Abstract
Macrophages in atherosclerotic lesions promote plaque progression and are an attractive therapeutic target in cardiovascular research. Here we present a protocol for synthesis of small interfering RNA (siRNA) nanoparticles (NP) that target lesional macrophages as a potential treatment for atherosclerosis. Ca2+/calmodulin-dependent protein kinase γ (CaMKIIγ) activity in macrophages of advanced human and mouse atherosclerotic plaques drives necrosis via down-regulating the expression of the efferocytosis receptor MerTK. Therefore, selective inhibition of CaMKIIγ in lesional macrophages holds great promise for the treatment of advanced atherosclerosis. We have recently developed a siRNA NP platform that can selectively silence CaMKIIγ in macrophages, resulting in increased plaque stability. We provide a detailed protocol for the synthesis of NP components, the preparation and characterization (physicochemical and in vitro) of siRNA NPs, and the evaluation of in vivo therapeutic effects of siRNA NPs and their biocompatibility in atherosclerotic mice. Our siRNA-loaded polymer-lipid hybrid NPs are constructed via a robust self-assembly method, exhibiting excellent in vivo features for systemic siRNA delivery. Following this protocol, it takes 3-5 d to prepare the siRNA NPs, 8-10 d to characterize the NPs, and 4-5 weeks to evaluate their therapeutic effects in established atherosclerotic mice. By changing the RNA molecules loaded in the NPs, lesional macrophages can be targeted for the exploration and validation of new targets/pathways in atherosclerosis.
Introduction
Macrophage activation has been implicated in the pathogenesis of many human diseases, including atherosclerosis, obesity, diabetes, cancer, and skin diseases.1 Among them, atherosclerosis, an inflammatory disease involving arterial plaque deposition which increases the risk of cardiovascular disease and stroke, is highly correlated with macrophage activation.2,3 Therefore, inhibiting the activation of pro-atherogenic pathways in macrophages holds great promise for the treatment of atherosclerotic vascular diseases.4 However, to date, only suboptimal therapeutic effects have been achieved due to the lack of therapeutics or treatments with high specificity and efficacy.
RNA interference (RNAi) is a powerful method capable of selectively silencing any gene of interest, showing great potential to treat various diseases.5-10 The success of RNAi therapy largely depends on the efficient in vivo delivery of therapeutic small interfering RNA (siRNA) to the target cells. To reach the RNAi machinery in the cytoplasm, siRNA molecules need to overcome several physiological barriers, including being degraded by nucleases, being rapidly cleared by the mononuclear phagocyte system (MPS) or renal filtration,11 poor cellular uptake, and inefficient endosomal escape.8 Although the rapid development of siRNA technology has yielded relatively stable siRNA with reduced side effects through chemical modification and sequence optimization,12-14 the efficient delivery of siRNA into target cells is still challenging. Therefore, it is highly desirable to develop a safe and efficient delivery vehicle that can protect the siRNA from enzymatic degradation, deliver it to target cells and facilitate its cellular uptake and endosomal escape.
To this end, various delivery systems have been developed for more effective delivery of siRNA.15 Many of them have been investigated in clinical trials for the treatment of different diseases, including cancer, genetic disorders, fibrosis, hypercholesterolemia, and viral infections.16 The research interests of the scientific community in siRNA-based therapy have been fueled by the first U.S. Food and Drug Administration (FDA)-approved nano-formulated siRNA drug (Patisiran, Alnylam Pharmaceuticals), treating a rare genetic disorder.17 Although several polymeric or lipid nanoparticle (NP)-based siRNA delivery systems have been developed for the treatment of vascular diseases,18-24 siRNA-based therapy via targeting macrophages in atherosclerotic lesions for atherosclerosis treatment is still in its infancy. It is worth mentioning that Leuschner et al. pioneered the siRNA-based therapy using cationic lipid NPs for in vivo treatment of atherosclerosis via targeting macrophages.25 While these polymeric or lipid NP-based systems have shown satisfying therapeutic effects, they might not be applicable in the treatments where higher gene therapy efficacy are required. Therefore, novel strategies which can further enhance the protection of siRNA and prolong its in vivo circulation time are needed.
Development of the Protocol
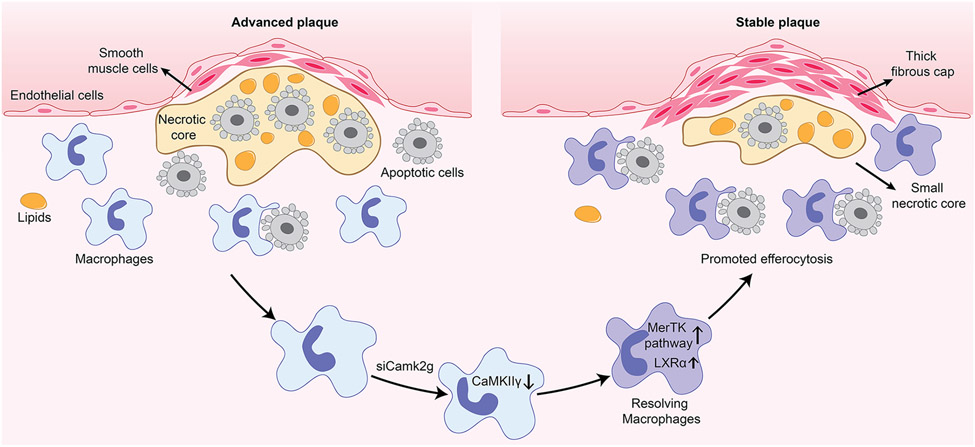
To address outstanding limitations in nucleic acid delivery to macrophages, we developed a macrophage-targeting siRNA NP platform for the treatment of atherosclerosis via selectively silencing a functional gene in macrophages of atherosclerotic lesions.26 The macrophage gene Camk2g, encoding a calcium-activated kinase named CaMKIIγ (Ca2+/calmodulin-dependent protein kinase γ), was chosen as the target based on our previous work. We demonstrated that the activation of lesional macrophage CaMKIIγ in advanced human and mouse atherosclerotic plaques was a major stimulus for the formation of necrotic lesions covered with thin fibrous caps27. Efferocytosis is a specialized phagocytic process for the removal of dead cells.28 Mechanistic studies revealed that the CaMKIIγ suppresses the activation of transcription factor 6 (ATF6)/liver X receptor alpha (LXRα)/c-Mer proto-oncogene tyrosine kinase (MerTK) pathway that usually promotes the efferocytosis. Consequently, the inefficient efferocytosis causes uncleared cells secondary necrosis, which eventually results in plaque necrosis and fibrous cap thinning (Fig. 1).27 Thin-capped, necrotic lesions destabilize the plaques in humans, leading to harmful consequences such as plaque rupture, acute luminal thrombosis, and various acute atherothrombotic vascular events.29
Fig. 1. Schematic of CaMKIIγ-mediated plaque stability.
The introduction of siCamk2g into the macrophages silences CaMKIIγ, resulting in the activation of the MerTK pathway which further enhances efferocytosis. The increased efferocytosis leads to a decrease in plaque necrosis and fibrous cap thinning, which synergistically improve the plaque stability.26,27
Our siRNA NPs are rationally designed and constructed. First, a cationic lipid is used to complex the siRNA via electrostatic interactions. Then, a hydrophobic poly(lactic-co-glycolic) acid (PLGA) polymer further interacts with the siRNA/cationic lipid complex via hydrophobic interactions, followed by PEGylation of the complex using lipid-polyethylene glycol (lipid-PEG), yielding the siRNA NPs. To enable the targeted delivery of siRNA to macrophages, the macrophage-targeting peptide ligand S2P is conjugated to the siRNA NPs through the lipid-PEG. In a fat-fed Ldlr−/− mouse model with established atherosclerosis, the administration of the S2P-siCamk2g NPs can silence the CaMKIIγ of the lesional macrophage and subsequently enhance efferocytosis, resulting in thicker fibrous cap and less atherosclerotic plaque necrosis. Through this formulation, we developed a promising siRNA NP platform for the treatment of atherosclerosis via genetic manipulation of a specific molecule in lesional macrophages, providing a new therapeutic strategy for atherosclerosis and other-related vascular diseases.
Here we outline the procedures for the preparation and characterization of siRNA NPs, and the evaluation of in vivo therapeutic effects of siRNA NPs in atherosclerotic mice. The NP components cationic lipid (G0-C14) and peptide-modified lipid-PEG (DSPE-PEG-S2P) can be easily synthesized by a one-step reaction. The siRNA-loaded polymer-lipid hybrid NPs are conveniently achieved by dropwise addition of the siRNA complex into the lipid-PEG aqueous solution at room temperature (25 °C). After quick purification by ultrafiltration, the resulting siRNA NPs can be readily used for in vitro and in vivo evaluation of gene silencing efficiency and therapeutic effects for atherosclerosis. We anticipate that these procedures will be instrumental for researchers seeking to build siRNA delivery systems to treat atherosclerosis and other diseases.
Overview of the procedure
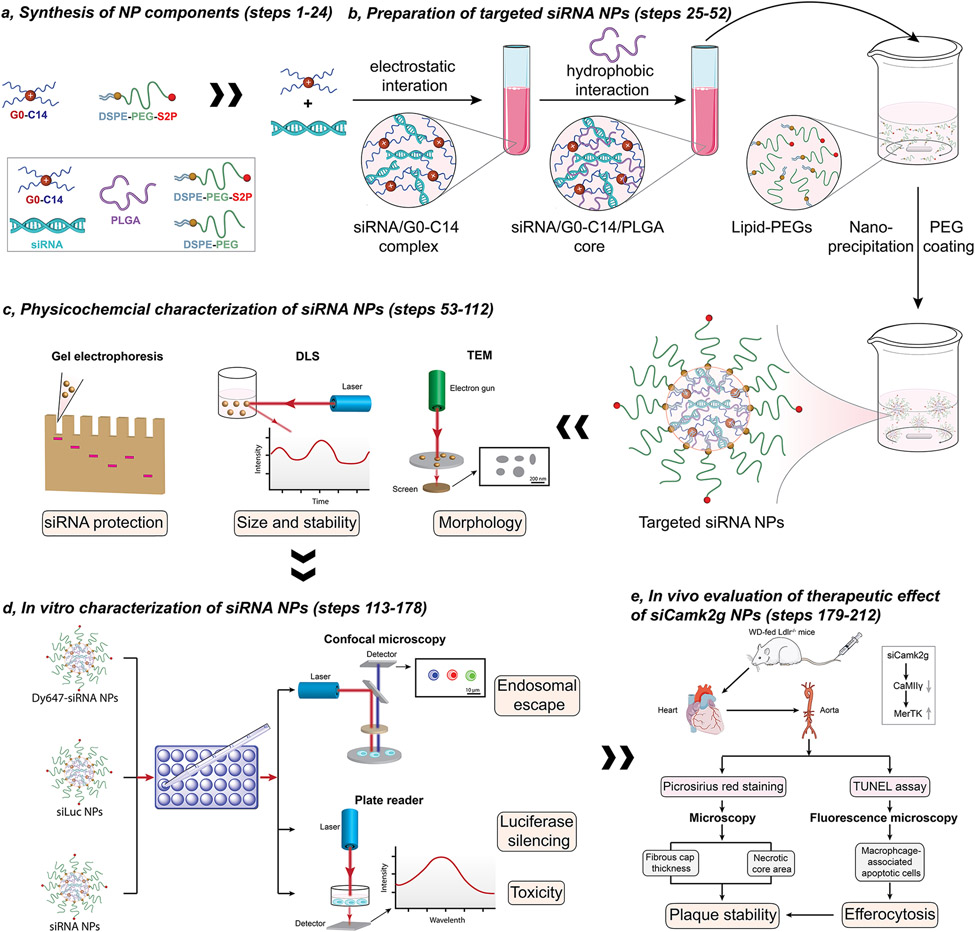
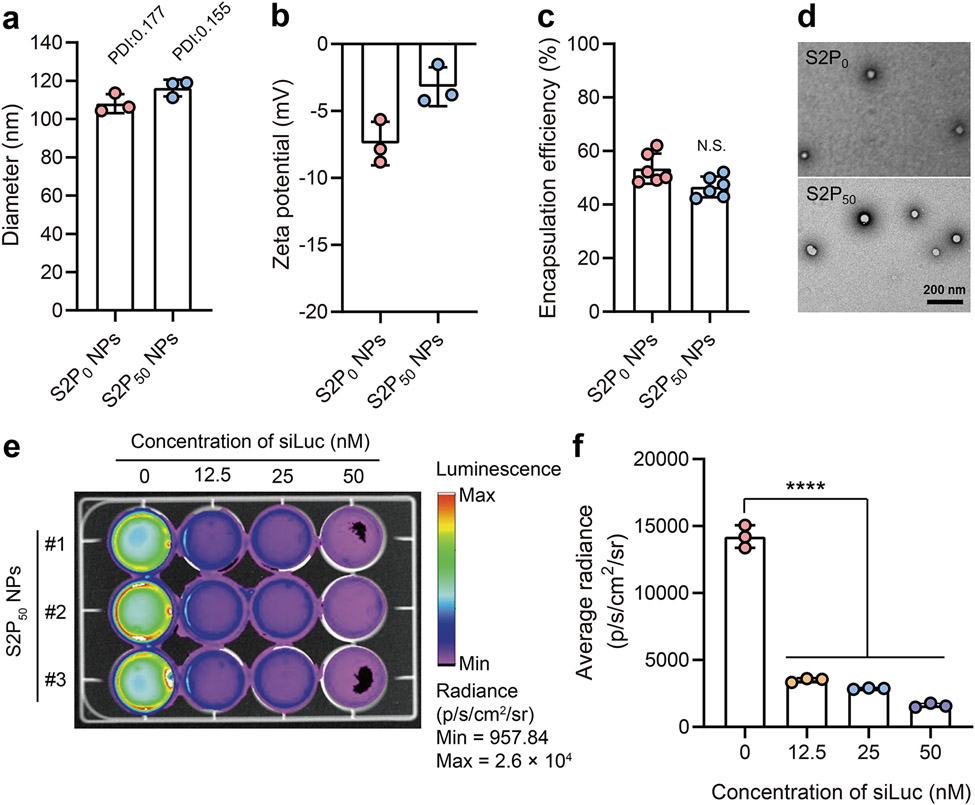
The activation of lesional macrophages is one of the causes of the instability of the atherosclerotic plaques. We present here a robust strategy for the treatment of atherosclerosis in mice using lesional macrophage-targeting siRNA NPs. This protocol contains five main stages (Fig. 2). We first describe the synthesis and purification of NP components, including cationic lipid (G0-C14) and targeted lipid-PEG (DSPE-PEG-S2P) (Fig. 2a). Targeting is achieved by modifying the lipid with a peptide sequence that binds to/interacts with the macrophage receptor stabilin-2. Nuclear magnetic resonance (NMR) is used to confirm the structure of the compounds. We then provide a step-by-step nano-precipitation approach for the preparation of targeted siRNA NPs (Fig. 2b). The preparation and optimization of the macrophage-targeting siRNA NPs are key features of the protocol. Five components, including the synthesized (G0-C14, DSPE-PEG-S2P) and commercially available (siRNA, PLGA, DSPE-PEG) compounds, are used to construct the siRNA NPs. The ratio of components, the formulation, the stirring speed, and the incubation time significantly impact the properties of the resulting NPs. For example, if the stirring speed is much lower than the recommended speed (1000 rpm), large NPs with low siRNA encapsulation efficiency will be formed. All the optimized parameters are discussed in this protocol. To confirm the successful formation of siRNA NPs, their physicochemical properties are fully characterized (Fig. 2c). Dynamic light scattering (DLS) is used to determine the size and colloidal stability of siRNA NPs. Transmission electron microscopy (TEM) is employed to characterize the morphology of siRNA NPs. Gel electrophoresis is used to investigate the stability of siRNA encapsulated by NPs. The resulting siRNA NPs are further characterized in vitro (Fig. 2d). Confocal microscopy is used to evaluate the endosomal escape ability of siRNA NPs by measuring the fluorescent signals of dye-labeled siRNA. A plate reader is implemented to quantify the gene silencing efficiency of the siRNA targeting luciferase (siLuc) NPs by measuring the bioluminescence signals. A plate reader is also used to assess the in vitro toxicity of siRNA NPs (the alamarBlue cell viability reagent). Finally, we evaluate the in vivo therapeutic effect of siCamk2g NPs in a WD-fed Ldlr−/− mouse model with established atherosclerosis (Fig. 2e). To confirm that the siCamk2g NPs can improve the plaque stability, microscopy is employed to determine the fibrous cap thickness and necrotic core area (picrosirius red staining). To further demonstrate that the enhanced plaque stability is ascribed to the promoted efferocytosis, fluorescence microscopy is implemented to characterize the macrophage-associated apoptotic cells (TUNEL assay). In addition, we evaluate the in vivo toxicity of the siRNA NPs using H&E staining and hematological analysis. Throughout the procedure (Fig. 2), we discuss the parameters that need to be optimized and how they influence the properties of the siRNA NPs, and how to troubleshoot any problems encountered when following the procedures.
Fig. 2. Workflow of the protocol.
The protocol comprises five main stages, including: a, synthesis of components (steps 1-24); b, preparation of the targeted siRNA NPs (steps 25-52); c, physicochemical characterization of the siRNA NPs (steps 53-108); d, in vitro characterization of the siRNA NPs (steps 109-164); and e, in vivo therapeutic effect evaluation of the siCamk2g NPs (steps 165-189).
