Abstract
We investigated the role of the functional domains of anthrax toxins during infection. Three proteins produced by Bacillus anthracis, the protective antigen (PA), the lethal factor (LF), and the edema factor (EF), combine in pairs to produce the lethal (PA+LF) and edema (PA+EF) toxins. A genetic strategy was developed to introduce by allelic exchange specific point mutations or in-frame deletions into B. anthracis toxin genes, thereby impairing either LF metalloprotease or EF adenylate cyclase activity or PA functional domains. In vivo effects of toxin mutations were analyzed in an experimental infection of mice. A tight correlation was observed between the properties of anthrax toxins delivered in vivo and their in vitro activities. The synergic effects of the lethal and edema toxins resulted purely from their enzymatic activities, suggesting that in vivo these toxins may act together. The PA-dependent antibody response to LF induced by immunization with live B. anthracis was used to follow the in vivo interaction of LF and PA. We found that the binding of LF to PA in vivo was necessary and sufficient for a strong antibody response against LF, whereas neither LF activity nor binding of lethal toxin complex to the cell surface was required. Mutant PA proteins were cleaved in mice sera. Thus, our data provide evidence that, during anthrax infection, PA may interact with LF before binding to the cell receptor. Immunoprotection studies indicated that the strain producing detoxified LF and EF, isogenic to the current live vaccine Sterne strain, is a safe candidate for use as a vaccine against anthrax.
Bacillus anthracis, a spore-forming bacterium, is the causative agent of anthrax. Virulent encapsulated strains secrete two toxins composed of three proteins: the protective antigen (PA; 83 kDa), the lethal factor (LF; 85 kDa), and the edema factor (EF; 89 kDa) (16) encoded by the pag, lef, and cya genes, respectively (2, 6, 21, 41). These genes are carried by the virulence plasmid, pXO1 (185 kbp) (18). The lethal toxin (PA+LF; Letx) causes the death of animals after intravenous injection (1). The edema toxin (PA+EF; Edtx) induces the formation of an edema at the inoculation site (33). PA is the common binding moiety, and EF and LF are the intracellular enzymes that damage the cells. The crystal structure of the monomeric PA has been determined at a resolution of 2.1 Å (24). It shows that the molecule is folded into four functionally independent domains. Such an organization is consistent with previous in vitro experiments (17, 23). Each domain is required for a specific step in the intoxication process. PA binds to the cell receptor via its carboxy-terminal extremity (domain 4) (4, 7, 31, 39). An exposed 19-amino-acid loop located within this domain is involved in the binding of the toxin to the cell surface (4). The amino-terminal domain (domain 1) is then cleaved at the consensus RKKR sequence recognized by furin-like proteases (12, 30). This processing results in the release of a 20-kDa amino-terminal fragment (PA20), the heptamerization of a 63-kDa carboxy-terminal fragment (PA63) bound to the receptor, and the subsequent binding of EF or LF (19, 20). Deletion of the furin-sensitive sequence abolishes the cleavage of PA and the effects of the toxins (30). The toxic complexes (PA63-LF or PA63-EF) are internalized via receptor-mediated endocytosis (9). Two phenylalanine residues, F313 and F314, located in domain 2 are involved in the translocation of EF and LF into the cytoplasm (24, 32). Mutations in the sequence encoding ATP-binding site of EF (k346GlnvhGKS), decrease the calmodulin-dependent adenylate cyclase activity of this protein (14, 15, 42). LF is a zinc metalloprotease (13). Mitogen-activated protein kinase kinases 1 and 2 (MAPKK1 and MAPKK2) have been identified as substrates for LF (5, 40). Mutations affecting the catalytic site of LF (H686EfgH) result in the loss of Letx cytotoxic activity against macrophages and abolish MAPKK cleavage and the mitogenic effect of Letx (9, 10, 13).
The anthrax toxins play a key role in anthrax pathogenesis both in the early stages and during disease progression (11). The pathogenesis of anthrax has been studied by experimental infection of mice. Animals injected subcutaneously with live spores of the toxinogenic B. anthracis Sterne strain exhibit characteristic symptoms of the disease: edema and shock-like death. Recombinant B. anthracis with one or two of the toxin genes deleted is much less virulent than the parental Sterne strain (25, 26). The specific serum antibody response to LF is also significantly stronger in mice immunized with strains that produce PA, demonstrating the importance of interaction between PA and LF in the immune response (27). Studies in recent years of the functional organization of toxin components have provided a molecular basis for analyzing the interaction of toxins with the host during infection and the contribution of toxins to the development of anthrax immunity. In this work we analyzed the lethality and edema formation induced by strains of B. anthracis producing site-directed mutants of PA, LF, and EF in mice. The antibody response against mutant PA and LF molecules was also used as a tool to study the interaction between these two molecules in vivo. The ability of B. anthracis mutant strains to protect mice against a lethal challenge was analyzed.
MATERIALS AND METHODS
Bacterial strains and media.
