SESSION 1: BREAST
1. Axillary Clearance For Cn0 Breast Cancer When Z011 Criteria Are Not Met - Is It Worth It?
Colm Neary, Nicola Raftery, Anna Heeney, Maurice Stokes, John Mitchel Barry, Malcolm Kell, Siun Walsh
Oncoplastic Breast Surgery, Mater Misericordiae Hospital, Eccles St., Dublin, Ireland
Introduction
For women who do not meet Z0011 criteria, axillary lymph node dissection (ALND) is recommended. A proportion of this population may harbor no residual metastatic disease, and thus the benefit of ALND is questionable.
Aim
This study aims to identify risk factors for further nodal disease and determine the benefit of ALND in this group.
Methods
All patients who had sentinel lymph node biopsy (SLNB) followed by ALND from 2010–2015 in our unit were included. Those who has neoadjuvant treatment were excluded. Regression analysis was performed to identify pre-operative variables associated with further nodal burden, and predictors of distant recurrence free survival (DRFS) and overall survival (OS).
Results
Among 67 patients who met inclusion criteria, 44 (65.7%) had no additional positive nodes. Mastectomy (50.7%) followed by extra-nodal extension (37.3%) were the most common reasons Z0011 criteria were not met. On multivariable analysis only extranodal extension was predictive of further nodal metastases (HR 3.74 {CI 1.17 – 11.9}, p = .02). The presence of additional positive nodes on ALND was not associated with decreased DRFS (HR 1.76 {CI 0.47 – 6.5}, p = .39) or OS (HR 0.46 {CI 0.48 – 4.4}, p = .46).
Conclusion
The majority of patients who did not meet Z0011 criteria had no additional nodal burden. Moreover, additional positive nodes on ALND was not independently associated with DRFS or OS on multivariate analysis, meaning it is rarely clinically useful. Further research is warranted to develop tools which predict risk of further disease, potentially sparing many the morbidity of ALND.
2. Published.
https://www.breastsurgeons.org/meeting/2022/docs/2022_Official_Proceedings_ASBrS.pdf
3. The Incidence and Significance of Breast Lesions Identified Incidentally on Non-Dedicated Computed Tomography in a Tertiary Referral Centre
Ryan Donnelly, Markus K Kostka, Shane Keogh, Aisling Fawaz, Jason Mahony, Gerry O'Donoghue
Breast and General Surgery, University Hospital Waterford, Ireland
Introduction
Despite computed tomography (CT) not being the primary screening tool for breast evaluation it does incorporate the whole breast tissue and its increased use in clinical practice is leading to an increased incidence of ‘incidental’ breast lesions.
Aim
Incompletely assessed lesions can result in missed malignancy therefore an understanding of the significance of these CT findings is important for clinical decision making.
Method
A retrospective analysis of breast lesions detected incidentally on CT scans between January 2016 and September 2021 was conducted.Patients with known breast cancer or undergoing CT for staging and surveillance were excluded. Clinical correlation and follow-up investigations, including histopathology, were reviewed from the electronic radiology and pathology reporting system.
Results
Out of 3367 screened CT’s, 257 satisfied the inclusion criteria. Of these, 113 contained concerning incidental breast findings or clinical correlation was advised. 54 of these 113 (48%) patients underwent mammographic screening investigation. Of these 54 cases, 17 (31%) had a ultrasound guided core needle biopsy. Of these 17 biopsied patients, 9 (53%) had malignant lesions. All were Grade 1–3 Ductal cancers. Overall, 13 benign breast abnormalities were detected amongst the 113 (11.5%) (5 fibroadenoma, 4 cysts, 3 unspecific fibrous change, 1 myofibroblastoma).
The overall malignancy rate in all patients with an incidental breast finding on CT was 9 out of 113 (7.9%).
Conclusion
Increased radiological awareness and prompt specialised breast unit follow up is important to improve diagnostic efficacy but the overall incidence of malignant histological findings is very low.
4. Qualitative Study of Therapeutic Mammoplasty as Surgical Treatment for Breast Cancer by One Surgeon at a District Hospital
Tessa Walton, Manvydas Varzgalis
General Surgery, Letterkenny University Hospital, Letterkenny, Ireland
Introduction
Wide local excision followed by radiotherapy is the accepted surgical management of breast cancer, however, patients with large ptotic breasts, large tumours, multifocal or multicentric disease often have poor cosmetic outcomes or require mastectomy. Therapeutic mammoplasty is an option for such patients with the aim to avoid mastectomy and achieve good oncological and cosmetic outcomes.
Aim
To demonstrate that therapeutic mammoplasty is an acceptable and safe alternative to wide local excision in select patients with breast cancer.
Method
Retrospective analysis was performed on patients who underwent therapeutic mammoplasty for breast cancer between 2017–2021. Cases were assessed for cancer subtypes and radiological and histological cancer size. Prospective analysis of wound complications, cosmetic outcome and cancer recurrence was performed. Cosmetic outcomes were assessed using the BREAST-Q questionnaire.
Results
Ten patients underwent therapeutic mammoplasty during the specified time frame. The average radiological cancer size was 51.7 mm (SD 39.1) and the average histological cancer size 50.5 mm (SD 40.1). The average specimen weight was 511 g (SD 287.2). All the patients underwent adjuvant treatment as per breast cancer MDT advice. There were no immediate or delayed surgical complications, with most patients experiencing mild side effects of radiotherapy. One patient had axillary recurrence and is undergoing treatment for it. Good cosmetic outcome was reported by all patients.
Conclusion
Our review demonstrates that therapeutic mammoplasty offers an acceptable and safe alternative to wide local excision as surgical treatment for selected patients. Our data is in keeping with similar studies showing low surgical complications and patient satisfaction.
5. Outcomes of Older Patients with Non-Metastatic Breast Cancer Treated with Primary Hormonal Therapy
SW Koh, M Morrogh, M Corrigan, L Kelly, MJ O'Sullivan, EM Quinn
Breast Surgery, Cork University Hospital, Wilton Manor, Cork, Ireland
Introduction
Women over 70 years of age with oestrogen-receptive positive breast cancer may be less likely to be offered primary surgery, without a formal assessment of their frailty.1
Aim
The aim of this study was to assess outcomes of older patients with non-metastatic breast cancer treated with primary hormonal therapy.
Methods
All patients over the age of 70 diagnosed with oestrogen-receptor positive breast cancer in 2019 at our unit, who were not offered surgery as their primary treatment, were included in the study. Patients with metastatic disease at diagnosis were excluded. Patient charts were reviewed and data collected in relation to patient demographics, disease characteristics, comorbidities, formal frailty assessment, treatment prescribed, disease progression and survival.
Results
A total of 49 patients were included. Complete data is currently available for 20 patients. Patients had a mean of 3.9 documented comorbidities (range 1–5). However, no patient had a formal clinical frailty score or performance status score recorded. Mean follow-up was 29.2 months. In this timeframe, 2 patients (10%) required treatment changes due to disease progression. Fourteen patients (70%) remain alive.
Conclusion
Primary hormonal therapy can provide effective cancer treatment in patients who are too frail or who do not wish for surgery. However, high survival rates and the potential development of treatment resistance suggest formal frailty assessments could help subselect a cohort of older patients for whom surgery could be offered as primary treatment.
6. Published.
https://link.springer.com/article/10.1007/s11845-022-02966-3
7. Published.
https://academic.oup.com/bjsopen/article/6/2/zrac022/6563503
8. Evaluating the Necessity of Routine Sentinel Lymph Node Biopsy in Postmenopausal Patients being Treated for Clinically Node Negative Breast Cancer the Era of RxPONDER
Eoin Kerin 1 , Matthew Davey 1 , Ray McLaughlin 2 , Karl Sweeney 2 , Michael Barry 2 , Carmel Malone 2 , Aoife Lowery 1,2 , Michael Kerin 1,2
1. Surgery, Lambe Institute for Translational Research, University of Galway, Ireland;
2. Surgery, Galway University Hospitals, Galway, Ireland
Introduction
Traditionally, sentinel lymph node biopsy (SLNB) was performed to inform adjuvant chemotherapy (AC) prescription in breast cancer. Following RxPONDER, the OncotypeDX Recurrence Score (RS) now guides adjuvant chemotherapy prescription for all postmenopausal patients with estrogen receptor positive, human epidermal growth factor receptor-2 negative (ER+/HER2-) breast cancer with 0–3 positive lymph nodes (0-3+LN).
Aims
To establish the oncological safety of omitting SLNB in postmenopausal patients with ER+/HER2- breast cancer with clinically negative axillae (cLN-) and to evaluate the primary determinants of AC prescription in these patients.
Methods
A single centre, retrospective cohort study was undertaken. Cox regression and Kaplan Meier analyses were performed. Data analytics was performed using SPSS v26.0.
Results
687 patients were included (mean age: 66.5 years, range: 45–96). The median follow-up was 97.2 months (range: 3.0–181.6). Of the 575 patients undergoing SLNB (83.7%), just 12 patients had positive nodes (SLNB+) (2.1%). Using Cox regression analysis, SLNB+ independently predicted poorer disease-free survival (hazard ratio: 1.000, 95% confidence interval (95% CI): 1.000–1.001, P = 0.029). However, using Kaplan Meier analyses, SLNB+ failed to impact recurrence (P = 0.766) or mortality (P = 0.310). Finally, logistic regression analysis identified RS as the sole independent predictor of AC prescription (OR: 1.171, 95% CI: 1.097–1.250, P < 0.001).
Conclusion
These provisional results suggest omitting SLNB may be safe and justifiable in postmenopausal patients with ER+/HER2-cLN- breast cancer. Following RxPONDER, RS is the most important guide of AC use in those with 0-3+LN and SLNB may be less important than previously perceived. Nevertheless, prospective, randomised clinical trials are required to fully establish the oncological safety of omitting SLNB in this setting.
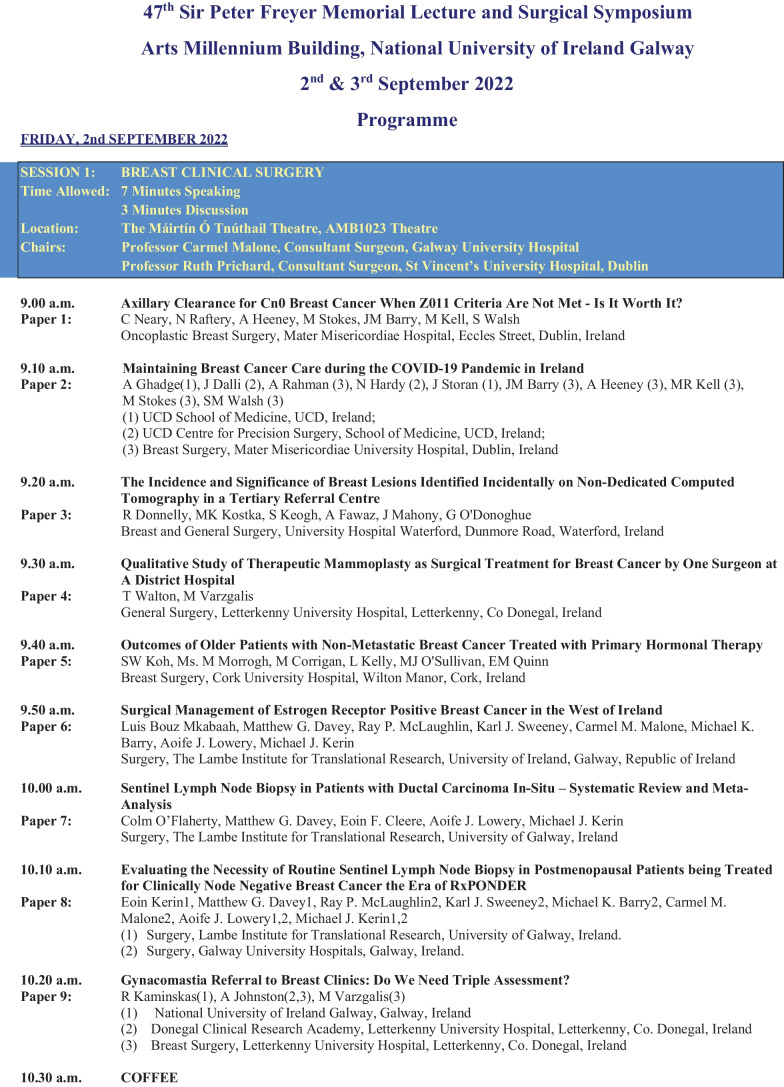
9. Gynacomastia Referral to Breast Clinics: Do We Need Triple Assessment?
R Kaminskas 1 , A Johnston 2,3 , M Varzgalis 3
1. National University of Ireland Galway, University Rd, Galway
2. Donegal Clinical Research Academy, Letterkenny University Hospital, Letterkenny, Co. Donegal, Ireland
3. Breast Surgery, Letterkenny University Hospital, Letterkenny, Co. Donegal, Ireland
Introduction
Male Breast Cancer (MBC) has an incidence of < 1% of breast cancers. Gynecomastia, the most common male benign condition seen in symptomatic breast units (SBUs) does not require all aspects of triple assessment (TA). Investigative processes vary across SBUs.
Aims
To appraise the requirement of TA and assess the value of clinical examination (CE) on male breast patients referred to our SBU.
Methods
An ethically approved study of all males undergoing assessment from 2010 to 2020 was undertaken. Demographics, TA and incidence of malignancy data was collected from Dendrite Clinical Systems Ltd. Clinical, radiological and pathological findings were compared using a standardized SRB grading system to assess diagnostic accuracy.
Results
A total of 20,289 patients, 649 (3.2%) male underwent TA with mean age 49.6 (11–92), SD 21.5. Male referral numbers trended upwards ranging from 59 (2010) to 83 (2020). 400/640 (62.4%) had radiology, 76/400 (19%) had clinical and radiological findings confirmed by biopsy with 5 cancers (0.78%) diagnosed. All clinically benign cases that were biopsied were histologically benign. No statistically significant difference noted between clinical and radiological diagnostic methods (p = 0.317).
Table 1 Sensitivities and specificities for components of TA
| Clinical Examination | Mammogram | Ultrasound | |
|---|---|---|---|
| Sensitivity (95% CI) | 80% (28.36–99.49) | 100% (39.76- 100.00) | 100% (47.82–100.00) |
| Specificity (95% CI) | 97.18% (90.19–99.66) | 95.56% (84.85–99.46) | 96.92% (89.32–99.63) |
% (39.76–100.00) 100% (47.82–100.00)
Conclusion
CE is a reliable diagnostic tool in detecting lumps requiring further investigation by TA. Local guidelines need review. Imaging is warranted with a suspicious lump. Routine imaging for benign clinical findings should be discouraged.
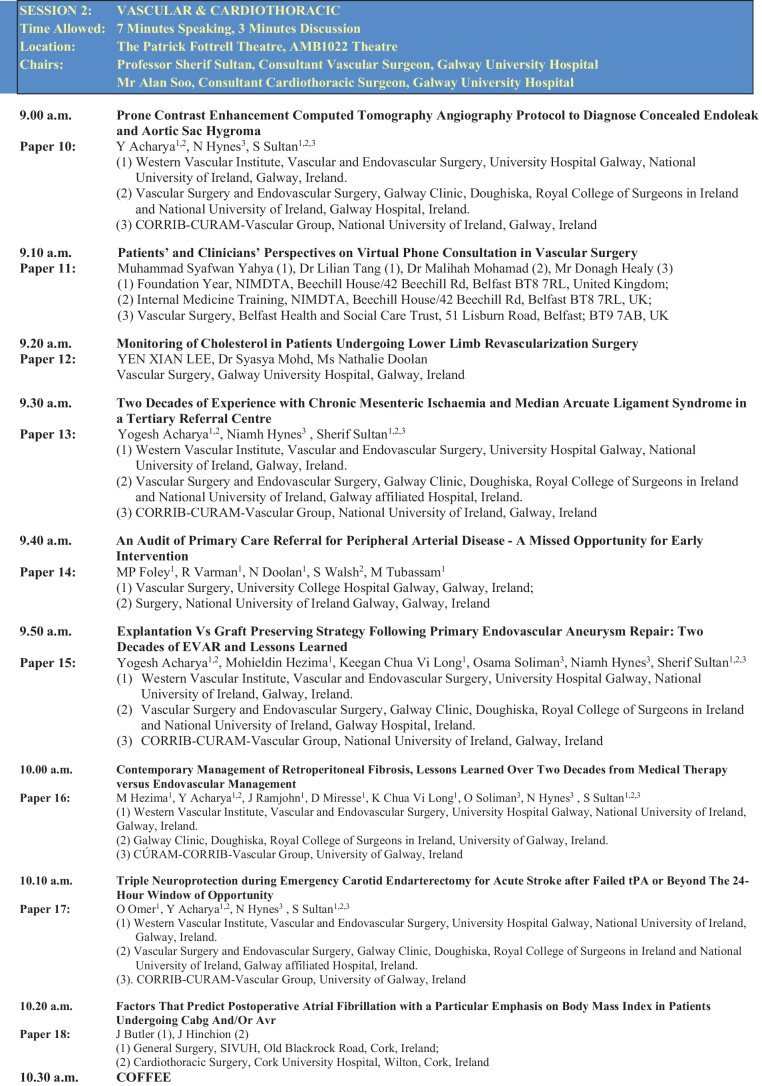
SESSION 2: VASCULAR AND CARDITHORACIC SURGERY
10. Published.
https://www.summit-ctap.com/2022/eposter/eposter_abstract_view.php?code=ABS20211125_0013
11. Patients’ and Clinicians’ Perspectives on Virtual Phone Consultation in Vascular Surgery
Muhammad Syafwan Yahya 1 , Lilian Tang 1 , Malihah Mohamad 2 , Donagh Healy 3
1. Foundation Year, NIMDTA, Beechill House/42 Beechill Rd, Belfast BT8 7RL, United Kingdom;
2. Internal Medicine Training, NIMDTA, Beechill House/42 Beechill Rd, Belfast BT8 7RL, United Kingdom;
3. Vascular Surgery, Belfast Health and Social Care Trust, 51 Lisburn Road, Belfast; United Kingdom
Introduction
We started a virtual phone consultation (VPC) program at the start of the pandemic. A survey were done to evaluate further improvements.
Aim
To evaluate patients’ and clinicians’ perspectives on our VPC and to identify areas for improvement.
Methods
100 patients and 11 clinicians were surveyed between December 2021 and February 2022. We included questions on practical aspects of our VPC and on how it could be improved. Our results were presented as proportions and mean scores from 5-point Likert scales with standard deviation (SD).
Results
The average satisfaction score for patients’ most recent VPC was 4.42/5 (SD 0.90). The main benefits of VPC from patients’ perspectives were lower infection risk, lack of need to travel and increased efficiency. Many patients did not know that face to face (F2F) review could be requested instead of VPC.
