Abstract
Introduction
Coronavirus disease is a fatal viral disease caused by severe acute respiratory syndrome coronavirus 2. This study was aimed to assess the attitude, level of COVID-19 vaccine uptake, and its determinants among patients with chronic diseases visiting Debre Tabor Comprehensive Specialized Hospital, Northwest Ethiopia.
Methods
An institutional-based cross-sectional study was conducted among 422 randomly selected patients with chronic disease visiting Debre Tabor Comprehensive Specialized Hospital from February 1 to March 30, 2022. Bivariable and multivariable binary logistic regression analyses were done to identify associations between dependent and independent variables.
Results
Among all participants, only 29.6% of patients were vaccinated with any of the COVID-19 vaccines at least one dose. Age from 31 to 40 years (AOR = 6.26, 95% CI: 2.69–14.56), attended collage and above (AOR = 6.3, 95% CI: 1.37, 28.68), positive attitude towards COVID-19 vaccine (AOR = 9.07, 95% CI: 4.51–18.22), good knowledge (AOR = 7.63, 95% CI: 1.08–16.85), history of COVID-19 (AOR = 4.33, 95% CI: 1.85–10.17), family history of COVID-19 (AOR = 3.99, 95% CI = 1.89–8.48), ever been tested for COVID-19 (AOR = 0.33, 95% CI: 0.15–0.74) were determinant factors for COVID-19 vaccine uptake.
Conclusion
COVID-19 vaccine uptake among patients with chronic disease was very low. The main reasons for not being vaccinated were doubts about vaccine efficacy, the vaccine may cause disease by itself, and fear of adverse effects. Therefore, different stakeholders should enforce vaccine uptake and awareness creation.
Introduction
Coronavirus disease (COVID-19) is highly contagious viral infection caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. SARS-CoV-2 belongs to the family of β-coronavirus which hinders pulmonary gas exchange and triggers cytokine storms. Intense inflammation, hypercoagulation, a drop in lymphocytic count, and an increase in neutrophilic count are observed in the second week after the onset of disease [2]. The clinical spectrum of COVID-19 is broad, ranging from mild flu-like symptoms to severe respiratory problems, organ dysfunction, and death. The symptoms of COVID-19 include fever, dry cough, sneezing, shortness of breath, and respiratory distress. Individuals with weak immunity, old age, diabetes, cardiovascular diseases, and other comorbidities are more susceptible to the attack of coronavirus infection [2, 3]. Since December 2019, COVID-19 has emerged as a major worldwide health threat, causing high rates of morbidity, mortality, serious economic and social impact [1]. The World Health Organization officially declared the spread of the COVID-19 virus as a global pandemic on March 11, 2020 and it is responsible for serious fatalities [4]. The virus has now spread all over the world, and the number of deaths continues to rise at an alarming rate [5]. As of April 21, 2022, it ravaged the world severely, with more than 505,035,185 confirmed cases and 6,210,719 deaths [6].
Among the different preventive measures to stop the spread of coronavirus, social distancing, vaccination, wearing gloves and face masks, and the use of sanitizer plays a vital role [2].
Vaccines are life-saving inventions that have helped to eradicate and control a wide range of infectious diseases. COVID-19 infection can be prevented through vaccination, especially in high-risk groups like healthcare professionals, the elderly, and people with chronic conditions [7]. Vaccination is safe, effective, and it is the most promising strategy to control the COVID-19 pandemic [8]. The vaccine has been shown to minimize infections even among those who have not been vaccinated, through the establishment of herd immunity, which occurs when a large percentage of the population is immunized [9]. Countries around the world may need to make a greater effort in vaccination policies to control the pandemic and resume normal living [10].
Since the end of 2020, several COVID-19 vaccines have been officially approved with emergency use authorization and provided to the population. This includes adenoviral vector (Ad26/Ad5) vaccines of Gamaleya’s Sputnik V (Gam-COVID-Vac) in Russia, Pfizer-BioNTech in the US, Moderna COVID-19 mRNA vaccines in EU, AstraZeneca (AZ) in UK and EU, inactivated Bharat Biotech BBV152 COVAXIN in India, Johnson and Johnson (J&J)/Janssen in the US, Anhui-Zhifei recombinant protein vaccine, Sinopharm, Sinovac and CanSino (adenovirus 5 vector) in China [11]. The common side effects of COVID-19 vaccine are pain at the injection site, fever, headache, tiredness, muscle pain, joint pain, chest pain, dizziness, and chills [12, 13].
