Abstract
Assessment of apical periodontitis (AP) is a challenging task. This case report highlights the CBCT diagnosis and monitoring of periapical radiolucency (PR) using ITK-SNAP software 3.8v in a complex clinical scenario of three traumatized anterior teeth. An 11-year-old male patient complained of recurrent swelling and pain in the maxillary incisor region (teeth #11 and #21). His parents reported a history of traumatic injury affecting these teeth two years back. Digital periapical radiographic (DPR) and cone-beam computed tomography (CBCT) were requested. PR was identified on teeth #11, #21, and # 22. In tooth #22, besides a PR, an area suggesting internal root resorption or oblique root fracture was observed. The teeth were shaped and dressing with calcium hydroxide Ca(OH)2. MTA repair was delivered to the apical portion of the canals (approximately 3 mm). The remainder of the canal was filled with thermoplastic gutta-percha and Endosequence sealer. After one year, the patient returned complaining of pain in tooth #11. Radiographically, the PR of tooth #11 did not reduce. A CBCT was taken, showing a reduction of radiolucency. The patient was clinical and radiographically re-evaluated for 6 months, and he remained asymptomatic. After three years of follow-up, the patient suffered a new trauma on teeth #11 and #21. As tooth #11 presents mobility and biting pain, a new CBCT was requested due to the risk of a possible root fracture. So, the PR was synchronously monitored with linear measurements and volumetric analysis using ITK-SNAP software 3.8v. In this case, the volumetric evaluation was essential to identify the PR's correct dimensions, reducing image interpretation's subjectivity. At 48-month follow-up, the patient was symptoms free and radiographically showed a reduction in the PR's size, compatible with osseous healing.
Key Words: Apical Periodontitis, Cone-beam Computed Tomography, Computer-generated 3D Imaging, Volume Computed Tomography
Introduction
The diagnosis of apical periodontitis (AP) is a challenge in endodontic practice [1, 2]. It can be primarily evaluated based on clinical and radiographic findings [1]. The quantitative measurement of dimensional changes in conventional pre-and postoperative radiography depending upon the stage of the disease. Periapical radiolucency (PR) can only be identified when osteolysis affects 30-50% of the mineral bone density [3, 4]. Thus, cone-beam computed tomography (CBCT) has been recommended for better PR detection accuracy, mainly when it was covered by a thick cortex [3, 4].
The periapical index (PAI) was proposed to categorize AP based on radiographic features correlated with the confirmed histological aspects [5]. With the advent of CBCT use in dentistry, the CBCT-PAI was introduced for PR's linear measurement, reducing false-negative diagnosis incidence [6, 7].
In this context, open-source software for post-processing tomographic images, such as ITK SNAP software, was introduced. They allow automatic, semi-automatic, and manual segmentation of craniofacial structures and osteolytic lesions. The construction of 3D virtual models, color mapping, and "point value" allows the volume assessment and identification of bone remodeling after therapy or pathology development [8, 9].
This case report describes an alternative approach to using CBCT-PAI and volumetric PR measurements by post-processing open-source software. The segmentation made it possible to visualize RP reduction through qualitative and quantitative assessment using virtual 3D models and volumetric analysis. The synchronized use of both methods for long-term monitoring of PR healing has not been previously described. The volumetric evaluation was essential to obtain the periapical radiolucency correct dimensions.
Case Report
This case report was reported according to the PRICE 2020 guidelines [10]. A healthy 11-year-old male patient was referred to the endodontic clinic at the Pontifical Catholic University of Minas Gerais (PUC Minas), complaining of recurrent swelling and pain in the region of maxillary incisors (teeth #11 and #21) in September 2016. His parents reported a history of traumatic injury affecting these teeth two years back when he presented with a laceration in the upper lip and crown fracture in teeth #11 and #21. At the time of the accident, tooth #21 was endodontically accessed and dressing with Ca(OH)2 for two consecutive years by a general dentist. Furthermore, they commented that, after the trauma, the patient showed resistance to attending school, questions about losing his teeth, and difficulty social interaction. The patient was also referred for psychological assessment/therapy.