Conclusions
Clinicians felt that the benefits of VPC were increased efficiency, lower infection risk and reduced cost. Clinicians felt that patients with normal scan results and patients unable to travel were most suitable for VPC. The main disadvantage of VPC that was identified by clinicians was the inability to do physical examination and the clinicians felt that this might delay diagnoses and treatments. Furthermore, clinicians felt that giving patients a written summary of the VPC would be beneficial.
12. Monitoring of Cholesterol in Patients Undergoing Lower Limb Revascularization Surgery
Yen Xian Lee, Syasya Mohd, Nathalie Doolan
Vascular Surgery, Galway University Hospital Galway, Ireland
Introduction
Hyperlipidaemia is one of the modifiable risk factors for peripheral vascular disease. Clinical practice guidelines for both peripheral and coronary artery disease recommend primary and secondary prevention with a lipid-lowering agent. The results of fasting serum lipid profiles should be considered by both GPs and Vascular Surgeons to ensure patients are benefiting from best medical therapy.
Aim
Not all of our PVD patients will have had their cholesterol levels checked as an inpatient as it requires a fasting sample. This audit is to investigate clinician practice regarding the monitoring of cholesterol levels in patients with peripheral vascular disease who have undergone lower limb revascularization surgery.
Method
A retrospective review of charts were done within the year of 2019. 65 cases included all patients with peripheral vascular disease who had any lower limb revascularization surgery performed in 2019.
Results
Data analysis showed that there was evidence of an inpatient fasting lipid profile obtained between 2018–2020 in 52.3% (n = 34).
Conclusion
Only half of our inpatients undergoing lower limb revascularization surgery in 2019 had fasting lipid profiles checked prior to or after their procedure.
We theorise that there are likely two main obstacles to obtaining lipid profiles in our patient cohort:
1) Fasting bloods are required for lipid profiles, and;
2) Lack of a formal pathway on admission that includes relevant bloodwork.
We have developed a formal pathway to obtain relevant bloodwork on inpatients with PVD. This will be re-audited in 4 months time.
13. Published.
14. An Audit of Primary Care Referral for Peripheral Arterial Disease—A Missed Opportunity for Early Intervention
Megan Power Foley 1 , Riya Varman 1 , Nathalie Doolan 1 , Stewart Walsh 2 , Muhammad Tubassam 1
1. Vascular Surgery, University College Hospital Galway, Ireland,
2. Surgery, University of Galway, Ireland
Introduction:
Symptomatic peripheral arterial disease (PAD), either claudication or chronic limb-threatening ischaemia (CLTI), is a common cause for vascular surgery referral. Best medical therapy (BMT), encompassing anti-platelet therapy, statins, smoking cessation, blood pressure and glycaemic control, is a cornerstone of PAD management. We have noticed these easily-modifiable risk factors are often left unaddressed by GPs at time of referral.
Methods:
A random selection of electronic referrals by GPs to the vascular department for symptomatic PAD between between July 2021-March 2022 were audited prospectively. Referrals were individually reviewed for demographic characteristics, referral indication, medical history, smoking status and current medications. Data was analysed using Microsoft Excel.
Results:
One-hundred-and-sixteen referrals were analysed. The mean age was 69.0 years (range 35–94) and 67% (n = 78) were male. The typical vasculopath comorbidity profile was noted. Fifty-one percent (n = 59) were referred with claudication-type pain and 24% (n = 28) with CLTI, respectively. Seventy-nine percent of referrals (n = 92) included peripheral pulse examination findings. Twenty-eight percent (n = 33) of new referrals were active smokers, while 31% (n = 36) had no smoking status documented. Regarding BMT, only 34.5% (n = 40) and 52% (n = 60) were on anti-platelets and statins, respectively. Overall, only eleven referral letters specifically mentioned discussing risk factor optimisation with patients during the consultation.
Conclusions:
Our first-cycle results demonstrate a significant number of new PAD referrals were not receiving BMT in the community. For our intervention, we need to communicate how optimal PAD management begins in primary care and ensure GPs have sufficient knowledge to tackle these challenging, high-risk patients.
15. Published.
https://www.thieme-connect.de/products/ejournals/abstract/10.1055/s-0042-1750956
16. Published.
https://www.frontiersin.org/articles/10.3389/fsurg.2022.946675/full
17. Published.
https://cslide.ctimeetingtech.com/cirse2021/attendee/confcal_1/show/session/207
18. Factors That Predict Postoperative Atrial Fibrillation with a Particular Emphasis on Body Mass Index in Patients Undergoing Cabg and/or Avr
James Butler 1 , John Hinchion 2
1. General Surgery, St Vincent’s University Hospital, Old Blackrock Road, Cork City, Ireland;
2. Cardiothoracic Surgery, Cork University Hospital, Wilton, Cork City, Ireland
Introduction
Post-operative Atrial Fibrillation (POAF) is a frequent complication of cardiac surgery and associated with significant morbidity and mortality. Identifying predictors that contribute to its occurrence may help to reduce the incidence of this common arrhythmia.
Aims
Our aim is to identify peri-operative variables that contribute to POAF propagation and determine if there is an association between BMI and POAF.
Methods
The data of 683 patients who underwent cardiac surgery in CUH and had no prior history of AFIB were included. Two groups were formed, the POAF Group and Non POAF group. Their demographics and clinical characteristics were analysed to determine what factors contributed to POAF.
Results
The overall incidence of POAF was 19.2%. Results of first Multivariate regression analysis found advancing age (OR 1.088, 95% CI: 1.058–1.118 p = 0.0001), prolonged cross clamp time (OR 1.014, 95% CI: 1.003–1.025 p = 0.012), prolonged stay in days (OR 1.017,95% CI: 1.001–1.033 p = 0.040) and body mass index as a continuous variable (OR 1.057, 95% CI:1.014–1.102) p = 0.037 to be predictors of POAF.
Results of Second multivariate regression analysis found BMI as a categorical value to not be significant, however the other predictors were matching with those found in the first regression model: advancing age (OR 1.088, 95% CI 1.057–1.119 p = < 0.0001), cumulative cross clamp time (OR 1.014, 95% CI 1.003–1.026 p = 0.015) and prolonged stay in days (OR 1.014, 95% CI .998–1.031 p = 0.040).
Conclusion
We found advancing age, prolonged cross clamp time, prolonged hospital stay in days and BMI as a continuous variable to be independent predictors of POAF.
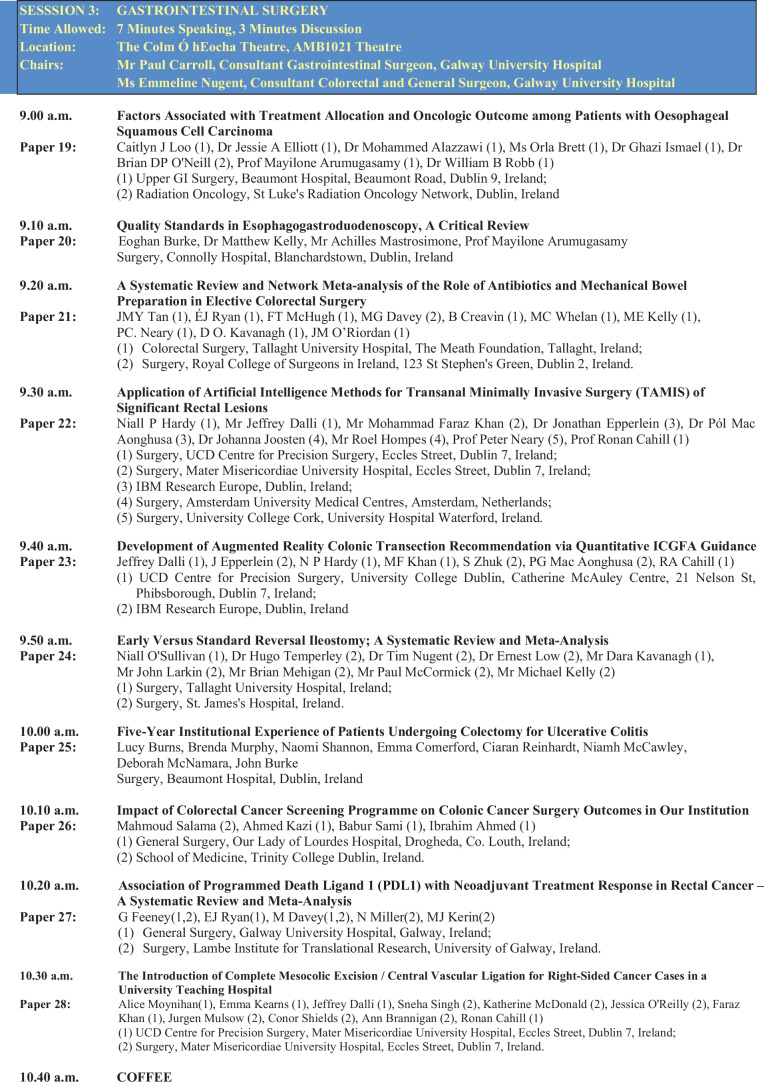
SESSION 3: GASTROINTESTINAL SURGERY
19. Factors Associated With Treatment Allocation and Oncologic Outcome among Patients with Oesophageal Squamous Cell Carcinoma
Caitlyn J Loo 1 , Jessie A Elliott 1 , Mohammed Alazzawi 1 , Orla Brett 1 , Ghazi Ismael 1 , Brian DP O'Neill 2 , Mayilone Arumugasamy 1 , William B Robb 1
1. Upper GI Surgery, Beaumont Hospital, Beaumont Road, Dublin 9, Ireland;
2. Radiation Oncology, St Luke's Radiation Oncology Network, Dublin, Ireland
Introduction:
The optimal strategy for management of localised squamous cell carcinoma (SCC) of middle and lower oesophagus is uncertain.
Aim:
The study aimed to determine current practice and outcomes with respect to curative management of oesophageal SCC.
Methods:
Consecutive patients diagnosed with non-metastatic SCC of the middle and lower oesophagus between January 2013 and December 2018 were studied. Clinicopathologic, treatment, and survival data were collected. Univariable and multivariable logistic and Cox proportional hazards regression analysis were undertaken to analyse factors predictive of treatment allocation and overall survival (OS).
Results:
123 patients were included (middle third, n = 83; locally advanced cT3/T4, n = 91; cN1-3, n = 61). Treatment with curative-intent was possible in 76 (61.8%), of whom 2 underwent endoscopic resection, 7 primary surgery, 24 neoadjuvant chemoradiotherapy and surgery (nCRT-S), and 43 definitive chemoradiation (dCRT). 6 patients treated with dCRT subsequently proceeded to salvage oesophagectomy, 2 of whom have unresectable disease. Younger age (P < 0.001) and localised T stage (P = 0.011) were independently predictive of allocation to curative-intent treatment. Median OS for patients treated with primary surgery was 63.4 months. There was no significant difference in OS among patients treated with dCRT versus nCRT-S on univariable (median OS, not reached versus 44.5 months, P = 0.337) or multivariable analysis (P = 0.159).
Conclusion:
Treatment with nCRT-S resulted in similar outcomes to dCRT and salvage surgery among patients with oesophageal SCC in this series. Further studies should examine the differential impact of treatment approach on health-related quality of life, treatment-associated morbidity, and suitability of surgical resection in older patients.
20. Quality Standards in Oesophagogastroduodenoscopy, A Critical Review
Eoghan Burke, Matthew Kelly, Achilles Mastrosimone, Mayilone Arumugasamy
Connolly Hospital, Blanchardstown, Dublin, Ireland
Introduction
Oesophagogastroduodenoscopy (OGD) remains the gold standard in diagnosing many upper gastrointestinal (UGI) pathologies. In 2017 the British society of gastroenterology (BSG) released a position statement on quality standards in OGD. These standards include guidelines on anatomical landmark photo-documentation, biopsy protocol to diagnose eosinophilic oesophagitis, biopsy protocol for workup of iron-deficiency anaemia and the approach to documentation and biopsy of gastric polyps.
Aim
To assess our units adherence to the guidelines set out by BSG for quality standards in OGD.
Methods
Retrospective review of OGD reports as stored on Endorad from elective non-therapeutic OGDs performed from 19/2/21.
Results
180 consecutive elective, non-therapeutic OGDs were reviewed. The most common indication was reflux (26%). The most common pathological finding was gastritis (32%). 2% of the OGDs had adequate photo-documentation of the recommended anatomical landmarks. The most poorly documented landmark was the gastric body (17%). Correct biopsy protocol for eosinophilic oesophagitis, anaemia workup and polyp evaluation was followed in 38%, 65% and 86% of OGDs respectively. 17% of OGDs were reported as normal yet of these only 3% had adequate objective photodocumentation.
Conclusion
We believe a national audit of the quality standards of OGD should be undertaken with a view to updating the current key performance indicators for OGD.
21. A Systematic Review and Network Meta-analysis of the Role of Antibiotics and Mechanical Bowel Preparation in Elective Colorectal Surgery
Jonavan Ming Yao Tan 1 , Éanna J. Ryan 1 , Fiachra T. McHugh 1 , Matthew G. Davey 2 , Ben Creavin 1 , Maria C. Whelan 1 , Michael E. Kelly 1 , Paul C. Neary 1 , Dara O. Kavanagh 1 , James M. O’Riordan 1
(1) Colorectal Surgery, Tallaght University Hospital, The Meath foundation, Tallaght, Ireland;
(2) Surgery, Royal College of Surgeons in Ireland, 123 St Stephen's Green, Dublin 2, Ireland
Introduction
Use of intravenous(IV) antibiotics at anaesthetic induction is well known to reduce surgical site infection(SSI) rates in colorectal surgery and has long been standard of care. However, the role of mechanical bowel preparation(MBP), enemas(EN), oral antibiotics(OAB), and their effect on SSI, anastomotic leak(AL) rates and other perioperative outcomes remains controversial.
Aim
To determine the optimal preoperative bowel preparation strategy in elective colorectal surgery.
Methods
A systematic review and network meta-analysis(NMA) of randomised controlled trials(RCTs) was performed from inception to December 2021. Primary outcomes included SSI and AL. Secondary outcomes included 30-day mortality, ileus, length of stay, return to theatre, other infections, and preparation adverse effects.
Results
Fifty-six RCTs involving 15,159 patients were included in final analysis– 2941(19.4%) had IV antibiotics, 5255(34.7%) had IV+MBP, 1147(7.57%) had IV+OAB, 4143(27.3%) had IV+OAB+MBP, 262(1.72%) had IV+EN and 1411(9.31%) had OAB+MBP. Using the group receiving solely IV antibiotics as a baseline comparator, NMA demonstrated significant reduction in risk of SSI with IV+OAB(OR:0.45; 95% CI:0.27, 0.75) and IV+OAB+MBP(OR:0.55; 95% CI:0.38, 0.81). OAB+MBP had higher SSI rates compared to IV alone(OR:2.10; 95% CI:1.30, 3.39). AL rates were lower with IV+OAB(OR:0.56;95%CI:0.32,0.97) and IV+OAB+MBP(OR:0.63%;95%CI:0.41,0.98) compared to IV alone. There was minimal difference in outcomes with MBP in the absence of IV and OAB. There were minimal differences in secondary outcomes.
Conclusions
This NMA suggests that intestinal microbiome plays an important role in anastomotic wound healing and provides high-level evidence that combination preoperative IV+OAB reduces SSI and AL rates. Combined OAB and IV antibiotic bowel preparation should therefore represent the standard of care for elective colorectal surgery.
22. Application of Artificial Intelligence Methods for Transanal Minimally Invasive Surgery (TAMIS) of Significant Rectal Lesions
Niall P Hardy 1 , Jeffrey Dalli 1 , Mohammad Faraz Khan 2 , Jonathan Epperlein 3 , Pól Mac Aonghusa 3 , Johanna Joosten 4 , Roel Hompes 4 , Peter Neary 5 , Ronan Cahill 1
1. Surgery, UCD Centre for Precision Surgery, Eccles Street, Dublin 7, Ireland;
2. Surgery, Mater Misericordiae University Hospital, Eccles Street, Dublin 7, Ireland;
3. IBM Research Europe, Dublin, Ireland;
4. Surgery, Amsterdam University Medical Centres, Amsterdam, Netherlands;
5. Surgery, University College Cork, University Hospital Waterford, Ireland
Introduction
Transanal minimally invasive surgery (TAMIS) can cure large benign tumours and earliest stage cancers of the rectum. Despite equipment and training improvements, its application is limited by the current state of the art re patient selection (preoperative imaging and colonoscopic biopsy are frequently inaccurate in lesions > 2 cm). We sought to digitally characterise rectal lesions in patients potentially amenable to local resection as cancer or benign at endoscopy/TAMIS using dynamic fluorescence perfusion detailing with machine learning (ML) assessment to potentially solve this issue.
Methods
Forty consecutive patients with rectal tumours undergoing diagnostic and therapeutic procedures at three university hospitals were imaged transanally for up to 10 continuous minutes following ICG administration (0.25 mg/kg) using a commercially available near infra-red imaging system (Pinpoint, Stryker, NCT04220242). Time-fluorescence profiles from lesion and healthy control visual regions were extracted from each video for algorithmic analysis in comparison to operator and final pathological assessment (benign vs malignant) as well as 2D heatmap representation.
Results
ML characterisation was > 95% accurate when compared to final pathology in this clinical series whereas the initial clinical/radiological impression (benign or malignant) was either uncertain or ultimately incorrect in 14 (35%). Eight (20%) patients with benign/non-diagnostic biopsies at initial lesion sampling were correctly predicted by ML to have invasive cancer. Full 2D lesional representation provided similar characterisation without the need for user-supervision/interaction.
Conclusion
Objective digital perfusion signalling can non-invasively characterise and delineate malignancy in significant rectal polyps and tumours clinically in a manner that is more accurate than conventional standard of care.
Funding Statement
This work was funded through the Disruptive Technologies Innovation Fund (DTIF) as part of a project entitled ‘The Future of Colorectal Cancer Diagnosis and Treatment: Combining Tissue Responsive Probes, AI and Machine Learning to Transform Medical Care’. The DTIF is administered by Enterprise Ireland on behalf of the Department of Enterprise, Trade and Employment.
23. Development of Augmented Reality Colonic Transection Recommendation via Quantitative ICGFA Guidance
Jeffrey Dalli 1 , Jonathan Epperlein 2 , Niall P Hardy 1 , Mohammad Faraz Khan 1 , Sergiy Zhuk 2 , Pol G Mac Aonghusa 2 , Ronan A Cahill 1
1. UCD Centre for Precision Surgery, University College Dublin, Catherine McAuley Centre, 21 Nelson St, Phibsborough, Dublin 7, Ireland;
2. IBM Research Europe, Dublin, Ireland
Introduction
ICGFA (Indocyanine Green Fluorescence Angiography) allows operative colonic perfusion assessment with the goal of diminishing malperfusion-related anastomotic leakage. However, its interpretation has been shown to be inconsistent especially without experience and computational methodology could enable automation of this intraoperative decision.
