Abstract
Introduction:
Articaine is reported to have a fast onset and a short-acting pulpal anesthesia in inferior alveolar nerve blocks. Clonidine is an α2-adrenoceptor agonist and is used as an adjunct to enhance the anesthetic efficacy and induce greater analgesia. In an attempt to search for more effective ways to achieve profound analgesia after root canal treatment, this randomized clinical trial assessed the efficacy of clonidine added to articaine/epinephrine solution on post-operative pain relief after root canal treatment in mandibular molars with irreversible pulpitis.
Materials and Methods:
Our randomized clinical trial study enrolled one hundred patients with symptomatic irreversible pulpitis in mandibular molars. They were divided into two groups, each group received either 0.2 mL 150 µg/mL clonidine or distilled water added to 1.8 mL of 4% articaine with 1:100,000 epinephrine cartridge. The alveolar nerve block in the two groups was administered by the same clinician and the subject’s pain scores were recorded at 6, 12, 24, 48 and 72 h post-operatively using a Heft-Parker visual analog scale. Data were analyzed using t, chi-square and repeated-measures ANOVA statistical tests.
Results:
The mean pain scores for clonidine group were significantly lower than control at all the time intervals after treatment (P<0.05). We did not notice any clinical and there were no complaints from the patients either.
Conclusion:
Based on this randomized clinical trial study the addition of clonidine to the articaine/epinephrine solution using an inferior alveolar nerve block during root canal treatment in mandibular molars with irreversible pulpitis may be effective in reducing post-operative pain.
Key Words: Articaine, Clonidine, Inferior Alveolar Nerve Block, Post-operative Pain, Root Canal Therapy
Introduction
An essential part of root canal therapy is to prevent and manage post-operative pain [1], which may persist after treatment [2, 3]. However, acquiring adequate pain control has been challenging as the frequency of post-operative pain after endodontic treatment is reported to be 3-58% [4]. Ways to achieve profound analgesia after root canal treatment are therefore imperative for the patient [5]. Currently, local anesthetic drugs, such as lidocaine, articaine, prilocaine, mepivacaine and bupivacaine, are commonly used to reduce pain during dental procedures[6]. In 2000, 4% articaine with epinephrine was approved for dental use by the Food and Drug Administration in the United States [7]. Articaine is an amide anesthetic containing a lipophilic part, connected to a hydrophilic part. Although the thiophene ring in the lipophilic part differentiates articaine from other amide anesthetics; many studies have suggested that this structure causes higher neurotoxicity [8]. Pharmokinetics of articaine leads to a fast onset and a short-acting pulpal anesthesia in inferior alveolar nerve block (IANB), compared to lidocaine [9]. In recent years, more adjunctive drugs have been used to increase analgesia during and after dental procedures, and the combinatorial use of medications has been advocated [10].
Clonidine is an α2-adrenoceptor agonist. It is used as an adjunct to enhance the anesthetic efficacy and induce greater analgesia in various injections such as dentoalveolar [11], spinal [12], epidural [13], brachial plexus, and peripheral nerve block anesthesia [14]. A previous study suggested that addition of a low dose of clonidine to bupivacaine in the supraclavicular brachial plexus block significantly prolonged the analgesic duration without producing any significant clinical complications [15]. Three other studies also reported that the adjunctive use of clonidine to lidocaine reduced pain after inferior alveolar nerve block (IANB) [16, 17], and substantially increased the success rate of anesthesia [11]. There are reports that recommend the addition of clonidine to articaine/epinephrine local infiltration anesthesia in pediatric dental setting due to the great increase in depth and duration of anesthesia [18].
Although both articaine and clonidine have been extensively studied in the past, a review of the literature revealed that there has been no study to date on the effect of clonidine in combination with articaine/epinephrine on post-operative pain in endodontics. Therefore, wished to determine the effect of adding clonidine to articaine/epinephrine on post-operative pain relief in patients with irreversible pulpitis.
Materials and Methods
Patient recruitment
Our double-blind clinical trial was conducted in Isfahan Dental School with a total of 105 patients who provided informed consent. All included patients were aged 15-60 years and healthy (Grade I, according to the classification of American Society of Anesthesiologists). Patients with underlying diseases such as diabetes, hypertension or other cardiovascular diseases or contraindication to clonidine, articaine, or epinephrine were not included in the study. In order to be included in the study, they were required to have a symptomatic irreversible pulpitis. The clinical diagnosis was based on subjective and objective findings indicating that the vital inflamed pulp is incapable of healing and the tooth exhibiting intermittent or spontaneous pain in a mandibular posterior tooth [19].
