Abstract
The prevalence of Major Depressive Disorder in men is half that of women, yet depression affects approximately 109 million men worldwide. Alarmingly, men account for three quarters of suicides in Western countries but are unlikely to seek help for mental health concerns. It is possible that existing mental health treatments are not engaging or accessible to men. The aim of this review was to quantify the number of men involved in randomised trials of psychotherapy or lifestyle behaviour change targeting depression. Results found men represented 26% of participants in 110 eligible articles compared to 73% women. Men’s representation was low across all intervention characteristics (e.g., delivery mode). No studies used a completely male sample, compared to 19 studies targeting women only. Men are substantially underrepresented in research trials targeting depression.
Supplementary information
The online version contains supplementary material available at 10.1007/s12144-022-04017-7.
Keywords: Depression, Men, Help-seeking, Psychotherapy, Lifestyle behaviour change
Major depressive disorder (depression) is a chronic mental health condition characterised by persistent low mood, loss of interest in activities, and internalising symptoms of sadness, hopelessness, and guilt (American Psychiatric Association [APA], 2013). Between 1990 and 2017, the worldwide prevalence of depression increased by almost 50% (Liu et al., 2020) affecting approximately 4.4% of the population (World Health Organisation [WHO], 2017). COVID-19 has increased the prevalence of depression globally by approximately 28% (Santomauro et al., 2021). Depression is associated with a range of other mental and physical health conditions including anxiety (Hirschfeld, 2001), substance use (Hasin et al., 2005), diabetes, cardiovascular disease, and arthritis (Lotfaliany et al., 2018; Moussavi et al., 2007), making it a leading cause of disability worldwide (James et al., 2018).
The prevalence of depression, based on diagnosed cases, is higher in women than men; in 2015 global prevalence was 5.1% and 3.6% respectively (WHO, 2017). However, gender plays an important and complex role in depression diagnosis, with research showing both physicians and family members display gender bias towards attributing depression to women rather than men (Bertakis et al., 2001; Brommelhoff et al., 2004). Similarly, men are potentially underdiagnosed with depression due to diagnostic criteria not considering male specific aspects of depression and masculinity leading men to respond to depression by acting out (Martin et al., 2013; Magovcevic & Addis, 2008). Notably, gender sensitive scales which include externalising symptoms of depression have shown greater sensitivity for detecting change in treatment than traditional scales in some groups of men (Rice et al., 2013, Rice et al., 2020). Despite this, approximately 109 million men worldwide are currently experiencing traditional depressive disorders, which highlights the urgent need to support this at-risk subgroup (Global Burden of Disease [GBD], 2022).
Despite increasing access to mental health care in recent decades (Harris et al., 2015), men are less likely than women to seek help for mental health problems, including depression (Liddon et al., 2018; Oliver et al. 2005; Rice et al., 2017). One reason for this difference is stigma associated with mental illness. Some men endorse that mental health problems and help-seeking are signs of weakness (Judd et al., 2008; Lynch et al., 2018), also known as negative self-stigma (Vogel et al., 2006). In part, these views stem from adherence to traditional masculine norms in most Western societies, such as stoicism, emotional restraint, and self-reliance; which are associated with decreased help seeking (Addis & Mahalik, 2003; Seidler et al., 2016), poor mental health status (Primack et al., 2010), and suicidality (Pirkis et al., 2017).
It is also possible that existing mental health treatments may not be engaging or accessible to men (Bilsker et al., 2018; Seidler et al., 2018). When men are diagnosed with depression, they are often referred to psychotherapy for treatment. Psychotherapy is a general term used to describe interventions based on a scientific theoretical background and that use psychological techniques to reduce symptoms through modifying motivational, emotional, cognitive, behavioural, or interpersonal processes (Linde et al., 2015). Although evidence exists supporting the efficacy of various types of psychotherapy (Barth et al., 2016), some men have reported negative attitudes towards treatments (Levant et al., 2011), viewing psychotherapy as unappealing and anti-masculine (Berger et al., 2013; Englar-Carlson & Stevens, 2006). Men may also be deterred from certain aspects of therapy such as personal disclosure, emotional expression, and vulnerability, due to the impact of dominant masculine norms (Mahalik et al., 2003). Further, many services fail to consider gender and structural barriers, such as time and resources, and unappealing service environments are common (Seidler et al., 2018).
According to common wisdom, men are also less likely than women to participate in research testing interventions for depression, meaning that less evidence is available to suggest how interventions or service provision could be tailored to better address their needs. Whilst some psychotherapy reviews for depression neglect reporting gender outcomes (Newby et al., 2016), others have confirmed their samples are predominantly female (Berryhill et al., 2019; Castro et al., 2020; Nieuwsma et al., 2012). In this regard, ‘male gender blindness’ describes how men’s needs are implicitly overlooked (Seager et al., 2014). When studies do report gender data, the understanding gained is limited to the population or intervention investigated (Josephine et al., 2017). As such, the overall representation of men across all depression-focused intervention studies remains unclear, as are the outcomes of these studies in relation to addressing the identified gaps in service delivery for men with depression.
What does engage men
To better engage men, a substantial body of research has sought to understand what is engaging. Several recommendations have been made by clinicians and researchers regarding how to work therapeutically with men, which generally focus on themes such as making services gender-sensitive (APA, 2018; Mahalik et al., 2012). Substantially less is known about what specific intervention characteristics are best practice with men and how this relates to their experience of depression specifically. Research investigating sex differences in preferences for therapy has found that men engage more with treatments that take into account gender-specific preferences (Seidler et al., 2018). For example, men have indicated a preference for practical, action-focused interventions, such as cognitive behaviour therapy (CBT), over other forms of ‘talk therapy’ or emotion-focused therapy (Emslie et al., 2007; Seidler et al., 2016). Men have also indicated a preference for individual over group therapy (Kealy et al., 2021; Sierra Hernandez et al., 2014). eHealth interventions (which rely on end users to self-direct their intervention) have the potential to better engage men because they are confidential, non-confrontational, and promote autonomy and self-sufficiency (Berger et al., 2013; Ellis et al., 2013; Wang et al., 2016). These qualitative differences in gender-based preferences are important, but a gap remains regarding how these preferences reflect study enrolment rates and engagement practices for men on a larger scale.
Depression is associated with several lifestyle behaviours such as physical inactivity (Gianfredi et al., 2020), poor diet (Molendijk et al., 2018), disturbed sleep (Fang, Tu, Sheng, & Shao, 2019), and increased alcohol consumption (Churchill & Farrell, 2017). Multiple reviews have indicated that physical activity is an effective strategy for treating depression (Cooney et al., 2013; Josefsson et al., 2014; Schuch et al., 2016), and the evidence for interventions based on improving diet and sleep is growing (Firth et al., 2019; Gee et al., 2019). Observational evidence suggests men more frequently present with disruptions in these health behaviours rather than the cognitive or emotional symptoms of depression (Proudfoot et al., 2015). It is often these health behaviours that act as a prompt for men to seek help (Addis & Mahalik, 2003). Thus, lifestyle interventions have been highlighted as a promising approach for treating depression in men (Seaton et al., 2017), especially those who conform to traditional masculine norms (Berger et al., 2013) or are reluctant to acknowledge that they have depression (Fields & Cochran, 2011). A recent review of lifestyle programs found no studies with substantive mental health support for men with pre-existing mental health conditions and adequate power to detect changes in mental health outcomes (Drew et al., 2020), indicating a current lack of programs specifically targeting men’s mental health through lifestyle change.
Why it is important to do this review
Although qualitative research exists exploring men’s experience of depression treatment (Seidler et al., 2018), and sex differences in depression prevalence have been reported (Liddon et al., 2018), no study has simultaneously investigated the proportion of males included in intervention trials targeting depression and examined whether men’s involvement is moderated by key study or intervention characteristics. Research has shown that men will engage in treatment when it is accessible, appropriate, and engaging (Seidler et al., 2016). Therefore, it is crucial to understand which interventions men find most appealing (Addis, 2008).
Thus, we conducted this review to investigate the following research questions: (i) what is the number of males engaging in trials targeting major depression, (ii) have there been any published studies targeting males only, or are specifically designed for men, (iii) do male enrolment rates differ across certain intervention and trial design characteristics, (iv) have any attempts been made to increase the involvement of males, (v) are low rates of male involvement identified as a limitation, and (vi) are studies testing for sex differences in outcome?