Aim
We have thus developed computational methods of simple and complex quantitative ICGFA analysis representation via image augmentation applicable to in-surgery deployment.
Method
Within a clinical trial (IRB 1/378/2092) patients undergoing elective colorectal resections received ICG(0.1 mg/kg) following mesentery preparation for ICGFA using a commercially available near-infrared laparoscopic stack (PINPOINT, Stryker). Video recordings were stabilised, and time fluorescence plots generated on a per pixel basis. Computationally generated metadata for the centre of mass, Fmax (peak intensity), Tmax (Time to Fmax) and T1/2(time to half Fmax):Tmax ratio were overlayed on the displayed image via colour gradients, producing an augmented display (heatmap).
Results
Heatmap imagery was obtained for 16 patients (mean age 66.5 years, 13 men, 11 with colorectal cancer) undergoing left (n = 10) and right (n = 6) sided resections with anastomosis being performed in 15 (one with end colostomy). Recording, tracking and per pixel quantification was performed at 30 frames/second. Motion and instrument intrusion compromised image stabilisation while prolonged recordings degraded images.
Conclusion
Full field of view analysis allows the augmentation of surgical imagery chronologically summarising simple (Fmax and Tmax) and complex (T1/2/Tmax and Centre of Mass) quantitative data. Image stabilisation and computational visual augmentation allows data-overlay onto imagery from commercially available systems with the scope of guiding colonic transection.
Trial registry
ClinicalTrials.gov Identifier: NCT04220242
Funding
This research is funded by the DTIF(Disruptive Technologies Innovation Fund), Republic of Ireland and Dr Jeffrey Dalli is a recipient of the TESS scholarship, Malta.
24. Published.
https://link.springer.com/article/10.1007/s10151-022-02629-6
25. Five-Year Institutional Experience of Patients Undergoing Colectomy for Ulcerative Colitis
Lucy Burns, Brenda Murphy , Naomi Shannon, Emma Comerford, Ciaran Reinhardt, Niamh McCawley, Deborah McNamara, John Burke
Surgery, Beaumont Hospital, Dublin, Ireland
Introduction
Despite medical therapies, up to 30% of patients with Ulcerative Colitis (UC) will require a colectomy. We present a five-year institutional experience of colectomies performed.
Methods
Patient demographics were obtained from an electronic patient record system and clinical notes were reviewed. All data were anonymised and analysed using GraphPad Prism v9.2.
Results
From January 2016 to December 2020, 83 colectomies (emergency 48, elective 35) were performed (M = 51, F = 32). Median age of all patients was 33 (17–79) for elective cases and 44 (17–76) for emergencies. Median length of stay was 9 days for elective and 20 days for emergency. 13 patients had an elective panproctocolectomy with 6 IPAAs fashioned immediately and a further 5 as a second stage procedure. 45 patients underwent an emergency subtotal colectomy of which 14 subsequently had a completion proctectomy with 8 IPAAs fashioned as a second stage procedure. 77% of patients undergoing elective surgery had received steroids within 12 weeks of surgery with 51% having received biologics. For emergency resections, this was 93% and 80%, respectively. 60 surgeries (72%) were performed laparoscopically. 30-day morbidity was 19% for emergency cases and 7% for elective. Morbidities included post-operative ileus (n = 3), surgical site infection (n = 6), blood transfusions (n = 2). No patients required a return to theatre on the same admission. There were no mortalities.
Conclusions
Our practice reflects the evolution of surgery for UC and changing trends in modern management, reinforcing that optimally timed operative intervention leads to favourable peri-operative and long-term outcomes.
26. Impact of Colorectal Cancer Screening Programme on Colonic Cancer Surgery Outcomes in our Institution
Mohamed Salama 1 , Wael Shabo 1 , Ahmed Salamna 2
1. General Surgery, Our Lady of Lourdes Hospital, Drogheda, Co. Louth, Ireland;
2. School of Medicine, University of Galway, Galway, Ireland
Introduction
Colorectal Cancer (CRC) cases have significantly increased in Ireland. The CRC screening programme was implemented in our institution in 2013. Despite considerable improvement in CRC management, there is a great variation of outcomes among different hospitals.
Aim
To evaluate the impact of CRC screening programme on patient outcomes after CRC surgery in our institution.
Method
A retrospective study of CRC patients treated at our institution between 2013 and 2018. These were classified into 3 subgroups: 1) Age ≤ 50 years, 2) Age > 50 and < 75 years, 3) Age ≥ 75 years. Data collected: age, gender, location, and staging.
Results
Total number: 342, age range: 30–96y. Group 1: 29, Group 2: 177, Group 3: 136. 4 patients underwent palliative treatment (3 advanced stage, 1 elderly). 29 patients (8.5%) underwent emergency surgery secondary to obstruction or perforation. With respect to tumour stage, 93% of Group 1, 91% of Group 2 and 86% of Group 3 presented with stage 3 or more. The total mortality rate of 25.4% (Group 1: 10.3%, Group 2: 27.1% and Group 3: 26.4%).
Conclusion
In our study, most cases were diagnosed late (Stage 3 and 4). It is probably due to comprehensive investigations in the perioperative period, causing a shift in stage allocation from stages 1 and 2 to stages 3 and 4. The bowel screening programme includes individuals aged 60 to 69 years. This narrow age range means that the potential benefits of screening are unlikely to be achieved in the short term.
27. Association of Programmed Death Ligand 1 (PDL1) with Neoadjuvant Treatment Response in Rectal Cancer- A Systematic Review and Meta-Analysis
G Feeney 1,2 , EJ Ryan 1 , M Davey 1,2 , N Miller 2 , M Joyce 1 , M Kerin 2
1. General Surgery, Galway University Hospital, Galway, Ireland
2. Surgery, Lambe Institute for Translational Research, University of Galway, Galway, Ireland
Introduction
PDL-1 plays an integral role in the immune systems response to neoplastic cells. Increased PD-1 has been recognised to be associated with reduced survival outcomes. Conversely, tumours with elevated PD-1 have been more sensitive to neoadjuvant therapy.
Aim
To examine potential association between elevated PDL1 expression in tumour tissue and incidence of complete pathological response to neoadjuvant therapy in locally advanced rectal cancer.
Methods
Systematic review was performed in accordance with PRISMA guidelines. Primary endpoint was defined as pathological complete response (pCR). Secondary endpoints included extramural venous invasion (EMVI), nodal metastases and local recurrence. Statistical analysis was performed with RevMan software.
Results
Overall, 7 studies involving 861 patients were included for analysis. PDL-1 was quantified via immunohistochemistry in all cases with elevated expression documented in 298 (34.6%) patients. pCR was recorded in 114 (13.2%) cases. Of these, 46.5% demonstrated elevated PDL-1 (OR = 0.79, CI 0.5–1.27, p = 0.34). Of the secondary endpoints, reduced PDL-1 expression was associated with EMVI positivity (OR 2.6, CI 1.26–5.37, p = 0.009) and Overall Survival (OR1.79, CI 1.03–3.11, p = 0.04). No significant associations were found between PDL-1 expression and Nodal Metastases, Advanced Stage or Local Recurrence.
Conclusion
Our study has demonstrated an association between increased PDL-1 expression and measures of response to NA therapy in locally advanced rectal cancer. This was not found to be statistically significant. We have also outlined that reduced PDL-1 expression is associated with EMVI positivity and improved OS rates in our study. These findings are in keeping with previously published literature on PDL-1.
28. The Introduction of Complete Mesocolic Excision / Central Vascular Ligation for Right-Sided Cancer Cases in a University Teaching Hospital
Emma Kearns (1), Sneha Singh (2), Katherine McDonald (2), Jessica O'Reilly (2), Faraz Khan (1), Jurgen Mulsow (2), Conor Shields (2), Ann Brannigan (2), Ronan Cahill (1)
1. UCD Centre for Precision Surgery, Mater Misericordiae University Hospital, Eccles Street, Dublin 7, Ireland;
2. Surgery, Mater Misericordiae University Hospital, Eccles Street, Dublin 7, Ireland
Introduction
Complete mesocolic excision with central vascular ligation for right colon cancer remains controversial despite evidence of superior oncological outcomes compared with standard resection due to concerns re safety and technical complexity.
Aims
To compare perioperative outcomes between CME/CVL cases and a control group.
Methods
Consecutive laparoscopic right hemicolectomy cases (December 2019-January 2022) where CME/CVL was performed with the use of personalized 3-D reconstructive images were audited against a control group of laparoscopic right hemicolectomies via standard resection in terms of perioperative outcomes.
Results
Twenty-two patients were included in the CME/CVL group and twenty in the control group. There were no significant differences in terms of age (71.55 ± 11 vs 70.1 ± 10.4, p = 0.33), gender (50% versus 45% males, p = 0.38), cancer stage (T1(n = 1):T2(n = 6):T3(n = 6):T4(n = 5) versus T1(n = 3):T2(n = 2):T3(n = 9):T4(n = 2), p = 0.07) between CME/CVL group and control group, respectively. There were no intraoperative complications in the CME/CVL group and one conversion to open for bowel ischaemia in the control group. There was no significant increase in early post operative morbidity (18% versus 30%, p = 0.19), length of hospital stay (8 days ± 3 versus 11 days ± 13, p = 0.18), 30-day readmission rates (5% versus 9%, p = 0.3), between the CME/CVL group and control group, respectively, while 30-day reoperation rates were lower in the CME/CVL group (0% versus 15% (n = 3), p = 0.04). Intraoperative time was found to be significantly longer in the CME/CVL group (208 ± 42.9 min versus 152 ± 66.9, p = 0.002), however, operative times for CME/CVL decreased significantly over the study timeframe.
Conclusion
Implementation of CME/CVL for right-sided colorectal cancer was safe in our institution without an increased rate of intraoperative or postoperative complication.
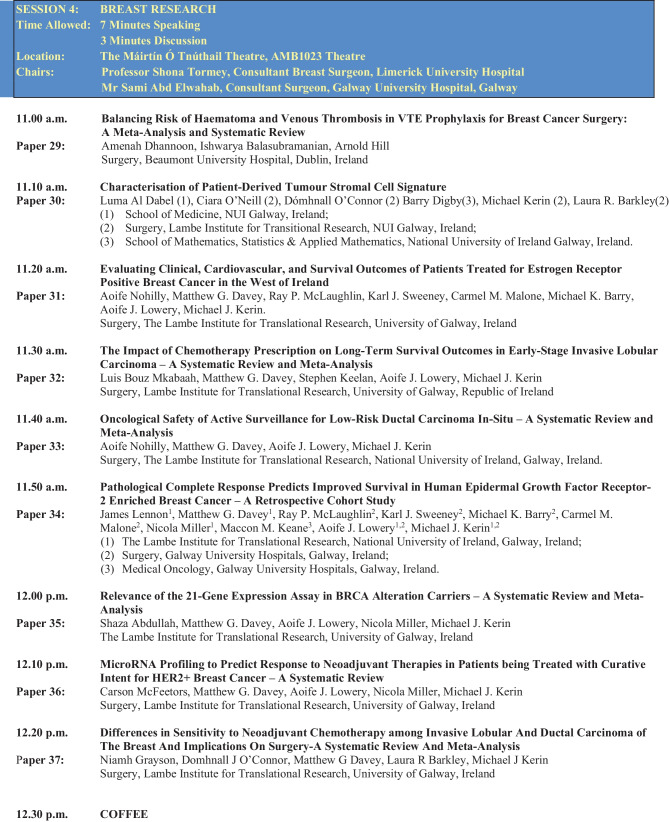
SESSION 4: BREAST RESEARCH
29. Balancing Risk of Haematoma and Venous Thrombosis in VTE Prophylaxis for Breast Cancer Surgery: A Meta-Analysis and Systematic Review
Amenah Dhannoon, Ishwarya Balasubramanian, Arnold Hill
Surgery, Beaumont University Hospital, Ireland
Introduction
Venous thromboembolism (VTE) is a largely preventable cause of morbidity and mortality in post-operative patients. Guidelines for VTE prophylaxis in breast cancer surgery are not well-established.
Methods
A comprehensive search was undertaken of all studies that described the role of VTE prophylaxis in breast cancer surgery. Comparative studies that reported on postoperative outcomes between patients who received VTE prophylaxis (prophylaxis) and those who did not (no prophylaxis) were included in the analysis. A meta-analysis using random-effects model was used to analyze key outcomes, with data presented as odds ratio (OR).
Results
A total of 2470 patients from 6 studies were included in this study. Of these patient, 60.9% (n: 1504) received prophylaxis. The haematoma rate in this study is 0.05% (n: 133). The incidence of haematoma was significantly associated with the use of prophylaxis (6.85% versus 3.11%, p: 0.001). Surgical intervention for haematomas was also significantly associated in this group (3.15% versus 0.83%, p: 0.004). However there was no difference in VTE events between both groups (0.26% versus 0.36%, p: 0.88).
Conclusion
The use of VTE prophylaxis in breast cancer surgery is associated with increased haematomas without any benefit in preventing venous thromboembolic events. Further studies that examine the use of risk assessment tools for VTE prophylaxis in high risk patients may be beneficial.
30. Characterisation of Patient-Derived Tumour Stromal Cell Signature
Luma AlDabel 1 , Ciara O’Neill 2 , Dómhnall O’Conno 2 Barry Digby 3 , Michael J Kerin 2 , Laura R. Barkley 2
1. School of Medicine, University of Galway, Ireland;
2. Surgery, Lambe Institute for Transitional Research, University of Galway, Ireland;
3. School of Mathematics, Statistics & Applied Mathematics, University of Galway, Ireland
Introduction
Tumour stromal cells (TSCs) are an important population of cells within the tumour microenvironment (TME) that play a major role in tumour formation, immunosuppression, and chemo-resistance. Stromal cells are also present at metastatic lesions (MET) making the site receptive to tumour cell engraftment and growth. Identifying and targeting these TSCs may impact breast cancer therapeutics and improve prognosis.
Aim
To evaluate a predertemined TSC gene signature in a breast cancer patient cohort to differentiate gene expression between TSCs, metastatic lesions, and tumour associated normal (TAN) stromal cells isolated from the same patient.
Methods
TSCs, TANs and MET stromal cells were isolated from breast cancer patients (n = 5) at Galway University Hospital. Cells were cultured and grown in incubation, then counted. Soluble and insoluble protein samples were prepared to carry out immunoblot (Western) analysis. RNA samples were isolated to perform RT-qPCR and validate TSC gene signature.
Results
SLC7A2, GPR116, PCDH10, WT-1 and GPR37 gene expression were upregulated in TSCs compared to TANs in 2 out of 3 of the patients. These genes were also upregulated in stromal cells isolated from a metastatic lesion compared to normal stromal cells.
Conclusion
These provisional results illustrated the importance of this gene signature in identifying TSCs within the TME, acting as potential therapeutic targets as well as predictors of metastasis. Further preclinical research is required to further establish the role of this genetic signature in breast cancer.
This work was supported by a HRB summer scholarship (SS-2021–004) and NBCRI.
31. Evaluating Clinical, Cardiovascular, and Survival Outcomes of Patients Treated for Estrogen Receptor Positive Breast Cancer in the West of Ireland
Aoife Nohilly, Matthew Davey, Ray McLaughlin, Karl Sweeney, Carmel Malone, Michael Barry, Aoife Lowery, Michael Kerin
Surgery, The Lambe Institute for Translational Research, University of Galway, Ireland
Introduction
Estrogen receptor positive (ER+) breast cancer makes up 70–80% of breast cancer diagnoses. Assessment of clinicopathological data, cardiovascular disease (CVD), and survival outcomes within this subgroup are important to improve patient prognosis.
Aims
To establish the oncological, cardiovascular, and survival outcomes of patients treated with ER+ breast cancer in a large European tertiary referral centre.
Methods
A single centre, retrospective cohort study was undertaken. All patients with ER+ breast cancer patients diagnosed between January 2005 and December 2015 were included. Descriptive data was performed to inform patient outcomes. Analysis will be performed using SPSS v26.
Results
2660 patients were included with median age of 59.6 ± 13.3 years (21–99). At median follow-up of 97.2 months (3.0–181.2), 12.4% of patients suffered a recurrence (450/2660): 2.1% of patients suffered a locoregional recurrence (56/2660) and 10.3% patients suffered distant recurrence (394/2660). The median time to relapse for patients suffering locoregional recurrence was 53.1 months versus 48.1 months for those suffering distant recurrence. Of those suffering disease recurrence or death, bone was the most common initial site of distant recurrence (18.7%, 74/394), followed by liver (18.1%, 71/394) followed by lung recurrences (5.3%, 21/394) and then brain recurrences (5.1%, 20/394). In total, 0.6% patients suffered CVD related-death (16/2,660) with a mean time to CVD-related death of 59.6 months (16.3 – 132.2 months).
Conclusion
Oncological and survival outcomes are favourable in ER+ breast cancer. Further evaluation of CVD-related death within cancer patients is required.
32. The Impact of Chemotherapy Prescription on Long-Term Survival Outcomes in Early-Stage Invasive Lobular Carcinoma – A Systematic Review and Meta-Analysis
Luis Bouz Mkabaah, Matthew Davey, Stephen Keelan, Aoife Lowery, Michael Kerin
Surgery, Lambe Institute for Translational Research, University of Galway, Ireland
Introduction:
Invasive lobular carcinoma (ILCs) are typically endocrine responsive breast cancers which respond poorly to chemotherapy. The long-term survival advantage of prescribing chemotherapy in such cases remains unclear.
Aims:
To perform a systematic review and meta-analysis assessing the impact of prescribing chemotherapy in such patients on long-term disease-free (DFS) and overall (OS) survival outcomes.
Methods:
A systematic review and meta-analysis was performed in accordance with the PRISMA guidelines. 10-year DFS and OS were pooled as odds ratios (ORs) with 95% confidence intervals (CI) using the Mantel–Haenszel method. Time-to-effect modelling was performed using the generic inverse variance method.
Results:
Overall, 9 studies including 28,218 patients were included. The mean follow-up was 74 months (range: 0 – 150 months) and mean age was 60 years (range: 22 – 90 years). Of these, 34.7% received chemotherapy (9,797/28,218) and 66.3% did not receive chemotherapy (18,421/28,218). Chemotherapy prescription failed to improve 10-year DFS (OR: 0.89, 95% CI: 0.65 – 1.23) and OS (OR: 0.92, 95% CI: 0.72 – 1.18). When using time-to-effect modelling, chemotherapy prescription failed to improve DFS (hazard ratio (HR): 1.01, 95% CI: 0.78 – 1.31) and OS (HR: 1.07, 95% CI: 0.89 – 1.27, I2 = 67%).
