Abstract
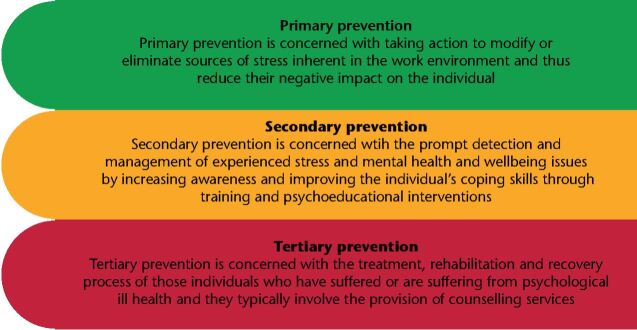
Introduction UK dentists experience high levels of stress, anxiety and burnout. Poor mental health can lead practitioners to exit the profession, contributing to workforce and service loss. Therefore, there is a need to focus on interventions to protect the mental health and wellbeing of dental teams. Three levels of intervention can be deployed in the workplace to support mental health and wellbeing: primary prevention, secondary prevention, and tertiary prevention.
Aim The aim of this systematic review was to identify evidence on interventions used to prevent, improve or tackle mental health issues among dental team members and dental profession students in countries of very high development.
Methods This systematic review was conducted according to a predefined protocol and reported according to PRISMA guidelines. The MEDLINE, Embase CINAHL, DOSS, Scopus, and PsycINFO databases were searched. Prospective empirical studies were considered for inclusion. The Effective Public Health Practice Project Quality Assessment Tool (EPHPP) was used to assess the methodological quality of the included studies. The identified interventions were categorised according to level of prevention.
Results The search yielded 12,919 results. Eight studies met the inclusion criteria. All of the studies concerned dentists or dental students. There were no studies for other groups of dental professionals. No primary prevention-level studies were identified. Secondary prevention-level studies (n = 4) included various psychoeducational interventions aiming to raise awareness and improve coping skills and led to significant improvements in stress levels and burnout of dentists and dental students. Tertiary prevention-level studies (n = 4) mainly employed counselling which was shown to be beneficial for dentists and students experiencing psychological ill-health.
Conclusions Mental wellbeing awareness should be put at the centre of dental education and the workplace. Leadership and innovation are required to design primary-level interventions which can be implemented in the UK dental sector, with its distinct organisational and service characteristics.
Supplementary Information
Zusatzmaterial online: Zu diesem Beitrag sind unter 10.1038/s41432-022-0831-0 für autorisierte Leser zusätzliche Dateien abrufbar.
Key points.
There is a paucity of research and evaluation on interventions to improve mental health and wellbeing within the dental sector, especially at primary prevention level.
There is a need for robust studies to evaluate the effectiveness of psychoeducational and/or organisation/systems-level interventions. Examples of such interventions can be adapted from other healthcare professions to fit in with the distinct nature and characteristics of dental education and dental practice.
Raising awareness and facilitating early recognition of poor mental health as well as effectively responding to these early signs should take place as early as a dental professional's training and continue throughout their professional lives.
Introduction
UK dentists report high levels of stress, anxiety, and burnout, with general dental practitioners (GDPs) and community dentists as well as dentists working in England being more severely affected than dentists in other fields of practice.1,2 Signs of burnout may appear as early as the undergraduate years and the first years of clinical practice.3,4 Despite these indications, data on dental care professionals' mental wellness are currently scarce.5
Dental care teams face numerous stressors in their daily practice; namely: business-led stressors, clinical situations-led stressors, society and person-led stressors, regulation-led stressors and working environment-led stressors.5 Additional stressors due to the COVID-19 pandemic have also been reported among dental professionals, such as fears for the health of friends and family, financial viability, and personal protection.6,7A model developed by Salazar et al. (2019) depicts the complex interplay between different determinants of dentists' mental health and wellbeing including personal factors, career stage, professional and social relationships, job specification, workplace characteristics, dental healthcare systems and regulation.8 A study by the British Dental Association (BDA) suggested that working conditions, working environment, regulatory bodies, and the NHS were the most significant factors impacting dentists' mental health and wellbeing.9 Regulation and fear of litigation have been identified as the most stressful aspects of practising dentistry in the UK.2,10
Poor mental health and wellbeing can affect dentists' decision-making and performance which could impact on patient care and safety.11,12,13,14 Poor mental health and wellbeing can also have a negative impact on workforce sustainability. Dentists facing mental health and wellbeing difficulties may consider exiting the profession/UK practice; for example, through retirement, migration, or changing career.13,14,15 The profession is currently facing a sustainability crisis and thus interventions to safeguard the mental health and wellbeing of dental teams are urgently needed.16,17,18 When it comes to preventing mental health and wellbeing issues in the workplace, three levels of intervention can be employed: primary prevention, secondary prevention and tertiary prevention.19 A definition for each intervention/prevention level is provided in Figure 1. Each level in turn places separate but related responsibilities on both the individual and the system or environment they operate in (that is, practice, service, organisation, healthcare system).19 The available evidence identified in the literature will be discussed in turn as regards to these levels.