Following isolation with cotton rolls, and drying the tooth with air syringe, an endodontist, who was not involved in the study, performed a cold test to confirm the diagnosis. He used Endo Ice (1,1,1,2 tetrafluoroethane; Hygenic Corp, Akron, OH, USA) on a cotton pellet and covered it for maximum of 15 sec on the middle third of the buccal surface of the tooth until the patient responded. Any exaggerated reaction to cold stimulant & lingering of discomfort for more than 10 sec or more after removal of stimulant was recorded. Those with no response, periodontal problems or active signs of oral infection or inflammation were excluded. Their periosteal bone and periradicular tissues were evaluated radiographically. None of the selected patients showed any pathology on their radiographs, other than widened periodontal ligament space. Patients with clinical and radiographic signs of pulpal necrosis or non-vital coronal pulp tissue upon access cavity preparation (partial necrosis) were excluded.
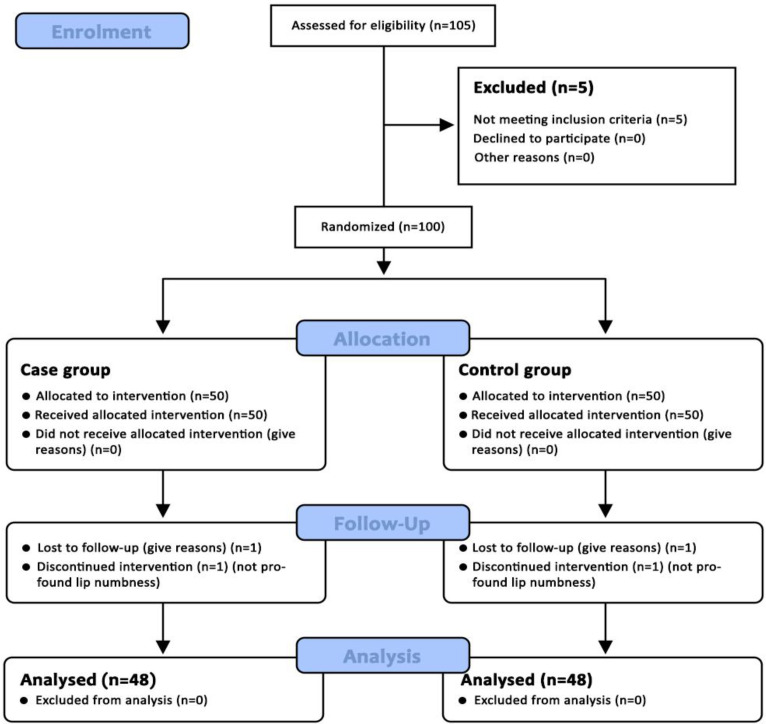
Patients who required multiple dental treatments or had consumed opioids during the week before or 72 h after the procedure were excluded from the study. Pregnant or lactating mothers, drug abusers, and β-blocker users were also excluded from the study. Patients who did not cooperate in pain assessment or needed additional anesthetic injections due to block failure were also excluded. Those with a changed treatment plan were excluded as well. After approval by the Institutional Ethics Committee of Isfahan Dental School (ID: IR.MUI.REC.1396.3.272), the study was registered in the Iranian Registry of Clinical Trials (ID: IRCT20201031049199N1). After an oral explanation of the procedure and possible complications was given, written informed consent was obtained from all patients. To ensure transparence and quality, the CONSORT (Consolidated Standards of Reporting Trials) checklist was followed (Figure 1).
Figure 1.
Flowchart of participants’ disposition through the trial based on CONSORT
Preparation of anesthetic solutions
In order to make the study double-blind, the anesthetic solutions were prepared and encoded by a dental student who was not involved in the study. Using a 30-gauge insulin syringe (Keltenstrabe, Tuttlingen, Germany), either clonidine or distilled water was inserted into a cartridge of 4% articaine with 1:100,000 epinephrine, which increased the total volume of each vial content to 2 mL. The cartridges with and without clonidine were labelled No. 1 and No. 2, respectively. The solutions were prepared daily under aseptic conditions.