Even though a great effort is being made in vaccination, vaccine hesitancy and resistance are continued as a major obstacles to achieve a successful vaccination campaign around the world, with a large section of the population in many countries refusing to be vaccinated against COVID-19 [14, 15]. Questions about a vaccine’s safety and a general lack of confidence, as well as concerns about the vaccine’s efficacy, were the most common reasons for hesitancy [7, 16, 17]. Multiple beliefs and misconceptions among various population groupings can influence acceptance of the COVID-19 vaccination [18]. In low-resource settings, the refusal to take this vaccine is more pronounced [19]. Since March 7, 2021, the Ethiopian Ministry of Health has officially initiated COVID-19 immunization for prioritized populations such as health professionals, the elderly, and patients with chronic diseases above the age of 55. In addition, on November 16, 2021, the Ministry initiated a COVID-19 vaccination program with the goal of vaccinating everyone aged 12 and above. For the campaign, it has distributed over 6.2 million doses of COVID-19 vaccine (Sinopharm, AstraZeneca, Johnson, and Pfizer Biontch). Only the Pfizer Biontch vaccine was provided to individuals aged 12 to 18 years, while the other vaccines were given to those aged 18 years and above across the country. Jansen is given in a single dose and all others are given in two doses where the second dose is administered 3 to 4 weeks after the first dose, except for AstraZeneca where the second dose is given after 6–12 weeks of the first dose [10].
Therefore, understanding the existing level of vaccination and identifying common barriers and facilitators of uptake of the COVID-19 vaccine is crucial for increasing vaccination coverage and reducing COVID-19 cases, hospitalizations, and fatalities.
To our knowledge, there is no prior study on the level of COVID-19 vaccine uptake and determinant factors among patients with chronic disease in the study area. Therefore, this study was aimed to assess the attitude, level of COVID-19 vaccine uptake, and its determinants among patients with chronic diseases visiting Debre Tabor Comprehensive Specialized Hospital, Northwest Ethiopia.
Materials and methods
Study design and setting
An institutional-based cross-sectional study was conducted among 422 patients with chronic disease visiting Debre Tabor Comprehensive Specialized Hospital from February 1 to March 30, 2022. The hospital is located in Debre Tabor town which is the zonal center of South Gondar Zone, Amhara region, Northwest Ethiopia. The town is located 667 km from Addis Ababa and 98 km from Bahir Dar. The hospital serves around 2.2 million population across the region and provides a broad range of medical services for all age groups.
Participants
The source populations were all patients with chronic diseases who had visited Debre Tabor Comprehensive Specialized Hospital. While all patients with chronic diseases who had visited the hospital during the data collection time were study populations.
All patients with chronic diseases who are aged above 18 years and volunteered to participate in the study during the data collection period were included in the study. However, those who did not have the willingness to participate and were critically ill (unable to respond) were excluded.
Study variables
COVID-19 vaccine uptake (yes/no response) was the outcome variable. The independent variables included Sociodemographic (age, sex, ethnicity, religion, occupation, educational status, marital status, and income), health status-related (history of contact with confirmed COVID-19 patients, family history of COVID-19, ever been tested for COVID-19, history of COVID-19 infection, type of chronic diseases), knowledge and attitude towards COVID-19 vaccine.
Sample size determination and sampling technique
The sample size was determined using a single population proportion formula by considering a 95% confidence interval (CI), p = 50% (proportion of vaccination among chronically diseased patients), 5% margin of error, and a 10% non-response rate. The final sample size was 422. Based on the eligibility criteria, a systematic random sampling technique was employed until the necessary samples were obtained.
Operational definitions
COVID-19 vaccine uptake: is the number of people who have received a specified vaccine dose (at least one dose of a COVID-19 vaccine) during the study period. It was assessed by the closed-ended question “Have you been vaccinated with any of the COVID-19 vaccines at least once currently?” and the responses were “Yes” and “No [20].
Attitude to COVID-19 vaccine: The attitude of the respondents was determined based on 8 attitude assessment questions. Respondents who scored greater than or equal to the mean score of attitude assessment questions were considered to have a positive attitude, while those who scored less than the mean score were considered as having a negative attitude towards the COVID-19 vaccine [21, 22].
Knowledge on COVID-19 vaccine: was assessed by six knowledge assessment questions. Participants who scored greater than or equal to the mean score of knowledge assessment questions were considered as having good knowledge, while those who scored less than the mean score were considered as having poor knowledge towards the COVID-19 vaccine [21, 22].
Data collection and quality assurance
The data were collected by five nurse professionals through a face-to-face interview method using the pretested structured questionnaire, which was adapted after reviewing relevant literatures. The questionnaire was prepared first in English and translated into Amharic and then translated back to English to ensure the accuracy of the translated version. The questionnaires included socio-demographic, health status-related, COVID-19 vaccine uptake, and knowledge and attitude towards COVID-19 vaccine-related variables.
Before the actual data collection, a pretest was done on 5% of study participants at Ebinat Primary Hospital. Three days of training were also given for data collectors. Daily supervision was done during the data collection period.