Fig. 1.
Levels of intervention for prevention of mental health and wellbeing issues in the workplace19
The aim of the present review is to answer the following research question: 'What interventions have been used and evaluated to prevent, improve, or tackle mental health issues among dental team members and dental profession students in countries of very high development?'
Materials and methods
Protocol
This systematic review was conducted according to a predefined protocol and reported according to PRISMA guidelines. The protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) under the registration number CRD42021261854. This review is an update of a rapid evidence assessment commissioned by the General Dental Council.5
Selection criteria
Studies evaluating the effectiveness of interventions implemented in a dental setting (education, primary or secondary care) in countries of very high development as indicated by the Human Development Index (HDI),20 to improve mental health and wellbeing were considered for inclusion. Studies presenting self-reported coping strategies or interventions whose effect had not been evaluated were not considered for inclusion. Only studies reported in English were included.
Search strategy
A sensitive and comprehensive search strategy was developed by an information specialist. The strategy was comprised of terms for mental health or wellbeing, and dentistry. The following bibliographic databases were searched on 28 June 2021: MEDLINE, Embase, CINAHL, DOSS, Scopus and PsycINFO. The search strategy used for MEDLINE is provided in online Supplementary File 1. Supplemental searching including backward and forward citation searching against the included studies was also performed.
Screening and selection of studies
The citations retrieved from the above search were inserted into the reference management software Endnote X9. The first author screened all the titles and abstracts of the retrieved citations using the Rayyan systematic review web app,21 while the second reviewer independently assessed 20% of the results set. Inter-rater agreement was very high (97%) for this random sample of citations. Full-text screening was completed independently by the two reviewers. Any differences concerning eligibility after full-text screening were resolved through consensus. A record of reasons for excluding studies was kept during the review process and presented in online Supplementary File 2.
Critical appraisal
The quality of the included studies was assessed independently by both authors using the Effective Public Health Practice Project Quality Assessment Tool (EPHPP). Any disagreement in the ratings was resolved with discussion.
Data extraction
The data of included studies were extracted by a single reviewer and verified by the second reviewer, using a piloted data extraction form. Any disagreement was resolved with discussion.
Results
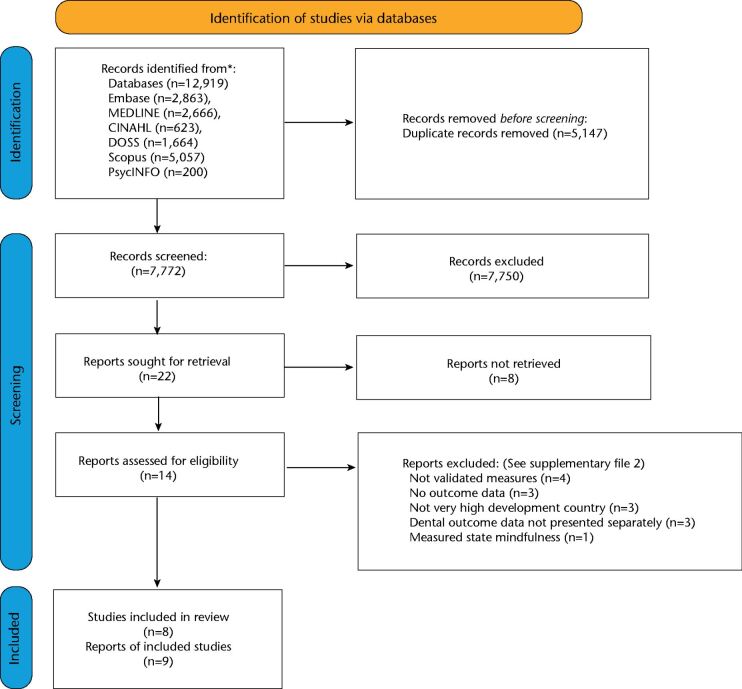
The electronic searches yielded 12,919 citations. After the duplicates were removed, 7,772 titles and abstracts were screened for relevance. Of those, 22 were considered eligible for full-text screening and nine articles met the inclusion criteria. Two articles presented results of the same study in different time points, and hence are treated as the same study.22,23 Therefore, eight studies were included in this systematic review. The selection process for relevant studies and the numbers at each stage are shown in Figure 2. No new studies were found after performing forward and backward citation searching against the included studies.
Fig. 2.
PRISMA 2020 flowchart: study selection process
Study characteristics
The study characteristics are presented in online Supplementary File 3. Overall, the study samples were low, ranging from 5-103 participants. Three studies were conducted in the US,24,25,26 two in England,27,28 one in the Netherlands,22,23 one in Saudi Arabia,29 and one in Chile.30 The majority of studies recruited dental students,24,25,26,29,30 while only three studies recruited dental practitioners.22,23,27,28 There were no studies recruiting other dental professional groups.