Method
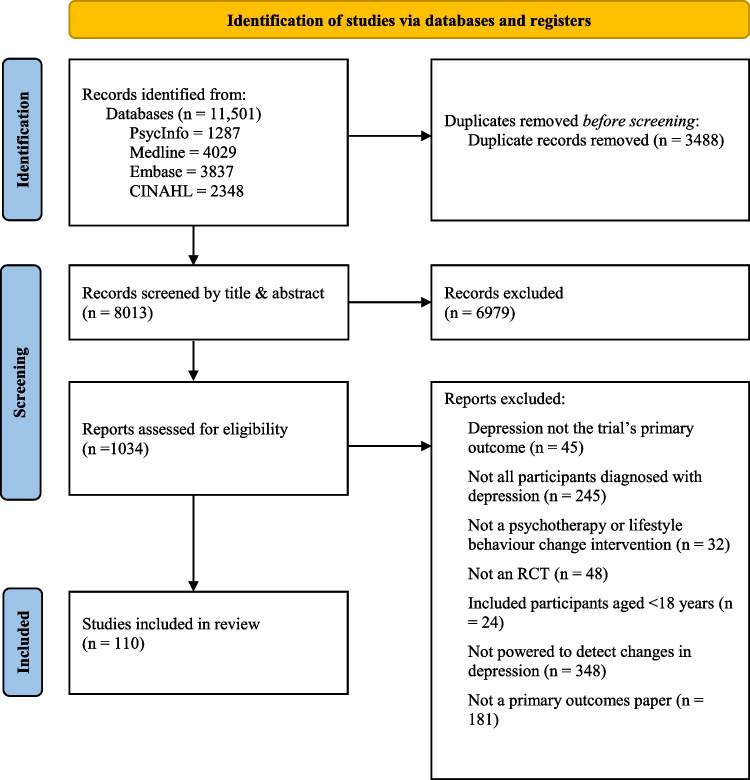
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) statement (Moher, Liberati, Tetzlaff, & Altman, 2010).
Eligibility criteria
Types of participants: Adults aged 18 and over who scored in a clinical range on a validated measure of depression (e.g., PHQ-9), or were diagnosed with major depression via interview. See Supplemental material 1 for the cut-off scores used.
-
Types of intervention: Studies were included if they tested at least one psychotherapy or lifestyle intervention. For this review, an intervention was considered psychotherapy if it was based on a scientific theoretical background and used psychological techniques to reduce symptoms and improve general well-being through modifying motivational, emotional, cognitive, behavioural, or interpersonal processes. For inclusion, it needed to have been performed either as a tailored, verbal communication process between a patient (or a group of patients) and a health care professional in direct or remote (e.g., telephone) contact, or as a less intense or self-guided intervention using written information material (e.g., book or computer program) that the patient worked through more or less independently (Linde et al., 2015). Eligible forms of psychotherapy were adapted based on existing reviews (e.g., CBT, behavioural activation therapy, problem solving therapy, psychodynamic therapy, non-directive supporting therapy (e.g., counselling) (Cuijpers et al., 2021; Cuijpers et al., 2008).
Eligible lifestyle interventions provided patients with knowledge and skills to promote meaningful changes to at least one lifestyle behaviour (e.g., physical activity). Mechanistic studies that manipulated health behaviours in a lab environment without a clear intent to create lasting behaviour change were excluded (e.g., acute impact of supervised exercise on depressive symptoms).
Comparator: Psychotherapy or lifestyle intervention arms could be compared to a control group or another intervention.
Outcomes: To be eligible, studies needed to explicitly report a power calculation at 80% to detect a change in the primary outcome related to depression (e.g., symptoms, prevalence, remission rates). Given the large number of depression trials published, this criterion was applied to reduce the number of included articles and to act as a proxy for study quality.
Types of studies: The review included randomized trials published in peer-reviewed, English language journals, from 2011 to 2021.
Information sources and search
An electronic database search of PsycInfo, Medline, Embase, and CINAHL was conducted on April 13th 2021. Search terms were divided into three groups: (a) intervention (e.g., psychotherapy, treatment); (b) study design (e.g., RCT, controlled trial, clinical trial); and (c) depression (e.g., major depression, MDD, depressive disorder). Medical subject heading terms were used when possible (e.g., Counselling/, Major Depression/, Clinical Trials/). Where possible, the following limits were applied: English language, last 10 years, adults (over 18 years of age), and clinical trials. See Supplemental material 2 for search syntax and results for all databases.
Study selection
In the first stage of study selection, one reviewer (JK) screened 8013 title and abstracts. Following this, three reviewers (JK, BB, JW) independently screened 1034 full-text studies. A sample of 50 studies were screened for inclusion or exclusion with excellent interrater reliability (absolute agreement = 0.92). Discrepancies were resolved by the primary author and discussion between reviewers. The final sample included 110 studies (see Fig. 1).
Fig. 1.
Participant flowchart
Data extraction
Three coders (JK, KW, CM) extracted the data from the eligible studies using a double-coding method. To improve interrater reliability, three rounds of preliminary coding with a random sample of 20 studies was conducted, and discrepancies were discussed as a group to identify areas of potential concern. Any discrepancies identified during the formal coding process were resolved via discussion. Protocol papers were searched for relevant outcomes where required. Data for research questions 2, 4, and 5 were extracted by one reviewer (JK) reading each article and coding as yes or no, and specific responses were recorded verbatim. The data file for this project is stored in the Centre for Open Science data repository. Link: https://osf.io/4r6zn/?view_only=9ae914f335d34f9baa873fa44eccada6.
Number of participants randomised
Sex of participants
Data were extracted for the sex of participants as male, female, other, or not reported. Interrater agreement on this item was > 99%. In studies that reported sex data for a completer’s sample rather than the entire randomised sample, unidentified participants were categorised as ‘not reported’. A single study used an ‘other’ category for participants who did not identify as male or female. As such, for the purpose of this study, where the number of females was the only sex reported, it was assumed that the rest of the sample was male (and vice versa).
Country
The country each trial was conducted in was coded verbatim (agreement1 = 100%).
Year
Year of publication was coded based on the year the paper was published in a specific issue (agreement = 98%).
Co-occurring physical health condition
Whether or not studies included participants with a specific co-occurring physical health condition, to depression, was coded as yes or no (agreement = 99%).
Co-occurring mental health diagnosis
Whether or not studies included participants with a co-occurring mental health diagnosis, to depression, was coded as yes or no (agreement = 99%).
Depression determination method
The method of diagnosing depression was coded as: screening tool (e.g., PHQ), clinical/diagnostic interview, or both which was a combination of screening tool and interview (agreement = 77%).
Recruitment method
The recruitment method was either classified as direct, indirect, or a combination of each. In studies that used direct recruitment, potential participants were personally invited to participate in the study. In studies that used indirect recruitment, potential participants were exposed to non-specific study information (typically characterised by advertisements) and took initiative to register. A combination of each approach was coded as a separate category (agreement = 77%).
Intervention type
Within each study, individual interventions were categorised as psychotherapy, lifestyle, a combined psychotherapy and lifestyle approach, other therapeutic interventions, or control groups. Other therapeutic interventions were those that did not meet the criteria for being a psychotherapy or lifestyle program, such as medication. All interventions labelled as control groups, including usual care, were coded accordingly (agreement = 92%).
Intervention style
Given the published literature on men’s potential preference for Cognitive Behaviour Therapy over other types of therapy, the intervention style in psychotherapy interventions was coded as either Cognitive Behavioural Therapy or all other types of psychotherapy interventions (e.g., psychodynamic therapy, emotion-focused therapy). Interventions were considered part of the Cognitive Behaviour Therapy umbrella of interventions if they were based on first wave (e.g., behavioural activation), second wave (e.g., CBT) or third wave therapies (e.g., Acceptance and Commitment Therapy). For lifestyle programs, the style was selected from a range of options, such as physical activity or diet. However, physical activity programs were the only style of lifestyle program used outside of those in combined psychotherapy and lifestyle studies or not categorised studies, which used different styles across each arm (agreement = 89%).
Mode of delivery
Delivery mode was coded as face-to-face group, face-to-face individual, distance methods (online/technology/phone calls/printed materials), and unclear/not reported. These data were coded based on the primary mode of delivery, judged by time of contact (agreement = 89%).
Contact
Whether the intervention required contact with other people, including professionals, peers, family members, was coded into four groups: (1) involved contact with others, (2) self-guided with minimal contact (e.g., seeing someone briefly at the beginning or end), and (3) completely self-guided (agreement = 89%).
Sessions per week
The total duration of the intervention was coded in weeks and number of sessions was recorded. Where necessary, sessions were discrete contacts with individuals delivering the program, or in the case of self-guided interventions, modules were considered sessions. These two variables were combined to create sessions/per week (agreement = 75%). Where either number of sessions or length of intervention was unclear/not reported, sessions per week could not be calculated.
Data analysis
All analyses were conducted using IBM SPSS Statistics (version 27) predictive analytics software. Means for quantitative variables and percentages for categorical variables were calculated. To investigate the first research question, the representation of men was examined as a proportion of total participants across all studies, and within studies that allowed males to participate. For the second research question, independent samples t tests and analyses of variance investigated whether the proportion of male participants across the studies varied by key study or intervention characteristics. Because the RCT design precludes participants from choosing a particular intervention arm, studies testing multiple interventions that differed on a particular characteristic (e.g., online mode of delivery vs. face-to-face mode of delivery) were not included in that particular analysis. Similarly, studies that explicitly excluded males or females were also excluded from the moderator analyses.
Results
Most studies were published in the United States (29%), followed by the United Kingdom (16%), The Netherlands (7%), and Germany (6%). The number of studies published has increased over time, with 10% of studies published in 2011–2012 and 29% published between 2019 and 2021. Regarding co-occurring conditions with depression, 21% of studies explicitly recruited participants with a co-occurring physical health condition, but only 2% targeted those with co-occurring mental health condition. Approximately half of the studies diagnosed depression using both a screening tool and diagnostic interview (51%); a quarter used a screening tool only (26%); and a quarter used a diagnostic interview only (23%). The most common recruitment method was direct recruitment (67%), followed by a combination of direct and indirect, (20%) followed by indirect alone (13%).
