Abstract
Background
Esophageal duplication cyst (EDC) is a type of gastrointestinal duplication cyst that involves congenital malformations of the gastrointestinal tract. EDCs are frequently found in the mediastinum and thoracoabdominal region, but rarely occur in the abdominal cavity. However, intra-abdominal EDCs are frequently found in the upper abdomen near the abdominal esophagus. Here, we report, for the first time, a case of intra-abdominal EDC that occurred in the ileum.
Case presentation
A 14-year-old female patient presented to our hospital with complaints of epigastric pain and vomiting. Abdominal computed tomography (CT) revealed a cystic tumor in the pelvis, suspected of ovarian origin. She was admitted to our gynecology department and underwent emergency surgery. The laparoscopic examination revealed that both ovaries were intact and that a primary tumor had developed from the ileal mesentery. Since the patient’s condition was not urgent at the time of the gynecological surgery, the procedure was completed by only performing exploratory laparotomy; the patient was admitted to our department after the surgery. Pelvic magnetic resonance imaging performed on the next day revealed a cystic mass measuring 90 × 65 mm with a smooth margin and homogeneous signal intensity, arising posterior to the uterus. The mass was suspected as an intestinal duplication cyst. On another day, after the examinations were completed, we resected the portion of the small intestine containing the tumor by laparoscopy. The patient had a successful postoperative course and was discharged on the 5th postoperative day. Histological examination showed that the cyst was lined by stratified squamous epithelium, contained esophageal glands, and had a two-layer muscularis propria. Therefore, a diagnosis of intra-abdominal EDC was performed.
Conclusions
An intra-abdominal EDC cyst is relatively rare; this is the first case reported at the distal ileum.
Keywords: Intra-abdominal esophageal duplication cyst, Ileum, Laparoscopic surgery
Background
Esophageal duplication cysts (EDCs) are alimentary duplications and rare congenital malformations [1]. Gastrointestinal duplication is an abnormal development of the gastrointestinal tract involving the formation of spherical or tubular structures either in continuity or adjacent to the gastrointestinal tract [2]. Gastrointestinal duplication frequently occurs in the small and large intestines; however, EDCs occur most commonly near the esophagus. Most reports have described EDCs developing from the cervical to the abdominal esophagus. EDCs rarely occur outside the esophagus and are particularly rare in the upper abdomen (around the pancreas and duodenum) [3, 4].
We encountered a case of an intra-abdominal EDC that occurred at the distal ileum. This is a rare case because the esophageal tissue (which is of foregut origin) was found in the terminal ileum (which is of midgut origin). Embryologically, the esophageal tissue is hypothesized to become an ectopic lesion after invading the ileum during development, as in the ectopic pancreas [5]. In addition, the findings, in this case, are consistent with the histopathological findings, which support the diagnosis of an EDC. Based on the summary of previous literature, this is the first reported case of an EDC occurring at the distal ileum.
Case presentation
A 14-year-old female patient with no significant medical history presented to our hospital with complaints of epigastric pain and vomiting for a few days. Computed tomography (CT) scan showed a tumor in the pelvis. The right ovary was visible rather than in the left ovary. She was admitted to our gynecology department due to a suspected ovarian tumor and underwent emergency surgery. A laparoscopic examination of the pelvic cavity revealed normal ovaries bilaterally and a tumor originating from the ileal mesentery. Since the patient’s condition was not urgent at the time of the gynecological surgery, the procedure was completed by only performing exploratory laparotomy. Subsequently, the patient was referred to our department for a detailed examination. Contrast-enhanced pelvic CT was performed on the next day, which revealed a 90 × 65-mm cystic mass with a smooth margin and internal homogenous density, arising posterior to the uterus. Contrast-enhanced pelvic magnetic resonance imaging (MRI) revealed a mass that showed slightly higher signals than those of water on T1-weighted images and lower signals on T2-weighted images (Fig. 1). In addition, the MRI findings showed no evidence of communication between the cyst and the adjacent intestinal tract. Laparoscopic surgery was performed for a tentative preoperative diagnosis of intestinal duplication. Subsequently, we performed a three-port laparoscopic surgery (Fig. 2). The umbilical port was a 12-mm camera port, and the other two ports were used for handling the forceps. Intraoperative findings revealed a primary cystic tumor of the ileal mesentery in the pelvis, which was soft, elastic, and mobile with no adhesions. Subsequently, the umbilical port wound was extended to a 4-cm small laparotomy incision, and a wound protector (S) was attached. Finally, partial intestinal resection was performed by removing the portion of the small intestine containing the tumor and pulling it out of the abdominal cavity through the small umbilical laparotomy wound (Fig. 3). The excised specimen showed no communication between the cyst and intestinal tract (Fig. 4). Postoperatively, patient symptoms resolved, and her condition was stable; therefore, she was discharged on the 5th postoperative day.