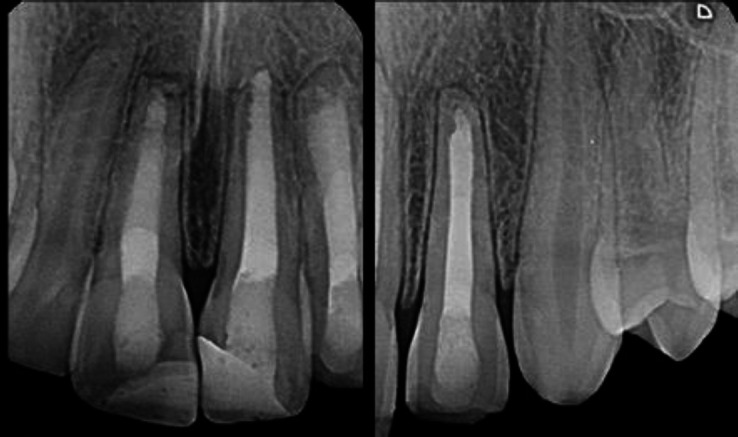
The site's clinical examination revealed swelling located in the buccal mucosa and sensibility to percussion in teeth #11, #21, and #22. The teeth did not respond to Endo-Ice and electric pulp tester. Digital periapical radiography (DPR) was performed at various angles. It was observed that teeth #11 and #21 presented incompletely formed apexes, with PR. In tooth #22, besides an extensive PR, an area suggesting internal root resorption or oblique root fracture was observed (Figure 1A). A CBCT was requested to assist in the diagnosis and treatment plan.
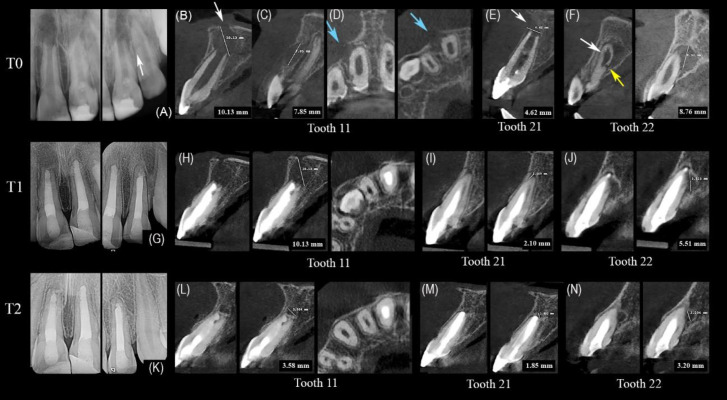
Figure 1.
A) Initial digital periapical radiographs (DPR) of #11, #21, and #22. In #22 was observed in an area suggested as internal root resorption perforating or oblique root fracture (white arrow); B-D) CBCT images of #11 in T0 showing a hypodense image, disruption of the nasal cavity floor, expansion and destruction of the cortex (white and blue arrows) and another periradicular radiolucency in the buccal middle-third of tooth #11; E) Sagittal slice of #21 evidencing hypodense image associated expansion and destruction of buccal cortical bone (white arrow); F) Sagittal views of the #22 with hypodense image compatible with internal root resorption (white arrow), hypodense line in the middle third of the root (yellow arrow) and the lesion measurement; G, K) DPR and CBCT-PAI in the first follow-up (T1) (H-J) and T2 (L-N), respectively. CTBC-PAI: Cone-beam computed tomography-periapical index
A high-resolution CBCT (HR-CBCT) scan, with a reduced field of view (FOV) and voxel, was obtained by ORTHOPHOS SL 3-in-1® (Sirona, Bensheim, Germany). The acquisitions were performed with an 8.0 × 5.5 cm FOV, 60-90 Kv, 3-16 mA, 12 sec exposure time, and 0.159 mm isotropic voxel size. CBCT analysis of the PR included evaluating the extent or scope, margins, and effects on the surrounding teeth or anatomic structures in multiplanar reconstructions using the ITK-Snap v3.8 software (Cognitica, Philadelphia, PA, USA) (http://www.itksnap.org/pmwiki/ pmwiki.php). All radiological protection protocols recommended by the International Commission on Radiological Protection (ICRP) (Radiation Protection No. 172) were adopted [11].
From the initial HR-CBCT images taken in 2016 (T0) (Figure 1), in the sagittal section of tooth #11, PR was observed with disruption of the nasal cavity floor (Figure 1B). Moreover, another periradicular radiolucency in the buccal middle-third of tooth #11 was identified (Figure 1C). In the axial section, a change in the middle-third buccal root contour, which compatible with external root resorption, could be seen (Figure 1D). In tooth #21, radiopacities were noted within the root canal at the middle-third level, consistent with Ca(OH)2 dressing and the presence of a PR with expansion (Figure 1E). In tooth #22, a hypodense image, located on the palatal side of the middle third of the root was identified, suggestive of internal root resorption, promoting communication of the root canal with periodontal tissues or root crack/fracture stimulating advanced PR (Figure 1F).