Randomization
An endodontist, who was blind to the contents of the cartridges, threw a dice just before treatment. No. 1 cartridge was used when an odd number came out and a No. 2 cartridge was used with an even number. Therefore, both the patient and the investigator were unaware of the type of local anaesthesia used. This randomization protocol can lead to a selection bias, but it was unavoidable due to limited time and financial sources.
Anesthesia
After diagnosis of irreversible pulpitis for the target tooth, a questionnaire including demographic information, medical history and pain intensity using a 170 mm Heft-Parker visual analog scale (VAS) was given to each patient [20]. The clonidine group, cartridge No 1 (n=50), received an IANB with 0.2 mL clonidine (Catapressan amp, 150 µg/mL; Boehringer Ingelheim, Ingelheim am Rhein, Germany) in addition to 1.8 mL of 4% articaine with 1:100,000 epinephrine (Daropakhsh, Tehran, Iran). The control group (No 2, n=50) received an IANB with 0.2 mL distilled water in addition to 1.8 mL 4% articaine with 1:100,000 epinephrine (Daropakhsh, Tehran, Iran).
Topical anesthetic gel of 20% benzocaine (Denticare, Medicom, Canada) was applied at the IANB site for one min using a cotton swab. A standard IANB was performed with a 27-gauge 1.5-inch needle by one endodontist. After touching the medial border of the mandibular ramus (which located lateral to the pterygomandibular fold and the sphenomandibular ligament [21] from the top of the opposite side premolars, the needle was withdrawn by 1 mm. After aspiration, the anesthetic solution was deposited for 2 min. If profound lip numbness was not obtained within 15 min, the block was considered failed and the patient was excluded from the study. For each patient, blood pressure and heart rate were measured before and 5 min [11] after the anesthetic administration using a digital blood pressure monitor (Omron M3; Omron Healthcare Co., Kyoto, Japan). The treatment was done in a single-visit using RaCe rotary system (FKG Dentaire, La-Chaux-de Fonds, Switzerland) according to the manufacturer instructions [22, 23]. Finally, the access cavity was sealed with eugenol temporary dressing (Zonalin; Associated Dental Products, Wiltshire, United Kingdom). The occlusion was checked to remove any occlusal interference.
Evaluation of post-operative pain
We evaluated the post-operative pain with HP VAS which was given to each patient. VAS is divided into 4 categories (no pain: 0 mm; mild pain: > 0 mm and ≤ 54 mm; moderate pain: > 54 mm and < 114 mm; severe pain: ≥114 mm). Patients were followed up via phone calls or text massages at 6, 12, 24, 48 and 72 h after the root canal treatment. All participants were asked about nausea, vomiting, drowsiness, dizziness and headaches. They were also asked about post-operative analgesic consumption and instructed to use up to 400 mg of ibuprofen (Gelofen; Jaber Ebne Hayyan Pharmaceutical Mfg. Co., Tehran, Iran) in case of an emergency pain [24]. The few that did have to consume analgesia post-operatively (only one person in clonidine group), were excluded in data analysis in order to prevent calculation error.
Statistical analysis
Based on the previous studies (10), it was estimated that 50 subjects were required per group. Data were analyzed with SPSS software (SPSS version 20.0, SPSS, Chicago, IL, US).
Mean post-operative pain scores and Hemodynamic parameters of the two groups were compared using an independent-samples and paired sample t-test. Data on gender and age and initial pain were analyzed using the chi-squared and independent t-tests. To investigate the main and interaction effects, data subjected to the two-way repeated-measures ANOVA and a significance level of 0.05 was defined throughout the analysis.
Results
A total of 105 patients were recruited in our study. Five volunteers/subjects did not meet the inclusion criteria (two patients took β-blockers; one had analgesics the day before; one was pregnant; and one had diabetes). Four patients were excluded from the study after enrollment: two patients (one from each group) were excluded because of IANB failure, defined as no profound lip numbness within 15 min post-injection. One patient in the clonidine group was excluded due to analgesic consumption after treatment, and another was omitted in the control group due to lack of cooperation with pain assessment. Therefore, nine out of 105 patients were excluded and the remaining 96 patients were included for analysis (48 subjects in each group) (Figure 1). Age, gender and initial pain level of the two groups are presented in Table 1. There was no statistically significant difference between the two groups regarding age (P= 0.2), gender (P=0.5) and initial pain (P=0.6).