Fig. 1.
Preoperative pelvic magnetic resonance imaging. Preoperative images show a tumor (yellow arrow) that was a cystic mass measuring 90 × 65 mm with a smooth margin and homogeneous signal intensity on the right dorsal side of the uterus (a–d). Coronal image (c), sagittal image (d). T1-weighted images present slightly higher signals than those of water, and T2-weighted images show low signals. No apparent communication was found between the cyst and the intestinal tract
Fig. 2.
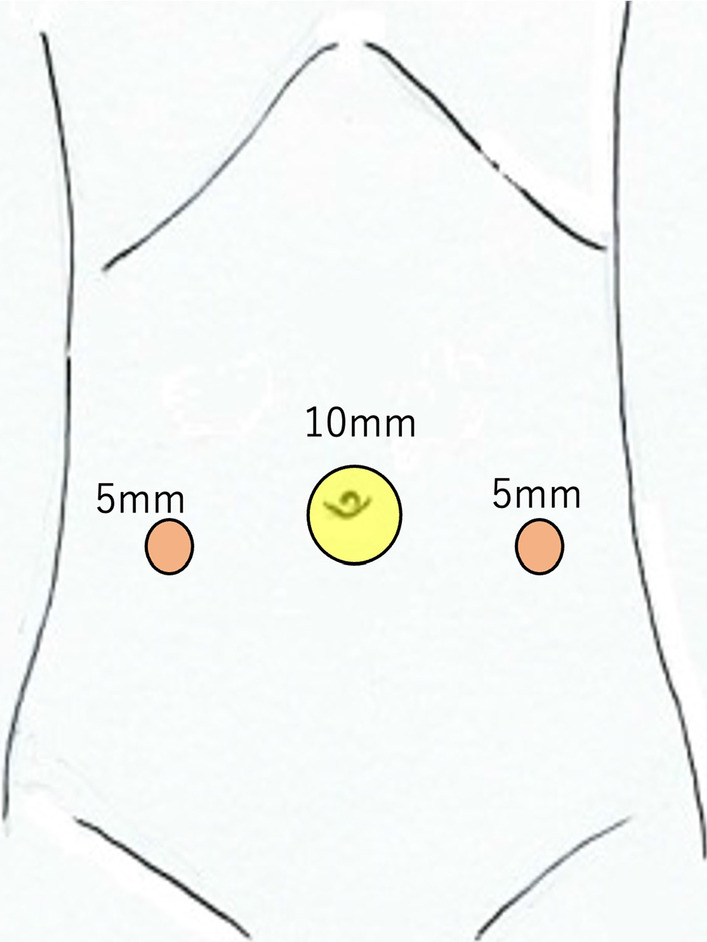
Port site placement. The image shows the three ports of laparoscopic surgery. The umbilical port is a 12-mm camera port (yellow circle), and the bilateral abdomen port is a 5-mm working port for handling the forceps (red circle)
Fig. 3.
Intraoperative laparoscopic view. The image shows a tumor as a lesion that fits into the pelvis (a). The lesion has good mobility without adhesions in the pelvis and can exit the body cavity from the umbilical region (b, c). The cystic tumor was located on the mesenteric side, approximately 40 cm proximal to the distal ileum. The boundary with the adjacent intestinal tract is unclear in the intraoperative findings, and partial resection of the small intestine containing the tumor was performed
Fig. 4.