Conclusion:
This meta-analysis illustrates no long-term survival advantage associated with chemotherapy prescription in the setting of early-stage ILC. In the absence of well-designed, prospective clinical trials evaluating the impact of chemotherapy on long-term outcomes in ILC, these results should be considered by the multidisciplinary team when deciding on the value of systemic chemotherapy prescription in ILC.
33. Oncological Safety of Active Surveillance for Low-Risk Ductal Carcinoma In-Situ – A Systematic Review and Meta-Analysis
Aoife Nohilly, Matthew G. Davey, Aoife J. Lowery, Michael J. Kerin
Surgery, The Lambe Institute for Translational Research, University of Galway, Ireland
Introduction
Current standard of care for patients diagnosed with ‘low-risk’ ductal carcinoma in-situ (DCIS) involves surgical resection. Ongoing phase III clinical trials are hoping to establish the oncological safety of active surveillance (AS) in managing ‘low-risk’ DCIS.
Aims
To evaluate the oncological safety of AS versus surgery for ‘low-risk’ DCIS.
Methods
A systematic review was performed in accordance with PRISMA guidelines. Survival outcomes were expressed as dichotomous variables and reported as odds ratios (OR) with 95% confidence intervals (95%CI) using the Mantel–Haenszel method.
Results
4 studies including 9,626 patients were included, 3.9% of which were managed using AS (374/9,626) and 96.1% with surgery (9,252/9,626). The mean age of included patients was 50.3 years (range: 30–99 years) and mean follow-up was 6.1 years. Invasive cancer detection after surgery and AS were similar (OR: 0.93, 95% CI: 0.41–2.11, P = 0.860, heterogeneity (I2) = 0%). At 5-years, BCSS (surgery - 99.5% vs. AS - 98.7%, P = 0.116) and OS (surgery - 95.8% vs. AS - 95.7%, P = 0.876) were similar for both groups. At 10-years, BCSS (surgery - 98.7% vs. AS - 98.6%, P = 0.789) and OS (surgery - 87.9% vs. AS - 90.9%, P = 0.183) were similar for both groups. Overall, 10-year OS outcomes were similar for both management strategies (OR:0.32, 95% CI: 0.02–6.42, P = 0.460, I2 = 69%).
Conclusion
This study outlines the provisional oncological safety of AS for cases of ‘low-risk’ DCIS. While survival outcomes were comparable for both management strategies, ratification of these results in the ongoing phase III clinical trials is still required prior to changes to current management strategies.
34. Published.
https://www.sciencedirect.com/science/article/pii/S0960977621003982?via%3Dihub
35. Published.
https://doaj.org/article/b593074ff6694140a3278072c11969e5
36. Published.
https://journals.sagepub.com/doi/10.1177/11782234221086684
37. Published.
https://www.thebreastonline.com/article/S0960-9776(21)00999-1
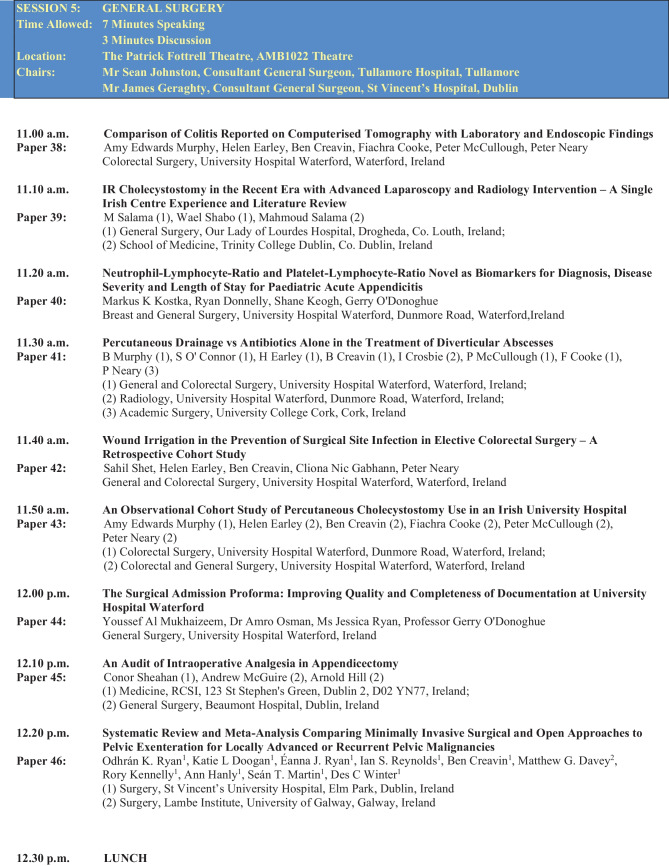
SESSION 5: GENERAL SURGERY
38. Comparison of Colitis Reported on Computerised Tomography with Laboratory and Endoscopic Findings
Amy Edwards Murphy, Helen Earley, Ben Creavin, Fiachra Cooke, Peter McCullough, Peter Neary
Colorectal Surgery, University Hospital Waterford, Waterford, Ireland
Introduction
The aetiology of colitis is diagnosed using clinical, laboratory, colonoscopy and biopsy findings. A cohort of patients have incidental findings suggestive of colitis on computerised tomography (CT), without clinical suspicion.
Aim
The aim of the study was to stratify appropriate investigations for these patients to determine aetiology.
Methods
A search of all abdominal imaging performed from 01/08/2017–31/12/2020 with an incidental CT finding of colitis or features suggestive of colitis was performed. Exclusion criteria included prior known diagnosis of colitis or inflammatory bowel disease.
Results
201 patients were eligible for inclusion. Mean age was 60 years was years (16–94). 9.5% of reports were suggestive of IBD, typhlitis, pancolitis and enterocolitis (n = 11, n = 2, n = 4, n = 2). The remainder reported a specific location of colitis but no suggested aetiology. Stool cultures for clostridium difficile were performed in 57% (n = 114). Of those screened, 7.8% (n = 9) were positive. Molecular Enteric Screening was performed in 56% in whom 8% were positive. 40% of the cohort proceeded to endoscopy, of whom 46.9% had positive relevant findings. 14% of scopes were macroscopically and microscopically normal (n = 12).
Conclusion
As the number of CTs performed increases, it is necessary to rationalise use of further investigations for incidental findings of colitis. Stools cultures proved to be a high yield investigation and should be performed as a first line investigation for all incidental findings suggestive of colitis. Access to endoscopy is a limited resource and should be reserved for those in whom no other cause for colitis is found.
39. IR Cholecystostomy intThe Recent Era with Advanced Laparoscopy and Radiology Intervention – A Single Irish Centre Experience and Literature Review
Mohamed Salama 1 , Wael Shabo 1 , Mahmoud Salama 2
1. General Surgery, Our Lady of Lourdes Hospital, Drogheda, Co. Louth, Ireland;
2. School of Medicine, Trinity College Dublin, Co. Dublin, Ireland
Introduction
Laparoscopic cholecystectomy is the gold standard treatment for acute cholecystitis. The role of percutaneous cholecystostomy (PC) as an alternative treatment in high surgical risk patients remains debatable.
Aims
-To evaluate the role of PC in the management of acute cholecystitis in high surgical risk patients not responding to conservative treatment.
-To establish how PCs are inserted and managed in our department.
Methods
All patients that underwent PC in our unit between 2010 and 2021 were retrospectively reviewed. Data was collected from HIPE, NIMIS and Medical charts.
Results
During this period, 6026 were admitted to our hospital with cholecystitis. 2414 of them had cholecystectomy and 49 underwent PC (Transhepatic: 15, Transperitoneal: 34).
PC indications: Cholecystitis in unfit patients: 36, GB Perforation: 8, Empyema: 5. Out of PC group, 19 had interval laparoscopic cholecystectomy. PC complications: 15 (7 dislodged tubes, 2 liver abscesses, 2 minimal bleeding, 2 pneumonias and 2 sub hepatic collections).
Average time between PC and laparoscopic cholecystectomy: 154.7 days and the average time the drain stayed was 78.4 days. We had 5 mortalities post-PC due to old age and multiple comorbidities. No mortality was directly related to PC complication.
Conclusions
Laparoscopic cholecystectomy is the gold standard treatment for acute cholecystitis.
PC is a feasible and safe intervention for critically ill and elderly patients. Some patients who are too ill to receive interval cholecystectomy can only live with gallstones while others who recover from acute phase can undergo interval cholecystectomy. There is no standardised strategy for PC catheter management.
40. Neutrophil–Lymphocyte-Ratio and Platelet-Lymphocyte-Ratio Novel as Biomarkers for Diagnosis, Disease Severity and Length of Stay for Paediatric Acute Appendicitis
Markus K Kostka, Ryan Donnelly, Shane Keogh, Gerry O'Donoghue
Breast and General Surgery, University Hospital Waterford, Waterford, Ireland
Introduction
Paediatric acute appendicitis is one of the most common surgical presentations to emergency departments (ED) worldwide. Timely diagnosis and appendectomy prevents complications, improves outcomes and reduces length of hospital stay (LOS). Despite well known signs and symptoms, and assessing the risk of complicated appendicitis (CA) vs. uncomplicated appendicitis (UA) is challenging.
Aim
Biochemical ratios such a neutrophil lymphocyte ratio (NLR) and platelet lymphocyte ratio (PLR) may have utility for the diagnosis of acute appendicitis and assessing disease activity.
Method
A retrospective study of paediatric patients who underwent a laparoscopic appendectomy, between 2018–2021 was preformed. NLR, PLR, C-reactive protein (CRP), WCC, LOS and histology where examined and diagnostic accuracy of each biomarker was assessed.
Results
A total of 329 patients with a mean age of 12.2 years were identified. 69.9% had a histological diagnosis of AA, of these 77.4% UA and 22.6% CA. 31.1% had a normal appendix. The mean NLR value (9,42) was higher in the AA group compared to normal (4.03). Within the AA group the NLR was higher in the CA compared to UA (11.8 vs. 6.62). LOS was higher in the CA group (4.79 vs. 2.17 days). NLR and CRP are correlated with LOS. NLR had the greatest accuracy of the biomarker ratios in predicting CA.
Conclusion
NLR levels on admission predicted the presence of CA and a longer LOS. NLR is a useful adjunct in stratifying paediatric patients with AA. PLR did not identify AA within this paediatric population.
41. Percutaneous Drainage vs Antibiotics Alone in the Treatment of Diverticular Abscesses
Brian Murphy 1 , Stephanie O’ Connor 1 , Helen Earley 1 , Ben Creavin 1 , Ian Crosbie 2 , Peter McCullough 1 , Fiachra Cooke 1 , Peter Neary 3
1. General and Colorectal Surgery, University Hospital Waterford, Waterford, Ireland;
2. Radiology, University Hospital Waterford, Waterford, Ireland;
3. Academic Surgery, University College Cork, Cork, Ireland
Introduction
Diverticular abscesses account for a significant proportion of emergency surgical presentations. Recently, placement of image-guided guided percutaneous drains (PD) has an increasing role in the management these patients. NICE guidelines suggest that abscesses above 4 cm should be considered for PD.
Aim
To quantify the use of PD in the management of diverticular abscess at an Irish University Hospital.
To compare the outcomes of those treated with image-guided percutaneous drainage and antibiotics (PD Group) to those who had antibiotics alone (AA Group),
Method
A retrospective observational study of patients treated with AA or PD or over a ten-year period from 2011 to 2020 was carried out. Data were obtained from NIMIS imaging and patient records. Inclusion criteria included: Acute diverticulitis diagnosed on CT, with associated measurable abscess or collection – Modified Hinchey Stage 1b or 2. Exclusion criteria included: Post-operative collections, malignancy, or fistula.
Results
67 met the criteria, 7 of these underwent PD. Mean abscess size in the PD group was 9 cm compared to 4.6 cm in the AA group. When groups were size-matched, length of stay was 15 days in the PD group and 25 days in the size-matched AA group. Failure of initial management was 50% in the AA group vs 14% in the PD group. 28% had future emergency or elective surgery in the PD group vs 25% in the AA group.
Conclusion
At this institution PD use is limited and reserved for larger abscesses, highlighting potential for increased use of PD in these patients.
42. Wound Irrigation in the Prevention of Surgical Site Infection in Elective Colorectal Surgery – A Retrospective Cohort Study
Sahil Shet, Helen Earley, Ben Creavin, Cliona Nic Gabhann, Peter Neary
General and Colorectal Surgery, University Hospital Waterford, Waterford, Ireland
Introduction
Surgical site infection (SSI) in colorectal surgery is associated with significant cost and increased length of hospital stay. Recently, there has been interest in the use of pulsed-lavage to reduce the risk of SSI in wounds. In orthopaedic surgery, pulsed-lavage and has been shown to reduce concentration of debris in the surgical field, and reduce bacterial load. However, it’s effectiveness in colorectal surgery has been poorly documented.
Aim
To investigate the incidence of SSI within 30 days of elective colorectal surgery in patients who underwent wound irrigation with pulse lavage vs standard closure.
Methods
A retrospective study was conducted at a University Hospital over a two-year period between January 2020 and December 2021. All patients who underwent elective colorectal surgery were included. Standard closure was defined as PDS and clips to the skin. The intervention group underwent pulse lavage using and closure with PDS and 2-0 vicryl and 4-0 monocryl.
Results
222 patients were analysed. 39 SSIs were reported (17.6%). 76 patients underwent pulse-lavage while 146 underwent standard closure. Infection rates in the pulse-lavage group were lower at 13% compared to 20% in the standard closure group, however on statistical analysis using the Chi-sqaure test, the difference in infection rates did not reach significance (P = 0.213).
Conclusion
These data demonstrated a reduction in the incidence of SSI in patients who underwent pulse-lavage. Although it did not reach statistical significance, it warrants further investigation in the setting of colorectal surgery. Observed infection rates were in keeping with the literature.
43. An Observational Cohort Study of Percutaneous Cholecystostomy Use in an Irish University Hospital
Amy Edwards Murphy 1 , Helen Earley 2 , Ben Creavin 2 , Fiachra Cooke 2 , Peter McCullough 2 , Peter Neary 2
1. Colorectal Surgery, University Hospital Waterford, Waterford, Ireland;
2. Colorectal and General Surgery, University Hospital Waterford, Waterford, Ireland
Introduction:
Cholecystostomy tube (CCT) insertion is an accepted treatment for cholecystitis where cholecystectomy is not immediately appropriate. It is an adjunct to antimicrobial therapy in achieving source control of sepsis, particularly in comorbid patients. However, concern exists that cholecystostomy use may result in a more complex operative course at subsequent cholecystectomy.
Aim:
1. To evaluate trends in the current use of cholecystostomy 2. Determine outcomes including length of stay (LOS), mortality, subsequent definitive management or need for hepatobiliary specialist intervention.
Methods:
A retrospective, observational cohort study of all percutaneous CCT insertions at a University Hospital was conducted between January 2021 and January 2022.
Results:
12 patients underwent CCT insertion during the study period. All were transhepatic cholecystostomy drains. The mean age was 64 years (33–88), 58% male. All patients had cross-sectional imaging. 33% had no comorbidities. 50% had cardiovascular comorbidities, hypertension, atrial fibrillation, ischaemic heart disease, congestive cardiac failure. The average length of stay was 15 days. 3 patients (25%) required ICU admission. One patient died following prolonged ICU admission. 25% had the cholecystostomy removed as an outpatient and elected for no further intervention given comorbidities and age. 25% proceeded to elective laparoscopic cholecystectomy in the index hospital within 3 months of CCT insertion. 41% were referred to a hepatobiliary service for definitive management.
Conclusions:
These data support a role for CCT as a useful adjunct in management of cholecystitis, particularly in high-risk surgical candidates. This patient cohort are high risk for ICU admission or requirement for hepatobiliary opinion.
44. The Surgical Admission Proforma: Improving Quality and Completeness of Documentation at University Hospital Waterford
Youssef Al Mukhaizeem, Amro Osman, Jessica Ryan, Gerry O’Donoghue
General Surgery, University Hospital Waterford, Blackrock, Dublin, Ireland
Introduction
Accurate and complete documentation is essential and frequently referred to during handover of care. The current outdated proforma used to admit the acute general surgical take being four pages in length, with 168 different data points was in need of change. Due to the cubersome nature of documentation, key patient details were often omitted.
Aim
Introduction of an updated and simplified surgical admission proforma with the aim of improving standard of documentation for patients admitted under the acute general surgical service at University Hospital Waterford.
Method
Admission proformas for patitents admitted via the emergency department were analysed prospectively over a two-week period in April 2021 and in December 2021 following the introduction of the new proforma. Data were collected for 32 criteria taken from the Royal College of Surgeons of England guidelines for Clinicians on Medical Records and Notes (1994).
Results
A total of 47 admission proformas were analysed during the first audit cycle and 56 in the second cyle. An improvement of a total of 27 out of 32 criteria were observed following the introduction of the new proforma. Twenty criteria had more than or equal to 75% completeness in the new proforma versus 6 in the old proforma. The greatest improvement was documentation of grade of clerking doctor (96.4% vs 4.3% P < 0.001) and time seen by doctor (94.6% vs 4.3% P < 0.001).
Conclusion
This audit had demonstrated that significant improvements in documentation can be achieved through simple interventions. The updated proforma has ensured quality of our documentation.
45. An Audit of Intraoperative Analgesia in Appendicectomy
Conor Sheahan 1 , Andrew McGuire 2 , Arnold Hill 2
1. Medicine, RCSI, 123 St Stephen's Green, Dublin 2, Ireland;
2. General Surgery, Beaumont Hospital, Beaumont, Dublin, Ireland
Introduction
Appendicitis is the most common cause of the acute abdomen and emergency surgery. A hospital wide randomised controlled trial to compare Laparoscopic Transversus Abdominis Plane Block (LTAP Block) for appendicectomy versus standard treatment to standard port sites (control group) is being carried out later this year. Prior to commencement of LTAP block trial an audit of the current analgesic practices used in appendicectomy in the hospital was carried out.
Aim
Determine types of analgesia given intraoperatively and postoperatively during appendicectomy.
Determine if there is variation in the analgesia administered compared to a protocol developed for LTAP block study.
Methods
Clinical audit including patients who underwent appendicectomy for the management of acute appendicitis. Patients were identified using a combination of operating theatre lists and theatre log books.
Results
29 patients (14 male 15 female) were identified. Median age of both groups was older than described in the literature. Compliance with Paracetamol intraoperative protocol was 68.9% and 100% post-operatively. Ketorolac had the poorest compliance of the intraoperative regime with 0% compliance over collection period. Compliance with Ibuprofen was 3.4% of patients receiving as per the analgesic protocol. Poor compliance intraoperative Oxycodone with only 34.5% of patients receiving the drug per the protocol. In the post-operative period 27.6% of patients. In the post-operative period 48.3% of patients were prescribed over the protocol of Oxycodone.