Methodological quality
All studies used quasi-experimental designs. Two were judged as of moderate quality24,29 and the rest of weak quality.22,23,25,26,27,28,30 The critical appraisal ratings are presented in Table 1.
Table 1.
Critical appraisal results
| Study | Selection bias | Study design | Confounders | Blinding | Data collection method | Withdrawals and dropouts | Global rating |
|---|---|---|---|---|---|---|---|
| Aboalshamat et al. (2020) | Moderate | Moderate | Strong | Weak | Strong | Strong | Moderate |
| Adams (2017) | Weak | Weak | Weak | Weak | Strong | Weak | Weak |
|
Brake et al. (2001) Gorter et al. (2001) |
Weak | Moderate | Weak | Weak | Strong | Strong | Weak |
| Chapman et al. (2017) | Weak | Moderate | Strong | Weak | Strong | Moderate | Weak |
| Gonzalez & Quezada (2016) | Weak | Weak | Weak | Weak | Strong | Strong | Weak |
| Metz et al. (2020) | Strong | Moderate | Strong | Weak | Strong | Strong | Moderate |
| Newton et al. (2006) | Weak | Moderate | Weak | Weak | Strong | Weak | Weak |
| Piazza-Waggoner et al. (2003) | Strong | Moderate | Weak | Weak | Strong | Weak | Weak |
Outcome measures
A summary of the outcome measures used in the identified studies alongside a short description of the tools used is given in Table 2.
Table 2.
Outcome measures
| Outcome measure/tool | Description of tool | Citations |
|---|---|---|
| Anxiety | ||
| Dentists Anxieties in Clinical Situation Scale (DACSS) | It consists of 20 frequently experienced stressful situations. Dentists are asked to rate their anxiety for each situation on an 11-point Likert scale anchored 0 (not at all) & 10 (the most intense emotion you can experience). For each item they are asked, 'Does the anxiety ever change something about the way you work?' and are asked to indicate yes or no (Y/N). The scale has 2 subscales; the DACSS-R which rated anxiety and the DACSS-C which reported change in decision-making. | Chapman et al. (2017)27 |
| Depression, Anxiety and Stress Scale (DASS-21) | It is used to measure the levels of depression, anxiety, and stress. It contains 21 questions with subscales for each of the three domains. Each question has four answers, ranging from 0 'Did not apply to me at all' to 3 'Applied to me very much, or most of the time.' The score in each subscale ranges from 0 to 21, and the lower the score, the lower the level of psychological distress. | Aboalshamat et al. (2020)29 |
| Spielberger State-Trait Anxiety Inventory (STAI) | There are 2 subscales within this measure. First, the State Anxiety Scale (S-Anxiety) evaluates the current state of anxiety, asking how respondents feel 'right now' using items that measure subjective feelings of apprehension, tension, nervousness, worry, and activation/arousal of the autonomic nervous system. The Trait Anxiety Scale (T-Anxiety) evaluates relatively stable aspects of 'anxiety proneness' including general states of calmness, confidence, and security. The STAI has 40 items, 20 items allocated to each of the S-Anxiety and T-Anxiety subscales. | Piazza-Waggoner et al. (2003)26 |
| Burnout | ||
| Malshach Burnout Inventory (BMI) | It contains 22 statements which relate to each of the three burnout domains, emotional exhaustion (EE), depersonalisation (DP) and personal accomplishment (PA). Respondents are asked to use a seven-point Likert scale to indicate the frequency with which they experience the feeling described by the statement, ranging from 0 (never) to 6 (every day). Summing the appropriate items derives scores for each of the three domains. Indicative of burnout are high scores on EE and DP and low scores on PA. No summative burnout score is made. |
Brake (2001)22 Chapman et al. (2017)27 Gorter (2001)23 |
| Depression | ||
| Depression, Anxiety and Stress Scale (DASS-21) | It is used to measure the levels of depression, anxiety, and stress. It contains 21 questions with subscales for each of the three domains. Each question has four answers, ranging from 0 'Did not apply to me at all' to 3 'Applied to me very much, or most of the time.' The score in each subscale ranges from 0 to 21, and the lower the score, the lower the level of psychological distress. | Aboalshamat et al. (2020)29 |
| Impostor syndrome | ||
| Clance Impostor Phenomenon Scale (CIPS) | It consists of 20 Likert-scale questions, with responses ranging from (1) not at all true to (5) very true. A total score ranges from 20 to 100. The higher the score, the more frequently and seriously the Impostor Phenomenon interferes in a person's life. | Metz et al. (2020)24 |
| Resilience | ||
| Resilience scale RS-14 | It is a seven-point Likert scale. Total scores range from 14 to 98, and the higher the score, the greater the resilience. | Aboalshamat et al. (2020)29 |