E. coli and B. anthracis strains were cultured in Luria broth and brain heart infusion (BHI; Difco, Detroit, Mich.) medium, respectively (29). Ampicillin (100 μg/ml), spectinomycin (60 μg/ml), kanamycin (40 μg/ml), and erythromycin (5 and 180 μg/ml for B. anthracis and E. coli, respectively) were added as appropriate. The Sterne vaccine strain of B. anthracis 7702(pXO1+) from the Institut Pasteur Collection and the virulent capsulated strain 17JB (kindly provided by Rhône-Merieux) were also used (38). The strains produced in this work are listed in Table 1.
TABLE 1.
B. anthracis strains
| Strain | Genotypea | Antibiotic resistance | Toxin components produced
|
Parental strain | ||
|---|---|---|---|---|---|---|
| PA | LF | EF | ||||
| 7702 | pXO1 | None | PA | LF | EF | Sterne strain (Pasteur collection) |
| RPA | pXO1-pagΔ(1805–2871) | Spc | LF | EF | 7702 | |
| RPA200 | pXO1-pagΔ(1805–4105) | Erm | LF | EF | 7702 | |
| RPL | pXO1-lefΔ(2105–2970) | Spc | PA | EF | 7702 | |
| RPL200 | pXO1-lefΔ(486–2911) | Erm | PA | EF | 7702 | |
| RPE | pXO1-cyaΔ(400–2311) | Spc | PA | LF | 7702 | |
| RPE346 | pXO1-cya346/353 | None | PA | LF | EF346/353 | RPE |
| RPL686 | pXO1-lef686 | None | PA | LF686 | EF | RPL |
| RPL686Δcya | pXO1-cyaΔ(1414–2420) | Kan | PA | LF686 | RPL686 | |
| RPLC2 | pXO1-lef686-cya346/353 | None | PA | LF686 | EF346/353 | RPL686Δcya |
| RPA163 | pXO1-pagΔ(2376–2395) | None | PA163 | LF | EF | RPA |
| RPA313 | pXO1-pagΔ(2826–2833) | None | PA313 | LF | EF | RPA |
| RPA705 | pXO1-pagΔ(4005–4053) | None | PA705 | LF | EF | RPA200 |
| RPA608 | pXO1-pag608 | None | PA608 | LF | EF | RPA200 |
The numbers after “Δ” indicate the nucleotides at which the deletions start and finish. Erm, Kan, and Spc indicate the insertion of erythromycin, kanamycin, and spectinomycin resistance cassettes, respectively, into the disrupted toxin genes. None, no resistance.
Mutagenesis of toxin genes.
Mutations (pag163, lef686, and cya346/353) were introduced into wild-type genes cloned in M13 bacteriophages by site-directed mutagenesis (Sculptor Kit; Amersham, Cleveland, Ohio). The allele encoding PA313 was obtained by PCR-based mutagenesis of pACP41, which carries the wild-type pag gene (26) (QuikChange Site-Directed Mutagenesis Kit; Stratagene, La Jolla, Calif.). Domain 4 PA mutants (PA608 and PA705) were produced by PCR as previously described (4).
Mating procedure.
Toxin mutant genes were inserted into the integrative pAT113 (37) and pXF113 vectors, derived from pAT113 by replacement of the erythromycin resistance gene by the spectinomycin cassette from Tn544 of Staphylococcus aureus (22). HB101(pRK24) was used as the donor E. coli strain for conjugation (34, 37). The B. anthracis recombinant strains were obtained by heterogramic mating as previously described (25). The kanamycin, erythromycin, and spectinomycin resistance genes used in this study have been described elsewhere (22, 35, 36). B. anthracis strains carrying a mutant gene in place of the wild-type allele were constructed in two steps (see Results). Recombinant plasmids integrated by a single crossover into the B. anthracis pXO1 were selected after mating on agar plates containing the antibiotic required for plasmid maintenance. The resulting merodiploids (∼5 μl of culture; optical density at 600 nm [OD600] = 0.8) were diluted in 5 ml of fresh BHI medium and were grown for 16 h at 37°C without any antibiotic. After 7 to 15 subcultures, ca. 1 to 10% of the bacteria were found to be sensitive to the marker antibiotics and harbored a mutated toxin gene. Each recombinant strain was checked by PCR and sequencing of the mutated region (Sequenase Kit; Amersham).
Detection of B. anthracis toxin components.
Recombinant B. anthracis were grown in R medium supplemented with 0.4% (wt/vol) sodium bicarbonate at 37°C in tightly closed flasks, to an OD600 of 0.7 (28). Proteins in the culture supernatant were precipitated in 10% trichloroacetic acid and subjected to electrophoresis in a 10% denaturing polyacrylamide gel. The proteins were transferred to a nitrocellulose membrane (Hybond-C; Amersham) for immunoblot analysis. Monoclonal antibodies specific for PA, EF, or LF (provided by Hybridolab, Institut Pasteur) were used at a dilution of 1/5,000. A secondary antibody, anti-mouse immunoglobulin coupled to horseradish peroxidase, was added at a dilution of 1/20,000. The immunocomplexes were detected by enhanced chemiluminescence (Amersham).
Cleavage of mutant PA proteins by serum.
