Abstract
There is a bidirectional relationship between climate change and health care. Climate change threatens public health, and health care contributes to climate change. For example, surgery is the most energy-intensive practice in the health-care sector, and gastrointestinal conditions are responsible for a substantial environmental burden. However, environmental costs associated with health care are often overlooked. This issue has been examined more closely in current times. Emerging data are mainly focused on surgery, as the most resource-intensive practice. However, there is still a lack of global awareness and guidance on sustainable surgical practices. This Perspective aims to reassess the evidence on health care and surgery carbon footprints, focusing on gastrointestinal conditions, identify issues that need to be addressed to achieve a more sustainable practice and develop perspectives for future surgical procedures. The proposed framework to mitigate the environmental effects of surgery could be translated to other health-care sectors.
Subject terms: Surgery, Gastroenterology
Health care contributes to the climate change burden, and measures should be taken to mitigate these effects. This Perspective discusses the carbon footprint of surgery in gastroenterology and hepatology and offers an overview of sustainable strategies.
Introduction
Climate change is one of the greatest threats to public health worldwide. The association of air pollution, rising temperatures, flooding and drought with changes in the spread of vector diseases presents a risk to humanity1. Also, the health-care sector is one of the largest waste-generating entities contributing to climate change. For example, in the USA, health care produces 655 million tons of carbon dioxide equivalent (CO2e) per year, representing 8–10% of all national greenhouse gas emissions1.
Among health-care sectors, operating theatres are the most energy-intensive sites, three to six times more energy intensive than the rest of the hospital, greatly contributing to this environmental burden1,2. Thus, achieving sustainability in surgery is emerging as a strategy to reduce environmental effects3. Data on the surgical carbon footprint are emerging1,4. However, there have been insufficient efforts to address this problem5. Finally, gastrointestinal diseases are one of the world’s largest therapeutic areas and represents a heavy global burden. Peery et al.6 showed that, annually, in the USA, there are more than 43.4 million ambulatory visits and 3.8 million hospitalizations due to a primary gastrointestinal diagnosis. Moreover, 284,844 new gastrointestinal cancers were diagnosed in 2019. The diagnosis of gastrointestinal diseases and their advanced management substantially affect the generation of health-associated waste and the consumption of environmental resources7–9.
This Perspective aims to reassess the evidence on health care, the carbon footprint of surgery and gastrointestinal diseases, identify issues that need to be addressed to achieve more sustainable practice and develop strategies for more environmentally friendly surgery and gastrointestinal practice.
Climate change effects on health
Health promotion remains a development goal defined by the WHO10. Health professionals are crucial to this health promotion path, working directly with patients, from health centres to university hospitals. However, health facilities are greatly responsible for greenhouse gas emissions and global warming, directly related to health-promoting strategies and diseases10. Climate change affects public health, and the environmental footprint deserves all our attention with regard to health promotion development.
Global warming affects health in several ways. For example, over the past 20 years, high temperatures and heat waves have been responsible for a global 53.7% increase in heat-related mortality in people older than 65 years, owing to the exacerbation of cardiovascular and respiratory diseases10,11. In addition, climate change represents the ideal setting for spreading viral, bacterial and vector-borne infections12–14. Since the 1950s, there has been a higher incidence and broader distribution of dengue, malaria and Vibrio bacterial infections12,13 As an example, the worldwide incidence of dengue has increased 30-fold over the past 50 years14, and the daily mean temperature, temperature variation and precipitation extremes are considered the most important drivers14.
However, the effect of climate change on gastrointestinal diseases seems to go beyond the global warming and infectious diseases tie-up. Seo et al.15 developed a mathematical model using meteorological factors and air pollutants obtained from eight metropolitan areas and showed a significant correlation between air pollutants such as carbon monoxide and gastro-oesophageal reflux disease (GERD), according to data from the GERD-related medical care utilization of the Korean National Health Insurance Service between 2002 and 2007 (r2 = 0.22; P < 0.001).
Undernutrition due to challenges with food production and the mental health effects of floods and droughts are also outcomes of the emerging global warming crisis in China, Bangladesh, Ethiopia and South Africa16,17.
Regarding pregnancy and obstetric outcomes, a 2020 systematic review, with 68 studies from the USA that analysed 32,798,152 births, concluded that air pollution and high-temperature exposure increased the risk of low birth weight and preterm labour18. These factors can exacerbate asthma in children, as confirmed in two studies with 990 and 315 children19–21. In addition, Fecht et al.22 observed higher rates of cardiac arrest and emergency admissions for stroke and asthma on days of high air pollution in England. Research in this field is emerging, and it is anticipated that more health outcomes due to climate change will be observed soon10. Consequently, WHO predicts that by 2030, there might be 250,000 additional deaths globally per year due to climate change23,24.
Carbon footprint definitions
Harmonization of the definitions and technical aspects of climate change and carbon footprint is crucial because it enables researchers to share the same language across different sectors. For example, if one aims to analyse the overall carbon footprint of rectal cancer diagnostic work-up, it is necessary to account for endoscopies, CT and magnetic resonance scans. However, it will not be easy to reach this understanding if the effect of these diagnostic procedures is measured in different units. On the other hand, if their functional units were converted into the CO2e (ref.25) standard metric, adequate comparisons and summing could be performed. Most typically, CO2e emission is obtained by multiplying the emission of a greenhouse gas by its global warming potential for a 100-year time horizon. However, there are several ways to compute such equivalent emissions and choose appropriate time horizons25. Thus, different entities have defined carbon footprint methods of estimation. Wiedmann and Minx26 elaborated on these different methods and the associated methodological issues. For example, one can use a process analysis developed to understand the environmental impact of a product’s life cycle, an environmental input–output analysis that combines environmental data and economic data or a hybrid approach, integrating the two methods. The method of choice will depend on the investigator’s aim and data availability26.
The Intergovernmental Panel on Climate Change guidelines define greenhouse gases as “gaseous atmosphere constituents that absorb and emit radiant energy within the thermal infrared range”, responsible for the greenhouse gas effect27. The term ‘carbon footprint’ was also defined as “the greenhouse gas produced by activities of an organisation measured in units of CO2e”10,25. Thus, the carbon footprint is an objective measure of the greenhouse gas emissions “emitted into the atmosphere by an individual, organisation, process, product, or event” measured in CO2e (refs.25,28). However, the carbon footprint measurement is not limited to quantification of greenhouse gases. Life-cycle assessments are part of this complex process because both the product and its production and disposal have an environmental effect19. Life-cycle assessments integrate a ‘cradle to grave’ analysis, including material manufacturing, transport, decontamination (for reusable products) and disposal3. Familiarity with these definitions is crucial for understanding the effect of various sectors on the environment and identifying measures that can mitigate this impact (Box 1).
Box 1 Definitions and nomenclature commonly used to characterize climate change and measure its impact.
Greenhouse gas: gaseous constituents in the atmosphere that absorb and emit radiant energy within the thermal infrared range
Carbon dioxide equivalent (CO2e): a standard metric used to compare the emissions from various greenhouse gases based on their global warming potential over a specified timescale to express a carbon footprint
Carbon footprint: an objective measure of the quantity of greenhouse gas emissions emitted into the atmosphere by an individual, organization, process, product or event measured in CO2e
Life-cycle assessments: methodological and detailed ways to assess the financial cost and environmental impact of a product from its production until its disposal
Health-care carbon footprint
Impact of the health-care sector on global carbon footprint
Climate change substantially affects public health and constitutes a barrier to health promotion. However, in the past few years, attention has been drawn to the effect of the health-care sector on climate change. Globally, the health-care sector was responsible for 4.6% of global greenhouse gas emissions in 2017 (ref.10). However, the figures might be higher per territory. For example, the health-care sector in the UK accounts for approximately 6% of the country’s total CO2e emissions29; Australia’s health-care contribution is 7%; the health-care sector of the USA represents nearly 10% of the country’s total CO2e emissions29,30. Importantly, these estimates are not yet available for many territories, and the figures are getting higher. In the USA, for example, greenhouse gas emissions have increased by more than 30% over the past decade compared with the the country’s previous emissions31.