Regarding intervention characteristics, most studies tested psychotherapy interventions only (82%), followed by integrated interventions that included both psychotherapy and lifestyle components (6%). Only 3% of studies tested lifestyle approaches exclusively and 10% were not categorised, indicating that intervention types were not consistent across study arms (e.g., psychotherapy arm vs. lifestyle arm). In terms of intervention style, the most common was CBT and third wave cognitive therapies (52%), followed by all other types of psychotherapy (20%), followed by physical activity (3%), and 26% were not categorised due to differences across study arms. Most studies tested interventions that were delivered individually face-to-face (49%) compared to remote interventions (26%, e.g., online/tech interventions, phone consultations, printed materials) or face-to-face group sessions (16%). Most studies tested interventions that involved repeated contact with another person (86%) with fewer studies involving one-off contact (6%), or no contact at all (4%). Intervention dose was mostly one session per week (48%), followed by less than one session per week (30%), and greater than one session per week (22%; 0.1-7 per week) (Table 1).
Table 1.
Characteristics of included studies
| Study characteristic | Studies, n | Study, % |
|---|---|---|
| Country | 110 | 100 |
| United States | 32 | 29 |
| United Kingdom | 18 | 16 |
| Netherlands | 8 | 7 |
| Germany | 7 | 6 |
| Australia | 5 | 5 |
| Othera | 40 | 36 |
| Year | ||
| 2011–2012 | 11 | 10 |
| 2013–2014 | 20 | 18 |
| 2015–2016 | 24 | 22 |
| 2017–2018 | 23 | 21 |
| 2019–2021 | 32 | 29 |
| Study sample | ||
| Female only | 19 | 17 |
| Male only | 0 | 0 |
| Allowed men to participate* | 90 | 82 |
| Sex data not reported | 1 | 1 |
| Co-occurring physical health condition | ||
| Yes | 23 | 21 |
| No | 87 | 79 |
| Co-occurring mental health condition | ||
| Yes | 2 | 2 |
| No | 108 | 98 |
| Depression determination method | ||
| Screening tool | 29 | 26 |
| Clinical/diagnostic interview | 25 | 23 |
| Both screening tool & clinical/diagnostic interview | 56 | 51 |
| Recruitment method | ||
| Direct | 74 | 67 |
| Indirect | 14 | 13 |
| Both direct & indirect | 22 | 20 |
| Intervention type | ||
| Psychotherapy | 90 | 82 |
| Lifestyle | 3 | 3 |
| Combined | 6 | 6 |
| Not categorised b | 11 | 10 |
| Intervention style | ||
| CBT & third wave | 57 | 52 |
| All other types of psychotherapy intervention | 22 | 20 |
| Physical activity | 3 | 3 |
| Not categorised b | 28 | 26 |
| Mode of delivery | ||
| Face-to-face Group | 18 | 16 |
| Face-to-face Individual | 54 | 49 |
| Online/tech/phone calls/printed materials | 29 | 26 |
| Unclear/not reported | 3 | 3 |
| Not categorised b | 6 | 5 |
| Contact | ||
| Involved contact | 95 | 86 |
| Self-guided with minimal contact | 7 | 6 |
| Completely self-guided | 4 | 4 |
| Not categorised b | 4 | 4 |
| Sessions per week | ||
| < 1 | 23 | 30 |
| 1 | 37 | 48 |
| > 1 | 17 | 22 |
a Spain (n = 4), Finland (n = 3), Denmark (n = 3), India (n = 3), Pakistan (n = 3), Brazil (n = 3), Iran (n = 3), Japan (n = 3), South Korea (n = 2), Nigeria (n = 2), Switzerland (n = 2), Turkey (n = 1), Korea (n = 1), Canada (n = 1), Hong Kong (n = 1), Italy (n = 1), New Zealand (n = 1), Sweden (n = 1), Kenya (n = 1), Taiwan (n = 1). b Study included > 1 intervention arm that differed on this characteristic (e.g., online vs. face to face). * Refers to studies which did not restrict eligibility to males or females
Research question 1: what is the representation of males in psychotherapy and lifestyle interventions targeting depression?
Across all 110 eligible studies (n = 24,397), males represented 26% (n = 6,303) of participants, females represented 73% (n = 17,712), 2% (n = 381) were unclear, and a single participant did not identify as male or female. Within the 90 (n = 20,252) studies that allowed both men and women to participate, males represented 31% (n = 6,303) of participants compared to 68% (n = 13,738) female, and 1% (n = 210) were unclear (Table 2).
Table 2.
Participant representation across all studies
| n | % (of randomised) | % (of reported) | |
|---|---|---|---|
| All studies (n = 110) | 24,397 | ||
| Male | 6,303 | 26 | 26 |
| Female | 17,712 | 73 | 73 |
| Other | 1 | 0 | 0 |
| Not reported | 381 | 2 | n/a |
| Studies including both genders (n = 90) | 20,252 | ||
| Male | 6,303 | 31 | 31 |
| Female | 13,738 | 68 | 69 |
| Other | 1 | 0 | 0 |
| Not reported | 210 | 1 | n/a |
Note. 19 studies either recruited women only as the target group or excluded men from participating. One study didn’t explicitly exclude men, but had a 100% female sample
Research question 2: were any attempts made to increase the involvement or, and if so, what were they?
No studies reported any explicit attempt to increase the involvement of men through targeted strategies.
Research question 3: are males more or less likely to participate in studies with certain characteristics? (Tables 3 and 4)
Table 3.
Male representation across study characteristics
| Study characteristic | N (%) | % Male (M, SD) | p-value |
|---|---|---|---|
| Year | |||
| 2011–2015 | 35 (39) | 30 (17) | |
| 2016–2018 | 30 (33) | 33 (13) | |
| 2019–2021 | 25 (28) | 32 (18) | 0.83 |
| Co-occurring physical or mental health condition | |||
| Yes | 19 (21) | 29 (17) | |
| No | 71 (79) | 32 (15) | 0.46 |
| Diagnosis | |||
| Screening tool | 19 (21) | 35 (17) | |
| Clinical/diagnostic interview | 23 (25) | 32 (20) | |
| Both | 48 (54) | 30 (12) | 0.60 |
| Recruitment method | |||
| Direct | 58 (64) | 34 (17) | |
| Indirect | 13 (14) | 28 (14) | |
| Both | 19 (21) | 27 (12) | 0.22 |
Table 4.
Male representation across intervention level characteristics
| Intervention level | N (%) | % Male (M, SD) | p-value |
|---|---|---|---|
| Intervention type | |||
| Psychotherapy | 73 (91) | 32 (16) | |
| Combined + Lifestyle | 7 (9) | 24 (10) | 0.19 |
| Psychotherapy stylea | |||
| CBT/ Third Wave | 48 (75) | 33 (17) | |
| All other types | 16 (25) | 30 (13) | 0.58 |
| Mode | |||
| Face-to-face (group) | 14 (17) | 28 (13) | |
| Face-to-face (individual) | 45 (54) | 32 (16) | |
| Online/tech/phone calls/printed materials | 24 (29) | 30 (12) | 0.58 |
| Contact | |||
| Involved Contact | 76 (88) | 32 (16) | |
| Self-guidedb | 10 (12) | 29 (11) | 0.65 |
| Dose (sessions per week) | |||
| < 1 | 18 (28) | 30 (10) | |
| 1 | 30 (47) | 30 (19) | |
| > 1 | 16 (25) | 33 (16) | 0.80 |
a Refers to types of psychotherapy only. b Includes studies that were self-guided with minimal contact or completely self-guided
Year
Male involvement did not vary significantly over time (F2,87 = 0.19, p = 0.83). To account for the escalating publication rate, studies were analysed in three groups of approximately equal size. Overall, males represented 30%, 33%, and 32% of participants in studies published from 2011 to 2015, 2016 to 2018, and 2019 to 2021, respectively.
Co-occurring physical or mental health condition
There was no significant difference in male involvement between studies targeting participants with a co-occurring physical or mental health condition (29%) or those without a co-occurring condition (32%; t88 = -7.40, p = 0.46). The most common co-occurring physical health conditions targeted were diabetes (4 studies), overweight or obesity (2 studies), and chronic pain (2 studies).
Depression determination method
Male involvement did not differ significantly depending on the method of diagnosing depression (F2,87 = 0.51, p = 0.60). Although trials that used a screening tool only had a higher proportion of males (35%) compared to trials that used an interview only (32%), and trials that used both a screening tool and interview (30%), the difference was not significant.
Recruitment method
Recruitment method did not have a significant influence on male involvement (F2,87 = 1.55, p = 0.22). The highest mean proportion of males were recruited directly (33%), compared to indirect recruitment (28%), and when a combination of methods were used (27%).
Intervention type
In this analysis, studies that tested integrated interventions and lifestyle interventions alone were combined, as only one lifestyle intervention allowed men to participate. The mean proportion of males participating in studies testing psychotherapy interventions (32%) was higher than in studies testing integrated interventions or lifestyle interventions combined (24%), however, the mean difference was not significant (t78 = 1.32, p = 0.19).