Cleavage experiments were performed as described by Ezzell et al. (8). Mutant proteins were incubated for 60 min at 37°C in filtered mice serum (final concentration, 100 μg/ml). Proteins (100 ng) were subjected to electrophoresis in a 10% denaturing polyacrylamide gel and transferred to a nitrocellulose membrane (Hybond-C) for immunoblot analysis. Rabbit polyclonal antibodies specific for PA were used at a dilution of 1/10,000.
In vivo experiments.
Seven-week-old female OF/1 outbred mice (Iffa Credo, l'Arbresle, France) were used for virulence and immunization experiments. The 50% lethal dose (LD50) corresponding to the dose of spores killing half the animals was determined in mice (10 per dose) by subcutaneous injection of mutant strains, as previously described (25). Animals were immunized with 1 × 108 to 2 × 108 spores. Sera were taken from the retroorbital plexus 35 days after injection, as previously described (27). The titers of antibodies (total immunoglobulin) specific for the purified PA and LF toxin components were determined by enzyme-linked immunosorbent assay (ELISA) as previously described (27). Edema formation was assessed by infecting groups of five mice by injection of 5 × 108 spores (in a volume of 50 μl) into the right hind footpad. The size of the footpad edema was measured at intervals with dial callipers (Schnelltaster, Hessen, Germany) and compared with that of the contralateral, noninfected footpad. In the protection experiments, groups of 10 mice injected with 108 spores of the recombinant strains to be tested were challenged subcutaneously 35 days after immunization with 2 × 103 or 2 × 104 spores per animal of the virulent capsulated strain 17JB (4 and 40 times the LD50, respectively).
Statistics.
All statistical analyses were performed using Student's unpaired t test.
RESULTS
Construction and characterization of B. anthracis strains mutated in the pag, lef, and cya genes.
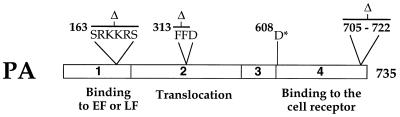
B. anthracis recombinant strains carrying mutations that have been shown in cellular models (i) to disrupt selectively the functional domains of PA (Fig. 1) and (ii) to knock out the biological activities of LF and EF were constructed. LF686 (H686→A) and EF346/353 (K346→Q and K353→Q) totally lack metalloprotease and adenylate cyclase activities respectively (13, 14, 42). PA proteins with deletions of the carboxy-terminal domain (PA608) or of the loop within this domain (PA705) are impaired in binding to the target cell receptor (4). Deletions of the S163RKKRS (PA163) and F313FD (PA313) sequences prevent the binding of EF and LF to PA63 and their translocation into the cytoplasm, respectively (30, 32). We have also shown that PA608, PA313, and PA163, in combination with LF, do not kill Fischer 344 rats after intravenous injection, whereas wild-type Letx is lethal within 45 min (1, 3).
FIG. 1.
Schematic representation of the mutagenesis of PA. PA (residues 1 to 735) is shown without its leader peptide. The four folding domains, according to the crystal structure, are represented by rectangles and are numbered (24). The positions of short in-frame deletions (Δ) and of the stop codon (∗) are indicated.
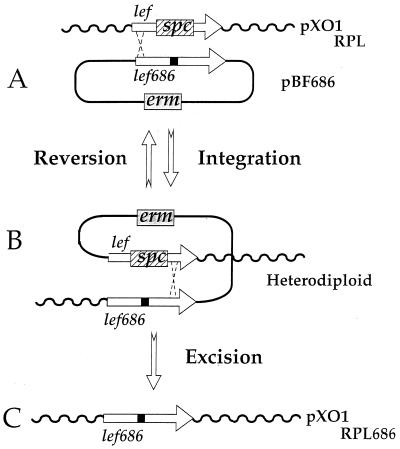
We designed a strategy for substituting the wild-type toxin genes for corresponding mutated genes on pXO1 plasmid of the Sterne strain (Table 1). The construction of the RPL686 strain is presented as an example in Fig. 2. The suicide plasmid, pBF686, conferring resistance to erythromycin and containing the lef gene mutated at codon 686 (lef686), was introduced by heterogramic mating into B. anthracis RPL. This strain carries a spectinomycin resistance cassette replacing the deleted fragment from the lef gene (Fig. 2A) (Table 1). The integration of pBF686 into pXO1 by a single crossover event was selected by growing the heterodiploid strains on agar medium containing both spectinomycin and erythromycin (Fig. 2A to B). The heterodiploids were then cultured in the absence of antibiotic selection pressure, thereby facilitating a second crossover. This process resulted in either a reversion event (Fig. 2B to A) or in the expected B. anthracis recombinants (Fig. 2B to C). As the gene disruption in the RPL strain encompasses the codon at position 686, the bacteria that became susceptible to antibiotics did so due to allelic exchange of the disrupted lef gene for a lef686 mutated copy. Thus, RPL686 (Fig. 2C) was isolated as a strain sensitive to erythromycin and spectinomycin and was shown to harbor the lef686 allele by sequence analysis. The RPL686 strain was therefore isogenic to the Sterne strain except for the nucleotide changes at position 686 in the lef gene. The same strategy was used to construct the other isogenic Sterne strains mutated in the various domains of toxin components (Table 1).
FIG. 2.