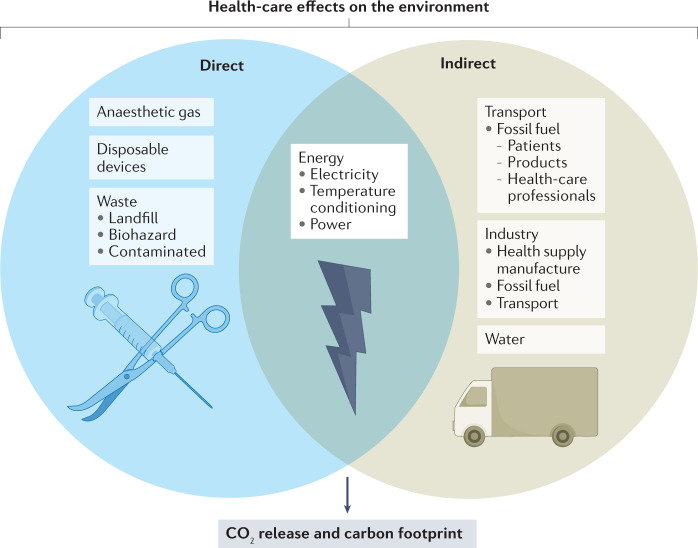
The sources of these emissions can be directly related to health-care activities, representing 17% of the sector’s worldwide carbon footprint; to indirect emissions related to energy consumption (electricity, temperature conditioning and power), representing approximately 12% of the health-care sector’s footprint; and to the health-care chain supply (energy, transport, use and disposal of materials), representing approximately 71% of the total emissions worldwide30,32,33. Finally, the use of goods and services, such as pharmaceuticals and medical devices, cannot be ignored because manufacturing is also energy demanding30 (Fig. 1).
Fig. 1. Health-care impact on the environment.
Health-care directly contributes to climate change. This contribution comes from various vectors. Anaesthetic gases, waste generation and disposable devices are considered direct vectors. Energy use, such as electricity and temperature conditioning, also contributes to the carbon footprint of health care. Indirect vectors, such as fossil fuel used for transport of patients and health-care providers and the life-cycle assessment of the health supply manufacture (such as its production, including transportation and water use), are all contributors to this environmental effect. CO2, carbon dioxide.
Surgical carbon footprint
Hospitals are considered the second most energy-intensive buildings in the USA30,34. Unsurprisingly, although operating theatres represent a small area in the hospital, they are more energy intensive than clinical wards and generate 50–70% of total hospital clinical waste2. Indeed, in the USA, operating theatres are the most resource-intensive practice in the health-care sector35. For example, one surgical procedure generates the same amount of waste as a family of four weekly in the USA36. In addition, most operating theatres are ready to serve 24 h a day, 7 days per week. Maintaining this activity level requires lighting, heating, ventilation and strict air conditioning settings1. These requirements account for up to 40% of global health-care emissions19,37.
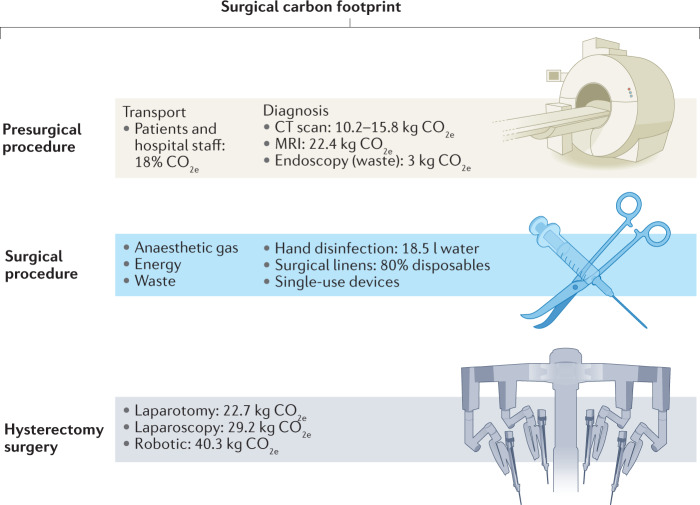
The surgical pathway can be further divided into pre-procedure and intraprocedural timetables to determine the surgical carbon footprint and identify potentially approachable issues to address its environmental burden (Fig. 2).
Fig. 2. Surgical carbon footprint.
Surgical environmental impact can be evaluated before, during and after surgery. Patient and staff transport is responsible for 18% of all health-care emissions. The diagnostic work-up before surgery accounts for a significant impact driven by CT scans, MRI and endoscopy. During surgery, there are multiple vectors to consider: water waste due to hand disinfection; anaesthetic gases are responsible for 40% of ‘surgical emissions’; operating theatre energy and temperature conditioning; disposable surgical linens; and single-use devices. Moreover, different surgical approaches have different carbon footprints. Data on hysterectomy show that laparotomy has a lesser carbon footprint, followed by laparoscopy and robotics. CO2e, carbon dioxide equivalent.
Before the surgical procedure
The first step in this pathway is transfer of the patient and staff to the hospital. In England, this journey occurs by public transport in only a minority of cases and accounts for up to 18% of the CO2e health-care emissions38.
Before surgery, the patient usually needs to undergo a diagnostic work-up for which the carbon footprint is often substantial. For example, if a patient needs CT, the environmental footprint will be 10.2–15.8 kg CO2e per patient39. By contrast, the carbon footprint for MRI is 22.4 kg CO2e per patient40. Finally, endoscopies are procedures with considerable environmental effects owing to waste generation, accounting for approximately 3.09 kg of waste per bed per day, which is equivalent to 3 kg CO2e (ref.41). In addition, the use of disposable equipment, the decontamination process of reusable scopes and patient travel should be added to the endoscopic environmental burden42 (Fig. 2).
During the surgical procedure
After the diagnostic work-up, the patient arrives at the operating theatre, and anaesthesia is the first vector for analysis. The current data show that an anaesthetic plan can considerably affect the environment. Inhaled anaesthetic agents are mainly expired and are released directly into the atmosphere. These gases (sevoflurane, isoflurane and desflurane) are potent greenhouse gases19,43,44. A study that compared the carbon footprint of inhaled agents and propofol concluded that desflurane had the highest footprint, 15 times greater than isoflurane and 20 times greater than sevoflurane. Furthermore, 80% of all volatile anaesthetic pollution results from desflurane29,45. Importantly, propofol had the lowest carbon footprint. Regarding global warming potential, desflurane has a global warming potential of 2,540 (that is, 1 g of desflurane has the same global warming potential as 2,540 g of CO2), sevoflurane 130 and isoflurane 510 (ref.29).
Surgical hand disinfection traditionally requires 18.5 l of water46. Current guidelines recommend using water with antiseptic in the first operating theatre procedure and alcohol gel in subsequent procedures47. Adopting these recommendations could save water and reduce costs48. After hand disinfection, one must consider surgical linens such as gowns, drapes and table covers. Despite the availability of reusable ones, disposables (single-use) are more commonly used worldwide49.
Finally, for the surgery itself, surgical packs of sterile instruments are frequently opened before surgery begins50. Eighty per cent of surgical solid waste is generated before the patient enters the operating theatre, and most of this waste is associated with packaging51,52. There is a lack of robust evidence on how much waste could be avoided if sterile pack openings were delayed until the start of surgery. The introduction of minimally invasive surgery over the past 20 years has brought undeniable benefits to patients53. However, this type of surgery involves more single-use instruments (disposables)54, mistakenly viewed as a more economical choice, and all hidden costs (for example, disposal, loss of resources when a not-needed device is opened, maintaining a high-volume inventory) are often skipped54. Infection control is one of the premises used to justify use of single-use instruments. However, the data show that the infection rates are comparable to those with reusable instruments5,55. In a study with 100 patients submitted to appendectomy using reusable or single-use instruments, the infection rates were similar (2% in each group; P = 0.536)56. In addition, when the environmental effects and costs are accounted for, the negative effect of single-use instruments on the environment is evident5,57. Notably, a multicentre audit in the UK concluded that 40% of the waste generated in operating theatres was potentially recyclable58. However, operating theatre recycling is not largely applied59.
Studies have broadly examined minimally invasive surgery. Laparoscopic and robotic approaches are associated with higher carbon footprints than the open approach. Woods et al.60 concluded that an abdominal hysterectomy performed using an open approach (laparotomy) accounted for 22.7 kg CO2e. In comparison, the laparoscopic and robotic procedures were responsible for 29.2 kg CO2e and 40.3 kg CO2e, respectively (Table 1). Notably, data on the effect of different surgical approaches are scarce and limited by not considering all surgical pathways60–62. Evaluating surgical procedures without assessing inpatient days and patient outcomes is reductive from the clinical and environmental perspectives.
Table 1.