Based on the clinical, radiographic, and HR-CBCT findings, pulp necrosis diagnosis, an acute apical abscess, was established for tooth #11. Previously treated; asymptomatic apical periodontitis for tooth #21 and pulp necrosis; asymptomatic apical periodontitis for tooth #22. The patient and his parents accepted the proposed treatment plan and signed the consent and permission forms. At the first treatment appointment, local anesthesia was achieved with 2% lidocaine with epinephrine 1:200,000 (Alphacaine; DFL, Rio de Janeiro, RJ, Brazil). A rubber dam was placed in the involved teeth (Hygenic®, Coltene, Altstätten, Switzerland) and fixed with Top Dam® gingival barrier (FGM, Joinville, SC, Brazil). A conservative access cavity was prepared. Working length was achieved using an electronic apex locator Root Z X2 (J Morita, Kyoto, Japan) and confirmed by DPR. The teeth were shaped with manual and rotatory files and copiously irrigated with 5.25% sodium hypochlorite solution. The final irrigation was made with 17% ethylenediamine tetra-acetic acid (EDTA; Lenza Pharma, MG, Brazil). The teeth were sequentially dried with absorbent paper points and dressed with calcium hydroxide paste (Lenza Pharma, MG, Brazil). The teeth were sealed with a double provisional restorative material (Coltosol; Coltene/Whaledent Inc, Cuyahoga Falls, OH, USA) and Flow SureFil resin (Dentsply, Weybridge, England).
After 30 days, the patient returned with no signs or symptoms of the infection. A 4-mm apical plug of MTA Repair (Angelus, Londrina, Brazil) was established in all teeth. Shortly after that, the teeth were filled with gutta-percha and EndoSequence sealer (Brasseler, Savannah, GA, USA) and definitively sealed with Flow SureFil resin (Dentsply, Weybridge, England).
One year later, the patient returned with percussion sensitivity in tooth #11. An occlusal interference was identified in protrusion movement. So, the occlusal adjustment was made. DPR demonstrated a reduction in PR in teeth #21 and #22, but no reduction in tooth 11 (Figure 1G). Then, a new CBCT wasrequested (T1) to clarify the findings. Initially, linear measurement of the PR was performed by CTBC-PAI, and no reduction of the PR was observed (Figure 1B and 1H). Shortly after that, the Volume was evaluated, and a small decrease in the PR was verified. As tooth #11 had no mobility and no pocket, it was decided to monitor clinically and radiographically. In 2019, the patient returned with a new trauma on teeth #11 and #21 resulting from an accident with a broomstick. Tooth #11 presented slight mobility, and the patient complained of discomfort with bitting. Due to the risk of a possible root fracture and the inability to identify it by DPR (Figure 1K), a new HR-CBCT was requested (T2) (Figure 1 L-N). The CBCT images showed no fracture. However, it was possible to verify the reduction of PR in all teeth.
CBCT-PAI follow-up using ITK-SNAP
For linear evaluation of periradicular lesions according to the CBCT-PAI, the "line and ruler mode" tool of ITK-SNAP software was used, based on the largest diameter of PR.
In the first year of follow-up (T1), there was no reduction in the PR associated with tooth #11, which continued to measure 10.13 mm in the largest diameter and showed cortical disruption of the nasal cavity floor. The middle-third buccal radiolucency had wholly healed (Figure 1H). In teeth #21 and #22, bone neoformation was suggested compared to the previous assessment (T0), with reductions of 2.10 and 5.51 mm, respectively (Figures 1I-J). In the third year of follow-up (T2), DPR and HR-CBCT indicated that the PR associated with tooth #11 was reduced (Figure 1L), and significant reduction of the PR was seen in tooth #21 (from 4.62 to 1.85 mm) (Figure 1M); while in tooth #22, the PR was reduced to 3.2 mm (Figure 1N). The results of the monitoring parameters of the CBCT-PAI follow-up are given in Table 1.
Table 1.