Extracted specimen. The image shows the specimen at the ileal lumen (a). No change in the lumen and no apparent communication were observed with the cyst. The image shows the lumen of the cyst (b)
Histological examination of the specimen showed that the cyst wall was lined by stratified squamous epithelium (Fig. 5a) and shared the smooth muscle of the intact intestine. Several esophageal glands were also observed (Fig. 5b). In addition, the muscular layer had a two-layer structure—the inner circular and outer longitudinal muscle layers—with nerves and ganglion cells (Auerbach plexus) between the layers. There was no evidence of cytologic epithelial atypia or malignancy, and no cartilage or bone tissue was found. Therefore, the condition was diagnosed as intra-abdominal EDC. The patient was followed up for 5 years postoperatively and was recurrence-free.
Fig. 5.
Histopathological findings. The cystic epithelium appears as stratified squamous epithelium (hematoxylin–eosin [HE], ×100) (a). The esophageal glands are observed in the submucosa, which has mucous glands and ducts (HE, ×100) (b). The muscular layer has a two-layer structure with inner circular and outer longitudinal muscle layers (c). In addition, nerves and ganglion cells (Auerbach plexus, yellow arrow) are found between the two layers (HE, ×100)
Discussion
EDC is an abnormal esophageal development that occurs during the 5th to the 8th gestational weeks when the primitive foregut forms the gastrointestinal tract [4, 6–8]. A previous report showed that EDCs are frequently found in the mediastinum and thoracoabdominal region but rarely in the abdominal cavity and that intra-abdominal EDCs are frequently observed in the upper abdomen near the abdominal esophagus [9]. In contrast, the esophageal tissue was found in the ileum in this case. Various theories exist on the mechanism underlying EDC development [7, 10]. In this case, it is more likely that the esophageal tissue may become an ectopic lesion after invading the ileum during development. A similar condition is an ectopic pancreas, where the pancreatic tissue (which is of foregut origin) is ectopically found in the small intestine (which is of midgut origin) [5].
The pathological criteria for EDCs are as follows [11]: (1) attachment to the esophageal wall, (2) presence of stratified squamous epithelium, and (3) presence of two layers of muscularis propria. According to several reports, the first criterion is not always necessary to diagnose EDCs [3, 4, 9, 12]. However, this case met the second and third criteria. Furthermore, the absence of cartilage and bone tissue led to the diagnosis of EDC. This sporadic case proves that intra-abdominal EDC can occur in the ileum.
There are only 25 reported cases of intra-abdominal EDCs [1–4, 6–10, 12–24], including our case. We have summarized these reports in Table 1. In recent cases, intra-abdominal EDCs occurred in the upper abdomen, except in this case, with a median age of 50 years (range, 1 month to 70 years). This lesion has been reported in 9 men and 16 women. Most cases of intra-abdominal EDCs are asymptomatic; however, symptoms such as epigastric pain and nausea are occasionally present. The median maximum diameter of the tumor is 45 mm. Evidence suggests that as the tumor grows, it causes gastrointestinal obstruction, bleeding, perforation, and abscess formation. The tumor is frequently found on abdominal imaging when examining for abdominal symptoms, and a preoperative diagnosis is rarely performed. Moreover, it is frequently found on postoperative histological examination. Due to recent developments in imaging examinations, abdominal cystic masses can be detected before birth in some cases [24].
Table 1.