Environmental burden of the various processes during the surgical pathway
| Study | Method | Aim | Speciality | Environmental effect measure | Outcome |
|---|---|---|---|---|---|
| Esmaeili et al. (2015)39 | Multicentre, retrospective cohort study | “Provide quantitative information to radiologists so that they can be involved in making energy improvements while maintaining quality patient care.” | Radiology — CT | Life-cycle assessment (energy and consumables), kg CO2e | CT 5.1–7.3 kg CO2e |
| Esmaeili et al. (2018)40 | Multicentre, retrospective cohort study | “Provide a detailed accounting of energy and materials consumed during magnetic resonance imaging (MRI).” | Radiology — MRI | Life-cycle assessment (energy and consumables), kg CO2e | MRI 22.54 kg CO2e |
| Woods et al. (2015)60 | Single-centre, retrospective cohort study | “Our research intends to quantify the carbon footprint of the procedures based on their energy consumed and waste produced.” | Gynaecology — hysterectomy (robotic; laparoscopic; open approach) | Waste and energy, kg CO2e |
Robotics 40.3 kg CO2e Laparoscopic 29.2 kg CO2e Open 22.7 kg CO2e |
| Thiel et al. (2018)127 | Single-centre, prospective cohort study | “To determine the carbon footprint of various sustainability interventions used for laparoscopic hysterectomy.” | Gynaecology — hysterectomy (laparoscopic approach) | Hybrid environmental life-cycle assessment, kg CO2e | Laparoscopic hysterectomy 562 kg CO2e |
| Rizan and Bhutta (2022)61 | Single centre | “Compare the environmental and financial life cycle cost of currently available hybrid instruments for laparoscopic cholecystectomy and compare these to single-use equivalents.” | General surgery; cholecystectomy | Life-cycle assessment of the single-use and non-single-use (hybrid), kg CO2e |
Hybrid: 1,756 kg CO2e Single-use: 7,194 kg CO2e |
| Vaccari et al. (2018)41 | Single-centre, prospective, cohort study | “Understand the nature of the relationship between generation patterns hazardous health-care waste and the associated costs.” | All specialities (anaesthetics, paediatric; ICU; digestive endoscopy) | Amount of hazardous waste, kg |
Anaesthetics 5.96 kg per day per bed ICU 3.37 kg per day per bed Digestive endoscopy 3.09 kg per day per bed |
A summary of articles that measured the environmental effect of diagnostic modalities (CT, MRI and digestive endoscopy), surgical procedures (hysterectomy and cholecystectomy) and surgical approaches (open, laparoscopic and robotic). CO2e, carbon dioxide equivalent; ICU, intensive care unit.
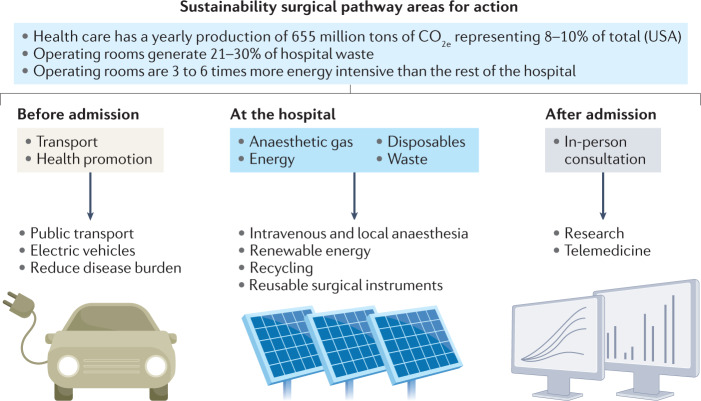
Sustainable surgery
Sustainability applied to health systems is defined by the WHO as a process to “improve, maintain, or restore health while minimizing negative effects on the environment”63–65. As health professionals working in a high-impact field, surgeons should be proactive and openly promote sustainable surgery. Guidance on this pathway was disclosed in 2012 by Kagoma et al.5, focusing on the 5R principles of waste management (reduce, reuse, recycle, rethink and research) to outline solutions to decrease the waste generated in operating theatres5. However, in addition to solutions to decrease waste generation, these principles can be broadly applied as future strategies for more sustainable surgical practice (Fig. 3). The authors of this Perspective believe that the proposed framework to mitigate the environmental effects of surgery could be translated to other fields.
Fig. 3. Areas for action to make the surgical pathway more sustainable.
Before patient admission, health promotion measures and the use of sustainable means of transport by patients, health-care professionals and products are important interventions. At the hospital, using renewable energy sources and optimizing electricity and cooling systems should be considered. During surgery, avoiding anaesthetic gases and promoting intravenous and local anaesthesia can have a remarkable effect. Additionally, reducing disposables and implementing recycling would reduce waste production. Telemedicine represents a good example of how technology can facilitate sustainability. Research and education are important to evaluate the impact of sustainable actions and can help to continue this process across generations. CO2e, carbon dioxide equivalent.
Reduce
The reduction principle can be applied before and beyond surgery. For example, data published in 2015 showed that 143 million additional surgical procedures were required annually to prevent disability66. The calculation was made using “the frequency of operation per WHO Global Health Estimate disease subcategory” and then “the estimated surgical frequency for each disease subcategory to condition prevalence data for each global region” was applied66. Thus, health promotion to reverse these statistics should be the first priority66. Health promotion is a global responsibility that involves patients, caregivers, health professionals and governments. Reducing the disease burden through healthy behaviour could reduce disease-related health-care requirements and surgical demand.
Addressing waste generation in operating theatres could further reduce the surgical carbon footprint. Correct segregation process, recycling59 and reformulating prepackaged surgical kits and instrument boxes (by removing inessential items and plastic components)67 could serve this purpose. A study in the USA on hand surgery showed that these measures alone reduced 2.3 kg of waste and saved US$10.64 per case68. These principles could be further applied to endoscopy units.
Water waste from hand disinfection has already been addressed. According to current international guidelines, water consumption and its direct environmental effect can be easily reduced47,48. Accordingly, after an adequate first hand wash with water, choosing alcohol gel for the second hand wash might reduce water consumption by 2.7 million litres over 1 year67 and reduce costs by 67%69.
Finally, energy consumption should also be addressed. As previously mentioned, operating theatres are the most energy-intensive sector in hospitals. However, operating theatres in northern America are unoccupied up to 40% of the time over a 24 h period5. For example, in Washington State, USA, a hospital reduced energy consumption by 60% by decreasing ventilation output during inactive periods63,70.
Reuse
Reusable surgical linens and instruments are considered to be environmentally friendly. Preferring reusables will lead to less waste generation and reduce landfill and incineration costs. In addition, when all processes are accounted for, from production to sterilization, the reusable carbon footprint remains favourable compared with disposable products57. For example, using reusable surgical devices (port trocars and clip appliers) in laparoscopic cholecystectomy surgery can save approximately 122 kg of waste per case71. Moreover, reusable gowns could lead to a 70% final waste reduction. Currently, reusable gowns are preferred by surgeons and operating theatre technicians, but disposable ones are still broadly used72.
The reprocessing of single-use devices is controversial. Health-care personnel might think reprocessing single-use devices can be associated with an increased infection rate, but this might not be correct36,73. For example, a study of 590 patients that compared reprocessed versus original single-use endolaser probes in ophthalmological surgery (215 versus 375 patients) showed no infections in either group74. In a similar study involving 733 patients submitted to gastrointestinal surgery with original and reprocessed advanced energy devices and gastrointestinal staplers, there was no difference between the infection rates in the two groups (12.9% original and 13.4% reprocessed; P = 0.664)75. However, devices initially labelled as single-use can often be repaired and sterilized, making their reuse safe76. Although reprocessing is not a standard procedure and protocols might differ according to territory36, in 2019, the FDA and the European Commission developed regulations to control in-hospital reprocessing77. Moreover, outsourcing of commercial reprocessing that complies with these regulations is emerging. According to the Association of Medical Device Reprocessors, 5,438,254 kg of medical waste was diverted from incinerators worldwide through remanufactured single-use devices in 2020 (ref.78). Reuse through reprocessing and remanufacturing is expanding and offers environmental and financial benefits. For example, the authorities in the USA support reprocessing under approved conditions. However, reprocessing is not a standard procedure, and protocols differ according to country36,55,79. Thus, awareness and support from the medical device industry are crucial for the broader implementation of this practice36,57.
Recycle
In England, 80% of operating theatre waste is generated preoperatively, 90% is misallocated and 40% is potentially recyclable. Thus, implementing and disseminating the recycling process in the operating theatre and beyond is crucial52,63,80.
However, recycling in the health-care setting presents several challenges. Educating operating theatre staff on waste handling and strict infection control rules will help to overcome the fear of contamination63,81. A cohort study that evaluated the waste generated by 237 operations concluded that recycling is not associated with additional costs and has several advantages if the practice is globally expanded82.
Rethink
Sustainability should be a part of health-care professionals’ practice. Patient health and outcomes will always be the main focus. However, the consequences of climate change on current and future generations must not be ignored, and strategies to address this issue should not be delayed. Rethinking entails selecting the most sustainable choice to treat patients without causing any harm. For example, the American Society of Anaesthesiologists Task Force on the Environment recommended using regional and total intravenous anaesthesia as the most sustainable option (instead of high-impact inhaled anaesthetics such as desflurane and sevoflurane) when clinically appropriate2,59.
The severe acute respiratory syndrome coronavirus 2 pandemic forced us to rethink how we practise medicine. Telemedicine has emerged as an adequate solution that is appropriate for professionals and patients for the follow-up of chronic conditions83–85. This emergency and contingency solution can be maintained in the future when appropriate, as telemedicine reduces patient travel and vehicle emissions. Also, some applications could work with telemedicine, allowing patients to remotely monitor their health status, reducing pressure on oversaturated health systems85,86. Furthermore, technology might be applied to training and education as a distance-learning tool, allowing telementoring in surgery and beyond. For example, this modality is gaining popularity at virtual conferences87. Telementoring enables international networking and avoids unnecessary travel.