Schematic representation of the production of the B. anthracis RPL686 mutant. (A) The integrative plasmid, pBF686, carrying an erythromycin resistance cassette (erm) and the lef686 toxin gene, was integrated into the pXO1 of the RPL strain. This strain has a lef deletion and a spectinomycin resistance cassette (spc) insertion (Table 1). (B) The resulting heterodiploid clone was grown in the absence of antibiotic selection pressure. We screened for a second crossover resulting in either the expected allelic exchange (B to C) or a reversion event (B to A). The black square indicates the point mutation (H686→A) in lef686.
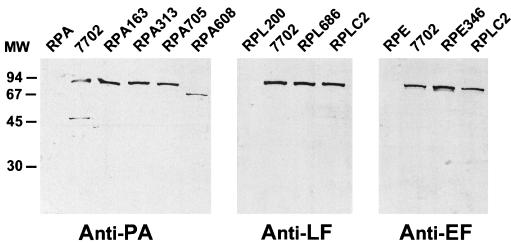
The various recombinant strains were grown in R medium supplemented with bicarbonate to induce the synthesis of toxin components. The secreted proteins were analyzed by Western blotting by using monoclonal antibodies specific for PA, EF, and LF (Fig. 3). The apparent molecular masses of the proteins detected were as expected (83 kDa for PA, PA705, PA313, and PA163; 70 kDa for PA608; 89 kDa for EF and EF346/353; and 85 kDa for LF and LF686). These results confirm that the mutated toxin genes, integrated at their corresponding locus on pXO1, are regulated similarly to their wild-type counterparts. Thus, the mutated toxins should be produced in vivo in quantities similar to those of the wild-type strain.
FIG. 3.
In vitro characterization of B. anthracis recombinant strains. The B. anthracis recombinants were grown in R medium for toxin production. Supernatants from 500 μl of culture were analyzed by sodium dodecyl sulfate-polyacrylamide gel electrophoresis and Western blotting with PA-, LF-, and EF-specific monoclonal antibodies. MW, molecular weight in thousands.
Pathogenic effects of the B. anthracis mutant strains.
B. anthracis spores were injected into Swiss mice, and the number of deaths and edema formation were monitored. The effects of a functional lethal toxin were assessed by determination of the LD50 (Table 2). As previously described, strains that did not produce Letx following disruption of either the lef (RPL200) or pag (RPA) gene were unable to kill the animals (LD50 > 109 spores) (25). The recombinant B. anthracis producing either the metalloprotease site knockout LF686 (RPL686 and RPLC2) or the PA mutants, PA608, PA163, and PA313 (RPA608, RPA163, and RPA313), did not kill mice (LD50 > 109 spores). Only RPA705, which produces the PA molecule truncated in the domain 4 loop, killed animals, although it was much less virulent (LD50 = 5 × 108 spores) than the parental Sterne strain (LD50 = 105 spores). Therefore, the functional domains of PA and the metalloprotease site of LF defined in vitro were required for lethality in the mice model. The LD50 of strains producing Letx in the absence of EF (RPE) or in the presence of the inactive Edtx (RPE346) was 100 times higher than that of the parental Sterne strain, indicating a synergic effect of Edtx on Letx-induced lethality.
TABLE 2.
Lethality and immunogenicity of B. anthracis mutant strains
| Strain | Toxin components produced
|
LD50a | Antibody titer in response tob:
|
|||
|---|---|---|---|---|---|---|
| PA | EF | LF | PA | LF | ||
| Sterne | PA | EF | LF | 105 | ND | ND |
| RPE | PA | LF | 107 | ND | ND | |
| RPE346 | PA | EF346/353 | LF | 107 | ND | ND |
| RPL200 | PA | EF | >109 | 1,750 | <10 | |
| RPL686 | PA | EF | LF686 | >109 | 7,000 | 1,600 |
| RPLC2 | PA | EF346/353 | LF686 | >109 | 2,400 | 1,055 |
| RPA | EF | LF | >109 | <10 | 50 | |
| RPA163 | PA163 | EF | LF | >109 | 2,160 | 110 |
| RPA313 | PA313 | EF | LF | >109 | 5,500 | 4,300 |
| RPA705 | PA705 | EF | LF | 5 × 108 | 4,100 | 4,500 |
| RPA608 | PA608 | EF | LF | >109 | 140 | 1,880 |
Spores per animal.
Titers of antibodies against PA or LF were determined by ELISA. The values given are the reciprocal geometric mean titers of serum for 10 Swiss mice. ND, not determined.
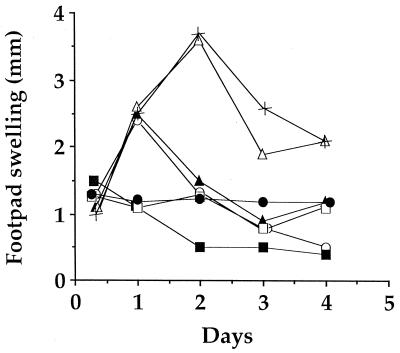
Edema was monitored by measuring the swelling of the footpads at intervals after the injection of the spores. The Sterne and RPA705 strains induced a persistent edema that lasted 4 days and was maximal after 48 h (Fig. 4). The adenylate cyclase site knockout Edtx-producing strain (RPE346), like the EF-deficient strain (RPE), did not cause an edema. The strain producing Edtx in absence of Letx (RPL200) induced an edema that regressed after 48 h. A similar transient edema was also observed for the strain producing Edtx in the presence of Letx deficient in metalloprotease activity (RPL686). The formation of an edema in vivo therefore requires the production of active Edtx. The persistence of the edema is, however, also dependent on the metalloprotease activity of Letx.