Psychotherapy intervention style
Among studies that tested psychotherapy interventions only, male involvement did not differ between studies testing CBT/Third wave cognitive therapies (33%) compared to other types of psychotherapy therapy (30%; t62 = 0.55, p = 0.58).
Mode of delivery
Mode of delivery did not have a significant effect on male involvement (F2,80 = 0.54, p = 0.58). The mean number of males was similar across all three modes: face-to-face group (28%), face-to-face individual (32%), remote delivery (online/technology/phone calls/printed materials; 30%). The various modes included in the remote delivery group were combined because they are conceptually similar in that they require low contact.
Contact
There was no difference in male participation between interventions that involved repeated contacts with intervention or research staff (32%), compared to self-guided or minimal contact interventions (29%; t84 = 0.46, p = 0.65). The self-guided group consisted of studies that involved some contact (e.g., a single face-to-face session followed by 10 online modules), and completely self-guided interventions. These two groups were combined because they are conceptually similar in both requiring low contact and only four studies tested completely self-guided interventions.
Dose (sessions per week)
No association was detected between male participation and the dose of the intervention (F2,61 = 0.23, p = 0.80). Slightly more men participated in studies testing interventions that were delivered using > 1 sessions per week (33%) than < 1 session per week (30%) and 1 session per week (30%).
Research question 4: did any studies specifically target men only, and/or tested gender-tailored interventions designed for men?
No studies targeted men only, and by virtue of this no studies tested interventions that were gender tailored towards men. Both studies with > 90% males were war veteran samples. The next highest representation of men was 67% in alcohol dependent individuals followed by 65% in a prison sample. In contrast, 19 studies explicitly recruited females only (17%) whilst two others consisted of a 100% female sample despite allowing men to participate.
Research Question 5: in studies with < 40% males, did the authors identify the lack of men as a limitation?
Out of 72 studies that had less than 40% males, including two studies that had complete female samples (but had not actually excluded men from participating), ten studies (14%) identified that the underrepresentation of men (or the overrepresentation of women) was a limitation. Consistent with a previous review, underrepresentation was defined as < 40% males (Pagoto et al., 2012).
Research Question 6: how many studies explicitly reported testing for sex differences in study outcome, or reported outcomes for men and women separately?
Out of 90 studies, 12 (13%) explicitly reported testing for sex differences as a moderator or reported primary outcomes for men and women separately. Ten of these studies reported no difference in intervention effect between males and females, one study reported women performed better than men, and one study was unclear due to gender outcomes being reported as part of racial subgroups rather than male and female groups.
Discussion
To our knowledge, this is the first scoping review to quantify the number of males involved in psychotherapy and lifestyle interventions targeting depression and identify any key study characteristics that moderate male involvement. Across all included studies, men represented only 26% of randomised participants. The review did not identify any randomised trials that have tested the efficacy of a psychotherapy or lifestyle-based intervention specifically targeting depression in men. In contrast, 19 studies (17%) specifically targeted females. No study or intervention characteristics moderated the level of male representation, with males underrepresented across all study types. Despite this, only ten studies suggested that the lack of male participants was a limitation.
The principal finding that men represent 26% of participants in RCTs targeting depression confirms a significant translational gap exists in clinical decision making for depression. Our results are similar to a review of psychosocial interventions for suicidal ideation and behaviour, which are both constructs related to depression (Nock et al., 2009). The proportion of men in the trials ranged from 37% in self-harm behaviour follow-up studies to 48% in school-based interventions (Krysinska et al., 2017). Although male depression prevalence is approximately half of female prevalence (WHO, 2017), with some evidence suggesting this is an underestimation of male cases (Martin et al., 2013), our results indicate males represent less than half of participants. Given men are less likely to seek help for depression than women (Addis & Mahalik, 2003), it is not surprising that fewer men are involved in depression trials than women. This gap is likely wider outside of research trials, given the men participating in RCTs are considered ‘help-seekers’ as they have generally attended a health service and been referred to the trial or signed up on their own volition. Previous research has indicated that negative self-stigma associated with help-seeking (Vogel et al., 2006) may contribute to men’s underrepresentation in both treatment services and research (Mahalik & Di Bianca, 2021; Mahalik et al., 2003). Thus, it is unlikely that the identified group of studies for the current review provide a good scope of barriers and facilitators to the engagement of men in the context of depression.
The current review found no studies testing interventions that were specifically designed for men, or studies testing standard interventions in male-only environments. In contrast, 19 studies used completely female samples and generally targeted peri or post-natal depression. Our results are similar to other reviews (Castro et al., 2020). For example, Strokoff, Halford, and Owen (Strokoff et al., 2016) conducted a review of 15 studies employing male-targeted psychotherapy treatment approaches and identified only a single, small (n = 23), randomised study examining a treatment specifically tailored for men (Syzdek et al., 2014). This study tested the effect of single session gender-based motivational interviewing on mental health symptoms, stigma, and help-seeking in a community sample of 23 men with mild to moderate internalising symptoms; none of the findings were significant (Syzdek et al., 2014). Similarly, a review of male-only lifestyle behaviour change interventions retrieved no studies that: (i) targeted pre-existing mental health conditions, or (ii) were powered to detect changes in mental health outcomes, or included substantive mental health support (Drew et al., 2020). Research has shown that men will seek help when it is accessible, appropriate, and engaging (Seidler et al., 2016). However, men remain unlikely to attend a full course of psychotherapy (Zimmermann et al., 2017) and report negative attitudes towards psychotherapy treatments (Levant et al., 2011). In a sample of Australian men who had previously attended therapy, a drop-out rate of 44.8% reflects the current state of services experienced by many men in Western mental healthcare (Harris et al., 2015; Seidler, Rice, Ogrodniczuk, et al., 2018; Seidler et al., 2021). Concerningly, recommendations for large-scaled controlled trials testing tailored treatments for men were made over 15 years ago (Cochran, 2005). Despite some theoretical advancement (Addis, 2008), along with recommendations and guidelines for clinical practice with males (APA, 2018; Mahalik et al., 2012), our results indicate that development of programs targeting men’s mental health remains a key area of future research. Without evidence based programs, men’s mental health will perpetually fall short of policy consideration, clinical attention, and required funding (Seidler et al., 2018).
The representation of men in depression trials has not increased over the past decade. This finding is somewhat surprising given the field of men’s health in general has gained traction in recent years (Addis & Cohane, 2005). Public health approaches (e.g., Real Men Real Depression) (Rochlen et al., 2005) play an important part in increasing men’s uptake of mental health services, and appear to be having some positive effects; men’s help seeking for mental and substance use disorders increased from 32% in 2006–2007 to 40% in 2011–2012 (Harris et al., 2015). However, our results show that an increase in help-seeking is not translating into participation in research trials. More targeted recruitment strategies, such as gender-tailored brochures, are effective for improving men’s attitudes towards help-seeking, but like public campaigns, they do not guarantee men will receive an engaging treatment upon seeking help (Seidler et al., 2018). Indeed, the process of help-seeking does not solely involve the act of ‘reaching out’, but also the treatments that follow (Seidler et al., 2016). As such, lower rates of help-seeking in men may be better attributed to the lack of engaging, relevant or accessible mental health treatments (Bilsker et al., 2018; Seidler et al., 2018).
Men’s representation did not differ depending on the presence of a co-occurring mental or physical health condition. However, targeting men with co-occurring conditions might still be a valuable engagement strategy. Substance use disorders are highly prevalent in men and co-occurrence with depression is common (Burns & Teesson, 2002). Similarly, a reciprocal link exists between depression and overweight or obesity (Luppino et al., 2010), particularly in men (Magovcevic & Addis, 2008). In our review, two of the most common co-occurring physical health conditions targeted were diabetes and overweight or obesity. Although we found men’s representation did not differ based on the presence of co-occurring conditions, it is not surprising given men’s representation was low overall. As such, offering integrated programs targeting multiple conditions remains a potential solution to improving men’s representation in mental health trials (Kingerlee et al., 2014; McGale et al., 2011).
Interestingly, this review found that men were equally likely to participate in psychotherapy interventions compared to lifestyle interventions. Observational data indicates physical activity and healthy eating are two of the top five strategies men with depression use to manage their mental health (Proudfoot et al., 2015). Additionally, mental health promotion can be integrated into lifestyle programs once men are engaged (Sharp et al., 2018; Sharp et al., 2022). Despite the proclaimed utility of lifestyle approaches (Sharp et al., 2018), the low representation of men in these interventions is consistent with a systematic review of male inclusion in lifestyle behaviour change programs finding that men represented only 27% of participants (Pagoto et al., 2012). These findings may be attributed to the lack of male-only studies, as men can be deterred by the presence of women in lifestyle programs (Morgan et al., 2011). To better engage men, ‘gender-tailored’ programs which specifically account for men’s unique preferences and values are being developed and tested (Morgan et al., 2009; Morgan et al., 2011). These programs have provided promising results for both engagement and effectiveness in treating mental and physical health (Sharp et al., 2020; Sharp et al., 2021; Young et al., 2012; Young et al., 2021). Despite this, no gender-tailored lifestyle programs were found in this review. Men’s representation was slightly higher (32%) in psychotherapy interventions compared to lifestyle interventions (24%), but the difference was not significant, and the lack of male-specific approaches limits the conclusions that can be drawn. To properly investigate the question of whether men prefer a lifestyle approach or mental health approach for managing depression, male-only programs of each type must be developed and tested.