Statistical analysis
After the collected data were checked for completeness, clarity, and accuracy, it was entered into EPI Info version 7.7.1 and then exported to Statistical Package for Social Sciences (SPSS) version 26 for analysis. The characteristics of the study participants were analyzed using descriptive statistics such as frequency and percentage and presented in tables and figure. Both bivariate and multivariate logistic regression analyses were used to explore the association between the dependent and the outcome variable. In the bivariable analysis, variables with p-values of less than 0.2 were entered into multivariable analysis to analyze the association between the outcome variable and predictor variables. Then in multivariable analysis, variables with p-values of less than 0.05 were taken as determinant factors significantly associated with COVID-19 vaccine uptake.
Ethical considerations
The study was conducted after ethical approval was obtained from the ethical review committee of the College of Health Sciences, Debre Tabor University. Written informed consent which was approved by the ethical review committee was obtained from each participant after the purpose and procedure of the study was well explained and their willingness to participate in the study or not was asked. The participants were assured that their responses will remain secured and confidential.
Results
Socio-demographic characteristics of participants
A total of 422 chronically diseased patients of different types were included in the study, with a response rate of 100%. The mean age of participants was 43.2 years (SD-13.7 years) with 29.6% aged between 41 to 50 years. Nearly half (227, 53.8%) of the respondents were males and 109 (25.8%) were government employees. Majority of participants belonged to Amhara, 410 (97.2%) by ethnicity and Orthodox Christian, 358 (84.8%) by religion. Around 173 (41%) participants attended college or above (Table 1).
Table 1. Socio-demographic characteristics of patients with chronic disease visiting Debre Tabor Comprehensive Specialized Hospital, Northwest Ethiopia, 2022.
| Variables | Frequency (%) | |
|---|---|---|
| Age | 18–30 | 90 (21.3%) |
| 31–40 | 104 (24.6%) | |
| 41–50 | 125 (29.6%) | |
| 50 and above | 103 (24.4%) | |
| Sex | Male | 227 (53.8%) |
| Female | 195 (46.2%) | |
| Marital status | Married | 263 (62.3%) |
| Single | 91 (21.6%) | |
| Widowed | 43 (10.2%) | |
| Divorced | 25 (5.9%) | |
| Educational status | No formal education | 46 (10.9%) |
| Primary education | 94 (22.3%) | |
| Secondary education | 109 (25.8%) | |
| Collage and above | 173 (41%) | |
| Occupation | Housewife | 55 (13%) |
| Farmer | 28 (6.6%) | |
| Private employ | 70 (16.6%) | |
| Daily laborer | 39 (9.2%) | |
| Merchant | 85 (20.1%) | |
| Gov’t employs | 109 (25.8%) | |
| Other | 36 (8.5%) | |
| Ethnicity | Amhara | 410 (97.2%) |
| Oromo | 9 (2.1%) | |
| Tigrai | 3 (0.7%) | |
| Religion | Orthodox | 358 (84.8%) |
| Catholic | 9 (2.1%) | |
| Protestant | 37 (8.8%) | |
| Muslim | 18 (4.3%) | |
| Family size | <5 | 308 (73%) |
| ≥5 | 114 (27%) | |
| Monthly income | <5000ETB | 112 (26.5%) |
| 5000-9999ETB | 179 (42.4%) | |
| 10,000-1499ETB | 98 (23.2%) | |
| ≥15,000ETB | 33 (7.8%) | |
| Residence | Rural | 133 (31.5%) |
| Urban | 289 (68.5%) | |
Health-related characteristics of participants
Nearly two-thirds of study participants (288, 68.3%) were five years or above since being diagnosed with the disease. Hypertension (33.4%) was the most commonly reported chronic disease followed by diabetes mellitus (19.9%). About 83 (19.7%) patients had a history of COVID-19 infection and 86 (20.4%) of participants had a family history of COVID-19 infection. Around 138 (32.7%) participants had history of contact with confirmed COVID-19 patients. Of 119 (28.2%) respondents who had been tested for COVID-19, about 43.7% of them had a positive test result. More than half (297, 70.4%) thought that the disease will make them more vulnerable to COVID-19 than non-diseased individuals (Table 2).
Table 2. Health status-related characteristics of patients with chronic disease visiting Debre Tabor Comprehensive Specialized Hospital, Northwest Ethiopia, 2022.