FIG. 4.
Edema formation induced by B. anthracis mutants in mice footpads. Groups of five mice were injected in the right footpad with 5 × 108 spores from various B. anthracis strains. Strains: 7702 (×), RPL200 (○), RPL686 (▴), RPE (□), RPE346 (●), RPLC2 (■), and RPA705 (▵). Swelling was monitored at intervals by measuring, three times for each mouse, the thickness of the infected footpad relative to the contralateral footpad.
Antibody response to PA and LF.
The antibody response to LF after immunization with mutant B. anthracis strains is dependent on the production of PA (27). LF-specific antibody titers are significantly higher if PA is also produced by the bacterium. We thought that this adjuvant effect might be mediated by the interaction between PA and LF. To elucidate the molecular mechanisms underlying this phenomenon, we immunized mice with a single dose of 108 spores of the various nonlethal B. anthracis mutants and of the strain RPA705 (LD50 = 5 × 108 spores). The titers of antibodies directed against PA and LF were determined by ELISA (Table 2). The involvement of LF-metalloprotease activity in the immune process could be ruled out because a strong antibody response to LF was also observed with the LF686-producing strain. The response to PA was high in all strains except the one producing PA608, in which the whole of domain 4 was deleted. The titers of antibodies against LF were low, both with the strain deficient in PA (RPA) and with strain RPA163, which produces a PA molecule resistant to protease cleavage and consequently deficient in LF binding. The titers of induced antibodies against LF and LF686 were higher in all other strains (P < 0.02). This was also true for strain RPA608, which produced the C-terminal truncated PA. Since the binding of PA to the cell surface receptor was not required for the potentiation of the LF-specific response, these experiments strongly suggest that, in vivo, the processed PA and LF molecules were able to associate before any interaction with the target cells.
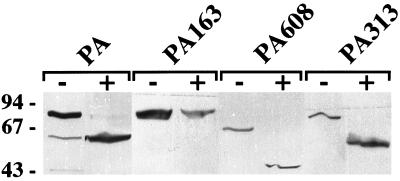
We analyzed the cleavage of PA mutants in mice sera. Ezzell and Abshire showed that wild-type PA is processed by a calcium-dependent, heat-labile serum protease, allowing the subsequent binding of LF (8). Incubation of wild-type PA with serum yielded the 63-kDa form produced by cleavage of the molecule at the furin-sensitive site (Fig. 5). The same processing was observed with the mutant PA313 protein, which is unable to translocate LF and EF. PA608, unable to bind to the cell surface, was also processed, giving a protein of similar size to that observed after in vitro cleavage with trypsin (4). In contrast, no cleavage occurred if PA163, in which the furin-sensitive site is deleted, was incubated with serum. It therefore seems that wild-type PA, PA313, and PA608 are processed in serum during infection and bind LF, which accounts for the strong antibody response against LF induced by the RPA608 strain.
FIG. 5.
Cleavage of wild-type and mutant PA proteins in serum. PA proteins (100 ng per sample) were incubated for 60 min at 37°C with (+) or without (−) mouse serum. The samples were then subjected to electrophoresis, and the PA proteins were detected by Western blotting by using polyclonal antibodies specific for PA.
Protection of mice with mutant strains.
The protection afforded by the strains RPLC2 and RPA608 against a lethal challenge with the virulent capsulated strain, 17JB, was tested in mice. Animals were immunized once with 108 spores and were challenged 35 days later with 40 LD50 of 17JB. A 100% protection was observed in mice immunized with the RPLC2 strain, whereas only 60% of those immunized with RPA608 survived this challenge. The survival rate increased to 80% if the challenge was performed with fewer spores (4 LD50). In contrast, in animals immunized with the PA-deficient strain, RPA, protection was not even observed, when the challenge was performed with lethal doses of the attenuated Sterne strain.
DISCUSSION
We studied the role of functional domains of toxin components in anthrax pathogenesis and immune responses. A genetic strategy was developed in which the marker, knockout mutant genes were replaced by alleles carrying mutations specifically affecting toxin component activities. These B. anthracis mutant strains were devoid of antibiotic markers and were isogenic to the parental Sterne strain, except for the selected mutation. Analysis of the pathogenic effects of these strains made it possible to evaluate the in vivo significance of current knowledge about the structural and functional organization of anthrax toxins. Point mutations affecting the enzyme activities of EF and LF were sufficient to abolish edema and lethality, as observed with strains RPE346/353 and RPL686, respectively. The properties of these strains provided insight into the synergy between Letx and Edtx. Such synergy has been reported in previous studies on the action of toxin components in animals (33) and in in vivo studies conducted with toxin mutants (25). The EF- and LF-deficient strains were less effective at causing death and edema, respectively, than the parental EF-LF-producing strain. This was also observed in this work, with the mutants producing inactive EF346/353 and LF686 molecules. Since these strains are isogenic to the Sterne strain, it is likely that synergy directly involves toxin activities and does not reflect a side effect due to a difference in toxin component ratios. Thus, toxins probably act together within the host.