Conclusions
There is under prescribing of NSAID's and overprescribing of opioids. Highlights the need to make the LTAP block protocol known prior to the study commencing.
46. Systematic Review and Meta-Analysis Comparing Minimally Invasive Surgical and Open Approaches to Pelvic Exenteration for Locally Advanced or Recurrent Pelvic Malignancies
Odhrán Ryan 1 , Katie Doogan 1 , Éanna Ryan 1 , Ian Reynolds 1 , Ben Creavin 1 , Matthew Davey 2 , Rory Kennelly 1 , Ann Hanly 1 , Seán Martin 1 , Des Winter 1
1. Surgery, St Vincent’s University Hospital, Elm Park, Dublin, Ireland
2. Surgery, Lambe Institute for Translational Research, University of Galway, Ireland
Introduction
Pelvic exenteration is a complex multivisceral surgical procedure that poses significant technical challenges. Developments in minimally invasive surgical (MIS) approaches and enhanced peri-operative care have facilitated improved long term outcomes, however, the optimum approach to pelvic exenteration remains controversial.
Aim
To compare MIS approaches versus the open approach for pelvic exenteration for locally advanced or recurrent pelvic malignancies.
Methods
A systematic literature search was conducted in accordance with PRISMA guidelines to identify studies comparing MIS (robotic or laparoscopic) approaches for pelvic exenteration versus the open approach, and a meta-analysis was conducted.
Results
10 studies were identified for inclusion. This included 1865 patients, of whom 204 (11%) underwent MIS pelvic exenteration approaches. The open approach showed increased lymph node yield (Weighted Mean Difference [WMD] 3.69, 95% Confidence Interval [95% CI] 1.91, 5.48, p,0.0001), however this did not impact the quality of R0 resections. The MIS group had a trend towards improved survival and recurrence outcomes, although, this did not reach statistical significance. MIS was associated with prolonged operating times (WMD 106.28, 95% CI 83.34, 129.23, p < 0.00001), however, this correlated with less intra-operative blood loss, less blood transfusions, and a shorter length of post-operative stay (WMD -3.45, 95% CI -4.39, -2.51, p < 0.00001). Readmission rates were higher with MIS, although, post-operative morbidity and mortality were comparable between both groups.
Conclusion
MIS approaches are a safe and feasible option for pelvic exenteration, with no differences in survival or recurrence outcomes compared to the open approach. MIS also reduced the length of post-operative stay and decreased blood loss, offset by increased operating time.
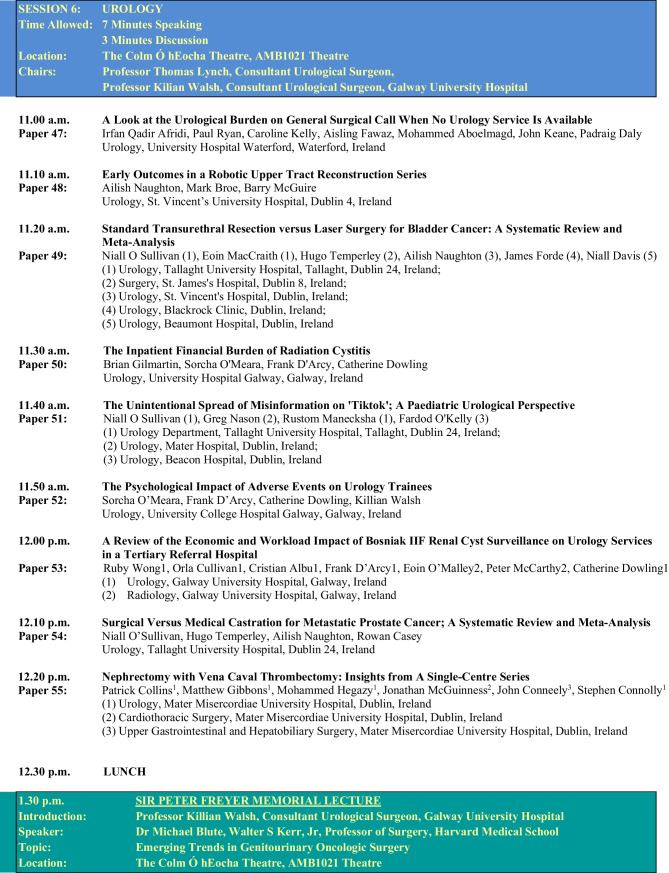
SESSION 6: UROLOGY
47. A Look at the Urological Burden on General Surgical Call When No Urology Service is Available
Irfan Qadir Afridi, Paul Ryan, Caroline Kelly, Aisling Fawaz, Mohammed Aboelmagd, John Keane, Padraig Daly
Urology, University Hospital Waterford, Waterford, Ireland
Introduction
Urology on-call services are available in most teaching hospitals. Some hospitals handover these services to the surgical team overnight. This can compromise the urgent management of patients and may result in unnecessary admission of others, due to the lack of a senior urology decision maker.
Aim
To audit the number of urology patients arriving through our emergency department out of hours over an 8-month period.
Methods
A retrospective review of a surgical admission logbook was performed for urology admissions between July 2021 and March 2022. The chief complaint of each patient was recorded. The theatre logbook was retrospectively evaluated for all emergency urology procedures carried out over the same period.
Results
A total of 260 patients were referred to the surgical on-call team with urological issues over this period. 161 of these patients were admitted for review. Mean length-of-stay was 4.27 days (range 1 – 23 days). 17 emergency urological procedures were performed by the general surgical team. 5 patients required urgent transfer to a neighboring hospital for specialist urology intervention by an on-call urology service.
Conclusion
Out of hours urology activity constitutes a significant burden on the workload of the general surgical team whilst also restricting essential training opportunities for urology trainees. Limiting urology cover can delay the treatment of urological emergencies and therefore compromise patient safety, whilst also resulting in the admission of patients who may otherwise have been discharged by a senior urology decision maker, therefore, adding to the burden on bed capacity at our institution.
48. Early Outcomes in a Robotic Upper Tract Reconstruction Series
Ailish Naughton, Mark Broe, Barry McGuire
Department of Urology, St. Vincent’s University Hospital, Dublin 4, Ireland
Introduction
The scope of robotic surgery has expanded to include reconstructive procedures, offering an alternative to the traditional approaches.
Aim
To assess perioperative and postoperative outcomes for patients undergoing robotic upper urinary tract reconstruction.
Methods
A prospective database of patients attending SVUH for robotic upper urinary tract reconstructive procedures was established in April 2018. Data recorded included patient demographics, intra-operative findings, post-operative recovery, and long-term outcomes. All procedures were performed by a single surgeon.
Results
74 patients to date have undergone robot-assisted reconstructive procedures for a range of underlying pathologies. Average patient age was 43.8 years (range 16–73). The most performed procedure was robotic pyeloplasty (n = 47). 9 buccal mucosa ureteroplasties were performed. 9 patients underwent ureteric reimplantation (7 with psoas hitch, 3 with Boari flap). Other reconstructive operations included appendix onlay ureteroplasty, non-transecting ureteric reimplantation (n = 2), ureterocalycostomy (n = 3), Uretero-uretero anastomosis (n = 2). Mean operation time was 2 h 49 min. Mean blood loss was 69.8mls. All patients followed an ERAS protocol. Median length of stay was 2 days. Mean length of follow up was 21.7 months (range 2 – 48). 4% of patients (n = 3) required a further procedure. There were two failures which were converted to Memokath nitinol stent successfully.
Conclusion
Robotic-assisted reconstruction of the upper urinary tract is a safe and feasible approach even in complex reconstructive cases with satisfactory short-term and long-term outcomes.
49. Standard Transurethral Resection versus Laser Surgery for Bladder Cancer: A Systematic Review and Meta-Analysis
Niall O Sullivan 1 , Eoin MacCraith 1 , Hugo Temperley 2 , Ailish Naughton 3 , James Forde 4 , Niall Davis 5
1. Urology, Tallaght University Hospital, Tallaght, Dublin 24, Ireland;
2. Surgery, St. James's Hospital, Dublin 8, Ireland;
3. Urology, St. Vincent's Hospital, Dublin, Ireland;
4. Urology, Blackrock Clinic, Dublin, Ireland;
5. Urology, Beaumont Hospital, Dublin, Ireland
Introduction
Transurethral resection of bladder tumour (TURBT) remains the gold standard method of diagnosing and treating non-muscle invasive bladder cancer. Laser resection has been demonstrated as a safe and efficacious alternative, however its mainstream use remains limited.
Aim
The aim of this review is to comparatively evaluate clinical outcomes of TURBT and laser resection of bladder tumour (LRBT) for bladder cancer.
Methods
A systematic review of the literature was performed for studies comparing TURBT and LRBT for bladder cancer. Outcome measurements were recurrence rates, complication rates, patient demographics, operative duration and inpatient stay. Meta-analysis was performed using Review Manager 5.
Results
Recurrence rates were similar between TURBT and LRBT (29.1% versus 28.2%%, p = 0.12). TURBT had a significantly greater obturator kick rate (11.5% versus 0.4%, p < 0.0001) and perforation rate (3.7% versus 0.009%, p = < 0.0001). In the six studies which reported on presence of detrusor muscle in the specimen, it was significantly greater in the LRBT group (96.6% versus 88.1%, p = 0.01). There was no significant different in operative time between the two groups. TURBT was associated with a significantly longer catheter duration (MD 0.98 days shorter in LBRT group; 95% CI, -1.45 to -0.5, p = < 0.00001), and length of stay (MD 1.12 days shorter in LRBT group, 95% CI; -1.7 to -0.54, p = 0.0001).
Conclusions
LRBT for bladder cancer has the benefit of reduced catheter duration, length of stay and perforation without impacting negatively on operation duration, recurrence rates or specimen quality.
50. The Inpatient Financial Burden of Radiation Cystitis
Brian Gilmartin, Sorcha O’Meara, Frank T D'Arcy, Catherine M Dowling
Urology, University Hospital Galway, Galway, Ireland
Introduction
Radiotherapy can be utilised as a treatment modality for pelvic malignancies. Complications of radiotherapy can lead to chronic management challenges. Radiation cystitis may result from radiotherapy for pelvic malignancies. Radiation cystitis develops in a small but significant proportion of the treated population with frequencies in the region of 5% to 10%1.
Aim
To establish the economic cost burden for inpatient care associated with radiation cystitis over a two-year period in University Hospital Galway.
Method
HIPE data was collated for patients with the diagnostic codes haematuria and radiation cystitis in 2018 and 2019. A retrospective review of electronic patient charts was performed to exclude patients presenting for reasons other than radiation cystitis. Costs were estimated in consultation with the hospital finance department and using HSE data on average inpatient bed day costs2, 3.
Results
A total of 23 individual patients were identified over a 2-year period. 96% male, 4% female. Mean age was 77 years. Radiation cystitis accounted for 621 inpatient bed days. Twelve patients required a flexible cystoscopy on the day ward. Seven patients required investigation and treatment in theatre under anaesthetic. Nine CT urograms and 10 Ultrasound kidneys were performed. The average running cost of an inpatient hospital bed is €878 per night3. Therefore, inpatient care cost was approximately €545,238, with a mean of €23,706 per patient.
Conclusions
Radiation cystitis accounts for a significant amount of inpatient bed days. A conservative estimate of cost was €23,706 per patient for inpatient care over the study period.
51. Published.
https://www.sciencedirect.com/science/article/abs/pii/S1477513122000961?via%3Dihub
52. The Psychological Impact of Adverse Events on Urology Trainees
Sorcha. O’Meara, Frank D’Arcy, Catherine Dowling, 1 Killian Walsh
Urology, University College Hospital Galway, Galway, Ireland
Introduction
Adverse events (AE) are an inevitable reality in healthcare, with an incidence of 12.6% in Irish hospital admissions.1 AEs have been recognised to cause psychological and emotional distress in healthcare workers, with surgical trainees being particularly susceptible.2,3 We report the first Irish data on experience of surgical trainees when dealing with AEs.
Methods
We distributed a web-based survey to all urology trainees in the Republic of Ireland. The questionnaire focused on trainees’ personal account of AEs within the previous six months, their emotional response, perceived contributing factors, and perceived benefit of support systems. The primary care PTSD screen (PC-PTSD-V) assessed for PTSD.
Results
A total of 16 responses were received from 12 (75%) registrars and 4 (25%) SHOs. Of the AEs reported, 12 (75%) were ≥ clavien-dindo 3b. Contributing factors identified included lapse of judgement (n = 6, 37.5%), risk of procedure (n = 7, 43%), lack of experience (n = 4, 25%). Anxiety (n = 8, 50%), guilt (n = 7, 44%) and sleep problems (n = 4, 25%) were the most reported emotional responses. Physical symptoms were reported in 2 (12%) trainees. A PC-PTSD-V score ≥ 3 was reported in 2 (12%) trainees. Most trainees (n = 13, 81%) reported talking to someone following the event with most (n = 12, 93%) talking to a consultant or NCHD colleague. Most trainees (n = 14, 87%) surveyed agreed that their training could better prepare them for the personal impact of AEs.
Conclusion
Urology trainees report negative psychological and emotional responses in the aftermath of an AE in keeping with international data. Those surveyed felt that their training could better prepare them for the personal impact of such events.
References
1. Rafter N, Hickey A, Conroy RM, et al. The Irish National Adverse Events Study (INAES): the frequency and nature of adverse events in Irish hospitals—a retrospective record review study. BMJ Quality & Safety 2017;26:111–119.
2. Han K, Bohnen JD, Peponis T, Martinez M, Nandan A, Yeh DD, Lee J, Demoya M, Velmahos G, Kaafarani HMA. The Surgeon as the Second Victim? Results of the Boston Intraoperative Adverse Events Surgeons' Attitude (BISA) Study. J Am Coll Surg. 2017 Jun;224(6):1048–1056. https://doi.org/10.1016/j.jamcollsurg.2016.12.039. Epub 2017 Jan 16. PMID: 28,093,300.
3. West CP, Huschka MM, Novotny PJ, et al. Association of Perceived Medical Errors With Resident Distress and Empathy: A Prospective Longitudinal Study. JAMA. 2006;296(9):1071–1078. https://doi.org/10.1001/jama.296.9.1071
53. Published.
https://link.springer.com/article/10.1007/s11845-022-02919-w
54. Surgical Versus Medical Castration for Metastatic Prostate Cancer; A Systematic Review And Meta-Analysis
Niall J. O’Sullivan, Hugo Temperley, Ailish Naughton, Rowan G. Casey
Urology, Tallaght University Hospital, Dublin 24, Ireland
Introduction
Metastatic disease is found in up to 20% of prostate cancer cases at diagnosis. Since their introduction in the 1980s, long acting gonadotropin releasing hormone (GnRH) analogues, administered subcutaneously or intramuscularly every one to six months have widely replaced bilateral orchidectomy as the method of castration for this cohort of patients. Recent evidence suggests that surgical castration confers a superior side effect profile and cost. We aimed to perform a systematic review and meta-analysis to compare these two treatment methods particularly in terms of survival, side effect profile and cost-effectiveness.
Methods
A systematic review of the literature was performed for studies comparing medical and surgical castration for metastatic prostate cancer. Outcome measurements included overall survival, side effect profile and cost.
Results
Fourteen studies on 38,877 participants (n = 35,584 for medical and n = 3,293 for surgical) met inclusion criteria. Our analysis demonstrated a significant difference in overall survival rates in favour of surgical castration (hazard ratio 0.81, 95% CI, 0.67 – 0.98, p = 0.03), less cardiovascular risk factors in the surgical group (OR 0.79, 95% CI, 0.62 – 1.00, p = 0.05) and nadir PSA levels in favour of medical castration (MD PSA 1.17 less in medical castration group, 95% CI, 0.67 – 1.67, p = < 0.00001).
Conclusion
Surgical castration appears to be a safe, feasible and efficacious alternative to medical castration, with evidence to suggest a potential survival benefit and limited evidence of a financial benefit in the treatment of men with metastatic prostate cancer. Further studies are required to further quantify the financial burden of one method over another, as well as to identify which subgroup of patients respond best to each method of castration.
55. Nephrectomy with Vena Caval Thrombectomy: Insights from a Single-Centre Series
Patrick Collins 1 , Matthew Gibbons 1 , Mohammed Hegazy 1 , Jonathan McGuinness 2 , John Conneely 3 , Stephen Connolly 1
1. Urology, Mater Misercordiae University Hospital, Dublin, Ireland
2. Cardiothoracic Surgery, Mater Misercordiae University Hospital, Dublin, Ireland
3. Upper Gastrointestinal and Hepatobiliary Surgery, Mater Misercordiae University Hospital, Dublin, Ireland
Introduction
Despite its technical complexity, surgical resection remains the mainstay treatment for locally-advanced kidney cancer. The aim of this study was to report on our centre’s contemporary experience with radical nephrectomy and inferior vena caval (IVC) thrombectomy.
Methods
Consecutive patients undergoing nephrectomy with IVC thrombectomy from 2016 to 2022 were retrospectively identified from a prospectively maintained operative database. Clinicopathological characteristics, operative details, and outcome were recorded.
Results
Twenty-four patients were included, with mean age 67.2 years. Half of patients were female. Most patients (78.3%) had right-sided tumours, with mean maximum tumour dimension of 93 mm. At presentation, 1 patient had known metastatic disease. Mean (SD) operative duration was 307.4(76.3) minutes. Level 1, 2, 3 and 4 thrombus was identified in 7(29%), 11(46%), 4(17%), and 2(8%) patients respectively. Cardiopulmonary bypass was required in 1 case. Graft reconstruction of the IVC was required in 2 cases. Most patients (91.7%) were initially managed in the high-dependency unit post-operatively. Median (IQR) overall length of stay was 10.5(7) days. Five patients experienced a grade 3 or greater complication. One patient died within 30 days of surgery. The most common (66.7%) histopathological finding was of clear cell renal cell carcinoma. Disease recurrence was observed in 50%, median (IQR) time to which was 11(10) months. However, three-year overall survival was 79.9 ± 9.2%.
Conclusion
We report on the feasibility and acceptable surgical morbidity profile of resection of locally advanced kidney cancer. These rare cases display aggressive tumour biology, and present a unique operative challenge, often requiring multi-specialty involvement.
References
1. Kaag MG, Toyen C, Russo P, et al. Radical nephrectomy with vena caval thrombectomy: a contemporary experience. BJU international. 2011;107(9):1386–1393.