In addition, the medical device industry should be part of this rethinking process. Single-use devices are more profitable for medical companies than reusable ones78. For example, in a laparoscopic cholecystectomy study of 1,803 surgeries, the costs of disposables (including trocars, ports and clip applicators) were found to be 6.4 times higher than reusables71. Therefore, the creation and promotion of reusable medical devices are of utmost importance, and this reflection should begin within the industry, presenting sustainable devices to medical professionals.
The carbon cost of various treatment options for the same disease will also probably need to be equated in the future. Two multicentre studies88,89 on GERD surgery (288 patients) compared with medical therapy (266 patients) were carried out. The first multicentre study focused on clinical outcomes: for up to 3 years, 90% of the patients in the surgical arm remained in remission compared with 93% in the medical arm (P = 0.25)88. In the second study, Gatenby90 studied the carbon footprint of the two approaches. The surgical arm was more sustainable than the medical arm (30 kg CO2 versus 100 kg CO2 per year, respectively). Although these estimates pointed out methodological flaws, because the data used were collected from a large multicentre cohort created for another purpose and the model did not take into account different manufacturing origins, which can have different carbon footprints90, this study raised questions regarding the need to equate carbon cost with different treatment options.
Finally, systematic measurement is necessary to reduce the surgical carbon footprint adequately. Scales to standardize carbon footprint measurement have been developed, such as the Spark2 (ref.91) for the broad surgical process or those described by Misrai et al.52 for the evaluation of disposable minimally invasive surgical devices52,91. Technology that will allow for global implementation of these scales is under development, and this will warrant a systematic measurement and identify health-care sectors in which sustainable intervention is necessary (Open Medical). In addition to the remote monitoring of patients, technology could be applied to monitor hospital material, track maintenance and replacement timings, and boost the efficiency of hospital supplies (Loopcycle).
Research
Climate change and health have attracted the attention of scientists in the past few years, and novel data on the environment and health are being issued daily. However, only 9.2% of the available literature focuses on the environmental effects of the health-care sector on health57, and this topic has not received the attention it deserves from researchers92. For example, endoscopy is an important diagnostic procedure for many surgical patients. Although there has been an increased focus on sustainable surgery, research on more sustainable endoscopy practices is still in the early stages of development.
Gastroenterologists and surgeons are leaders in wards, endoscopy units, operating theatres and scientific research. There have been excellent examples of surgical leadership in developing and delivering global quality research that affects patients’ lives and medical practices93,94. It is time to gather the same energy and effort for sustainability in surgery and beyond. Sustainable surgery must be evidence based, and there must be a real investment in quality research to achieve this. Although the motivation of practitioners and researchers is crucial, the support of national and international entities is needed to address this issue adequately. Environmental choices are typically economical, and promoting more sustainable surgical practice would advocate environmental protection and financial savings. This financial benefit is a strong argument, and further high-quality research to demonstrate this premise is required.
Re-educate
The authors of this Perspective consider the lack of awareness and education on sustainability in surgery as a reality. The surgical carbon footprint has been demonstrated2, and guidance on possible solutions to address some of the carbon footprint drivers has been available since 2012 (refs.5,90,95–97). However, sufficient real-world effort has not been made.
A survey published in 2020 showed that 19% of ophthalmology surgeons in New Zealand believe that climate change is not due to human activity and does not require any human action98. Moreover, 61% affirmed that they were not concerned about sustainability in their current practice98. In addition, fewer than 20% had received education or guidance regarding this subject. These data conclusively show that education regarding surgery sustainability is urgently needed.
The UK is at the forefront of sustainability education in health care. For example, the General Medical Council and Nursing Midwifery Council require education and the clinical application of sustainable methods99,100. In addition, in the UK, guidance starts in universities with lectures on sustainable health care for prospective doctors and nurses101.
The ‘re-education process’ has already begun. Sustainability in surgery is being promoted by multiple organizations worldwide created to address this issue. Also, European surgical societies such as the European Society of Coloproctology102 and the European Society of Gastrointestinal Endoscopy103 are developing campaigns to address sustainability102. However, more focus should be placed on sustainability during surgical conferences, social media channels and medical and surgical training to better educate current and future generations of surgeons.
Notably, accounting for clinical best practices and patient safety is mandatory in a sustainable surgical model. The ultimate goal of surgery is to cure and offer a good health-related quality of life. Clinical best practices are starting to recognize sustainability as an aim, and ‘doing no harm’ is starting to concern both patients and the environment59,104. In the available studies on this topic, implementing sustainable policies in surgery did not increase the risk of adverse events nor result in suboptimal treatment outcomes54,105,106. Patients must also be integrated into this novel approach to surgery1,19. Future studies on sustainability in surgery should confirm the acceptability and safety of a ‘greener’ surgical path by evaluating patient-reported and surgical outcomes1,19.
Gastroenterology and hepatology
Gastrointestinal conditions
In the USA, gastrointestinal diseases are a source of substantial burden and costs, and this burden is likely to continue increasing6,8. Several considerations explain why this field should be considered central to — and should likely lead to — a change in practice towards a sustainable approach (Box 2). The prevalence of these conditions is one of the most important aspects, and the associated need for invasive treatment, such as appendectomy, which is among the most common procedures performed globally, with increasing figures over the past few years107. Screening and treatment for cancers of the digestive system represent another major determinant. According to the International Agency for Research on Cancer of WHO, in 2020, approximately 31,179 million people had had cancer of the stomach, colon and rectum, or liver and intrahepatic bile ducts. Figures on these specific cancers are expected to increase to 36,795 million by 2040 (+59.7%)108. Notably, although the rates and cumulative risk of prostate (age-specific rate (ASR) 65.5) and lung (ASR 41.7) cancers were the highest globally in men in 2010, gastrointestinal tract cancers (oesophagus, stomach, colon, rectum and anus, liver, gallbladder and pancreas) were by far the first if taken all together (ASR 6.6, 15.9, 22.7, 16.3, 9.1, 2.3, 8.1, respectively)109. The prevalence of obesity and overweight should also be considered because this affects the number of patients requiring surgical or endoscopic interventions for such conditions, often involving minimally invasive approaches and single-use consumables. Unprecedented adoption of minimally invasive surgery has been recorded during the past decade for treating gastrointestinal diseases110, which seems to have surpassed the rates of open surgery between 2012 and 2018 in the USA, and the associated implications for the environment can easily be inferred. Thus, it becomes apparent that treatment of gastrointestinal diseases is a major player in determining the sustainability of health care — and at the same time, this sector represents an opportunity to drive the development and implementation of novel strategies to protect the environment (Box 2).
Box 2 Relevance of gastroenterology and hepatology to sustainable health-care practices.
Priority
Epidemiological relevance (gastro-oesophageal reflux disease; functional disorders; gastrointestinal infections; chronic liver disease; inflammatory bowel disease; gastrointestinal cancer)
One of the world’s largest therapeutic areas representing a heavy global burden
Advanced management demand (endoscopy, surgery)
Endoscopy is a burdensome practice owing to waste generation, disposable equipment, and energy and water consumption
Sustainable applications
Disease prevention (vaccination, policies to counteract alcohol abuse and healthy lifestyle advocation)
Use of lower effect and more widely accessible medications that are safe and effective (for example, biosimilars)
Reduce unnecessary patient travelling (subcutaneous alternatives to intravenous medication; teleconsultation)
‘5Rs plus one’ interventions in endoscopy units and gastroenterology departments
Ethics
Reuse through reprocessing and remanufacturing (regulation development and advice from the medical device industry)
Ensure acceptability and safety of sustainable choices through outcome measures (patient-reported; productivity estimates)
Digestive endoscopy principles
It has been estimated that between 11 and 15 million colonoscopies and 6 and 7 million upper gastrointestinal endoscopies are performed in 1 year in the USA alone6. This Perspective deconstructs the carbon footprint of the surgical pathway, as discussed earlier, and, indeed, endoscopy is part of this pathway, and its carbon footprint is substantial41,42,111. However, most endoscopy environmental effect drivers overlap the surgical ones, and these areas share solutions and barriers to mitigate climate change effects. Haddock et al.112 emphasized the importance of energy and water use, waste generation and handling, minimization of packaging and education of the staff on sustainable activities such as recycling and reducing unnecessary resource use. This Perspective promotes application of the ‘reduce, reuse and recycle’ principles but acknowledges that funding benchmarking research and education are important efforts towards sustainability112. Thus, the previously presented solutions (5Rs plus 1) apply to the daily practice of endoscopy (Box 2).