The RPA163 and RPA313 strains had no pathogenic effects. It is therefore likely that (i) the furin-cleavage RKKR site of PA is the only sequence the cleavage of which results in the formation of lethal and edema toxins in vivo and (ii) the FFD sequence of PA is required for LF and EF activities within host target cells. This demonstrates the importance of these sequences in the infectious process and indicates that the processing of PA at these sites cannot be bypassed in vivo. Deletion of the exposed loop of domain 4 of PA has been shown to impair the binding of the molecule to its cell receptor (4). Strain RPA705, which produces such a mutant protein, was much less virulent than the Sterne strain, with an LD50 5,000 times higher, demonstrating the significance of the loop in pathogenesis.
New insight was obtained into the mechanisms involved in the adjuvant effect of PA by studying the immune response conferred by the various mutant strains. The titer of antibody against LF induced by the RPLC2 strain, which produces inactive Letx and Edtx, was significantly higher than that obtained with the PA-deleted strain. This clearly demonstrates that the adjuvant effect of PA in the humoral response against LF is not dependent on the activities of the toxins. In contrast, the adjuvant effect was abolished in the RPA163 strain, which produces a PA protein unable to bind LF. Since the titer of antibody against LF induced by the RPA608 strain, which produces a PA molecule unable to bind to the cell receptor, was also high, it is clear that the adjuvant effect requires the binding of LF to PA in vivo, but not the subsequent binding of the complex to cells. The mutant protein PA608 was shown to be cleaved in mouse sera at the furin-sensitive site. Therefore, PA608 produced in vivo is processed by furin-like proteases present in the serum, enabling it to bind LF. These data provide evidence that the wild-type PA may undergo similar cleavage in serum and bind LF without necessarily interacting with its cell receptor. This type of processing is consistent with previous studies (8) and should be considered in the cellular model of toxin action. The RPA608 strain induced only a weak antibody response against PA, although PA608, which is truncated, seemed to be stable in vivo, as shown by its ability to potentiate the antibody response against LF. These data are consistent also with the partial protection against a virulent capsulated strain observed in mice immunized with RPA608. Therefore, immunodominant protective epitopes may be present in the carboxy-terminal domain of PA that are missing in PA608 or the binding of PA to the cell receptor and the subsequent steps in intracellular trafficking, processing, or presentation of the molecule are required to induce a strong protective humoral response against PA. However, whereas no protection was observed with a PA-deficient strain, RPA608 gave satisfactory protection. This probably reflects the high titer of antibodies against LF and/or the presence of other protective epitopes in the first 608 amino acids of PA. The RPLC2 strain, which is isogenic to the Sterne strain and produces LF and EF with mutations in their catalytic sites, conferred full protection against a lethal challenge with the virulent strain. For the future development of a safe live vaccine against anthrax, this strain is an excellent candidate as a replacement for the Sterne strain currently used in veterinary vaccination.
ACKNOWLEDGMENTS
We thank C. Guidi-Rontani and A. Fouet for critical reading of the manuscript and M. Haustant for excellent technical assistance.
F.B. was supported by the Ministère de l'Enseignement Supérieur et de la Recherche.
REFERENCES
- 1.Beall F A, Taylor M J, Thorne C B. Rapid lethal effects in rats of a third component found upon fractionating the toxin of Bacillus anthracis. J Bacteriol. 1962;83:1274–1280. doi: 10.1128/jb.83.6.1274-1280.1962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bragg T S, Robertson D L. Nucleotide sequence and analysis of the lethal factor gene (lef) from Bacillus anthracis. Gene. 1986;81:45–54. doi: 10.1016/0378-1119(89)90335-1. [DOI] [PubMed] [Google Scholar]
- 3.Brossier F, Guidi-Rontani C, Mock M. Anthrax toxins. C R Soc Biol. 1998;192:437–444. [PubMed] [Google Scholar]