Table 1.
Demographic data (n=48)
| Parameters | Clo+Articaine+Epi | Articaine+Epi | P -value |
|---|---|---|---|
| Age (mean±SD) | 32.68±12.30 | 30.13±12.66 | 0.2 |
| Gender | 24 males 24 females |
23 males 25 females |
0.5 |
| Initial pain | 106±15 | 104±18 | 0.6 |
Comparisons were non-significant (P>0.05); Epi: Epinephrine; Clo: Clonidine; SD: Standard Deviation
The mean pain scores for the clonidine group were significantly lower than the control group at all time-intervals post-treatment (P<0.05). The mean pain scores of each group, measured at 6, 12, 24, 48 and 72 h after treatment, are shown in Table 2.
Table 2.
Mean pain scores at different time intervals for 72 hours (h) post-operatively (Mean±SD)
| Intervals | Solutions | Mean HP VAS | P -values |
|---|---|---|---|
| 6 h | A+E | 69.52±39.21 | <0.001* |
| A+E+C | 34.30±33.91 | ||
| 12 h | A+E | 44.22±38.43 | 0.011* |
| A+E+C | 25.10±35.61 | ||
| 24 h | A+E | 34.04±39.74 | 0.028* |
| A+E+C | 18.66±28.22 | ||
| 48 h | A+E | 27.34±37.50 | <0.001* |
| A+E+C | 6.06±14.48 | ||
| 72 h | A+E | 16.88±33.22 | 0.003* |
| A+E+C | 2.18±7.79 |
Expressed as mean±standard deviation; VAS: visual analog scale; A: articaine; E: epinephrine; C: clonidine; *Independent t test
Two-way repeated measured ANOVA for post-operative pain showed a significant group effect (P = 0.000) and time effect at 24, 48, 72 h after treatment (P ≤ 0.001) but there was no significant difference related to the time intervals (with "Between-subject effect test" P = 0.1, F=2.753). Comparison of time interval groups showed that pain scores were significantly different over the time (with "Between- subject effect test" P=0.000, F=15).
There was no significant difference in systolic and diastolic blood pressure and heart rate between the two groups, both before and 5 min after the treatment (Table 3). In the control group, the mean heart rate increased significantly after the block. On the other hand, there was no significant increase in the mean heart rate after injection in clonidine group. None of the patients reported headaches, nausea, vomiting, drowsiness or dizziness after treatment.
Table 3.
Systolic blood pressure, diastolic blood pressure and heart rates before and at 5 minutes after treatment (Mean±SD)
| Parameters | Interval | A+E+C | A+E |
|---|---|---|---|
| SBP | Before | 121.52±8.5 | 123.08±9.17 |
| After | 122.81±10.91 | 124.91±9.29 | |
| DBP | Before | 79.38±6.56 | 79.58±5.75 |
| After | 78.79±5.87 | 79.98±4.8 | |
| HR | Before | 79.06±9.12 | 80.42±9.65 |
| After | 79.60±6.42 | 81.81±7.76 * |
A: articaine, E: epinephrine, C: clonidine; SPB: systolic blood pressure, DBP: diastolic blood pressure, HR: heart rate; *P=0.03 compared to values before injection; Comparisons were non-significant in the parameters between groups (P>0.05)
Discussion
We assessed the efficacy of clonidine on post-operative pain management in patients with irreversible pulpitis in mandibular molars. In our randomized clinical trial, adhering to CONSORT guidelines we found that patients who received the clonidine solution had less post-operative pain than those that received only articaine/epinephrine solution. No significant differences in mean age, gender and initial pain between the two groups were found. This indicates that these two groups were comparable in terms of demographic factors and preoperative pain levels, thereby reducing the risk of bias of our study. From our results, we can confidently say that the addition of clonidine to the articaine/epinephrine local anaesthesia demonstrated the effectiveness of clonidine in reducing the severity of post-operative pain.