SESSION 9: PLENARY SESSION
56. Anticoagulation for DVT Post-Endovascular ablation of Varicose Veins: Network Meta-analysis
Daniel Westby, Mohamed Elsharkawi, Fiona Nolan, Nathalie Doolan, Megan Power-Foley, Stewart Walsh
Vascular and Endovascular Surgery, Galway University Hospital, Galway, Ireland
Introduction
Deep vein thrombosis (DVT) is an established risk associated with endovascular ablation for varicose veins, < 1%. Anticoagulantion is the mainstay of treatment in the event of a DVT. Several anticoagulants ar available to choose from. This network meta-analysis compares anticoagulation regimes used in patients who develop a DVT post endovascular ablation for varicose veins.
Aim
Primary aim is to compare anticoagulation therapies and duration used in the event of DVT post endovascular ablation of varicose veins. Secondary aim to quantify the extent of secondary bleeding due to anticoagulation.
Methods
Medline, Embase, CINAHL and Cochrane Library databases were searched using appropriate terms for all studies reporting on DVT post endovascular ablation for varicose veins. Methodological quality of included studies was quantified using the Downs and Black checklist.
Results
407 articles were identified from preliminary searches with 22 studies satisfying the inclusion criteria. The analysis consisted of 63,076 patients with post-ablative DVT occurring in 358 patients. The anticoagulation regime was left to the treating physician in majority of cases. Agents commonly used were low-molecular weight heparin (LMWH), warfarin, a combination of both or direct oral anticoagulants (DOAC). Duration of therapy varied considerably among studies. Bleeding events related to anticoagulation are low and the need for intervention is lower again.
Conclusion
Although there has been a move towards DOAC in recent years, LMWH appears to remain the agent of choice for patients with post ablative DVT. The consensus for the duration of treatment is yet to be determined.
57. Surveillance, Oncologic Outcome and Health-Related Quality of Life: A Report from the ENSURE Study
Jessie A Elliott 1 , Sheraz R Markar 2 , George B Hanna 2 , John V Reynolds 1 , ENSURE Study Group 1 , Fredrik Klevebro 3 , Asif Johar 3 , Lucas Goense 4 , Pernilla Lagergren 3 , Giovanni Zaninotto 2 , Richard van Hillegersberg 4 , Mark Ivan Berge Henegouwen 5 , Magnus Nilsson 3
1. Surgery, Trinity Centre for Health Sciences, St. James's Hospital, Dublin, Ireland;
2. Surgery and Cancer, Imperial College London, United Kingdom;
3. Karolinska Institutet, Department of Molecular Medicine and Surgery, Sweden;
4. Surgery, University Medical Center Utrecht, Utrecht University, Utrecht, Netherlands;
5. Surgery, Cancer Center Amsterdam, Amsterdam UMC, University of Amsterdam, Netherlands
Introduction
Established and emerging therapies for recurrent oesophageal cancer may impact survival and health-related quality-of-life (HRQL), however surveillance protocols after primary curative treatment are inconsistent.
Methods
ENSURE was an international multicenter observational study of consecutive patients undergoing curative-intent surgery for oesophageal and junctional cancers (2009–2015) across 20 European and North American centers (NCT03461341). The initial report from ENSURE assessed the impact of intensive imaging surveillance on the primary outcome measure of overall survival (OS); secondary outcomes included treatment, disease-specific survival, recurrence pattern, and HRQL. In the present study, multivariable linear, logistic and Cox proportional hazards regression analyses were performed to determine the independent impact of surveillance modalities on oncologic outcome.
Results
4,682 patients were studied (72.6% adenocarcinoma, 69.1% neoadjuvant therapy). Routine biochemistry, nutritional profiling, tumor markers, endoscopy and flexible nasolaryngoscopy were assessed in 37, 33, 15, 19 and 7% of Centers, respectively. Among all patients, endoscopic surveillance was independently associated with increased probability of isolated local or anastomotic recurrence (OR1.49 [1.05–2.14]), but not with improved OS. Endoscopic surveillance was associated with improved OS (HR0.73 [0.55–0.98]) among patients with Barrett’s oesophagus, while flexible nasolaryngoscopy was associated with improved OS among patients with SCC (HR0.19 [0.05–0.80]). On multivariable analysis, nutritional surveillance was associated with increased tumor-directed therapy, improved HRQL (P = 0.015) and OS (HR0.89 [0.80–0.99]), while a multimodal surveillance approach was also associated with improved OS (HR0.83 [0.72–0.95]) among all patients.
Conclusion
These data suggest that a multimodal and tailored surveillance approach may improve oncologic outcomes following curative-intent surgery for oesophageal cancer.
58. Surgical Approach for Partial Nephrectomy in the Management of Small Renal Masses: A Systematic Review and Network Meta-Analysis
Ailish Naughton 1 , Eanna Ryan 2 , Robert Keenan 3 , Arun Thomas 1 , Lisa Smyth 1 , Rustom Manecksha 1 , Robert Flynn 1 , Rowan Casey 1
1. Urology, Tallaght University Hospital, Tallaght, Dublin 24, Ireland;
2. Surgery, Tallaght University Hospital, Dublin 24, Ireland;
3. Urology, University Hospital Limerick, Co. Limerick, Ireland
Introduction
A variety of surgical and non-surgical management options for small renal masses (SRMs) exist. Surgery, in the form of partial nephrectomy (PN) has three different approaches. It is unclear which partial nephrectomy approach, if any, offers superior clinical outcomes.
Aim
To compare outcomes in patients with SRMs less than 4 cm undergoing PN via open (OPN), laparoscopic (LPN) or robotic (RPN) approach, and to establish the advantages and disadvantages of the various approaches.
Methods
A systematic literature search was conducted for studies comparing at least two of the above techniques. 18 studies and 17,013 patients were included in our study. A network meta-analysis with a frequentist framework was performed. OPN was used as the baseline comparator. The pre-specified primary outcome was R0 resection rates. Secondary outcomes included operating time, ischaemia time, blood loss, transfusion rates, urine leak rates, significant morbidity, length of stay and recurrence.
Results
There was no significant difference between the techniques in terms of R0 rates, tumour recurrence, urine leak rates, renal function and > 3a Clavien-Dindo complications. LPN had a longer ischaemic time and operating time. OPN had a longer length of stay and higher average intraoperative blood loss. RPN had lower blood transfusion rates.
Conclusion
All approaches are acceptable from an oncological perspective. The minimally invasive approach (i.e.RPN and LPN) offer advantages in terms of morbidity; however, LPN may increase ischaemic time and operative duration. Variations between perioperative outcomes may influence choice of approach on a case-by-case and institutional basis.
59. Published.
https://journals.sagepub.com/doi/10.1177/11782234221086684
60. Published.
https://www.mdpi.com/2075-4418/12/4/794
61. Endocytosis Regulates Uptake of Indocyanine Green in an In Vitro Spheroid Model of Colorectal Cancer
Anwesha Sarkar 1 , Niall Hardy 2 , Donal O'Shea 3 , Stephen Thorpe 4 , Ronan Cahill 2
1. UCD School of Medicine, UCD Precision Medicine, UCD Conway Institute, University College Dublin, Dublin 4, Ireland;
2. Surgery, UCD Precision Surgery, Mater Misericordiae University Hospital, Dublin 7, Ireland;
3. Chemistry, Royal College of Surgeons in Ireland, Dublin 2, Ireland;
4. UCD School of Medicine, UCD Conway Institute, University College Dublin, Dublin 4, Ireland
Introduction
Surgical resection plays an important role in the treatment of colorectal cancer. Fluorescence guidance utilising the intravenously delivered fluorophore indocyanine green (ICG) is commonly used to identify intestinal perfusion following tumour resection. ICG accumulates in colorectal tumour tissue and methods have been developed to identify cancerous lesions based on the dynamics of ICG retention in vivo. Understanding the mechanism through which ICG accumulates is important.
Aim
This study aims to investigate cellular uptake mechanisms of ICG using both 2D and 3D spheroids model of colorectal cancer as in vitro representations of both malignant cell and tissues.
Methods
Assessment of active cellular processes potentially driving ICG uptake in HT-29 adenocarcinoma cells cultured in both 2D (with both low and high density plating) and 3D cultures. FFPE sections were made for characterisation of spheroids, followed by H&E staining. ICG treated spheroid cryosections were made for imaging. Analysis was done with near infrared fluorescence imaging digital scanner and an epifluorescent microscope.
Results
ICG uptake was dependent on the media ICG concentration (5–50 µg/mL). Cells cultured at 4 °C had reduced ICG uptake in both 2D and 3D cultures (p < 0.001). Inhibition of clathrin-mediated endocytosis with an inhibitor (Pitstop2) reduced ICG uptake in both 2D and 3D cultures at 50 µg/mL ICG (p < 0.001) but not at the more clinically relevant concentration of 5 µg/mL ICG. ICG uptake however increased with tight junction absence (p = 0.007).
Conclusion
Tight junction-related uptake is more likely then clathrin-mediated endocytosis to drive tumoral ICG uptake at clinically relevant concentrations.
62. Optimisation of a Peptide Hydrogel-Based Model for Pancreatic Cancer
Ciara Doyle 1 , Ella Kearns 1 , Elena Mangul 2 , Stephen Thorpe 1
1. School of Medicine, University College Dublin, Conway institute, Belfield, Dublin 4, Ireland;
2. School of Mechanical and Materials Engineering, University College Dublin, Belfield, Dublin 4, Ireland
Introduction
Pancreatic cancer, pancreatic ductal adenocarcinoma (PDAC) being the most common form, has one of the lowest survival rates of all cancers worldwide at 4–9%. PDAC is a dense hypovascular tumour, which shields it from traditional therapy such as chemotherapy. Personalised medicine such as immunotherapy offers potential to improve mortality rates. Patient-derived organoids are cell cultures derived from tumour biopsies in a 3D matrix, providing an ex vivo mimic of tumour structure and function.
Aim
Currently organoids are derived in Matrigel, a solubilised basement membrane. Disadvantages of Matrigel include batch-to-batch variability, its xenogeneic nature given its mouse origin, and it is difficult to control its physical or biochemical properties. Synthetic hydrogels offer advantages including control over growth conditions in a xenogeneic-free scenario to better replicate the stiff PDAC microenvironment.
Method
To optimise peptide hydrogels to model PDAC, three peptide sequences (Manchester BIOGEL) with varying concentration (stiffness) were used. Cell types included a metastatic PDAC cell line, SUIT2, a non-metastatic PDAC cell line, BxPC3 and primary human pancreatic stellate cells (hPSCs) as a cancer associated fibroblast source. Hydrogel architecture was assessed using scanning electron microscopy (SEM). Live-Dead staining and Cell Titre-Glo 3D were used to assess cell viability and proliferation. Cell morphology was assessed using fluorescent microscopy.
Results
Results indicate both cancer cells and hPSCs can be cultured successfully in peptide hydrogels without any extracellular matrix (ECM) addition.
Conclusion
Ongoing work will assess whether it is necessary to incorporate ECM or ECM-mimicking peptide sequences to derive patient organoids with application in personalised medicine.
63. Assessing the Relevance of Circulating MicroRNAs as Prognostic Biomarkers in Breast Cancer
Matthew Davey 1 , Andrew McGuire 1 , Maire Caitlin Casey 1 , Ronan Waldron 1 , Maxwell Paganga 2 , Emma Holian 2 , John Newell 2 , Helen Heneghan 1 , Ailbhe McDermott 1 , Maccon Keane 3 , Aoife Lowery 1 , Nicola Miller 1 , Michael Kerin 1,4
1. Discipline of Surgery, Lambe Institute for Translational Research, University of Galway, Ireland;
2. School of Mathematics, Statistics and Applied Mathematics, University of Galway, Ireland
3. Medical Oncology, Galway University Hospital, Galway, Ireland
4. Cancer Trials Ireland, Innovation House, Dublin, Ireland
Introduction
Deciphering patients who are likely to experience breast cancer relapse remains challenging to the multidisciplinary team. MiRNAs are small non-coding RNA which act at a post-transcriptional level influence protein synthesis by binding to messenger RNA. Their relevance in predicting breast cancer recurrence is uncertain.
Aim
To assess the value of circulating miRNAs in predict breast cancer recurrence.
Methods
ICORG10/11 was a prospective, multicenter trial which recruited patients undergoing neoadjuvant chemotherapy in 8 Irish hospitals. A miRNA panel were quantified from bloods at diagnosis and during neoadjuvant chemotherapy using RQ-PCR. MiRNA profiles were correlated with recurrence-free (RFS) and disease-free (DFS) survival. Data analytics was performed using R 3.2.3.
Results
124 patients with a median tumour size of 38.0 mm and follow-up of 8.6 years were recruited. Increased miR-145 expression predicted RFS (Hazard Ratio (HR): 0.00, 95% confidence interval (CI): 0.00–0.99, P = 0.05) with a relative cut-off of ≤ 0.2 for predicting an increased risk of recurrence using survival regression tree analysis (P = 0.04). Increased miR-145 expression trended towards predicting DFS (HR: 0.00, 95%CI: 0.00–1.42, P = 0.07) with a relative cut-off of ≤ 0.2 for predicting an increased risk of recurrence, new cancers, or death (P = 0.01).
Conclusion
This analysis illustrates the importance of using miRNAs as circulatory biomarkers capable of predicting recurrence in breast cancer patients. Validation of these findings is mandatory before the translation of these results into clinical practice.
SATURDAY, 3 RD SEPTEMBER 2022
SESSION 10: TRAINING AND EDUCATION
64. Assessment of the Use of Blood Cultures in the Detection of Bacteraemia: Phase 2 of an Experimental
Vianka Marcelino 1 , Dermot Hehir 1 , Sean Johnston 2
1. School of Medicine, University of Limerick, Castletroy, Limerick, Ireland;
2. Surgery, Midland Regional Hospital Tullamore, Offaly, Ireland
Introduction
Blood stream infection is one of the highest ranked problems in patient care due to its association with morbidity and mortality. The only consistent guideline for taking blood cultures (BCx) Ireland is the Sepsis 6 criteria. Research has shown that this approach yields a low rate of true positive samples, leading to misdiagnoses and delayed or over treatment. A prospective cohort study was undertaken in Midland Regional Hospital Tullamore (MRHT) from October to December 2020 to determine the number of true positive BCx, indicators prompting the BCx investigation and rate of contamination. A true positive rate of 8% and a contamination rate of 4% was found.
Aim
The aim of this study was to i) define indications for taking BCx; ii) reduce contamination rates following the implementation of novel interventions.
Method
A bespoke protocol for MRHT was drafted and circulated to all incoming non consultant hospital doctors (NCHD). Data from all BCx collected from July 10 2021 – July 31 2021 was studied prospectively.
Results
The key indicators identified were: pyrexia, tachycardia, tachypnoea, leucocytosis, neutrophilia, hyperlactataemia and raised CRP.
Blood Culture Results: 156 BCx Taken
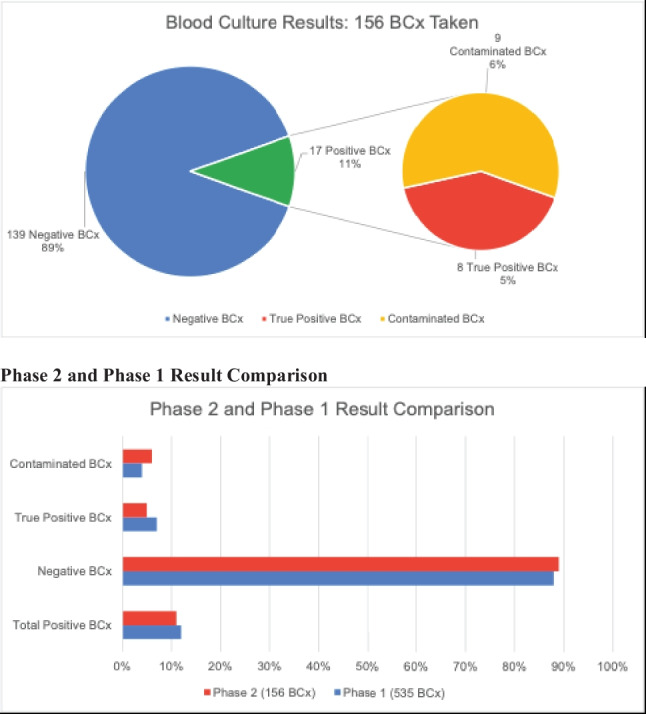
Conclusion
The findings show no improvement in true positive rates or a decrease in contamination rates following the implementation of the bespoke protocol. This is possibly due to a significantly smaller population, non-compliance or inadequate distribution of the protocol. We recommend ( i) that this study be continued with an appropriate sample size over a longer period of time(ii) redistribution of the protocol to all staff along with a tutorial.
65. Generating A Prioritised List of Operative Procedures for Simulation-Based Assessment Using A Modified Copenhagen Needs Assessment Framework
Conor Toale, Marie Morris, Adam Roche, Leonie Heskin, Dara Kavanagh
Surgical Affairs, Royal College of Surgeons in Ireland, St. Stephen's Green, Dublin, Ireland
Introduction
From August 2021, surgical training in Ireland has become explicitly outcomes based. The implementation of such competency-based training programs requires robust methods of summative assessment.
Aim
This study sought to outline a consensus on the general surgery procedures appropriate for use in simulation-based operative competency assessments for general surgery trainees at two stages of progression identified by the ISCP curriculum 2021: phase 2 (indicative time 4 years post- core surgical training) and phase 3 (end of training certification).
Methods
A modified Copenhagen Needs Assessment Framework utilising an iterative survey process was used to generate a prioritised list of procedures, using responses from a group of surgical trainers and a steering committee of five surgical education researchers. The 'impact', 'frequency', and 'risk' of a pre-defined procedure list was ranked. The steering group further ranked each procedure using three feasibility metrics. The provisional list of procedures was then returned to surgical trainers for re-ranking and consensus on final inclusion.
Results
Thirty surgical trainers were presented with 90 procedures derived from the JCST/ ISCP competency expectations. Seventeen procedures were subsequently included on recommendation of included participants. After iterative ranking, a provisional prioritised list of 30 procedures for each stage of training was produced. Appendicectomy was the top ranked procedure for operative competence assessments at ST6 (score 4.23/5.00), while cholecystectomy was the top ranked procedure for assessments at ST8 (score 4.35/5).
Conclusion
This study generated a prioritised list of procedures for use in simulation-based operative assessments, aligned with JCST expectations.
66. Published.
https://www.sciencedirect.com/science/article/abs/pii/S0748798322000695?via%3Dihub
67. A Blended Learning Approach to Surgical Teaching; What We Can Learn From The Student Experience
Darren Mc Cormack 1 , Jamie Martin-Smith 1 , Peter Cantillon 2
1. Plastic Surgery, Beaumont Hospital, Beaumont, Dublin, Ireland;
2. Clinical Education, University of Galway, Ireland
Introduction:
There is a growing trend of shifting medical education towards an online and simulation-based approach. The traditional hands on or experimental approach to medical education, is becoming less acceptable due to a myriad of legal and ethical issues. The shift to virtual delivery of content has been accelerated due to the covid 19 pandemic. Medical students have been propelled into this form of learning and this represents a paradigm shift in medical training and assessment. From informal discussions with undergraduate medical students, there is discontent with the move towards a blended approach with a variable amount of physical clinical exposure. This shift has also commenced despite a very poor evidence base to support this move. I was intrigued by the experiences the students were having and wanted to explore what they felt they were missing when the content was delivered online and if we can learn from them, as to how we can improve the delivery of surgical teaching with a blended delivery approach.