Characteristics of 25 published cases of intra-abdominal esophageal duplication cyst (EDC), including our case
| Reference | Age | Sex | Symptom | Location | Maximum tumor size | Treatment | Postoperative hospital day | Recurrence |
|---|---|---|---|---|---|---|---|---|
| Ruffin et al | 38 years | F | Epigastric pain, nausea, and vomiting | Distal esophagus | 40 mm | Laparotomy | N/A | N/A |
| Harvell et al | 57 years | F | Epigastric pain | Pancreas | 22 mm | Laparoscopic resection | N/A | N/A |
| Karahasanoglu et al | 51 years | M | Dysphagia, weight loss, and epigastric pain | Distal esophagus | 110 mm | Laparotomy | 10 | No recurrence |
| Janssen and Fiedler | 56 years | F | Decreased appetite, weight loss | Superior to the left kidney | 80 mm | Biopsy | N/A | N/A |
| Rathaus et al | 5 years | F | Epigastric pain | Distal esophagus | 10 mm | Laparotomy | N/A | N/A |
| Nelms et al | 44 years | M | Low back pain | Distal esophagus | 70 mm | Laparoscopic resection | N/A | N/A |
| Vijayaraghavan et al | 70 years | F | Retching, giddiness, headache | Distal esophagus | 75 mm | Laparotomy | N/A | N/A |
| Noguchi et al | 26 years | F | N/A | Distal esophagus | 40 mm | Laparoscopic resection | 8 | No recurrence |
| Kin et al | 51 years | F | N/A | Distal esophagus | 45 mm | Laparoscopic resection | N/A | N/A |
| Kim et al | 52 years | F | N/A | Distal esophagus | 40 mm | Laparotomy | 9 | No recurrence |
| Martin et al | 60 years | M | Epigastric pain, gastric outlet obstruction | Duodenum | 100 mm | Laparotomy | 3 | No recurrence |
| Martin et al | 50 years | F | Left side flank pain | Pancreas | 65 mm | Laparotomy | N/A | No recurrence |
| Naritaka et al | 57 years | M | Epigastric pain | Distal esophagus | 50 mm | Laparotomy | 16 | No recurrence |
| Aldrink et al | 2 years | M | N/A | Distal esophagus | 30 mm | Laparoscopic resection | 3 | No recurrence |
| Gümüs et al | 18 years | F | Dyspeptic complaints | Distal esophagus | 42 mm | Laparotomy | N/A | N/A |
| Bhamidipati et al | 69 years | M | N/A | Distal esophagus | 44 mm | Laparoscopic resection | 3 | No recurrence |
| Pujar et al | 13 years | F | Epigastric pain and vomiting | Distal esophagus | 50 mm | Laparoscopic resection | 6 | N/A |
| Mori et al | 9 years | M | N/A | Distal esophagus | 22 mm | Laparoscopic resection | 8 | No recurrence |
| Castelijns et al | 20 years | M | Nausea and colic pain | Distal esophagus | 30 mm | Laparoscopic resection | 2 | No recurrence |
| Huang et al | 20 years | F | N/A | Stomach | 138 mm | Laparoscopic resection | 8 | No recurrence |
| Watanabe et al | 50 years | M | Epigastric pain and dysphagia | Distal esophagus | 35 mm | Laparoscopic resection | 10 | No recurrence |
| Khatib et al | 1 week | F | N/A | Distal esophagus | N/A | Laparotomy | N/A | No recurrence |
| Khatib et al | 1 week | F | N/A | Distal esophagus | N/A | No surgery | N/A | N/A |
| Mori et al | 64 years | F | N/A | Distal esophagus | 70 mm | Laparoscopic resection | 9 | No recurrence |
| Ours | 14 years | F | Epigastric pain | Ileum | 90 mm | Laparoscopic resection | 5 | No recurrence |
N/A not applicable
Complete resection of the tumor is the recommended treatment since EDCs may become cancerous [25, 26]. However, depending on the patient’s condition, some cases only require a puncture or biopsy and conservative treatment [12, 24, 27]. In addition, reports of recurrence exist due to the remnants of excision [28]. In our patient, the torsion of an ovarian tumor was suspected; therefore, emergency surgery was performed. Compared to the previously reported epigastric lesions, cystic lesions in the pelvis must be differentiated from gynecological diseases, and emergency surgery must be considered.
Conclusion
This is the first reported case of intra-abdominal EDC occurring in the ileum.
Acknowledgements
We would like to thank Editage (www.editage.com) for the English language editing.
Abbreviations
- CT
Computed tomography
- EDCs
Esophageal duplication cysts
- MRI
Magnetic resonance imaging
- N/A
Not applicable
Author contributions
SO conceived of the case presentation and drafted the manuscript. KT, TN, TT, and TS edited and commented on the manuscript drafts. MM and TN performed surgery and perioperative management. NK diagnosed the pathology of the EDC in this case. TN provided academic consideration. All authors read and approved the final manuscript.
Funding
No funding was obtained from the private or public sector for this research.
Availability of data and materials
The datasets used or analyzed in this study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
All procedures were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its subsequent amendments.
Consent for publication
Written informed consent was obtained from the patient to publish this case report.
Competing interests
The authors declare that they have no competing interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shosaburo Oyama, Email: shooyama0530@gmail.com.