CBCT-PAI and volume assessments of PR associated with teeth #11, #21 and #22 in T0, T1 and T2 measured by ITK-SNAP software 3.8v
| CBCT-PAI (mm/score) | Volume (mm 3 ) | ||||||
|---|---|---|---|---|---|---|---|
| CBCT | #11 | #21 | #22 | Red (#11) | Blue (#11) | Pink (#21) | Yellow (#22) |
| TO (2016) | 10.13/5D | 4.62/4ED | 8.76/5 | 246.40 | 65.00 | 34.44 | 461.10 |
| 7.8/4* | |||||||
| T1 (2017) | 10.13/5D | 2.10/3 | 5.51/4 | 239.20 | healed | 4.50 | 40.33 |
| 0.0/0* | |||||||
| T2 (2019) | 3.58/3 | 1.85/2 | 3.2/3 | 10.02 | healed | 1.33 | 7.40 |
| 0.0/0* | |||||||
*Periradicular buccal lesion; *Cone beam computed tomography-periapical index (CTBC-PAI); the variables E (expansion of cortical bone) and D (destruction of cortical bone) were added to each score, if either of these conditions was detected in the CBCT analysis.
Volumetric follow-up using ITK-SNAP software
Additionally, using the "thresholding" and "edge attraction" tools of the ITK-SNAP software, semi-automatic segmentation of PR associated with teeth #11, #21, and #22 were performed in the HR-CBCT images T0 (Figure 2), T1, and T2.
Figure 2.
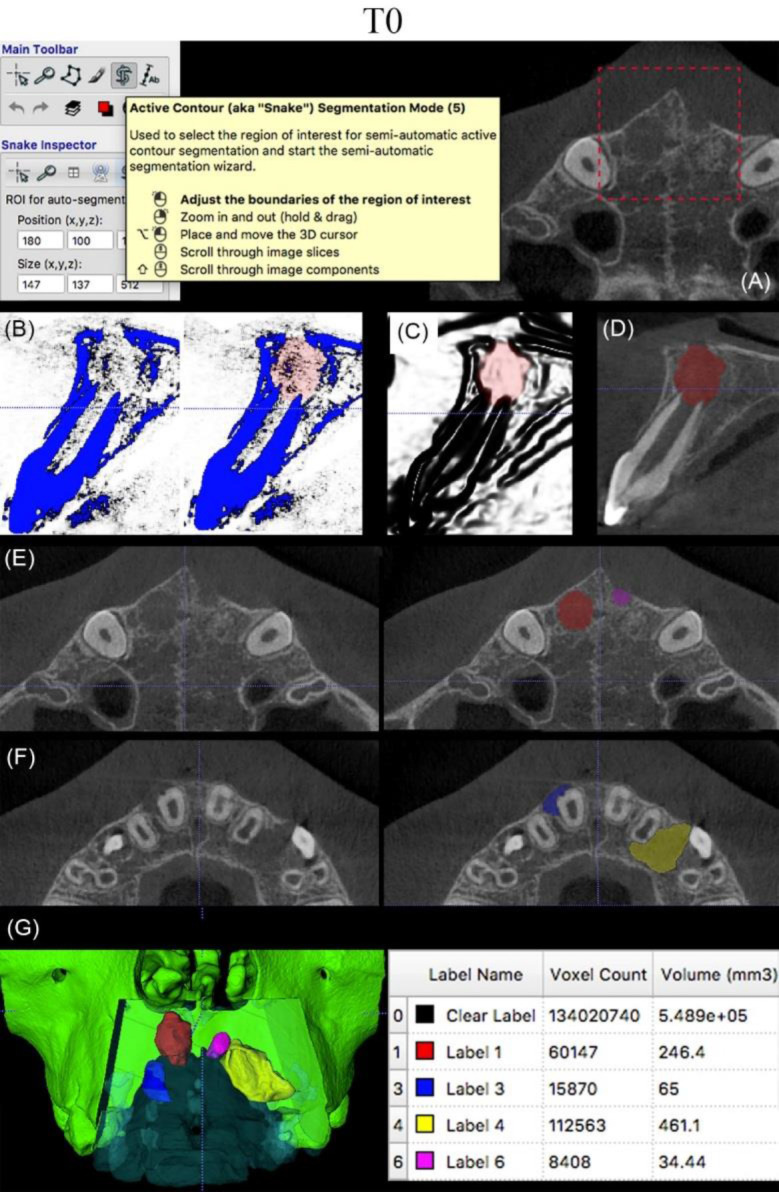
A) The "Active contour segmentation mode" tool of ITK-SNAP software was used to select the region of interest (ROI); B, C) Semi-automatic segmentation of the bone rarefaction using "thresholding" and "edge attraction" tools; D) Segmentation of periapical bone rarefaction associated with #11; E, F) CBCT axial slices (T0) showing the segmentation of bone rarefactions related to teeth #11, #21, and #22; G) 3D virtual models of the lesions with volumetric analysis. (The color codes: Labels: 1-RED-PR tooth #11; 3-BLUE-Buccal radiolucency tooth #11; 4-YELLOW-PR tooth #22; 6-PINK-PR tooth # 21)