Aims:
Understand the student experiences that influence effective delivery of surgical clinical skills through a blended learning approach.
Methods:
Qualitative data collection will be carried from video analysis. From this data we will try to determine the factors involved in the student experience or clinical skills and what elements of the hidden curriculum are essential in delivering an effective surgical skills session.
Sampling method:
Final year medical students currently on placement in Beaumont hospital who have volunteered to take part after invitation.
68. Trends in Irish Surgical Research
Nathalie Doolan 1 , Stewart Walsh 2
1. Vascular Surgery, University Hospital Galway, Galway, Ireland;
2. National Surgical Research Support Centre, RCSI, Dublin, Ireland
Introduction
Participation in high quality surgical research is important for surgeons in training and those practicing as consultants. It forms a cornerstone of evidence based medicine. Randomized prospective studies are amongst the highest forms of scientific evidence, however the perceived complicated nature of designing and conducting them can be discouraging for researchers. Pre-registration of a trial is required for publication to most international journals and has been required by the International Committee of Medical Journal Editors since 2005. International registration of clinical trials has increased exponentially since then.
Aims
We sought to review if Irish surgical data reflected international research trends and to analyse the registration and publication of trials here amongst surgical specialities.
Methods
Data was extrapolated from clinicaltrials.gov for all national and international collaborative trials between 2012 and 2022. This data was cross referenced with Pubmed to examine what trials had been completed and published.
Results
Surgical groups registered 96 trials over this period of which 31% were international collaborations. Of the Irish trials, 71% were randomized control trial protocols and 29% observational (retrospective and prospective). General surgery represented 50% of the registered trials. There was no increased in trial activity over the past 10 years to match international trends. 31% of the trials had published their findings at the time of the review.
Conclusions
This preliminary study demonstrates that we are not matching international colleagues in our involvement in randomized trials. There may be a role for increasing support to surgical researchers to encourage their involvement.
69. Burnout among Surgical Staff at a Tertiary Hospital One Year From the Start of COVID-19 Pandemic
Amenah Dhannoon 1 , Emmeline Nugent 2
1. Surgery, Beaumont University Hospital, Dublin, Ireland;
2. Surgery, University Hospital Galway, Ireland
Introduction
COVID-19 pandemic has had significant impact on every department in our healthcare system. Our objective was to survey healthcare professionals in the surgical department in a tertiary hospital a year after the start of the pandemic to evaluate the impact of Covid-19 pandemic on burnout level, closely identify the causative factors as well as potential key solutions to improve wellbeing.
Methods
An online survey was sent to all doctors working in various surgical departments. Burnout level was assessed using the Maslach Burnout Inventory (MBI), a 22-question survey assessing the three components of the burnout syndrome-emotional exhaustion (EE), depersonalisation (DP) and personal achievement (PA).
Results
65 doctors responded to the questionnaire of all grades from consultant (30%) to interns (27%). With the majority in the age range 24–34 years and overall male: female of 36: 28. Most common marital status was married 47%. Eighty-three percent of respondents reported increased risk of burnout during the pandemic. The most commonly reported cause was inability to meet and socialise with friends and family (92%). The mean EE was elevated (32.15), DP level was also high (16.58). However, sense of personal achievement was notably low. The three components indicated high burnout level. Both local and national changes were suggested to reduce burnout level.
Conclusion
Even during the second wave of COVID-19 pandemic, surgical staff showed high level burnout. Not surprisingly, hospitals could have alleviate this by providing basic services like maintaining the residents place, providing parking space and food facilities during out-of-hour.
70. Development of a Novel Near-Peer Surgical Simulation-based Teaching Programme for Intern Doctors in the Mid-West Region
Bridgid Ferriter 1 , Barbara Julius 1 , Julie Evers 1 , Sarita Ankatiah 1 , Uchechukwu Alanza 1 , Sinead Burke 1 , Natasha Slattery 1 , Shona Tormey 1 , Anne Merrigan 1
Surgery, University Hospital Limerick, Dooradoyle, Limerick, Ireland
Introduction
Trends in healthcare have caused a shift in training towards more competency based programmes. The COVID-19 pandemic has reduced time available for direct exposure and clinical learning, necessitating incorporation of simulation in training.
Aim
The objectives of this study were to develop, pilot and evaluate a four week simulation based surgical teaching programme.
Method
Interns pursuing a career in surgery joined a near-peer surgical training programme delivered by NCHDs. A survey established a baseline competency. Four skills workshops were delivered. Outcomes were measured using data from pre and post course surveys and a surgical skills competition.
Results
Of the 12 trainees, 71% had scrubbed in theatre before. 50% were already confident to scrub independently, increased to 75% post training. 28% were confident gowning/gloving, increased to 75% post training. 28% were confident to place a simple suture in theatre, this did not increase despite training. 42% were confident performing an instrument tie, increased to 75% post training. 14% were confident hand tying knots, this increased to 62%. 14% of participants were comfortable performing excisional biopsy in theatre, increased to 62% post training. Preparation and administration of local anaestetic could be performed confidently by 14% before training, this increased to 87%. On completion, a surgical skills competition showed that 100% were able to satisfactorily perform basic skills.
Conclusion
Near-peer delivery of surgical training has enhanced the basic surgical skills of interns. Similar programmes in other sites would ensure that interns have the skills required to safely care for surgical patients.
71. Implementation and Impact of a Bespoke Simulation Surgical Consent Workshop For Medical Undergraduates
Niamh Moynagh, Emma Kearns, Ronan Cahill
UCD Precision Surgery, Mater University Hospital, Dublin, Ireland
Introduction
Communication skills are essential for effective clinical practice. Non-technical surgical skills training is a core component of our national surgical training scheme. We implemented and audited a similar model for medical students during their core surgical rotations.
Aim
To design, effect and assess a medical student communication workshop based around consent.
Methods
Over a twelve week term, weekly tutor-led communication workshops were held. Each week 10–12 students attended a 90-min session including a simulation consent scenario. Participants were invited to complete an anonymous survey via electronic channels including Yes/No questions, Likert-based scales and free text boxes to gauge their opinion and confidence levels re patient communication/consent.
Results
100% (n = 40) of responding students stated this teaching was beneficial, relevant and should be repeated in the future. > 90% of those surveyed felt their confidence in patient communication improved secondary to the session. 80% of students stated they weren't formally taught communication skills elsewhere, with > 90% indicating they would like broader inclusion of this across their curriculum. Interactive small group sessions were highlighted as the best mode of delivery for these sessions, followed by informal clinical observation and didactic teaching. Self-rated confidence levels were positive with regards to structure of conversation (90%, n = 36), discussion of risks (77.5%, n = 31), explanation of the procedure (85%, n = 34) and ability to empathise with patients (82.5%, n = 33).
Conclusion
Consent and communication based teaching was positively received by participants with students feeling a clear, positive outcome in comfort with consent communication as a result copperfastening this learning innovation in our curriculum.
72. Medical Students’ Perspectives on the Use of 3-D Reconstructive Models in Colorectal Surgery
Emma Kearns 1 , Niamh Moynagh 1 , Christian Myles 2 , James Jones 2 , Faraz Khan 1 , Ronan Cahill 1
1. UCD Centre for Precision Surgery, Mater Misericordiae University Hospital, Dublin 7, Ireland;
2. UCD School of Medicine and Medical Sciences, UCD, Belfield, Dublin 4, Ireland
Introduction
Three-dimensional (3-D) reconstructions of patients’ individualised anatomy can accelerate personalized, precision minimally invasive surgery. Beyond their purpose in surgical planning, they could have a role in medical education.
Aims
To gain insight into medical students’ perspectives on the utility of such 3-D reconstructions.
Methods
Students were shown 3-D reconstructive virtual models and one physical 3-d printed model previously created for right-sided colorectal cancer operations as part of an interactive tutorial. A mixed-methods survey was then distributed to students following the session.
Results
Forty-eight students completed the survey. Themes drawn from open-ended questions included their utility in engagement of and as a learning resource for students in theatre, in preoperative planning and intraoperative navigation for surgeons and in patient education. 97% (n = 44) agreed that the reconstructions are an excellent resource for trainees and medical students with 86% (n = 37) preferring the virtual reconstructions to the physical model. Reasons for this included more accessibility, practicality and ease of manipulation. 93% (n = 42) agreed the images would be useful for understanding the relations of the relevant vasculature with 88% (n = 40) agreeing that they found assessing these vessels difficult via CT imaging alone. 95% (n = 43) agreed that they would be useful at the time of surgery and that they would like to have access to these reconstructions to look at other areas of anatomy.
Conclusion
Feedback on the use of 3-D reconstructive models was generally positive, with the majority of students favouring virtual models over physical ones. Students identified usefulness of these models for surgeons, patients and medical students.
SESSION 11: PLASTIC , RECONSTRUCTIVE AND HAND SURGERY
73. The Margin of Safety: A Systematic Review of the Surgical Strategy and Recurrence Rates In Lentigo Maligna
Ellen Geary 1 , Aoife Granahan 2 , Aoife Lally 2 , Roisin Dolan 1
1. Plastic and Reconstructive Surgery, St Vincent's University Hospital, Elm Park, Dublin, Ireland;
2. Dermatology, St Vincent's University Hospital, Ireland
Introduction
Lentigo Maligna (LM) is a subtype of melanoma in-situ that typically presents as a slow growing, irregularly pigmented macule. If left untreated the risk of progression to invasive disease is estimated as high as 20%. Whilst there is significant variation in the treatment approach for LM, surgical excision with a margin of 5–10 mm remains the gold standard with reported recurrence rates (RR) ranging from 6–20%.
Aim
We aim to determine the optimum histological margins required to achieve complete clearance and minimise recurrence.
Method
A literature review of the National Library of Medicine per PRISMA guidelines was conducted by a medical librarian using Pubmed, MEDLINE, Embase, Science Direct and Cochrane Library databases. All articles and clinical studies relating to the surgical management and RR of LM up to and including October 22nd 2021 were included.
Results
A total of 17 studies met inclusion criteria. 77% of studies had a retrospective observational study design with a mean sample size of 142.8. The average RR was reported at 7.5% with a mean histological margin of 5.7 mm. Of these 7 studies included, only 5 report on time to recurrence at 50.84 months on average. T5 studies report on wound closure technique, with 30% and 25% requiring skin flap and graft reconstructions respectively.
Conclusion
Following surgical excision, we report comparable recurrence rates with histological margins of 5 mm and above. We report that a wider excision may not be necessary to achieve safe histological margin.
74. Amelanotic Melanoma in Ireland
Darren Mc Cormack 1 , Jamie Martin-Smith 1 , Natasha Christodalides 2 , Michael O`Shaugnessy 1 , Lucy Burns 1
1. Plastic Surgery, Beaumont Hospital, Beaumont, Dublin, Ireland;
2. Plastic Surgery, Cork University Hospital, Cork, Ireland
Introduction
According to the National Cancer Registry of Ireland, less than 5 AM have been recorded during 2014–2016, representing 0.45% of all melanomas recorded (personal communication National Cancer Registry) 7. The prevalence of AM is not known in an Irish context.
Methods
This is a retrospective cohort study of AM patients with melanoma diagnoses made in 2019 in two large Irish hospitals (Beaumont Hospital (BH) and Cork University Hospital (CUH)).
Results
A total of 175 patients in CUH and 97 patients in BH met the eligibility criteria for further assessing their records. Following examination of the medical records and checking the histology reports, a total of 25 (14.4%) in CUH and 21 (22%) in BH were identified as amelanotic resulting in an overall prevalence of 16.9%. Incidence was calculated based on the size of the target population in the area covered by the two hospitals. Based on this population, the incidence of AM was calculated to be 5.41 per 100,000 population.
Conclusion
Our study has identified a major discrepancy between the figures supplied by the national cancer registry of Ireland, who report a prevalence of 0.5%, and our finding of 17% in two hospitals in Ireland. AM is far more prevalent than reported in an Irish context 9. This underreporting has important implications for the detection of AM. It is known that AM can present with an increased Breslow thickness which is associated with worse outcomes and decreased overall survival.
75. Frailty as a Predictor of Adverse Outcomes in Head and Neck Reconstruction: A Systematic Review
Dhruv Kapoor 1 , Eoin Cleere 2 , Ciaran Hurley 1 , Catherine de Blacam 1 , Christoph Theopold 1 , Eamon Beausang 1
1. Plastic and Reconstructive Surgery, St James's Hospital, James Street, Dublin 8, Ireland;
2. Otolaryngology Head and Neck Surgery, Galway University Hospital, Galway, Ireland
Introduction:
Frailty has been shown to adversely impact outcomes in a number of surgical disciplines. In head and neck reconstructive surgery, frailty represents a risk factor that may aid in predicting post-operative adverse outcomes in a surgical population that is typically at high risk of complications.
Aim:
To summarise the available evidence about frailty as a predictor of postoperative complications, length of hospital stay and quality of life, in patients undergoing head and neck reconstructive surgery.
Method:
A prospectively registered (PROSPERO - CRD42022302899) systematic review in keeping with PRISMA guidelines was performed. MEDLINE, EMBASE, Scopus and Cochrane databases were assessed. Bias was assessed via Newcastle Ottawa Scores. All eligible articles evaluating the effect of pre-operative frailty on peri-operative surgical, social and quality of life related outcomes were included. Qualitative synthesis was undertaken due to heterogeneity in the reporting of outcomes.
Results:
Nine studies, which reported data on 10,323 patients undergoing reconstruction of the head and neck were included in the review. A number of different tools were used to assess frailty, with the modified frailty index used most frequently. In total, 8 studies reported increased rates of complications in patients with increased levels of frailty, irrespective of the frailty tool used.
Conclusion:
An association is observed between increased rates of peri-operative complications and increased levels of frailty in patients undergoing head and neck reconstruction. Frailty tools may represent a useful method to risk stratify patients undergoing reconstructive head and neck surgery.
76. The Lessons Learned From Managing Malignant Melanoma during COVID-19 in a Plastic Surgery Unit in Ireland
Amenah Dhannoon 1 , Ciaran Martin Hurely 2 , Laura Wrafter 2 , Padraic J Regan 2
1. Surgery, Beaumont University Hospital, Ireland;
2. Plastic and Reconstructive Surgery, Galway University Hospital Ireland.
Introduction
The COVID-19 pandemic has resulted in a pragmatic shift in practice of plastic surgery units worldwide. During this period, many units reported a significant fall in urgent melanoma referrals, resulting in presentation with advanced disease.
Aim
Our objective was to evaluate our units experience with both non-invasive and invasive melanoma during the COVID-19 pandemic and compare it to that experienced by our neighbours in the UK, mainland Europe and North America.
Methods
A retrospective chart review was performed on all patients diagnosed with invasive and non-invasive cutaneous melanoma between March to December of 2019 (control) compared to 2020 (COVID-19 pandemic) in a single plastic surgery unit in Ireland.
Results
A total of 589 patients were included in the study. Of these, 314 (53%) with invasive melanoma, compared to 275 (47%) with non-invasive disease. Overall, more patients were diagnosed with both invasive and non-invasive melanoma in 2020 than 2019 (p < 0.05). However, significantly longer waiting times in 2020 (64 days) compared to 2019 (28 days) (p < 0.05) with the majority of referral being from GP in 2019 (83%) compared to 61% in 2020. Positive sentinel lymph node were higher in 2019 at 56% (n = 28) compared to 24% (n = 22) in 2020. There was no statistical significant difference in the tutor characteristics or metastasis status.
Conclusion
Our study highlights that with prompt efficient restructuring of services, effective telemedicine triaging system, specialised skin cancer nurse with regular virtual skin cancer MDT, we could reserve successful management of skin cancer even in the most devastating times.
77. The Psychology of Surgery - the Application of High-Performance Sports Psychology to Surgical Training
Gary Fenn 1 , Stephanie Bollard 1 , Christine Quinlan 1 , Shirley Potter 1 , Kate Kirby 2 , James Matthews 3
1. Plastic and Reconstructive Surgery, Mater Hospital, Mater Hospital, Eccles St, Dublin 7, Ireland;
2. Sport Ireland Institute, Sport Ireland Institute, Dublin, Ireland;
3. UCD School of Public Health, Physiotherapy and Sports Science, University College Dublin, Dublin, Ireland
Introduction
Surgery is a craft-specialty, and like elite sport, successful training relies upon mastery of motor skills, as well as maintenance of concentration and management of stress. In the sporting setting, training in techniques to refine concentration, regulate emotion and sustain motivation, are commonplace, and may be applicable to surgery.
Aim
This study aims to assess the impact of mental skill training, based upon techniques used in high-performance settings, on performance anxiety levels of surgical trainees.
Methods
A prospective cohort study was performed, inviting surgical trainees to attend two small group mental skills training sessions led by an experienced Sports and Performance Psychology faculty. The programme delivered was designed around the Biopsychosocial model of Challenge and Threat. Performance anxiety was measured using the Sports Anxiety Scale-2 (SAS-2), which assesses somatic, worry and concentration disruption, before and after the workshop.
Results
The programme was attended by n = 9 trainees, with a median age of 31 years [25–39], and median training level of ST5 [1–8]. The mean pre-workshop SAS-2 score was 32. All participants reported using the techniques at least one to three times per week following the workshops. A significant decrease was seen in the SAS-2 scores, with a mean post-workshop score of 23 (p = 0.038). There was also a significant decrease observed in the mean ‘worry’ score (p = 0.017).
Conclusion
Dedicated mental skills training, using techniques utilised in high-performance settings, reduces the performance anxiety scores of surgical trainees. This is likely indicative of an improvement in self-regulation skills in stressful performance settings.
78. The Spiderman Sign - a Novel Method to Identify the Distal End of the Carpal Tunnel
Darren Mc Cormack, Ryan Sugrue
Plastic Surgery, Connolly Hospital, Blanchardstown, Dublin 15, Ireland
Aim
Identify the distal end of the carpal tunnel safely and effectively, by passive flexion of their ring and middle finger.
Method
We assessed 20 patients, prior to carpal tunnel decompression surgery and recorded the findings. A number of measurements were taken. The line at which the flexed ring and middle finger lay on the palm was marked, then following surgical exploration measurements were made with the distal end of the carpal tunnel and assessed how accurately this lined up with our pre-operative markings.
Results
Of 20 patients assessed the distal end of the carpal tunnel aligned with the pre operative markings made using the patients flexed fingers. 100% of cases the pre operative markings aligned with the distal end of the carpal tunnel found on surgical exploration.