- 4.Brossier F, Sirard J C, Guidi-Rontani C, Duflot E, Mock M. Functional analysis of the carboxy-terminal domain of Bacillus anthracis protective antigen. Infect Immun. 1999;67:964–967. doi: 10.1128/iai.67.2.964-967.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duesbery N S, Webb C P, Leppla S H, Gordon V M, Klimpel K R, Copeland T D, Ahn N G, Oskarsson M K, Fukasawa K, Paull K D, Vande woude G F. Proteolytic inactivation of map-kinase-kinase by anthrax lethal factor. Science. 1998;280:734–737. doi: 10.1126/science.280.5364.734. [DOI] [PubMed] [Google Scholar]
- 6.Escuyer V, Duflot E, Sezer O, Danchin A, Mock M. Structural homology between virulence-associated bacterial adenylate cyclases. Gene. 1988;71:293–298. doi: 10.1016/0378-1119(88)90045-5. [DOI] [PubMed] [Google Scholar]
- 7.Escuyer V, Collier R J. Anthrax protective antigen interacts with a specific receptor on the surface of CHO-K1 cells. Infect Immun. 1991;59:3381–3386. doi: 10.1128/iai.59.10.3381-3386.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ezzell J W, Abshire T G. Serum protease cleavage of Bacillus anthracis protective antigen. J Gen Microbiol. 1992;138:543–549. doi: 10.1099/00221287-138-3-543. [DOI] [PubMed] [Google Scholar]
- 9.Friedlander A M. Macrophages are sensitive to anthrax lethal toxin through an acid-dependent process. J Biol Chem. 1986;261:7123–7126. [PubMed] [Google Scholar]
- 10.Guidi-Rontani C, Duflot E, Mock M. Anthrax lethal toxin-induced mitogenic response of human T-cells. FEMS Lett. 1997;157:285–289. doi: 10.1111/j.1574-6968.1997.tb12786.x. [DOI] [PubMed] [Google Scholar]
- 11.Guidi-Rontani C, Weber-Levy M, Labruyere E, Mock M. Germination of Bacillus anthracis within alveolar macrophages. Mol Microbiol. 1999;31:9–17. doi: 10.1046/j.1365-2958.1999.01137.x. [DOI] [PubMed] [Google Scholar]
- 12.Klimpel K R, Molloy S S, Thomas G, Leppla S H. Anthrax toxin protective antigen is activated by a cell surface protease with the sequence specificity and catalytic properties of furin. Proc Natl Acad Sci USA. 1992;89:10277–10281. doi: 10.1073/pnas.89.21.10277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klimpel K R, Arora N, Leppla S H. Anthrax toxin lethal factor contains a zinc metalloprotease consensus sequence which is required for lethal toxin activity. Mol Microbiol. 1994;13:1093–1100. doi: 10.1111/j.1365-2958.1994.tb00500.x. [DOI] [PubMed] [Google Scholar]
- 14.Labruyère E, Mock M, Surewick W K, Mantsch H H, Rose T, Munier H, Sarfati R S, Barzu O. Structural and ligand-binding properties of a truncated form of Bacillus anthracis adenylate cyclase and of a catalytically inactive variant in which glutamine substitutes for lysine-346. Biochemistry. 1991;30:2619–2624. doi: 10.1021/bi00224a008. [DOI] [PubMed] [Google Scholar]
- 15.Leppla S H. Anthrax toxin edema factor: a bacterial adenylate cyclase that increases cyclic AMP concentrations in eukaryotic cells. Proc Natl Acad Sci USA. 1982;79:3162–3166. doi: 10.1073/pnas.79.10.3162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leppla S H. Production and purification of anthrax toxin. Methods Enzymol. 1988;165:103–116. doi: 10.1016/s0076-6879(88)65019-1. [DOI] [PubMed] [Google Scholar]
- 17.Little S F, Novak J M, Lowe J R, Leppla S H, Singh Y, Klimpel K R, Lidgerding B C, Friedlander A M. Characterization of lethal factor binding and cell receptor binding domains of protective antigen of Bacillus anthracis using monoclonal antibodies. Microbiology. 1996;142:707–715. doi: 10.1099/13500872-142-3-707. [DOI] [PubMed] [Google Scholar]
- 18.Mikesell P, Ivins B E, Ristroph J D, Dreier T M. Evidence for plasmid-mediated toxin production in Bacillus anthracis. Infect Immun. 1983;39:371–376. doi: 10.1128/iai.39.1.371-376.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Milne J C, Collier R J. pH-dependent permeabilization of the plasma membrane of mammalian cells by anthrax protective antigen. Mol Microbiol. 1993;10:647–653. doi: 10.1111/j.1365-2958.1993.tb00936.x. [DOI] [PubMed] [Google Scholar]
- 20.Milne J C, Furlong D, Hanna P C, Wall J S, Collier R J. Anthrax protective antigen forms oligomers during intoxication of mammalian cells. J Biol Chem. 1994;269:20607–20612. [PubMed] [Google Scholar]
- 21.Mock M, Labruyère E, Glaser P, Danchin A, Ullmann A. Cloning and expression of the calmodulin-sensitive Bacillus anthracis adenylate cyclase in Escherichia coli. Gene. 1988;64:277–284. doi: 10.1016/0378-1119(88)90342-3. [DOI] [PubMed] [Google Scholar]
- 22.Murphy E, Huwyler L, de Freire Bastos C M. Transposon Tn544: complete nucleotide sequence and isolation of transposition-defective and antibiotic-sensitive mutants. EMBO J. 1985;4:3357–3365. doi: 10.1002/j.1460-2075.1985.tb04089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Novak J M, Stein M P, Little S F, Leppla S H, Friedlander A M. Functional characterization of protease-treated Bacillus anthracis protective antigen. J Biol Chem. 1992;267:17186–17193. [PubMed] [Google Scholar]