Applications of the method
The key features of this protocol are the preparation, optimization and characterization of the siRNA-loaded polymer-lipid hybrid NPs, which have various applications in the biomedical field. The first application of this siRNA NP platform is the treatment of atherosclerosis which is described in this protocol using a mouse model. It has been previously established that the activation of lesional macrophage CaMKIIγ in advanced human and mouse atherosclerotic plaques is a major stimulus for the formation of necrotic lesions covered with thin fibrous caps.27 Therefore, the macrophage gene Camk2g, encoding CaMKIIγ, was chosen as the target for RNAi therapy. After administration to the mouse model with atherosclerosis, the targeted S2P-siCamk2g NPs were able to selectively silence the CaMKIIγ of the lesional macrophage and subsequently enhance efferocytosis, resulting in thicker fibrous cap and less atherosclerotic plaque necrosis.26 These siRNA NPs hold great promise for the treatment of atherosclerosis as demonstrated in a mouse model. For the treatment of other diseases, potential users can obtain tailored siRNA NP platforms conveniently by replacing the siRNA used in this protocol with another functional siRNA sequence. For example, this siRNA NP platform has also been used successfully for the treatment of non-small cell lung cancer (NSCLC) in a mouse model as demonstrated by another study in our group, in which, Prohibitin 1 (PHB1) was chosen as the target to silence. The siPHB1-loaded NPs were <100 nm in diameter, had long blood circulation time (t1/2 of ~8.1 h), had high tumor accumulation (~5.2 mg/kg), and could effectively inhibit tumor growth in mice bearing NCI-H460 and A549 tumors.6 In addition to siRNA delivery, the present NP platform can also be used for the delivery of large nucleic acid molecules such as mRNA with proper optimization.30,31
The wide deployment of two highly effective NP-based mRNA COVID-19 vaccines (mRNA-1273, Moderna32; and BNT162b2, Pfizer33) have fueled the research interests in NP-based mRNA delivery.34-37 It is worth noting that the NPs used in these two vaccines are chemically dissimilar to our NPs. For example, they contain ionizable lipids rather than cationic lipids, and they do not contain PLGA or targeting ligands. Despite that, the application of our polymer-lipid hybrid NP platform for mRNA delivery for cancer therapy has been demonstrated in mouse models in two other studies by our group.30,31 Phosphatase and tensin homologue deleted on chromosome 10 (PTEN) is a well-defined tumor suppressor gene that is lost or mutated in various human cancers.38 The restoration of functional PTEN in PTEN-null tumor cells has been shown to suppress, at least temporarily, the growth of tumors. Indeed, the PTEN-mRNA can be efficiently incorporated into our polymer-lipid hybrid NPs with slight optimization to the protocol presented here. The resulting PTEN-mRNA-loaded NPs exhibit good stability in physiological environments and achieve high PTEN-mRNA transfection efficiency in prostate cancer cells without eliciting significant cytotoxicity. Furthermore, in serval mouse models of prostate cancer, the systemic administration of the PTEN-mRNA-loaded NPs effectively inhibited the tumor growth in the mice.30 Similarly, another tumor suppressor gene named p53 can also be employed as the therapeutic target for cancer therapy. We demonstrated that p53-mRNA-loaded polymer-lipid hybrid NPs can inhibit the tumor growth of mice bearing different tumor models, and also sensitize the tumors to mTOR inhibition.31 Several recently published reviews have discussed the potential of our polymer-lipid hybrid NPs as an efficient siRNA or mRNA delivery platform for the treatment of different diseases.39-44
Overall, the polymer-lipid hybrid NP platforms generated by following our protocol are able to efficiently deliver siRNA and mRNA to target sites in vivo for the treatments of atherosclerosis and cancer, as validated by the studies of our group.6,26,30,31 The NPs we prepared here have been modified with the targeting peptide S2P, a peptide that recognizes the macrophage receptor stabilin-2, allowing for the specific targeting of lesional macrophages. Besides the application for the treatment of atherosclerosis, our polymer-lipid hybrid NPs without any targeting ligand have been reported to show significant accumulations in tumors, holding great promise for cancer therapy.6 Proper modifications are required before these NPs can be used for other applications. We anticipate that this protocol will be of interest to researchers who are developing RNA NPs to treat atherosclerosis, cancer, and beyond. The techniques involved in this protocol can also be used by specialists in the fields of chemistry, nanotechnology, cardiovascular diseases, biology, RNA therapeutics, and pharmacy.
Comparison with other methods
The present protocol describes the construction of a siRNA-loaded polymer-lipid hybrid NP platform for the treatment of atherosclerosis in mice via the regulation of lesional macrophage activation. Although our siRNA NPs-based therapeutic strategy for atherosclerosis has been rarely reported, a variety of other siRNA NP platforms have been developed for the treatment of a wide range of diseases.15 One of the widely investigated siRNA NP platforms is the polymeric NP. For example, a PEGylated poly guanidinium (PEG-pGu)-based siRNA NP platform has been developed for Alzheimer’s disease (AD) therapy.45 To increase the blood-brain barrier (BBB) penetration, a galactose (Gal) ligand was introduced to the siRNA NPs. In a transgenic AD mouse model, the administrated Gal-siRNA NPs were able to cross the BBB via glycemia-controlled glucose transporter-1 (Glut1)-mediated transport, improving the cognitive behavior of the mice. One concern of this cationic polymer system is the potential toxicity. To address this issue, a degradable influenza virus-inspired cationic polymer system was prepared for siRNA delivery.46 Upon internalization by the cells, the resulting siRNA NPs could quickly escape from the endosome through an influenza virus mimicking endosomal escape mechanism, releasing the siRNA into the cytosol via the degradation of the polymer. Despite the fact that the toxicity issues of cationic polymers can be alleviated by the incorporation of degradable bonds, the instability of the polymeric NPs can be problematic when administrated in vivo. The only driving force for the siRNA/cationic polymer complex is electrostatic interactions, which can be largely weakened in the ionic strength condition of the body.
Another siRNA NP delivery platform is the DNA nanostructure.47,48 As one of the well-characterized DNA nanostructures, DNA tetrahedron has been widely used for the delivery of therapeutics including siRNA. For instance, a self-assembled DNA tetrahedron was prepared for in vivo siRNA delivery.49 The siRNA cargos were conveniently incorporated onto one of the six edges of the DNA tetrahedrons through one-step self-assembly. Importantly, different cancer-targeting ligands could be easily conjugated to surfaces of the DNA tetrahedrons via DNA hybridization. The high programmability of the DNA strands allowed the precise control of the size of the tetrahedrons, spatial orientation, and density of the ligands. The siRNA-loaded DNA tetrahedral NPs could deliver the therapeutic siRNA to the tumor and silence the target genes. A similar siRNA-loaded DNA tetrahedral NP platform has also been developed for targeted delivery of therapeutic siRNA to the kidney of the mice, treating acute kidney injury (AKI).50 In addition, a DNA nanosuitcase platform51 and a DNA nanotube platform52 have also been constructed for siRNA delivery. A major advantage of all these DNA nanostructure-based NP platforms is their negligible toxicity owing to the inherent biocompatibility of DNA materials. However, these DNA nanostructures do not provide enough protection for the siRNA cargos, making them vulnerable to enzymatic degradation.
Among all the siRNA NP platforms, the lipid NP is the most clinically advanced platform. Indeed, the first FDA-approved siRNA therapeutic (Patisiran) is based on lipid NP formulations.17 This type of lipid NP is typically composed of: the ionizable lipid, phospholipid, cholesterol, lipid-PEG, and siRNA.53 Homogenous lipid NPs with a diameter ~50-100 nm can be formed by rapidly mixing siRNAs with other components using a microfluidic mixing technique.54 Notably, these lipid NPs are neutral at pH 7.4, but protonated in the acidic environment of endosomes, improving the endosomal escape of siRNA via the fusion of lipids with the membrane of endosomes. Despite the successful applications of siRNA lipid NPs,55,56 specific designs might be required to improve their delivery efficiency for different diseases.57 For example, for specific cell types-related diseases such as macrophage-related atherosclerosis, a macrophage-targeting ligand can be introduced to the NPs to improve their therapeutic efficiency. Recently, a well-designed selective organ targeting (SORT) NP platform shows its capability to specifically deliver the therapeutics (Cas9 mRNA, single guide RNA) to lung, spleen and liver to enable efficient gene editing, holding great promise for the treatment of diverse organs-related diseases.58,59
Here, we provide a detailed protocol for the development of a polymer-lipid hybrid NP platform for efficient in vivo delivery of siRNA.6,26 To date, siRNA-loaded polymer-lipid hybrid NPs have been typically synthesized by solvent evaporation or double emulsion methods.60-63 However, our siRNA-loaded polymer-lipid hybrid NP is prepared through a simple nano-precipitation method, and has a unique structure consisting of a siRNA/cationic lipid/PLGA polymer core and a lipid-PEG shell. Compared to the ionizable lipid NP platform, we have introduced an extra hydrophobic polymer core to our platform, aiming to further protect the unstable nucleic acid cargo and prolong the blood circulation time. We have previously prepared different polymer-lipid hybrid NPs with serval different cationic lipids, and the most efficient NP was prepared with G0-C14 lipid which contains five tertiary amines and seven hydrocarbon tails.6 We use the lowest concentration of G0-C14 (siRNA/G0-C14 weight ratio,1:15) that is able to condense the siRNA to prepare our siRNA NPs, while no significant in vitro and in vivo toxicities of the NPs are observed. The tertiary amines can provide sufficient positive charges to condense the negatively charged nucleic acids, and the hydrocarbon tails can bind to the hydrophobic polymer via hydrophobic interaction. Therefore, the amines and hydrocarbon tails are pivotal for the construction of our platform, whereas ionizable lipids do not have sufficient cationic charge to be suitable for our platform.
Our polymer-lipid hybrid NP platform has several advantages over the other in vivo delivery platform discussed above. First, the NPs have a long blood circulation time (t1/2 of ~8.1 h compared to t1/2 of ~4 h for a MC3-based lipid NP64). The formation of the NPs is driven by the electrostatic interactions between the anionic nucleic acids and cationic lipids, and the hydrophobic interaction between the hydrophobic PLGA and lipid tails. Utilizing both electrostatic and hydrophobic forces produces NPs with high in vivo stability.6 Second, targeting ligands can be easily introduced to the NPs. Given the multicomponent structure of the NPs, different targeting ligands can be conveniently introduced to the lipid-PEG shell without changing the main structure of the NPs. The ligand modification is described in this protocol.26 In addition, to realize the on-demand release of the therapeutics, the hydrophobic PLGA polymer of the NPs can be replaced by a stimuli-responsive hydrophobic polymer. For example, we developed a redox responsive NP platform by replacing the PLGA polymer with a reduction-responsive polymer.31 Taken together, our polymer-lipid hybrid NP platform is highly flexible (to be engineered with different functions) and easy-to-prepare, holding great promise for efficient delivery of siRNA and other types of nucleic acids.
Experimental design
Here we describe the design and rationale for each procedure in this protocol.
Synthesis of cationic lipid and ligand (Steps 1-24)
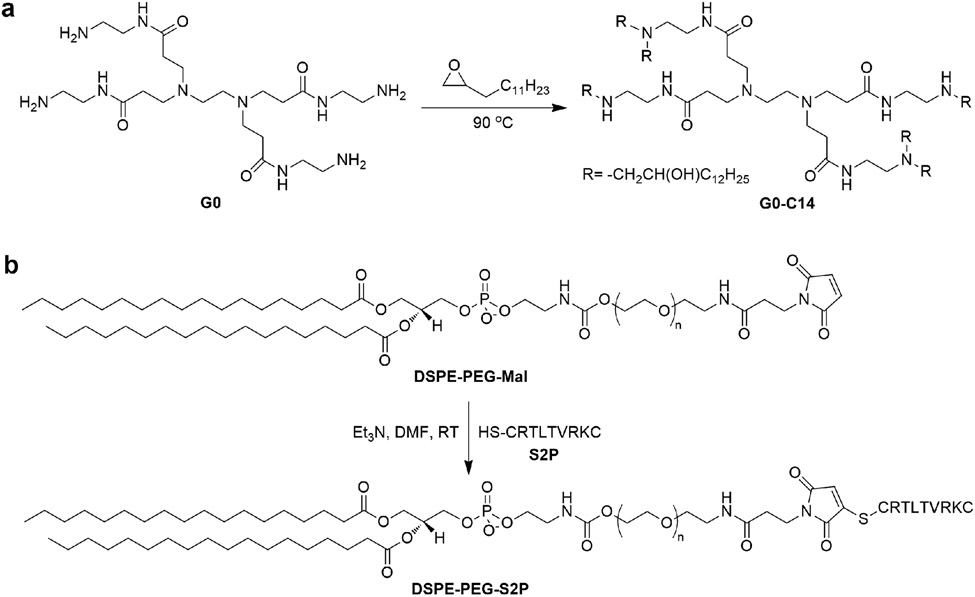
The cationic lipid termed G0-C14 is synthesized by a unique synthetic strategy involving effective ring-opening of epoxide (1,2-epoxytetradecane) by amine compound (poly (amido amide) (PAMAM) dendrimer G0) (Fig. 3a).60 This synthetic strategy requires no solvent and protection/deprotection steps, making it highly suitable for high-throughput screening of cationic lipids for superior nucleic acid delivery.65 The generation 0 of PAMAM dendrimer is employed for the synthesis of cationic lipids based on its capability to condense the siRNA and its lower cytotoxicity than higher generations. In addition, we have previously synthesized cationic lipids using different cationic amino molecules, including G0, branched polyethylenimine (Mw ~ 800) (PEI), polypropylenimine tetramine dendrimer, generation 1 (DAB) and diethylene triamine. Among them, the G0-lipid shows the highest siRNA delivery efficiency.6 We chose 1,2-epoxytetradecane for the synthesis of cationic lipid because lipid-like compounds with 14 carbons have been shown to be optimal for siRNA delivery.65 The maximal amounts of lipid tails that can be conjugated to G0 are eight according to the four free amines of G0. To obtain G0-C14 with one less tail than the fully conjugated G0-C14, seven equivalents (eq.) of lipid tails (1,2-epoxytetradecane) are reacted with one eq. of G0. The obtained crude product can be purified by silica gel chromatography with gradient elution (CH2Cl2→75:22:3 CH2Cl2/MeOH/NH4OH). The chemical structure of the G0-C14 can be determined by 1H NMR (The purified G0-C14 contains about 7 lipid tails as calculated from the 1H NMR spectrum60).
Fig. 3. Synthesis of cationic lipid and ligand.
a, G0-C14. Adapted with permission from ref.60, National Academy of Sciences; b, DSPE-PEG-S2P. Adapted with permission from ref.26, American Association for the Advancement of Science.
The ligand-modified lipid-PEG (DSPE-PEG-S2P) is prepared by an efficient and widely used click reaction between the thiol group of the targeting peptide sequence: CRTLTVRKC (S2P) and the maleimide (Mal) group of Mal-modified DSPE-PEG (DSPE-PEG-Mal) (Fig. 3b). We use thiol-maleimide click chemistry for two reasons. First, the thiol group can be easily and conveniently introduced during the custom synthesis of the peptide. Hence, the peptide ligand can be conjugated to the lipid-PEG in one step. Second, the thiol and maleimide groups are stable in both organic and aqueous solutions, leading to high reaction efficiency. The resulting crude DSPE-PEG-S2P can be purified through washes with cold methanol. The successful conjugation of S2P to DSPE-PEG can be validated by 1H NMR. If a user wants to target another cell type or organ, we recommend using an alternative cysteine-terminated peptide or other targeting ligand in place of S2P.
Preparation of nucleic acid-loaded NPs (Steps 25-52)
The siRNA NPs are prepared by a robust nano-precipitation method that is well-established by our group. Due to the vulnerability of free siRNA to nucleases, the siRNA needs to be fully protected before it reaches its intended destination. To this end, our NPs are designed to have a core-shell structure, where the siRNA is loaded in the core and protected from enzymatic degradation. To fabricate the siRNA-containing core, we first condense the siRNA with cationic lipid G0-C14 through electrostatic interaction between the negatively charged siRNA and the positively charged G0-C14. However, the siRNA/G0-C14 complex might not be stable because the electrostatic interaction may be easily weakened by the high ionic strength condition of the body. Therefore, a hydrophobic polymer PLGA is used to cover the siRNA/G0-C14 complex via the hydrophobic interaction between the hydrophobic lipid tails of C0-C14 and the hydrophobic PLGA. It is worth noting that the cationic lipid G0-C14 plays a pivotal role in the fabrication of siRNA NPs. The cationic part of the G0-C14 should have enough positive charges to efficiently condense the negatively charged siRNA and the lipid part of the G0-C14 should have enough hydrophobicity to interact with the hydrophobic PLGA. To reduce the non-specific cellular uptake of the NPs and therefore prolong their blood circulation time in vivo, many neutral hydrophilic polymers have been used to modify the surfaces of the NPs.66 Among them, PEG is the most popular polymer due to its low toxicity and simple chemistry. Based on this, we introduced a PEG shell to cover the siRNA/G0-C14/PLGA core to increase the stability and blood circulation time of the siRNA NPs. The PEGylation process can be easily conducted by dropwise addition of the organic solution containing the siRNA/G0-C14/PLGA core to the aqueous solution containing the DSPE-PEG shell. For the introduction of targeting ligand such as S2P to the NPs, researchers just need to add the DSPE-PEG-S2P (or other targeting ligand-modified lipid) to the aqueous solution during the preparation of NPs. The targeting capability of the siRNA NPs is enabled by the S2P ligand, therefore, a high DSPE-PEG-S2P/DSPE-PEG ratio of 1:1 is recommended to maximize the targeting effect of the siRNA NPs to macrophages. Here, the DSPE-PEG-S2P/DSPE-PEG ratio of 1:1 was used for all in vitro and in vivo experiments. An optimal G0-C14/siRNA weight ratio was used to ensure the condensation of the siRNA by G0-C14; an optimal PLGA/siNRA weight ratio was used to ensure the protection of siRNA by PLGA; an optimal lipid-PEG/siRNA weight ratio was used to ensure the formation of stable siRNA NPs. In addition, an optimal stirring speed was used to achieve NPs with high siRNA encapsulation efficiency and proper size; an optimal incubation time was used to make sure the formation of siRNA NPs and avoid the degradation of the siRNA.
To remove the small amount of organic solvent in the NP solutions, the NPs are further washed several times with water using an ultrafiltration purification method. We chose the ultrafiltration purification method based on the following considerations. First, it saves a lot of time since the purification can normally be done in one or two hours. Short operation time lowers the risk of degradation of siRNA during the purification process, and is especially important if the NP platform is used to deliver very unstable RNA therapeutics such as mRNA. Second, the concentration of the NPs can be easily adjusted. The ultrafiltration can result in a highly concentrated solution of NPs, which can be easily redispersed in any buffers to obtain NPs with any desired concentration according to different needs. This is quite useful when the NPs are applied in vivo, where high concentrations of NPs are normally required. In addition, our siRNA NP solution can be frozen and kept in the freezer for a few weeks, and then thawed for use. The thawed siRNA NPs show no significant changes in activity, size and polydispersity index (PDI). We used a 20-mL glass vial to produce maximal 400 μL of NPs (siRNA 5μM). If larger volume of NPs (e.g. 2 mL) is required, the researchers can easily produce 2 mL of NPs by using 5 glass vials (20-mL).