Moreover, Siddhi et al.113 highlighted that the challenges to achieving environmentally sustainable endoscopic practice range from standardized and reproducible carbon footprint measurement to transforming industrial, governmental and public health policies. The same multidisciplinary approach needs to be implemented in surgery and other health-care sectors to mitigate the climate change burden. Lastly, some endoscopy-specific factors should be considered — the first concerns endoscope reuse, which is currently a source of major debate114. Reprocessing entails costs, but manufacturing, assembly and transportation might result in a higher environmental burden. Secondly, faecal immunohistochemical testing could be a sustainable strategy to triage patients for the risk of harbouring colorectal cancer and potentially be used to prioritize endoscopic procedures115. However, further research and cut-off level adjustment might be needed115.
Sustainability of invasive procedures
Disease prevention and prompt treatment are of utmost importance in addressing the indirect environmental burden of diseases. Furthermore, climate change can negatively affect the gastrointestinal tract and its function. The incidence of gastrointestinal infectious disease parallels global warming116, and GERD-related medical care utilization increases in air-polluted environments (defined according to carbon monoxide and particulate matter with a diameter of ≤2.5 µm)15. However, if these are relatable associations, other correlations might not be straightforward, such as those linking functional gastrointestinal diseases to climate change17,117 and inflammatory bowel disease (IBD) to aeroallergens and air pollution118. It is very difficult to tackle environmental challenges beyond clinicians’ practice. Clean energy promotion towards a fossil-free recovery and recognizing the importance of biodiversity preservation are some of the measures in the COP 26 special report by WHO, focusing on “the health argument for climate action”119. However, there are potential paths for health professionals and health-care administrations regarding diseases such as IBD that might result in more sustainable practices compared with current practices.
For example, biosimilars are bending the cost curve120 and might represent wider global access to therapy for IBD and patients with cancer than currently. The wider availability of these therapies might allow reduction in the disease burden, which is a sustainable measure as it promotes health. Also, the emergence of subcutaneous alternatives to the conventional formulations of biologic agents for IBD reduces unnecessary patient travelling and hospital burden because patients can administer these therapies at home121. IBD and other chronic gastrointestinal disorders might lead to iron deficiency anaemia. Comorbid anaemia is an important predictor of increased risk of hospitalization and patient mortality. There is evidence regarding the use of ferric carboxymaltose as the most sustainable intravenous iron preparation owing to the lower number of infusions needed, this reducing hospital burden and costs related to individual patient management122.
Another example is patients with chronic liver diseases, who are high need and high cost. Governmental health agencies should implement policies to prevent hepatitis transmission, counteract alcohol abuse and encourage lifestyles that prevent obesity and metabolic syndrome123. As stated, these interventions advocating a healthier lifestyle could further reduce the need for obesity surgery and bariatric endoscopy. Hepatitis B vaccine equity, recommended for all newborns and individuals in high-risk groups, could profoundly affect not only reduction of the hepatocellular carcinoma burden worldwide but also reduction of disease vulnerability in low and lower-middle-income countries. As stated by WHO, “until everyone is safe, no one is safe”119.
Barriers to sustainable health care
Various barriers (‘roadblocks’ that prevent the adoption of strategies to reduce climate change) have been reported and categorized throughout the past few years124. However, these barriers are not hurdles specific to health systems. Various contexts, such as health care, households, cities and agriculture, will share barriers that hold back climate change mitigation; these are all relevant when developing sustainable medical and surgical practice. For example, barriers faced by cities that aim to reduce greenhouse gas emissions and become more resilient to face the effects of climate change (for example, “access to funding is the single biggest obstacle to cities delivering greater climate action”) are similar to the barriers faced by health systems (for example, “the financial environment of health-care conflicts with climate change mitigation”)125 (Box 3).
Health systems operate in a constrained context that aims for optimal clinical care delivery, and sustainability considerations are seldom made117. Nevertheless, there is evidence that initiatives to promote sustainable development are being made. However, health-care system transformations to address climate deterioration will require paradigm shifts in health-care aims and practices126, and changing behaviours is challenging. This necessity suggests the importance of an additional principle to the 5Rs rule because re-education can be a pillar in facilitating cultural change that should not be neglected.
Box 3 Common barriers to adopting a sustainable approach that apply to health care.
Economic and financial — access to funding to implement greater climate action
Policy and leadership — difficulties in implementing long-term measures when governments usually change on shorter-term cycles
Institution, regulatory and legislative — conflicting interests
Information and knowledge — lack of global awareness and advice
Social and cultural — influence, adaptation, change and decision-making
Technology and infrastructure
Physical and human context — adaptive capacity limited by human resources
Conclusion
Surgery is the most energy-intensive sector, and achieving sustainability in surgery is an emerging strategy for decreasing the carbon footprint of the health-care system (see Box 4). However, environmental costs associated with surgical care are often overlooked, and this issue has been largely ignored in the past but is gaining increased recognition. Therefore, it is vital to undertake high-quality research to demonstrate that promoting more sustainable surgical practice protects the environment and results in financial savings that would serve political interests. Specific areas for further investigation include the environmental burden of various surgical approaches, the implementation of operating theatre recycling, the promotion of reusables, advocacy for sustainable anaesthetic options, the environmental gains associated with telemedicine, telementoring and technological developments, and looking beyond specific surgical procedures to the overall surgical pathway.
In conclusion, climate change and environmental burdens are global problems. However, the environmental effect of health systems goes beyond surgical practice. Indeed, endoscopy, gastroenterology and hepatology are versatile areas in which sustainability interventions are also pertinent. The framework presented here to mitigate the effects of surgery can be easily transferred to other departments and health services. The insights provided in a stepwise manner can be applied to surgical departments and beyond (hospitals and health services) within a multidisciplinary perspective, leading to the implementation of climate change mitigation efforts.
Box 4 Key points on environmental effects of surgical procedures and strategies for sustainable surgery.
Climate change dramatically threatens public health and the health-care sector.
Surgery is the most energy-intensive practice, directly contributing to climate change.
Gastrointestinal diseases are among the most common conditions requiring invasive diagnostic and therapeutic procedures globally.
Sustainable gastroenterology and endoscopy practices are still in the early stages of development.
The ‘5Rs plus 1’ principle (reduce, reuse, recycle, rethink, research and re-educate) can be used as a template for more sustainable surgical practice. It can be easily applied to other health-care fields.
Sustainability in surgery encompasses a surgical pathway that aims to achieve the best outcomes for patients in an environmentally friendly way.
The impact of the health-care sector should be addressed from a multidisciplinary perspective, including health professionals, patients, companies, health-care managers and governments.
Acknowledgements
The authors thank P. Castelo Branco for his insights during manuscript revision and J. Roseira for her support with this article.
Author contributions
The authors contributed equally to all aspects of the article.
Peer review
Peer review information
Nature Reviews Gastroenterology & Hepatology thanks Craig McClain, Nitin Ahuja and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Miguel F. Cunha, Email: miguelcunha86@gmail.com
Gianluca Pellino, Email: gipe1984@gmail.com.