| Variables | Frequency | Percentage | |
|---|---|---|---|
| Duration since diagnosed with the disease | <5 years | 134 | 31.8% |
| 5–10 years | 200 | 47.4% | |
| >10 years | 88 | 20.9% | |
| Type of chronic disease | Hypertension | 141 | 33.4% |
| Diabetes mellitus | 84 | 19.9% | |
| Heart disease | 37 | 8.8% | |
| HIV/AIDS | 41 | 9.7% | |
| Renal disease | 32 | 7.6% | |
| Respiratory disease | 58 | 13.7% | |
| Other* | 29 | 6.9% | |
| History of COVID-19 infection | Yes | 83 | 19.7% |
| No | 339 | 80.3% | |
| Family History of COVID-19 infection | Yes | 86 | 20.4% |
| No | 336 | 67.3% | |
| History of contact with confirmed COVID-19 case | Yes | 138 | 32.7% |
| No | 284 | 67.6% | |
| Tested for COVID-19 infection | Yes | 119 | 28.2% |
| No | 303 | 71.8% | |
| If tested, the test result | Positive | 52 | 43.7% |
| Negative | 67 | 56.3% | |
| The disease makes them more vulnerable to COVID-19 | Yes | 297 | 70.4% |
| No | 125 | 29.6% | |
Knowledge towards COVID-19 vaccine
Less than half 168 (39.8%) of participants had good knowledge towards COVID-19 vaccine. Majority 341 (80.9%) of the respondents correctly replied that COVID-19 vaccines are currently given in Ethiopia. About 172 (40.7%) study participants knew that vaccines are important to prevent COVID-19. Furthermore, 166 (39.3%) participants knew that COVID-19 vaccines are safe for patients with chronic illnesses (Table 3).
Table 3. Knowledge towards COVID-19 vaccine among patients with chronic disease visiting Debre Tabor Comprehensive Specialized Hospital, Northwest Ethiopia, 2022.
| Variables | Response | Frequency (%) |
|---|---|---|
| Do you think that COVID-19 vaccine is currently given in Ethiopia? | Yes | 341 (80.9) |
| No | 81 (19.1) | |
| Do you think vaccines are important to prevent COVID-19? | Yes | 172 (40.7) |
| No | 250 (59.3) | |
| Do you think that the COVID-19 vaccine has side effects or risks? | Yes | 196 (46.4) |
| No | 226 (53.6) | |
| Do you think that COVID-19 vaccines are effective? | Yes | 164 (38.8) |
| No | 258 (61.2) | |
| Do you think patients with chronic disease should be given priority for the vaccine? | Yes | 248 (58.8) |
| No | 274 (41.2) | |
| Do you think the COVID-19 vaccine is safe in patients with chronic illness? | Yes | 166 (39.3) |
| No | 256 (60.7) |
Attitude towards COVID-19 vaccine
Less than half 172 (40.8%) of the respondents had a positive attitude towards the COVID-19 vaccine. Only 36.5% of participants agreed that COVID-19 vaccines are safe, and 39.3% of respondents agreed that COVID-19 vaccination is mandatory for all populations. Similarly, about half (51.7%) of the respondents agreed that the vaccine is accessible to all. Nearly half of the respondents (47.4%) agreed that the vaccine could reduce the spread of the virus in the community (Table 4).
Table 4. Attitude towards COVID-19 vaccine among patients with chronic disease visiting in Debre Tabor Comprehensive Specialized Hospital, Northwest Ethiopia, 2022.
| Variables | Response | Frequency (%) |
|---|---|---|
| COVID-19 can be prevented by the vaccine. | Agree | 247 (58.5) |
| Neutral | 57 (13.5) | |
| Disagree | 118 (28) | |
| The current COVID-19 vaccine is effective. | Agree | 162 (38.4) |
| Neutral | 107 (25.4) | |
| Disagree | 153 (36.3) | |
| COVID-19 vaccine will not be effective in patients with chronic disease. | Agree | 115 (27.3) |
| Neutral | 189 (44.7) | |
| Disagree | 118 (28) | |
| COVID-19 vaccine is safe in patients with chronic illness. | Agree | 154 (36.5) |
| Neutral | 115 (27.3) | |
| Disagree | 153 (36.3) | |
| The information given by official media on COVID-19 vaccine is trustable. | Agree | 209 (49.5) |
| Neutral | 68 (16.1) | |
| Disagree | 142 (33.6) | |
| COVID-19 vaccine can reduce the spread of the virus in the community. | Agree | 200 (47.4) |
| Neutral | 111 (26.3) | |
| Disagree | 111 (26.3) | |
| It is not possible to reduce COVID-19 without vaccination. | Agree | 169 (39.8) |
| Neutral | 78 (18.5) | |
| Disagree | 176 (41.7) | |
| COVID-19 vaccine should be mandatory for all populations. | Agree | 166 (39.3) |
| Neutral | 99 (23.5) | |
| Disagree | 157 (37.2) |
COVID-19 vaccine uptake
Of all study participants, 125 (29.6%) were vaccinated with any of the COVID-19 vaccines at least one dose. Of those participants who took the vaccine (n = 125), 39 (31.2%) had received the vaccine in the first round. Majority of the respondents had no symptoms after vaccination. However, 40% of respondents had symptoms after vaccination: the main symptoms reported were fever (56.3%), chills (10%), and headache (18%).