Our polymer-lipid hybrid NPs can also be used as efficient delivery platforms for mRNA.30,31 However, slight modifications are necessary for the preparation of mRNA NPs compared to the siRNA NP formulation presented here. The mRNA molecules are much larger than the siRNA molecules, and therefore the mRNA/G0-C14 weight ratio needs to be optimized to ensure the sufficient condensation of the mRNA by the cationic lipids. Compared to the preparation of siRNA NPs, where the siRNA/G0-C14 ratio of 1:10 is required, the preparation of mRNA NPs needs a larger amount of cationic G0-C14 lipids (mRNA/G0-C14 weight ratio,1:15). In addition, the stability of large and single-strand mRNA is much lower than the small and double-strand siRNA. Therefore, the working area and all the tools need to be cleaned carefully with RNaseZAP to remove all the RNase contamination before starting to work with mRNA. Meanwhile, it is important to maintain the mRNA and mRNA NPs at a low temperature of 4 °C or below since mRNA is prone to degradation at room temperature.
Dynamic light scattering (DLS) characterization of siRNA NPs (Steps 53-58)
It has been previously reported that particles with diameters greater than ~200 nm cannot pass the spleen’s fenestrations which are typically below 200-500 nm in width.67,68 Thus, NPs with diameters in the range of 30-200 nm are ideal for systemic in vivo delivery because they can remain in circulation and avoid rapid renal clearance. To form siRNA NPs with ideal size, dynamic light scattering (DLS) is employed to monitor the size of each NP formulation. Most of the DLS instruments are able to detect NPs with sizes from 10 nm to 1μm within a few minutes. Normally, 1.5 mL of sample is enough for detection, and it can be recycled for other tests. DLS can also be used to measure the zeta potential of the NPs. Any surface modifications of the NPs can lead to changes in zeta potential. Thus, by monitoring the changes in zeta potentials of the NPs, we can determine whether the surface modifications and alterations in surface charge are successful. If different users need to reproduce the NPs according to this protocol, DLS can be used to quickly confirm the successful production of the NPs.
Transmission electron microscope (TEM) characterization of siRNA NPs (Steps 59-68)
Based on our design for the siRNA NPs, a core-shell structure is important with regard to protecting the siRNA from enzymatic degradation and prolonging the blood circulation time. The transmission electron microscope (TEM) can clearly characterize the morphology and structure of the NPs. We thus use the TEM to confirm the core-shell structure of the siRNA NPs. In order to improve the contrast of the sample in TEM images, 1 % (wt/vol) of uranyl acetate is used to provide negative stain contrast in TEM images. The TEM images of the siRNA NPs in this protocol are produced using a JEOL 1200EX electron microscope at 80 kV.
Gel electrophoresis of siRNA NPs (Steps 69-91)
Our polymer-lipid hybrid NPs are designed to protect the loaded siRNA from enzymatic degradation. To confirm the protective effect of the NPs, the serum stability of siRNA NPs is assessed using agarose gel electrophoresis by monitoring the siRNA band. We incubate the siRNA-loaded NPs in a solution containing 50% (vol/vol) serum at 37 °C, a condition mimicking the in vivo environments, for different time periods. Theoretically, the enzymes in the serum can quickly degrade the siRNA at 37 °C upon direct exposure, resulting in the fading or disappearance of the siRNA band in agarose gel electrophoresis. In order to directly compare the siRNA that is loaded in the NPs with the free siRNA, the siRNA in the NPs is isolated before loading onto the agarose gel. To isolate the siRNA from the NPs, siRNA NPs are first pelleted using Amicon Ultra-15 centrifugal filter units (MWCO, 100 kDa). Then, the pellet is dissolved in chloroform to destroy the core-shell structure of the NPs, releasing the incorporated siRNA which is extracted from chloroform using 0.5 M NaCl containing 0.1% (wt/vol) SDS.6 The siRNA protection efficacy of siRNA by the polymer-lipid hybrid NPs is determined by gel electrophoresis using ethidium bromide-infused E-Gel 4% (wt/vol) agarose gels which are imaged under ultraviolet (UV) light.
Determination of siRNA encapsulation efficiency (EE) (Steps 92-101)
Fluorescence detection is a highly sensitive technique widely used for the detection of compounds in solution even at very low concentrations. To determine the siRNA encapsulation efficiency (EE) of the NPs, we label the siRNA with a fluorescent dye Dy647 (Dy647-siRNA). Alternatively, the siRNA EE of the NPs can be directly determined using ribogreen, one of the most sensitive fluorescent dyes for the detection of RNA in solution. Instead of ribogreen, we used dye-labeled siRNA (Dy647-siRNA) as this was also required for other experiments. The Dy647-siRNA is loaded into the NPs following the approaches we described above. The unloaded Dy647-siRNA can be easily removed in the ultrafiltration purification step. The encapsulation of fluorescent molecules into the cores of the NPs can result in changes in their fluorescence signals. Therefore, the Dy647-siRNA needs to be released from the NPs before it can be precisely determined by fluorescence detection. To this end, Dy647-siRNA-loaded NPs are dissolved in organic solvent dimethyl sulfoxide (DMSO), a solvent that can destroy the NPs by dissolving all the NP components, to release the encapsulated Dy647-siRNA. The fluorescence of the free siRNA can then be measured using a fluorescent plate reader, such as the Infinite M200 PRO spectrophotometer. The initial amount of Dy647-siRNA loaded into the NPs is also dissolved in DMSO and its fluorescence is measured. The fluorescence of only DMSO is also measured and used as a blank control. All the measurements are conducted in triplicate. The siRNA EE of NPs can be calculated according to the following equation:
Evaluation of the stability of siRNA NPs (Steps 102-108)
The stability of the siRNA NPs in biological media is critical to their long blood circulation, which allows the accumulation of siRNA NPs at lesional sites. To determine the stability of NPs in vitro, NPs are incubated with PBS containing 10% (vol/vol) serum (mimicking the in vivo environments) and their sizes are measured by DLS after different incubation time periods (up to 3 days). All the measurements are conducted in triplicates. The siRNA NPs after incubation for different time periods are considered to be stable at these conditions if their sizes show no significant changes compared to that of the freshly prepared NPs.
Characterization of endosomal escape of siRNA NPs (Steps 109-121)
The inefficient endosomal escape of siRNA NPs is reported to be a limiting factor for efficient siRNA delivery.57,69 Therefore, the endosomal escape ability of NPs can increase siRNA delivery efficiency. To investigate the endosomal escape ability of our siRNA NPs, we first label NPs via labeling the encapsulated siRNA with a fluorescent dye Dy647 (red). So, we can track the locations of siRNA NPs in the cells (we used HeLa cells) by monitoring the red fluorescence. Then, we use LysoTracker Green (green) to stain the late endosome whose locations in cells can be tracked via monitoring the green fluorescence. Upon incubation with Dy647-siRNA NPs for different time periods (1 or 4 h), the HeLa cells are first stained with LysoTracker Green for late endosome staining and then stained with Hoechst 33342 (blue) for nuclei staining. The cells are observed and imaged using an FV1000 laser scanning confocal microscope. The overlap of the red and green fluorescence signals of cells suggests that siRNA NPs are trapped inside the endosomes. The successful endosomal escape of siRNA NPs is defined by the separation of the red and green fluorescence signals of the cells.
In vitro evaluation of gene silencing by siRNA NPs (Steps 122-131)
Before the evaluation of siRNA NPs in vivo, we assess the gene silencing ability of siRNA NPs in vitro. To this end, one of the most widely used reporter gene systems based on luciferase-expressing HeLa (HeLa-Luc) cells is used for gene silencing assessment. Normally, the gene silencing efficiency of siRNA NPs can be determined by measuring the protein expression levels using western blot analysis, which is relatively costly and time-consuming. The advantage of the HeLa-Luc system is that the gene silencing efficiency of the siRNA NPs can be quickly determined by measuring the bioluminescence using a plate reader or an In-Vivo Xtreme imaging system with a charge-coupled device (CCD) camera. A luciferase substrate must be added to the cells and incubated for 5 min before the measurements. Both quantitative data and images can be generated and used for gene silencing efficiency analysis. The gene silencing of our siRNA NPs is evaluated by incubating the siLuc NPs with HeLa-Luc cells for 24 h in 12-well plates using RPMI 1640 medium containing 10% (vol/vol) FBS as the culture medium. Upon 24 h incubation, the bioluminescence of the cells is measured using an In-Vivo Xtreme imaging system with a CCD camera. The bioluminescence signal of cells treated with PBS is measured and used as a PBS control. The treatment of PBS should not lead to any silencing effect of the Luc gene. All the measurements are conducted in triplicate. To quantify the gene silencing efficiency, the average radiance (photons per second per cm2 per steradian) within regions of interest is quantified using Bruker MI SE software.
In vitro viability, apoptosis, and proliferation assessment of siRNA NPs (Steps 132-164)
Biocompatibility is a prerequisite in the development of NPs as safe in vivo siRNA delivery systems. In addition to the in vivo safety issues, the toxicity of the delivery systems can also interfere with the in vitro evaluations. For example, a false gene silencing effect can be achieved after incubating toxic siLuc NPs with HeLa-Luc cells. This can be ascribed to the fact that the toxicity of siLuc NPs can also decrease Luc expression by suppressing the growth of HeLa-Luc cells. To evaluate the safety of our siRNA NPs, we first investigate their in vitro toxicity. Different cells, including HeLa-Luc, RAW 264.7, and HEK-293 cells, are incubated with various amounts of siLuc NPs in 96-well plates for 24 h. After which, the medium of the cells is replaced with a fresh medium and incubated for another 48 h. After the addition of the alamarBlue cell viability and proliferation reagent, the viability of the cells can be determined by measuring the absorbance at 570 nm using a plate reader. The absorbance of alamarBlue-treated medium is also measured and used as a blank control. The absorbance of cells treated with PBS is measured and used as a PBS control. The treatment of PBS should not lead to any cytotoxicity in the cells. All the measurements are conducted in 5 replicates. The viability of NP-treated cells can be calculated according to the following equation:
Some reagents can induce cell apoptosis, especially early apoptosis, which may not be detected by a cell viability reagent. We therefore also assess the apoptosis of cells treated with our siRNA NPs. RAW 264.7 cells are incubated with siLuc NPs containing 50 nM siLuc in 24-well plates for 24 h. After which, the medium of the cells is replaced with a fresh medium and incubated for another 48 h. After the double staining with Annexin V-FITC and propidium iodide (PI) (Annexin V-FITC Apoptosis Detection kit), the apoptosis of the cells can be determined by flow cytometry. The apoptosis of cells treated with PBS is measured and used as a PBS control. The treatment of PBS should not lead to any significant apoptosis to the cells. All the measurements are conducted in triplicates. The early apoptosis of cells is defined by Annexin V-FITC positive and PI negative; and the late apoptosis or dead cells are defined by both FITC Annexin V and PI positive.
To investigate whether the siRNA NPs have an adverse effect on the growth of cells that is not detectable in the short term, we evaluate the proliferation of siRNA NPs-treated cells over 7 days. RAW 264.7 cells are incubated with siLuc NPs containing 50 nM siLuc in 96-well plates for 24 h. After which, the medium of the cells is replaced with a fresh medium and incubated for another 7 days. After the addition of the alamarBlue cell viability and proliferation reagent, the proliferation of cells can be determined by measuring the absorbance at 570 nm using a plate reader. Notably, alamarBlue is a non-toxic agent that can be applied repeatedly on the same samples, allowing continuous monitoring of the samples.70 Thus, the proliferation of cells is monitored every day and the medium containing alamarBlue reagent is replaced by a fresh medium after each measurement. The absorbance of alamarBlue-treated medium is also measured and used as a blank control. The absorbance of cells treated with PBS is measured and used as a PBS control. The treatment of PBS should not lead to any inhibition to the growth of cells. All the measurements are conducted in 5 replicates. The proliferation of the NP-treated cells can be calculated according to the following equation:
In vivo evaluation of the therapeutic effect of siRNA NPs (Steps 165-189)
To assess the in vivo therapeutic effect of siRNA NPs for the treatment of atherosclerosis, we first establish a mouse model of atherosclerosis. It is well-documented that the Ldlr gene-deficient mice can easily develop atherosclerotic plaques without any surgeries or injections by only feeding the mice with a high-fat Western diet (WD) for 6 to 8 weeks. Therefore, eight- to ten-week-old male mice with deficient Ldlr gene (Ldlr−/−) are obtained from Jackson laboratory, and fed with WD for 8 weeks to develop the atherosclerotic plaques. It is worth noting that the influence of sex may need to be considered in many mouse models for human diseases.71 We have used eight- to ten-week-old male mice with deficient Ldlr gene (Ldlr−/−) for the evaluation of the therapeutic effect of siRNA NPs. However, we speculate that this procedure would also be applicable to female mice since all the atherosclerosis-related phenotypes, including cholesterol, high-density lipoprotein (HDL), low-density lipoprotein (LDL), triglycerides, and Apolipoprotein B (ApoB), elevate similarly both in male and female Ldlr knockout mice as demonstrated by Jackson laboratory (supplier of lab mice). Therefore, sex should not have a significant influence on the results generated by this protocol. The mice are randomly divided into 3 groups (with 7-9 mice per group) and injected with two doses of PBS, control siRNA NPs or siCamk2g NPs per week, respectively. After 4 weeks of treatment, the mice are euthanized with CO2 and their hearts with attached aortic roots are either fixed in 4% (wt/vol) paraformaldehyde followed by paraffin embedding or treated with optical cutting temperature (OCT) compound and frozen. Sections of the aortic root with different sizes are isolated from the paraffin-embedded or frozen samples for the analysis of atherosclerotic lesions.
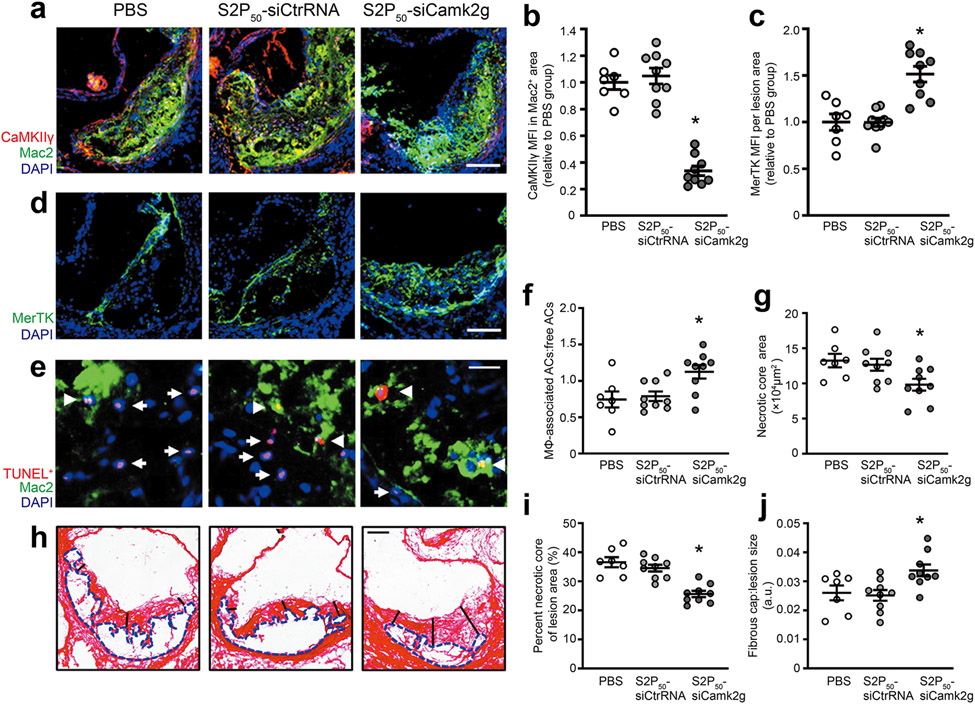
According to the proposed therapeutic mechanism of our siCamk2g NPs (Fig. 1), the treatment of siCamk2g NPs can knock down the expression of CaMKIIγ, resulting in the activation of the MerTK pathway in macrophages of the atherosclerotic lesions. To validate this mechanism, the expressions of CaMKIIγ and MerTK in lesional macrophages are characterized by immunofluorescence imaging. After blocking with bovine serum albumin (BSA), the obtained aortic root sections are first stained with primary anti-Mac2 and anti-MerTK and subsequently stained with fluorescently labeled secondary antibodies after PBS rinses. The nuclei of the macrophages are further stained with 4′,6-diamidino-2-phenylindole phenylindole (DAPI). The stained sections are imaged by a Zeiss epifluorescence microscope and the images are analyzed by FIJI software. For statistical analysis, n = 7 to 9 mice per group.
Then, to further validate that the activation of the MerTK pathway can promote the efferocytosis of the lesional macrophages, the apoptotic cells in aortic root sections are detected by a TUNEL (terminal deoxynucleotidyl transferase-mediated deoxyuridine triphosphate nick-end labeling) assay, a method for detecting apoptotic cells, using immunofluorescence imaging. The aortic root sections are first stained with TUNEL staining reagents and washed with PBS. Then, the sections are blocked with BSA, stained with primary anti-Mac2 antibody, incubated with fluorescently labeled secondary antibodies and stained with DAPI. The stained sections are imaged using a Zeiss epifluorescence microscope and the images are analyzed using FIJI software. The apoptotic cells (TUNEL+) should be surrounded by Mac2+ macrophages when efferocytosis occurs. In contrast, isolated apoptotic cells have condensed nucleus and low antibody reactivity and are not associated with neighboring macrophages. Thus, the lesional efferocytosis can be quantified as the ratio of TUNEL+ cells (red) in contact with Mac2+ macrophages (green) to isolated TUNEL+ cells. For statistical analysis, n = 7 to 9 mice per group.
Finally, to confirm that the promoted efferocytosis can improve the plaque stability by reducing plaque necrosis and inhibiting fibrous cap thinning, the necrotic core area and fibrous cap thickness of the plaques in aortic root sections are determined by picrosirius red staining-based microscopy imaging. The picrosirius red staining is a widely used histological method to visualize collagen in paraffin-embedded tissue sections. Thus, the collagen of aortic root sections is stained with picrosirius red and imaged with light microscopy. The necrotic core area can be obtained directly from the images; the fibrous (collagen) cap thickness is quantified from one midpoint and two shoulder regions of the plaque and normalized to the lesion size.72 For statistical analysis, n = 7 to 9 mice per group.