References
- 1.Rizan C, et al. The carbon footprint of surgical operations: a systematic review. Ann. Surg. 2020;272:986–995. doi: 10.1097/SLA.0000000000003951. [DOI] [PubMed] [Google Scholar]
- 2.MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health. 2017;1:e360–e367. doi: 10.1016/S2542-5196(17)30162-6. [DOI] [PubMed] [Google Scholar]
- 3.Rizan C, Bhutta MF. Strategy for net-zero carbon surgery. Br. J. Surg. 2021;108:737–739. doi: 10.1093/bjs/znab130. [DOI] [PubMed] [Google Scholar]
- 4.Alshqaqeeq F, Amin Esmaeili M, Overcash M, Twomey J. Quantifying hospital services by carbon footprint: a systematic literature review of patient care alternatives. Resour. Conserv. Recycl. 2020;154:104560. doi: 10.1016/j.resconrec.2019.104560. [DOI] [Google Scholar]
- 5.Kagoma Y, Stall N, Rubinstein E, Naudie D. People, planet and profits: the case for greening operating rooms. CMAJ. 2012;184:1905–1911. doi: 10.1503/cmaj.112139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Peery AF, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology. 2019;156:254–272.e11. doi: 10.1053/j.gastro.2018.08.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baddeley R, Aabakken L, Veitch A, Hayee B. Green endoscopy: counting the carbon cost of our practice. Gastroenterology. 2022;162:1556–1560. doi: 10.1053/j.gastro.2022.01.057. [DOI] [PubMed] [Google Scholar]
- 8.Chudy-Onwugaje K, von Rosenvinge EC. Improving global digestive health: the gastroenterologists’ role. Lancet Gastroenterol. Hepatol. 2020;5:882–883. doi: 10.1016/S2468-1253(20)30206-5. [DOI] [PubMed] [Google Scholar]
- 9.Peery AF, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–1187. doi: 10.1053/j.gastro.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Watts N, et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2021;397:129–170. doi: 10.1016/S0140-6736(20)32290-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu Z, FitzGerald G, Guo Y, Jalaludin B, Tong S. Impact of heatwave on mortality under different heatwave definitions: a systematic review and meta-analysis. Environ. Int. 2016;89–90:193–203. doi: 10.1016/j.envint.2016.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Lyon B, Dinku T, Raman A, Thomson MC. Temperature suitability for malaria climbing the Ethiopian Highlands. Environ. Res. Lett. 2017;12:064015. doi: 10.1088/1748-9326/aa64e6. [DOI] [Google Scholar]
- 13.Semenza JC, et al. Systemic resilience to cross-border infectious disease threat events in Europe. Transbound. Emerg. Dis. 2019;66:1855–1863. doi: 10.1111/tbed.13211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ebi KL, Nealon J. Dengue in a changing climate. Environ. Res. 2016;151:115–123. doi: 10.1016/j.envres.2016.07.026. [DOI] [PubMed] [Google Scholar]
- 15.Seo HS, Hong J, Jung J, Jung J. Relationship of meteorological factors and air pollutants with medical care utilization for gastroesophageal reflux disease in urban area. World J. Gastroenterol. 2020;26:6074–6086. doi: 10.3748/wjg.v26.i39.6074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Herring SC, Christidis N, Hoell A, Hoerling MP. Explaining extreme events of 2018 from a climate perspective. Bull. Am. Meteorol. Soc. 2020;101:1–128. doi: 10.1175/BAMS-ExplainingExtremeEvents2018.1. [DOI] [Google Scholar]
- 17.Leddin D, et al. Uniting the global gastroenterology community to meet the challenge of climate change and non-recyclable waste. Gastroenterology. 2021;161:1354–1360. doi: 10.1053/j.gastro.2021.08.001. [DOI] [PubMed] [Google Scholar]
- 18.Bekkar B, Pacheco S, Basu R, Basu R, Denicola N. Association of air pollution and heat exposure with preterm birth, low birth weight, and stillbirth in the US: a systematic review. JAMA Netw. Open. 2020;3:e208243. doi: 10.1001/jamanetworkopen.2020.8243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yates EF, et al. Empowering surgeons, anesthesiologists, and obstetricians to incorporate environmental sustainability in the operating room. Ann. Surg. 2021;273:1108–1114. doi: 10.1097/SLA.0000000000004755. [DOI] [PubMed] [Google Scholar]
- 20.Schildcrout JS, et al. Ambient air pollution and asthma exacerbations in children: an eight-city analysis. Am. J. Epidemiol. 2006;164:505–517. doi: 10.1093/aje/kwj225. [DOI] [PubMed] [Google Scholar]
- 21.Mann JK, et al. Short-term effects of air pollution on wheeze in asthmatic children in Fresno, California. Environ. Health Perspect. 2010;118:1497–1503. doi: 10.1289/ehp.0901292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fecht D, et al. Exposure to elevated nitrogen dioxide concentrations and cardiac remodeling in patients with dilated cardiomyopathy. J. Card. Fail. 2022;28:924–934. doi: 10.1016/j.cardfail.2021.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.IEA. SDG7: Data and Projections. IEAhttps://www.iea.org/reports/sdg7-data-and-projections (2020).
- 24.WHO. Quantitative risk assessment of the effects of climate change on selected causes of death, 2030s and 2050s (WHO, 2014).
- 25.Gitarskiy ML. The refinement to the 2006 IPCC Guidelines for National Greenhouse Gas Inventories. Fundam. Appl. Climatol. 2019;2:5–13. doi: 10.21513/0207-2564-2019-2-05-13. [DOI] [Google Scholar]
- 26.Wiedmann, T. & Minx, J. in Ecological Economics Research Trends (ed. Pertsova, C. C.) 1–11 (Nova Science Publishers, 2007).
- 27.STERN. STERN Review on the Economics of Climate Change. Annex I: User guide and access to more detailed information (STERN, 2006).
- 28.Pandey D, Agrawal M, Pandey JS. Carbon footprint: current methods of estimation. Environ. Monit. Assess. 2011;178:135–160. doi: 10.1007/s10661-010-1678-y. [DOI] [PubMed] [Google Scholar]
- 29.McGain F, Muret J, Lawson C, Sherman JD. Environmental sustainability in anaesthesia and critical care. Br. J. Anaesth. 2020;125:680–692. doi: 10.1016/j.bja.2020.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eckelman MJ, Sherman J. Environmental impacts of the U.S. health care system and effects on public health. PLoS ONE. 2016;11:e0157014. doi: 10.1371/journal.pone.0157014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Resources Institute. CAIT Climate Data Explorer [web tool]. CAIT Historical - Explore Historic Greenhouse Gas Emissions (World Resources Institute, 2018).
- 32.Chung JW, Meltzer DO. Estimate of the carbon footprint of the US health care sector. JAMA Surg. 2009;302:1970–1972. doi: 10.1001/jama.2009.1610. [DOI] [PubMed] [Google Scholar]
- 33.Karliner, J. et al. Health care’s climate footprint. Health Care Harmhttps://noharm-global.org/sites/default/files/documents-files/5961/HealthCaresClimateFootprint_092319.pdf (2019).
- 34.EIA. CBECS 2012: Energy Usage Summary. US Governmenthttps://www.eia.gov/consumption/commercial/reports/2012/energyusage/ (2016).
- 35.Thiel CL, et al. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ. Sci. Technol. 2015;49:1779–1786. doi: 10.1021/es504719g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sanabria A, et al. Considerations for environmentally sustainable head and neck surgical oncology practice. Am. J. Otolaryngol. 2020;41:102719. doi: 10.1016/j.amjoto.2020.102719. [DOI] [PubMed] [Google Scholar]
- 37.FSM A, et al. The study of sustainable green HVAC systems in health care facilities. J. Archit. Eng. Technol. 2015;05:1000160. doi: 10.4172/2168-9717.1000160. [DOI] [Google Scholar]
- 38.Tomson C. Reducing the carbon footprint of hospital-based care. Future Hosp. J. 2015;2:57–62. doi: 10.7861/futurehosp.15.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Esmaeili A, et al. Scope for energy improvement for hospital imaging services in the USA. J. Health Serv. Res. Policy. 2015;20:67–73. doi: 10.1177/1355819614554845. [DOI] [PubMed] [Google Scholar]
- 40.Esmaeili A, et al. Environmental impact reduction as a new dimension for quality measurement of healthcare services. Int. J. Health Care Qual. Assur. 2018;31:910–922. doi: 10.1108/IJHCQA-10-2016-0153. [DOI] [PubMed] [Google Scholar]
- 41.Vaccari M, Tudor T, Perteghella A. Costs associated with the management of waste from healthcare facilities: an analysis at national and site level. Waste Manag. Res. 2018;36:39–47. doi: 10.1177/0734242X17739968. [DOI] [PubMed] [Google Scholar]
- 42.Maurice JB, et al. Green endoscopy: a call for sustainability in the midst of COVID-19. Lancet Gastroenterol. Hepatol. 2020;5:636–638. doi: 10.1016/S2468-1253(20)30157-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ryan SM, Nielsen CJ. Global warming potential of inhaled anesthetics: application to clinical use. Anesth. Analg. 2010;111:92–98. doi: 10.1213/ANE.0b013e3181e058d7. [DOI] [PubMed] [Google Scholar]
- 44.Guetter CR, et al. Greening the operating room. Am. J. Surg. 2018;216:683–688. doi: 10.1016/j.amjsurg.2018.07.021. [DOI] [PubMed] [Google Scholar]
- 45.Sherman J, Le C, Lamers V, Eckelman M. Life cycle greenhouse gas emissions of anesthetic drugs. Anesth. Analg. 2012;114:1086–1090. doi: 10.1213/ANE.0b013e31824f6940. [DOI] [PubMed] [Google Scholar]
- 46.Jehle K, Jarrett N, Matthews S. Clean and green: saving water in the operating theatre. Ann. R. Coll. Surg. Engl. 2008;90:22–24. doi: 10.1308/003588408X242277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Loveday HP, et al. epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J. Hosp. Infect. 2014;86:S1–S70. doi: 10.1016/S0195-6701(13)60012-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Javitt MJ, Grossman A, Grajewski A, Javitt JC. Association between eliminating water from surgical hand antisepsis at a large ophthalmic surgical hospital and cost. JAMA Ophthalmol. 2020;138:382–386. doi: 10.1001/jamaophthalmol.2020.0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.McQuerry M, Easter E, Cao A. Disposable versus reusable medical gowns: a performance comparison. Am. J. Infect. Control. 2021;49:563–570. doi: 10.1016/j.ajic.2020.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rosenblatt WH, Chavez A, Tenney D, Silverman DG. Assessment of the economic impact of an overage reduction program in the operating room. J. Clin. Anesth. 1997;9:478–481. doi: 10.1016/S0952-8180(97)00104-9. [DOI] [PubMed] [Google Scholar]
- 51.Donaldson, K. Save the planet: recycling in the OR. Infection Control Today (1 July 2000).