| Psychological health and wellbeing | ||
| Clinical Outcomes in Routine Evaluation (CORE) | It is a self-report measure of psychological distress designed to be administered before and after counselling or psychotherapy. The client is asked to respond to questions about how they have been feeling over the last week, using a 5-point scale ranging from 'not at all' to 'most or all of the time'. It covers four dimensions: subjective wellbeing, problems/symptoms, life functioning and risk/harm. | Newton et al. (2006)28 |
| Counselling Centre Assessment of Psychological Symptoms - 34 (CCAPS-34) | It is a 34-item, standardised, multidimensional assessment tool designed to be administered before and after counselling or psychotherapy. It provides a brief measurement tool targeting symptoms and presenting problems that most commonly affect students in university settings. Items on the CCAPS-34 are scored along a 5-point, Likert-type rating scale. | Adams (2017)25 |
| General Health Questionnaire (GHQ-12) | It consists of 12 items, each assessing the severity of a mental problem over the past few weeks using a 4-point scale (from 0 to 3). It is comprised of 6 positive and 6 negative items to assess positive and negative mental health. The score can range from 0 to 36, with higher scores indicating worse conditions. A bimodal scoring can also be used, ranging from 0 to 12, in which case a cut-off point of >3 is a determinant for psychological ill health. | Newton et al. (2006)28 |
| Outcome Questionnaire - 45.2 (OQ 45.2) | It comprises of 45 items associated with a person's quality of life, designed to measure repeatedly changes during and after counselling or psychotherapy. It yields a total score in which higher scores indicate lower levels of general wellbeing. Its cut-off point is 73, therefore scores under 73 belong to the normal population and those above 73 belong to the dysfunctional population. It also provides information on three sub-scales: anxiety-depressive symptomatology (DS), interpersonal relations (IR), and social relations (SR), whose cut-off points are 43, 16 and 14, respectively. Scores above these values imply significant interference in the life of the individual. | Gonzalez & Quezada (2016)30 |
| Outcome Rating Scale (ORS) | It is a four-item measure designed to assess overall counselling or psychotherapy outcomes. The items assess individual, interpersonal, social, and overall wellbeing. | Adams (2017)25 |
| Psychological Well-Being Scale - Short (PWB-S) | It is an 18-item seven-point Likert-type scale with responses ranging from 1 'strongly disagree' to 7 'strongly agree.' It measures six psychological fields of wellbeing: autonomy, environmental mastery, self-acceptance, positive relations with others, purpose in life, and personal growth. Each one of the domains is calculated by sum field's questions. PWB-S is not represented as one total score. Lower scores reflect low levels of psychological wellbeing. | Aboalshamat et al. (2020)29 |
| Stress | ||
| Dental Environment Stress questionnaire (DES) | The DES questionnaire assesses sources of stress associated with undergraduate course work and training in dental students. The DES can be used in two versions, the 38-item full version or the 16-item short version. Each item is scored in a four-point Likert scale, with scores ranging from one (not stressful) to four (very stressful). Higher scores on this scale indicate greater levels of stress. It includes six areas: academic load; pre-clinical and clinical practice; treatment of patients; faculty and administration; interpersonal relations and others. However, these domains may be adapted to each dental school's needs and characteristics. | Gonzalez & Quezada (2016)30 |
| Depression, Anxiety and Stress Scale (DASS-21) | It is used to measure the levels of depression, anxiety, and stress. It contains 21 questions with subscales for each of the three domains. Each question has four answers, ranging from 0 'Did not apply to me at all' to 3 'Applied to me very much, or most of the time.' The score in each subscale ranges from 0 to 21, and the lower the score, the lower the level of psychological distress. | Aboalshamat et al. (2020)29 |
| Work Stress Inventory (WSI) | This scale comprises a number of sources of stress and respondents are asked to indicate which source of stress they have experienced in their work life recently. Higher scores on this scale indicate higher amounts of stress. | Newton et al. (2006)28 |
Primary prevention
No primary prevention studies were identified in the dental literature.