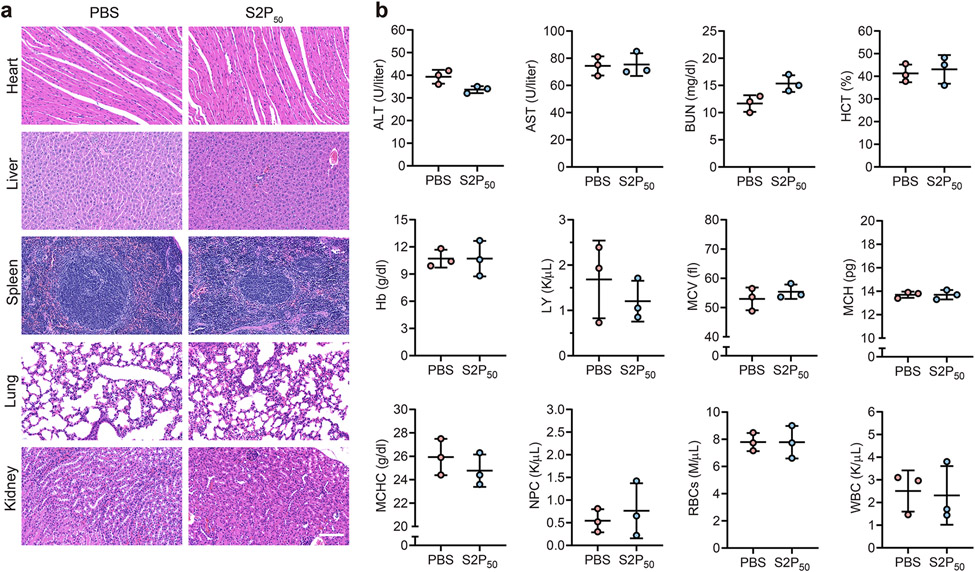
In vivo evaluation of the toxicity of the siRNA NPs (Steps 190-198)
The biosafety of the siRNA NPs is essential for their use in vivo. We therefore investigate the in vivo toxicity of the siRNA NPs under the same conditions (e.g. dose, frequency) as the therapeutic effect assay. Six-week-old female BALB/c mice obtained from Jackson laboratory are injected intravenously with two doses of PBS, or S2P50 siCamk2g NPs (1 nmol siRNA per injection) per week for 4 weeks. The mice are euthanized by CO2 inhalation three days after the last administration. To evaluate whether the siRNA NPs can cause any damage to the organs of the mice, the major organs are fixed in 4% (wt/vol) paraformaldehyde followed by paraffin embedding. Sections with different sizes are isolated from the paraffin-embedded samples and subjected to H&E staining. In addition, the blood from the mice is collected and various hematological parameters are evaluated, including alanine aminotransferase (ALT), aspartate aminotransferase (AST), blood urea nitrogen (BUN), hematocrit (HCT), hemoglobin (Hb), lymphocyte count (LY), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), neutrophil count (NPC), red blood cell count (RBC), and white blood cell count (WBC). For statistical analysis, n = 3 mice per group.
Recommended controls in the procedures
We recommend preparing the following control samples:
Step 71 Untreated extracted siRNA control: extracted siRNA from siRNA S2P50 NPs without incubation with serum.
Step 73 Untreated siRNA control: free siRNA without incubation with serum (incubate with PBS instead).
Step 99 Blank control: transfer 90 μL of 95% (vol/vol) DMSO solution to the 96-well plate.
Step 107 Untreated siRNA NPs control: the freshly prepared siLuc NPs without incubation with PBS containing 10% (vol/vol) serum.
Step 124 PBS control (or 0 nM siLuc): for the bioluminescence signal of cells treated with PBS.
Step 132 Blank control: the absorbance of medium without any cells.
Step 134 PBS control: the absorbance of cells treated with PBS.
Step 145 PBS control: the apoptosis of cells treated with PBS.
Step 151 Blank control: unstained cells; AV-FITC control: cells stained with AV-FITC (no PI); PI control: cells stained with PI (no AV-FITC).
Step 153 Blank control: the absorbance of medium without cells.
Step 176 PBS treated control: gene silencing of sections from mice treated by PBS; siCtrl NPs treated control: gene silencing of sections from mice treated by S2P50 siCtrl NPs.
Step 185 PBS treated control: efferocytosis of sections from mice treated by PBS; siCtrl NPs treated control: efferocytosis of sections from mice treated by S2P50 siCtrl NPs.
Step 189 PBS treated control: plaque stability of sections from mice treated by PBS; siCtrl NPs treated control: plaque stability of sections from mice treated by S2P50 siCtrl NPs.
Step 198 PBS treated control: H&E staining of sections from mice treated by PBS; hematological parameters of the blood from mice treated by PBS.
Expertise needed to implement the protocol
This protocol describes all the procedures for each experiment in detail and is easy to follow. Any researchers trained in nanotechnology, gene delivery, or biochemistry should be able to implement the protocol.
Limitations
The highly stable lipid-PEG shell of the NPs can reduce their cellular uptake, making them less suitable for in vitro or ex vivo applications, especially in situations where fast gene transfection is required. One solution to this issue is the introduction of targeting ligands. As demonstrated in this protocol, an S2P ligand is employed to improve the specific uptake of NPs by macrophages.26 Another solution to this issue is the replacement of lipid-PEG. We have previously established that lipid-PEGs with long and saturated lipophilic tails had a long dissociation half-life (t1/2) when presented on NPs.73 Therefore, the cellular uptake efficiency of the NPs can be tuned by using lipid-PEGs with short or unsaturated lipophilic tails. Despite the encouraging preclinical results that have been achieved using our polymer-lipid hybrid NP platform, the translation of our platform to clinical application needs further optimization. For example, the cationic lipids in our platform are biocompatible with most of the applications. However, in settings that require a high concentration of cationic lipids for NP synthesis, toxicity becomes an issue. Although negligible cytotoxicity was observed in cells treated with our NPs (siRNA 6.25-50 nM), we speculated that cytotoxicity > 20 % could be observed with siRNA doses > 50 nM (Supplementary Fig. 4a). This issue might be addressed by developing novel stimuli-responsive cationic lipids which can be degraded in the presence of various internal stimuli.74
Materials
Biological Materials
- Mouse model of interest. ! CAUTION All experiments involving live animals must conform to the requirements of your institutional animal care and use committee (IACUC) and be performed strictly following protocols that are approved by IACUC. All our procedures were conducted in accordance with the protocols reviewed and approved by IACUC at Harvard Medical School and Columbia University Irving Medical Center. To produce the results shown here, we used:
- Ldlr−/− mice, eight- to ten-week-old male mice (The Jackson Laboratory, B6.129S7-Ldlrtm1Her/J, Stock No: 002207)
- BALB/c mice, six-week-old female BALB/c mice (The Jackson Laboratory, BALB/cJ, Stock No: 000651)
- Cells of interest. ! CAUTION It is important to make sure that all the cell lines used in your research have no issues of cell line misidentification and cross-contamination. Our cell lines used in all the procedures had no issues of cell line misidentification and cross-contamination according to the latest report provided by International Cell Line Authentication Committee (ICLAC). http://iclac.org/databases/cross-contaminations/. ! CAUTION All the cell lines used in your research should be tested periodically to ensure they are authentic and not infected with mycoplasma. Our cell lines used in all the procedures were free of mycoplasma as determined by Mycoplasma Detection Kit (Thermo Fisher Scientific, M7006). To produce the results shown here, we used:
- HeLa-Luc cells (a HeLa cell line stably transfected with a firefly luciferase reporter gene, Sigma-Aldrich, cat. no. 11033106). https://scicrunch.org/resolver/RRID75: CVCL_2939. (ECACC Cat# 11033106, RRID:CVCL_2939)
- RAW 264.7 (ATCC, TIB-71™). https://scicrunch.org/resolver/RRID: CVCL_0493. (ATCC Cat# TIB-71, RRID:CVCL_0493)
- HEK-293 (ATCC, CRL-1573™). https://scicrunch.org/resolver/RRID: CVCL_0045. (ATCC Cat# CRL-1573, RRID:CVCL_0045)
Reagents
G0 (amine) (Sigma-Aldrich, cat. no. 412368, CAS. no. 155773-72-1)
Methanol (MeOH, Sigma-Aldrich, cat. no. 322415, CAS. no. 67-56-1). ! CAUTION Methanol is vaporizable and harmful to naked eyes. Work with personal protective equipment when handling methanol (e.g. safety goggles and face shields).
1,2-epoxytetradecane (epoxide) (Sigma-Aldrich, cat. no. 260266, CAS. no. 3234-28-4). ! CAUTION 1,2-epoxytetradecane can cause severe damage to the respiratory system. Perform all operations under a chemical fume hood.
Dichloromethane (CH2Cl2, Sigma-Aldrich, cat. no. 34856, CAS. no. 75-09-2). ! CAUTION Transferring dichloromethane that involves cannulas and needles (syringe) should be careful. Piercing the needles containing a residual amount of dichloromethane into tissues can cause severe injuries.
Ammonium hydroxide solution (NH4OH, Sigma-Aldrich, cat. no. 338818). ! CAUTION Ammonium hydroxide solution can cause damage to the respiratory system. Handle this reagent under a chemical fume hood.
Silica gel (high-purity grade, average pore size 60 Å, 70-230 mesh, 63-200 μm, cat. no. 60741-1KG)
Silica-gel-coated plates (Millipore Sigma, cat. no. MC1156840001)
DSPE-PEG-Mal (Nanocs Inc., cat. no. PG2-DSML-3k, 3400 Da)
DSPE-PEG (Avanti Polar Lipids, cat. no. 880320, 3400 Da)
Targeting peptide CRTLTVRKC (S2P) (GLS Biochem Systems Inc., cat. no. 65235)
Nuclease-free water (HyPure water) (Fisher Scientific, cat. no. SH3053801)
RNaseZAP (Fisher Scientific, cat. no. AM9785)
Acetone (Sigma-Aldrich, cat. no. 650501, CAS. no. 67-64-1). ! CAUTION Flammable and vaporizable acetone is harmful to the central nervous system. Work with acetone under a fume hood.
N,N-Dimethylformamide (DMF, Sigma-Aldrich, cat. no. 227056, CAS. no. 68-12-2) ! CAUTION N,N-Dimethylformamide may cause abdominal pain, headache, skin problems, constipation, nausea and vomiting. Wear personal protective equipment (e.g. eyeshields, face shields, lab coats and gloves) during operation.
50:50 Poly(DL-lactide-co-glycolide) (PLGA, LACTEL Absorbable Polymers, cat. no. B6013-2, Inherent Viscosity dL/g: 0.55 - 0.75)
1X PBS (Fisher Scientific, cat. no. SH3025601, pH 7.4)
NaOH solution (1M, Sigma-Aldrich, cat. no. 1091371000 )
HCl solution (1M, Sigma-Aldrich, cat. no. 1506961000)
UAR-EMS Uranyl acetate (Electron Microscopy Sciences, cat. no. 22405)
Fetal bovine serum (FBS, Thermo Fisher Scientific, cat. no. 26140095)
Chloroform (CHCl3, Sigma-Aldrich, cat. no. C2432, CAS. no. 67-66-3). ! CAUTION Chloroform is toxic and can cause severe health problems, including central nervous system damage, irritation of skin and eyes, etc. Perform all operations under a chemical fume hood.
Ethidium bromide-infused E-Gel 4% (wt/vol) agarose gel (Thermo Fisher Scientific, cat. no. G501804)
10X BlueJuice Gel Loading Buffer (Thermo Fisher Scientific, cat. no. 10816015)
Dimethyl sulfoxide (DMSO, Sigma-Aldrich, cat. no. 276855, CAS. no. 67-68-5).
RPMI 1640 medium (Thermo Fisher Scientific, cat. no. 11875119)
Penicillin-Streptomycin (10,000 U/mL Penicillin, 10,000 μg/mL Streptomycin, Thermo Fisher Scientific, cat. no. 15140122)
Hoechst 33342 (Thermo Fisher Scientific, cat. no. H1399)
LysoTracker™ Green (Thermo Fisher Scientific, cat. no. L7526)
Steady-Glo Luciferase reagent (Promega Corporation, cat. no. E2520)
Dulbecco's Modified Eagle Medium (DMEM, Thermo Fisher Scientific, cat. no. 11965092)
AlamarBlue cell viability reagent (Thermo Fisher Scientific, cat. no. DAL1100)
Annexin V-FITC Apoptosis Detection kit (Thermo Fisher Scientific, cat. no. V13245)
“Western” purified atherogenic diet (Envigo, TD.88137 Adjusted calories diet, 42% kcal from fat)
Paraformaldehyde Solution, 4% (wt/vol) in PBS (Fisher Scientific, cat. no. AAJ19943K2)
Bovine serum albumin (BSA, Sigma-Aldrich, cat. no. A2153, CAS. no. 9048-46-8)
10X Tris Buffered Saline (10X TPS, Bio-Rad Laboratories, Inc. cat. no. 1706435)
Tween 20 (Sigma-Aldrich, cat. no. P2287)
Goat serum (Sigma-Aldrich, cat. no. G9023)
Triton™ X-100 (Sigma-Aldrich, cat. no. X100)
4′,6-diamidino-2-phenylindole phenylindole (DAPI, Sigma-Aldrich, cat. no. D8417, CAS. no. 28718-90-3)
Picrosirius red (Polysciences, cat. no. 24901A)
Anti-luciferase RNA (siLuc), Dy647-labelled siLuc (Dy647-siLuc), and anti-CaMKIIγ RNA (siCamk2g) (Dharmacon, custom siRNA, siRNA sequence can be found in Table 1).
Table 1 ∣.
The siRNA sequences used in this protocol.
| NP formulations | siRNA | Strands | Sequences |
|---|---|---|---|
| S2P50 siLuc NPs | siLuc | Sense | 5’-CUU ACG CUG AGU ACU UCG AdTdT-3’ |
| Antisense | 5’-UCG AAG UAC UCA GCG UAA GdTdT-3’ | ||
| S2P50 siCtrl NPs | siLuc used as a control | Sense | 5’-CUU ACG CUG AGU ACU UCG AdTdT-3’ |
| Antisense | 5’-UCG AAG UAC UCA GCG UAA GdTdT-3’ | ||
| S2P50 Dy647-siLuc NPs | Dy647-siLuc | Sense | 5’-Dy647-CUU ACG CUG AGU ACU UCG AdTdT-3’ |
| Antisense | 5’-UCG AAG UAC UCA GCG UAA GdTdT-3’ | ||
| S2P50 siCamk2g NPs | siCamK2g | Sense | 5’-AAC GUG GUA CAU AAU GCU ACA-3’ |
| Antisense | 5’-UGU AGC AUU AUG UAC CAC GUU-3’ |
Equipment
Heating plate (Isotemp™ Hot Plate, Fisher Scientific, cat. no. HP88857296). ! CAUTION Avoid contacting heated part of the plate during heating operation, which can cause severe burns.
25-mL round bottom flask (Chemglass, cat. no. CG-618-01)
500-mL round-bottom flask (Chemglass, cat. no. CG-618-09)
Blood collection tube (Greiner bio-one, cat. no. 454012)
Amicon Ultra-15 centrifugal filter units (Sigma-Aldrich, cat. no. UFC9003, Mw cutoff, 3 kDa)
10-mL glass vial (Chemglass, cat. no. CG-4908-05).
20-mL glass vial (Chemglass, cat. no. CG-4908-01)
Gel loading tips (Fisher Scientific, cat. no. 02-707-139)
Carbon support copper grids (Electron Microscopy Sciences, cat. no. FCF200-CU)
96-well plate (Fisher Scientific, cat. no. CLS3595)
Nunc glass-bottom dish (Thermo Fisher Scientific, cat. no. 150680)
12-well plate (Fisher Scientific, cat. no. CLS3512)
6-well plate (Fisher Scientific, cat. no. CLS3516)
Syringes (BD, 1/2 cc insulin syringe U-100)
Oil bath
Rotary evaporator (Buchi Labortechnik AG)
Centrifuge (Thermo Scientific Sorvall Legend X1R Centrifuge cat. no. 75004263)
Orion Star™ A221 Portable pH Meter (Sigma-Aldrich, cat. no. STARA221)
Nanodrop spectrophotometer (Thermo Fisher Scientific, NanoDrop™ 1000 Spectrophotometer)
Sonication bath (Fisher Scientific, cat. no. FB11207)
Digital Vortexer (Fisher Scientific, cat. no. 0215370)
DLS measurement (Brookhaven Instruments Corporation)
Transmission electron microscopes (JEOL 1200EX)
E-Gel Power Snap Electrophoresis Device (Thermo Fisher Scientific, cat. no. G8100)
Confocal laser scanning microscope (Olympus FLUOVIEW FV1000)
Flow cytometer (BD LSR Fortessa)
Bioluminescence imaging system (Bruker In-Vivo Extreme II Optical/X-ray system)
Plate reader (Tecan, Infinite® M200 PRO)
GraphPad (https://www.graphpad.com)
FIJI software (https://imagej.net/Fiji).
Reagent setup
-
HEPES solution (Thermo Fisher Scientific, 1 M, pH 7.0-7.6, cat. no. 15630080):
To adjust the pH of HEPES solution to pH 6.5, introduce HCl while monitoring the pH with a pH meter. If the pH goes too low, raise it by carefully adding NaOH. ! CAUTION Users should exercise extreme caution when working with NaOH and HCl. Wear gloves, eye protection, face shields, and lab coats during operation. The buffer can be stored at 4 °C for up to 6 months.
-
RPMI 1640 cell culture medium:
To prepare the cell culture medium, add 50 mL FBS and 5 mL Penicillin-Streptomycin into 450 mL RPMI 1640 medium. The as-prepared cell culture medium contains 10% (vol/vol) FBS, 100 U/mL penicillin and 100 μg/mL streptomycin. The medium can be stored at 4 °C for up to 6 weeks.