Our finding that men’s representation did not differ between CBT and other treatment types is inconsistent with evidence CBT is men’s preferred treatment (Emslie et al., 2007; Liddon et al., 2018; Seidler et al., 2016), and recommendations by researchers supporting its utility with men (Englar-Carlson & Stevens, 2006; Spendelow, 2015). For example, behavioural interventions delivered with the context of CBT, such as behavioural activation (Skärsäter et al., 2003), are dubbed male-friendly due to their practical and tangible nature (Brooks, 2010). Recently, a vignette-based study found gender role socialisation, self-stigma, and attitudes towards professional psychotherapy help negatively predicted willingness to engage in psychotherapy regardless of therapy orientation, including CBT (Cole et al., 2019), suggesting that therapy type is irrelevant for these men. Comparatively, the men in the current sample are largely help-seekers, which may suggest that type of therapy is also irrelevant when help-seeking intentions are present. However, given men’s representation was low across all programs, our ability to draw a definitive conclusion is limited.
This review found men’s representation did not differ across delivery mode, the level of contact with other people in the intervention, or dose. Specifically, the finding that men’s representation was similar for individual and group delivery is inconsistent with previous research suggesting men prefer individual therapy (Kealy et al., 2021; Sierra Hernandez et al., 2014). Moreover, despite recent research suggesting that online interventions may be particularly appealing to men (Berger et al., 2013; Ellis et al., 2013; Wang et al., 2016), our results suggest men were less likely to engage in online studies compared to those testing face-to-face delivery modes. Similarly, they did not appear to prefer self-guided interventions to those which required more regular contact with the intervention team. However, research investigating preferences for therapy type (e.g., CBT) and trial characteristics has typically used survey methods whereby preferences are selected based on vignettes or prior experience (Cole et al., 2019; Kealy et al., 2021; Liddon et al., 2018; Sierra Hernandez et al., 2014). An issue with this approach is that it fails to consider the impact of multiple intervention characteristics on men’s choices. Comparatively, our results must be viewed in context of trials comprising many combinations of type, mode, and length. As such, previous findings regarding preferences that are independent of other trial components are unlikely to be translated into real world representation. Ultimately, our results suggest that men’s preferences are heterogenous and a suite of intervention options are required that provides men the ability to choose (Seaton et al., 2017).
Our review found that men’s representation did not differ between direct or indirect recruitment. Similarly, it did not differ between the method of determining depression status (interview, screening tool, or both). When considered together, these two findings indicate current methods of recruiting and including men into depression trials are inadequate. Further, we found that no attempts were made to increase the involvement of men (e.g., through targeted recruitment). It is important to conduct more research in this area as men are more difficult to recruit, because they are reluctant to admit they have depression (Firth et al., 2019), are less likely to be diagnosed (Cochran & Rabinowitz, 2003; Kessler, 2000; Oliffe & Phillips, 2008), and are affected by social and self-stigma due to rigid masculine norms. Yet, targeted efforts to recruit men in male-only lifestyle programs have demonstrated some success (Seaton et al., 2017). For example, the SHED-IT (Self-Help, Exercise and Diet using Information Technology): Recharge program recruited men with overweight or obesity and depressive symptoms through gender-tailored advertising (e.g., “lose weight without giving up beer”) and using the programs credibility as a university-based intervention for further appeal (Drew et al., 2021) which aligned with insights from other gender-tailored programs (Aguiar et al., 2017; Morgan et al., 2011; Morgan et al., 2016). Similar male-specific recruitment methods, such as using sports language (e.g., ‘mental fitness’) rather than mental illness are useful in the mental health context (Cooper et al., 2015). However, minimal research has been conducted on recruiting men into gender-neutral programs, particularly for psychotherapy, and trials typically do not report details on recruitment strategies making it difficult to know what extent targeted strategies were used. A potential way of increasing male engagement without targeted recruitment efforts is using male-specific psychometric tools to evaluate study eligibility, as men are often less willing to report depressive symptoms using existing diagnostic scales (Fields & Cochran, 2011). Scales such as the Masculine Depression Scale (MDS; Magovcevic & Addis, 2008) and Masculine Depression Risk Scale (MDRS-22; Rice et al., 2013) have been designed to detect externalising symptoms of depression common in men, but are yet to be adopted into mainstream research practices (Rice et al., 2019).
Despite the clear underrepresentation of men in the studies, very few identified that this was a limitation. Similarly, few explicitly reported testing for sex as a potential moderator of intervention effects. These results are similar to a review of psychosocial interventions for suicidal ideation and behaviour which found 18% of 154 trials reported or examined differences in gender subgroups and only a single study used an all-male sample (Krysinska et al., 2017). Although psychotherapy outcomes are largely reported as similar for men and women (Staczan et al., 2017), some studies have had mixed findings (Ogrodniczuk et al., 2001; Parker et al., 2011). Crucially, many studies do not report gender differences in the outcome (Parker et al., 2011), including several meta-analyses of psychotherapy for depression (Cuijpers et al., 2021; Cuijpers et al., 2008; Nieuwsma et al., 2012). This is a considerable limitation (Butler et al., 2006), especially given men represented only a third of participants in this review, and limits generalisability of results. However, substantially more women are diagnosed with depression than men (WHO, 2017). One could therefore expect there to be less men involved in trials of depression. Yet, depressive disorders affect 109 million men worldwide (GBD, 2022). As such, the view that men are underrepresented in research trials due to inherently lower prevalence overlooks the needs of men and reinforces ‘male gender-blindness’ (Seager et al., 2014).
This review had several strengths. To our knowledge, it is the first review to quantify the number of men involved in psychotherapy and lifestyle interventions targeting depression. Regarding methodology, this reviewed considered adequately-powered RCTs only, given these are likely to be given the highest priority for informing evidence-based practice and guidelines. Finally, all data were extracted by two reviewers, and the conduct and reporting of the review adhered to the PRISMA guidelines. This review also has some limitations. Firstly, due to the considerable size of the depression literature, relevant subject headings were used to streamline the search process. Whilst our search was not exhaustive, we believe it was extensive and the included studies were likely representative of other studies that may not have been included. Secondly, by including studies that were explicitly powered at 80% to detect changes in depression, studies with adequate sample size may have been excluded based on not reporting a power calculation. However, power calculations are important for ensuring existing effects are able to be detected, using the appropriate amount of resources, and larger sample sizes provide better population estimates (Field, 2013; Noordzij et al., 2010).
Conclusion
The underrepresentation of men in psychotherapy or lifestyle intervention trials targeting depression is a significant concern given men’s substantial prevalence of depression and low rates of help-seeking (WHO, 2017). The results of this review suggest men are equally underrepresented across all intervention and study characteristics, despite male participants in trials already potentially having overcome many attitudinal and stigma-related barriers to help-seeking. To better understand men’s preferences, programs that are specifically designed for and appeal to men are urgently required, and research carried out to understand what prompts help seeking in men specifically. Continuing to deliver gender-neutral programs fails to recognise the needs of men and implicitly accepting that men participate in depression trials at lower rates than women is stalling the field of men’s mental health. This review highlights the need for a concerted effort from researchers to design and test therapeutic approaches that are engaging and appealing for men.
Supplementary information
Below is the link to the electronic supplementary material.
(DOCX 23.4 KB)
(DOCX 26.4 KB)
Acknowledgements
The first author (JK) is supported by the University of Newcastle’s Academic Career Preparation Scholarship.
Data availability
The data file for this project is stored in the Centre for Open Science data repository. Link: https://osf.io/4r6zn/?view_only=9ae914f335d34f9baa873fa44eccada6.
Declarations
Conflict of interest
The authors declare no conflict of interest.
Footnotes
Agreement was calculated by dividing the number of discrepancies by the total number of responses on each item.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Addis ME. Gender and depression in men. Clinical Psychology: Science and Practice. 2008;15(3):153. [Google Scholar]
- Addis ME, Cohane GH. Social scientific paradigms of masculinity and their implications for research and practice in men’s mental health. Journal of Clinical Psychology. 2005;61(6):633–647. doi: 10.1002/jclp.20099. [DOI] [PubMed] [Google Scholar]
- Addis ME, Mahalik JR. Men, masculinity, and the contexts of help seeking. American Psychologist. 2003;58(1):5. doi: 10.1037/0003-066x.58.1.5. [DOI] [PubMed] [Google Scholar]
- Aguiar EJ, Morgan PJ, Collins CE, Plotnikoff RC, Young MD, Callister R. Process evaluation of the type 2 diabetes mellitus PULSE program randomized controlled trial: recruitment, engagement, and overall satisfaction. American Journal of Men’s Health. 2017;11(4):1055–1068. doi: 10.1177/1557988317701783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders: DSM-5.