After the semi-automatic segmentation, a manual refinement was performed, using the “paintbrush” tool, for the construction of 3D virtual models and volumetric monitoring of the PR in T0 (Figure 2), T3=T2 tooth #11 (Figure 3), tooth #21 (Figure 4), and tooth #22 (Figure 5). For the segmentation of the lesion, a blue layer was used in the PR associated with tooth #11, buccally; red layer in the periradicular radiolucency associated with tooth #11; pink layer in the PR associated with tooth #21; and yellow layer in the PR associated with tooth #22, distally. For the segmentation of the maxilla and anterior teeth region, green and light blue layers were used, respectively. Then, the blue layer's opacity was reduced to allow visualization of the 3D virtual models corresponding to the PR through semi-transparency of the maxilla's anterior region (Figures 2). The volumetric assessment demonstrated volume reduction in the PR associated with teeth #11, #21, and #22 (Figures 2-5, and Table 1).
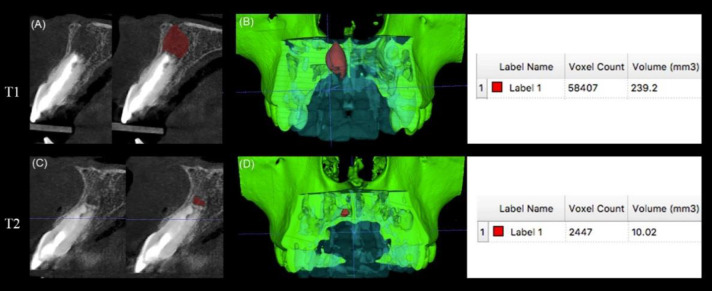
Figure 3.
A, B) Segmentation and volumetric follow-up of the periapical radiolucency associated with #11 in T1; C, D) T2, demonstrating a reduction in volume from 239.2 mm3 (T1) to 10.02 mm3 (T2) after endodontic treatment
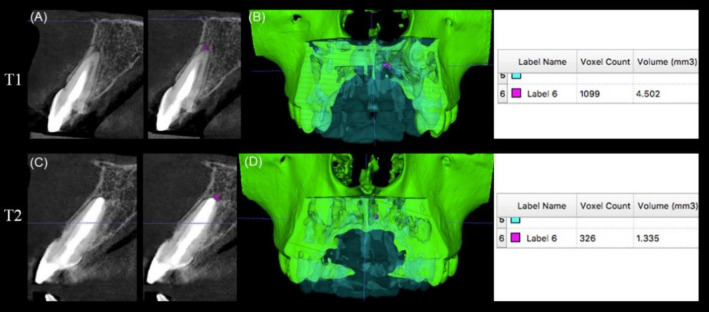
Figure 4.
A, B) Segmentation and volumetric follow-up of the periapical radiolucency associated with #21 in T1; C, D) T2, demonstrating a reduction in volume from 4.50 mm3 (T1) to 1.33 mm3 (T2) after endodontic treatment
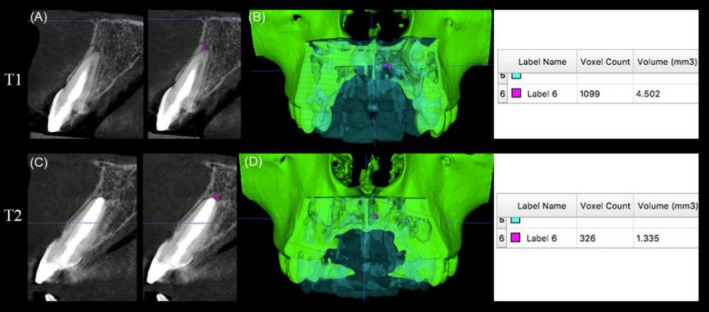
Figure 5.