Secondary prevention
Studies on dentists
Only one study, employing a psychoeducational intervention, recruited GDPs. Chapman et al. (2017) examined the effect of a cognitive behavioural therapy (CBT)-based bibliotherapy continuing professional development (CPD) psychoeducational programme on GDPs' mental health, wellbeing and decision-making.27 The study had two arms. Both arms received a self-help CBT package specially designed for dentists, which was written to tackle stress by building resilience. The second arm received an additional three-hour face-to-face workshop.27 Twenty dentists were allocated to each arm of the study based on their willingness to participate in the workshop. The results of the study revealed that depression (DASS-21) and stress (DASS-21) were significantly reduced at six weeks compared to the baseline, with the reductions maintained at six months (DASS-21). Anxiety was significantly reduced at six weeks (DASS-21), but it relapsed back to baseline levels in six months. Significant improvements in the participants' burnout scores were also observed. In particular, emotional exhaustion was significantly reduced at six weeks (MBI) with the reduction maintained at six months (MBI), while personal achievement was significantly improved at six weeks (MBI); however, this was not maintained at six months. The authors also observed an improvement in dentists' decision-making with a significant reduction in hypervigilance at six weeks compared to baseline values (MDMQ), which was maintained at six months (MDMQ). Notably, there was no significant difference in any of the outcome measures across mode of delivery (self-help vs guided self-help). The participating dentists were overwhelmingly positive in their evaluation of the project and reported that they used most of its contents.27
Studies on students
Aboalshamat et al. (2020) introduced a life coaching programme delivered by five senior dental students who had received intensive coaching training by an expert coach.29 Students in the life coaching intervention group (44 female students) attended five one-on-one standardised 15-minute phone coaching sessions at the beginning of each week, while the control group (44 female students) received no coaching or other intervention during that time. All participants in both groups were asked to select a goal they wanted to achieve by the end of the intervention period (five weeks). The results showed that there were significant differences between the groups in depression (DASS-21), stress (DASS-21), and self-acceptance (PWB-S). However, there was no statistically significant difference observed for anxiety (DASS-21), resilience (RS-14) and the other components of the psychological wellbeing scale (PWB-S: autonomy, environmental mastery, positive relations with others, purpose in life, and personal growth).29
Piazza-Waggoner et al. (2002) compared two psychoeducational interventions. In this study, one group received training on relaxation strategies (that is, deep breathing, progressive muscle relaxation) and the control group attended a lecture on the relation among stress, anxiety, and health.26 Although both groups showed a reduction in their anxiety levels, both state and trait anxiety (STAI), the differences between groups did not reach statistical significance.26
Finally, Metz et al. (2020) assessed the impact of a psychoeducational intervention on dental students' feeling of impostorism.24 One hundred and three first-year dental students were recruited and were shown an 'Impostor Video'. The video's content included taped confessions from former dental students regarding their impostor thoughts and an explanation of the basic traits of the condition. The video elaborated on the impostor cycle and identified six specific coping mechanisms for impostor thoughts. The coping mechanisms presented in the video focused on preventing procrastination through study schedules and reducing the time spent on non-essential tasks. After the video, students were provided with small, double-sided reminder cards, containing a graphic of the impostor cycle and a summary of the six coping mechanisms. There was a statistically significant decrease in impostor thoughts following the intervention (CISP). The percentage of students exhibiting intense impostor experiences decreased from 13.6% to 4.9%. The majority of students indicated that the video was successful in raising awareness of the impostor phenomenon, and they recommended repeated exposures to the video throughout their course.24
Tertiary prevention
Studies on dentists
One UK-based study by Newton et al. (2006) evaluated the Dental Practitioner Support Service (DPSS) in Kent, available to dentists facing high levels of stress.28 This service included an initial assessment by a counsellor, followed by a maximum of six one-hour counselling sessions in a personalised, problem-focused programme. The programme sessions covered areas including personal issues such as high expectations of self; low self-esteem; unresolved traumatic experiences; home/work balance; practice issues such as paperwork and patient complaints; interpersonal stress within the practice; and concern regarding the ubiquity of stress among NHS dentists. The counsellors adopted various techniques included counselling and therapeutic approaches, teaching and role play, and the identification of information and resources. Of the 20 GDPs initially recruited, 16 participated in the study, and 9 completed a one-month follow-up. A statistically and clinically meaningful decrease in psychological health and distress (GHQ) was observed. Participants found the service acceptable and rated their progress in dealing and coping with their stress as good.28
In a study by Gorter et al. (2001), 19 Dutch dentists experiencing burnout received intensive counselling and three group sessions over six months. The control group was composed of 103 dentists similarly at risk of burnout, but who did not want to participate in the intervention. The dentists in the control group were subsequently divided into those who spontaneously took some action to alleviate their burnout, and those who did not take any further actions. Participants in the psychological intervention showed decreased burnout scores (MBI) at the end of the intervention.23 Dentists in the self-initiative group showed improvements in emotional exhaustion and personal accomplishment, while those who did nothing showed no improvement in MBI scores.23 However, Brake et al. (2001), presenting one-year follow-up results, demonstrated that participants in the intervention group demonstrated relapse in their burnout scores; however, those who had spontaneously acted to reduce their stress showed sustained improvements.22
Studies on students
In a very small-scale study (five participants) in Chile, dental students were offered eight 45-minute weekly psychotherapy sessions.30 These sessions aimed to educate the participants about symptomatology and help them cope with dental environment-related problems. After attending the eight sessions, all five participants reduced their perceived stress (DES).30 Two of the participants initially had dysfunctional psychological health scores (OQ-45.2) and their scores were deemed normal by the end of the therapy. The rest of the participants retained their scores within the normal range. Additionally, all participants reported that the intervention helped them improve their coping skills.30