It is common knowledge that α2-adrenoceptors are located in the pre-synaptic terminal of afferent neurons and are involved in secretion of pain-mediating neurotransmitters [25]. Stimulation of these receptors leads to inhibition of substance P, which has a strong sensitizing effect on sensory nerves [26]. The stimulation of α2-adrenoceptors activates the descending inhibitory pathways and inhibits the secretion of pro-nociceptive mediators, directly effecting pain modulation [27]. Clonidine, an α2-adrenoceptor agonist, is able to reduce pain experienced by the dental patient. This may explain our results: the frequency of moderate and severe post-operative pain in the clonidine group was lower than the control group during most of the time intervals (6, 12, 48, and 72 h after the treatment).
Failure of IANBs is not uncommon in patients presenting with aching tooth, and post-operative pain management with irreversible pulpitis have been achieved by a direct supplemental infiltration of an adjunct or by addition of an adjunct into an anesthetic solution in order to enhance the anesthetic efficacy [28-30]. Clonidine has been used as an adjunct to enhance analgesia and post-operative pain control. Chakraborty et al. [15] found that adding 30 µg of clonidine to bupivacaine in a brachial plexus block on patients undergoing upper limb orthopedic surgery increased the duration of analgesia without any clinical complications. The results of this study are consistent with our findings, although the type of local anesthetic and the neural block performed were vastly different in terms of anatomy and treatment procedures. Unlike the present study, epinephrine was not included in the local anesthetic solution and a brachial plexus block was given with bupivacaine instead of articaine in IANB.
The results of the present study corroborate the finding of dental clinical trial [16]. In uncomplicated upper third molar extraction patients with hypertension, they found that adding 30 µg of clonidine to lidocaine for an intraoral block resulted in further post-operative pain relief, less analgesic consumption, and more hemodynamic stability, compared to epinephrine. Although their findings confirm clonidine’s efficacy in post-operative analgesia, it is important to note that our study used a combination of clonidine and a local anesthetic solution with epinephrine, while Patil et al. [17] used clonidine and epinephrine separately and compared the two. A similar study conducted by Brkovic et al. [16] added either clonidine or epinephrine to lidocaine in an IANB and also revealed that post-operative pain and the need for analgesics in the clonidine group were lower than the epinephrine group. This finding is consistent with of Patil et al. [17] and our randomized controled clinical trial. A study by Shadmehr et al. [11] that looked at intraoperative pain also backs our results. They compared clonidine to lidocaine/epinephrine in patients with irreversible pulpitis and showed that the addition of clonidine to lidocaine resulted in greater success of IANB and reduction in reporting severe pain incidence during procedure. However, Shadmehr et al. [11] evaluated intraoperative pain, while the present study assessed post-operative pain. They used lidocaine as an anesthetic of choice, we used articaine, however clonidine showed analgesic OR anesthetic efficacy in both [11].
Chowdhury et al. [15] reported results that differ from our study. They found that adding clonidine to lidocaine did not influence the pain intensity, while lowering blood pressure and heart rates. Their patients underwent removal of bilateral impacted third molars in mandible or maxilla (using IANB or infiltration due to the target jaw). This difference may be due to the small sample size of Chakraborty et al.’s study [15](30 patients) and possibly the different and more aggressive nature of the dental treatment and preoperative patient stress associated with extractions. They also used more different types of anesthetic solution than our study as the addition of either epinephrine or clonidine to a lidocaine solution was performed. Moreover, pain levels were measured intra-operatively with no post-operative pain assessment [31].
Articaine is an anesthetic agent that is commonly used in European countries for dental procedures [32] and was first used in the USA. Generally, amide anesthetics used in dental nerve blocks consist of an amide chain that connects a hydrophilic part to a lipophilic part. Instead of a benzene ring connected to the lipophilic part in other anesthetics, articaine has a thiophene ring which increases lipid solubility and therefore anaesthesia. This ring could also cause higher neurotoxicity and risk of paresthesia [8], although some animal and in vitro studies do not support this statement. Articaine has been shown to have a higher rate of neurotoxicity in comparison with other anesthetics [33, 34]. It is known to be more potent than lidocaine, especially in first molars [35]. The success rates of both mandibular block and infiltration anesthesia with articaine have been shown to be significantly greater than lidocaine [36]. Remarkably, articaine has proven itself more effective than lidocaine for supplementary infiltrations to an IANB in patients with irreversible pulpitis undergoing endodontic treatment [37]. Therefore, our study chose articaine as our anesthetic of choice in an attempt to find the best method to acquire adequate post-operative pain management after endodontic treatment.