A, B) Segmentation and volumetric follow-up of the periapical radiolucency associated with #22 in T1 C, D) T2, demonstrating a reduction in Volume from 40.33 mm3 (T1) to 7.40 mm3 (T2) after endodontic treatment.
Clinical and radiography follow-up
At the 4-year time point follow-up, the patient was clinically symptom-free. It was possible to observe a regular contour radiographically in the lamina dura, without surrounding discontinuity. The adjacent periodontal ligament space was uniform, compatible with bone healing in teeth #11, #21, and #22 (Figure 6).
Figure 6.
Digital periapical radiography at 4-year follow-up. The space of the periodontal ligament was uniform, compatible with bone regeneration in anterior teeth
Discussion
According to the literature, endodontic treatment's primary goal is to reduce intracanal bacteria to compatible with periapical healing [12]. However, the follow-up of teeth with PR is still a challenge in endodontic practice [1, 4]. Usually, follow-ups are recommended from 6 months to 5 years after treatment until completely healthy periapical structures can be verified in DPR and CBCT [1, 6]. However, some authors have classified cases as success or failure after shorter periods, but when there is doubt, the patient should be reexamined three years later [1, 3]. In the current report, a significant reduction in PR in teeth #11, #21, and #22 were observed after the second year of CTBC follow-up (T2).
Traditionally, periapical radiography is considered the initial imaging modality in endodontics with its inherent high spatial resolution. However, this should be done with care for PR's detection because of the possibility of a false-negative diagnosis [6]. Digital subtraction radiography (DSR) and CBCT images have also been used [4]. However, DSR demands strict rules concerning radiation, geometry, and contrast, making the general clinician's method arduous [13]. In this sense, CBCT imaging has become an essential tool for diagnosing and managing endodontic complications requiring three-dimensional imaging. But it must be used cautiously. The potential benefits, as well as risks, must be evaluated [14, 15].
In the present case, to avoid any subjectivity in interpreting the image, volumetric evaluation through semi-automatic and manual segmentation was used simultaneously with CBCT-PAI. The segmentation consists of a dynamic method, with accuracy proven in previous studies [9, 13, 16], which facilitates visualization of the PR reduction. There are differences between the segmentation methods, which can be associated with one another to enable greater precision. In the present study, semi-automatic and manual segmentation methods were used together to combine the most accurate method (manual) and high efficiency and repeatable method (semi-automatic method) [17-19].
The volumetric measurements, over time by CBCT, were fundamental to clinical decision-making. Some authors agree that in 100% of cases, CBCT influenced the definitive treatment plans and diagnosis in clinical scenarios commonly encountered in pediatric dentistry, such as dental trauma, and 44% of treatment plans in these patients were changed after CBCT [20]. Dutra et al. [21], in a systematic review and meta-analysis, found that CBCT provided greater diagnostic accuracy for AP. In this case, after one year, the child returned with complaints of percussion pain on tooth #11. Radiographically, the PR of tooth #11 was unchanged. Then, a new CBCT was requested to clarify the findings (T1). If the radiographic findings had been considered exclusively, re-intervention would have been unnecessarily proposed. Segmentation made it possible to visualize the reduction of PR's size through qualitative and quantitative assessment using virtual 3D models and volumetric analysis, respectively (Figures 2-5).
As previously described [11], HR-CBCT made it possible to measure the PR employing the brightness and contrast tools of the ITK-SNAP software, thus enabling visualization of changes not demonstrated by DPR. In the tomographic images (T0), it was possible to see the disruption of the nasal cavity floor by the PR, expansion, disruption of the buccal bone cortex, and external root resorption associated with tooth #11. Slight growth and disruption of the buccal bone cortex in the PR associated with tooth #21 were also visualized (T1 and T2) and internal root resorption in tooth #22. It should be highlighted that although tooth #21 suggested radiographic healing, in T1 and T2 by CBCT-PAI and volumetric monitoring, the PR did not disappear completely. These findings agree with previous studies that observed that incipient lesions, which are away from the cortex or do not rupture the cortex, might be superimposed by the bone table and do not appear on the radiograph [3, 4].
The radiolucency in the buccal middle-third of tooth #11 and distal to tooth #22 was also measured. From the measurements made, the radiolucency had disappeared completely on tooth #11 (T1). However, the lateral radiolucency associated with the middle-third of tooth #22 remained until T2. Commonly, the CTBC-PAI is applied to lesions limited to the root's apical region (6). Still, its scope for lateral radiolucency can be suggested once it was useful for the management and monitoring of this periradicular radiolucency.
