Abstract
Background
Adverse life events such as life-threatening accidents, domestic and/or sexual violence, organic diseases (i.e., cancer), or COVID-19 can have a strong traumatic impact – generating reactions as intrusive thoughts, hyperarousal, and avoidance. Indeed, the traumatic impact of COVID-19 seems to lead individuals to experience anxiety and depression. However, the Anxiety-Buffer Hypothesis suggests that self-esteem could be considered a shield (buffer) against traumatic experiences and their outcomes (i.e., anxiety and depression). The present study has two objectives. First, to develop a measure of the impact of the traumatic event considering the aforementioned reactions. Second, to test the process – triggered by COVID19-related traumatic experience – in which self-esteem buffers the path that leads to anxiety and depression.
Method
In Study 1 (N = 353), the Post-Traumatic Symptom Questionnaire (PTSQ) was developed and a deep investigation of its psychometric properties was conducted. In Study 2 (N = 445), a structural equation model with latent variables was performed to assess the buffering effect of self-esteem.
Results
The PTSQ has excellent fit indices and psychometric properties. According to the ABH, results confirm the buffering effect of self-esteem in the relationships between traumatic symptoms and both anxiety and depression.
Conclusion
On the one hand, the PTSQ is a solid and reliable instrument. On the other hand, that self-esteem is a protective factor against anxiety and depression related to a traumatic experience – such as COVID-19. Targeted psychological interventions should be implemented to minimize the psychological burden of the illness while promoting adaptation and positive aspects of oneself.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40653-022-00503-z.
Keywords: Trauma, Anxiety buffer hypothesis, terror management theory, anxiety, depression
Introduction
Accidents endangering one’s own life, the tragic death of some of our loved ones, domestic and/or sexual violence, and serious organic diseases (e.g., cancer or COVID-19) are all potentially traumatic events that can have a dramatic psychological impact (Friedman et al., 2007; Rossi et al., 2022a; Thakur & Jain, 2020; Zhang et al., 2021). The impact of the traumatic event can be associated with a wide range of physical as well as psychological difficulties and disorders in adults, children, and adolescents (Briere & Spinazzola, 2005; Friedman et al., 2007; Kratovic et al., 2021).
On the one hand, scientific literature showed that the impact of traumatic events can be so strong that can have a serious long-term influence on physical health (Sareen et al., 2007) in terms of poor quality of life (QOL), general health symptoms, general medical conditions, pain (e.g., musculoskeletal), cardio-respiratory symptoms, and gastrointestinal health (Brosschot et al., 2016; Yaribeygi et al., 2017; Zhang et al., 2021) – for a review (Pacella et al., 2013).
On the other hand, the psychological impact of traumatic events can be so strong that can lead to developing post-traumatic stress symptoms (PTSS) and/or post-traumatic stress disorder (PTSD) – consisting in the late onset and persistence of mental disorders caused by experiencing, suffering or encountering one or more threats for themselves or others (Agaibi & Wilson, 2005) – even 10 years after its onset (Kessler et al., 1995). Moreover, individuals who have experienced a traumatic event are between 2 and 6 times more likely to present with psychiatric comorbidities, including anxiety, depression, suicidal ideation, and self-injury behaviors (Breslau & Davis, 1992; Breslau et al., 1991; Karatzias et al., 2019; Tessitore et al., 2022). Also, approximately 40% of individuals who have experienced a traumatic event continue to present relevant symptomatology (Djelantik et al., 2020; Kessler et al., 1995; Orcutt et al., 2002) – probably due to the presence of maladaptive psycho(physio-)logical mechanisms that contribute to the development and the maintenance of anxiety and depression symptoms.
Indeed, the psychological impact of traumatic events often entails persistent reenactment of the event, avoidance symptoms, negative change in general reactivity, and increased arousal and reactivity (American Psychiatric Association, 2013).
According to the terror management theory (TMT) (Greenberg et al., 1986), individuals’ awareness of mortality – elicited by a traumatic event (e.g., accidents, experienced violence, or severe organic disease) and the continuously dwelling – generates terrifying fears of death and thus anxiety and depression that constantly conflicts with humans’ intrinsic desire to live and their natural tendency to survive. (Rossi et al., 2020).
Moreover, scientific literature has shown that adverse events can generate three main psycho(physio-)logical reactions/domains (Pacella et al., 2013; Yaribeygi et al., 2017) – intrusivity, hyperarousal, and avoidance – and all of them are associated with heightened anxiety reactions. Firstly, intrusivity refers to the intrusions of unwanted cognitive and/or sensorial stimuli recalling the traumatic event that re-expose the person to that feared event – and can thus generate an intense sense of anxiety as the original event did. Secondly, traumatic events can generate hyperarousal reactions, a state of chronic hypervigilance for potential threats and heightened arousal, that prompts the individual to amplify anxious reactions in response to (also neutral) stimuli, thus contributing to the development and the maintenance of anxiety as the anticipation of future (potential) threats (Barlow, 2002; Harding et al., 2008). Lastly, traumatic events can generate the need for avoidance – both cognitive and behavioral. Avoidance is a coping strategy that the individual implements to protect himself or herself from the possibility that the traumatic event may recur by avoiding all the trauma-related experiences – aiming at preventing further damage to an already weakened psychological structure (Bishop et al., 2018). However, even this coping strategy – when abused – often contributes to maintaining and amplifying dysfunctional anxiety states (Bishop et al., 2018).
Consequently, these three main reactions/domains to traumatic events (overlapping with symptoms of PTSS and PTSD) seem to converge under the overarching factor related to the suffered trauma – the so-called ‘impact of the event’ – which makes the individual more prone to develop and maintain anxious symptomatology (Gagne et al., 2018). The negative/adverse event and the subsequent possible development of trauma can influence the way individuals think and behave – thus representing an important risk factor for mental health – making them more prone to develop anxious and depressive symptoms (Kessler et al., 2017).
Furthermore, although traumatic events can lead to the development of depressive symptoms (as aforementioned), several research shows that also prolonged and chronic states of anxiety can lead to the development of depressive symptoms (Rossi et al., 2020) – by intensifying the negative expectations, negative repetitive thoughts (i.e., worry, rumination), pessimism, and negative feelings (Starr & Davila, 2012; Thompson et al., 2005). Such depressive symptomatology includes sadness, loss of positive feelings, and Beck’s negative triad (Beck, 1979) – consisting of a negative view of the self, the world, and the future (Rossi et al., 2021). Moreover, traumatic events-related depressive symptomatology should not be underrated due to its association with anticonservative ideation and attempts (Breslau & Davis, 1992; Breslau et al., 1991; Karatzias et al., 2019; McIntyre & Lee, 2020; Thakur & Jain, 2020).
Therefore, the impact of a traumatic event (in addition to possible PTSS and PTDS) can lead the individual to develop conditions of intrusivity, hyperarousal, and avoidance which – in turn – contribute to the development and maintenance of anxiety states, which can lead to the development of depressive symptoms (Santini et al., 2020; Thakur & Jain, 2020).
However, over the past 20 years, the literature has shown that certain psychological variables can play a key role in protecting – as a psychological shield – the individual from the negative consequences (i.e., anxiety and depression) of traumatic events (Benight, 2012). The anxiety-buffer hypothesis (ABH) (Greenberg et al., 1992) – from the TMT (Greenberg et al., 1986) – suggests that self-esteem has a shielding (buffering) effect on the relationship between the impact of traumatic events and both anxiety and depression (Benight, 2012; Rossi et al., 2020). More in detail, self-esteem – conceived as the beliefs and evaluations of individuals towards themselves, and the attitudes that derive from them – is based on personal values deeply rooted in the culture and social context of the individual from which one’s own personal value (Becker, 1971, 1973). Therefore, by respecting the standards of one’s own culture of belonging and worldview, self-esteem is strengthened both by the social validation of oneself and by the intimate and personal feeling of being an individual with a certain degree of value and who assumes a significant role in one’s society (Pyszczynski et al., 2004; Solomon et al., 2004). In this context, the ABH (Greenberg et al., 1992) hypothesizes that – by reconnecting the individual to an enlarged universe of purely individual and intimately personal meanings and values – self-esteem could act as a protective shield (buffer) against the damaging psychological effects of life threats and stressors. Consequently, self-esteem should buffer the negative consequences of traumatic events.
Considering this background, a major traumatic event has hit the world: the COVID-19 pandemic (Brooks et al., 2020; Torales et al., 2020; Wang et al., 2020; Zhang et al., 2021). COVID-19 is a serious and potentially deadly infectious disease that threatened the entire world population, since-at the time of its outbreak-there was no preventive immunity or even a well-defined cure or vaccine (Baud et al., 2020); and it still causes deaths. According to scientific literature, COVID-19 represented a challenge to the physical and mental health of individuals and generated widespread post-traumatic reactions (Esterwood & Saeed, 2020; Fisher et al., 2020; Shevlin et al., 2021; Silver, 2020; Waseem et al., 2021). A recent review by Zhang and colleagues demonstrated that during the COVID-19 pandemic in all countries the general population developed PTSS to varying degrees, with a PTSD prevalence of 15% (Zhang et al., 2021). Moreover, it is important to highlight that even people not infected by COVID-19 still experienced high psychological stress (Zhang et al., 2021). In addition, scientific studies on the psychological impact of COVID-19 highlighted that specific categories of the population are more prone than others to develop psychological issues, in particular, individuals in the emerging adulthood phase also referred to as young adults (18–30 y.o.) (Parola, 2020; Parola et al., 2020). Indeed, in the last two years, scientific research has highlighted that in the emerging adulthood individuals present heightened levels of psychological difficulties, including symptoms of distress, anxiety, and depression (Panzeri et al., 2021; Parola et al., 2020). Importantly, emerging adulthood may expose to a higher risk of developing psychological issues because individuals in this part of the lifespan go through a process of individualization, structuring self-esteem, and personal growth (van den Berg et al., 2021) – in which they progressively rediscuss and strengthen their role in the society, relationships, and the professional field (Graupensperger et al., 2022). Thus, the trauma associated with the pandemic situation and its limitations may have disrupted this process, hence hindering the possibility to fulfill personal, professional, and relational wills (Cao et al., 2020; Cheng et al., 2014; Zhang et al., 2021). Taken together, all these evidence strongly advice to assessing and monitoring the psychological condition of individuals, in particular of those in the emerging adulthood phase.
In light of this, the present study has two aims. First, to develop a self-report questionnaire measuring the impact of the traumatic event that specifically takes into account intrusivity, hyperarousal, and avoidance. Second, to test the hypothesis that if COVID-19 was an event that had a traumatic impact – especially on young adults (Parola, 2020; Parola et al., 2020) – that led to anxiety and depressive symptoms, then, according to the ABH, self-esteem (acting as a shield) should buffer the relationship from the impact of traumatic event to anxiety, which in turn should lead to depression.