Kenji Tanaka, Email: kenji-tanaka@nsaisei.or.jp.
Masaaki Moriyama, Email: mashamashamorinky5@gmail.com.
Takashi Nonaka, Email: tnonaka@nagasaki-u.ac.jp.
Tetsuro Tominaga, Email: tetsuro.tominaga@nagasaki-u.ac.jp.
Terumitsu Sawai, Email: sawai@nagasaki-u.ac.jp.
Naoe Kinoshita, Email: nkinoshita@nsaisei.or.jp.
Takeshi Nagayasu, Email: nagayasu@nagasaki-u.ac.jp.
References
- 1.Mori M, Shuto K, Hirano A, Kosugi C, Narushima K, Koda K. Laparoscopic surgery for an esophageal duplication cyst using a near-infrared indocyanine green fluorescence system: a case report. Asian J Endosc Surg. 2020;13:211–214. doi: 10.1111/ases.12729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pujar VC, Kurbet S, Kaltari DK. Laparoscopic excision of intra-abdominal oesophageal duplication cyst in a child. J Minim Access Surg. 2013;9:34–36. doi: 10.4103/0972-9941.107137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harvell JD, Macho JR, Klein HZ. Isolated intra-abdominal esophageal cyst. Case report and review of the literature. Am J Surg Pathol. 1996;20:476–479. doi: 10.1097/00000478-199604000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Martin ND, Kim JC, Verma SK, Rubin R, Mitchell DG, Bergin D, et al. Intra-abdominal esophageal duplication cysts: a review. J Gastrointest Surg. 2007;11:773–777. doi: 10.1007/s11605-007-0108-0. [DOI] [PubMed] [Google Scholar]
- 5.Bromberg SH, Camilo Neto C, Borges AF, Franco MI, França LC, Yamaguchi N. Pancreatic heterotopias: clinicopathological analysis of 18 patients. Rev Col Bras Cir. 2010;37:413–419. doi: 10.1590/s0100-69912010000600007. [DOI] [PubMed] [Google Scholar]
- 6.Huang L, Gao S, Dai R, Chen D, Shi H, Song Q, et al. Laparoscopic resection of intra-abdominal esophageal duplication cyst near spleen: a case report. Int J Clin Exp Pathol. 2015;8:2186–2190. [PMC free article] [PubMed] [Google Scholar]
- 7.Kim YW, Sohn TI, Shim HS, Kim CB. Intra-abdominal esophageal duplication cyst in an adult. Yonsei Med J. 2005;46:859–861. doi: 10.3349/ymj.2005.46.6.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Watanobe I, Ito Y, Akimoto E, Sekine Y, Haruyama Y, Amemiya K, et al. Laparoscopic resection of an intra-abdominal esophageal duplication cyst: a case report and literature review. Case Rep Surg. 2015;2015:940768. doi: 10.1155/2015/940768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nelms CD, White R, Matthews BD, Ballinger WE, Jr, Sing RF, Heniford BT. Thoracoabdominal esophageal duplication cyst. J Am Coll Surg. 2002;194:674–675. doi: 10.1016/s1072-7515(02)01164-x. [DOI] [PubMed] [Google Scholar]
- 10.Mori H, Ishibashi H, Sato H, Kuyama H, Asanoma M, Shimada M. Complete laparoscopic surgery for a 9-year-old patient with abdominal esophageal duplication cyst; report of a case. Shikoku Acta Med. 2013;69:251–256. [Google Scholar]
- 11.Arbona JL, Fazzi JG, Mayoral J. Congenital esophageal cysts: case report and review of literature. Am J Gastroenterol. 1984;79:177–182. [PubMed] [Google Scholar]
- 12.Janssen H, Fiedler PN. Isolated intraabdominal esophageal cyst. Am J Roentgenol. 1998;170:389–390. doi: 10.2214/ajr.170.2.9456951. [DOI] [PubMed] [Google Scholar]
- 13.Ruffin WK, Hansen DE. An esophageal duplication cyst presenting as an abdominal mass. Am J Gastroenterol. 1989;84:571–573. [PubMed] [Google Scholar]