- American Psychiatric Association (2018). APA guidelines for psychological practice with boys and men. https://www.apa.org/about/policy/boys-men-practice-guidelines.pdf
- Barth J, Munder T, Gerger H, Nüesch E, Trelle S, Znoj H, Cuijpers P. Comparative efficacy of seven psychotherapeutic interventions for patients with depression: A network meta-analysis. Focus. 2016;14(2):229–243. doi: 10.1176/appi.focus.140201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger JL, Addis ME, Green JD, Mackowiak C, Goldberg V. Men’s reactions to mental health labels, forms of help-seeking, and sources of help-seeking advice. Psychology of Men & Masculinity. 2013;14(4):433. doi: 10.1037/a0030175. [DOI] [Google Scholar]
- Berryhill MB, Culmer N, Williams N, Halli-Tierney A, Betancourt A, Roberts H, King M. Videoconferencing psychotherapy and depression: A systematic review. Telemedicine and e-Health. 2019;25(6):435–446. doi: 10.1089/tmj.2018.0058. [DOI] [PubMed] [Google Scholar]
- Bertakis KD, Helms LJ, Callahan EJ, Azari R, Leigh P, Robbins JA. Patient gender differences in the diagnosis of depression in primary care. Journal of Women’s Health & Gender-based Medicine. 2001;10(7):689–698. doi: 10.1089/15246090152563579. [DOI] [PubMed] [Google Scholar]
- Bilsker D, Fogarty AS, Wakefield MA. Critical issues in men’s mental health. The Canadian Journal of Psychiatry. 2018;63(9):590–596. doi: 10.1177/0706743718766052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brommelhoff JA, Conway K, Merikangas K, Levy BR. Higher rates of depression in women: Role of gender bias within the family. Journal of Women’s Health. 2004;13(1):69–76. doi: 10.1089/154099904322836474. [DOI] [PubMed] [Google Scholar]
- Brooks, G. R. (2010). Beyond the crisis of masculinity: A transtheoretical model for male-friendly therapy. American Psychological Association.
- Burns L, Teesson M. Alcohol use disorders comorbid with anxiety, depression and drug use disorders: Findings from the Australian National Survey of Mental Health and Well Being. Drug and Alcohol Dependence. 2002;68(3):299–307. doi: 10.1016/s0376-8716(02)00220-x. [DOI] [PubMed] [Google Scholar]
- Butler AC, Chapman JE, Forman EM, Beck AT. The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review. 2006;26(1):17–31. doi: 10.1016/j.cpr.2005.07.003. [DOI] [PubMed] [Google Scholar]
- Castro A, Gili M, Ricci-Cabello I, Roca M, Gilbody S, Perez-Ara M, McMillan D. Effectiveness and adherence of telephone-administered psychotherapy for depression: A systematic review and meta-analysis. Journal of Affective Disorders. 2020;260:514–526. doi: 10.1016/j.jad.2019.09.023. [DOI] [PubMed] [Google Scholar]
- Churchill SA, Farrell L. Alcohol and depression: Evidence from the 2014 health survey for England. Drug and Alcohol Dependence. 2017;180:86–92. doi: 10.1016/j.drugalcdep.2017.08.006. [DOI] [PubMed] [Google Scholar]
- Cochran SV. Evidence-based assessment with men. Journal of Clinical Psychology. 2005;61(6):649–660. doi: 10.1002/jclp.20100. [DOI] [PubMed] [Google Scholar]
- Cochran SV, Rabinowitz FE. Gender-sensitive recommendations for assessment and treatment of depression in men. Professional Psychology: Research and Practice. 2003;34(2):132. doi: 10.1037/0735-7028.34.2.132. [DOI] [Google Scholar]
- Cole BP, Petronzi GJ, Singley DB, Baglieri M. Predictors of men’s psychotherapy preferences. Counselling and Psychotherapy Research. 2019;19(1):45–56. [Google Scholar]
- Cooney G, Dwan K, Greig C, Lawlor D, Rimer J, Waugh F, Dwan C. Exercise for depression Cochrane database. Systematic Reviews. 2013;9:CD004366. doi: 10.1002/14651858.cd004366.pub6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper P, Stringer W, Howes J, Norton J. The state of mind boot room: Reducing social isolation and promoting mental fitness. British Journal of Mental Health Nursing. 2015;4(3):136–139. doi: 10.12968/bjmh.2015.4.3.136. [DOI] [Google Scholar]
- Cuijpers P, Quero S, Noma H, Ciharova M, Miguel C, Karyotaki E, Furukawa TA. Psychotherapies for depression: A network meta-analysis covering efficacy, acceptability and long‐term outcomes of all main treatment types. World Psychiatry. 2021;20(2):283–293. doi: 10.1002/wps.20860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Van Straten A, Andersson G, Van Oppen P. Psychotherapy for depression in adults: A meta-analysis of comparative outcome studies. Journal of Consulting and Clinical Psychology. 2008;76(6):909. doi: 10.1037/a0013075. [DOI] [PubMed] [Google Scholar]
- Drew RJ, Morgan PJ, Kay-Lambkin F, Collins CE, Callister R, Kelly BJ, Young MD. Men’s perceptions of a gender-tailored eHealth program targeting physical and mental health: Qualitative findings from the SHED-IT recharge trial. International Journal of Environmental Research and Public Health. 2021;18(24):12878. doi: 10.3390/ijerph182412878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drew RJ, Morgan PJ, Pollock ER, Young MD. Impact of male-only lifestyle interventions on men’s mental health: A systematic review and meta‐analysis. Obesity Reviews. 2020;21(7):e13014. doi: 10.1111/obr.13014. [DOI] [PubMed] [Google Scholar]
- Ellis LA, Collin P, Hurley PJ, Davenport TA, Burns JM, Hickie IB. Young men’s attitudes and behaviour in relation to mental health and technology: Implications for the development of online mental health services. BMC Psychiatry. 2013;13(1):119. doi: 10.1186/1471-244x-13-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emslie C, Ridge D, Ziebland S, Hunt K. Exploring men’s and women’s experiences of depression and engagement with health professionals: More similarities than differences? A qualitative interview study. BMC Family Practice. 2007;8(1):1–10. doi: 10.1186/1471-2296-8-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Englar-Carlson, M. E., & Stevens, M. A. (2006). the room with men: A casebook of therapeutic change. American Psychological Association.
- Fang H, Tu S, Sheng J, Shao A. Depression in sleep disturbance: A review on a bidirectional relationship, mechanisms and treatment. Journal of Cellular and Molecular Medicine. 2019;23(4):2324–2332. doi: 10.1111/jcmm.14170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field, A. (2013). Discovering statistics using IBM SPSS statistics. Sage.
- Fields AJ, Cochran SV. Men and depression: Current perspectives for health care professionals. American Journal of Lifestyle Medicine. 2011;5(1):92–100. doi: 10.1177/1559827610378347. [DOI] [Google Scholar]
- Firth J, Marx W, Dash S, Carney R, Teasdale SB, Solmi M, Jacka F. The effects of dietary improvement on symptoms of depression and anxiety: A meta-analysis of randomized controlled trials. Psychosomatic Medicine. 2019;81(3):265. doi: 10.1097/psy.0000000000000673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Burden of Disease (2022). Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet Psychiatry. 10.1016/s2215-0366(21)00395-3 [DOI] [PMC free article] [PubMed]
- Gee B, Orchard F, Clarke E, Joy A, Clarke T, Reynolds S. The effect of non-pharmacological sleep interventions on depression symptoms: A meta-analysis of randomised controlled trials. Sleep Medicine Reviews. 2019;43:118–128. doi: 10.1016/j.smrv.2018.09.004. [DOI] [PubMed] [Google Scholar]
- Gianfredi V, Blandi L, Cacitti S, Minelli M, Signorelli C, Amerio A, Odone A. Depression and objectively measured physical activity: A systematic review and meta-analysis. International Journal of Environmental Research and Public Health. 2020;17(10):3738. doi: 10.3390/ijerph17103738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris MG, Diminic S, Reavley N, Baxter A, Pirkis J, Whiteford HA. Males’ mental health disadvantage: An estimation of gender-specific changes in service utilisation for mental and substance use disorders in Australia. Australian & New Zealand Journal of Psychiatry. 2015;49(9):821–832. doi: 10.1177/0004867415577434. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: Results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Archives of General Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM. The comorbidity of major depression and anxiety disorders: Recognition and management in primary care. Primary Care Companion to the Journal of Clinical Psychiatry. 2001;3(6):244. doi: 10.4088/pcc.v03n0609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, Abdelalim A. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 2018;392(10159):1789–1858. doi: 10.1016/s0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Josefsson T, Lindwall M, Archer T. Physical exercise intervention in depressive disorders: Meta-analysis and systematic review. Scandinavian Journal of Medicine & Science in Sports. 2014;24(2):259–272. doi: 10.1111/sms.12050. [DOI] [PubMed] [Google Scholar]
- Josephine K, Josefine L, Philipp D, David E, Harald B. Internet-and mobile-based depression interventions for people with diagnosed depression: A systematic review and meta-analysis. Journal of Affective Disorders. 2017;223:28–40. doi: 10.1016/j.jad.2017.07.021. [DOI] [PubMed] [Google Scholar]
- Judd F, Komiti A, Jackson H. How does being female assist help-seeking for mental health problems? Australian & New Zealand Journal of Psychiatry. 2008;42(1):24–29. doi: 10.1080/00048670701732681. [DOI] [PubMed] [Google Scholar]
- Kealy D, Seidler ZE, Rice SM, Oliffe JL, Ogrodniczuk JS, Kim D. Challenging assumptions about what men want: Examining preferences for psychotherapy among men attending outpatient mental health clinics. Professional Psychology: Research and Practice. 2021;52(1):28. doi: 10.1037/pro0000321. [DOI] [Google Scholar]
- Kessler, R. C. (2000). Gender differences in major depressiondepression: Epidemiological findings. In E. Frank (Ed.), Gender and its effects on psychopathology (pp. 61–84). Washington, DC: American Psychiatric Publishing.