Study 1. Development of the Post-Traumatic Symptom Questionnaire (PTSQ)
Materials and methods
Sample Size Determination
The subject-per-parameter ratio “n:q criterion” (subjects per free model parameter) was used to plan a priori the minimum number of subjects needed given the main statistical analyses of this study (see dedicated section). A ratio of 5 subjects per parameter was guaranteed (Brown, 2015; Hu & Bentler, 1999; Kline, 2016).
Enrollment Procedure
Using the snowball sampling method (Johnson, 2014), participants were recruited from the general population through advertisements on social media (e.g., Facebook, Twitter, etc.).
Inclusion criteria were: (A) having experienced at least a traumatic event that the subject remembers well to this day, (B) being aged between 18 and 30 y.o., (C) being a native Italian speaker; (D) providing informed consent; (E) do not provide missing answers, (F) have no inability to complete the assessment procedure; and (G) do not complete the procedure in less than 4 or greater than 8 min.
At the beginning of the survey, participants were asked if they had experienced a traumatic event that they remember well to this day. Based on the aforementioned inclusion/exclusion criteria, only those who had this characteristic went on to complete the survey and were enrolled in the study.
Participants
A sample of 412 subjects was eligible to complete the survey. However, 59 questionnaires were excluded due to missing data/answers (n = 36) and/or inappropriate completion times (< 4 or > 8 min; n = 23).
The final sample included 353 participants: 111 males (31.4%) and 242 females (68.6%), aged from 18 to 30 y.o. (mean = 26.13, SD = 2.96) – all of them reported having experienced a traumatic event. Most of the sample was in a relationship (58.4%), 32.6% were single, 8.5% were cohabitants, and 0.6% were married. Considering the level of education, most of the sample had a bachelor/master’s degree (48.4%), 37.1% had a high school license, 9.9% had a master’s degree/higher specialization degree, and 4.5% had a middle school license. Lastly, considering employment status, 36.1% were dependent workers followed by students (36%) and student/workers 19.7% were students/workers; the remaining part of the sample was unemployed (8.2%). Each of the participants experienced a traumatic event. 22.1% reported to have experienced a ‘severe accident (e.g., car crash, domestic accident, etc.) that threatened his/her own life, followed by ‘severe organic illness, still ongoing (i.e. cancer)’ (21.8%); ‘threat to one’s life (e.g. being hit/hurt) from family members and/or partners and/or strangers’ (15.9%); and ‘having been sexually abused by family members and/or partner and/or strangers’ (12.5%). Moreover, 10.8% ‘loss of a member of one’s immediate family in a tragic way (e.g., serious and long physical illness, car accident, plane crash, suicide)’, followed by ‘witnessing traumatic event experienced by another person’ (9.1%) and ‘other’ (7.9%).
The Development Procedure of the Questionnaire
The Post-Traumatic Symptom Questionnaire (PTSQ) was created to fill some of the gaps in previous instruments for measuring post-traumatic symptoms. First, it was chosen to use a number of items that would allow for easy and rapid administration suitable in all types of contexts – both clinical and research settings – thus differentiating it from longer instruments such as the Impact of Event Scale-Revised (IES-R), which is much longer with its 22 items (Weiss, 2007; Weiss & Marmar, 1996). Second, unlike the original Impact of Event Scale (Horowitz et al., 1979), the PTSQ was created with the intention of also measuring the dimension of hyperarousal according to DSM-5-TR.
In line with previous studies, the item pool for the Post-Traumatic Symptom Questionnaire (PTSQ) was developed using a three-step double-blind study procedure (Milavic et al., 2019; Pietrabissa, Rossi, Borrello, et al., 2020; Pietrabissa, Rossi, Simpson, et al., 2020; Rossi et al., 2021). The detailed procedure is reported in the supplementary material 1.
Measures
A biographic information form collected general demographic information (e.g., sex, age, civil status, education level, and employment status). Moreover, participants were asked what type of traumatic event they had experienced.
The Post-Traumatic Symptom Questionnaire (PTSQ)
The Post-Traumatic Symptom Questionnaire (PTSQ) is a 12-items questionnaire measuring the three main reactions/domains of the impact of traumatic events: (A) intrusivity, (B) avoidance, and (C) hyperarousal. The first domain, (A) intrusivity (INTR), measures the extent to which the subject who has experienced a traumatic event reports having intrusive thoughts and images – as well as unpleasant emotions – that recall the traumatic event itself. The second domain, (B) avoidance (AV), measures the extent to which the subject tends to avoid things, situations, and people – as well as thoughts and behaviors – that may remind them of the traumatic event. Lastly, the third domain, (C) hyperarousal (HY.AR), measures the extent to which the subject reports having excessive reactions of hypervigilance, fear, and alertness in their daily lives after experiencing the traumatic event.
Items are rated on a 5-point Likert-type scale, from 1 (= “not at all”) to 5 (= “extremely”). Higher scores indicate higher levels in that domain. Moreover, consistently with the proposed theoretical background, an overarching second-order general was assumed: post-traumatic symptoms (PTS). See Appendix ‘A’ and ‘B’ for the English and the Italian versions of the PTSQ, respectively.
Statistical Analysis
The R software was used with the following packages: lavaan (lavaan, 2012), psych (Revelle, 2018), and semPlot (Jorgensen et al., 2019).
To test the factorial structure of the PTSQ, a confirmatory factor analysis (CFA) was performed. Considering the theoretical background as well as the semantic content of the items, a second-order factorial structure (Brown, 2015) was specified: each item loaded onto its specific first-order factors reflecting the main three reactions/domains of traumatic events – namely, (A) intrusivity, (B) avoidance, and (C) hyperarousal – and an overarching general factor so-called ‘post-traumatic symptoms’ (PTS) (Fig. 1). Given the response scale of the PTSQ, the diagonal weighted least square (DWLS) estimator was used to perform the CFA (Brown, 2015; Forero et al., 2009; Li, 2016; Parola et al., 2022).
Fig. 1.
Study 1. Graphical representation of the PTSQ model
Model fit was assessed using the Chi-square statistics (χ2), the Root-Mean Square Error of Approximation (RMSEA), the Comparative Fit Index (CFI), and the Standardized Root Mean Residual (SRMR) (Brown, 2015; Hoyle, 2012; Kline, 2016; van de Schoot et al., 2012). The following cut-off criteria were chosen to evaluate the goodness of fit: (A) statistically non-significance of the χ2, (B) an RMSEA lower than 0.08, (C) a CFI higher than 0.95, and (D) an SRMR lower than 0.08 (Brown, 2015; Hoyle, 2012; Hu & Bentler, 1999; van de Schoot et al., 2012).
Additionally, the ability of the items to discriminate subjects with a low or high level of the measured construct was tested using the item discriminant power (IDP) (Chiorri, 2011; Ebel, 1965). Moreover, adjusted item-total correlation (rit−tot) was also computed (Tabachnick & Fidell, 2014).
Given the problems and criticisms associated with Cronbach’s alpha (Barbaranelli et al., 2014; Raykov, 2011; Raykov, 2012; Raykov & Marcoulides, 2011), the internal consistency of each scale was also calculated with McDonald’s omega (McDonald, 1999). Also, correlations between items and domains were computed (Tabachnick & Fidell, 2014).
Lastly, a multivariate analysis of variance (one-way MANOVA) was conducted to assess for possible statistical differences between the different traumatic experiences, on the PTSQ subscales simultaneously. For multiple comparisons, the strength of differences was interpreted using partial eta-squared (η2p) whereas, for pairwise comparisons, Hedge’s g (Hedges, 1981) was used.
The strength of the differences was interpreted using Cohen’s benchmarks (Cohen, 1988): null (η2p < 0.010; g < 0.20), small (η2p from 0.011 to 0.059; g from 0.20 to 0.49), moderate (η2p from 0.060 to 0.139; g from 0.50 to 0.79), and large (η2p > 0.140; g > 0.80). Games-Howell post-hoc correction for multiple comparisons was applied (Howell, 2013).
Results
Structural Validity
The PTSQ showed a good fit to the data. Despite that the Chi-square statistic was statistically significant [χ2 (51) = 133.686; p < .001], all other fit indices revealed a good fit to the data: RMSEA = 0.068; 90%CI[0.054, 0.082], CFI = 0.997, SRMR = 0.057. As reported in Table 1, all items’ loadings were statistically significant and ranged from 0.735 (item#10; HY.AR.) to 0.968 (item#3, INTR).
Table 1.
Study 1. Item descriptive statistics, item psychometric properties, and confirmatory factor analysis
| Descriptive statistics | IDP | r Adj | CFA | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | SK | K | t | d | λ | R 2 | ||||
| Item#1 | 3.159 | 1.169 | -0.011 | -0.778 | -29.62 | 4.19 | 0.836 | 0.905 | 0.819 | ||
| Item#2 | 3.031 | 1.193 | 0.021 | -0.842 | -30.17 | 4.25 | 0.832 | 0.899 | 0.807 | ||
| Item#3 | 3.164 | 1.139 | -0.036 | -0.785 | -34.08 | 4.81 | 0.883 | 0.968 | 0.936 | ||
| Item#4 | 3.232 | 1.198 | -0.097 | -0.895 | -28.96 | 4.12 | 0.782 | 0.839 | 0.703 | ||
| Item#5 | 2.895 | 1.377 | 0.071 | -1.186 | -28.28 | 4.18 | 0.644 | 0.761 | 0.579 | ||
| Item#6 | 2.813 | 1.392 | 0.115 | -1.198 | -22.85 | 3.37 | 0.645 | 0.796 | 0.634 | ||
| Item#7 | 2.686 | 1.338 | 0.175 | -1.150 | -27.20 | 3.98 | 0.636 | 0.810 | 0.656 | ||
| Item#8 | 2.776 | 1.307 | 0.183 | -0.981 | -28.88 | 4.25 | 0.761 | 0.855 | 0.731 | ||
| Item#9 | 2.445 | 1.289 | 0.455 | -0.905 | -18.78 | 2.91 | 0.558 | 0.640 | 0.410 | ||
| Item#10 | 2.705 | 1.301 | 0.225 | -0.988 | -22.50 | 3.48 | 0.611 | 0.735 | 0.541 | ||
| Item#11 | 2.754 | 1.318 | 0.148 | -1.052 | -33.01 | 5.12 | 0.772 | 0.929 | 0.862 | ||
| Item#12 | 2.646 | 1.302 | 0.275 | -0.943 | -24.46 | 3.80 | 0.661 | 0.808 | 0.653 | ||
| INTR | 12.586 | 4.263 | 0.036 | -0.803 | -21.93 | 3.34 | 0.615 | 0.815 | 0.664 | ||
| AV | 11.170 | 4.443 | 0.036 | -0.955 | -19.97 | 3.03 | 0.446 | 0.554 | 0.306 | ||
| HY.AR | 10.550 | 4.216 | 0.222 | -0.691 | -26.12 | 3.95 | 0.656 | 0.955 | 0.912 | ||
| PTS | 34.306 | 10.500 | 0.105 | -0.486 | |||||||
Notes: INTR = Intrusivity; AV = Avoidance; HY.AR = Hyperarausal; PTSQ = Post-Traumatic Symptom, IDP = Item discriminant power t = independent sample t-test, d = Cohen’s d (effect size). CFA = confirmatory factor analysis. In the CFA columns, absolute values of standardized factor loading (|λ|) are reported. λ = factor loading onto the specific factor (i.e., INTR, AV, or HY.AR); for INTR, AV, and HY.AR, λ = refers to factor loading of the first-order factors onto the general factor (i.e., ‘post-traumatic symptoms’).
