Adolescents With Major Depressive Disorder. Journal of Clinical Child and Adolescent Psychology, 45(1), 69–83. 10.1080/15374416.2015.1072823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sosic-Vasic Z, Kröner J, Schneider S, Vasic N, Spitzer M, & Streb J (2017). The association between parenting behavior and executive functioning in children and young adolescents. Frontiers in Psychology, 8, 472. 10.3389/fpsyg.2017.00472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti CN, Spoor S, Presnell K, & Shaw H (2008). Dissonance and healthy weight eating disorder prevention programs: long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology, 76(2), 329–340. 10.1037/0022-006X.76.2.329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stichter JP, Christ SE, Herzog MJ, O’Donnell RM, & O’Connor KV (2016). Exploring the role of executive functioning measures for social competence research. Assessment for Effective Intervention, 41(4), 243–254. 10.1177/1534508416644179 [DOI] [Google Scholar]
- Su Y, D'Arcy C, Yuan S, & Meng X (2019). How does childhood maltreatment influence ensuing cognitive functioning among people with the exposure of childhood maltreatment? A systematic review of prospective cohort studies. Journal of Affective Disorders, 252, 278–293. 10.1016/j.jad.2019.04.026 [DOI] [PubMed] [Google Scholar]
- Toplak ME, West RF, & Stanovich KE (2013). Practitioner review: Do performance-based measures and ratings of executive function assess the same construct? Journal of Child Psychology and Psychiatry, 54, 131–143. doi: 10.1111/jcpp.12001 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau (2019, July 1). Quick facts: Orange County, California. Retrieved June 2, 2020, from https://www.census.gov/quickfacts/orangecountycalifornia.
- Valcan DS, Davis H, & Pino-Pasternak D (2018). Parental behaviours predicting early childhood executive functions: A meta-analysis. Educational Psychology Review, 30(3), 607–649. 10.1007/s10648-017-9411-9 [DOI] [Google Scholar]
- Vernon-Feagans L, Willoughby M, Garrett-Peters P, & Family Life Project Key Investigators (2016). Predictors of behavioral regulation in kindergarten: Household chaos, parenting, and early executive functions. Developmental Psychology, 52(3), 430–441. 10.1037/dev0000087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilgis V, Silk TJ, & Vance A (2015). Executive function and attention in children and adolescents with depressive disorders: a systematic review. European Child & Adolescent Psychiatry, 24(4), 365–384. doi: 10.1007/s00787-015-0675-7 [DOI] [PubMed] [Google Scholar]
- Visted E, Vøllestad J, Nielsen MB, & Schanche E (2018). Emotion Regulation in Current and Remitted Depression: A Systematic Review and Meta-Analysis. Frontiers in Psychology, 9, 756. 10.3389/fpsyg.2018.00756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner S, Müller C, Helmreich I, Huss M, & Tadić A (2015). A meta-analysis of cognitive functions in children and adolescents with major depressive disorder. European Child & Adolescent Psychiatry, 24(1), 5–19. 10.1007/s00787-014-0559-2 [DOI] [PubMed] [Google Scholar]
- Wang LJ, Lee SY, Tsai CS, Lee MJ, Chou MC, Kuo HC, & Chou WJ (2019). Validity of visual and auditory attention tests for detecting ADHD. Journal of Attention Disorders, 1087054719887433. Advance online publication. 10.1177/1087054719887433 [DOI] [PubMed] [Google Scholar]
- Weissman MM, Orvaschel H, & Padian N (1980). Children's symptom and social functioning self-report scales. Comparison of mothers' and children's reports. The Journal of Nervous and Mental Disease, 168(12), 736–740. 10.1097/00005053-198012000-00005 [DOI] [PubMed] [Google Scholar]
- Zebdi R, Goyet L, Pinabiaux C, & Guellaï B (2016). Psychological disorders and ecological factors affect the development of executive functions: Some perspectives. Frontiers in Psychiatry, 7, 195. 10.3389/fpsyt.2016.00195 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