A new CBCT (T2) was requested explicitly because the adolescent suffered a further trauma on teeth #11 and #21, with a suspected fracture. In this context, the benefits of three-dimensional images outweighed the risk of radiation dose and higher costs. The CBCTs were collimated only for the maxilla, as recommended by SEDENTEXCT guidelines [22], and the patient used thyroid shielding as described in a previous report [23].
Conclusions
In conclusion, this case report contributed to the knowledge about clinical approaches using ITK-SNAP software 3.8v as a valuable tool to monitor PR's 2D and 3D parameters in a complex clinical scenario of three traumatized anterior teeth. It can help endodontists and radiologists perform a long-term PR evaluation, reducing image interpretation's subjectivity.
Acknowledgment
This study was supported by grants from Conselho Nacional de Desenvolvimento Científico e Tecnológico-CNPq Fundacão de Amparo à Pesquisa do Estado de Minas Gerais-FAPEMIG.
Conflict of Interest:
‘None declared’.
References
- 1.Patel S, Wilson R, Dawood A, Foschi F, Mannocci F. The detection of periapical pathosis using digital periapical radiography and cone beam computed tomography - part 2: a 1-year post-treatment follow-up. Int Endod J. 2012;45(8):711–23. doi: 10.1111/j.1365-2591.2012.02076.x. [DOI] [PubMed] [Google Scholar]
- 2.Andreasen FM, Kahler B. Diagnosis of acute dental trauma: the importance of standardized documentation: a review. Dent Traumatol. 2015;31(5):340–9. doi: 10.1111/edt.12187. [DOI] [PubMed] [Google Scholar]
- 3.Cohenca N, Simon JH, Roges R, Morag Y, Malfaz JM. Clinical indications for digital imaging in dento-alveolar trauma Part 1: traumatic injuries. Dent Traumatol. 2007;23(2):95–104. doi: 10.1111/j.1600-9657.2006.00509.x. [DOI] [PubMed] [Google Scholar]
- 4.de Carvalho FB, Gonçalves PS, Lima RK, Guerreiro-Tanomaru JM, Rasquin LC, Tanomaru-Filho M. Use of cone-beam tomography and digital subtraction radiography for diagnosis and evaluation of traumatized teeth treated with endodontic surgery and MTA A case report. Dent Traumatol. 2013;29(5):404–9. doi: 10.1111/j.1600-9657.2011.01092.x. [DOI] [PubMed] [Google Scholar]
- 5.Maia Filho EM, Calisto AM, De Jesus Tavarez RR, de Castro Rizzi C, Bezerra Segato RA, Bezerra da Silva LA. Correlation between the Periapical Index and Lesion Volume in Cone-beam Computed Tomography Images. Iran Endod J. 2018;13(2):155–8. doi: 10.22037/iej.v13i2.15040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Estrela C, Bueno MR, Azevedo BC, Azevedo JR, Pécora JD. A new periapical index based on cone beam computed tomography. J Endod. 2008;34(11):1325–31. doi: 10.1016/j.joen.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 7.Safi Y, Fazlyab M, Asgary S, Fazlalipour S. A Novel Technique for Minimizing the Metal Artifacts on Anterior Teeth in Cone-Beam Computed Tomography. Iran Endod J. 2019;14(1):79–83. doi: 10.22037/iej.v14i1.21636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Esposito S, Cardaropoli M, Cotti E. A suggested technique for the application of the cone beam computed tomography periapical index. Dentomaxillofac Radiol. 2011;40(8):506–12. doi: 10.1259/dmfr/78881369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schloss T, Sonntag D, Kohli MR, Setzer FC. A Comparison of 2- and 3-dimensional Healing Assessment after Endodontic Surgery Using Cone-beam Computed Tomographic Volumes or Periapical Radiographs. J Endod. 2017;43(7):1072–9. doi: 10.1016/j.joen.2017.02.007. [DOI] [PubMed] [Google Scholar]
- 10.Nagendrababu V, Chong BS, McCabe P, Shah PK, Priya E, Jayaraman J, Pulikkotil SJ, Setzer FC, Sunde PT, Dummer PMH. PRICE 2020 guidelines for reporting case reports in Endodontics: a consensus-based development. Int Endod J. 2020;53(5):619–26. doi: 10.1111/iej.13285. [DOI] [PubMed] [Google Scholar]