Psychometric Properties
Considering the three domains, the IDP analysis showed that 12 items of the PTSQ discriminated well between subjects with a low or high level of the construct (Table 1). The discrimination parameter ti ranged from − 18.78| (item#19 – HY.AR) to -34.08 (item#3 – INTR), with an associated effect size (Cohen’s d) ranging from 2.91 (large) to 4.81 (large), respectively. In addition, the item-total correlation (adjusted) revealed a moderate-to-strong association between each item and its PTSQ factor. Considering the general factor (PTS), the IDP analysis showed that three domains of the PTSQ discriminated well between subjects with a low or high level of impact of the traumatic event (Table 1). The discrimination parameter ti ranged from − 19.97 (AV) to -26.12 (HY.AR), with an associated effect size (Cohen’s d) ranging from 3.03 (large) to 3.95 (large), respectively. Also in this case, the item-total correlation (adjusted) revealed a moderate-to-strong association between each domain and the PTSQ general score.
Considering internal consistency, the Cronbach’s alpha revealed that the PTSQ showed good internal consistency for each domain: INTR = 0.928, 95%CI[0.915, 0.940]; AV = 0.838, 95%CI[0.808, 0.864]; HY.AR = 0.824, 95%CI[0.792, 0.852]. Also the McDonald’s omega revealed that the PTSQ showed good internal consistency for each domain: INTR = 0.928, 95%CI[0.916, 0.941]; AV = 0.839, 95%CI[0.811, 0.866]; HY.AR = 0.831, 95%CI[0.802, 0.859].
Moderate-to-large correlations among the three domains and the general total score were found. A moderate correlation was found between the INTR domain and the AV domain (r = .383, p < .001) whereas a strong correlation was found between the INTR domain and the HY.AR domain (r = .665; p < .001). A moderate correlation was found between the AV domain and the HY.AR domain (r = .431, p < .001). Lastly, large correlations were found between the general factor (PTS) and the INTR domain (r = .835, p < .001), the AV domain (r = .752, p < .001), and the HY.AR domain (r = .854, p < .001). Correlations between items are reported in Supplementary material (Table S1).
Differences Among Traumatic Experiences
A statistically significant multivariate effect was found among type of traumatic experience on the three post-traumatic domains: Wilks’ Λ = 0.675; F = 8.071, p < .001; η2p = 0.123 – Fig. 2; Table 2.
Fig. 2.
Study 1. boxplot
Table 2.
Study 1. Item descriptive statistics, and post-hoc comparisons among different kind of traumatic events
| A | B | C | D | E | F | G | Post-hoc comparisons | |
|---|---|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | ||
| INTR | 13.32 (4.35) | 13.88 (3.70) | 14.18 (3.62) | 13.58 (4.25) | 11.29 (3.41) | 9.50 (2.78) | 8.00 (3.31) |
A > F**; A > G**; B > E*; B > F**; B > G**; C > E*; C > F**; C > G**; D > E*; D > F**; D > G**; E > G* |
| AV | 12.00 (4.39) | 13.59 (3.67) | 12.70 (3.25) | 9.26 (4.60) | 11.21 (4.34) | 9.19 (4.34) | 9.07 (3.68) |
A > D*; A > F*; A > G*; B > D**; B > F**; B > G**; C > D**; C > F*; C > G*; |
| HY.AR | 10.95 (4.23) | 11.46 (4.02) | 11.34 (4.07) | 11.83 (4.02) | 9.79 (4.30) | 7.91 (3.41) | 6.89 (2.53) |
A > F*; A > G**; B > F*; B > G**; C > F**; C > G**; D > F**; D > G**; E > G*; |
| PTS | 36.27 (10.74) | 38.93 (8.63) | 38.23 (8.59) | 34.68 (11.01) | 32.29 (9.71) | 26.59 (7.24) | 23.96 (6.39) |
A > F**; A > G**; B > E*; B > F**; B > G**; C > F**; C > G**; D > F**; D > G**; E > G*; |
* p < .01; ** p < .001; redundant comparisons (e.g., B > E and E < B) were not reported in the table. Considering MANOVA’s assumption, for the general total score (composite score, PTS) a separate One-Way ANOVA was performed with Games-Howell post-hoc comparisons. Note: A = ‘severe accident (e.g., car crash, domestic accident, etc.) that threatened his/her own life’; B = ‘threat to one’s life (e.g. being hit/hurt) from family members and/or partners and/or strangers’; C = ‘having been sexually abused by family members and/or partner and/or strangers’; D = ‘severe organic illness, still ongoing (i.e. cancer)’; E = ‘loss of a member of one’s immediate family in a tragic way (e.g., serious and long physical illness, car accident, plane crash, suicide)’; F = ‘witnessing traumatic event experienced by another person’; G = ‘other’
Considering ‘intrusivity’, a statistically significant univariate effect was found: F = 14.449, p < .001, η2p = 0.200. More in detail, statistically significant differences were found between (A) ‘severe accident’ and (F) ‘witnessing traumatic event’ (g = -0.964) and (G) ‘other’ (g = -1.296). Moreover, statistically significant differences were found between (B) ‘threat to one’s life by another person’ and (E) ‘loss of a family member’ (g = -0.722), (F) ‘witnessing a traumatic event’ (g = -1.289), and (G) ‘other’ (g = -1.644). Also, statistically significant differences were found between (C) ‘have been sexually abused’ and (E) ‘loss of a family member’ (g = -0.82), (F) ‘witnessing a traumatic event’ (g = -1.421), and (G) ‘other’ (g = -1.764). In addition, statistically significant differences were found between (D) ‘severe chronic illness (still ongoing)’ and (E) ‘loss of a family member’ (g = -0.573), (F) ‘witnessing traumatic event’ (g = -1.051), and (G) ‘other’ (g = -1.386). Lastly, statistically significant differences were found between (E) ‘loss of a family member’ and (G) ‘other’ (g = -0.977).
Considering ‘avoidance’, a statistically significant univariate effect was found: F = 9.868, p < .001, η2p = .146. More in detail, statistically significant differences were found between (A) ‘severe accident’ and (D) ‘severe chronic illness (still ongoing)’ (g = -0.609), (F) ‘witnessing traumatic event’ (g = -0.642) and (G) ‘other’ (g = -0.695). Statistically significant differences were found between (B) ‘threat to one’s life by another person’ and (D) ‘severe chronic illness (still ongoing)’ (g = -1.023), (F) ‘witnessing traumatic event’ (g = -1.121), and (G) ‘other’ (g = -1.231). Also, statistically significant differences were found between (C) ‘have been sexually abused’ and (D) ‘severe chronic illness (still ongoing)’ (g = -0.826), (F) ‘witnessing traumatic event’ (g = -0.937), and (G) ‘other’ (g = -1-061).
Considering ‘hyperarousal’, a statistically significant univariate effect was found: F = 8.859, p < .001, η2p = 0.133. More in detail, statistically significant differences were found between: (A) ‘severe accident’ and (F) ‘witnessing traumatic event’ (g = -0.758) and (G) ‘other’ (g = -1.051). Moreover, statistically significant differences were found between (B) ‘threat to one’s life by another person’ and (F) ‘witnessing a traumatic event’ (g = -0.931), and (G) ‘other’ (g = -1.27). Also, statistically significant differences were found between (C) ‘have been sexually abused’ and (F) ‘witnessing a traumatic event’ (g = -0.901), and (G) ‘other’ (g = -1.251). In addition, statistically significant differences were found between (D) ‘severe chronic illness (still ongoing)’ and (F) ‘witnessing a traumatic event’ (g = -1.017), and (G) ‘other’ (g = -1.339). Lastly, statistically significant differences were found between (E) ‘loss of a family member’ and (G) ‘other’ (g = -0.793).
Considering the total score ‘post-traumatic symptoms’, a statistically significant univariate effect was found: F = 13.218, p < .001, η2p = 0.186. More in detail, statistically significant differences were found between: (A) ‘severe accident’ and (F) ‘witnessing traumatic event’ (g = -0.981) and (G) ‘other’ (g = -1.256). Moreover, statistically significant differences were found between (B) ‘threat to one’s life by another person’ and (E) ‘loss of a family member’ (g = -0.731), (F) ‘witnessing a traumatic event’ (g = -1.513), and (G) ‘other’ (g = -1.88). Also, statistically significant differences were found between (C) ‘have been sexually abused’ and (F) ‘witnessing a traumatic event’ (g = -1.446), and (G) ‘other’ (g = -1.826). In addition, statistically significant differences were found between (D) ‘severe chronic illness (still ongoing)’ and (F) ‘witnessing a traumatic event’ (g = -0.759), and (G) ‘other’ (g = -1.026). Lastly, statistically significant differences were found between (E) ‘loss of a family member’ and (G) ‘other’ (g = -0.985).
Study 2. The Anxiety Buffer Hypothesis: self-esteem as a Shield. A Structural Equation Model Approach
Materials and methods
Sample Size Determination
In line with Study 1, the “n:q criterion” was still used to determine a priori the minimum sample to be enrolled. A ratio of 5 subjects per parameter was guaranteed (Brown, 2015; Hu & Bentler, 1999; Kline, 2016).
Procedure
In line with Study 1, the same snowball sampling method (Johnson, 2014) was used to enroll participants from the general population through personal invitations or materials advertised via social media platforms (e.g. Facebook, Twitter, etc.).
Inclusion criteria were: (A) having experienced COVID-19 as a traumatic event, (B) being aged between 18 and 30 y.o., (C) being a native Italian speaker; (D) providing informed consent; (E) do not provide missing answers, (F) have no inability to complete the assessment procedure; and (G) do not complete the procedure in less than 8 or greater than 20 min. In line with previous studies (e.g. Rossi et al., 2020), data were entirely collected in a single week-interval to avoid confounding effects due to the pandemic fluctuations.
In line with the Study 1, at the beginning of the survey, participants were asked whether they had experienced COVID-19 as a traumatic event. Based on the above inclusion/exclusion criteria, only those with this feature completed the survey and were enrolled in the study.