Reasons for not being vaccinated COVID-19 vaccine
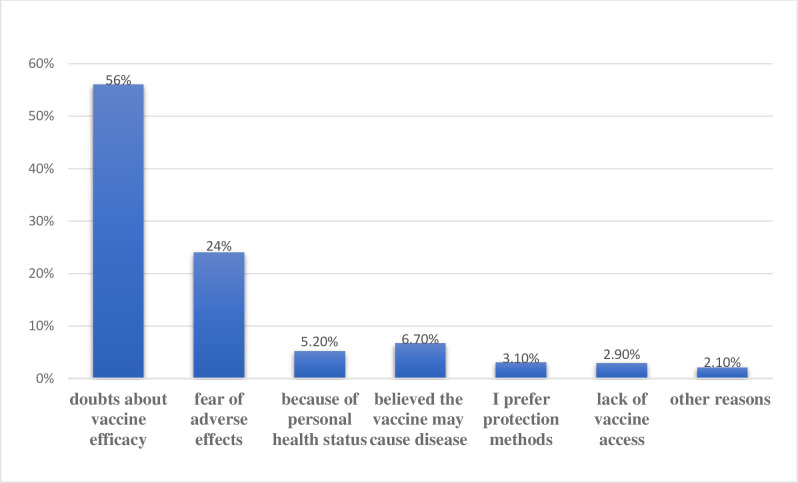
The main reasons for not receiving the vaccine were 166 (56%) doubts about vaccine efficacy, 72 (24%) fear of adverse effects, 20 (6.7%) believed the vaccine may cause disease by itself, 16 (5.2%) unable to withstand the vaccine because of an underlying chronic disease, and 9 (3.1%) prefer other non-vaccine preventive measures (Fig 1).
Fig 1. Respondents’ main reason for not being vaccinated in patients with chronic disease, 2022.
Determinant factors of COVID-19 vaccine uptake
In multivariable binary logistic regression analysis, variables such as age, educational status, history of COVID-19 infection, family history of COVID-19, ever been tested for COVID-19, knowledge, and attitude towards COVID-19 vaccine were statistically associated with COVID-19 vaccine uptake. However, some variables such as religion, ethnicity, marital status and residence, types of chronic disease, income, and family sizes were excluded because their p-value was >0.2 on binary logistic regression analysis.
Patients aged from 31 to 40 years were 6.3 times more likely to uptake COVID-19 vaccine (AOR = 6.26, 95% CI: 2.69–14.56) and younger age (18–30 years) patients were 4.47 times (AOR = 4.47, 95% CI: 1.74–11.5) more likely to get vaccinated than older age groups. Patients who had a positive attitude towards the COVID-19 vaccine were 9 times more likely to uptake the COVID-19 vaccine (AOR = 9.07, 95% CI: 4.51–18.22) than those who had a negative attitude. The likelihood of receiving the COVID-19 vaccine was 7.63 times (AOR = 7.63, 95% CI: 1.08–16.85) higher in those patients with chronic diseases who had good knowledge about the vaccine than in those who had poor knowledge. Those who had a history of COVID-19 infection were 4.33 times (AOR = 4.33, 95% CI: 1.85–10.17) more likely to uptake the COVID-19 vaccine than those who had no history of COVID-19 infection. Participants who had a family history of COVID-19 were 4 times more likely to uptake COVID-19 vaccine (AOR = 3.99, 95% CI: 1.89–8.48) compared to those who had no family history of COVID-19. The probability of COVID-19 vaccine uptake by those who had been tested for COVID-19 was reduced by 32.9% (AOR = 0.329, 95% CI: 0.15–0.74) compared to those who had never been tested for COVID-19 (Table 5).
Table 5. Determinant factors of COVID-19 vaccine uptake among patients with chronic disease visiting Debre Tabor Comprehensive Specialized Hospital, Northwest Ethiopia, 2022.