Similarly, a US Dental School in Iowa offered counselling by a full-time psychologist in an in-house counselling office embedded within the school.25 Fifty-five students attended 251 counselling appointments, with an average of 4.5 appointments per student. A positive relationship was found between the number of counselling appointments and overall functioning and psychological wellbeing (CCAPS-34).25 Within the same dental school, lunchbreak outreach educational group sessions were offered, which students could voluntarily attend. These sessions were designed to increase student knowledge, awareness, and self-efficacy regarding psychological stress management practices and led to a moderate improvement in awareness, knowledge, and coping skills, but not an increase in willingness to engage in counselling.25 Interestingly, some of the students reported an increased willingness to seek counselling when the office was relocated to a more confidential setting in the building.25
Discussion
Although there is some research activity at the secondary and tertiary level within the dental sector, this review identified a lack of primary or organisation and systems-level strategies. Similarly, no studies have yet recruited dental professionals, other than dentists and dental students. Individualised counselling was found to be useful for dentists and students who have suffered or are suffering from psychological ill-health.28 These services are more likely to be accessed and used if they are confidential and they take into account the nuances of the dental environment.9,25
Psychoeducational interventions sit at the secondary prevention level and aim to facilitate early recognition of symptoms of poor mental health and wellbeing, while tackling the stigma around mental wellness. These interventions address the consequences rather than the sources of stress by improving the adaptability of the individual to the workplace environment, and the organisation or system's structure and culture.19 Evidence from the wider health sector suggests that psychoeducational interventions have a small albeit statistically significant and meaningful effect in reducing healthcare professionals' burnout and stress levels.31,32,33 These results are in line with findings in the dental literature with a bibliotherapy CBT CPD programme designed for GDPs being deemed successful in reducing practitioners' burnout and improving their decision-making.27 Well-powered and methodologically robust studies employing psychoeducational activities such as communication and coping skills training, emotional intelligence training, stress management training, resilience training, mindfulness-based practice, or combination are urgently needed.
Although secondary- and tertiary-level interventions have a useful role to play in the prevention and rehabilitation of mental health and wellbeing issues, their long-term effectiveness as stand-alone interventions may be questionable, unless attempts are also made to address the sources of stress alongside the organisational and systems structures and culture through primary-level prevention. The evidence from the broader healthcare literature advocates organisation-directed interventions as being more effective in improving healthcare workers' mental health and wellbeing.32 Most of these interventions aim to lessen workload pressures by reducing or changing shift patterns, while multifaceted approaches including structural changes, quality improvement and psychoeducational training have also been utilised in a minority of studies.32 Such interventions are currently not widely in use within dentistry.
While some stressors faced by dental professionals can be controlled by the individual, a systems-level approach would allow for modification or elimination of the stressor in the first place. For example, workload pressures imposed by the need to catch up with UDA targets in England is a frequently occurring stressor among GDPs.2,9,12 At a practice or service level, incorporating short breaks or time away from clinics within the work schedule or staff rotas may decrease the stress related to the heavy workload. On the other hand, at policy level, moving away from a target-based dentist remuneration system may be needed in order to positively impact GDPs' mental health and wellbeing through dental contract reform.
Such system-level change would be complex, and necessitate consideration of a wide range of factors beyond professionals' mental wellbeing, but may be even more pressing in the post-pandemic era. COVID-19 restrictions have adversely affected the capacity of NHS primary dental care services, causing a backlog in patient appointments and a widening gap in dental access across different population groups.17
Primary prevention strategies are often a vehicle for cultural change.19 In light of the impact of regulation and litigation on dentists' mental health and wellbeing, shifting the culture in dentistry from a blame culture to a safety culture is timely.34,35 'Safety culture' relates to the extent to which organisations or systems prioritise and support improvements in safety.36 A punitive approach to error, for example, encourages a blame culture and an increase in malpractice litigation, which can have a detrimental effect on practitioners' mental health and wellbeing. In addition, it can also lead to defensive behaviours and in turn, potentially jeopardise patient safety.37
It therefore becomes apparent that the collective attention and collaboration of UK policymakers, regulators and relevant stakeholders is urgently warranted. It is imperative we use the COVID-19 pandemic as an opportunity to put mental wellbeing awareness at the centre of the dental workplace and education, so that dental professionals and dental teams feel empowered to thrive and patient safety is optimised.38 The recently published Mental Health Wellness in Dentistry Framework provides a unique opportunity to make mental health a key priority and to encourage early recognition, intervention and safe signposting among all dental professionals and drive change through a systems-level approach.38
Conclusion
Mental wellbeing awareness should be put at the centre of the dental workplace and education. Early recognition of poor mental health as well as timely and effective response to these early signs should take place as early as a dental professional's training and continue throughout their professional lives. The findings of this review highlight the need to address 'latent' or 'system-related' factors in order to safeguard the mental wellbeing of dental team members and secure a sustainable workforce. Leadership and innovation are required to design and implement primary-level interventions in the UK dental sector, within its distinct organisational and service characteristics.