Participants
An initial sample of 510 individuals was eligible to complete the survey. However, 42 individuals were excluded due to the presence of missing values and 23 individuals did not complete the procedure within the given time frame. Thus, the final sample consisted of 445 participants: 76 males (17.1%) and 369 females (82.9%) aged from 18 to 30 years (mean = 26.18, SD = 2.89). All of the participants experienced COVID-19 as a traumatic event. Most of the participants were in a relationship (56.4%), 32.1% were single, 10.8% were cohabitants, and 0.7% were married. Considering the level of education, most of the sample had a bachelor/master’s degree (48.8%), 36.2% had a high school license, 10.3% had a master’s degree/higher specialization degree, and 4.7% had a middle school license. Lastly, considering employment status, 37.3% were dependent workers followed by students (36.4%) and student/workers 19.6% were students/workers; the remaining part of the sample was unemployed (6.5%).
Measures
The socio-demographic information form used in Study 1 and the Post-Traumatic Symptom Questionnaire (PTSQ) were administered. In this study, the PTSQ still provides good internal consistency with both Cronbach’s alpha (INTR = 0.781, 95%CI[0.746, 0.813]; AV = 0.838, 95%CI[0.812, 0.861]; HY.AR = 0.818, 95%CI[0.788, 0.844]) and McDonalds’ Omega (INTR = 0.786, 95%CI[0.753, 0.818]; AV = 0.840, 95%CI[0.815, 0.864]; HY.AR = 0.819, 95%CI[0.791, 0.846]). In addition, the following self-report measures were administered.
Rosenberg Self-Esteem Scale (RSE)
The RSE (Rosenberg, 1965) is one of the most used scales for assessing self-esteem. It consists of 10 statements assessing feelings about one’s self. Respondents express their degree of agreement with each statement on a 4-point Likert-type scale (ranging from 1 = “not at all” to 4 = “always”), and it provides a single-factor structure. Higher values indicate greater self-esteem. In the present study, the RSE showed a high internal consistency: Cronbach’s alpha = 0.860, 95%CI[0.841, 0.877]; McDonalds’ Omega = 0.871, 95%CI[0.854, 0.889].
Anxiety Subscale of the Symptom Checklist-90Revised (SCL-90R – ANX)
The SCL-90R ANX subscale (Derogatis & Unger, 2010) is one of the most used worldwide scales for assessing anxiety symptoms. It is a 10-item measuring physical, cognitive, and psychological signs of anxiety within the past week. Respondents rate the severity of their symptoms on a 5-point Likert-type scale (ranging from 1 = “not at all” to 5 = “always”). The ANX provides a single-factor structure. Higher values indicate more severe anxiety symptoms. In the present study, the ANX subscale showed a high internal consistency: Cronbach’s alpha = 0.924, 95%CI[0.914, 0.934]; McDonalds’ Omega = 0.928, 95%CI[0.918, 0.938].
Depression Subscale of the Symptom Checklist-90Revised (SCL-90R – DEP)
The SCL-90R DEP subscale (Derogatis & Unger, 2010) is one of the most used self-report scales for assessing depression symptoms. It is a 13-item measuring cognitive, emotive, and somatic signs of depression during the past week. Respondents rate the gravity of their symptoms on a 5-point Likert-type scale (ranging from 1 = “not at all” to 5 = “always”). The DEP provides a single-factor structure. Higher values indicate more severe depressive symptoms. In the present study, the DEP subscale showed a high internal consistency: Cronbach’s alpha = 0.912, 95%CI[0.900, 0.923]; McDonalds’ Omega = 0.917, 95%CI[0.905, 0.928].
Statistical Analyses
The R software was used with the following packages: lavaan (lavaan, 2012) and psych (Revelle, 2018). Graphical representations were performed with GraphViz in DiagrammeR (Iannone, 2018).
Preliminarily, multivariate multiple regression was performed to exclude the potential confounding effects of covariates on psychological variables. Also, the Pearson correlation coefficient (r) was computed to evaluate the relationships between variables (Tabachnick & Fidell, 2014). These analyses are reported in the supplementary material – Table S2 and S3.
A structural equation modeling (SEM) approach with latent variables was used. The steps described below were followed.
First. Before testing the hypothesized model, the structural validity of each scale used in this study was evaluated using CFAs, separately. The DWLS estimator was used. Model fit was assessed using the aforementioned fit indices (χ2, RMSEA, CFI, SRMR) and their cutoff values for good model fit (Brown, 2015; Hoyle, 2012; Kline, 2016; van de Schoot et al., 2012).
Second. The ‘common method bias’ was checked using Harman’s single-factor test (Harman, 1976; Podsakoff et al., 2003; Brown 2015). First, a six correlated factors model was specified according to the measurement model of each questionnaire (PTSQ – three factors, RSE – single factor, ANX – single factor, and DEP – single factor). Second, a first-order single factor model was specified (all the items loaded onto a single latent dimension). Models were compared: a statistically significant chi-square difference (Δχ2; p < .050), a ΔRMSEA greater than .015, and a ΔCFI greater than .010 suggest the absence of the bias (Brown, 2015; Cheung & Rensvold, 2002; Millsap, 2012).
Third. A partially disaggregated parcel approach was used: item parcels were used as indicators (i.e., items) of latent variables (Coffman & MacCallum, 2005; Little et al., 2002; Little et al., 2013). At least 3-item-parcel were created for each latent variable (each factor should be at least ‘just identified’) (Hoyle, 2012; Kline, 2016; Little et al., 2013) – statistics of item parcels are reported in the supplementary material. The ‘item-to-construct balance strategy’ (Little et al., 2013) was used to create parcels of the three unidimensional scales (RSE, ANX, and the DEP) – by inspecting factor loadings resulting from each measurement model (Little et al., 2002; Little et al., 2013). The ‘domain-representative strategy’ (Little et al., 2002; Little et al., 2013) was used to create parcels of the hierarchical second-order structure of the PTSQ – by aggregating together items of each dimension.
Fourth. Item parcels’ descriptive statistics were examined: a normal distribution was found for the large majority of item parcels (see supplementary material). Consequently, the maximum likelihood (ML) estimator was used to test the hypothesized SEM (Hoyle, 2012; Kline, 2016). A 10,000 bootstrap resampling procedure was applied (MacKinnon, 2012).
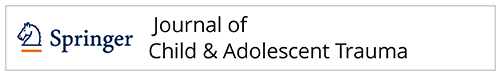
Fifth. The multiple mediation model with latent variables was tested using a three-step approach (Daniel et al., 2015; Hayes, 2022; MacKinnon, 2012; MacKinnon et al., 2007; VanderWeele & Vansteelandt, 2014). First, a predictor-only model was specified: the traumatic experience of COVID-19 (X) predicts depressive symptoms (Y). Second, a simple mediation model was specified by excluding the effect of self-esteem (buffering variable): the traumatic experience of COVID-19 (X) predicts depressive symptoms (Y) through anxiety symptoms (M). Statistical analyses of these intermediate models are reported in the supplementary material – Figure S1 and Figure S2. Lastly, a sequential multiple mediation model (full model) was specified (Fig. 3). The variance of each latent variable was fixed to unity. More in detail, the traumatic experience of COVID-19 (X) predicts depressive symptoms (Y) through anxiety symptoms (M2). However, according to the ABH, self-esteem (M1) should protect against the negative consequences – anxiety (M2) and depression (Y) – of the traumatic experience of COVID-19 (X). The goodness of the model was evaluated by using the abovementioned ‘goodness-of-fit’ indices (χ2, RMSEA, CFI, SRMR) and their cutoff values. Finally, all regression coefficients (β) reported in the text were unstandardized, whereas in Table 3 standardized regression coefficients (B) were also displayed.
Fig. 3.
Study 2. Conceptual graphical representation of the structural equation model
Table 3.
Summary of Standardized Parameter Estimates (Beta) with 95% Confidence Intervals for Key Pathways Tested (Fig. 4 )
| Path | B | β (SE) | 95%CI [L - U] | z-value | p-value | R2 | |
|---|---|---|---|---|---|---|---|
| Traumatic experience of COVID19 (X) → Self-esteem (M1) | (a1) | − 0.516 | -0.602 (0.075) | [-0.754; -0.464] | -8.059 | p < .001 | 0.266 |
| Self-esteem (M1) → Anxiety (M2) | (d) | − 0.154 | -0.162 (0.065) | [-0.292; -0.037] | -2.500 | p = .012 | 0.339 |
| Anxiety (M2) → Depression (Y) | (b2) | 0.413 | 0.703 (0.096) | [0.536; 0.910] | 7.333 | p < .001 | 0.772 |
| Traumatic experience of COVID19 (X) → Anxiety (M2) | (a2) | 0.488 | 0.601 (0.088) | [0.434; 0.782] | 6.796 | p < .001 | |
| Self-esteem (M1) → Depression (Y) | (b1) | − 0.407 | -0.731 (0.114) | [-0.977; -0.530] | -6.395 | p < .001 | |
| Traumatic experience of COVID19 (X) → Depression (Y) | (c1) | 0.260 | 0.544 (0.114) | [0.344; 0.788] | 4.794 | p < .001 | |
| Indirect effect of X on Y via M1 | (a1*b1) | 0.210 | 0.440 (0.082) | [0.305; 0.625] | 5.359 | p < .001 | |
| Indirect effect of X on Y via M2 | (a2*b2) | 0.202 | 0.422 (0.075) | [0.291; 0.586] | 5.627 | p < .001 | |
| Indirect effect of X1 on Y via M1 and M2 | (a1*d*b2) | 0.033 | 0.069 (0.031) | [0.015; 0.137] | 2.179 | p < .001 | |
| Total effect X1 on Y | 0.705 | 1.476 (0.169) | [1.197; 1.856] | 8.711 | p < .001 |
Note: B = standardized beta; β = unstandardized beta; 95%CI = 95% confidence intervals (lower and upper bound) for the unstandardized beta; R2 = explained variance
Results
Preliminary Analysis
The multivariate multiple regression analysis showed no statistically significant effects of potential confounding external variables. In addition, correlation analyses suggested small-to-large associations between the variables involved in the multiple mediation model – Supplementary material, Table S2 and Table S3.
Structural Models
The PTSQ showed adequate goodness-of-fit indices: χ2 (51) = 190.880; p < .001; RMSEA = 0.079, 90%CI[0.067, 0.091], p(RMSEA < 0.05) < .001; CFI = 0.989; SRMR = 0.061. Factor loadings of the first-order items ranged from 0.704 (item#4; INTR) to 0.836 (item#11 – HY.AR) (INTR: mean = 0.77, SD = 0.06; AV: mean = 0.82; SD = 0.06; HY.AR: mean = 0.79; SD = 0.04). Factor loadings of the second-order variable ranged from 0.682 (AV) to 0.974 (HY.AR) (mean = 0.80; SD = 0.13).
Even the RSE revealed good fit indices: χ2 (35) = 102.124; p < .001; RMSEA = 0.066, 90%CI[0.051, 0.081], p(RMSEA < 0.05) = .039; CFI = 0.992; SRMR = 0.054. Factor loadings of the items ranged from 0.427 (item#9) to 0.821 (item#10) (mean = 0.69; SD = 0.14).