- 52.Misrai V, et al. A standardized method for estimating the carbon footprint of disposable minimally invasive surgical devices. Ann. Surg. Open. 2021;2:e094. doi: 10.1097/AS9.0000000000000094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kamarajah SK, et al. Robotic versus conventional laparoscopic pancreaticoduodenectomy a systematic review and meta-analysis. Eur. J. Surg. Oncol. 2020;46:6–14. doi: 10.1016/j.ejso.2019.08.007. [DOI] [PubMed] [Google Scholar]
- 54.Siu J, Hill AG, MacCormack AD. Systematic review of reusable versus disposable laparoscopic instruments: costs and safety. Anz. J. Surg. 2017;87:28–33. doi: 10.1111/ans.13856. [DOI] [PubMed] [Google Scholar]
- 55.Grantcharov P, Ahmed S, Wac K, Rivas H. Reprocessing and reuse of single-use medical devices: perceptions and concerns of relevant stakeholders toward current practices. Int. J. Evid. Based Healthc. 2019;17:53–57. doi: 10.1097/XEB.0000000000000146. [DOI] [PubMed] [Google Scholar]
- 56.Mihanović J, et al. Comparison of new versus reused Harmonic scalpel performance in laparoscopic appendectomy in patients with acute appendicitis — a randomized clinical trial. Langenbeck’s Arch. Surg. 2021;406:153–162. doi: 10.1007/s00423-020-02039-y. [DOI] [PubMed] [Google Scholar]
- 57.Weiss A, et al. Environmentalism in surgical practice. Curr. Probl. Surg. 2016;53:165–205. doi: 10.1067/j.cpsurg.2016.02.001. [DOI] [PubMed] [Google Scholar]
- 58.Hutchins DCJ, White SM. Coming round to recycling. BMJ. 2009;338:746–748. doi: 10.1136/bmj.b609. [DOI] [PubMed] [Google Scholar]
- 59.Sherman JD, et al. The Green Print: advancement of environmental sustainability in healthcare. Resour. Conserv. Recycl. 2020;161:104882. doi: 10.1016/j.resconrec.2020.104882. [DOI] [Google Scholar]
- 60.Woods DL, et al. Carbon footprint of robotically-assisted laparoscopy, laparoscopy and laparotomy: a comparison. Int. J. Med. Robot. 2015;11:406–412. doi: 10.1002/rcs.1640. [DOI] [PubMed] [Google Scholar]
- 61.Rizan C, Bhutta MF. Environmental impact and life cycle financial cost of hybrid (reusable/single-use) instruments versus single-use equivalents in laparoscopic cholecystectomy. Surg. Endosc. 2022;36:4067–4078. doi: 10.1007/s00464-021-08728-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Power NE, Silberstein JL, Ghoneim TP, Guillonneau B, Touijer KA. Environmental impact of minimally invasive surgery in the United States: an estimate of the carbon dioxide footprint. J. Endourol. 2012;26:1639–1644. doi: 10.1089/end.2012.0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wong YL, Noor M, James KL, Aslam TM. Ophthalmology going greener: a narrative review. Ophthalmol. Ther. 2021;10:845–857. doi: 10.1007/s40123-021-00404-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Urquhart R, et al. Defining sustainability in practice: views from implementing real-world innovations in health care. BMC Health Serv. Res. 2020;20:87. doi: 10.1186/s12913-020-4933-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.WHO Regional Office for Europe. Environmentally Sustainable Health Systems (2015).
- 66.Meara JG, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569–624. doi: 10.1016/S0140-6736(15)60160-X. [DOI] [PubMed] [Google Scholar]
- 67.Chaplin CL, Wernham AGH, Veitch D. Environmental sustainability in dermatological surgery. Br. J. Dermatol. 2021;184:952–953. doi: 10.1111/bjd.19668. [DOI] [PubMed] [Google Scholar]
- 68.Van Demark RE, Smith VJS, Fiegen A. Lean and green hand surgery. J. Hand Surg. 2018;43:179–181. doi: 10.1016/j.jhsa.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 69.Tavolacci M-P, et al. Prevention of nosocomial infection and standard precautions: knowledge and source of information among healthcare students. Infect. Control Hosp. Epidemiol. 2008;29:642–647. doi: 10.1086/588683. [DOI] [PubMed] [Google Scholar]
- 70.Practice Greenhealth. The Business Case for Greening the OR. Practice Greenhealthhttps://www.c4spgh.org/HCW1_Presentations/GOR_FullSet_Guidance%20Docs_Web_042711.pdf (2022).
- 71.Slater M, Booth MI, Dehn TCB. Cost-effective laparoscopic cholecystectomy. Ann. R. Coll. Surg. Engl. 2009;91:670–672. doi: 10.1308/003588409X12486167521154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Conrardy J, Hillanbrand M, Myers S, Nussbaum GF. Reducing medical waste. AORN J. 2010;91:711–721. doi: 10.1016/j.aorn.2009.12.029. [DOI] [PubMed] [Google Scholar]
- 73.Thiel C, Duncan P, Woods N. Attitude of US obstetricians and gynaecologists to global warming and medical waste. J. Health Serv. Res. Policy. 2017;22:162–167. doi: 10.1177/1355819617697353. [DOI] [PubMed] [Google Scholar]
- 74.Zacharias LC, et al. Safety and cost-effectiveness of single-use endolaser probe reprocessing in vitreoretinal surgery. Int. J. Retina Vitreous. 2021;7:22. doi: 10.1186/s40942-021-00292-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.De Sousa Martins B, Melo JQE, Logarinho Monteiro J, Rente G, Bastos PT. Reprocessing of single-use medical devices: clinical and financial results. Port. J. Public Health. 2018;36:150–156. doi: 10.1159/000496299. [DOI] [Google Scholar]
- 76.Kwakye G, Pronovost PJ, Makary MA. Commentary: a call to go green in health care by reprocessing medical equipment. Acad. Med. 2010;85:398–400. doi: 10.1097/ACM.0b013e3181cd5a71. [DOI] [PubMed] [Google Scholar]
- 77.Association of Medical Device Reprocessors. Legislation/Regulation - AMDR. AMDR-Generated Resource. AMDRhttp://amdr.org/legislationregulation/ (2019).
- 78.Association of Medical Device Reprocessors. Reprocessing by the Numbers. AMDR-Generated Resource. AMDRhttp://amdr.org/reprocessing-by-the-numbers/ (2019).
- 79.French-Mowat E, Burnett J. How are medical devices regulated in the European Union? J. R. Soc. Med. 2012;105:S22. doi: 10.1258/jrsm.2012.120036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kwakye G, Brat GA, Makary MA. Green surgical practices for health care. Arch. Surg. 2011;146:131–136. doi: 10.1001/archsurg.2010.343. [DOI] [PubMed] [Google Scholar]
- 81.Southorn T, Norrish AR, Gardner K, Baxandall R. Reducing the carbon footprint of the operating theatre: a multicentre quality improvement report. J. Perioper. Pract. 2013;23:144–146. doi: 10.1177/175045891302300605. [DOI] [PubMed] [Google Scholar]
- 82.McGain F, et al. Auditing operating room recycling: a management case report. A A Case Rep. 2015;5:47–50. doi: 10.1213/XAA.0000000000000097. [DOI] [PubMed] [Google Scholar]
- 83.Urrea C, Venegas D. Automatized follow-up and alert system for patients with chronic hypertension. Health Inform. J. 2020;26:2625–2636. doi: 10.1177/1460458219900446. [DOI] [PubMed] [Google Scholar]
- 84.Dixon RF, Rao L. Asynchronous virtual visits for the follow-up of chronic conditions. Telemed. e-Health. 2014;20:669–672. doi: 10.1089/tmj.2013.0211. [DOI] [PubMed] [Google Scholar]
- 85.Buyting R, et al. Virtual care with digital technologies for rural Canadians living with cardiovascular disease. CJC Open. 2022;4:133–147. doi: 10.1016/j.cjco.2021.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bokolo AJ. Exploring the adoption of telemedicine and virtual software for care of outpatients during and after COVID-19 pandemic. Ir. J. Med. Sci. 2021;190:1–10. doi: 10.1007/s11845-020-02299-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Butt KA, Augestad KM. Educational value of surgical telementoring. J. Surg. Oncol. 2021;124:231–240. doi: 10.1002/jso.26524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Lundell L, et al. Comparing laparoscopic antireflux surgery with esomeprazole in the management of patients with chronic gastro-oesophageal reflux disease: a 3-year interim analysis of the LOTUS trial. Gut. 2008;57:1207–1213. doi: 10.1136/gut.2008.148833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Epstein D, et al. Laparoscopic fundoplication compared with medical management for gastro-oesophageal reflux disease: cost effectiveness study. BMJ. 2009;339:152–155. doi: 10.1136/bmj.b2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Gatenby PAC. Modelling the carbon footprint of reflux control. Int. J. Surg. 2011;9:72–74. doi: 10.1016/j.ijsu.2010.09.008. [DOI] [PubMed] [Google Scholar]
- 91.Ewbank C, et al. The development of a surgical care and climate change matrix: a tool to assist with prioritization and implementation strategies. Ann. Surg. 2020;273:e50–e51. doi: 10.1097/SLA.0000000000003980. [DOI] [PubMed] [Google Scholar]
- 92.Bhopal A, Norheim OF. Priority setting and net zero healthcare: how much health can a tonne of carbon buy? BMJ. 2021;375:e067199. doi: 10.1136/bmj-2021-067199. [DOI] [PubMed] [Google Scholar]
- 93.COVIDSurg Collaborative. Timing of surgery following SARS-CoV-2 infection: an international prospective cohort study. Anaesthesia. 2021;76:748–758. doi: 10.1111/anae.15458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bhangu A, et al. Mortality and pulmonary complications in patients undergoing surgery with perioperative sars-cov-2 infection: an international cohort study. Lancet. 2020;396:27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Morris DS, Wright T, Somner JEA, Connor A. The carbon footprint of cataract surgery. Eye. 2013;27:495–501. doi: 10.1038/eye.2013.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Sailhamer EA, Sokal SM, Chang Y, Rattner DW, Berger DL. Environmental impact of accelerated clinical care in a high-volume center. Surgery. 2007;142:343–349. doi: 10.1016/j.surg.2007.03.015. [DOI] [PubMed] [Google Scholar]
- 97.Khajuria A. Robotics and surgery: a sustainable relationship? World J. Clin. Cases. 2015;3:265. doi: 10.12998/wjcc.v3.i3.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Chandra P, Gale J, Murray N. New Zealand ophthalmologists’ opinions and behaviours on climate, carbon and sustainability. Clin. Exp. Ophthalmol. 2020;48:427–433. doi: 10.1111/ceo.13727. [DOI] [PubMed] [Google Scholar]
- 99.Nursing and Midwifery Council. Standards of Proficiency for Midwives. NMChttps://www.nmc.org.uk/globalassets/sitedocuments/standards/standards-of-proficiency-for-midwives.pdf (2019).