-
1X Tris Buffered Saline with 0.1% (vol/vol) Tween 20:
Dilute 100 mL 10X Tris Buffered Saline with 900 mL deionized water, and add 1 mL Tween 20. A brief sonification will help to homogeneously mix the as-prepared 1X Tris Buffered Saline with 0.1% (vol/vol) Tween 20. The buffer can be stored at 4 °C for up to 3 months.
-
Blocking buffer (1× PBS containing 5% (vol/vol) normal serum and 0.3% (vol/vol) Triton™ X-100):
To prepare a 10 mL blocking buffer, add 0.5 mL normal goat serum into 9.5 mL 1× PBS. While stirring, add 30 μl Triton™ X-100 into the above solution. The buffer should be freshly prepared before use.
-
Antibody Dilution Buffer (1× PBS containing 1% (wt/vol) BSA and 0.3% (vol/vol) Triton X-100):
To prepare a 10 mL antibody dilution buffer, add 30 μl Triton™ X-100 into 10 mL 1× PBS. Then add 0.1 g BSA to the solution. Make sure the solution is homogeneously mixed. The buffer should be freshly prepared before use.
-
Anti-CaMKIIγ (1:400, Novus Biologicals, cat. no. NBP2-15685). https://scicrunch.org/resolver/RRID: AB_2892990. (Novus, Cat# NBP2-15685, RRID:AB_2892990)
Dilute the primary antibody with antibody dilution buffer. The buffer should be freshly prepared before use.
-
Anti-Mac2 antibody (1:10, 000, Cedarlane Labs, cat. no. CL8942AP). https://scicrunch.org/resolver/RRID: AB_2814900. (Fluidigm Cat# 3153026B, RRID:AB_2814900)
Dilute the primary antibody with antibody dilution buffer. The buffer should be freshly prepared before use.
-
Anti-MerTK (1:500, R&D Systems, cat. no. AF591). https://scicrunch.org/resolver/RRID: AB_2098565. (R and D Systems Cat# AF591, RRID:AB_2098565).
Dilute the primary antibody with antibody dilution buffer. The buffer should be freshly prepared before use.
-
Alexa Fluor 647 Goat-anti Mouse IgG (Life Technologies, A-28181). https://scicrunch.org/resolver/RRID: AB_2536165. (Thermo Fisher Scientific Cat# A28181, RRID: AB_2536165).
Dilute the second antibody with antibody dilution buffer. The buffer should be freshly prepared before use.
-
Mouse model of atherosclerosis:
To establish a mouse model of atherosclerosis, purchase eight- to ten-week-old male mice with deficient Ldlr gene (Ldlr−/−) from Jackson laboratory. Then, feed the mice with a high-fat Western diet (WD) for 8 weeks to develop atherosclerotic plaques.26
Procedure
Synthesis of cationic lipid (G0-C14) ● Timing ~ 3 d
CRITICAL This procedure should result in about 1.9 g of purified cationic lipid.
-
Weigh 1.0 g (1.936 mmol, 1 eq.) of G0 (amine) and add it to a 25-mL round bottom flask.
▲ CRITICAL STEP The G0 is 20 % (wt/vol) in methanol, so 1.0 g of G0 is equal to 1.0/0.2 = 5.0 g G0 solution.
-
Weigh 2.878 g (13.552 mmol, 7 eq.) of 1,2-epoxytetradecane (epoxide) and add it to the round bottom flask containing G0.
▲ CRITICAL STEP The 2-epoxytetradecane has a purity of 85% (wt/wt), so 2.878 g of 1,2-epoxytetradecane is equal to 2.878/0.85 = 3.386 g crude 1,2-epoxytetradecane. The ratio of the amines (G0) and hydrocarbon tails (C14) are critical for the construction of our platform. G0 has four primary amines that can maximally react with 8 lipid tails (1,2-epoxytetradecane). The feeding ratio of epoxide and G0 is 7:1 here because we want to form products with 7 lipid tails as these materials display high siRNA delivery efficiency.
Add a magnetic bar to the round bottom flask and equip the flask with a drying tube.
Place the flask in an oil bath supported by a hot-plate magnetic stirrer and start stirring the reaction solution.
Set the heating temperature to 90 °C and start heating the solution.
-
After 30 min, when all of the solvent (methanol) evaporates, replace the drying tube with an argon balloon.
▲ CRITICAL STEP Argon protection is mandatory due to the involvement of amine in the reaction.
-
Stir the reaction solution at 90 °C for 48 h under argon atmosphere.
▲ CRITICAL STEP The viscosity of the reaction mixture increases with the evaporation of the methanol. Ensure your magnetic stir bar is large enough so that it continues stirring in the increased viscosity solution.
-
After the completion of the reaction, remove the balloon and the magnetic stir bar.
CRITICAL STEP This is a solvent-free reaction, no need to remove solvent after the reaction.
Add 2.0 mL of CH2Cl2 to dissolve the reaction mixture.
-
Purify the product by flash silica gel column chromatography (silica gel, high-purity grade). Load the crude product solution to the silica column (diameter 40 mm, height 400 mm), remove the unreacted starting materials using CH2Cl2, and then elute the product using 75:22:3 CH2Cl2/MeOH/NH4OH. The purified G0-C14 contains 7 lipid tails as calculated from the 1H NMR spectrum60
? TROUBLESHOOTING
Collect the eluents in, 20-mL fractions using 30-mL tubes, around 25 fractions should be collected. Monitor the fractions by thin-layer chromatography (TLC) using silica-gel-coated plates and 75:22:3 CH2Cl2/MeOH/NH4OH as eluent (Rf is about 0.3 for product). Visualize the eluted product on the TLC plate by I2.
Product is expected to appear between fraction No.5 and No.10. Combine and transfer all the fractions containing pure product to a clean 500-mL round-bottom flask. Remove all the solvents using a rotary evaporator at 150 mbar and 25 °C in a water bath. The maximum temperature can be used is 45 °C and it normally takes 1-2 h to get the oily product.
Place the flask under a high vacuum for 24 h to remove any residual solvent.
-
Weigh the pure G0-C14, calculate the yield and store it at −20 °C.
? TROUBLESHOOTING
■ PAUSE POINT The pure G0-C14 can be store at −20 °C for at least 1 year.
Synthesis of ligand-modified lipid-PEG (DSPE-PEG-S2P) ● Timing ~ 3 d
CRITICAL This procedure should result in about 105 mg of purified ligand-modified lipid.
-
15
Weigh 200.0 mg (0.059 mmol, 1.0 eq.) of DSPE-PEG-Mal and add it to a 10-mL round bottom flask.
-
16
Weigh 63.7 mg (0.059 mmol, 1.0 eq.) of targeting peptide CRTLTVRKC (S2P) and add it to the round bottom flask containing DSPE-PEG-Mal.
-
17
Add 2 mL of 1 × HEPES buffer (pH 6.5) to dissolve the starting materials.
CRITICAL STEP Controlling the pH by HEPES buffer is important for the dissolution of S2P peptide and maximal reaction efficiency.
-
18
Add a magnetic bar to the round bottom flask and equip the flask with an argon balloon.
-
19
Place the flask on a hot-plate magnetic stirrer and start stirring the reaction solution.
-
20
Stir the reaction solution at room temperature for 48 h under argon atmosphere.
-
21
After the completion of the reaction, remove the balloon and the magnetic stir bar.
-
22
Pour the reaction solution into 30 mL of cold methanol in a 50-mL falcon tube to precipitate the product. Collet the precipitates by centrifugation (2305 × g, 5 min, 4 °C) and wash the precipitate 2 times with 15 mL of cold methanol.
▲ CRITICAL STEP Alternatively, purify the product with ultrafiltration using Amicon Ultra-15 centrifugal filter units (Mw cutoff, 3 kDa). After 5 rounds of washes, collect the filtrates containing pure product and remove the water by lyophilization.
-
23
Collect and transfer the precipitates to 2-mL Eppendorf tubes. Place the tubes under high vacuum for 24 h to remove any residual solvent.
-
24
Weigh the pure DSPE-PEG-S2P, calculate the yield and store it at −20 °C.
? TROUBLESHOOTING
■ PAUSE POINT The pure DSPE-PEG-S2P can be store at −20 °C for at least 1 year.
Preparation of siRNA stock solution ● Timing ~ 1 h
-
25
Order the anti-luciferase RNA (siLuc), Dy647-labelled siLuc (Dy647-siLuc), and anti-CaMKIIγ RNA (siCamk2g) (Table 1). We recommend ordering 1.0 μmol of each siRNA in order to perform the following in vitro and in vivo procedures.
-
26
Upon receiving the siRNA, spin down the lyophilized siRNA product.
CRITICAL STEP Normally, the lyophilized siRNAs are light and have very small volumes, thus they can be easily flushed out from the tubes by airflow when they are near the upper parts of the tubes. So, do not open the tubes before spin-down.
-
27
To make a siRNA stock solution of 100 μM, add 0.75 mL of nuclease-free water (HyPure water) to a tube containing 75 nmol siRNA.
-
28
Place the tube on a vortex for 30 s to dissolve the siRNA and spin down the solution. Repeat this process 3 times.
▲ CRITICAL STEP It takes time to dissolve the siRNA in water, so, make sure the siRNA is completely dissolved before it is used for further experiment. Otherwise, the concentration of siRNA cannot be precisely determined.
CRITICAL STEP Do not use a sonicator to facilitate the dissolution of the siRNA, because it can destroy the siRNA.
-
29
Transfer 1 μL of the obtained siRNA solution to a Nanodrop spectrophotometer to determine the concentration of the siRNA solution.
-
30
Aliquot the siRNA solution into 50-μL fractions and store them at −20 °C.
▲ CRITICAL STEP It’s important to aliquot the siRNA solution to minimize repeated freeze-thaw cycles, which can degrade the siRNA. Notably, we have not observed significant degradation of siRNA with 3 freeze-thaw cycles.
■ PAUSE POINT The siRNA aliquots can be store at −20 °C for 1 year.
Preparation of siRNA-loaded NPs ● Timing ~ 4 h
CRITICAL This procedure should produce about 400 μL of purified siRNA loaded NPs (5μM siRNA content). This scale is sufficient for most of the downstream characterization and in vitro and in vivo experiments. To perform downstream gel electrophoresis studies (Steps 69-91), this procedure will need to be scaled 7 times of siRNA NPs. For serum stability studies (Steps 102-108), this procedure will need to be scaled 2 times. For in vivo studies (Steps 165-170), this procedure will need to be scaled 5 times. See the Experimental Design section for advice on scaling the reaction.
-
31
Clean the working area and all the tools with RNaseZAP to remove all the RNase contamination.
▲ CRITICAL STEP This is especially important if the NPs are used to deliver more unstable nucleic acid cargoes, such as mRNA.
-
32
Weigh 10 mg of G0-C14 (from Step 14) and add it to a 10-mL glass vial.
-
33
To make an acetone solution containing 2.5 mg/mL G0-C14, add 4 mL of acetone to a glass vial and place the vial in a sonication bath for 10 min to dissolve the G0-C14.
▲ CRITICAL STEP The dissolution of G0-C14 in acetone is very slow even under sonication, so be patient to make sure that a clear solution is obtained (this usually takes 10 min). It is very difficult or impossible to dissolve the G0-C14 when its concentration is higher than 2.5 mg/mL. So the maximum G0-C14 concentration is 2.5 mg/mL. In another study of our group, we have shown that acetone can be replaced by dimethylformamide (DMF).31
-
34
Weigh 20 mg of PLGA and add it to a 10-mL glass vial.
-
35
To make an acetone solution containing 5 mg/mL PLGA, add 4 mL of acetone to the glass vial and place the vial in a sonication bath for 3 min to dissolve the PLGA.
-
36
Add a magnetic bar to a 20-mL glass vial and rinse the vial with 10 mL of HyPure water, repeat the rinse 3 times.
▲ CRITICAL STEP This wash step can reduce the RNase contamination of the vials and the magnetic bar.
-
37
Weigh 1 mg of hybrid lipid-PEGs containing different ratios of DSPE-PEG-S2P (from Step 24)/DSPE-PEG and add it to the 20-mL glass vial. Select the composition for your intended application using Table 2. We recommend 1:1 ratio for atherosclerotic lesional macrophages-targeting application. The targeting capability of the siRNA NPs is enabled by the S2P ligand, therefore, a high DSPE-PEG-S2P/DSPE-PEG ratio of 1:1 is recommended to maximize the targeting effect of the siRNA NPs to macrophages. Here, the DSPE-PEG-S2P/DSPE-PEG ratio of 1:1 was used for all in vitro and in vivo experiments.
-
38
To make an aqueous solution containing 0.1 mg/mL lipid-PEGs, add 10 mL of HyPure water to the glass vial and place the vial on a vortex for 30 s to dissolve the lipid-PEGs.
-
39
Place the glass vial on a magnetic stirrer and start stirring the lipid-PEG solution at a stirring speed of 600 rpm.
-
40
Thaw the siRNA aliquots on the ice. One aliquot is required for the preparation of 400 μL of siRNA loaded NPs (5μM siRNA content).
CRITICAL STEP Thawing siRNA aliquots on ice can minimize the degradation of siRNA. Do not thaw the siRNA aliquots at 37 °C water bath.
-
41
Transfer 20 μL of 100 μM stock siRNA solution (2 nmol) to a 1.7 mL Eppendorf tube.
▲ CRITICAL STEP To prepare NPs containing different types of siRNA, just use different siRNA sequences (e.g. siLuc, Dy647-siLuc, siCamk2g) during the preparation of NPs. No further modifications of the procedures are required.
-
42
Add 100 μL of 2.5 mg/mL G0-C14 acetone solution (250 μg, from Step 33) to the tube to complex the siRNA. Mix by gentle pipetting (10 s) to form siRNA/G0-C14 complexes via the electrostatic interactions.
? TROUBLESHOOTING
-
43
Add 500 μL of 5 mg/mL PLGA acetone solution (2.5 mg, from Step 35) to the tube. Mix by gentle pipetting (10 s) to achieve a homogeneous siRNA/G0-C14/PLGA solution.
-
44
Immediately add the siRNA/G0-C14/PLGA solution dropwise to the 20-mL vial containing 10 mL of the lipid-PEG solution (from Step 37) under stirring (600 rpm).
▲ CRITICAL STEP The acetone solution should be added to the aqueous solution dropwise to allow the assembly of the core-shell structure of the polymer-lipid hybrid NPs. Use the gel loading tips to add the solution, because the speed of adding solutions can be more precisely controlled by this type of tips compared to the normal tips. In addition, immerse the tips in the aqueous solution during the addition instead of on the top of it.
-
45
After the completion of the addition, raise the stirring speed to 1000 rpm and stir the solution at room temperature for 1 h.
▲ CRITICAL STEP The stirring speed is important because vigorous stirring can facilitate the formation of the polymer-lipid hybrid NPs. In another study of our group, we have shown that the stirring time can be shortened to 30 min to minimize the degradation of the nucleic acid cargos at room temperature.30
-
46
Rinse the Amicon Ultra-15 centrifugal filter unit (MW cutoff,100 kDa) with 10 mL of HyPure water, repeat this rinse process 3 times.
-
47
After the completion of the assembly of siRNA NPs, transfer the NP solution (from Step 45) to the Amicon tube.
-
48
Concentrate the NP solutions by centrifugation for 20 min at 3011 × g, 4 °C.
-
49
Wash the NPs by adding 10 mL of HyPure water to the Amicon tube, redisperse the NPs by pipetting. Concentrate the NP solutions by centrifugation for 20 min at 3011 × g, 4 °C.
-
50
Repeat the wash step 3 times.
▲ CRITICAL STEP The centrifugation requires a longer time after the first wash, so increase the time for centrifugation accordingly to make sure that most of the solution is removed by filtration at each wash.
-
51
After the final wash, add 400 μL of PBS (pH 7.4) to redisperse the siRNA NPs. This should result in an siRNA concentration of ~5 μM (RNA encapsulation efficiency is measured in Steps 92-101).
▲ CRITICAL STEP Control the final concentration of siRNA NP by adding a different volume of PBS according to different needs. For example, 400 μL of siRNA NPs with a high siRNA concentration (20 μM of siRNA) are required for Step 92. To this end, add 100 μL of PBS (pH 7.4) to redisperse the siRNA NPs to obtain 100 μL of siRNA NPs with ~20 μM siRNA, combine 4 batches of this solution to obtain 400 μL of siRNA NPs (20 μM of siRNA content).
-
52
Transfer the siRNA NPs (siRNA concentration, 5 μM, 400 μL) to a 1.7 mL Eppendorf tube and put it on ice immediately.
■ PAUSE POINT The siRNA NPs with siRNA concentration of 5 μM or higher can be used freshly prepared or stored at −20 °C for at least 1 month. One freeze-thaw cycle has no significant influence on the effectiveness of the siRNA NPs, however, repeated freeze-thaw cycles should be avoided. If mRNA NPs are prepared, they can be used freshly prepared or stored at −80 °C for two weeks.
Table 2 ∣.
The composition of different siRNA NPs.
| NP formulations | Weight (μg) | |||
|---|---|---|---|---|
| siRNA/G0-C14 (ratio) |
PLGA | DSPE-PEG | DSPE-PEG-S2P (from Step 24) |
|
| S2P0 NPs | 25/250 | 2500 | 1000 | 0 |
| S2P10 NPs | 25/250 | 2500 | 900 | 100 |
| S2P30 NPs | 25/250 | 2500 | 700 | 300 |
| S2P50 NPs | 25/250 | 2500 | 500 | 500 |
Dynamic light scattering (DLS) characterization of siRNA NPs ● Timing ~ 5 h
-
53
Prepare 400 μL of each siLuc NPs (S2P0, and S2P50 NPs, siLuc 5 μM) according to the procedures for the preparation of NPs (Steps 31-52 using the formulations specified in Table 2).
-
54
Add 150 μL of S2P0, or S2P50 NPs (siLuc, 5 μM) to a 1.7 mL Eppendorf tube.
-
55
Add 1.35 mL of PBS (pH 7.4) to the tube to dilute the siLuc NPs.
-
56
Vortex and spin down the solution to achieve 1.5 mL of siLuc NPs (siLuc, 0.5 μM).
▲ CRITICAL STEP The volume of the siLuc NPs has to be enough for the DLS measurement, otherwise unreliable results could be obtained.
-
57
Transfer the siLuc NPs to a cuvette and measure the size (intensity and distribution) of the siLuc NPs by DLS.