Also the ANX showed good indices: χ2 (35) = 127.717; p < .001; RMSEA = 0.077, 90%CI[0.063, 0.092], p(RMSEA < 0.05) = .001; CFI = 0.995; SRMR = 0.046. Factor loadings of the items ranged from 0.718 (item#2) to 0.879 (item#3) (mean = 0.81; SD = 0.06).
Lastly, the DEP revealed good fit indices: χ2 (65) = 161.861; p < .001; RMSEA = 0.058, 90%CI[0.047, 0.069], p(RMSEA < 0.05) = .117; CFI = 0.994,; SRMR = 0.056. Factor loadings of the items ranged from 0.461 (item#1) to 0.878 (item#8) (mean = 0.73; SD = 0.10).
Harman’s Single-Factor Test
The first CFA with six correlated factors provided good fit indices: χ2 (930) = 2075.199; p < .001; RMSEA = 0.053, 90%CI[0.050, 0.056], p(RMSEA < 0.05) = .074; CFI = 0.989; SRMR = 0.063. On the contrary, the CFA with a single latent factor provided poor fit indices: χ2 (945) = 8667.104; p < .001; RMSEA = 0.136, 90%CI[0.133, 0.138], p(RMSEA < 0.05) < .001; CFI = 0.923; SRMR = 0.120. The Harman’s single-factor test model comparison suggested the absence of the ‘common method bias’: Δχ2 (15) = 6591.9, p < .001; |ΔRMSEA| = 0.083, and |ΔCFI| = 0.065.
Sequential Mediation Model
The hypothesized model (Fig. 4, Table 3) provided adequate goodness-of-fit indices: χ2 (84) = 224.050; p < .001; RMSEA = 0.061, 90%CI[0.052, 0.071], p(RMSEA < 0.05) = .028; CFI = 0.972; SRMR = 0.035. All of the item-parcels showed a factor loading higher than 0.66 (Table S4, supplementary material). According to the ABH, traumatic experience of COVID-19 (X) was negatively associated with self-esteem (M1), path a1: β = -0.602 (SE = 0.075) [95%CI: -0.754; -0.464], z = -8.059, p < .001, and self-esteem – in turn – negatively predicted anxiety symptomatology (M2), path d: β = -0.162 (SE = 0.065) [95%CI: -0.292; -0.037], z = -2.500, p = .012 – thus showing the buffering effect of self-esteem. Lastly, anxiety symptomatology (M2) positively predicted depressive symptomatology (Y) path b2: β = 0.703 (SE = 0.096) [95%CI: 0.536; 0.910], z = 7.333, p < .001. In addition, still in line with the ABH, self-esteem (M1) was negatively associated with depressive symptomatology (Y), path b1: β = -0.731 (SE = 0.114) [95%CI: -0.977; -0.530], z = -6.395, p < .001 – further revealing the buffering effect of self-esteem also on traumatic-related depressive symptoms. Furthermore, traumatic experience of COVID-19 (X) was positively associated with both anxiety symptomatology (M2) [path a2: β = 0.601 (SE = 0.088) [95%CI: 0.434; 0.782], z = 6.769, p < .001] and depressive symptomatology (Y) [path c1: β = 0.544 (SE = 0.114) [95%CI: 0.344; 0.788], z = 4.794, p < .001] – suggesting a partially mediated model that highlighted the buffering effect of self-esteem.
Fig. 4.
Study 2. Graphical representation of the structural equation model (N = 445). Note. Model fit: χ2 (84) = 224.050; p < .001; RMSEA = 0.061; 90%CI: 0.052, 0.071; CFI = 0.972; SRMR = 0.035.
The total indirect effect (traumatic experience of COVID-19 → self-esteem → anxiety symptomatology → depressive symptomatology) was statistically significant: β = 0.069 (SE = 0.031) [95%CI: 0.015; 0.137], z = 2.179, p = .029. Also, the total model effect was statistically significant: β = 1.476 (SE = 0.169) [95%CI: 1.197; 1.856], z = 8.711, p < .001. The total explained variance (R2) was equal to 0.772.
Discussion
Scientific literature highlighted how traumatic events can have a negative impact on mental health (Benjet et al., 2016). Traumatic events represent a risk factor for the onset and worsening of anxious reactions, then followed by depressive symptoms. In this line, COVID-19 represented a traumatic event and triggered intense adverse psychological reactions such as anxiety and depression.
The present study had two aims. First, to develop and evaluate the psychometric properties of a self-report questionnaire measuring the impact of the traumatic event that specifically takes into account intrusivity, hyperarousal, and avoidance. Second, to understand the psychological impact of traumatic events and emphasized how self-esteem can protect (buffer effect) from the negative outcomes (i.e., anxiety and depression) of traumatic events.
Considering Study1, the PTSQ was developed using a solid and theoretically-driven methodology. It proved to be a reliable and psychometrically sound assessment tool to measure the psychological impact of traumatic events – specifically focused on the three main reactions/domains of intrusivity, hyperarousal, and avoidance. Moreover, it is important to note that although the sample was collected from the general population, the questionnaire was administered only to individuals who had actually reported experiencing a traumatic event such as a severe accident (e.g., car crash, domestic accident, etc.) that threatened his/her own life; or threat to one’s life (e.g. being hit/hurt) from family members and/or partners and/or strangers; or a severe organic illness (i.e. cancer). Moreover, the PTSQ showed a second-order (i.e., hierarchical) factorial structure with 3 well-separated (but reasonably correlated) first-order factors – clearly reflecting the three main reactions/domains of traumatic events – providing good fit indices. Also, all the items had excellent factorial loadings on the hypothesized factors. Moreover, item analysis showed the ability of the single indicator to discriminate between individuals with a low and high level of the measured construct. Furthermore, the PTSQ allowed observing how different traumatic experiences can have some aspects in common in the three components. Indeed, traumatic events that are experienced in first-person had a stronger psychological impact compared to traumatic events experienced in second-person (e.g., ‘witnessing traumatic event experienced by another person’).
Considering Study 2, the structural equation model used to test the research hypotheses provided good results. The first model tested (Model 1, predictors only – supplementary material) showed that a state of post-traumatic symptoms might lead to the development of depressive symptoms (Santini et al., 2020; Thakur & Jain, 2020): a one-point increase in the severity of post-traumatic symptoms was associated with an increase of 0.981 points in the severity of the depressive symptomatology.
Still, even when considering the mediation effect of anxiety symptoms (Model 2, simple mediation model – supplementary material), post-traumatic symptoms and depression exhibited a positive association in line with a consistent body of scientific literature (Rossi et al., 2020). Simultaneously, post-traumatic symptoms showed a strong and positive association with anxiety symptomatology (Friedman et al., 2007; Friedman et al., 2011) which in turn can lead to developing depressive symptoms (Bowman, 2001). This pattern suggests a partial mediation model from post-traumatic symptoms, to depression through anxiety – since the former are frequently characterized by intense experiences hyperarousal, startling, and concern about the past and the future (Gagne et al., 2018).
Nevertheless, according to the research hypotheses, the final model undisclosed the buffering effect of self-esteem on the relationship between traumatic symptoms to anxiety. Notwithstanding the strong positive association between post-traumatic symptoms and anxiety (β = 0.547), self-esteem was able to hinder it. This result is perfectly in line with the TMT and the ABH (Greenberg et al., 1986; Greenberg et al., 1992). Indeed, self-esteem acts as a shield by protecting the individual from the self-reinforcing mechanisms that go between negative psychological constructs. In practice, from a theoretical point of view, at the moment when the impact of the traumatic event leads the individual to develop anxiety and depressive symptoms, self-esteem – by recovering the individual’s personal and social value and meaning – interferes with this concatenation of negative states (Greenberg et al., 1986; Greenberg et al., 1992; Rossi et al., 2020). Consequently, from a statistical point of view, self-esteem shows negative associations (negative β-values) with the psychological constructs of outcome of the traumatic event (i.e., anxiety and depression).
However, it is important to note that since the relationship between posttraumatic symptoms, anxiety and depression was maintained even when their relationships were buffered by self-esteem, a partial mediation model is the one that best describes the psychological phenomenon inherent in TMT and ABH (Greenberg et al., 1986; Greenberg et al., 1992; Pyszczynski et al., 2004; Solomon et al., 2004). Moreover, these results (sequential partial mediation) suggest a possible explanation for the fact that self-esteem cannot – by itself – completely prevent the presence of anxiety and depression. Indeed, again considering that the relationship between the impact of the traumatic event and the negative outcomes are not totally mediated (buffered) by self-esteem, therefore, the relationship between the negative variables continues to hold – even though the shield (i.e., self-esteem) helps to dampen their strength (Salzman & Halloran, 2004).
These findings showed that self-esteem can buffer the adverse effect of anxiety symptoms generated by traumatic symptoms. Consequently, these results provide additional support for the soundness of the ABH – that highlighted the buffering role of self-esteem on the relationship between post-traumatic symptoms, anxiety, and depression (Pyszczynski et al., 2004).
Considering clinical implications, findings can suggest a potential line of intervention in order to offer psychological help for individuals facing the emerging adulthood phase and dealing with the adverse psychological outcomes of the impact of traumatic events such as the prolonged pandemic of COVID-19, with the aim to relieve it. As mentioned above, young adults are the category most at risk of traumatic consequences related to COVID-19 (Cao et al., 2020; Silva Junior et al., 2020). Although COVID-19 impacted individuals of all life ages, the consequences such as restrictions have especially impacted emerging adults’ opportunities for personal growth and the structuring of one’s personal identity and self-esteem (van den Berg et al., 2021). Specifically, the consequences of COVID-19 could exacerbate the vulnerabilities of emerging adulthood. Among the life span life, emerging adulthood is a crucial developmental period with significant changes in life roles (Arnett, 2006, 2016). Individuals are called to define and adapt self and identity (Arnett, 2016). This phase includes a large number of challenges and risks that can affect psychological adjustment (Berzin, 2010; Burt & Masten, 2010).
To this extent, the ABH posits that self-esteem can protect against various stressors, which in turn can intensify the need for self-esteem to buffer psychological difficulties (Harmon-Jones et al., 1997). As a result, improved self-esteem is supposed to serve as a buffer against anxiety, weakening the negative psychological reactions to stressors and threats to the individuals’ health. Therefore, implanting and improving psychological strategies to specifically target self-esteem may represent an efficient approach to reducing the adverse psychological consequences of traumatic symptoms related to post-traumatic events such as COVID-19 – in particular among young adults who showed to be more vulnerable and prone to develop them (Liu et al., 2020; Panzeri et al., 2021).
This study is not free of limitations. The observational/correlational research design did not allow for defining a causal relationship among variables, but only relationships of statistical predictions (Fiedler et al., 2011) – as in line with the aim of the study. Cross sectional research design has limitations compared to longitudinal designs but is still able to provide a photograph of the participants psychological conditions at a given time. Importantly, a considerable amount of scientific literature refers to ‘statistical mediation’ as ‘mediation’, but a desirable way to assess mediation would be through longitudinal studies. Moreover, the online survey consisting of self-reports may have been influenced by well-known biases, such as social desirability. Also, the sample presents a high prevalence of females (68.6%), despite no associated effects emerging from the preliminary analyses. Moreover, a multi-group analysis (moderated mediation) comparing the model across males and females was not performed because of the small presence of males – which would have not allowed to provide an accurate estimation of model parameters (Hoyle, 2012; Kline, 2016). Future research may try to overcome these limitations.