Supplementary Information
Author contributions
AP: First reviewer: review protocol, study selection, critical appraisal, data extraction, data synthesis, production of draft manuscript. MP: Second reviewer: study selection, critical appraisal, data extraction, data synthesis, and critical review of manuscript. MB: Third reviewer: available to resolve disagreement if consensus could not be reached, methodology advice, critical review of manuscript. LB: Information specialist: search strategy and electronic searches, management of citations, critical review of manuscript. ToB: Input in discussion (implications for education, practice and policy), critical review of manuscript. YH: psychology-related expertise, critical review of manuscript. RW: Input in discussion (implications for education, practice and policy); critical review of manuscript.
Ethics declaration
The authors declare no conflicts of interest. This research is an update of a bigger project commissioned by the General Dental Council (GDC): 'Mental Health and Wellbeing in Dentistry: A Rapid Evidence Assessment'. The views and opinions expressed in this publication are those of the authors and do not necessarily reflect those of the GDC.
References
- 1.Kemp M, Edwards H. Sources of Work-related Stress among Salaried Primary Care Dentists in the UK. 2014. Available at https://bda.org/about-the-bda/campaigns/Documents/Sources%20of%20stress%20among%20salaried%20dentists.pdf (accessed November 2021).
- 2.Collin V, Toon M, O'Selmo E, Reynolds L, Whitehead P. A survey of stress, burnout and well-being in UK dentists. Br Dent J 2019; 226: 40-49. [DOI] [PubMed]
- 3.Alzahem A M, van der Molen H T, Alaujan A H, Schmidt H G, Zamakhshary M H. Stress among dental students: a systematic review. Eur J Dent Educ 2011; 15: 8-18. [DOI] [PubMed]
- 4.Gorter R C, Storm M K, te Brake J H, Kersten H W, Eijkman M A. Outcome of career expectancies and early professional burnout among newly qualified dentists. Int Dent J 2007; 57: 279-285. [DOI] [PubMed]
- 5.Plessas A, Paisi M, Bryce M et al. Mental Health and Wellbeing in Dentistry: A Rapid Evidence Assessment. 2021. Available at https://www.gdc-uk.org/about-us/what-we-do/research/our-research-library/detail/report/mental-health-and-wellbeing-in-dentistry-a-rapid-evidence-assessment (accessed November 2021).
- 6.Mahendran K, Patel S, Sproat C. Psychosocial effects of the COVID-19 pandemic on staff in a dental teaching hospital. Br Dent J 2020; 229: 127-132. [DOI] [PMC free article] [PubMed]
- 7.DPL. Covid-19: Dental Protection survey reveals top 5 worries for dentists. 2020. Available at https://www.dentalprotection.org/uk/articles/covid-19-dental-protection-survey-reveals-top-5-worries-for-dentists (accessed November 2021).
- 8.Salazar F B C, Sipiyaruk K, White S, Gallagher J E. Key determinants of health and wellbeing of dentists within the UK: a rapid review of over two decades of research. Br Dent J 2019; 227: 127-136. [DOI] [PubMed]
- 9.Larbie J, Kemp M, Whitehead P. The Mental Health and Well-being of UK Dentists: A Qualitative Study. 2017. Available at https://bda.org/about-the-bda/campaigns/Documents/The%20Mental%20Health%20and%20Well-being%20of%20UK%20Dentists.pdf (accessed November 2021).
- 10.Toon M, Collin V, Whitehead P, Reynolds L. An analysis of stress and burnout in UK general dental practitioners: subdimensions and causes. Br Dent J 2019; DOI: 10.1038/sj.bdj.2019.46. [DOI] [PubMed]
- 11.Chapman H R, Chipchase S Y, Bretherton R. Understanding emotionally relevant situations in primary dental practice. 2. Reported effects of emotionally charged situations. Br Dent J 2015; 219: E8. [DOI] [PubMed]
- 12.Chipchase S Y, Chapman H R, Bretherton R. A study to explore if dentists' anxiety affects their clinical decision-making. Br Dent J 2017; 222: 277-290. [DOI] [PubMed]
- 13.Hill K B, Burke F J T, Brown J et al. Dental practitioners and ill health retirement: A qualitative investigation into the causes and effects. Br Dent J 2010; 209: E8. [DOI] [PubMed]
- 14.DPL. Breaking the burnout cycle. 2019. Available at https://www.dentalprotection.org/docs/librariesprovider4/dpl-publications/ireland/1907310561-ire-dp-burnout-policy-paper.pdf (accessed November 2021).