| Variables | COVID-19 vaccine uptake | COR (95%CI) | AOR (95%CI) | P-value | |
|---|---|---|---|---|---|
| Yes (%) | No (%) | ||||
| Age | |||||
| 18–30 | 30 (33.3%) | 60 (66.7%) | 3.18 (1.56–6.49) | 4.47 (1.74–11.50) | 0.00* |
| 31–40 | 44 (42.3%) | 60 (57.7%) | 4.66 (2.35–9.25) | 6.26 (2.69–14.56) | 0.02* |
| 41–50 | 37 (29.6%) | 88 (70.4%) | 2.67 (1.35–5.29) | 3.87 (1.59–9.43) | 0.003* |
| 50 and above | 14 (13.6%) | 89 (86.4%) | 1 | 1 | |
| Sex | |||||
| Male | 25 (25.1%) | 170 (74.9%) | 1 | 1 | |
| Female | 68 (34.9%) | 127 (65.1%) | 1.6 (1.04–2.44) | 1.56 (0.81–7.86) | 0.23 |
| Educational status | |||||
| No formal education | 5 (10.9%) | 41 (89.1%) | 1 | 1 | |
| Primary education | 32 (34%) | 62 (66%) | 4.23 (1.52–11.76) | 4.84 (1.29–18.04) | 0.01* |
| Secondary education | 34 (31.2%) | 75 (68.8%) | 3.71 (1.35–10.23) | 3.11 (1.06–11.83) | 0.04* |
| Collage and above | 54 (31.2%) | 119 (68.8%) | 3.72 (1.39–9.94) | 2.77 (1.09–10.01) | 0.01* |
| Duration since diagnosed with the disease | |||||
| <5 years | 46 (34.3%) | 88 (65.7%) | 1 | 1 | |
| 5–10 years | 51 (25.5%) | 149 (74.5%) | 0.65 (0.41–1.06) | 0.58 (0.30–1.15) | 0.12 |
| >10 years | 28 (31.8%) | 60 (68.2%) | 0.89 (0.0.5–1.58) | 0.51 (0.21–1.21) | 0.13 |
| Attitude towards COVID-19 vaccine | |||||
| Positive | 99 (57.6%) | 73 (42.4%) | 7.97 (4.61–13.76) | 9.07 (4.51–18.22) | 0.000** |
| Negative | 26 (10.4%) | 224 (89.6%) | 1 | 1 | |
| Knowledge towards COVID-19 vaccine | |||||
| Good | 102 (60.7%) | 66 (39.3%) | 7.04 (1.68–16.85) | 7.63 (1.08–16.85) | 0.000** |
| Poor | 23 (9.1%) | 231 (90.9%) | 1 | 1 | |
| History of COVID-19 infection | |||||
| Yes | 47 (56.6%) | 36 (43.4%) | 4.37 (2.64–2.43) | 4.33 (1.85–10.17) | 0.001* |
| No | 78 (23%) | 261 (77%) | 1 | 1 | |
| Family History of COVID-19 infection | |||||
| Yes | 50 (58.1%) | 36 (41.9%) | 4.83 (2.93–7.96) | 3.99 (1.89–8.48) | 0.0001** |
| No | 75 (22.3%) | 261 (77.7%) | 1 | 1 | |
| Ever been test for COVID-19 | |||||
| Yes | 70 (58.8%) | 49 (41.2%) | 2.09 (1.33–3.27) | 0.33 (0.15–0.74) | 0.007* |
| No | 76 (25.1%) | 227 (74.9%) | 1 | 1 | |
*P-value<0.05,
**P-value<0.001, COR- Crude odds ratio, AOR- Adjusted odds ratio, CI-Confidence interval
Discussion
The COVID-19 pandemic has become a major public health concern, resulting in high morbidity and mortality. The likelihood of acquiring hazardous COVID-19 symptoms is higher in high-risk population groups, such as people with chronic illnesses [23, 24]. Hence, priority access to the COVID-19 vaccine should be offered to these higher-risk populations.
About 83 (19.7%) of study participants have been infected with COVID-19, which is consistent with a study conducted among cancer patients in Addis Ababa [25]. In this study, 125 (29.6%) patients with chronic disease were vaccinated for COVID-19 at least once. This finding was significantly higher than the result reported from Addis Ababa (14.5%) [25]. However, it was lower than the study findings in China (84.22%) [26], France (69%) [27], Ontario, Canada (81.6%) [28], US (57%) [29], Harar region, Ethiopia (39.4%) [30], and Pennsylvania (59.3%) [31]. This discrepancy could be attributed to the study subjects being the general public, differences in awareness among the population groups, and easier access to information.
In this study, less than half (39.8%) of the patients had good knowledge towards the COVID-19 vaccine which was inline with the finding in Ethiopia (40.8%) [22]. However, it was lower than the finding reported from Dessie Comprehensive Specialized Hospital (62.7%) [21]. This low level of knowledge towards the vaccine may be attributed to the change in the target population, educational status, and use of different sources of information towards COVID-19 vaccines. About 40.8% of the participants had a positive attitude towards the vaccine which was higher than the finding in Ethiopia (24.2%) [22] but lower than the findings in Dessie Comprehensive Specialized Hospital (71.6%) [21] and China (70.07%) [26]. The possible reason for this variation may be due to the poor risk perception towards COVID-19.
Age, educational status, history of COVID-19 infection, ever been tested for COVID-19, family history of COVID-19, knowledge, and attitude toward COVID-19 vaccine were all found to be determinants of COVID-19 vaccine uptake in this study. COVID-19 vaccine uptake was also observed to be higher among younger and middle-aged patients with chronic disease (18–30, 31–40, and 41–50) compared to older patients with chronic disease (50 and above years). This is consistent with a study conducted in Addis Ababa [25]. However, it is incontrary to a study in US, which found that COVID-19 vaccination was highest in older adults [29].
In our study, patients who attended college and above were 2.77 times more likely to be vaccinated than those with no education. This is inconsistent with a study in the Harar region, Ethiopia [30] where people who had no schooling were 2.5 times more likely to be vaccinated than people who had attended above-secondary school. This could be due to the fact that educated people are more likely to accept the recommended vaccine.