- Kingerlee R, Precious D, Sullivan L, Barry J. Engaging with the emotional lives of men. Psychology. 2014;27(6):418–421. [Google Scholar]
- Krysinska K, Batterham PJ, Christensen H. Differences in the effectiveness of psychosocial interventions for suicidal ideation and behaviour in women and men: A systematic review of randomised controlled trials. Archives of Suicide Research. 2017;21(1):12–32. doi: 10.1080/13811118.2016.1162246. [DOI] [PubMed] [Google Scholar]
- Levant RF, Wimer DJ, Williams CM. An evaluation of the Health Behavior Inventory-20 (HBI-20) and its relationships to masculinity and attitudes towards seeking psychological help among college men. Psychology of Men & Masculinity. 2011;12(1):26. doi: 10.1037/a0021014. [DOI] [Google Scholar]
- Liddon L, Kingerlee R, Barry JA. Gender differences in preferences for psychological treatment, coping strategies, and triggers to help-seeking. British Journal of Clinical Psychology. 2018;57(1):42–58. doi: 10.1111/bjc.12147. [DOI] [PubMed] [Google Scholar]
- Linde K, Rücker G, Sigterman K, Jamil S, Meissner K, Schneider A, Kriston L. Comparative effectiveness of psychological treatments for depressive disorders in primary care: Network meta-analysis. BMC Family Practice. 2015;16:103–103. doi: 10.1186/s12875-015-0314-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q, He H, Yang J, Feng X, Zhao F, Lyu J. Changes in the global burden of depression from 1990 to 2017: Findings from the Global Burden of Disease study. Journal of Psychiatric Research. 2020;126:134–140. doi: 10.1016/j.jpsychires.2019.08.002. [DOI] [PubMed] [Google Scholar]
- Lotfaliany M, Bowe SJ, Kowal P, Orellana L, Berk M, Mohebbi M. Depression and chronic diseases: Co-occurrence and communality of risk factors. Journal of Affective Disorders. 2018;241:461–468. doi: 10.1016/j.jad.2018.08.011. [DOI] [PubMed] [Google Scholar]
- Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG. Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Archives of General Psychiatry. 2010;67(3):220–229. doi: 10.1001/archgenpsychiatry.2010.2. [DOI] [PubMed] [Google Scholar]
- Lynch L, Long M, Moorhead A. Young men, help-seeking, and mental health services: Exploring barriers and solutions. American Journal of Men’s Health. 2018;12(1):138–149. doi: 10.1177/1557988315619469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magovcevic M, Addis ME. The Masculine Depression Scale: Development and psychometric evaluation. Psychology of Men & Masculinity. 2008;9(3):117. doi: 10.1037/1524-9220.9.3.117. [DOI] [Google Scholar]
- Mahalik, J. R., & Di Bianca, M. (2021). Help-seeking for depression as a stigmatized threat to masculinity. Professional Psychology: Research and Practice, 52(2), 146–155. 10.1037/pro0000365
- Mahalik JR, Good GE, Englar-Carlson M. Masculinity scripts, presenting concerns, and help seeking: Implications for practice and training. Professional Psychology: Research and Practice. 2003;34(2):123. doi: 10.1037/0735-7028.34.2.123. [DOI] [Google Scholar]
- Mahalik JR, Good GE, Tager D, Levant RF, Mackowiak C. Developing a taxonomy of helpful and harmful practices for clinical work with boys and men. Journal of Counseling Psychology. 2012;59(4):591. doi: 10.1037/a0030130. [DOI] [PubMed] [Google Scholar]
- Martin LA, Neighbors HW, Griffith DM. The experience of symptoms of depression in men vs women: Analysis of the National Comorbidity Survey Replication. JAMA Psychiatry. 2013;70(10):1100–1106. doi: 10.1001/jamapsychiatry.2013.1985. [DOI] [PubMed] [Google Scholar]
- McGale N, McArdle S, Gaffney P. Exploring the effectiveness of an integrated exercise/CBT intervention for young men’s mental health. British Journal of Health Psychology. 2011;16(3):457–471. doi: 10.1348/135910710x522734. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. International Journal of Surgery. 2010;8(5):336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- Molendijk M, Molero P, Sánchez-Pedreño FO, Van der Does W, Martínez-González MA. Diet quality and depression risk: A systematic review and dose-response meta-analysis of prospective studies. Journal of Affective Disorders. 2018;226:346–354. doi: 10.1016/j.jad.2017.09.022. [DOI] [PubMed] [Google Scholar]
- Morgan PJ, Lubans DR, Collins CE, Warren JM, Callister R. The SHED-IT randomized controlled trial: Evaluation of an Internet‐based weight‐loss program for men. Obesity (Silver Spring, Md.) 2009;17(11):2025–2032. doi: 10.1038/oby.2009.85. [DOI] [PubMed] [Google Scholar]
- Morgan PJ, Warren JM, Lubans DR, Collins CE, Callister R. Engaging men in weight loss: Experiences of men who participated in the male only SHED-IT pilot study. Obesity Research & Clinical Practice. 2011;5(3):e239–e248. doi: 10.1016/j.orcp.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Morgan PJ, Young MD, Smith JJ, Lubans DR. Targeted health behavior interventions promoting physical activity: A conceptual model. Exercise and Sport Sciences Reviews. 2016;44(2):71–80. doi: 10.1249/jes.0000000000000075. [DOI] [PubMed] [Google Scholar]
- Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: Results from the World Health Surveys. The Lancet. 2007;370(9590):851–858. doi: 10.1016/s0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- Newby JM, Twomey C, Li SSY, Andrews G. Transdiagnostic computerised cognitive behavioural therapy for depression and anxiety: A systematic review and meta-analysis. Journal of Affective Disorders. 2016;199:30–41. doi: 10.1016/j.jad.2016.03.018. [DOI] [PubMed] [Google Scholar]
- Nieuwsma JA, Trivedi RB, McDuffie J, Kronish I, Benjamin D, Williams JW., Jr Brief psychotherapy for depression: A systematic review and meta-analysis. The International Journal of Psychiatry in Medicine. 2012;43(2):129–151. doi: 10.2190/pm.43.2.c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A, De Girolamo G. Cross-national analysis of the associations among mental disorders and suicidal behavior: Findings from the WHO World Mental Health Surveys. PLoS Medicine. 2009;6(8):e1000123. doi: 10.1371/journal.pmed.1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noordzij M, Tripepi G, Dekker FW, Zoccali C, Tanck MW, Jager KJ. Sample size calculations: Basic principles and common pitfalls. Nephrology Dialysis Transplantation. 2010;25(5):1388–1393. doi: 10.1093/ndt/gfp732. [DOI] [PubMed] [Google Scholar]
- Ogrodniczuk JS, Piper WE, Joyce AS, McCallum M. Effect of patient gender on outcome in two forms of short-term individual psychotherapy. The Journal of Psychotherapy Practice and Research. 2001;10(2):69. [PMC free article] [PubMed] [Google Scholar]
- Oliffe JL, Phillips MJ. Men, depression and masculinities: A review and recommendations. Journal of Men’s Health. 2008;5(3):194–202. [Google Scholar]
- Oliver MI, Pearson N, Coe N, Gunnell D. Help-seeking behaviour in men and women with common mental health problems: Cross-sectional study. The British Journal of Psychiatry. 2005;186(4):297–301. doi: 10.1192/bjp.186.4.297. [DOI] [PubMed] [Google Scholar]
- Pagoto SL, Schneider KL, Oleski JL, Luciani JM, Bodenlos JS, Whited MC. Male inclusion in randomized controlled trials of lifestyle weight loss interventions. Obesity (Silver Spring, Md.) 2012;20(6):1234–1239. doi: 10.1038/oby.2011.140. [DOI] [PubMed] [Google Scholar]
- Parker G, Blanch B, Crawford J. Does gender influence response to differing psychotherapies by those with unipolar depression? Journal of Affective Disorders. 2011;130(1–2):17–20. doi: 10.1016/j.jad.2010.05.020. [DOI] [PubMed] [Google Scholar]
- Pirkis J, Spittal MJ, Keogh L, Mousaferiadis T, Currier D. Masculinity and suicidal thinking. Social Psychiatry and Psychiatric Epidemiology. 2017;52(3):319–327. doi: 10.1007/s00127-016-1324-2. [DOI] [PubMed] [Google Scholar]
- Primack JM, Addis ME, Syzdek M, Miller IW. The men’s stress workshop: A gender-sensitive treatment for depressed men. Cognitive and Behavioral Practice. 2010;17(1):77–87. doi: 10.1016/j.cbpra.2009.07.002. [DOI] [Google Scholar]