- 15.DPL. 94% of dentists believe GDC investigations increase stress and anxiety. 2015. Available at https://www.dentalprotection.org/uk/articles/94-of-dentists-believe-gdc-investigations-increase-stress-and-anxiety (accessed November 2021).
- 16.Eaton K A. Oral healthcare workforce planning in post-Brexit Britain. Br Dent J 2020; 228: 750-752. [DOI] [PMC free article] [PubMed]
- 17.Westgarth D. How much longer does NHS dentistry have left? BDJ In Practice 2020; 33: 12-15.
- 18.Sellars S. Workforce. Br Dent J 2021; 231: 321. [DOI] [PMC free article] [PubMed]
- 19.Cooper C L, Cartwright S. An intervention strategy for workplace stress. J Psychosom Res 1997; 43: 7-16. [DOI] [PubMed]
- 20.Human Development Reports. 2020. Available at http://hdr.undp.org/en/composite/HDI (accessed November 2021).
- 21.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev 2016; 5: 210. [DOI] [PMC free article] [PubMed]
- 22.Brake H T, Gorter R, Hoogstraten J, Eijkman M. Burnout intervention among Dutch dentists: long-term effects. Eur J Oral Sci 2001; 109: 380-387. [DOI] [PubMed]
- 23.Gorter R C, Eijkman M A, Hoogstraten J. A career counseling programme for dentists: effects on burnout. Patient Educ Couns 2001; 43: 23-30. [DOI] [PubMed]
- 24.Metz C J, Ballard E, Metz M J. The stress of success: An online module to help first-year dental students cope with the Impostor Phenomenon. J Dent Educ 2020; 84: 1016-1024. [DOI] [PubMed]
- 25.Adams D F. The Embedded Counseling Model: An Application to Dental Students. J Dent Educ 2017; 81: 29-35. [PubMed]
- 26.Piazza-Waggoner C A, Cohen L L, Kohli K, Taylor B K. Stress management for dental students performing their first paediatric restorative procedure. J Dent Educ 2003; 67: 542-548. [PubMed]
- 27.Chapman H R, Chipchase S Y, Bretherton R. The evaluation of a continuing professional development package for primary care dentists designed to reduce stress, build resilience and improve clinical decision-making. Br Dent J 2017; 223: 261-271. [DOI] [PubMed]
- 28.Newton J T, Allen C D, Coates J, Turner A, Prior J. How to reduce the stress of general dental practice: The need for research into the effectiveness of multifaceted interventions. Br Dent J 2006; 200: 437-440. [DOI] [PubMed]
- 29.Aboalshamat K, Al-Zaidi D, Jawa D et al. The effect of life coaching on psychological distress among dental students: interventional study. BMC Psychol 2020; 8: 106. [DOI] [PMC free article] [PubMed]
- 30.Gonzalez G, Quezada V E. A brief cognitive-behavioural intervention for stress, anxiety and depressive symptoms in dental students. Res Psychother Psychopathol Proc Outcome 2016; 19: 68-78.
- 31.Alkhawaldeh J M A, Soh K L, Mukhtar F B M, Peng O C, Anshasi H A. Stress management interventions for intensive and critical care nurses: A systematic review. Nurs Crit Care 2020; 25: 84-92. [DOI] [PubMed]
- 32.Panagioti M, Panagopoulou E, Bower P et al. Controlled interventions to reduce burnout in physicians a systematic review and meta-analysis. JAMA Intern Med 2017; 177: 195-205. [DOI] [PubMed]
- 33.Venegas C L, Nkangu M N, Duffy M C, Fergusson D A, Spilg E G. Interventions to improve resilience in physicians who have completed training: A systematic review. PLoS One 2019; DOI: 10.1371/journal.pone.0210512. [DOI] [PMC free article] [PubMed]
- 34.General Dental Council. Corporate strategy 2020-2022: Right time, right place, right touch. 2019. Available at https://www.gdc-uk.org/about-us/our-organisation/our-corporate-strategy-and-business-plans (accessed November 2021).
- 35.NHS. The NHS Patient Safety Strategy.Safer culture, safer systems, safer patients. 2019. Available at https://www.england.nhs.uk/wp-content/uploads/2020/08/190708_Patient_Safety_Strategy_for_website_v4.pdf (accessed November 2021).
- 36.Halligan M, Zecevic A. Safety culture in healthcare: a review of concepts, dimensions, measures and progress. BMJ Qual Saf 2011; 20: 338-343. [DOI] [PubMed]
- 37.Catino M. Blame culture and defensive medicine. Cogn Technol Work 2009; 11: 245.
- 38.Dental Professional Alliance. Mental Health Wellness in Dentistry. 2021. Available at https://mhwd.org/download/mental-health-wellness-in-dentistry-framework/ (accessed November 2021).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.