In a clinical trial, Mel'nikova et al. [18] added a combination of clonidine and epinephrine to articaine in their pediatric patients and discovered less pain intensity and increased anesthesia duration in the children [18]. As their clinical trial involved pediatric patients, a lower concentration of clonidine was used. Also, they only assessed intraoperative pain instead of post-operative pain. However, the overwhelming data from these clinical trials point to the efficiency of clonidine in pain management (pre or post-operatively) when used adjunct to articaine.
The present study found that the addition of a low dose of 30 µg of clonidine did not affect hemodynamic factors. Epinephrine tends to cause an increase in heart rate and blood pressure via β1-receptor stimulation whereas clonidine, a commonly used antihypertensive agent, decreases heart rate and blood pressure as an α2-adrenoceptor agonist [17]. Therefore, we measured the change in hemodynamic factors, blood pressure and heart rate, to assess whether the addition of clonidine could prevent cardiotoxicity sometimes caused by 4% articaine with 1:100,000 epinephrine. Based on our findings, it appears that the use of low doses of clonidine with epinephrine in an articaine solution is not sufficient to cause noticeable changes in systolic and diastolic blood pressure.
Although this present study demonstrates the significant effectiveness of clonidine in pain management for patients undergoing endodontic treatment, some limitations need to be addressed. First, simple random sampling was used to select patients, which may have led to selection bias. Second, it is suggested that a similar study be performed using articaine added to clonidine in other age groups, as well as in other treatments.
Conclusion
Our randomized clinical trial study demonstrated effective reduction in post-operative pain in patients who presented in pain and underwent endodontic treatment when compared with control. The addition of 30 µg clonidine to 1.8 mL 4% articaine with1: 100,000 epinephrine solution in IANB anesthesia during root canal and other dental treatments should be seriously considered and further studied. Our low dose of clonidine did not cause any adverse complications including hypotension, drowsiness, dizziness, nausea, vomiting and headache.
Acknowledgment
This study is a thesis project for general dentistry, funded by the School of Dentistry, Isfahan University of Medical Sciences, Isfahan, Iran.
Conflict of Interest:
‘None declared’.
References
- 1.Gotler M, Bar-Gil B, Ashkenazi M. Postoperative pain after root canal treatment: a prospective cohort study. Int J Dent. 2012;2012:310467. doi: 10.1155/2012/310467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Law AS, Durand EU, Rindal DB, Nixdorf DR. "Doctor, why does my tooth still hurt"? Northwest Dent. 2010;89(1):33–6. [PMC free article] [PubMed] [Google Scholar]
- 3.Sadaf D, Ahmad MZ. Factors associated with postoperative pain in endodontic therapy. Int J Biomed Sci. 2014;10(4):243–7. [PMC free article] [PubMed] [Google Scholar]
- 4.Sathorn C, Parashos P, Messer H. The prevalence of postoperative pain and flare-up in single- and multiple-visit endodontic treatment: a systematic review. Int Endod J. 2008;41(2):91–9. doi: 10.1111/j.1365-2591.2007.01316.x. [DOI] [PubMed] [Google Scholar]
- 5.Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, Carter T, Cassidy CL, Chittenden EH, Degenhardt E, Griffith S, Manworren R, McCarberg B, Montgomery R, Murphy J. Management of Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131–57. doi: 10.1016/j.jpain.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 6.Allegretti CE, Sampaio RM, Horliana AC, Armonia PL, Rocha RG, Tortamano IP. Anesthetic Efficacy in Irreversible Pulpitis: A Randomized Clinical Trial. Braz Dent J. 2016;27(4):381–6. doi: 10.1590/0103-6440201600663. [DOI] [PubMed] [Google Scholar]