? TROUBLESHOOTING
-
58
After the size measurement, recover the sample and measure its zeta potential.
Transmission electron microscope (TEM) characterization of siRNA NPs ● Timing ~ 6 h
-
59
Prepare 400 μL of each siLuc NPs (S2P0, S2P10, S2P30 and S2P50 NPs; siLuc 5 μM) according to the procedure for the preparation of NPs (Steps 31-52 using the formulations specified in Table 2).
-
60
Put a filter paper on the bench.
-
61
Mount the carbon-coated copper grids in a tweezer and rest the tweezer on the filter paper.
-
62
Place 20 μL of S2P0, S2P10, S2P30, or S2P50 NPs on the grid and incubate at room temperature for 10 min.
▲ CRITICAL STEP The volume can be adjusted in the range of 3-20 μL according to the concentration of the NPs.
-
63
After sample incubation, blot the sample with filter paper.
-
64
Wash the sample by placing 3 μL of ultrapure water on the grid.
▲ CRITICAL STEP A second wash can be applied if too much salt is observed in TEM imaging.
-
65
Blot the water with filter paper.
-
66
Immediately place 3 μL of stain solution (UAR-EMS Uranyl acetate replacement stain) on the grid for 10 s and blot the stain solution with filter paper.
-
67
Dry the sample under air for more than 1 h.
-
68
When the sample is completely dry, image the sample using a JEOL 1200EX electron microscope at 80 kV.
? TROUBLESHOOTING
Gel electrophoresis of siRNA NPs ● Timing ~ 16 h
-
69
Prepare 2.8 mL of siLuc NPs (siLuc S2P50 NPs; siLuc 5 μM) according to the procedure for the preparation of NPs (Steps 31-52 using the formulations specified in Table 2. This is a 7-fold larger scale than reported in the above steps).
-
70
Prepare 5 Eppendorf tubes (1.7 mL), add 0.5 mL of fetal bovine serum (FBS) to each tube.
-
71
Add 0.5 mL of siLuc S2P50 NPs (siLuc 5 μM) to each of the 5 tubes containing serum. Prepare an untreated extracted siRNA control: extracted siRNA from siRNA S2P50 NPs without incubation with serum.
-
72
Mix the solution by vortexing and spin down the solution.
▲ CRITICAL STEP Use a solution containing as high as 50% (vol/vol) serum to mimic the in vivo environments.
-
73
Similarly, prepare 5 Eppendorf tubes (1.7 mL), add 0.5 mL of fetal bovine serum (FBS) to each tube. Add 0.5 mL of free siLuc PBS solution (siLuc 5 μM) to each of the 5 tubes containing serum. Mix the solution by vortexing and spin down the solution. Prepare an untreated siRNA control: free siRNA without incubation with serum (incubate with PBS instead).
-
74
Incubate all the 5 siLuc S2P50 NP samples and 5 free siLuc samples at 37°C in a water bath.
-
75
After incubation for different time periods (0, 3, 6, 9, or 12 h), take out one siLuc S2P50 NP sample and one siLuc sample at each time point.
-
76
Transfer the NP samples to Amicon Ultra-15 centrifugal filter units (MWCO, 100 kDa), concentrate the samples by centrifugation at 3011 × g, 4 °C for 15 min.
▲ CRITICAL STEP Adjust the time for centrifugation accordingly if necessary.
-
77
Transfer the concentrated NP samples to 1.7 mL Eppendorf tubes.
-
78
Add 0.5 mL of chloroform to each tube to dissolve the concentrated NP samples.
▲ CRITICAL STEP It’s critical to keep the volume of water in NP samples as low as possible, so the chloroform can efficiently destroy the core-shell structure of the NPs and release the encapsulated siRNA.
-
79
Extract the siLuc by adding 0.5 M NaCl containing 0.1% (wt/vol) SDS to each tube containing chloroform dissolved NP samples.
-
80
Vortex and spin down the solutions.
-
81
Collect the upper aqueous layers.
-
82
Repeat the extraction process 3 times.
-
83
Combine and transfer all the aqueous layers to 2 mL Eppendorf tubes.
-
84
Transfer the free siLuc samples to 2 mL Eppendorf tubes and dilute them to the same volume as the NP samples.
-
85
Store all the 5 NP samples and 5 free siLuc samples at −20 °C.
■ PAUSE POINT The samples can be stored at −20 °C for at least 2 weeks.
-
86
Unpack the ethidium bromide-infused E-Gel 4% (wt/vol) agarose gel and load the gel into a horizontal electrophoresis apparatus.
-
87
Add 20 μL of each of the 10 siRNA samples to 10 Eppendorf tubes (0.6 mL) along with control samples.
-
88
Add 2 μL of loading buffer to each tube, mix them by vortexing and spin down.
-
89
Load 20 μL of each of the 10 siRNA samples to the wells of the agarose gel.
-
90
Run the gel electrophoresis for 30 min using E-Gel Power Snap System (Voltage 48 V).
-
91
After the completion of gel electrophoresis, visualize the agarose gel in an ethidium channel using a Syngene PXi imager.
? TROUBLESHOOTING
Determination of siRNA encapsulation efficiency (EE) ● Timing ~ 4 h
-
92
Prepare 400 μL of Dy647-siLuc NPs (S2P0, and S2P50 NPs; Dy647-siLuc 20 μM) according to the procedure for the preparation of NPs (Steps 31-52 using the formulations specified in Table 2).
▲ CRITICAL STEP Conduct all the handling with Dy647-siLuc in the dark since the Dy647 is very sensitive to light exposure.
-
93
Add 5 μL of Dy647-siLuc S2P0 or S2P50 NPs to a 0.6 mL Eppendorf tube.
-
94
Add 95 μL of DMSO to the tube to dissolve the NPs and release the encapsulated Dy647-siLuc.
-
95
Mix the solution by vortexing and spin down the solution (final feeding Dy647-siLuc, 1 μM).
▲ CRITICAL STEP It is critical to completely dissolve the NPs in DMSO because the incomplete dissolution of the NPs can lead to the decrease of siRNA EE. Repeat the vortexing process if necessary.
-
96
Similarly, prepare a free Dy647-siLuc solution (Dy647-siLuc, 20 μM). Add 5 μL of free Dy647-siLuc to a 0.6 mL Eppendorf tube containing 95 μL of DMSO. Mix the solution by vortexing and spin down the solution (final free Dy647-siLuc, 1 μM).
-
97
Prepare all the samples in 6 replicates.
-
98
Transfer 90 μL of each sample to a 96-well plate.
-
99
Prepare a Blank control: Transfer 90 μL of 95% (vol/vol) DMSO solution to the 96-well plate.
-
100
Measure the fluorescence intensities of all the samples using an Infinite M200 PRO spectrophotometer (ex. 645 nm, em. 680 nm).
-
101The siRNA EE of NPs can be calculated according to the following equation:
? TROUBLESHOOTING
Evaluation of the stability of siRNA NPs ● Timing ~ 3 d
-
102
Prepare 800 μL of siLuc NPs (S2P0, and S2P50 NPs; siLuc, 5 μM) according to the procedure for the preparation of NPs (Steps 31-52 using the formulations specified in Table 2. The procedure will need to be doubled to produce the required amount of NPs for this assay).
-
103
Add 200 μL of siLuc S2P0 or S2P50 NPs to a 2 mL Eppendorf tube. Prepare all the samples in triplicates.
-
104
Add 1.6 mL of PBS and 200 μL of FBS to each of the tubes to dilute the siLuc NPs.
-
105
Mix the solution by vortexing and spin down the solution.
-
106
Incubate the siLuc NP solutions at 37 °C over 3 days. At different time points (0, 12, 24, 36, 48, 60, and 72 h), take out the siLuc NPs and transfer 1.5 mL of them to a cuvette.
-
107
Prepare an untreated siRNA NP control in triplicate: the freshly prepared siLuc NPs without incubation with PBS containing 10% (vol/vol) serum.
-
108
Monitor the sizes of the NPs by DLS, recover the samples, and then continue incubating them at 37 °C.
▲ CRITICAL STEP It is normal that the NPs in FBS show an extra 20 nm peak compared to the NPs in PBS, because this peak belongs to FBS.
Characterization of the endosomal escape of siRNA NPs ● Timing ~ 30 h
-
109
Seed 1 mL of HeLa-Luc cells in Nunc glass-bottom dishes at a density of 2 × 105 cells per well (complete RPMI 1640 medium). Incubate the cells at 37 °C in a humidified incubator containing 5% (vol/vol) CO2 for 24 h.
-
110
Prepare 400 μL of Dy647-siLuc NPs (S2P50 NPs; Dy647-siLuc 5 μM) according to the procedure for the preparation of NPs (Steps 31-52 using the formulations specified in Table 2)
-
111
Add 10 μL of Dy647-siLuc NPs to a 1.7 mL Eppendorf tube. Prepare the samples in duplicates.
-
112
Add 1 mL of RPMI 1640 medium to each of the tubes to dilute the NPs.
-
113
Mix the solution by pipetting gently.
-
114
Remove the cell medium (from Step 109), add 1 mL of medium containing Dy647-siLuc NPs to each of the two duplicate wells, respectively. The final concentration of Dy647-siLuc in each well is 50 nM.
-
115
Put the cells back in the incubator.
-
116
Remove the NPs after 1 h or 4 h incubation. Wash the cells 3 times with PBS.
-
117
Stain the late endosome of the cells by adding 1 mL of medium containing 50 μM Hoechst 33342 (stock solution 1 mM) and incubate for 30 min.
▲ CRITICAL STEP The incubation time can be varied from 30 min to 2 h depending on the cell type and density.
-
118
Remove the staining solution and rinse the cells 3 times with PBS.
-
119
Stain the nuclei of the cells by adding 1 mL of medium containing 5 μg/mL Hoechst 33342 (stock solution 10 mg/mL) and incubate for 20 min.
▲ CRITICAL STEP The nuclei can be easily over-stained, so decrease the incubation time if necessary.
-
120
Remove the staining solution and rinse the cells 3 times with PBS.
-
121
Add 1 mL of fresh medium to the cells, and then observe and image the cells using an FV1000 laser scanning confocal microscope.
? TROUBLESHOOTING
In vitro evaluation of gene silencing by siRNA NPs ● Timing ~ 2 d
-
122
Seed 1 mL of HeLa-Luc cells in a 12-well plate at a density of 6 × 104 cells per well (complete RPMI 1640 medium). Incubate the cells at 37 °C in a humidified incubator containing 5% (vol/vol) CO2 for 24 h (or until 50-70% confluent).
-
123
Prepare 400 μL of siLuc NPs (S2P50 NPs; Dy647-siLuc 5 μM) according to the procedure for the preparation of NPs (Steps 31-52 using the formulations specified in Table 2.)
-
124
Add 2.5, 5, and 10 μL of Dy647-siLuc NPs to 3 Eppendorf tubes (1.7 mL), respectively. Prepare all the samples in triplicates. Prepare a PBS control (or 0 nM siLuc): for the bioluminescence signal of cells treated with PBS.
-
125
Add 1 mL of RPMI 1640 medium to each of the tubes to dilute the NPs.
-
126
Mix the solution by pipetting gently.
-
127
Remove the cell medium, add 1 mL of the medium containing Dy647-siLuc NPs (or the PBS control) to the cells (in triplicate). Final concentrations of Dy647-siLuc in the wells are 0, 12.5, 25, and 50 nM, respectively.
▲ CRITICAL STEP For optimal gene silencing efficiency, make sure the cells are 50-70% confluent at the time of adding NPs.
-
128
Put the cells back in the incubator.
-
129
Remove the NPs after 24 h incubation. Add 1 mL of medium containing Steady-Glo Luciferase reagent (substrate) to the cells and keep the cells in the incubator for 5 min.
▲ CRITICAL STEP Steady-Glo Luciferase reagents can easily lose their activities through repeated freeze-thaw cycles, divide the reagent into aliquots and always protect from light.
-
130
Determine the luciferase expression of the cells by measuring their bioluminescence signals using an In-Vivo Xtreme imaging system with a charge-coupled device (CCD) camera.
-
131
Determine the gene silencing efficiency by quantifying the average radiance (photons per second per cm2 per steradian) within regions of interest using Bruker MI SE software.
? TROUBLESHOOTING
In vitro viability assessment of siRNA NPs ● Timing ~ 4 d
-
132
Seed 100 μL of HeLa-Luc (RPMI 1640 medium), RAW 264.7 (DMEM medium), and HEK-293 (EMEM medium) cells in three 96-well plates at a density of 5 × 103 cells per well, respectively. Incubate the cells at 37 °C in a humidified incubator containing 5% (vol/vol) CO2 for 24 h. Prepare a Blank control – wells without cells: to measure the absorbance of medium without any cells. Prepare enough wells to run 5 replicates of each sample.
-
133
Prepare 400 μL of siLuc NPs (S2P50 NPs; siLuc 5 μM) according to the procedure for the preparation of NPs (Steps 31-52 using the formulations specified in Table 2)
-
134
Add 2.5, 5, 10, and 20 μL of siLuc NPs to 4 Eppendorf tubes (2 mL), respectively. Add 2 mL of RPMI 1640 medium to each of the tubes to dilute the NPs. Prepare a PBS control: to measure the absorbance of cells treated with PBS.
-
135
Mix the solution by pipetting gently.
-
136
Remove the cell medium, add 100 μL of the medium containing siLuc NPs (or PBS control) to the wells of each plate. Prepare 5 replicate wells for each NP sample. The final concentrations of siLuc in the wells are 0, 6.25, 12.5, 25, and 50 nM, respectively.
-
137
Put the cells back in the incubator.
-
138
Remove the NPs after 24 h incubation. Add fresh medium to the cells and incubate for another 48 h.
▲ CRITICAL STEP The evaporation of cell medium in the outer wells of the 96 well plate is significant after 48 h incubation, which can influence the growth of cells. So, we recommend only using the inner wells of the plate.
-
139
Remove the cell medium and add 100 μL of medium containing alamarBlue cell viability and proliferation reagents (add 10 μL alamarBlue reagents to 90 μL of medium) to the cells.
-
140
Put the cells back in the incubator and incubate for 1 h.
-
141
Determine the viability of the cells by measuring the absorbance at 570 nm using a plate reader.
-
142Calculate the viability of NP-treated cells according to the following equation:
In vitro apoptosis assessment of siRNA NPs ● Timing ~ 4 d
-
143
Seed 0.5 mL of RAW 264.7 (DMEM medium) cells in a 24-well plate at a density of 3 × 104 cells per well. Incubate the cells at 37 °C in a humidified incubator containing 5% (vol/vol) CO2 for 24 h.
-
144
Prepare 400 μL of siLuc NPs (S2P0 NPs, S2P50 NPs; siLuc 5 μM) according to the procedure for the preparation of NPs (Steps 31-52 using the formulations specified in Table 2)
-
145
Add 20 μL of S2P0 NPs and S2P50 NPs to 2 Eppendorf tubes (2 mL), respectively. Add 2 mL of DMEM medium to each of the tubes to dilute the NPs. Prepare a PBS control: to later measure the apoptosis of cells treated with only PBS.
-
146
Mix the solution by pipetting gently.
-
147
Remove the cell medium, add 0.5 mL of medium containing siLuc NPs (or PBS control) to the cells. Prepare 3 replicates for each NP sample. The final concentration of siLuc in each well is 50 nM.
-
148
Put the cells back in the incubator.
-
149
Remove the NPs after 24 h incubation. Add fresh medium to the cells and incubate for another 48 h.
-
150
Remove the cell medium, wash once with PBS, detach cells with trypsin, wash and collect the cells by centrifugation (1000 × g, 4 °C, 5 min).
-
151
Double stain the cells with Annexin V (AV)-FITC and propidium iodide (PI) (Annexin V-FITC Apoptosis Detection kit). Prepare a Blank control: Unstained cells. Prepare a AV-FITC control: Cells stained with AV-FITC (no PI). Prepare a PI control: Cells stained with PI (no AV-FITC).
▲ CRITICAL STEP Keep the stained cells in dark or cover them with aluminum foil due to the light sensitivity of AV-FITC and PI.
-
152
Determine the degree of apoptosis of the cells by flow cytometry. Analyze AV-FITC staining using the FITC signal detector and PI staining using the phycoerythrin (PE) emission signal detector. For the gating strategy for flow cytometry: first, set a live gate (gate 1) in the FSC (forward scatter)/SSC (side scatter) plot to exclude cell debris. Then, use the cell populations from gate 1 for the downstream AV/PI display. Flow cytometry density plots show AV (X-axis) and PI (Y-axis) staining of cells. The right lower quadrant represents AV positive/PI negative staining indicating early apoptosis. The right upper quadrant represents both high AV and PI staining indicating late apoptosis. The left upper quadrant represents low AV and high PI staining indicating necrosis. The left lower quadrant indicates viable cells.
? TROUBLESHOOTING
In vitro proliferation assessment of siRNA NPs ● Timing ~ 8 d
-
153
Seed 2 mL of RAW 264.7 (DMEM medium) cells in a 6-well plate at a density of 2 × 104 cells per well. Incubate the cells at 37 °C in a humidified incubator containing 5% (vol/vol) CO2 for 24 h. Prepare enough cell-seeded wells to run triplicate of each sample. Leave several wells empty as a Blank control: to later measure the absorbance of medium without cells.
-
154
Prepare 400 μL of siLuc NPs (S2P0 NPs, S2P50 NPs; siLuc 5 μM) according to the procedure for the preparation of NPs (Steps 31-52 using the formulations specified in Table 2.)
-
155
Add 80 μL of S2P0 NPs and S2P50 NPs to 2 falcon tubes (15 mL), respectively. Add 8 mL of DMEM medium to each of the tubes to dilute the NPs.
-
156
Mix the solution by pipetting gently.
-
157
Remove the cell medium, add 2 mL of medium containing siLuc NPs (or PBS control) to the cells. Prepare 3 replicates for each NP sample. The final concentration of siLuc in each well is 50 nM.
-
158
Put the cells back in the incubator.
-
159
Remove the NPs after 24 h incubation. Add fresh medium to the cells and incubate for another 7 days.
-
160
At each time point (day 1, 2, 3, 4, 5, 6, and 7), remove the cell medium and add 2 mL of medium containing alamarBlue cell viability and proliferation reagents to the cells.
▲ CRITICAL STEP Handle the alamarBlue reagents in dark due to their light sensitivity.