Conclusion
There are various methods described to identify the distal end of the carpal tunnel. We feel our technique is a simple and effective method using the patients’ own anatomy to identify this important landmark, which we call the Spiderman sign.
79. TOxin for Treating Raynaud’s Conditions in Hands (The TORCh Study): A Systematic Review
Ellen Geary 1 , Patrick Gorman 1 , Kealan Blake 2 , Justin Wormald 3 , Roisin Dolan 2
1. UCD School of Medicine, St Vincent's University Hospital, Elm Park, Dublin, Ireland;
2. Plastic and Reconstructive Surgery Department, St Vincent's University Hospital, Dublin, Ireland;
3. University of Oxford, United Kingdom
Introduction
Raynaud’s disease of the hands is a complex disorder resulting in inappropriate constriction and/or insufficient dilation in microcirculation. Raynaud’s disease unresponsive to medical therapy is a significant problem for patients which can have a debilitating impact on a patient’s quality of life but a potential breakthrough in treatment could be found in botulinum toxin type-A (BXT-A).
Aim
The aims of this systematic is to qualitative synthesize the available literature to assess if BTX-A can prove an effective management strategy for primary and secondary Raynaud’s disease. Our secondary aim is to provide evidence for the design of a randomised control trial for using BXT-A in Raynaud’s disease.
Method
A medical librarian performed a literature search per PRISMA guidelines and for eligible articles using the Medline/PubMed database and Cochrane Collaboration to include studies up to, and including September 22nd 2021. Outcomes analysed were primary outcomes of each respective study; including visual analogue scale (VAS) score, healing of digital ulcers and disabilities of the arm, shoulder and hand (DASH) scores.
Results
In total, there 419 number of patients. With regards to primary outcomes assessed eight studies were concerned with improvement in VAS scores (75.7% of patients reported improvement). Nine healing of digital ulcers (74.2% of patients reported improvement). Five studies distinctively outline improvement in episodes (77.5% of patients reported improvement). Four studies reported improvement in temperature readings (78.3% of patients reported improvement).
Conclusion
This study illustrated that BTX-A can appears to be an effective management strategy for primary and secondary Raynaud’s disease.
80. A Needle in a Haystack
Lukas O Brien 1 , Mary-Ellen McMahon 2 , Ronan Cahill 3 , James Jones 4 , Barry O Sullivan 2 , Shirley Potter 1
1. Plastic Surgery, Mater Hospital, Eccles St, Dublin 7, Ireland;
2. Plastic Surgery, Beaumont Hospital, Beaumont, Dublin, Ireland;
3. Surgery, Mater Hospital, Eccles St, Dublin 7, Ireland;
4. Anatomy, University College Dublin, Belfield, Dublin 4, Ireland
Introduction
Unintentional intra-operative loss of surgical needles is a serious, yet infrequent complication during surgery. Suture calibre used for microvascular free flaps range from 8–0 to 10–0 sizes, making recovery of such needles difficult. Hospital protocols often recommend an intra-operative portable x-ray to locate the needles. There is a currently no evidence as to whether needles are visible on conventional xray.
Methods
Following ethical approval, sutures of varying needle calibres (3–0 to 10–0 Ethilon TM Ethicon) were placed on a cadaver. X-ray’s were obtained before and after needle placement. The sites imaged were the lower leg, forearm, chest, and neck, chosen to represent the areas most commonly involved in microsurgical procedures. Consultant and trainee surgeons, radiologists, and nursing staff were asked to identify the needles on the xray images.
Results
Of the 23 respondents, all participants successfully located 3/0, 4/0 5/0 and 6/0 needles on plain xrays taken at each of the 4 anatomical sites. Only 2 of the 23 participants were able to successfully localise an 8/0 needle, one on the neck xray and one on the forearm xray. None of the participants were able to successfully localise the 9/0 or 10/0 needles at any of the anatomical sites.
Conclusion
Portable xray has a definite role to play in the event of loss of needles size 3/0 to 6/0. This study has proven that suture needles smaller than 8/0 cannot be reliably detected on xray, and this modality is therefore not recommended. Hospital protocols should reflect this.
81. Applying Human Reliability Analysis to Identify and Reduce Risks in Carpal Tunnel Decompression
Áine Lucey, Sharon Kennedy, Alan Hussey, Niall Mcinerney, Jack Kelly, Kenneth Joyce
Plastic and Reconstructive Surgery, Galway University Hospital, Galway, Ireland
Introduction
Many surgical procedures are prone to human error, particularly in the learning phase of skill acquisition. Standardisation has been suggested as an approach to reducing such errors. This study used human reliability analysis methodologies to examine carpal tunnel decompression.
Methods
The subgoals, or individual steps, required to complete a carpal tunnel decompression were identified using hierarchical task analysis (HTA). The systematic human error reduction and prediction approach (SHERPA) was carried out by consensus of Subject Matter Experts in the Department of Plastic Surgery. This identified the potential human errors at each subgoal, the level of risk associated with each task and how these potential errors could be prevented.
Results
Carpal tunnel decompression was broken down into 46 subgoals, of which 21 (45%) were medium risk and 25 (55%) low risk. Of the 46 subgoals, 4 (9%) were assigned high probability, 18 (39%) assigned medium probability. High probability errors (> 1/50 cases) included selecting incorrect tourniquet size, failure to infiltrate local anaesthetic in a proximal-to-distal direction and completing WHO sign-out. Three (6%) of the subgoals were assigned high criticality which included failure to aspirate prior to anaesthetic injection, while 21 (45%) were assigned medium criticality and 22 (48%) were assigned low criticality. Remedial strategies for each potential error were then devised in order to reduce errors.
Conclusion
The use of human reliability analysis techniques provides surgeons with a platform to performing surgical procedures and identify critical steps which are prone to error. This approach will improve surgical training and enhance patient safety by reducing technical errors.
SESSION 12: TRAUMA AND ORTHOPAEDIC SURGERY
82. A Retrospective Analysis of the Incidence and Radiographic Parameters of Patients with Acetabular Protrusio Presenting For A Primary Total Hip Arthroplasty in a Tertiary Referral Centre in the Republic of Ireland.
David O Sullivan, Patrick Carroll, William Curtin, Colin Murphy
Trauma and Orthopaedic Surgery, Galway University Hospitals, Galway, Ireland
Introduction
Protrusio Acetabuli (PA) is defined as the medialisation of the femoral head relative to köhler's line and its incidence internationally is 5%. PA is multifactorial. Total Hip Arthroplasty (THA) is challenging in patients.
Aim
The aim of this study was to document the incidence of PA, the medical conditions associated with it and the technical challenges encountered in planning THA in this cohort.
Method
A retrospective analysis of patients presenting to our institution for an elective THA was performed. Radiographs were examined and the medialisation of the femoral head to köhler's line was used as the diagnosis of PA. In this cohort, a patient's medical condition or diagnosis was searched for. PA severity pre-operatively and lateralisation distance on post-operative radiographs was measured.
Results
The pre operative radiographs of 508 patients presenting for an elective THA over six years were reviewed. PA was identified in 4.3% (22/508) of patients, 73% female and 63% involving the right leg. 86% of THA were uncemented. Idiopathic PA was diagnosed in 55%, inflammatory arthropathy in 9% and cancer in 23%. Mean protrusion distance was 6.8 mm and mean lateralisation 9.59 mm.
Conclusion
The incidence of PA in our catchment area is in line with international incidence rates. These patients require considerable pre-operative planning and complex acetabular reconstruction. We propose the joint registry allows for the diagnosis of PA be included in its data collection.
83. Bibliometric Analysis on Top 50 Cited Randomised Controlled Trials in Shoulder and Elbow Surgery
Conor Kilkenny 1 , Eoghan Hurley 2 , Tom Moore 1 , Robert Hurley 2
1. Orthopaedic Surgery, Galway University Hospital, Galway, Ireland;
2. Orthopaedic Surgery, Mater University Hospital, Dublin, Ireland
Introduction
Bibliometric studies are valuable and interesting forms of research in assessing the impact of literature in a given field.
Aim
The purpose of this study was to assess the impact the top 50 cited Randomised Controlled Trials in Shoulder and Elbow Surgery are having on this subspecialty.
Methods
A Web of Science search with the keyword search of Shoulder and Elbow Surgery and Randomised Controlled Trial was performed. The top 50 cited studies were included. Data extracted were; Year most studies were published, most prominent Journals, country with most publications, number of patients involved in study, follow up time, pathology being studied and a fragility index was calculated.
Results
2011 was the most impactful year in terms of studies published with 11 papers published. The most prominent journal was The Journal of Shoulder and Elbow Surgery with 24/50 papers. Most of these studies were produced in USA with 14 papers. Follow up ranged from 0–30 months with the average follow up time being 13.7 months. Patient numbers in each study ranged from 20–660 with the average of 92. The most common pathology studied was rotator cuff tear with 22 studies. Fragility Index was calculated in 29/50 studies ranging from 0–10. 15 studies had a fragility index > 0.
Conclusion
This study analysis the most significant studies in the area of shoulder and elbow surgery. Interesting data can be concluded from this research however more high quality, less fragile and statistically significant research is needed in this sub-speciality.
84. Olecranon Fractures: Quality and Readability of Information Online
Heather Hassett, Gabrielle McDonagh, Geoff Crozier-Shaw, John Kelly
Trauma and Orthopaedic Surgery, Sligo University Hospital, Sligo, Ireland
Introduction
Patients are consuming more information online than ever before. This can lead to confusion and anxiety when reading information of poor quality, or that which is aimed at clinicians.
Aim
We aim to assess the quality and readability of online information on olecranon fractures.
Methods
Google, Bing and Yahoo were searched using terms “patient information on olecranon fractures”. DISCERN, JAMA, Health on the Net (HON), and an olecranon specific score measured quality and Flesch-Kincaid score assessed readability.
Results
70 unique websites were identified, 32 results being academic/physician focused, 38 being patient-focused. Mean Discern score was 47 for academic/physician websites, and 39.5 for patient focused (p = 0.0116). JAMA criteria were fulfilled in 43% of academic websites and 0% of the patient websites (p = 0.0001). The HON criteria were met in 9% of academic websites and 0% of patient websites (p = 0.09). For olecranon specific score, academic sites scored a mean of 1.84 compared to 1.11 mean score for patient websites (p = 0.04). On average, patient-aimed websites needed a higher reading level as compared to academic sites, mean score of 40.02 and 58.9 respectively (p = 0.0001).
Conclusion
This study found that online information on olecranon fractures was of poor quality and was often presented at an inappropriately high of a reading level, even on patient specific websites. Health care providers should direct them towards appropriate online resources when discussing management of their olecranon fractures.
85. Orthopaedic Trainee Knowledge of Metastastic Bone Disease
Ali Donnelly, Iain Feeley, Gary O’Toole, Alan Molloy
Department of Orthopaedic Surgery, St Vincent’s University, Elm Park, Dublin 4, Ireland
Introduction
Increased survivorship in patients with cancer has resulted in an increased incidence of patients presenting to orthopaedic services with metastatic bone disease. In response to this the British Orthopaedic Oncology Society and the British Orthopaedic Association produced guidelines on the best practice in metastatic bone disease.
Aim
To assess orthopaedic trainee knowledge and awareness of the guidelines for best practice in metastatic bone disease.
Method
We produced a survey of 20 questions from the guidelines but based on everyday practice in orthopaedic patients with metastatic bone disease. We also collected data based on trainee experience, prior exposure to orthopaedic oncology and whether they were pre or post FRCS examination.
Results
There was an 83% response rate to the survey. 45% of trainees were aware of the guidelines – this ranged from 20% awareness at ST3 to 100% awareness at ST8. The median score to the questionnaire was 60% (25%–90%). Those post FRCS exam scored a median of 75%, as did those with an exposure to orthopaedic oncology. The remaining scored a median of 55%. Scores did increase as training progressed. Analysis of the individual questions demonstrated a poor knowledge of the adjunct therapies and scoring systems in metastatic bone disease but a good understanding of the work-up and basic principles in surgical fixation.
Conclusion
Metastatic bone disease will be a more common presentation to future orthopaedic surgeons. Current trainees are not sufficiently aware of the current guidelines and potentially require more focused training in this area.
86. Prophylactic Use of Local Antibiotics in Open Fractures: A Systematic Review and Meta-Analysis
Dhruv Kapoor 1 , Ross Condell 2 , Niamh Kennedy 3 , Peyman Bakhshayesh 4
1. Trauma Science, Blizard Institute, Queen Mary University of London, London, United Kingdom;
2. Surgery, Galway University Hospital, Galway, Ireland;
3. Surgery, St James's Hospital, James Street, Dublin 8, Ireland;
4. Orthopaedic Trauma, Major Trauma Centre, Leeds General Infirmary, Leeds, United Kingdom
Introduction
The management of open long bone fractures is well described and has been standardised through a number of well established guidelines. However there is no consensus regarding the application of local antibiotics into the open fracture site as a means of reducing infection rates.
Aim
To summarise the literature and to assess if the prophylactic addition of local antibiotics to the standard treatment reduces infection rates at long bone open fracture sites.
Method
A systematic review and meta-analysis was undertaken as per PRISMA guidelines. PubMed, Embase, Scopus and CENTRAL were the databases assessed. The Newcastle Ottawa Scale and the Rob 2 Tool were used to assess bias. A qualitative synthesis of all included studies and meta-analysis of suitable subgroups was undertaken.
Results
In total, 12 studies (11 observational, 1 RCT) assessing 2431 open fractures were included for analysis. All compared the addition of a local antibiotic therapy to a standard treatment versus the standard treatment alone. The methods of delivery were vancomycin powder (4 papers), tobramycin polymethylmethacrylate beads (4 papers), gentamicin coated intramedullary (IM) nails (2 papers), gentamicin injections (1 paper) and antibiotic released IM core cement (1 paper). The addition of vancomycin powder did not decrease infection rates in comparison to intravenous antibiotics alone (OR 1.3, 95% CI (0.75–2.26)).
Conclusion
There are numerous methods available to deliver antibiotics locally to an open fracture site. Further high quality research is required to provide a definitive conclusion on their efficacy irrespective of delivery method.
87. Trauma Surgery Consent Documentation in Ireland
Mohamed ElZayat, Simon Callaghan, Geoffrey Crozier-Shaw, John Kelly
Orthopaedic Surgery, Sligo University Hospital, Sligo, Ireland
Aim
Ireland does not currently have a uniform and standardised method in which the consent proves is routinely documented. This study was designed to evaluate the standard consent forms used in trauma orthopaedic hospitals across Ireland while also evaluating the current guidelines regarding consent documentation in the trauma setting from Ireland and the UK.
Methods
Standard consent forms were obtained from the 16 public hospitals where trauma orthopaedic surgery is performed. These were analysed and compared based on the inclusion or exclusion of 22 unique consent related items or statements selected by the authors. Additionally the consent forms were analysed for readability, word count and format.
Results
Within the 16 public hospitals where trauma orthopaedic surgery is performed there are a variety of unique consent forms in use. There was a mean inclusion of 9 of the 22 unique items per form. This indicates many units are not utilising comprehensive consent documentation. The mean Flesch Reading Ease score was 45. The format varied throughout the consent forms and ranged in length from 1 to 4 pages.
Conclusion
This study shows the lack of uniformity being used in consent forms throughout the trauma orthopaedic units across Ireland both in terms of format and content. A national standardised consent documentation method may be useful to improve efficiency, patient experience and decreased litigation.
88. Published.
https://link.springer.com/article/10.1007/s11845-022-02939-6
89. Subscapularis Management during Open Latarjet Procedure- Does Subscapularis Split versus Tenotomy Matter? A Systematic Review & Meta-Analysis
Martin Davey, Matthew Davey, Eoghan Hurley, Hannan Mullett
Sports Surgery Clinic, Dublin, Ireland
Introduction
The aim of this study was to perform a systematic review and meta-analysis assessing clinical outcomes of open Latarjet (OL) procedure using either a Subscapularis Split (SS) or Tenotomy (ST).
Methods
A systematic review was performed as per PRISMA guidelines with studies reporting outcomes of OL procedure via a deltopectoral (DP) approach comparing both SS and ST being considered for inclusion.
Results
Overall, 5 studies including 615 shoulders (80.8% males), with average age of 27.8 ± 12.6 years (15–79) and mean follow-up of 50.1 ± 29.4 months (12–180) were included. There were 410 and 205 shoulders who underwent OL procedure via a DP approach using ST and SS techniques respectively, with both techniques resulting in significant increases in the Rowe scores postoperatively (both p < 0.0001). Additionally, there were significantly higher postoperative Constant scores in those who underwent OL using a SS technique, versus those in the ST groups (91.8 ± 7.2 vs 79.6 ± 16.1, p < 0.0001 respectively). Furthermore, there were significantly more patients in the ST group who were lift-off test positive when compared to the SS group at final follow-up (2.7% versus 10.0%, p = 0.01). However, the rate of recurrent instability was trending towards significance in favour of the SS group (0% vs 11.7%, p = 0.07).
Conclusion
For OL procedures being carried out via DP approach, the SS technique results in significantly better functional outcome measures and significantly lower rates of subscapularis insufficiency.
90. Orthopaedics Operative Notes Auditing, Improving Clinical Performance
Mohamed ElZayat, Annis Maatough, Ahmed Karkuri, John Kelly
Orthopeadic Surgery, Sligo University Hospital, Sligo, Ireland
Introduction
Precise and accurate documentation of surgical operative notes are pivotal in the postoperative care of patients. This prospective study audited the quality and completeness of documentation of all orthopaedic surgical operation performed in our unit over a 3 weeks period. Notes were assessed and compared to best practice guidelines from the Royal College of Surgeons in Ireland (2004) Good Surgical Practice guidelines and Code of Practice for Surgeons (2018).
Aim
The aim of this study was to audit performance and introduce a new operative note system, thereby improving clinical and compliance with best practice guidelines.
Method
A total of 50 operation notes were prospectively collected in a 3 week period. Documentation was measured against all 14 standards described in the Royal College of Surgeons Ireland guidelines. A list of suggested points and recommendations, including an operative proforma were formulated be presented to attempt and improve our operative documentations. Re-audit was performed and showed improvement in all standards.
Results
Our preliminary results showed that the current documentations are significantly deficient. We have recorded 100% adherence in documenting operative procedures and closure technique. But poorly in many other areas such as documenting the type of surgery (Elective or Emergency), operative time, date and medical council registration number. Re-Audit followed after 3 months of introduction of changes and new perfume and showed 95% improvement in all areas of standards described by the RCSI.
Conclusion
This study has demonstrated significant deficiencies in how operative procedures are recorded. This has facilitated the development of a new structured operative note which successfully meets all the RCSI recommended criteria, which has been introduced successfully to our unit.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.