Respondents with a history of COVID-19 infection were three times more likely than those without a history of COVID-19 illness to take the COVID-19 vaccine. In contrast, respondents with a history of COVID-19 infection were less likely to be vaccinated in research conducted in France [27].
Furthermore, participants with a good attitude toward a COVID-19 vaccine were 9 times more likely to get vaccinated, which was consistent with the data from Addis Ababa [25] and Dessie [21], which found that patients with a positive attitude were more likely to accept the vaccine. This was also true in Ethiopia [22] and China [26] where respondents who had a positive attitude towards the COVID-19 vaccine were more likely to uptake it. The possible reason might be a positive attitude toward COVID-19 vaccine may avoid misinformation regarding the vaccine and outweigh its importance and then encourage people to be vaccinated.
Doubts about vaccine efficacy (56%) and fear of adverse effects (24%) were the most common reasons for not being vaccinated, while in China the unvaccinated population (23.91%) is primarily due to personal health status [26]. A consistent finding was obtained from a study conducted among cancer patients in Addis Ababa where 84.4% of them had concerns about the safety and side effects of the vaccine [25].
The study has the following limitations: firstly, it was a cross-sectional study in which the identification of causal factors may be very difficult, and secondly, it is hard to follow up the future behaviors of those who have not been vaccinated.
Conclusion
The study revealed that COVID-19 vaccine uptake (29.6%) among patients with chronic illness was still low. Age, educational status, history of COVID-19 infection, ever been tested for COVID-19, family history of COVID-19, knowledge and attitude towards COVID-19 vaccine were all determinant factors that influence COVID-19 vaccine uptake among patients with chronic disease in Ethiopia. Doubts about vaccine efficacy, the vaccine may cause disease by itself, and fear of adverse effects were the primary reasons for not being vaccinated.
As a result, decision-makers and health managers should update and devise strategies to ensure COVID-19 vaccination uptake in conjunction with various stakeholders. The South Gondar Zone Health Bureau should continue to raise awareness about the safety, importance, and efficacy of the COVID-19 vaccine.
Data Availability
All relevant data are within the paper.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Kanyike AM, Olum R, Kajjimu J, Ojilong D, Akech GM, Nassozi DR, et al. Acceptance of the coronavirus disease-2019 vaccine among medical students in Uganda. Tropical medicine and health. 2021;49(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Noureen S, Rehman K, Akash H. Natural immunity boosters as therapeutic interventions in the era of COVID-19 pandemic. Endocrine, metabolic & immune disorders drug targets. 2022. [DOI] [PubMed] [Google Scholar]
- 3.Qureshi QH, Ashraf T, Rehman K, Khosa MK, Akash MSH. Therapeutic interventions of remdesivir in diabetic and nondiabetic COVID‐19 patients: a prospective observational study conducted on Pakistani population. Journal of Medical Virology. 2021;93(12):6732–6. doi: 10.1002/jmv.27256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cucinotta D, Vanelli M. WHO Declares COVID-19 a Pandemic. Acta bio-medica: Atenei Parmensis. 2020;91(1):157–60. doi: 10.23750/abm.v91i1.9397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sim MR. The COVID-19 pandemic: major risks to healthcare and other workers on the front line. Occupational and environmental medicine. 2020;77(5):281–2. doi: 10.1136/oemed-2020-106567 [DOI] [PubMed] [Google Scholar]
- 6.WHO. Coronavirus Disease (COVID-19) Dashboard. Accessed January 1, 2022.
- 7.Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public health. 2021;194:245–51. doi: 10.1016/j.puhe.2021.02.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tavilani A, Abbasi E, Ara FK, Darini A, Asefy Z. COVID-19 vaccines: Current evidence and considerations. Metabolism open. 2021;12:100124. doi: 10.1016/j.metop.2021.100124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes toward a potential SARS-CoV-2 vaccine: a survey of US adults. Annals of internal medicine. 2020;173(12):964–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Africa W. Ethiopia launches a COVID-19 vaccination campaign targeting the 12 years and above population. November 25, 2021. [Google Scholar]
- 11.Shao Y, Wu Y, Feng Y, Xu W, Xiong F, Zhang X. SARS-CoV-2 vaccine research and immunization strategies for improved control of the COVID-19 pandemic. Frontiers of medicine. 2022:1–11. doi: 10.1007/s11684-021-0913-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Oriji PC, Allagoa DO, Obagah L, Oguche OI, Ohaeri OS, Tekenah ES, et al. Side effect profile of COVID-19 vaccine among health workers in a tertiary health Institution in South-South Nigeria. European Journal of Medical and Health Sciences. 2021;3(3):59–64. [Google Scholar]
- 13.Food U. Drug Administration. Pfizer-BioNTech COVID-19 Vaccine. FDA; 2021.