- Proudfoot J, Fogarty AS, McTigue I, Nathan S, Whittle EL, Christensen H, Wilhelm K. Positive strategies men regularly use to prevent and manage depression: A national survey of Australian men. BMC Public Health. 2015;15(1):1–14. doi: 10.1186/s12889-015-2478-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice SM, Aucote HM, Parker AG, Alvarez-Jimenez M, Filia KM, Amminger GP. Men’s perceived barriers to help seeking for depression: Longitudinal findings relative to symptom onset and duration. Journal of Health Psychology. 2017;22(5):529–536. doi: 10.1177/1359105315605655. [DOI] [PubMed] [Google Scholar]
- Rice SM, Fallon BJ, Aucote HM, Möller-Leimkühler AM. Development and preliminary validation of the male depression risk scale: Furthering the assessment of depression in men. Journal of Affective Disorders. 2013;151(3):950–958. doi: 10.1016/j.jad.2013.08.013. [DOI] [PubMed] [Google Scholar]
- Rice SM, Kealy D, Seidler ZE, Oliffe JL, Levant RF, Ogrodniczuk JS. Male-type and prototypal depression trajectories for men experiencing mental health problems. International Journal of Environmental Research and Public Health. 2020;17(19):7322. doi: 10.3390/ijerph17197322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice SM, Ogrodniczuk JS, Kealy D, Seidler ZE, Dhillon HM, Oliffe JL. Validity of the male depression risk scale in a representative Canadian sample: Sensitivity and specificity in identifying men with recent suicide attempt. Journal of Mental Health. 2019;28(2):132–140. doi: 10.1080/09638237.2017.1417565. [DOI] [PubMed] [Google Scholar]
- Rochlen AB, Whilde MR, Hoyer WD. The real men. Real depression campaign: Overview, theoretical implications, and research considerations. Psychology of Men & Masculinity. 2005;6(3):186. doi: 10.1037/1524-9220.6.3.186. [DOI] [Google Scholar]
- Santomauro DF, Herrera AMM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, Aravkin AY. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet. 2021;398(10312):1700–1712. doi: 10.1016/s0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuch FB, Vancampfort D, Richards J, Rosenbaum S, Ward PB, Stubbs B. Exercise as a treatment for depression: A meta-analysis adjusting for publication bias. Journal of Psychiatric Research. 2016;77:42–51. doi: 10.1016/j.jpsychires.2016.02.023. [DOI] [PubMed] [Google Scholar]
- Seager, M., SuLLivan, L., & Barry, J. (2014). The male psychology conference, university college London, June 2014. New Male Studies, 3(2), 41–68.
- Seaton CL, Bottorff JL, Jones-Bricker M, Oliffe JL, DeLeenheer D, Medhurst K. Men’s mental health promotion interventions: A scoping review. American Journal of Men’s Health. 2017;11(6):1823–1837. doi: 10.1177/1557988317728353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidler ZE, Dawes AJ, Rice SM, Oliffe JL, Dhillon HM. The role of masculinity in men’s help-seeking for depression: A systematic review. Clinical Psychology Review. 2016;49:106–118. doi: 10.1016/j.cpr.2016.09.002. [DOI] [PubMed] [Google Scholar]
- Seidler ZE, Rice SM, Ogrodniczuk JS, Oliffe JL, Dhillon HM. Engaging men in psychological treatment: A scoping review. American Journal of Men’s Health. 2018;12(6):1882–1900. doi: 10.1177/1557988318792157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidler ZE, Rice SM, Oliffe JL, Fogarty AS, Dhillon HM. Men in and out of treatment for depression: Strategies for improved engagement. Australian Psychologist. 2018;53(5):405–415. doi: 10.1111/ap.12331. [DOI] [Google Scholar]
- Seidler ZE, Wilson MJ, Kealy D, Oliffe JL, Ogrodniczuk JS, Rice SM. Men’s dropout from mental health services: Results from a survey of Australian men across the life span. American Journal of Men’s Health. 2021;15(3):15579883211014776. doi: 10.1177/15579883211014776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp P, Bottorff JL, Hunt K, Oliffe JL, Johnson ST, Dudley L, Caperchione CM. Men’s perspectives of a gender-sensitized health promotion program targeting healthy eating, active living, and social connectedness. American Journal of Men’s Health. 2018;12(6):2157–2166. doi: 10.1177/1557988318799159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp P, Bottorff JL, Oliffe JL, Hunt K, Caperchione CM. Process evaluation of HAT TRICK: Feasibility, acceptability and opportunities for programme refinement. Health Education Research. 2020;35(6):605–617. doi: 10.1093/her/cyaa029. [DOI] [PubMed] [Google Scholar]
- Sharp P, Bottorff JL, Rice S, Oliffe JL, Schulenkorf N, Impellizzeri F, Caperchione CM. “People say men don’t talk, well that’s bullshit”: A focus group study exploring challenges and opportunities for men’s mental health promotion. PLoS ONE [Electronic Resource] 2022;17(1):e0261997. doi: 10.1371/journal.pone.0261997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp P, Stolp S, Bottorff JL, Oliffe JL, Hunt K, Caperchione CM. Can lifestyle interventions improve Canadian men’s mental health? Outcomes from the HAT TRICK programme. Health Promotion International. 2021;36(4):943–951. doi: 10.1093/heapro/daaa120. [DOI] [PubMed] [Google Scholar]
- Sierra Hernandez CA, Oliffe JL, Joyce AS, Söchting I, Ogrodniczuk JS. Treatment preferences among men attending outpatient psychiatric services. Journal of Mental Health. 2014;23(2):83–87. doi: 10.3109/09638237.2013.869573. [DOI] [PubMed] [Google Scholar]
- Skärsäter I, Dencker K, Häggström L, Fridlund B. A salutogenetic perspective on how men cope with major depression in daily life, with the help of professional and lay support. International Journal of Nursing Studies. 2003;40(2):153–162. doi: 10.1016/s0020-7489(02)00044-5. [DOI] [PubMed] [Google Scholar]
- Spendelow JS. Cognitive–behavioral treatment of depression in men: Tailoring treatment and directions for future research. American Journal of Men’s Health. 2015;9(2):94–102. doi: 10.1177/1557988314529790. [DOI] [PubMed] [Google Scholar]
- Staczan P, Schmuecker R, Koehler M, Berglar J, Crameri A, von Wyl A, Tschuschke V. Effects of sex and gender in ten types of psychotherapy. Psychotherapy Research. 2017;27(1):74–88. doi: 10.1080/10503307.2015.1072285. [DOI] [PubMed] [Google Scholar]
- Strokoff, J., Halford, T. C., & Owen, J. (2016). Men and psychotherapy. In Y. J. Wong & S. R. Wester (Eds.), APA handbook of men and masculinities (pp. 753–774). Washington, DC: American Psychological Association.
- Syzdek MR, Addis ME, Green JD, Whorley MR, Berger JL. A pilot trial of gender-based motivational interviewing for help-seeking and internalizing symptoms in men. Psychology of Men & Masculinity. 2014;15(1):90. doi: 10.1037/a0030950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogel DL, Wade NG, Haake S. Measuring the self-stigma associated with seeking psychological help. Journal of Counseling Psychology. 2006;53(3):325. doi: 10.1037/0022-0167.53.3.325. [DOI] [Google Scholar]
- Wang J, Lam RW, Ho K, Attridge M, Lashewicz BM, Patten SB, Gundu S. Preferred features of E-mental health programs for prevention of major depression in male workers: Results from a Canadian national survey. Journal of Medical Internet Research. 2016;18(6):e132. doi: 10.2196/jmir.5685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organisation (2017). Depression and other common mental disorders: global health estimates. https://apps.who.int/iris/handle/10665/254610
- Young M, Morgan P, Plotnikoff R, Callister R, Collins C. Effectiveness of male-only weight loss and weight loss maintenance interventions: A systematic review with meta‐analysis. Obesity Reviews. 2012;13(5):393–408. doi: 10.1111/j.1467-789x.2011.00967.x. [DOI] [PubMed] [Google Scholar]
- Young MD, Drew RJ, Kay-Lambkin F, Collins CE, Callister R, Kelly BJ, Morgan PJ. Impact of a self-guided, eHealth program targeting weight loss and depression in men: A randomized trial. Journal of Consulting and Clinical Psychology. 2021;89(8):682. doi: 10.1037/ccp0000671. [DOI] [PubMed] [Google Scholar]
- Zimmermann D, Rubel J, Page AC, Lutz W. Therapist effects on and predictors of non-consensual dropout in psychotherapy. Clinical Psychology & Psychotherapy. 2017;24(2):312–321. doi: 10.1002/cpp.2022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 23.4 KB)
(DOCX 26.4 KB)
Data Availability Statement
The data file for this project is stored in the Centre for Open Science data repository. Link: https://osf.io/4r6zn/?view_only=9ae914f335d34f9baa873fa44eccada6.