- 100.General Medical Council. Outcomes for graduates plus supplementary guidance. GMChttps://www.gmc-uk.org/education/standards-guidance-and-curricula/standards-and-outcomes/outcomes-for-graduates (2020).
- 101.Tun MS. Fulfilling a new obligation: teaching and learning of sustainable healthcare in the medical education curriculum. Med. Teach. 2019;41:1168–1177. doi: 10.1080/0142159X.2019.1623870. [DOI] [PubMed] [Google Scholar]
- 102.European Society of Coloproctology. ESCP Goes Green. ESCPhttps://www.escp.eu.com/news/2277-escp-goes-green (2022).
- 103.Rodríguez De Santiago E, et al. Reducing the environmental footprint of gastrointestinal endoscopy: European Society of Gastrointestinal Endoscopy (ESGE) and European Society of Gastroenterology and Endoscopy Nurses and Associates (ESGENA) Position Statement. Endoscopy. 2022;54:797–826. doi: 10.1055/a-1859-3726. [DOI] [PubMed] [Google Scholar]
- 104.Simpson KR. Choosing wisely. MCN Am. J. Matern. Child Nurs. 2016;41:196. doi: 10.1097/NMC.0000000000000238. [DOI] [PubMed] [Google Scholar]
- 105.Thiel CL, et al. Cataract surgery and environmental sustainability: waste and lifecycle assessment of phacoemulsification at a private healthcare facility. J. Cataract Refract. Surg. 2017;43:1391–1398. doi: 10.1016/j.jcrs.2017.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Goel H, et al. Improving productivity, costs and environmental impact in International Eye Health Services: using the ‘Eyefficiency’ cataract surgical services auditing tool to assess the value of cataract surgical services. BMJ Open Ophthalmol. 2021;6:642. doi: 10.1136/bmjophth-2020-000642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Eurostat. Surgical operations and procedures statistics-Statistics Explained (2015).
- 108.IARC. Global Cancer Observatory. Cancer Tomorrow. IARChttps://gco.iarc.fr/tomorrow/en/dataviz/tables?mode=population&cancers=8_9_11_7&group_cancers=1&multiple_cancers=1 (2021).
- 109.IARC. Global Cancer Observatory. Cancer Over Time. IARChttps://gco.iarc.fr/overtime/en/dataviz/tables?populations=3600_7600_10000_17000_11200_12400_15200_15600_19100_20300_20800_21800_23300_25000_27600_35200_35600_37200_37600_38000_41000_41400_42800_44000_47000_52800_55400_57800_61600_70300_70500_18800_39200 (2021).
- 110.Sheetz KH, Claflin J, Dimick JB. Trends in the adoption of robotic surgery for common surgical procedures. JAMA Netw. Open. 2020;3:e1918911. doi: 10.1001/jamanetworkopen.2019.18911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Gayam S. Environmental impact of endoscopy: ‘scope’ of the problem. Am. J. Gastroenterol. 2020;115:1931–1932. doi: 10.14309/ajg.0000000000001005. [DOI] [PubMed] [Google Scholar]
- 112.Haddock R, De Latour R, Siau K, Hayee B, Gayam S. Climate change and gastroenterology: planetary primum non nocere and how industry must help. Am. J. Gastroenterol. 2022;117:394–400. doi: 10.14309/ajg.0000000000001604. [DOI] [PubMed] [Google Scholar]
- 113.Siddhi S, Dhar A, Sebastian S. Best practices in environmental advocacy and research in endoscopy. Tech. Innov. Gastrointest. Endosc. 2021;23:376–384. doi: 10.1016/j.tige.2021.06.002. [DOI] [Google Scholar]
- 114.Agrawal D, Tang Z. Sustainability of single-use endoscopes. Tech. Innov. Gastrointest. Endosc. 2021;23:353–362. doi: 10.1016/j.tige.2021.06.001. [DOI] [Google Scholar]
- 115.Bjørsum-Meyer T, Toth E, Koulaouzidis A. Carbon footprint from superfluous colonoscopies: potentialities to scale down the impact. Gut. 2022 doi: 10.1136/gutjnl-2021-326587. [DOI] [PubMed] [Google Scholar]
- 116.Altizer S, Ostfeld RS, Johnson PTJ, Kutz S, Harvell CD. Climate change and infectious diseases: from evidence to a predictive framework. Science. 2013;341:514–519. doi: 10.1126/science.1239401. [DOI] [PubMed] [Google Scholar]
- 117.Desmond S. Implementing climate change mitigation in health services: the importance of context. J. Health Serv. Res. Policy. 2016;21:257–262. doi: 10.1177/1355819616645373. [DOI] [PubMed] [Google Scholar]
- 118.Herman SM, Zaborniak K, Bernstein CN. Insight into inflammatory bowel disease pathogenesis: is the answer blowing in the wind? Inflamm. Bowel Dis. 2022;28:486–491. doi: 10.1093/ibd/izab183. [DOI] [PubMed] [Google Scholar]
- 119.World Health Organization. COP26 Special Report on Climate Change and Health. The Health Argument for Climate Action (WHO, 2021).
- 120.Bria E, Conte P. Biosimilars as a strategy to improve sustainability. ESMO Open. 2017;2:10–11. doi: 10.1136/esmoopen-2017-000192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Fierens L, et al. Introduction of subcutaneous infliximab CT-P13 and vedolizumab in clinical practice: a multi-stakeholder position statement highlighting the need for post-marketing studies. J. Crohns Colitis. 2022;16:1059–1069. doi: 10.1093/ecco-jcc/jjac009. [DOI] [PubMed] [Google Scholar]
- 122.Poscia A, et al. Sustainability of endovenous iron deficiency anaemia treatment: hospital-based health technology assessment in IBD patients. Biomed. Res. Int. 2017;2017:3470893. doi: 10.1155/2017/3470893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Galle PR, et al. EASL clinical practice guidelines: management of hepatocellular carcinoma. J. Hepatol. 2018;69:182–236. doi: 10.1016/j.jhep.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 124.Eisenack K, et al. Explaining and overcoming barriers to climate change adaptation. Nat. Clim. Change. 2014;4:867–872. doi: 10.1038/nclimate2350. [DOI] [Google Scholar]
- 125.Thomas, K. E. 3 Biggest Barriers Holding Cities Back on Climate Change. Next Cityhttps://nextcity.org/urbanist-news/cities-acting-against-climate-change (2022).
- 126.Setoguchi S, Leddin D, Metz G, Omary MB. Climate change, health, and health care systems: a global perspective. Gastroenterology. 2022;162:1549–1555. doi: 10.1053/j.gastro.2022.02.037. [DOI] [PubMed] [Google Scholar]
- 127.Thiel CL, Woods NC, Bilec MM. Strategies to reduce greenhouse gas emissions from laparoscopic surgery. Am. J. Public Health. 2018;108:S158–S164. doi: 10.2105/AJPH.2018.304397. [DOI] [PMC free article] [PubMed] [Google Scholar]