Concluding, both theoretical and statistical reasons supported the choice of a mediation model rather than a moderation one. Theoretically, ABH and TMT (Greenberg et al., 1986; Greenberg et al., 1992) hypothesize self-esteem to be an intermediating shield (buffer) between stressors and anxiety (Pyszczynski et al., 2004), thus a mediation approach can better reflect this pattern. Indeed, self-esteem is both able to impact subjective anxiety and depression and it can also be modified by negative emotional traumatic experiences that can deeply (negatively) modify the evaluation of oneself (Greenberg et al., 1986; Heinrich & Gullone, 2006; Sowislo & Orth, 2013). Literature showed that, by activating negative cognitions and emotions, traumatic experiences can significantly worsen the self-evaluation and self-concept (Greenberg et al., 1986) (i.e., feeling a failure, feeling worthless) (Beck, 1979), also progressively reducing self-efficacy and self-esteem (Sowislo & Orth, 2013). For the abovementioned reasons, a moderation model would have not been in line with the theoretical background and could not allow considering the complexity of relationships among constructs.
The present study also has some strengths. First, both Study 1 and Study 2 are grounded on well-established theoretical foundations relying on several experimental and longitudinal studies’ support (Brage & Meredith, 1994; Greenberg et al., 1992; Heinrich & Gullone, 2006; Pyszczynski et al., 2004). Second, Study 1 provides a brief but solid measure to assess post traumatic symptoms. In fact, the PTSQ is much shorter than other common scales for assessing trauma response such as the impact of event scale – revised (IES-R) which has 22 items (Weiss, 2007; Weiss & Marmar, 1996) but the PTSQ is equally robust, psychometrically grounded. In addition, it is worth noting that the 15-item version of the IES (Horowitz et al., 1979) is missing the hyperarousal symptom dimension according to the DSM – which is measured by the PTSQ instead: indeed, the PTSQ accurately measures the three components of intrusiveness, avoidance, and hyperarousal. Moreover, the solid psychometric foundation of the instrument, is also seen in comparison with drastically shorter scales – such as the 6-item Impact of Event Scale (Giorgi et al., 2015). In fact, that scale having only two items for each of the 3 dimensions, turns out to be under-identified in the latter. The PTSQ, having 4 items per latent dimension, turns out to be over-identified – which is the ideal condition for measurement scales (Brown, 2015; Hoyle, 2012; Kline, 2016). Because of its length, the PTSQ can be easily integrated into surveys or batteries of instruments and has – in addition – proven to be a useful, accurate and valid measure of psychological constructs in research settings (Rossi et al., 2022; Schipolowski et al., 2014). Third, the sample size from the general Italian population allowed utilizing robust statistical analysis and methodologies (MacKinnon, 2012; MacKinnon et al., 2007) to offer interesting results. Additionally, all the models hypothesized and tested provided a good fit.
Moreover, findings from this research could be extended and generalized to people coping with the adverse impact of traumatic experiences, in particular health-related (e.g., smallpox and/or diagnosis of severe cancer) (Betancourt et al., 2016; Brown & Lees-Haley, 1992; Chew et al., 2020; Huremović, 2019). As an instance, these results could lead to useful applications to relieve the psychological consequences of traumatic reactions toward self-threats (Rossi Ferrario & Panzeri, 2020). For example, based on these findings, clinicians may develop interventions to improve people’s psychological health and well-being. Overall, this research provides a valuable contribution to the current stream of literature disentangling the psycho-social impact of COVID-19.
Future longitudinal studies are needed to understand how psychological difficulties-progressing over time may be affected by self-esteem. Also, future studies may deepen the process through which other protective or risk factors could impact psychological outcomes.
Conclusion
In conclusion, this study provides additional evidence about the anxiety-buffer effect on self-esteem, once again confirming the effectiveness and usefulness of TMT in providing valuable research and clinical insights into understanding and handling trauma-related experiences.
People dealing with traumatic-related events (and their impact) should be supported through targeted psychological interventions aiming at reducing the trauma’s psychological impact and favoring resilient psychological health outcomes.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Author Contributions
AAR: conceptualization, formal analysis, methodology, writing the original draft, review, and editing. A.Panzeri: data collection, writing the original draft, methodology, review, and editing. A.Parola: data collection, review, and editing. FT: contribution in developing the PTSQ, review, and editing. SM: review and editing.
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data Availability
The datasets presented in this article are not readily available because due to privacy restrictions, data were available from the corresponding author on a reasonable request.
Declarations
Ethical Approval
The study was in accordance with the ethical standards of the Ethical Committee of the University of Padua.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
1/6/2023
A Correction to this paper has been published: 10.1007/s40653-022-00512-y
References
- Agaibi CE, Wilson JP. Trauma, PTSD, and resilience:a review of the literature. Trauma Violence & Abuse. 2005;6(3):195–216. doi: 10.1177/1524838005277438. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Association.
- Arnett, J. J. (2006). Emerging Adulthood: understanding the New Way of coming of Age. Emerging adults in America: coming of age in the 21st century (pp. 3–19). American Psychological Association. 10.1037/11381-001.
- Arnett JJ. College Students as emerging adults:the Developmental Implications of the College Context. Emerging Adulthood. 2016;4(3):219–222. doi: 10.1177/2167696815587422. [DOI] [Google Scholar]
- Barbaranelli C, Lee CS, Vellone E, Riegel B. Dimensionality and reliability of the self-care of heart failure index scales: further evidence from confirmatory factor analysis. Research In Nursing & Health. 2014;37(6):524–537. doi: 10.1002/nur.21623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barlow, D. H. (2002). In D. H. Barlow (Ed.), Anxiety and its Disorders: the nature and treatment of anxiety and panic (2nd ed.). The Guilford Press.
- Baud D, Qi X, Nielsen-Saines K, Musso D, Pomar L, Favre G. Real estimates of mortality following COVID-19 infection. The Lancet Infectious Diseases. 2020;20(7):773. doi: 10.1016/s1473-3099(20)30195-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, A. T. (1979). In A. T. Beck (Ed.), Cognitive therapy of depression. The Guilford Press.
- Becker, E. (1971). Birth and death of meaning: an interdisciplinary perspective on the Problem of Man. Free Press.
- Becker, E. (1973). The denial of death. Simon & Schuster.
- Benight CC. Understanding human adaptation to traumatic stress exposure: beyond the medical model. Psychological Trauma: Theory Research Practice and Policy. 2012;4(1):1–8. doi: 10.1037/a0026245. [DOI] [Google Scholar]
- Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, Shahly V, Stein DJ, Petukhova M, Hill E, Alonso J, Atwoli L, Bunting B, Bruffaerts R, Caldas-de-Almeida JM, de Girolamo G, Florescu S, Gureje O, Huang Y, Lepine JP, Kawakami N, Kovess-Masfety V, Medina-Mora ME, Navarro-Mateu F, Piazza M, Posada-Villa J, Scott KM, Shalev A, Slade T, ten Have M, Torres Y, Viana MC, Zarkov Z, Koenen KC. The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychological Medicine. 2016;46(2):327–343. doi: 10.1017/s0033291715001981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berzin SC. Vulnerability in the transition to adulthood: defining risk based on youth profiles. Children and Youth Services Review. 2010;32(4):487–495. doi: 10.1016/j.childyouth.2009.11.001. [DOI] [Google Scholar]
- Betancourt TS, Brennan RT, Vinck P, VanderWeele TJ, Spencer-Walters D, Jeong J, Akinsulure-Smith AM, Pham P. Associations between Mental Health and Ebola-Related Health Behaviors: a regionally Representative cross-sectional survey in post-conflict Sierra Leone. PLOS Medicine. 2016;13(8):e1002073. doi: 10.1371/journal.pmed.1002073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bishop LS, Ameral VE, Palm Reed KM. The impact of Experiential Avoidance and Event Centrality in Trauma-Related rumination and posttraumatic stress. Behavior Modification. 2018;42(6):815–837. doi: 10.1177/0145445517747287. [DOI] [PubMed] [Google Scholar]
- Bowman GS. Emotions and illness. Journal of Advanced Nursing. 2001;34(2):256–263. doi: 10.1046/j.1365-2648.2001.01752.x. [DOI] [PubMed] [Google Scholar]
- Brage D, Meredith W. A causal model of adolescent depression. The Journal of psychology. 1994;128(4):455–468. doi: 10.1080/00223980.1994.9712752. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC. Posttraumatic stress disorder in an urban population of young adults: risk factors for chronicity. The American Journal of Psychiatry. 1992;149(5):671–675. doi: 10.1176/ajp.149.5.671. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC, Andreski P, Peterson E. Traumatic events and posttraumatic stress disorder in an Urban Population of Young adults. Archives Of General Psychiatry. 1991;48(3):216–222. doi: 10.1001/archpsyc.1991.01810270028003. [DOI] [PubMed] [Google Scholar]
- Briere J, Spinazzola J. Phenomenology and psychological assessment of complex posttraumatic states. Journal of Traumatic Stress. 2005;18(5):401–412. doi: 10.1002/jts.20048. [DOI] [PubMed] [Google Scholar]
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/s0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brosschot JF, Verkuil B, Thayer JF. The default response to uncertainty and the importance of perceived safety in anxiety and stress: an evolution-theoretical perspective. Journal of Anxiety Disorders. 2016;41:22–34. doi: 10.1016/j.janxdis.2016.04.012. [DOI] [PubMed] [Google Scholar]
- Brown RS, Lees-Haley PR. Fear of future illness, Chemical Aids, and Cancerphobia: a review. Psychological Reports. 1992;71(1):187–207. doi: 10.2466/pr0.1992.71.1.187. [DOI] [PubMed] [Google Scholar]
- Brown, T. A. (2015). Confirmatory factor analysis for Applied Research (Second ed.). The Guilford Press.
- Burt, K. B., & Masten, A. S. (2010). Development in the transition to adulthood: vulnerabilities and opportunities. In J. E. Grant, & M. N. Potenza (Eds.), Young adult mental health (pp. 5–18). Oxford University press.
- Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;287:112934. doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng C, Jun H, Baoyong L. Psychological Health Diathesis Assessment System: a nationwide survey of resilient trait scale for chinese adults. Studies of Psychology and Behavior. 2014;12(6):735–742. [Google Scholar]
- Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Structural equation modeling. 2002;9:233–255. doi: 10.1207/S15328007SEM0902_5. [DOI] [Google Scholar]
- Chew Q, Wei K, Vasoo S, Chua H, Sim K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: practical considerations for the COVID-19 pandemic. Singapore Medical Journal. 2020;61(7):350–356. doi: 10.11622/SMEDJ.2020046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiorri, C. (2011). Teoria e tecnica psicometrica. Costruire un test psicologico. McGraw-Hill Companies.