- 14.Green MS, Abdullah R, Vered S, Nitzan D. A study of ethnic, gender and educational differences in attitudes toward COVID-19 vaccines in Israel–implications for vaccination implementation policies. Israel Journal of Health Policy Research. 2021;10(1):26. doi: 10.1186/s13584-021-00458-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaadan MI, Abdulkarim J, Chaar M, Zayegh O, Keblawi MA. Determinants of COVID-19 vaccine acceptance in the Arab world: a cross-sectional study. Global Health Research and Policy. 2021;6(1):1–7. doi: 10.1186/s41256-021-00202-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fares S, Elmnyer MM, Mohamed SS, Elsayed R. COVID-19 Vaccination Perception and Attitude among Healthcare Workers in Egypt. 2021;12:21501327211013303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dereje N, Tesfaye A, Tamene B, Alemshet D, Abe H, Tesfa N, et al. COVID-19 vaccine hesitancy in Addis Ababa, Ethiopia: a mixed-methods study. MedRxiv. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Green MS, Abdullah R, Vered S, Nitzan D. A study of ethnic, gender and educational differences in attitudes toward COVID-19 vaccines in Israel—implications for vaccination implementation policies. Israel journal of health policy research. 2021;10(1):26. doi: 10.1186/s13584-021-00458-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mannan DKA, Farhana KM. Knowledge, attitude and acceptance of a COVID-19 vaccine: a global cross-sectional study. International Research Journal of Business and Social Science. 2020;6(4). [Google Scholar]
- 20.WHO. Behavioural considerations for acceptance and uptake of COVID-19 vaccines: WHO technical advisory group on behavioural insights and sciences for health meeting report. October 15, 2020.
- 21.Berihun G, Walle Z, Berhanu L, Teshome D. Acceptance of COVID-19 vaccine and determinant factors among patients with chronic disease visiting Dessie Comprehensive Specialized Hospital, Northeastern Ethiopia. Patient preference and adherence. 2021;15:1795. doi: 10.2147/PPA.S324564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mesesle M. Awareness and attitude towards COVID-19 vaccination and associated factors in ethiopia: cross-sectional study. Infection and Drug Resistance. 2021;14:2193. doi: 10.2147/IDR.S316461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.CDC. Certain Medical Conditions and Risk for Severe COVID-19 Illness; 2020. Available from: https://wwwcdcgov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditionshtml. Accessed April 15, 2022.
- 24.Gimeno-Miguel A, Bliek-Bueno K, Poblador-Plou B, Carmona-Pírez J, Poncel-Falcó A, González-Rubio F, et al. Chronic diseases associated with increased likelihood of hospitalization and mortality in 68,913 COVID-19 confirmed cases in Spain: A population-based cohort study. Plos one. 2021;16(11):e0259822. doi: 10.1371/journal.pone.0259822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Admasu FT. Knowledge and Proportion of COVID-19 Vaccination and Associated Factors Among Cancer Patients Attending Public Hospitals of Addis Ababa, Ethiopia, 2021: A Multicenter Study. Infection and Drug Resistance. 2021;14:4865. doi: 10.2147/IDR.S340324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kong Y, Jiang H, Liu Z, Guo Y, Hu D. The Uptake and Vaccination Willingness of COVID-19 Vaccine among Chinese Residents: Web-Based Online Cross-Sectional Study. Vaccines. 2022;10(1):90. doi: 10.3390/vaccines10010090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Belmin J, Lutzler P, Hidoux P, Drunat O, Lafuente-Lafuente C. First-Dose Coronavirus 2019 Vaccination Coverage among the Residents of Long-Term Care Facilities in France. Gerontology. 2021:1–5. doi: 10.1159/000517793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shariff SZ, Richard L, Hwang SW, Kwong JC, Forchuk C, Dosani N, et al. COVID-19 vaccine coverage and factors associated with vaccine uptake among 23 247 adults with a recent history of homelessness in Ontario, Canada: a population-based cohort study. The Lancet Public Health. 2022;7(4):e366–e77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Diesel J, Sterrett N, Dasgupta S, Kriss JL, Barry V, Esschert KV, et al. COVID-19 vaccination coverage among adults—United States, December 14, 2020–May 22, 2021. Morbidity and Mortality Weekly Report. 2021;70(25):922. doi: 10.15585/mmwr.mm7025e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alemayehu A, Yusuf M, Demissie A, Abdullahi Y. Determinants of COVID-19 vaccine uptake and barriers to being vaccinated among first-round eligibles for COVID-19 vaccination in Eastern Ethiopia: A community based cross-sectional study. SAGE Open Medicine. 2022;10:1177. doi: 10.1177/20503121221077585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krebs NM, D’Souza G, Bordner C, Allen SI, Hobkirk AL, Foulds J, et al. COVID-19 Vaccination Uptake and Hesitancy Among Current Tobacco Users. Tobacco use insights. 2021;14:1179173. doi: 10.1177/1179173X211068027 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.