- 11.The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP. 2007;37(2-4):1–332. doi: 10.1016/j.icrp.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 12.Siqueira JF Jr, Pérez AR, Marceliano-Alves MF, Provenzano JC, Silva SG, Pires FR, Vieira GCS, Rôças IN, Alves FRF. What happens to unprepared root canal walls: a correlative analysis using micro-computed tomography and histology/scanning electron microscopy. Int Endod J. 2018;51(5):501–8. doi: 10.1111/iej.12753. [DOI] [PubMed] [Google Scholar]
- 13.Villoria EM, Lenzi AR, Soares RV, Souki BQ, Sigurdsson A, Marques AP, Fidel SR. Post-processing open-source software for the CBCT monitoring of periapical lesions healing following endodontic treatment: technical report of two cases. Dentomaxillofac Radiol. 2017;46(1):20160293. doi: 10.1259/dmfr.20160293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Myers GL. Evaluation and diagnosis of the traumatized dentition. Dent Traumatol. 2019;35(6):302–8. doi: 10.1111/edt.12498. [DOI] [PubMed] [Google Scholar]
- 15.Patel S, Brown J, Semper M, Abella F, Mannocci F. European Society of Endodontology position statement: Use of cone beam computed tomography in Endodontics: European Society of Endodontology (ESE) developed by. Int Endod J. 2019;52(12):1675–8. doi: 10.1111/iej.13187. [DOI] [PubMed] [Google Scholar]
- 16.Gomes AF, Brasil DM, Silva AIV, Freitas DQ, Haiter-Neto F, Groppo FC. Accuracy of ITK-SNAP software for 3D analysis of a non-regular topography structure. Oral Radiol. 2020;36(2):183–9. doi: 10.1007/s11282-019-00397-y. [DOI] [PubMed] [Google Scholar]
- 17.Vallaeys K, Kacem A, Legoux H, Le Tenier M, Hamitouche C, Arbab-Chirani R. 3D dento-maxillary osteolytic lesion and active contour segmentation pilot study in CBCT: semi-automatic vs manual methods. Dentomaxillofac Radiol. 2015;44(8):20150079. doi: 10.1259/dmfr.20150079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Orhan K, Bayrakdar IS, Ezhov M, Kravtsov A, Özyürek T. Evaluation of artificial intelligence for detecting periapical pathosis on cone-beam computed tomography scans. Int Endod J. 2020;53(5):680–9. doi: 10.1111/iej.13265. [DOI] [PubMed] [Google Scholar]
- 19.Camargo RV, Mazzi-Chaves JF, Leoni GB, Vasconcelos KF, Lamira A, Jacobs R, Sousa-Neto MD. Quantitative Assessment of 2-dimensional Parameters in Tomographic Images by Using Different Segmentation Methods. J Endod. 2020;46(5):694–9. doi: 10.1016/j.joen.2020.01.012. [DOI] [PubMed] [Google Scholar]
- 20.Mizban L, El-Belihy M, Vaidyanathan M, Brown J. An audit and service evaluation of the use of cone beam computed tomography (CBCT) in a paediatric dentistry department. Dentomaxillofac Radiol. 2019;48(5):20180393. doi: 10.1259/dmfr.20180393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leonardi Dutra K, Haas L, Porporatti AL, Flores-Mir C, Nascimento Santos J, Mezzomo LA, Corrêa M, De Luca Canto G. Diagnostic Accuracy of Cone-beam Computed Tomography and Conventional Radiography on Apical Periodontitis: A Systematic Review and Meta-analysis. J Endod. 2016;42(3):356–64. doi: 10.1016/j.joen.2015.12.015. [DOI] [PubMed] [Google Scholar]
- 22.Radiation Protection No 172 - CBCT for dental and maxillofacial surgery: Evidence-based guidelines (The SEDENTEXCT Project). Brussels: European Commission. 2012. Available from: http://www.sedentexct.eu/files/radiation_protection_172.pdf.
- 23.Pauwels R, Horner K, Vassileva J, Rehani MM. Thyroid shielding in cone beam computed tomography: recommendations towards appropriate use. Dentomaxillofac Radiol. 2019;48(7):20190014. doi: 10.1259/dmfr.20190014. [DOI] [PMC free article] [PubMed] [Google Scholar]