- 7.Paxton K, Thome DE. Efficacy of articaine formulations: quantitative reviews. Dent Clin North Am. 2010;54(4):643–53. doi: 10.1016/j.cden.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 8.Hopman AJG, Baart JA, Brand HS. Articaine and neurotoxicity – a review. British Dental Journal. 2017;223(7):501–6. doi: 10.1038/sj.bdj.2017.782. [DOI] [PubMed] [Google Scholar]
- 9.Mikesell P, Nusstein J, Reader A, Beck M, Weaver J. A comparison of articaine and lidocaine for inferior alveolar nerve blocks. J Endod. 2005;31(4):265–70. doi: 10.1097/01.don.0000140576.36513.cb. [DOI] [PubMed] [Google Scholar]
- 10.Ceccheti MM, Negrato GV, Peres MP, Deboni MC, Naclério-Homem Mda G. Analgesic and adjuvant anesthetic effect of submucosal tramadol after mandibular third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117(3):e249–54. doi: 10.1016/j.oooo.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 11.Shadmehr E, Aminozarbian MG, Akhavan A, Mahdavian P, Davoudi A. Anaesthetic efficacy of lidocaine/clonidine for inferior alveolar nerve block in patients with irreversible pulpitis. Int Endod J. 2017;50(6):531–9. doi: 10.1111/iej.12659. [DOI] [PubMed] [Google Scholar]
- 12.Jamali S, Monin S, Begon C, Dubousset AM, Ecoffey C. Clonidine in pediatric caudal anesthesia. Anesth Analg. 1994;78(4):663–6. doi: 10.1213/00000539-199404000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Singh M, Pathak A, Khan AL, Srivastava A, Negi D. Comparative Study of Clonidine with Ropivacaine versus Ropivacaine Alone in Epidural Anesthesia for Lower Limb Orthopedic Surgery. Anesth Essays Res. 2017;11(4):1035–9. doi: 10.4103/aer.AER_67_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hrishi AP, Rao G, Lionel KR. Efficacy of Clonidine as an Additive on the Duration of Action of Brachial Plexus Block Performed Under Ultrasound and Nerve Locator Guidance: A Prospective Randomized Study. Anesth Essays Res. 2019;13(1):105–10. doi: 10.4103/aer.AER_6_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chakraborty S, Chakrabarti J, Mandal MC, Hazra A, Das S. Effect of clonidine as adjuvant in bupivacaine-induced supraclavicular brachial plexus block: A randomized controlled trial. Indian J Pharmacol. 2010;42(2):74–7. doi: 10.4103/0253-7613.64498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brkovic B, Todorovic L, Stojic D. Comparison of clonidine and epinephrine in lidocaine anaesthesia for lower third molar surgery. Int J Oral Maxillofac Surg. 2005;34(4):401–6. doi: 10.1016/j.ijom.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 17.Patil PM, Patil SP. Is clonidine an adequate alternative to epinephrine as a vasoconstrictor in patients with hypertension? J Oral Maxillofac Surg. 2012;70(2):257–62. doi: 10.1016/j.joms.2011.07.011. [DOI] [PubMed] [Google Scholar]
- 18.Mel'nikova AV, Shugaĭlov IA, Garus Ia N. [Efficiency of teeth local anesthesia by articaine-containing formulation with adrenaline and clonidine in pediatric dentistry] Stomatologiia (Mosk) 2014;93(2):43–6. [PubMed] [Google Scholar]
- 19.Stefanac SJ. 8 - Acute phase of treatment. In: Stefanac SJ, editor. Diagnosis and Treatment Planning in Dentistry (Third Edition) St. Louis (MO): Mosby; 2017. pp. 173–91. [Google Scholar]
- 20.Sirintawat N, Sawang K, Chaiyasamut T, Wongsirichat N. Pain measurement in oral and maxillofacial surgery. J Dent Anesth Pain Med. 2017;17(4):253–63. doi: 10.17245/jdapm.2017.17.4.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Herring Fa. Illustrated Anatomy of the Head and Neck. 2012. p. 216. [Google Scholar]