- 24.Petosa C, Collier R J, Klimpel K R, Leppla S H, Liddington R C. Crystal structure of the anthrax toxin protective antigen. Nature. 1997;385:833–838. doi: 10.1038/385833a0. [DOI] [PubMed] [Google Scholar]
- 25.Pezard C, Berche P, Mock M. Contribution of individual toxin components to virulence of Bacillus anthracis. Infect Immun. 1991;59:3472–3477. doi: 10.1128/iai.59.10.3472-3477.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pezard C, Duflot E, Mock M. Construction of Bacillus anthracis mutant strains producing a single toxin component. J Gen Microbiol. 1993;139:2459–2463. doi: 10.1099/00221287-139-10-2459. [DOI] [PubMed] [Google Scholar]
- 27.Pezard C, Weber M, Sirard J C, Berche P, Mock M. Protective immunity induced by Bacillus anthracis toxin-deficient strains. Infect Immun. 1995;63:1369–1372. doi: 10.1128/iai.63.4.1369-1372.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ristroph J D, Ivins B E. Elaboration of Bacillus anthracis antigens in a new, defined culture medium. Infect Immun. 1983;39:483–486. doi: 10.1128/iai.39.1.483-486.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sambrook J, Fritsch E F, Maniatis T. Molecular cloning: a laboratory manual. 2nd ed. Cold Spring Harbor, N.Y: Cold Spring Harbor Laboratory; 1989. [Google Scholar]
- 30.Singh Y, Chaudhary V K, Leppla S H. A deleted variant of Bacillus anthracis protective antigen is non-toxic and blocks anthrax toxin action in vivo. J Biol Chem. 1989;264:19103–19107. [PubMed] [Google Scholar]
- 31.Singh Y, Klimpel K R, Quinn C P, Chaudhary V K, Leppla S H. The carboxyl-terminal end of protective antigen is required for receptor binding and anthrax toxin activity. J Biol Chem. 1991;266:15493–15497. [PubMed] [Google Scholar]
- 32.Singh Y, Klimpel K R, Arora N, Sharma M, Leppla S H. The chymotrypsin-sensitive site, FFD(315), in anthrax toxin protective antigen is required for translocation of lethal factor. J Biol Chem. 1994;269:29039–29046. [PubMed] [Google Scholar]
- 33.Stanley J L, Smith H. Purification of factor I and recognition of a third factor of anthrax toxin. J Gen Microbiol. 1961;26:49–66. doi: 10.1099/00221287-26-1-49. [DOI] [PubMed] [Google Scholar]
- 34.Thomas C M, Smith C A. Incompatibility group p pasmids: genetics, evolution, and use in genetic manipulation. Annu Rev Microbiol. 1987;41:77–101. doi: 10.1146/annurev.mi.41.100187.000453. [DOI] [PubMed] [Google Scholar]
- 35.Trieu-Cuot P, Courvalain P. Nucleotide sequence of the Streptococcus faecalis plasmid gene encoding the 3′,5′-aminoglycoside phosphotransferase type III. Gene. 1983;23:331–341. doi: 10.1016/0378-1119(83)90022-7. [DOI] [PubMed] [Google Scholar]
- 36.Trieu-Cuot P, Carlier C, Poyart-Salmeron C, Courvalin P. Nucleotide sequence of the erythromycin resistance gene of the conjugative transposon Tn1545. Nucleic Acids Res. 1990;18:3660. doi: 10.1093/nar/18.12.3660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Trieu-Cuot P, Poyart-Salmeron C, Carlier C, Courvalain P. An integrative vector exploiting the transposition properties of Tn1545 for insertional mutagenesis and cloning genes from gram-positive bacteria. Gene. 1991;106:21–27. doi: 10.1016/0378-1119(91)90561-o. [DOI] [PubMed] [Google Scholar]
- 38.Uchida I, Hashimoto K, Terakado N. Virulence and immunogenicity in experimental animals of Bacillus anthracis strains harbouring or lacking 110 MDa and 60 MDa plasmids. J Gen Microbiol. 1986;132:557–559. doi: 10.1099/00221287-132-2-557. [DOI] [PubMed] [Google Scholar]
- 39.Varughese M, Teixeira A V, Liu S, Leppla S H. Identification of a receptor-binding region within domain 4 of the protective antigen component of anthrax toxin. Infect Immun. 1999;67:1860–1865. doi: 10.1128/iai.67.4.1860-1865.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vitale G, Pellizzari R, Recchi C, Napolitani G, Mock M, Montecucco C. Anthrax lethal factor cleaves the N-terminus of MAPKKs and induces tyrosine/threonine phosphorylation of MAPKs in cultured macrophages. Biochem Biophys Res Commun. 1998;248:706–711. doi: 10.1006/bbrc.1998.9040. [DOI] [PubMed] [Google Scholar]
- 41.Vodkin M H, Leppla S H. Cloning of the protective antigen gene of Bacillus anthracis. Cell. 1983;34:693–697. doi: 10.1016/0092-8674(83)90402-6. [DOI] [PubMed] [Google Scholar]
- 42.Xia Z, Storm D R. A-type ATP binding consensus sequences are critical for the catalytic activity of the calmodulin-sensitive adenylyl cyclase from Bacillus anthracis. J Biol Chem. 1990;265:6517–6520. [PubMed] [Google Scholar]