- Coffman DL, MacCallum RC. Using parcels to convert path analysis models into latent variable models. Multivariate Behav Res. 2005;40(2):235–259. doi: 10.1207/s15327906mbr4002_4. [DOI] [PubMed] [Google Scholar]
- Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates.
- Daniel RM, De Stavola BL, Cousens SN, Vansteelandt S. Causal mediation analysis with multiple mediators. Biometrics. 2015;71(1):1–14. doi: 10.1111/biom.12248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis, L. R., & Unger, R. (2010). Symptom Checklist-90-Revised. Corsini Encyclopedia of psychology. John Wiley & Sons, Inc. 10.1002/9780470479216.corpsy0970.
- Djelantik AAAMJ, Robinaugh DJ, Kleber RJ, Smid GE, Boelen PA. Symptomatology following loss and trauma: latent class and network analyses of prolonged grief disorder, posttraumatic stress disorder, and depression in a treatment-seeking trauma‐exposed sample. Depression and Anxiety. 2020;37:26–34. doi: 10.1002/da.22880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebel, R. L. (1965). Measuring educational achievement. Prentice-Hall.
- Esterwood, E., & Saeed, S. A. (2020). Past Epidemics, Natural Disasters, COVID19, and Mental Health: Learning from History as we Deal with the Present and Prepare for the Future. Psychiatric Quarterly, 91(4), 1121-1133. https://doi.org/10.1007/s11126-020-09808-4 [DOI] [PMC free article] [PubMed]
- Fiedler K, Schott M, Meiser T. What mediation analysis can (not) do. Journal of Experimental Social Psychology. 2011;47(6):1231–1236. doi: 10.1016/j.jesp.2011.05.007. [DOI] [Google Scholar]
- Fisher EB, Miller SM, Evans M, Luu SL, Tang PY, Valovcin D, Castellano C. COVID-19, stress, trauma, and peer support—observations from the field. Translational Behavioral Medicine. 2020;10(3):503–505. doi: 10.1093/tbm/ibaa056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forero CG, Maydeu-Olivares A, Gallardo-Pujol D. Factor analysis with Ordinal Indicators: a Monte Carlo Study comparing DWLS and ULS Estimation. Structural Equation Modeling: A Multidisciplinary Journal. 2009;16(4):625–641. doi: 10.1080/10705510903203573. [DOI] [Google Scholar]
- Friedman, M. J., Keane, T. M., & Resick, P. A. (2007). In M. J. Friedman, T. M. Keane, & P. A. Resick (Eds.), Handbook of PTSD: Science and Practice (3rd ed.). The Guilford Press.
- Friedman MJ, Resick PA, Bryant RA, Brewin CR. Considering PTSD for DSM-5. Depression and Anxiety. 2011;28(9):750–769. doi: 10.1002/da.20767. [DOI] [PubMed] [Google Scholar]
- Gagne C, Dayan P, Bishop SJ. When planning to survive goes wrong: predicting the future and replaying the past in anxiety and PTSD. Curr Opin Behav Sci. 2018;24:89–95. doi: 10.1016/j.cobeha.2018.03.013. [DOI] [Google Scholar]
- Giorgi G, Fiz Perez FS, Castiello D’Antonio A, Mucci N, Ferrero C, Cupelli V, Arcangeli G. Psychometric properties of the impact of event Scale-6 in a sample of victims of bank robbery. Psychol Res Behav Manag. 2015;8:99–104. doi: 10.2147/PRBM.S73901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graupensperger S, Calhoun BH, Patrick ME, Lee CM. Longitudinal effects of COVID-19-related stressors on young adults’ mental health and wellbeing. Applied Psychology: Health and Well-Being. 2022;14(3):734–756. doi: 10.1111/aphw.12344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg, J., Pyszczynski, T., & Solomon, S. (1986). The Causes and Consequences of a Need for Self-Esteem: A Terror Management Theory. In R. F. Baumeister (Ed.), Public Self and Private Self (pp. 189–212). Springer New York. 10.1007/978-1-4613-9564-5_10
- Greenberg J, Solomon S, Pyszczynski T, Rosenblatt A, Burling J, Lyon D, Simon L, Pinel E. Why do people need self-esteem? Converging evidence that self-esteem serves an anxiety-buffering function. J Pers Soc Psychol. 1992;63(6):913–922. doi: 10.1037/0022-3514.63.6.913. [DOI] [PubMed] [Google Scholar]
- Harding KJ, Skritskaya N, Doherty E, Fallon BA. Advances in understanding illness anxiety. Curr Psychiatry Rep. 2008;10(4):311–317. doi: 10.1007/s11920-008-0050-1. [DOI] [PubMed] [Google Scholar]
- Harmon-Jones E, Simon L, Greenberg J, Pyszczynski T, Solomon S, McGregor H. Terror management theory and self-esteem: evidence that increased self-esteem reduced mortality salience effects. J Pers Soc Psychol. 1997;72(1):24–36. doi: 10.1037/0022-3514.72.1.24. [DOI] [PubMed] [Google Scholar]
- Hayes, A. F. (2022). Introduction to mediation, moderation, and conditional process analysis: a regression-based approach (3rd ed.). Guilford publications.
- Hedges LV. Distribution theory for Glass’s Estimator of Effect size and related estimators. Journal of Educational Statistics. 1981;6(2):107–128. doi: 10.3102/10769986006002107. [DOI] [Google Scholar]
- Heinrich LM, Gullone E. The clinical significance of loneliness: a literature review. Clinical Psychology Review. 2006;26(6):695–718. doi: 10.1016/j.cpr.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Horowitz, M., Wilner, N., & Alvarez, W. (1979). Impact of Event Scale: A Measure of Subjective Stress.Psychosomatic Medicine, 41(3). https://journals.lww.com/psychosomaticmedicine/Fulltext/1979/05000/Impact_of_Event_Scale__A_Measure_of_Subjective.4.aspx [DOI] [PubMed]
- Howell, D. C. (2013). Statistical methods for psychology. Wadsworth, Cengage Learning.
- Hoyle, R. H. (2012). Handbook of Strucural equation modeling. The Guilford Press.
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural equation modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Huremović, D. (2019). Psychiatry of Pandemics. A Mental Health Response to Infection Outbreak (D. Huremović, Ed.). 10.1007/978-3-030-15346-5
- Iannone, R. (2018). DiagrammeR: Graph/Network Visualization. In (Version 1.0.0) https://CRAN.R-project.org/package=DiagrammeR
- Johnson, T. P. (2014). Snowball Sampling: Introduction. In Wiley StatsRef: Statistics Reference Online. 10.1002/9781118445112.stat05720
- Jorgensen, T. D., Pornprasertmanit, S., Schoemann, A. M., & Rosseel, Y. (2019). semTools: Useful tools for structural equation modeling. In (Version 0.5-2) https://CRAN.R-project.org/package=semTools
- Karatzias T, Hyland P, Bradley A, Cloitre M, Roberts NP, Bisson JI, Shevlin M. Risk factors and comorbidity of ICD-11 PTSD and complex PTSD: findings from a trauma-exposed population based sample of adults in the United Kingdom. Depression and Anxiety. 2019;36(9):887–894. doi: 10.1002/da.22934. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Aguilar-Gaxiola S, Alonso J, Benjet C, Bromet EJ, Cardoso G, Degenhardt L, de Girolamo G, Dinolova RV, Ferry F, Florescu S, Gureje O, Haro JM, Huang Y, Karam EG, Kawakami N, Lee S, Lepine JP, Levinson D, Navarro-Mateu F, Pennell BE, Piazza M, Posada-Villa J, Scott KM, Stein DJ, Ten Have M, Torres Y, Viana MC, Petukhova MV, Sampson NA, Zaslavsky AM, Koenen KC. Trauma and PTSD in the WHO World Mental Health surveys. European Journal of Psychotraumatology. 2017;8(sup5):1353383. doi: 10.1080/20008198.2017.1353383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives Of General Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kline, R. B. (2016). Principles and practice of structural equation modeling. The Guilford Press.
- Kratovic L, Smith LJ, Vujanovic AA. PTSD symptoms, suicidal ideation, and suicide risk in University students: the role of distress tolerance. Journal of Aggression Maltreatment & Trauma. 2021;30(1):82–100. doi: 10.1080/10926771.2019.1709594. [DOI] [Google Scholar]
- lavaan RY. An R Package for Structural equation modeling. Journal Of Statistical Software. 2012;48:1–36. [Google Scholar]
- Li CH. The performance of ML, DWLS, and ULS estimation with robust corrections in structural equation models with ordinal variables. Psychological Methods. 2016;21(3):369–387. doi: 10.1037/met0000093. [DOI] [PubMed] [Google Scholar]
- Little TD, Cunningham WA, Shahar G, Widaman KF. To Parcel or not to Parcel: exploring the question, weighing the merits. Structural Equation Modeling: A Multidisciplinary Journal. 2002;9(2):151–173. doi: 10.1207/s15328007sem0902_1. [DOI] [Google Scholar]
- Little TD, Rhemtulla M, Gibson K, Schoemann AM. Why the items versus parcels controversy needn’t be one. Psychological Methods. 2013;18(3):285–300. doi: 10.1037/a0033266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu CH, Zhang E, Wong GTF, Hyun S, Hahm HC. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Research. 2020;290:113172. doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon, D. P. (2012). Introduction to statistical mediation analysis. Routledge.
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58(1):593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald, R. P. (1999). Test theory: a unified treatment. Lawrence Erlbaum Associates.
- McIntyre RS, Lee Y. Preventing suicide in the context of the COVID-19 pandemic. World Psychiatry. 2020;19(2):250–251. doi: 10.1002/wps.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milavic, B., Padulo, J., Grgantov, Z., Milić, M., Mannarini, S., Manzoni, G. M., Ardigò, L. P., & Rossi, A. (2019). Development and factorial validity of the psychological skills inventory for Sports, Youth Version – Short Form: Assessment of the psychometric properties [Article]. PLoS One, 14(8), 10.1371/journal.pone.0220930. Article e0220930. [DOI] [PMC free article] [PubMed]
- Millsap, R. E. (2012). Statistical approaches to measurement invariance [Book]. Routledge. 10.4324/9780203821961.