-
161
Put the cells back to the incubator and incubate for 1 h.
-
162
Determine the proliferation of the cells by measuring the absorbance at 570 nm using a plate reader.
-
163
Remove the medium containing alamarBlue reagents after each measurement, and add fresh medium to cells to allow the continued growth of the cells.
-
164Calculate the proliferation of the cells according to the following equation:
Treatment of WD-fed Ldlr−/− mice with S2P50 siCamk2g NPs ● Timing ~ 4 weeks
-
165
Prepare 2 mL of S2P50 siCamk2g NPs and S2P50 siCtrl NPs (siRNA 5 μM) according to the procedure for the preparation of NPs (2 mL of NPs is required for single-dose injection for 7~9 mice). The siCtrl NPs is the control NPs prepared using non-therapeutic siLuc. Follow Steps 31-52 using the formulations specified in Table 2. This is 5-fold larger scale than reported in the above steps.
? TROUBLESHOOTING
-
166
After establishing the mouse model of atherosclerosis (see Reagent setup section), randomly divide the mice into 3 groups and inject intravenously two doses of PBS, S2P50 siCtrl NPs (1 nmol siRNA per injection, 200 μL), or S2P50 siCamk2g NPs (1 nmol siRNA per injection, 200 μL) per week to the mice, respectively. In each week, inject the second dose 3 or 4 days after the injection of the first dose. For statistical analysis, n = 7 to 9 mice per group are required per assay.
? TROUBLESHOOTING
-
167
Maintain the mice on the WD during the treatment period.
-
168
After 4 weeks of treatment, euthanize the mice with CO2, collect the blood by left ventricular puncture, and perfuse the vasculature with cold PBS.
-
169
Fix the heart with attached aortic roots in 4% (wt/vol) paraformaldehyde followed by paraffin embedding or treat it with optical cutting temperature (OCT) compound and freeze it.
-
170
Isolate sections of the aortic root with sizes of 8- or 6-μm from the acetone-fixed/paraffin-embedded or frozen samples for the analysis of atherosclerotic lesions.
Silence of CaMKIIγ in lesional macrophages of WD-fed Ldlr−/− mice ● Timing ~ 2 d
-
171
Block the obtained aortic root sections with 1% (wt/vol) bovine serum albumin (BSA) at room temperature for 1 h. For statistical analysis, n = 7 to 9 sections per group are required per assay.
-
172
Incubate the sections with primary anti-CaMKIIγ (1:400) and anti-Mac2 (1:10, 000), or with anti-MerTK (1:500) at 4°C overnight.
▲ CRITICAL STEP To maintain the optimal activity of the primary antibody, handle the antibodies on ice.
-
173
Rinse the sections with PBS three times.
-
174
Incubate the sections with fluorescently labeled secondary antibodies for 2 h at room temperature.
-
175
After rinsing the sections with PBS three times, incubate the sections with 4′,6-diamidino-2-phenylindole phenylindole (DAPI) for 20 min at room temperature.
▲ CRITICAL STEP Keep the stained sections in the dark or cover them with aluminum foil due to the light sensitivity of the dye-labelled antibodies and DAPI.
-
176
Rinse the sections (n = 7 to 9 sections per group) with PBS three times. Observe and image the sections using a Zeiss epifluorescence microscope, and analyze the images using FIJI software. The PBS treated control is used to investigate gene silencing of sections from mice treated by PBS. The siCtrl NPs treated control is used to investigate gene silencing of sections from mice treated by S2P50 siCtrl NPs.
? TROUBLESHOOTING
Efferocytosis in lesional macrophages of WD-fed Ldlr−/− mice ● Timing ~ 2 d
-
177
Incubate the Acetone-fixed aortic root sections (from Step 170) with TUNEL staining reagents at 37°C for 1 h. For statistical analysis, n = 7 to 9 sections per group are required per assay.
-
178
Wash the sections three times with PBS.
-
179
Block the sections with 1% (wt/vol) BSA at room temperature for 1 h.
-
180
Incubate the sections with primary anti-Mac2 (1:10, 000) at 4°C overnight.
-
181
Rinse the sections with PBS three times.
-
182
Incubate the sections with fluorescently labeled secondary antibodies for 2 h at room temperature.
-
183
After rinsing the sections with PBS three times, incubate the sections with DAPI for 20 min at room temperature.
▲ CRITICAL STEP Keep the stained sections in the dark or cover them with aluminum foil.
-
184
Rinse the sections with PBS three times. Observe and image the sections using a Zeiss epifluorescence microscope, and analyze the images using FIJI software.
-
185
Quantify the lesional efferocytosis as the ratio of TUNEL+ cells (red) in contact with Mac2+ macrophages (green) to isolated TUNEL+ cells. The PBS treated control is used to investigate efferocytosis of sections from mice treated by PBS. The siCtrl NPs treated control is used to investigate efferocytosis of sections from mice treated by S2P50 siCtrl NPs.
Plaque stability of WD-fed Ldlr−/− mice ● Timing ~ 2 d
-
186
Stain the collagen of aortic root sections (from Step 170) with picrosirius red according to the manufacturer’s instructions. For statistical analysis, n = 7 to 9 sections per group are required per assay.
-
187
Observe and image the sections with light microscopy.
-
188
Obtain the necrotic core area by measuring the area from the images.
-
189
Quantify the fibrous (collagen) cap thickness from one midpoint and two shoulder regions of the plaque and normalize it to the lesion size (Figure 5h, g, i, j). The PBS treated control is used to investigate plaque stability of sections from mice treated by PBS. The siCtrl NPs treated control is used to investigate plaque stability of sections from mice treated by S2P50 siCtrl NPs.
Fig. 5. In vivo therapeutic effect of siCamk2g NPs.
Eight-week WD-fed Ldlr−/− mice were injected intravenously with two doses of PBS, S2P50 siCtrl NPs (1 nmol siRNA per injection), or S2P50 siCamk2g NPs (1 nmol siRNA per injection) per week for 4 weeks. n = 7 to 9 mice per group. a-d, Sections of the aortic root were immunostained for CaMKIIγ, MerTK, and Mac2. Nuclei were stained with DAPI. Scale bars, 200 μm. The mean fluorescence intensity (MFI) of each group was normalized to the PBS group. e-f, TUNEL assay was used to characterize the apoptotic cells (ACs) of sections of the aortic root. The lesional efferocytosis was quantified as the ratio of TUNEL+ cells (red) in contact with Mac2+ macrophages (green) to isolated TUNEL+ cells. Arrows indicate isolated or free TUNEL+ cells, and arrowheads indicate TUNEL+ cells in contact with Mac2+ macrophages. Scale bars, 50 μm. g-j, Sections of the aortic root were stained with picrosirius red to determine the lesion size and necrotic core area. The fibrous (collagen) cap thickness is quantified from one midpoint and two shoulder regions of the plaque and normalized to the lesion size. Scale bars, 200 μm. *P < 0.05 in one-way ANOVA. Data are presented as mean ± SEM. a-j, Adapted with permission from ref.26, American Association for the Advancement of Science. All the animal procedures were conducted in accordance with the protocols reviewed and approved by IACUC at Harvard Medical School and Columbia University Irving Medical Center.
In vivo evaluation of the toxicity of S2P50 siCamk2g NPs ● Timing ~ 5 weeks
-
190
Purchase six-week-old female BALB/c mice from Jackson laboratory.
-
191
Conduct all the procedures under the protocols approved by the Institutional Animal Care and Use Committees at your institution.
-
192
Prepare 800 μL of S2P50 siCamk2g NPs (siRNA 5 μM) according to the procedure for the preparation of NPs. Follow Steps 31-52 using the formulations specified in Table 2. This is 2-fold larger scale than reported in the above steps.
-
193
Randomly divide the mice into 2 groups and inject intravenously two doses of PBS or S2P50 siCamk2g NPs (1 nmol siRNA per injection, 200 μL) per week to the mice, respectively. For statistical analysis, n = 3 mice per group.
-
194
After 4 weeks of administration, euthanize the mice with CO2 three days after the last administration, collect the blood by left ventricular puncture.
▲ CRITICAL STEP After blood collection, immediately turn the blood collection tubes upside down a few times to mix blood with the anticoagulants.
-
195
Collect the major organs and fix them in 4% (wt/vol) paraformaldehyde followed by paraffin embedding.
-
196
Isolate sections from the paraffin-embedded organs, statin them with hematoxylin solution and eosin Y solution (H&E) according to the manufacturer’s instructions.
-
197
Observe and image the sections with microscopy.
-
198
Evaluate various hematological parameters of the blood, including alanine aminotransferase (ALT), aspartate aminotransferase (AST), blood urea nitrogen (BUN), hematocrit (HCT), hemoglobin (Hb), lymphocyte count (LY), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), neutrophil count (NPC), red blood cell count (RBC), and white blood cell count (WBC). PBS treated control is used to investigate H&E staining of sections from mice treated by PBS; hematological parameters of the blood from mice treated by PBS.
Timing
Steps 1-14, synthesis of cationic lipid (G0-C14): 3 d
Steps 15-24, synthesis of ligand-modified lipid-PEG (DSPE-PEG-S2P): 3 d
Steps 25-30, preparation of siRNA stock solution: 1 h
Steps 31-52, preparation of siRNA-loaded NPs: 4 h
Steps 53-58, dynamic light scattering (DLS) characterization of siRNA NPs: 5 h
Steps 59-68, transmission electron microscope (TEM) characterization of siRNA NPs: 6 h
Steps 69-91, gel electrophoresis of siRNA NPs: 16 h
Steps 92-101, determination of the siRNA encapsulation efficiency (EE): 4h
Steps 102-108, evaluation of the stability of siRNA NPs: 3 d
Steps 109-121, characterization of the endosomal escape of siRNA NPs: 30 h
Steps 122-131, in vitro evaluation of gene silencing by siRNA NPs: 2 d
Steps 132-142, in vitro viability assessment of siRNA NPs: 4 d
Steps 143-152, in vitro apoptosis assessment of siRNA NPs: 4 d
Steps 153-164, in vitro proliferation assessment of siRNA NPs: 8 d
Steps 165-170, treatment of WD-fed Ldlr−/− mice with S2P50 siCamk2g NPs: 4 weeks
Steps 171-176, the silence of CaMKIIγ in lesional macrophages of WD-fed Ldlr−/− mice: 2 d
Steps 177-185, efferocytosis evaluation in lesional macrophages of WD-fed Ldlr−/− mice: 2 d
Steps 186-189, plaque stability evaluation of WD-fed Ldlr−/− mice: 2 d
Steps 190-198, in vivo evaluation of the toxicity of S2P50 siCamk2g NPs: 5 weeks
Troubleshooting
Troubleshooting advice can be found in Table 3
Table 3 ∣.
Troubleshooting table.
| Steps | Problem | Possible reason | Solution |
|---|---|---|---|
| 10 | No product | G0-C14 is stuck on the silica gel | Increase the percentage of MeOH to increase the polarity of the eluent |
| 14 | Low yield of G0-C14 product | The amines of G0 are partially oxidized, resulting in a yellow G0 solution | Always store the G0 solution in a 4 °C fridge and flush the bottle with argon after each use to protect the amines from oxidization. |
| 24 | Low yield of DSPE-PEG-S2P product | The peptide S2P is not completely dissolved. | Warm up the solution at 37 °C in a water bath or add more HEPES buffer. |
| 42 | Precipitation of siRNA | The vigorous mixing process changes the homogenous state of the siRNA/G0-C14 solution | Mixing the siRNA/G0-C14 solution by gentle pipetting. Do not vortex the solution |
| 57 | Poor reproducibility of DLS results | The siLuc NPs are too diluted and below the DLS detection limit or the extreme dilution destabilizes the NPs. | Adjust the dilution factor according to the detection limit of the DLS instrument and do not dilute too much. |
| 68 | Poor contrast of TEM images | The volume of staining solution is not large enough or incubation time is too short | Increase the volume of the staining solution or increase the incubation time |
| Very few samples in TEM images | The sample is too diluted | Increase the concentration of the sample, or repeat the sample loading procedure several times | |
| The background is too dark in TEM images | The incubation time for the staining solution is too long | Decrease the incubation time of the staining solution | |
| 91 | The gel bands are too weak | The siRNA concentration is too low | Before gel electrophoresis, concentrate the siRNA samples using Amicon tubes (MWCO, 10 kDa) |
| 101 | Low siRNA EE | Fail to transfer all the Dy647-siLuc NPs from the Amicon tube | Pipette the Dy647-siLuc NPs solution vigorously before transferring; Also, wash the tube one or two times with a small volume of PBS. |
| 121 | Low fluorescence signals of Dy647 | The concentration of Dy647-siLuc NPs is too low or the cell density is too high | Raise the concentration of Dy647-siLuc NPs or decrease the cell density. |
| 131 | Low bioluminescence signal | The bioluminescence signal decays | Prepare and warm up the imaging system before adding the substrate. Upon adding the substrate, finish the measurement within 10 min. |
| Low gene silencing efficiency | G0-C14 is degraded | The G0-C14 can be easily degraded after dissolution in the solvent. Aliquot the G0-C14 solution and store aliquots at −20 °C. Do not use the same batch more than three times. | |
| 152 | All the samples are PI positive | The PI staining process is too long | Shorten the PI staining process; Finish the measurement within 1 h after the PI staining |
| 165 | The centrifugation takes too much time | The concentration of siRNA NPs is too high, making the ultrafiltration difficult | Split the samples into more Amicon tubes for washing, combine and transfer all the samples to one Amicon tube to adjust the concentration of NPs for in vivo injection |
| 166 | The volume of the NPs is too large for injection | The siRNA concentration is too low | Add less PBS to redisperse the NPs during the preparation of NPs |
| 176 | Weak fluorescence signal of the sections | Low activity of the primary antibody or the primary antibody concentration is too low | Handle the primary antibodies on ice to retain their optimal activity; Decrease the dilution factor of the primary antibodies. |
Anticipated results
Following this protocol, researchers will be able to synthesize the NP components, prepare the siRNA-loaded polymer-lipid hybrid NPs and characterize the NPs. We also describe the in vivo treatment of atherosclerosis in a mouse model as one of the applications of our polymer-lipid hybrid NPs. The results generated by this protocol can be anticipated based on our previous studies.26,60 For the synthesis of G0-C14, a light green solid with a yield of about 50% was achieved from 1.0 g of G0 starting material. The conjugation of DSPE-PEG-Mal (200 mg) with S2P (63.7 mg) produced a white powder (DSPE-PEG-S2P) with a yield of about 30%. The structures of G0-C14 and DSPE-PEG-S2P were confirmed by 1H NMR analysis, which can be found in Supplementary Fig. 1.
The physicochemical properties of the siRNA NPs were characterized by DLS and TEM. The non-targeted siRNA NPs (S2P0 NPs) had a diameter of 108 ± 2.8 nm (intensity size distribution) and a zeta potential of −7.43 ± 0.94 mV (Fig. 4a, b). As expected, the conjugation of S2P ligand to the NPs resulted in targeted S2P50 NPs with a slightly increased diameter of 116.2 ± 2.5 nm (intensity size distribution) and zeta potential of −2.66 ± 1.01 mV. TEM images revealed that both the non-targeted (S2P0 NPs) and targeted (S2P50 NPs) NPs had spherical morphologies (Fig. 4d). It is worth noting that both S2P0 and S2P50 NPs had similar siRNA EE of about 50% (Fig. 4c). The stability of the siRNA NPs in biological media is critical to their long blood circulation, which allows the accumulation of siRNA NPs at lesional sites. We demonstrated that the S2P0 and S2P50 NPs were stable in PBS solution containing 10% (vol/vol) serum at 37 °C for at least 3 days as evidenced by the negligible changes in their particle size (Supplementary Fig. 2a, b). We further confirmed that the S2P50 NPs could efficiently protect the siRNA from enzymatic degradation when incubated in serum solution (Supplementary Fig. 2c). Importantly, our siRNA NPs were able to escape from the endosomes after 4 h incubation with HeLa-Luc cells as demonstrated by the confocal microscopy images (Supplementary Fig. 3).
Fig. 4. Physicochemical and in vitro characterization of siRNA NPs.
a-b, Size and zeta potential of siRNA NPs (S2P0 and S2P50) were determined by DLS. Polydispersity index (PDI). n = 3. c, siRNA encapsulation efficiency (EE) of S2P0 and S2P50 NPs was measured by plate reader. Dy647-siRNA was loaded into the NPs (n.s., not significant). n = 6. d, Transmission electron microscopy (TEM) images of S2P0 and S2P50 NPs. e-f, In vitro gene silencing of siRNA NPs. HeLa (HeLa-Luc) cells were incubated with S2P50 NPs containing varying concentrations of siLuc for 24 h, and their luciferase-expressing was characterized by bioluminescence imaging. The average radiance of the cells was quantified. n = 3. Data are presented as mean ± SEM. ****P < 0.0001 in one-way ANOVA. a-f, Adapted with permission from ref.26, American Association for the Advancement of Science.
We then evaluated the gene silencing effect of siRNA NPs in HeLa-Luc cells. Our siLuc-loaded S2P50 NPs were able to effectively silence the Luc expression of HeLa-Luc cells at a siLuc concentration as low as 12.5 nM as demonstrated by the bioluminescence imaging (Fig. 4e, f). In addition, the in vitro biocompatibility of the siRNA NPs was assessed by different assays. The HeLa-Luc, RAW 264.7 and HEK-293 cells treated with S2P50 NPs containing varying concentrations of siLuc (6.25-50 nM) displayed high cell viabilities of more than 80% (Supplementary Fig. 4a). The treatment of RAW 264.7 cells with S2P0 and S2P50 NPs (siLuc 50 nM) induced minimal cell apoptosis comparable to that induced by PBS (Supplementary Fig. 4b). Both of the S2P0 and S2P50 NPs (siLuc 50 nM) did not show any significant inhibitions to the growth of RAW 264.7 cells after monitoring their proliferation as long as 7 days (Supplementary Fig. 4c).