- 22.Hosseini HR, Parirokh M, Nakhaee N, P VA, Samani S. Efficacy of Articaine and Lidocaine for Buccal Infiltration of First Maxillary Molars with Symptomatic Irreversible Pulpitis: A Randomized Double-blinded Clinical Trial. Iran Endod J. 2016;11(2):79–84. doi: 10.7508/iej.2016.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sakhaeimanesh V, Khazaei S, Kaviani N, Saatchi M, Shafiei M, Khademi A. Anesthetic Efficacy of Articaine and Ketamine for Inferior Alveolar Nerve Block in Symptomatic Irreversible Pulpitis: A Prospective Randomized Double-Blind Study. Iran Endod J. 2017;12(4):449–53. doi: 10.22037/iej.v12i4.16224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Talebzadeh B, Nezafati S, Rahimi S, Shahi S, Lotfi M, Ghasemi N. Comparison of manual and rotary instrumentation on postoperative pain in teeth with asymptomatic irreversible pulpitis: A randomized clinical trial. Iran Endod J. 2016;11(4) doi: 10.22037/iej.2016.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carroll I, Mackey S, Gaeta R. The role of adrenergic receptors and pain: The good, the bad, and the unknown. Seminars in Anesthesia, Perioperative Medicine and Pain. 2007;26(1):17–21. [Google Scholar]
- 26.Kuraishi Y, Hirota N, Sato Y, Kaneko S, Satoh M, Takagi H. Noradrenergic inhibition of the release of substance P from the primary afferents in the rabbit spinal dorsal horn. Brain Res. 1985;359(1-2):177–82. doi: 10.1016/0006-8993(85)91426-x. [DOI] [PubMed] [Google Scholar]
- 27.Neil MJ. Clonidine: clinical pharmacology and therapeutic use in pain management. Curr Clin Pharmacol. 2011;6(4):280–7. doi: 10.2174/157488411798375886. [DOI] [PubMed] [Google Scholar]
- 28.Yavari HR, Jafari F, Jamloo H, Hallaj-Nezhadi S, Jafari S. The Effect of Submucosal Injection of Corticosteroids on Pain Perception and Quality of Life after Root Canal Treatment of Teeth with Irreversible Pulpitis: A Randomized Clinical Trial. J Endod. 2019;45(5):477–82. doi: 10.1016/j.joen.2019.01.005. [DOI] [PubMed] [Google Scholar]
- 29.Kreimer T, Kiser R, 2nd , Reader A, Nusstein J, Drum M, Beck M. Anesthetic efficacy of combinations of 0 5 mol/L mannitol and lidocaine with epinephrine for inferior alveolar nerve blocks in patients with symptomatic irreversible pulpitis. J Endod. 2012;38(5):598–603. doi: 10.1016/j.joen.2012.02.016. [DOI] [PubMed] [Google Scholar]
- 30.Bigby J, Reader A, Nusstein J, Beck M. Anesthetic efficacy of lidocaine/meperidine for inferior alveolar nerve blocks in patients with irreversible pulpitis. J Endod. 2007;33(1):7–10. doi: 10.1016/j.joen.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 31.Chowdhury S, Singh M, Shah A. Efficacy of lignocaine with clonidine and adrenaline in minor oral surgical procedure. Contemp Clin Dent. 2012;3(2):227–9. doi: 10.4103/0976-237X.96839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oertel R, Rahn R, Kirch W. Clinical pharmacokinetics of articaine. Clin Pharmacokinet. 1997;33(6):417–25. doi: 10.2165/00003088-199733060-00002. [DOI] [PubMed] [Google Scholar]
- 33.Malet A, Faure MO, Deletage N, Pereira B, Haas J, Lambert G. The comparative cytotoxic effects of different local anesthetics on a human neuroblastoma cell line. Anesth Analg. 2015;120(3):589–96. doi: 10.1213/ANE.0000000000000562. [DOI] [PubMed] [Google Scholar]
- 34.Baroni DB, Franz-Montan M, Cogo K, Berto LA, Volpato MC, Novaes PD, Groppo FC. Effect of articaine on mental nerve anterior portion: histological analysis in rats. Acta Odontol Scand. 2013;71(1):82–7. doi: 10.3109/00016357.2011.654243. [DOI] [PubMed] [Google Scholar]
- 35.Katyal V. The efficacy and safety of articaine versus lignocaine in dental treatments: a meta-analysis. J Dent. 2010;38(4):307–17. doi: 10.1016/j.jdent.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 36.Brandt RG, Anderson PF, McDonald NJ, Sohn W, Peters MC. The pulpal anesthetic efficacy of articaine versus lidocaine in dentistry: a meta-analysis. J Am Dent Assoc. 2011;142(5):493–504. doi: 10.14219/jada.archive.2011.0219. [DOI] [PubMed] [Google Scholar]
- 37.Kung J, McDonagh M, Sedgley CM. Does Articaine Provide an Advantage over Lidocaine in Patients with Symptomatic Irreversible Pulpitis? A Systematic Review and Meta-analysis. J Endod. 2015;41(11):1784–94. doi: 10.1016/j.joen.2015.07.001. [DOI] [PubMed] [Google Scholar]