- Orcutt HK, Erickson DJ, Wolfe J. A prospective analysis of Trauma exposure: the mediating role of PTSD Symptomatology. Journal of Traumatic Stress. 2002;15(3):259–266. doi: 10.1023/a:1015215630493. [DOI] [PubMed] [Google Scholar]
- Pacella ML, Hruska B, Delahanty DL. The physical health consequences of PTSD and PTSD symptoms: a meta-analytic review. Journal of Anxiety Disorders. 2013;27(1):33–46. doi: 10.1016/j.janxdis.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Panzeri, A., Bertamini, M., Butter, S., Levita, L., Gibson-Miller, J., Vidotto, G., Bentall, R. P., & Bennett, K. M. (2021). Factors impacting resilience as a result of exposure to COVID-19: the ecological resilience model [Article]. PLoS One, 16(8 August), 10.1371/journal.pone.0256041. Article e0256041. [DOI] [PMC free article] [PubMed]
- Parola, A. (2020). Novel coronavirus outbreak and Career Development: a narrative approach into the meaning of italian university graduates. Frontiers In Psychology, 11(2255), 10.3389/fpsyg.2020.02255. [DOI] [PMC free article] [PubMed]
- Parola A, Rossi A, Tessitore F, Troisi G, Mannarini S. Mental Health through the COVID-19 Quarantine: a growth curve analysis on italian young adults [Article] Frontiers In Psychology. 2020;11:567484. doi: 10.3389/fpsyg.2020.567484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parola, A., Fusco, L., & Marcionetti, J. (2022). The parental career-related behaviors questionnaire (PCB): Psychometric properties in adolescents and young adults in the Italian context. Current Psychology. 10.1007/s12144-022-02764-1.
- Pietrabissa G, Rossi A, Borrello M, Manzoni GM, Mannarini S, Castelnuovo G, Molinari E. Development and validation of a self-determination theory-based measure of motivation to Exercise and Diet in children [Article] Frontiers In Psychology. 2020;11:1299. doi: 10.3389/fpsyg.2020.01299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrabissa G, Rossi A, Simpson S, Tagliagambe A, Bertuzzi V, Volpi C, Fava G, Manzoni GM, Gravina G, Castelnuovo G. Evaluation of the reliability and validity of the italian version of the schema mode inventory for eating disorders: short form for adults with dysfunctional eating behaviors [Article] Eating and Weight Disorders. 2020;25(3):553–565. doi: 10.1007/s40519-019-00644-5. [DOI] [PubMed] [Google Scholar]
- Pyszczynski T, Greenberg J, Solomon S, Arndt J, Schimel J. Why do people need Self-Esteem? A theoretical and empirical review. Psychological Bulletin. 2004;130(3):435–468. doi: 10.1037/0033-2909.130.3.435. [DOI] [PubMed] [Google Scholar]
- Raykov T. Scale validity evaluation with congeneric measures in hierarchical designs. British Journal of Mathematical and Statistical Psychology. 2011;64(3):427–438. doi: 10.1348/000711009X484286. [DOI] [PubMed] [Google Scholar]
- Raykov, T. (2012). Scale construction and development using structural equation modeling. In R. H. Hoyle (Ed.), Handbook of structural equation modeling (pp. 472–492). The Guilford Press.
- Raykov, T., & Marcoulides, G. A. (2011). Introduction to psychometric theory. Routledge.
- Revelle, W. (2018). Psych: procedures for personality and Psychological Research. Northwestern University.
- Rosenberg, M. (1965). Society and the adolescent self-image. Princeton University Press.
- Rossi, A., Panzeri, A., Pietrabissa, G., Manzoni, G. M., Castelnuovo, G., & Mannarini, S. (2020). The Anxiety-Buffer Hypothesis in the Time of COVID-19: When Self-Esteem Protects From the Impact of Loneliness and Fear on Anxiety and Depression [Article]. Front Psychol, 11, Article 2177. 10.3389/fpsyg.2020.02177 [DOI] [PMC free article] [PubMed]
- Rossi, A. A., Marconi, M., Taccini, F., Verusio, C., & Mannarini, S. (2021). From fear to hopelessness: the buffering effect of patient-centered communication in a sample of oncological patients during covid-19 [Article]. Behavioral Sciences, 11(6), 10.3390/bs11060087. [DOI] [PMC free article] [PubMed]
- Rossi, A. A., Marconi, M., Taccini, F., Verusio, C., & Mannarini, S. (2022a). Screening for Distress in Oncological Patients: The Revised Version of the Psychological Distress Inventory (PDI-R) [Original Research]. Front Psychol, 13. 10.3389/fpsyg.2022.859478 [DOI] [PMC free article] [PubMed]
- Rossi, A. A., Panzeri, A., & Mannarini, S. (2022). The Italian Version of the Difficulties in Emotion Regulation Scale - Short Form (IT-DERS-SF): A Two-Step Validation Study. Journal of Psychopathology and Behavioral Assessment. https://doi.org/10.1007/s10862-022-10006-8
- Rossi Ferrario S, Panzeri A. Exploring illness denial of LVAD patients in cardiac rehabilitation and their caregivers: a preliminary study. Artificial Organs. 2020 doi: 10.1111/aor.13630. [DOI] [PubMed] [Google Scholar]
- Salzman, M. B., & Halloran, M. J. (2004). Cultural trauma and recovery: Cultural meaning, self-esteem and the reconstruction of the cultural anxiety buffer.
- Santini ZI, Jose PE, Cornwell Y, Koyanagi E, Nielsen A, Hinrichsen L, Meilstrup C, Madsen C, Koushede V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. The Lancet Public Health. 2020;5(1):e62–e70. doi: 10.1016/S2468-2667(19)30230-0. [DOI] [PubMed] [Google Scholar]
- Sareen J, Cox BJ, Stein MB, Afifi TO, Fleet C, Asmundson GJG. Physical and Mental Comorbidity, disability, and suicidal Behavior Associated with Posttraumatic stress disorder in a large community sample. Psychosomatic Medicine. 2007;69(3):242–248. doi: 10.1097/PSY.0b013e31803146d8. [DOI] [PubMed] [Google Scholar]
- Schipolowski S, Schroeders U, Wilhelm O. Pitfalls and challenges in constructing short forms of cognitive ability measures. Journal of Individual Differences. 2014;35:190–200. doi: 10.1027/1614-0001/a000134. [DOI] [Google Scholar]
- Shevlin, M., Butter, S., McBride, O., Murphy, J., Gibson-Miller, J., Hartman, T. K., Levita, L., Mason, L., Martinez, A. P., McKay, R., Stocks, T. V. A., Bennett, K., Hyland, P., & Bentall, R. P. (2021). Refuting the myth of a ‘tsunami’ of mental ill-health in populations affected by COVID-19: evidence that response to the pandemic is heterogeneous, not homogeneous. Psychological Medicine, 1–9. 10.1017/s0033291721001665. [DOI] [PMC free article] [PubMed]
- Silva Junior, F. J. G., d., Sales, J. C. S., Monteiro, C. F., d., S., Costa, A. P. C., Campos, L. R. B., Miranda, P. I. G., Monteiro, T. A. d., Lima, S., R. A. G., & Lopes-Junior, L. C. (2020). Impact of COVID-19 pandemic on mental health of young people and adults: a systematic review protocol of observational studies. BMJ Open, 10(7), e039426. 10.1136/bmjopen-2020-039426 [DOI] [PMC free article] [PubMed]
- Silver RC. Surviving the trauma of COVID-19. Science. 2020;369(6499):11–11. doi: 10.1126/science.abd5396. [DOI] [PubMed] [Google Scholar]
- Solomon, S., Greenberg, J., & Pyszczynski, T. (2004). The Cultural Animal: twenty years of Terror Management Theory and Research. Handbook of experimental existential psychology (pp. 13–34). Guilford Press.
- Sowislo JF, Orth U. Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychological Bulletin. 2013;139(1):213–240. doi: 10.1037/a0028931. [DOI] [PubMed] [Google Scholar]
- Starr LR, Davila J. Responding to anxiety with rumination and hopelessness: mechanism of anxiety-depression Symptom Co-Occurrence? Cognitive Therapy and Research. 2012;36(4):321–337. doi: 10.1007/s10608-011-9363-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick, B. G., & Fidell, L. S. (2014). Using Multivariate Statistics. Pearson.
- Tessitore F, Parola A, Margherita G. Mental Health risk and protective factors of nigerian male asylum seekers hosted in Southern Italy: a culturally sensitive quantitative investigation. J Racial Ethn Health Disparities. 2022 doi: 10.1007/s40615-022-01260-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thakur V, Jain A. COVID 2019-suicides: a global psychological pandemic. Brain Behavior and Immunity. 2020;88:952–953. doi: 10.1016/j.bbi.2020.04.062. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Thompson EA, Mazza JJ, Herting JR, Randell BP, Eggert LL. The mediating roles of anxiety, Depression, and hopelessness on adolescent suicidal behaviors. Suicide and Life-Threatening Behavior. 2005;35(1):14–34. doi: 10.1521/suli.35.1.14.59266. [DOI] [PubMed] [Google Scholar]
- Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. International Journal of Social Psychiatry. 2020;66(4):317–320. doi: 10.1177/0020764020915212. [DOI] [PubMed] [Google Scholar]
- van de Schoot R, Lugtig P, Hox J. A checklist for testing measurement invariance. European Journal of Developmental Psychology. 2012;9(4):486–492. doi: 10.1080/17405629.2012.686740. [DOI] [Google Scholar]
- van den Berg YHM, Burk WJ, Cillessen AHN, Roelofs K. Emerging adults’ Mental Health during the COVID-19 pandemic: a prospective longitudinal study on the importance of Social Support. Emerging Adulthood. 2021;9(5):618–630. doi: 10.1177/21676968211039979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele T, Vansteelandt S. Mediation analysis with multiple mediators. Epidemiologic Methods. 2014;2(1):95–115. doi: 10.1515/em-2012-0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., & Ho, R. C. (2020). Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health, 17(5), 1729. https://www.mdpi.com/1660-4601/17/5/1729 [DOI] [PMC free article] [PubMed]
- Waseem S, Nayar SK, Hull P, Carrothers A, Rawal J, Chou D, Khanduja V. The global burden of trauma during the COVID-19 pandemic: a scoping review. Journal of Clinical Orthopaedics and Trauma. 2021;12(1):200–207. doi: 10.1016/j.jcot.2020.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss, D. S. (2007). The impact of event scale: revised. In J. P. Wilson, & C. S. Tang (Eds.), Cross-cultural Assessment of Psychological Trauma and PTSD (pp. 219–238). Springer US. 10.1007/978-0-387-70990-1_10.
- Weiss, D. S., & Marmar, C. R. (1996). The impact of event scale - revised. In J. Wilson, & T. M. Keane (Eds.), Assessing psychological trauma and PTSD (pp. 399–411). Guilford Press.
- Yaribeygi H, Panahi Y, Sahraei H, Johnston TP, Sahebkar A. The impact of stress on body function: a review. EXCLI Journal. 2017;16:1057–1072. doi: 10.17179/excli2017-480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Pan R, Cai Y, Pan J. The prevalence of post-traumatic stress disorder in the General Population during the COVID-19 pandemic: a systematic review and single-arm Meta-analysis. Psychiatry Investig. 2021;18(5):426–433. doi: 10.30773/pi.2020.0458. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets presented in this article are not readily available because due to privacy restrictions, data were available from the corresponding author on a reasonable request.