Next, we assessed the in vivo applications of our polymer-lipid hybrid NPs using the treatment of atherosclerosis in a mouse model as an example. To this end, we first established a mouse model of atherosclerosis by feeding the Ldlr gene-deficient (Ldlr−/−) mice with a high-fat Western diet (WD) for 8 weeks. The resulting WD-fed Ldlr−/− mice were intravenously injected with either PBS, S2P50 siCtrl NPs, or S2P50 siCamk2g NPs. After the treatment, the sections of the aortic roots of the mice were isolated for analysis of the therapeutic effect of NPs. The immunofluorescence imaging revealed that the S2P50 siCamk2g NPs could efficiently silence the expression of the CaMKIIγ in the lesional macrophages, resulting in the activation of the MerTK pathway (Fig. 5a-d). TUNEL assay showed that the S2P50 siCamk2g NPs-induced activation of the MerTK pathway could significantly promote the lesional efferocytosis (Fig. 5e-f). Consequently, plaque stability was improved in the S2P50 siCamk2g NP-treated groups as evidenced by the smaller necrotic area and thicker fibrous cap compared to that of the PBS or S2P50 siCtrl NP-treated groups (Fig. 5g-j).
We also investigated the in vivo toxicity of our polymer-lipid hybrid NPs under the same conditions (e.g. dose, frequency) as the assay for therapeutic effect evaluation. To this end, BALB/c mice were injected intravenously with PBS or S2P50 siCamk2g NPs for 4 weeks, two doses per week. After the treatment, sections of the major organs and blood of the mice were isolated and collected for analysis of the toxicity of NPs. No obvious damage to the major organs of NP-treated mice was observed as indicated by the H&E staining images (Fig. 6a). In addition, blood from both PBS- and NP-treated mice showed no significant differences in a wide range of hematological parameters, including alanine aminotransferase (ALT), aspartate aminotransferase (AST), blood urea nitrogen (BUN), hematocrit (HCT), hemoglobin (Hb), lymphocyte count (LY), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), neutrophil count (NPC), red blood cell count (RBC), and white blood cell count (WBC) (Fig. 6b).
Fig. 6. In vivo toxicity assessment of siCamk2g NPs.
Six-week-old female BALB/c mice were injected intravenously with two doses of PBS or S2P50 siCamk2g NPs (1 nmol siRNA per injection) per week for 4 weeks. n = 3 mice per group. The mice were euthanized by CO2 inhalation three days after the last administration. a, the major organs were sectioned followed by H&E staining. Scale bars, 100 μm. b, Blood was collected and various hematological parameters were evaluated, including alanine aminotransferase (ALT), aspartate aminotransferase (AST), blood urea nitrogen (BUN), hematocrit (HCT), hemoglobin (Hb), lymphocyte count (LY), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean corpuscular hemoglobin concentration (MCHC), neutrophil count (NPC), red blood cell count (RBC), and white blood cell count (WBC). Data are presented as mean ± SEM. The differences between PBS and S2P50 siCamk2g NPs groups are not statistically significant for all parameters (Student’s t test). a-b, Adapted with permission from ref.26, American Association for the Advancement of Science. All the animal procedures were conducted in accordance with the protocols reviewed and approved by IACUC at Harvard Medical School and Columbia University Irving Medical Center.
Supplementary Material
Acknowledgements
This study is supported by the American Heart Association (AHA) Collaborative Science Award (No. 2018A004190; to W. Tao), Harvard Medical School/Brigham and Women’s Hospital Khoury Innovation Award (No. 2020A003219; to W. Tao), Anesthesiology Department Basic Scientist Grant (No. 2420 BPA075; to W. Tao), Center for Nanomedicine Research Fund No.2019A014810; to W. Tao), National Institutes of Health (HL127464, HL145228, and HL087123; to I. Tabas), and National Institutes of Health (R00 HL145131; to A. Yurdagul). W. Tao also received a start-up package (for 3 years) from the Department of Anesthesiology, Perioperative and Pain Medicine to establish his independent research laboratory at Harvard Medical School and Brigham and Women’s Hospital.
Appendix
Related links
Key references using this protocol
- Tao W et al. Sci. Transl. Med 12, eaay1063 (2020) (DOI: 10.1126/scitranslmed.aay1063): https://stm.sciencemag.org/content/12/553/eaay1063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu X et al. Proc. Natl. Acad. Sci 112, 7779–7784 (2015) (DOI: 10.1073/pnas.1505629112): https://www.pnas.org/content/112/25/7779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam MA et al. Nat. Biomed. Eng 2, 850–864 (2018) (DOI: 10.1038/s41551-018-0284-0): https://www.nature.com/articles/s41551-018-0284-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong N et al. Sci. Transl. Med 11, eaaw1565 (2019) (DOI: 10.1126/scitranslmed.aaw1565): https://stm.sciencemag.org/content/11/523/eaaw1565 [DOI] [PMC free article] [PubMed] [Google Scholar]
Footnotes
Competing interests
The authors declare no competing interests.
Supplementary information
Supplementary information is available for this paper.
Data availability
The authors declare that the main data discussed in this protocol are available in the supporting primary research papers (https://doi.org/10.1126/scitranslmed.aay1063) and https://doi.org/10.1073/pnas.1303958110). The raw datasets are available for research purposes from the corresponding authors upon reasonable request.
Reference
- 1.Schultze JL, Schmieder A & Goerdt S Macrophage activation in human diseases. Semin. Immunol 27, 249–256 (2015). [DOI] [PubMed] [Google Scholar]
- 2.Moore Kathryn J. & Tabas I Macrophages in the Pathogenesis of Atherosclerosis. Cell 145, 341–355 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ross R Atherosclerosis — An Inflammatory Disease. N. Engl. J. Med 340, 115–126 (1999). [DOI] [PubMed] [Google Scholar]
- 4.Kuznetsova T, Prange KHM, Glass CK & de Winther MPJ Transcriptional and epigenetic regulation of macrophages in atherosclerosis. Nat. Rev. Cardiol 17, 216–228 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shi J, Kantoff PW, Wooster R & Farokhzad OC Cancer nanomedicine: progress, challenges and opportunities. Nat. Rev. Cancer 17, 20–37 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhu X et al. Long-circulating siRNA nanoparticles for validating Prohibitin1-targeted non-small cell lung cancer treatment. Proc. Natl. Acad. Sci 112, 7779–7784 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davidson BL & McCray PB Current prospects for RNA interference-based therapies. Nat. Rev. Genet 12, 329–340 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Whitehead KA, Langer R & Anderson DG Knocking down barriers: advances in siRNA delivery. Nat. Rev. Drug Discovery 8, 129–138 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castanotto D & Rossi JJ The promises and pitfalls of RNA-interference-based therapeutics. Nature 457, 426–433 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen J et al. Synthesis and use of an amphiphilic dendrimer for siRNA delivery into primary immune cells. Nat. Protoc 16, 327–351 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loynachan CN et al. Renal clearable catalytic gold nanoclusters for in vivo disease monitoring. Nat. Nanotechnol 14, 883–890 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Terrazas M & Kool ET RNA major groove modifications improve siRNA stability and biological activity. Nucleic Acids Res. 37, 346–353 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sioud M, Furset G & Cekaite L Suppression of immunostimulatory siRNA-driven innate immune activation by 2′-modified RNAs. Biochem. Biophys. Res. Commun 361, 122–126 (2007). [DOI] [PubMed] [Google Scholar]
- 14.Choung S, Kim YJ, Kim S, Park H-O & Choi Y-C Chemical modification of siRNAs to improve serum stability without loss of efficacy. Biochem. Biophys. Res. Commun 342, 919–927 (2006). [DOI] [PubMed] [Google Scholar]
- 15.Kanasty R, Dorkin JR, Vegas A & Anderson D Delivery materials for siRNA therapeutics. Nat. Mater 12, 967–977 (2013). [DOI] [PubMed] [Google Scholar]
- 16.Yin H et al. Non-viral vectors for gene-based therapy. Nat. Rev. Genet 15, 541–555 (2014). [DOI] [PubMed] [Google Scholar]
- 17.Mullard A FDA approves landmark RNAi drug. Nat. Rev. Drug Discovery 17, 613–614 (2018). [DOI] [PubMed] [Google Scholar]
- 18.Frank-Kamenetsky M et al. Therapeutic RNAi targeting PCSK9 acutely lowers plasma cholesterol in rodents and LDL cholesterol in nonhuman primates. Proc. Natl. Acad. Sci 105, 11915–11920 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zimmermann TS et al. RNAi-mediated gene silencing in non-human primates. Nature 441, 111–114 (2006). [DOI] [PubMed] [Google Scholar]
- 20.Tadin-Strapps M et al. siRNA-induced liver ApoB knockdown lowers serum LDL-cholesterol in a mouse model with human-like serum lipids. J. Lipid Res 52, 1084–1097 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pan H et al. Anti-JNK2 peptide–siRNA nanostructures improve plaque endothelium and reduce thrombotic risk in atherosclerotic mice. Int. J. Nanomed 13, 5187 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flores AM et al. Nanoparticle therapy for vascular diseases. Arterioscler., Thromb., Vasc. Biol 39, 635–646 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sager HB et al. RNAi targeting multiple cell adhesion molecules reduces immune cell recruitment and vascular inflammation after myocardial infarction. Sci. Transl. Med 8, 342ra380–342ra380 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dahlman JE et al. In vivo endothelial siRNA delivery using polymeric nanoparticles with low molecular weight. Nat. Nanotechnol 9, 648 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leuschner F et al. Therapeutic siRNA silencing in inflammatory monocytes in mice. Nat. Biotechnol 29, 1005–1010 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tao W et al. siRNA nanoparticles targeting CaMKIIγ in lesional macrophages improve atherosclerotic plaque stability in mice. Sci. Transl. Med 12, eaay1063 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Doran AC et al. CAMKIIγ suppresses an efferocytosis pathway in macrophages and promotes atherosclerotic plaque necrosis. J. Clin. Investig 127, 4075–4089 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Doran AC, Yurdagul A & Tabas I Efferocytosis in health and disease. Nat. Rev. Immunol 20, 254–267 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Finn AV, Nakano M, Narula J, Kolodgie FD & Virmani R Concept of vulnerable/unstable plaque. Arterioscler., Thromb., Vasc. Biol 30, 1282–1292 (2010). [DOI] [PubMed] [Google Scholar]
- 30.Islam MA et al. Restoration of tumour-growth suppression in vivo via systemic nanoparticle-mediated delivery of PTEN mRNA. Nat. Biomed. Eng 2, 850–864 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kong N et al. Synthetic mRNA nanoparticle-mediated restoration of p53 tumor suppressor sensitizes p53-deficient cancers to mTOR inhibition. Sci. Transl. Med 11, eaaw1565 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Baden LR et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N. Engl. J. Med 384, 403–416 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Polack FP et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N. Engl. J. Med 383, 2603–2615 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tang Z et al. A materials-science perspective on tackling COVID-19. Nat. Rev. Mater, 1–14 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang Z et al. mRNA vaccine-elicited antibodies to SARS-CoV-2 and circulating variants. Nature 592, 616–622 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bradley T et al. Antibody responses after a single dose of SARS-CoV-2 mRNA vaccine. N. Engl. J. Med 384, 1959–1961 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tang Z et al. Insights from nanotechnology in COVID-19 treatment. Nano today 36, 101019 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Song MS, Salmena L & Pandolfi PP The functions and regulation of the PTEN tumour suppressor. Nat. Rev. Mol. Cell Biol 13, 283–296 (2012). [DOI] [PubMed] [Google Scholar]
- 39.Kowalski PS, Rudra A, Miao L & Anderson DG Delivering the messenger: Advances in technologies for therapeutic mRNA delivery. Mol. Ther 27, 710–728 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ahmadi S et al. Stimulus-responsive sequential release systems for drug and gene delivery. Nano Today 34, 100914 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu Y & Chen X Macrophage-targeted gene therapy to improve the atherosclerotic plaque stability. Matter 3, 621–622 (2020). [Google Scholar]
- 42.Zhao W, Hou X, Vick OG & Dong Y RNA delivery biomaterials for the treatment of genetic and rare diseases. Biomaterials 217, 119291 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang Y & Yu C Emerging concepts of nanobiotechnology in mRNA delivery. Angew. Chem. Int. Ed 59, 23374–23385 (2020). [DOI] [PubMed] [Google Scholar]
- 44.Vaughan HJ, Green JJ & Tzeng SY Cancer-targeting nanoparticles for combinatorial nucleic acid delivery. Adv. Mater 32, 1901081 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhou Y et al. Blood-brain barrier–penetrating siRNA nanomedicine for Alzheimer’s disease therapy. Sci. Adv 6, eabc7031 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Truong NP et al. An influenza virus-inspired polymer system for the timed release of siRNA. Nat. Commun 4, 1902 (2013). [DOI] [PubMed] [Google Scholar]
- 47.Hu Q, Li H, Wang L, Gu H & Fan C DNA nanotechnology-enabled drug delivery systems. Chem. Rev 119, 6459–6506 (2019). [DOI] [PubMed] [Google Scholar]
- 48.Hu Q, Wang S, Wang L, Gu H & Fan C DNA nanostructure-based systems for intelligent delivery of therapeutic oligonucleotides. Adv. Healthcare Mater 7, 1701153–1701172 (2018). [DOI] [PubMed] [Google Scholar]
- 49.Lee H et al. Molecularly self-assembled nucleic acid nanoparticles for targeted in vivo siRNA delivery. Nat. Nanotechnol 7, 389–393 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Thai HBD et al. Kidney-targeted cytosolic delivery of siRNA using a small-sized mirror DNA tetrahedron for enhanced potency. ACS Cent. Sci 6, 2250–2258 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bujold KE, Hsu JCC & Sleiman HF Optimized DNA “nanosuitcases” for encapsulation and conditional release of siRNA. J. Am. Chem. Soc 138, 14030–14038 (2016). [DOI] [PubMed] [Google Scholar]
- 52.Rahman MA et al. Systemic delivery of bc12-targeting sirna by DNA nanoparticles suppresses cancer cell growth. Angew. Chem. Int. Ed 56, 16023–16027 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Semple SC et al. Rational design of cationic lipids for siRNA delivery. Nat. Biotechnol 28, 172–176 (2010). [DOI] [PubMed] [Google Scholar]
- 54.Kulkarni JA, Witzigmann D, Chen S, Cullis PR & van der Meel R Lipid nanoparticle technology for clinical translation of siRNA therapeutics. Acc. Chem. Res 52, 2435–2444 (2019). [DOI] [PubMed] [Google Scholar]
- 55.Whitehead KA et al. Degradable lipid nanoparticles with predictable in vivo siRNA delivery activity. Nat. Commun 5, 4277 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wittrup A et al. Visualizing lipid-formulated siRNA release from endosomes and target gene knockdown. Nat. Biotechnol 33, 870–876 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sahay G et al. Efficiency of siRNA delivery by lipid nanoparticles is limited by endocytic recycling. Nat. Biotechnol 31, 653–658 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liu S et al. Membrane-destabilizing ionizable phospholipids for organ-selective mRNA delivery and CRISPR–Cas gene editing. Nat. Mater 20, 701–710 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cheng Q et al. Selective organ targeting (SORT) nanoparticles for tissue-specific mRNA delivery and CRISPR–Cas gene editing. Nat. Nanotechnol 15, 313–320 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Xu X et al. Enhancing tumor cell response to chemotherapy through nanoparticle-mediated codelivery of siRNA and cisplatin prodrug. Proc. Natl. Acad. Sci 110, 18638–18643 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wilson DS et al. Orally delivered thioketal nanoparticles loaded with TNF-α–siRNA target inflammation and inhibit gene expression in the intestines. Nat. Mater 9, 923–928 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Díez S, Miguéliz I & De Ilarduya CT Targeted cationic poly (D, L-lactic-co-glycolic acid) nanoparticles for gene delivery to cultured cells. Cell. Mol. Biol. Lett 14, 347–362 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Shi J, Xiao Z, Votruba AR, Vilos C & Farokhzad OC Differentially charged hollow core/shell lipid–polymer–lipid hybrid nanoparticles for small interfering RNA delivery. Angew. Chem. Int. Ed 50, 7027–7031 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Mui BL et al. Influence of polyethylene glycol lipid desorption rates on pharmacokinetics and pharmacodynamics of siRNA lipid nanoparticles. Mol. Ther.--Nucleic Acids 2, e139 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Love KT et al. Lipid-like materials for low-dose, in vivo gene silencing. Proc. Natl. Acad. Sci 107, 1864–1869 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Schöttler S et al. Protein adsorption is required for stealth effect of poly(ethylene glycol)- and poly(phosphoester)-coated nanocarriers. Nat. Nanotechnol 11, 372–377 (2016). [DOI] [PubMed] [Google Scholar]
- 67.Petros RA & DeSimone JM Strategies in the design of nanoparticles for therapeutic applications. Nat. Rev. Drug Discovery 9, 615–627 (2010). [DOI] [PubMed] [Google Scholar]
- 68.Moghimi SM, Hunter AC & Murray JC Long-circulating and target-specific nanoparticles: theory to practice. Pharmacol. Rev 53, 283–318 (2001). [PubMed] [Google Scholar]
- 69.Gilleron J et al. Image-based analysis of lipid nanoparticle–mediated siRNA delivery, intracellular trafficking and endosomal escape. Nat. Biotechnol 31, 638 (2013). [DOI] [PubMed] [Google Scholar]
- 70.Ahmed SA, Gogal RM Jr & Walsh JE A new rapid and simple non-radioactive assay to monitor and determine the proliferation of lymphocytes: an alternative to [3H] thymidine incorporation assay. J. Immunol. Methods 170, 211–224 (1994). [DOI] [PubMed] [Google Scholar]
- 71.Miller LR et al. Considering sex as a biological variable in preclinical research. FASEB J. 31, 29–34 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Fredman G et al. Targeted nanoparticles containing the proresolving peptide Ac2-26 protect against advanced atherosclerosis in hypercholesterolemic mice. Sci. Transl. Med 7, 275ra220–275ra220 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhu X et al. Surface de-PEGylation controls nanoparticle-mediated sirna delivery in vitro and in vivo. Theranostics 7, 1990–2002 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Liu J et al. Fast and efficient CRISPR/Cas9 genome editing in vivo enabled by bioreducible lipid and messenger RNA nanoparticles. Adv. Mater 31, 1902575 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ensuring accurate resource identification. Nat. Protoc 15, 1879–1880 (2020). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The authors declare that the main data discussed in this protocol are available in the supporting primary research papers (https://doi.org/10.1126/scitranslmed.aay1063) and https://doi.org/10.1073/pnas.1303958110). The raw datasets are available for research purposes from the corresponding authors upon reasonable request.