- 14.Karahasanoglu T, Ozbal A, Alcicek S, Goksel S, Altun M. Giant intra-abdominal esophageal duplication cyst. Endoscopy. 1997;29:S54–S55. doi: 10.1055/s-2007-1004332. [DOI] [PubMed] [Google Scholar]
- 15.Rathaus V, Feinberg MS. Subdiaphragmatic esophageal duplication cyst in a child. J Clin Ultrasound. 2000;28:264. doi: 10.1002/(sici)1097-0096(200006)28:5<264::aid-jcu10>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 16.Vijayaraghavan R, Belagavi CS. True giant intra-abdominal esophageal cyst. Indian J Gastroenterol. 2002;21:198–199. [PubMed] [Google Scholar]
- 17.Noguchi T, Hashimoto T, Takeno S, Wada S, Tohara K, Uchida Y. Laparoscopic resection of esophageal duplication cyst in an adult. Dis Esophagus. 2003;16:148–150. doi: 10.1046/j.1442-2050.2003.00314.x. [DOI] [PubMed] [Google Scholar]
- 18.Kin K, Iwase K, Higaki J, Yoon HE, Mikata S, Miyazaki M, et al. Laparoscopic resection of intra-abdominal esophageal duplication cyst. Surg Laparosc Endosc Percutan Tech. 2003;13:208–211. doi: 10.1097/00129689-200306000-00013. [DOI] [PubMed] [Google Scholar]
- 19.Naritaka Y, Kuhara K, Shimakawa T, Asaka S, Isohata N, Yamaguchi K, et al. Esophageal duplication cyst with abscessation. Ann Cancer Res Ther. 2009;17:7–10. doi: 10.4993/acrt.17.7. [DOI] [Google Scholar]
- 20.Aldrink JH, Kenney BD. Laparoscopic excision of an esophageal duplication cyst. Surg Laparosc Endosc Percutan Tech. 2011;21:e280–e283. doi: 10.1097/SLE.0b013e31822f1e67. [DOI] [PubMed] [Google Scholar]
- 21.Gümüş M, Önder A, Firat U, Kapan M, Önder H, Gırgın S. Hydatid cyst-like intra-abdominal esophageal duplication cyst in an endemic region. Turk J Gastroenterol. 2011;22:557–558. doi: 10.4318/tjg.2011.0305. [DOI] [PubMed] [Google Scholar]
- 22.Bhamidipati C, Smeds M, Dexter E, Kowalski M, Bazaz S. Laparoscopic excision of gastric mass yields intra-abdominal esophageal duplication cyst. Thorac Cardiovasc Surg. 2013;61:502–504. doi: 10.1055/s-0032-1322617. [DOI] [PubMed] [Google Scholar]
- 23.Castelijns PS, Woensdregt K, Hoevenaars B, Nieuwenhuijzen GA. Intra-abdominal esophageal duplication cyst: a case report and review of the literature. World J Gastrointest Surg. 2014;6:112–116. doi: 10.4240/wjgs.v6.i6.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khatib N, Beloosesky R, Blumenfeld Z, Bronshtein M. Early prenatal diagnosis of intraabdominal esophageal duplication cyst. Ultrasound Obstet Gynecol. 2016;48:796–797. doi: 10.1002/uog.15895. [DOI] [PubMed] [Google Scholar]
- 25.Tapia RH, White VA. Squamous cell carcinoma arising in a duplication cyst of the esophagus. Am J Gastroenterol. 1985;80:325–329. [PubMed] [Google Scholar]
- 26.Dai ZJ, Kang HF, Lin S, Bai MH, Ma L, Min WL, et al. Esophageal cancer with esophageal duplication cyst. Ann Thorac Surg. 2013;96:e15–e16. doi: 10.1016/j.athoracsur.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 27.Will U, Meyer F, Bosseckert H. Successful endoscopic treatment of an esophageal duplication cyst. Scand J Gastroenterol. 2005;40:995–999. doi: 10.1080/00365520510023125. [DOI] [PubMed] [Google Scholar]
- 28.Al-Sadoon H, Wiseman N, Chernick V. Recurrent thoracic duplication cyst with associated mediastinal gas. Can Respir J. 1998;5:149–151. doi: 10.1155/1998/305489. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used or analyzed in this study are available from the corresponding author upon reasonable request.






